Alora
Alora (Estradiol Transdermal System, USP)Continuous Delivery for Twice Weekly DosingRevised: November 2013Rx only200178-12Prescribing Information With Attached Patient Information Leaflet
FULL PRESCRIBING INFORMATION: CONTENTS*
- ALORA DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL STUDIES
- ALORA INDICATIONS AND USAGE
- ALORA CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- ALORA ADVERSE REACTIONS
- OVERDOSAGE
- ALORA DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PATIENT INFORMATION
FULL PRESCRIBING INFORMATION
|
Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is currently no evidence that the use of “natural” estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose [see WARNINGS, Malignant Neoplasms, Endometrial cancer].
CARDIOVASCULAR AND OTHER RISKS The Women’s Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo [see CLINICAL PHARMACOLOGY and CLINICAL STUDIES and WARNINGS , Cardiovascular Disorders and Malignant Neoplasms, Breast cancer ]. The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens plus medroxyprogesterone acetate relative to placebo. It is unknown whether this finding applies to younger postmenopausal women [see CLINICAL PHARMACOLOGY and CLINICAL STUDIES and WARNINGS, Dementia and PRECAUTIONS, Geriatric Use .) Other doses of oral conjugated estrogens with medroxyprogesterone acetate, and other combinations and dosage forms of estrogens and progestins were not studied in the WHI clinical trials and, in the absence of comparable data, these risks should be assumed to be similar. Because of these risks, estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman. |
ALORA DESCRIPTION
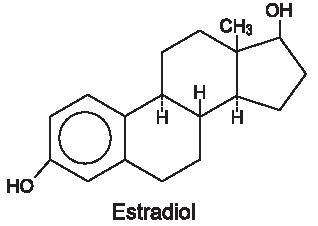
Alora (Estradiol Transdermal System, USP) is designed to deliver estradiol continuously and consistently over a 3 or 4-day interval upon application to intact skin. Four strengths of Alora are available, having nominal in vivo delivery rates of 0.025, 0.05, 0.075, and 0.1 mg estradiol per day through skin of average permeability (inter-individual variation in skin permeability is approximately 20%). Alora has contact surface areas of 9 cm2, 18 cm2, 27 cm2, and 36 cm2 and contains 0.77, 1.5, 2.3, and 3.1 mg of estradiol, USP, respectively. The composition of the estradiol transdermal systems per unit area is identical. Estradiol, USP is a white, crystalline powder that is chemically described as estra-1,3,5(10)-triene-3, 17β-diol, has an empirical formula of C18H24O2 and has molecular weight of 272.39. The structural formula is:
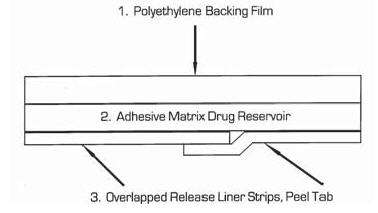
Alora consists of three layers. Proceeding from the polyethylene backing film as shown in the cross-sectional view below, the adhesive matrix drug reservoir that is in contact with the skin consists of estradiol, USP and sorbitan monooleate dissolved in an acrylic adhesive matrix. The polyester overlapped release liner protects the adhesive matrix during storage and is removed prior to application of the system to the skin.
Product meets USP Drug Release Test 3.
CLINICAL PHARMACOLOGY
Endogenous estrogens are largely responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Although circulating estrogens exist in a dynamic equilibrium of metabolic interconversions, estradiol is the principal intracellular human estrogen and is substantially more potent than its metabolites, estrone and estriol, at the receptor level. The primary source of estrogen in normally cycling adult women is the ovarian follicle, which secretes 70 to 500 mcg of estradiol daily, depending on the phase of the menstrual cycle. After menopause, most endogenous estrogen is produced by conversion of androstenedione, secreted by the adrenal cortex, to estrone by peripheral tissues. Thus, estrone and the sulfate conjugated form, estrone sulfate, are the most abundant circulating estrogens in postmenopausal women.
Estrogens act through binding to nuclear receptors in estrogen-responsive tissues. To date, two estrogen receptors have been identified. These vary in proportion from tissue to tissue. Circulating estrogens modulate the pituitary secretion of the gonadotropins, luteinizing hormone (LH) and follicle stimulating hormone (FSH) through a negative feedback mechanism. Estrogens act to reduce the elevated levels of these hormones seen in postmenopausal women.
Pharmacokinetics
The skin metabolizes estradiol only to a small extent. In contrast, orally administered estradiol is rapidly metabolized by the liver to estrone and its conjugates, giving rise to higher circulating levels of estrone than estradiol. Therefore, transdermal administration produces therapeutic plasma levels of estradiol with lower levels of estrone and estrone conjugates and requires smaller total doses than does oral therapy.
Estradiol is transported across intact skin and into the systemic circulation by a passive diffusion process, the rate of diffusion across the stratum corneum being the principal factor. Alora presents sufficient concentration of estradiol to the surface of the skin to maintain continuous transport over the 3 to 4 day dosing interval.
Direct measurement of total absorbed dose of estradiol through analysis of residual estradiol content of systems worn over a continuous 4-day interval during 251 separate occasions in 123 postmenopausal women demonstrated that the average daily dose absorbed from Alora was 0.003 ± 0.001 mg estradiol per cm2 active surface area. The nominal mean in vivo daily delivery rates of estradiol calculated from these data are 0.027 mg/day, 0.054 mg/day, 0.081 mg/day, and 0.11 mg/day for the 9 cm2, 18 cm2, 27 cm2, and 36 cm2 Alora, respectively.
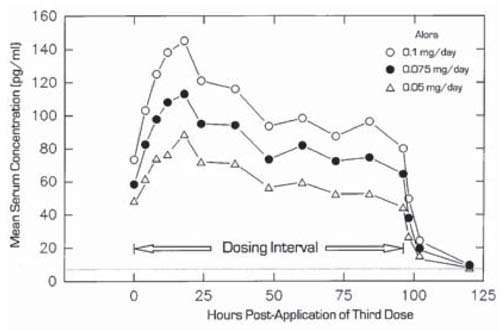
In another study, 20 women also were treated with three consecutive doses of Alora 0.05 mg/day, Alora 0.075 mg/day and Alora 0.1 mg/day on abdominal application sites. Mean steady-state estradiol serum concentrations observed over the dosing interval are shown in Figure 1.
Figure 1
Mean steady-state estradiol serum concentration during the third twice weekly dose of Alora 0.1 mg/day, Alora 0.075 mg/day, and Alora 0.05 mg/day in 20 postmenopausal women.
In a single dose randomized crossover study conducted to compare the effect of site of Alora application, 31 postmenopausal women wore single Alora 0.05 mg/day for 4-day periods on the lower abdomen, upper quadrant of the buttocks, and outside aspect of the hip. The estradiol serum concentration profiles are shown in Figure 2.
Figure 2
Mean estradiol serum concentrations during a single 4-day wearing of Alora 0.05 mg/day applied by 31 postmenopausal women to the lower abdomen, upper quadrant of the buttocks or outer aspect of the hip.

* Cmax and Cavg statistically different from abdomen
Table 1 provides a summary of the estradiol pharmacokinetic parameters studied during biopharmaceutic evaluation of Alora.
| Alora (mg/day) |
Application Site |
|
Dosing |
Cmax
(pg/ml) |
Cmin
(pg/ml) |
Cavg
(pg/ml) |
CL |
| 0.05 | Abdomen | 20 | Multiple | 92 (33) | 43 (12) | 64 (19) | 54 (18) |
| 0.075 | Abdomen | 20 | Multiple | 120 (60) | 53 (23) | 86 (40) | 53 (12) |
| 0.1 | Abdomen | 42 | Multiple | 144 (57) | 58 (20) | 98 (38) | 61 (18) |
| 0.05 | Abdomen | 31 | Single | 53 (23) | - | 41 (18) | 69 (22) |
| Buttock | 31 | Single | 67 (45) | - | 45 (21) | 66 (23) | |
| Hip* | 31 | Single | 69 (30) | - | 48 (17) | 62 (18) |
*Cmax and Cavg statistically different from abdomen
Steady-state estradiol serum concentrations were measured in two well-controlled clinical trials in the treatment of menopausal symptoms of 3 month duration (Studies 1 and 2), and one trial in the prevention of postmenopausal osteoporosis of 2 year duration (Study 3). Table 2 provides a summary of these data.
| Alora
(mg/day) |
Study 1 | Study 2 | Study 3 |
| 0.025 | - | - | 24.5 (12.4) |
| 0.05 | 46.9 (38.5) | 38.8 (38.0) | 42.6 (23.7) |
| 0.075 | - | - | 56.7 (36.8) |
| 0.1 | 99.2 (77.0) | 97.0 (87.5) | - |
In a 2-year, randomized, double-blind, placebo-controlled, prevention of postmenopausal osteoporosis study in 355 hysterectomized women, the average baseline-adjusted steady-state estradiol serum concentrations were 18.6 pg/ml (45 patients) for the 0.025 mg/day dose, 35.9 pg/ml (47 patients) for the 0.05 mg/day dose, and 50.1 pg/ml (46 patients) for the 0.075 mg/day dose. These values were linearly related and dose proportional.
No specific investigation of the tissue distribution of estradiol absorbed from Alora in humans has been conducted. The distribution of exogenous estrogens is similar to that of endogenous estrogens. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs. Estrogens circulate in the blood largely bound to sex hormone binding globulin (SHBG) and albumin.
Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women a significant portion of the circulating estrogens exists as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.
Estradiol, estrone and estriol are excreted in the urine along with glucuronide and sulfate conjugates. The apparent mean (SD) serum half-life of estradiol determined from biopharmaceutic studies conducted with Alora is 1.75 ± 2.87 hours.
Special Populations
Alora has been studied only in healthy postmenopausal women (approximately 90% Caucasian). There are no long term studies in postmenopausal women with an intact uterus. No pharmacokinetic studies were conducted in other special populations, including patients with renal or hepatic impairment.
Drug Interactions
In vitro and in vivo studies have shown that estrogens are metabolized partially by cytochrome P450 3A4 (CYP3A4). Therefore, inducers or inhibitors of CYP3A4 may affect estrogen drug metabolism. Inducers of CYP3A4 such as St. John’s Wort preparations (Hypericum perforatum), phenobarbital, phenytoin, carbamazepine, rifampin and dexamethasone may reduce plasma concentrations of estrogens, possibly resulting in a decrease in therapeutic effects and/or changes in the uterine bleeding profile. Inhibitors of CYP3A4 such as cimetidine, erythromycin, clarithromycin, ketoconazole, itraconazole, ritonavir, and grapefruit juice may increase plasma concentrations of estrogens and may result in side effects.
Adhesion
The adhesion potential of Alora was evaluated in a randomized clinical trial involving 408 healthy postmenopausal women who wore placebo systems corresponding to the 18 cm2 size Alora. The placebos were applied twice weekly for 4 weeks on the lower quadrant of the abdomen. It should be noted that the lower abdomen, the upper quadrant of the buttocks or outer aspect of the hip are the approved sites of application for Alora. Subjects were instructed not to do strenuous activities, take baths, use hot tubs or swim. In 968 observations, there was a partial or complete adhesion rate of approximately 97%. The total detachment rate was approximately 3%. Adhesion potentials of the 9 cm2, 27 cm2 and 36 cm2 sizes of Alora have not been studied.
CLINICAL STUDIES
Efficacy of Alora has been studied in a double blind/double dummy, randomized, parallel group, placebo-controlled trial involving a total of 268 postmenopausal women over a 12-week dosing period. Only women having estradiol and FSH serum concentrations in the postmenopausal range and who exhibited a weekly average of at least 60 moderate to severe hot flushes during the screening period were enrolled in the studies.
Patients received Alora 0.05 mg/day and a placebo system, or Alora 0.1 mg/day and a placebo system, or two placebo systems dosed twice weekly over a 12-week duration. Measures of efficacy included mean reduction in weekly number of moderate to severe vasomotor symptoms when compared to the mean baseline average determined during a 2-week pre-dosing screening period. Alora was shown to be statistically better than placebo at Weeks 4 and 12 for relief of both the frequency (see Table 3) and severity of vasomotor symptoms.
| Mean Change from Baseline | |||
| Week of Therapy | Alora 0.05 mg/day N = 87 Baseline = 90 |
Alora 0.1 mg/day N = 91 Baseline = 85 |
Placebo N = 90 Baseline = 92 |
4 |
-57 | -70 | -45 |
| 8 | -65 | -77 | -49 |
12 |
-68 | -79 | -54 |
Vaginal cytology was obtained pre-dosing and at last visit in 54 women treated with Alora 0.05 mg/day, in 45 women treated with Alora 0.1 mg/day, and in 46 women in the placebo group. Superficial cells increased by a mean of 18.7%, 23.7%, and 8.7% for the Alora 0.05 mg/day, Alora 0.1 mg/day, and placebo groups, respectively. Corresponding reductions in basal/parabasal and intermediate cells were also observed.
Lumbar spine bone mineral density (BMD) was measured by DEXA in a 2-year, randomized, multi-center, double-blind, placebo-controlled study in 355 hysterectomized, non-osteoporotic women (i.e., T-scores > -2.5). Eighty-six percent of the women were Caucasian, the mean age was 53.2 years (range 26 to 69), and the average number of years since menopause (natural or surgical) was not determined. Three Alora doses (0.025 mg/day, 0.05 mg/day, and 0.075 mg/day) were compared to placebo in terms of the % change in BMD from baseline to Year 2. The systems were applied every 3 or 4 days on alternate sides of the lower abdomen. All patients received 1000 mg of oral elemental calcium daily. The average baseline lumbar spine T-score was -0.64 (range -2.7 to 3.8). The % changes in BMD from baseline are illustrated in Figure 3.
Figure 3
Mean % change in BMD from baseline at 1 and 2 years after initiation of therapy with Placebo and Alora 0.025, 0.05, and 0.075 mg/day in the completer and intent-to-treat population with last observation carried forward (LOCF)
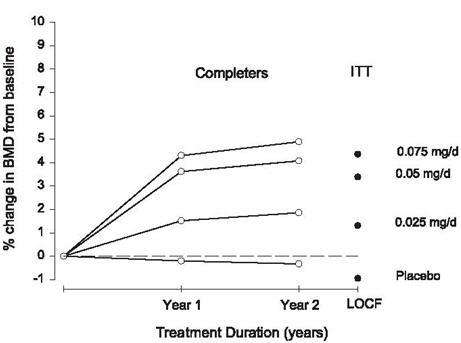
A total of 196 patients (44 – 0.025 mg/d, 49 – 0.05 mg/d, 45 – 0.075 mg/d, and 58 – placebo) were included in the completer population compared with 258 patients (59 – 0.025 mg/d, 64 – 0.05 mg/d, 63 – 0.075 mg/d, and 72 – placebo) in the intent-to-treat, last observation carried forward population.
All Alora doses were statistically superior to placebo for the primary endpoint, percent change in BMD from baseline. The mean 2-year (LOCF) percent changes in BMD for 0.025 mg/d, 0.05 mg/d, 0.075 mg/d, and placebo were 1.45%, 3.39%, 4.24%, and –0.80% respectively.
The Women’s Health Initiative (WHI) enrolled a total of 27,000 predominantly healthy postmenopausal women to assess the risks and benefits of either the use of 0.625 mg conjugated estrogens (CE) per day alone or the use of oral 0.625 mg conjugated estrogens plus 2.5 mg medroxyprogesterone acetate (MPA) per day compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of coronary heart disease (CHD) [nonfatal myocardial infarction and CHD death], with invasive breast cancer as the primary adverse outcome studied. A “global index” included the earliest occurrence of CHD, invasive breast cancer, stroke, pulmonary embolism (PE), endometrial cancer, colorectal cancer, hip fracture, or death due to other cause. The study did not evaluate the effects of CE or CE/MPA on menopausal symptoms.
The CE/MPA substudy was stopped early because, according to the predefined stopping rule, the increased risk of breast cancer and cardiovascular events exceeded the specified benefits included in the “global index.” Results of the CE/MPA substudy, which included 16,608 women (average age of 63 years, range 50 to 79; 83.9% White, 6.5% Black, 5.5% Hispanic), after an average follow-up of 5.2 years are presented in Table 4 below:
| Eventc | Relative Risk CE/MPA vs placebo at 5.2 years (95% CI*) | Placebo n=8102 |
CE/MPA n=8506 |
|
| Absolute Risk per 10,000 Person-years |
||||
| CHD events | 1.29 (1.02-1.63) | 30 | 37 | |
| Non-fatal MI | 1.32 (1.02-1.72) | 23 | 30 | |
| CHD death | 1.18 (0.70-1.97) | 6 | 7 | |
| Invasive breast cancerb | 1.26 (1.00-1.59) | 30 | 38 | |
| Stroke | 1.41 (1.07-1.85) | 21 | 29 | |
| Pulmonary embolism | 2.13 (1.39-3.25) | 8 | 16 | |
| Colorectal cancer | 0.63 (0.43-0.92) | 16 | 10 | |
| Endometrial cancer | 0.83 (0.47-1.47) | 6 | 5 | |
| Hip fracture | 0.66 (0.45-0.98) | 15 | 10 | |
| Death due to causes other than the events above | 0.92 (0.74-1.14) | 40 | 37 | |
| Global Indexc | 1.15 (1.03-1.28) | 151 | 170 | |
| Deep vein thrombosisd | 2.07 (1.49-2.87) | 13 | 26 | |
| Vertebral fracturesd | 0.66 (0.44-0.98) | 15 | 9 | |
| Other osteoporotic fracturesd | 0.77 (0.69-0.86) | 170 | 131 | |
a adapted from JAMA, 2002; 288:321-333
b includes metastatic and non-metastatic breast cancer with the exception of in situ breast cancer
c a subset of the events was combined in a “global index”, defined as the earliest occurrence of CHD events, invasive breast cancer, stroke, pulmonary embolism, endometrial cancer, colorectal cancer, hip fracture, or death due to other causes
d not included in Global Index
* normal confidence intervals unadjusted for multiple looks and multiple comparisons
For those outcomes included in the “global index,” absolute excess risks per 10,000 person-years in the group treated with CE/MPA were 7 more CHD events, 8 more strokes, 8 more PEs, and 8 more invasive breast cancers, while absolute risk reductions per 10,000 women-years were 6 fewer colorectal cancers and 5 fewer hip fractures. The absolute excess risk of events included in the “global index” was 19 per 10,000 women-years. There was no difference between the groups in terms of all-cause mortality [see
BOXED WARNINGS
,
WARNINGS
, and
PRECAUTIONS
].
The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, enrolled 4,532 predominantly healthy postmenopausal women 65 years of age and older (47% were age 65 to 69 years, 35% were 70 to 74 years, and 18% were 75 years of age and older) to evaluate the effects of CE/MPA (0.625 mg conjugated estrogens plus 2.5 mg medroxyprogesterone acetate) on the incidence of probable dementia (primary outcome) compared with placebo.
After an average follow-up of 4 years, 40 women in the estrogen/progestin group (45 per 10,000 women-years) and 21 in the placebo group (22 per 10,000 women-years) were diagnosed with probable dementia. The relative risk of probable dementia in the hormone therapy group was 2.05 (95% CI, 1.21 to 3.48) compared to placebo. Differences between groups became apparent in the first year of treatment. It is unknown whether these findings apply to younger postmenopausal women [see BOXED WARNINGS and WARNINGS, Dementia , and PRECAUTIONS, Geriatric Use ].
ALORA INDICATIONS AND USAGE
Alora is indicated in:
-
Treatment of moderate to severe vasomotor symptoms associated with the menopause.
-
Treatment of moderate to severe symptoms of vulvar and vaginal atrophy associated with the menopause. When prescribing solely for the treatment of symptoms of vulvar and vaginal atrophy, topical vaginal products should be considered.
-
Treatment of hypoestrogenism due to hypogonadism, castration or primary ovarian failure.
-
Prevention of postmenopausal osteoporosis. When prescribing solely for the prevention of postmenopausal osteoporosis, therapy should only be considered for women at significant risk of osteoporosis and non-estrogen medications should be carefully considered.
The mainstays for decreasing the risk of postmenopausal osteoporosis are weight bearing exercise, adequate calcium and vitamin D intake, and, when indicated, pharmacologic therapy. Postmenopausal women require an average of 1500 mg/day of elemental calcium to remain in neutral calcium balance. Therefore, when not contraindicated, calcium supplementation may be helpful for women with suboptimal dietary intake. Vitamin D supplementation of 400-800 IU/day may also be required to ensure adequate daily intake in postmenopausal women.
ALORA CONTRAINDICATIONS
Alora should not be used in individuals with any of the following conditions:
-
Undiagnosed abnormal genital bleeding.
-
Known, suspected, or history of cancer of the breast.
-
Known or suspected estrogen-dependent neoplasia.
-
Active deep vein thrombosis, pulmonary embolism or a history of these conditions.
-
Active or recent (e.g., within the past year) arterial thromboembolic disease (e.g., stroke, myocardial infarction).
-
Liver dysfunction or disease.
-
Alora should not be used in patients with known hypersensitivity to its ingredients.
-
Known or suspected pregnancy. There is no indication for Alora in pregnancy. There appears to be little or no increased risk of birth defects in children born to women who have used estrogens and progestins from oral contraceptives inadvertently during early pregnancy (see PRECAUTIONS).
WARNINGS
See BOXED WARNINGS.
The use of unopposed estrogens in women who have a uterus is associated with an increased risk of endometrial cancer.
1. Cardiovascular Disorders.
Estrogen and estrogen/progestin therapies have been associated with an increased risk of cardiovascular events such as myocardial infarction and stroke, as well as venous thrombosis and pulmonary embolism (venous thromboembolism or VTE). Should any of these occur or be suspected, estrogens should be discontinued immediately.
Risk factors for arterial vascular disease (e.g., hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and obesity) and/or venous thromboembolism (e.g., personal history or family history of VTE, obesity, and systemic lupus erythematosus) should be managed appropriately.
Coronary heart disease and stroke. In the Women’s Health Initiative (WHI) study an increased risk of stroke was observed in women receiving CE compared to placebo.
In the CE/MPA substudy of WHI an increased risk of coronary heart disease (CHD) events (defined as non-fatal myocardial infarction and CHD death) was observed in women receiving CE/MPA compared to women receiving placebo (37 vs. 30 per 10,000 women-years). The increase in risk was observed in Year 1 and persisted.
In the same substudy of WHI, an increased risk of stroke was observed in women receiving CE/MPA compared to women receiving placebo (29 vs. 21 per 10,000 women-years). The increase in risk was observed after the first year and persisted [see CLINICAL PHARMACOLOGY , and CLINICAL STUDIES ].
In postmenopausal women with documented heart disease (n=2,763, average age 66.7 years) a controlled clinical trial of secondary prevention of cardiovascular disease (Heart and Estrogen/ Progestin Replacement Study; (HERS)) treatment with CE/MPA–0.625 mg/2.5 mg per day demonstrated no cardiovascular benefit. During an average follow-up of 4.1 years, treatment with CE/MPA did not reduce the overall rate of CHD events in postmenopausal women with established coronary heart disease. There were more CHD events in the CE/MPA-treated group than in the placebo group in Year 1, but not during the subsequent years. Participation in an open label extension of the original HERS trial (HERS II) was agreed to by 2,321 women. Average follow-up in HERS II was an additional 2.7 years, for a total of 6.8 years overall. Rates of CHD events were comparable among women in the CE/MPA group and the placebo group in HERS, HERS II, and overall.
Large doses of estrogen (5 mg conjugated estrogens per day), comparable to those used to treat cancer of the prostate and breast, have been shown in a large prospective clinical trial in men to increase the risks of nonfatal myocardial infarction, pulmonary embolism, and thrombophlebitis.
Venous thromboembolism (VTE). In the Women’s Health Initiative (WHI) study, an increased risk of deep vein thrombosis was observed in women receiving CE compared to placebo.
In the CE/MPA substudy of WHI, a 2-fold greater rate of VTE, including deep venous thrombosis and pulmonary embolism, was observed in women receiving CE/MPA compared to women receiving placebo. The rate of VTE was 34 per 10,000 women-years in the CE/MPA group compared to 16 per 10,000 women-years in the placebo group. The increase in VTE risk was observed during the first year and persisted [see CLINICAL PHARMACOLOGY , and CLINICAL STUDIES ].
If feasible, estrogens should be discontinued at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism, or during periods of prolonged immobilization.
2. Malignant Neoplasms.
a.
The use of unopposed estrogens in women with intact uteri has been associated with an increased risk of endometrial cancer. The reported endometrial cancer risk among unopposed estrogen users is about 2 to 12-fold greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than 1 year. The greatest risk appears associated with prolonged use, with increased risks of 15 to 24-fold for 5 to 10 years or more, and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued.
Clinical surveillance of all women taking estrogen/progestin combinations is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer.
The use of estrogens and progestins by postmenopausal women has been reported to increase the risk of breast cancer. The most important randomized clinical trial providing information about this issue is the WHI substudy of CE/MPA [see CLINICAL PHARMACOLOGY , and CLINICAL STUDIES ]. The results from observational studies are generally consistent with those of the WHI clinical trial and report no significant variation in the risk of breast cancer among different estrogens or progestins, doses, or routes of administration.
The CE/MPA substudy of WHI reported an increased risk of breast cancer in women who took CE/MPA for a mean follow-up of 5.6 years. Observational studies have also reported an increased risk for estrogen/progestin combination therapy, and a smaller increased risk for estrogen alone therapy, after several years of use. In the WHI trial and from observational studies, the excess risk increased with duration of use. From observational studies, the risk appeared to return to baseline in about 5 years after stopping treatment. In addition, observational studies suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen/progestin combination therapy as compared to estrogen alone therapy.
In the CE/MPA substudy, 26% of the women reported prior use of estrogen alone and/or estrogen/progestin combination hormone therapy. After a mean follow-up of 5.6 years during the clinical trial, the overall relative risk of invasive breast cancer was 1.24 (95% confidence interval 1.01 - 1.54), and the overall absolute risk was 41 vs. 33 cases per 10,000 women-years, for CE/MPA compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86, and the absolute risk was 46 vs. 25 cases per 10,000 women-years, for CE/MPA compared with placebo. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09, and the absolute risk was 40 vs. 36 cases per 10,000 women-years for CE/MPA compared with placebo. In the same substudy, invasive breast cancers were larger and diagnosed at a more advanced stage in the CE/MPA group compared with the placebo group. Metastatic disease was rare with no apparent difference between the two groups. Other prognostic factors such as histologic subtype, grade and hormone receptor status did not differ between the groups.
The use of estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation. All women should receive yearly breast examinations by a healthcare provider and perform monthly self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.
3. Dementia.
In the estrogen plus progestin WHIMS, a population of 4,532 postmenopausal women aged 65 to 79 years was randomized to CE/MPA or placebo. After an average follow-up of 4 years, 40 women being treated with CE/MPA (1.8%, n=2,229) and 21 women in the placebo group (0.9%, n=2,303) received diagnoses of probable dementia. The relative risk for CE/MPA versus placebo was 2.05 (95% confidence interval 1.21 - 3.48), and was similar for women with and without histories of menopausal hormone use before WHIMS. The absolute risk of probable dementia for CE/MPA versus placebo was 45 vs. 22 cases per 10,000 women-years and the absolute excess risk for CE/MPA was 23 cases per 10,000 women-years. It is unknown whether these findings apply to younger postmenopausal women [see CLINICAL PHARMACOLOGY , CLINICAL STUDIES and PRECAUTIONS, Geriatric Use ].
4. Gallbladder Disease.
A 2 to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal women receiving estrogens has been reported.
5. Hypercalcemia.
Estrogen administration may lead to severe hypercalcemia in patients with breast cancer and bone metastases. If hypercalcemia occurs, use of the drug should be stopped and appropriate measures should be taken to reduce the serum calcium level.
6. Visual Abnormalities.
Retinal vascular thrombosis has been reported in patients receiving estrogens. Discontinue medication pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia, or migraine. If examination reveals papilledema or retinal vascular lesions, estrogens should be discontinued.
PRECAUTIONS
Studies of the addition of a progestin for 10 or more days of a cycle of estrogen administration, or daily with estrogen in a continuous regimen, have reported a lowered incidence of endometrial hyperplasia than would be induced by estrogen treatment alone. Endometrial hyperplasia may be a precursor to endometrial cancer.
There are, however, possible risks that may be associated with the use of progestins with estrogens compared to estrogen-alone regimens. These include:
-
A possible increased risk of breast cancer
-
Adverse effects on lipoprotein metabolism (e.g., lowering HDL, raising LDL)
-
Impairment of glucose tolerance
In a small number of case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. Blood pressure should be monitored at regular intervals with estrogen use.
In patients with pre-existing hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis and other complications.
Estrogens may be poorly metabolized in patients with impaired liver function. For patients with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, caution should be exercised and in the case of recurrence, medication should be discontinued.
Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. Patients with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T4 and T3 serum concentrations in the normal range. Patients dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. These patients should have their thyroid function monitored in order to maintain their free thyroid hormone levels in an acceptable range.
Because estrogens may cause some degree of fluid retention, conditions which might be influenced by this factor, such as patients with asthma, epilepsy, migraine, and cardiac or renal dysfunction, warrant careful observation when estrogens are prescribed.
The CE/MPA substudy of WHI reported that estrogen plus progestin increased the risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for CE/MPA vs. placebo was 1.58 (95% confidence interval 0.77-3.24) but was not statistically significant. The absolute risk for CE/MPA vs. placebo was 4.2 vs. 2.7 cases per 10,000 women-years. In some epidemiologic studies, the use of estrogen alone, in particular for ten or more years, has been associated with an increased risk of ovarian cancer. Other epidemiologic studies have not found these associations.
Endometriosis may be exacerbated with administration of estrogens. A few cases of malignant transformation of residual endometrial implants have been reported in women treated post-hysterectomy with estrogen alone therapy. For patients known to have residual endometriosis post-hysterectomy, the addition of progestin should be considered.
Estrogens should be used with caution in individuals with severe hypocalcemia.
Estrogens may cause an exacerbation of asthma, diabetes mellitus, epilepsy, migraine, porphyria, systemic lupus erythematosus, and hepatic hemangiomas and should be used with caution in women with these conditions.
B. Patient Information
See text of Patient Information. Physicians are advised to discuss the PATIENT INFORMATION leaflet with patients for whom they prescribe Alora.
C. Laboratory Tests
Estrogen administration should be guided by clinical response at the lowest dose for the treatment of vasomotor symptoms and vulvar and vaginal atrophy. Laboratory parameters may be useful in guiding dosage for the treatment of hypoestrogenism due to hypogonadism, castration and primary ovarian failure.
D. Drug/Laboratory Test Interactions
-
Accelerated prothrombin time, partial thromboplastin time, and platelet aggregation time; increased platelet count; increased factors II, VII antigen, VIII antigen, VIII coagulant activity, IX, X, XII, VII-X complex, II-VII-X complex, and beta-thromboglobulin; decreased levels of anti-factor Xa and antithrombin III, decreased antithrombin III activity; increased levels of fibrinogen and fibrinogen activity; increased plasminogen antigen and activity.
-
Increased thyroid-binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 levels (by column or by radioimmunoassay) or T3 levels by radioimmunoassay. T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Patients on thyroid replacement therapy may require higher doses of thyroid hormone.
-
Other binding proteins may be elevated in serum, i.e., corticosteroid binding globulin (CBG), sex hormone-binding globulin (SHBG), leading to increased circulating corticosteroids and sex steroids, respectively. Free hormone concentrations may be decreased. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-1-antitrypsin, ceruloplasmin).
-
Increased plasma HDL and HDL2 cholesterol subfraction concentrations, reduced LDL cholesterol concentration, increased triglycerides levels.
-
Impaired glucose tolerance.
-
Reduced response to the metyrapone test.
E. Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term continuous administration of natural and synthetic estrogens in certain animal species increases the frequency of carcinomas of the breast, uterus, cervix, vagina, testis, and liver.
Long-term continuous administration of estrogen, with or without progestin, in women with or without a uterus, has shown an increased risk of endometrial cancer, breast cancer, and ovarian cancer. ( See BOXED WARNINGS, WARNINGS, and PRECAUTIONS.)
F. Pregnancy Category X
Alora should not be used during pregnancy [see CONTRAINDICATIONS ].
G. Nursing Mothers
Estrogen administration to nursing mothers has been shown to decrease the quantity and quality of the milk. Detectable amounts of estrogens have been identified in the milk of mothers receiving estrogen therapy. Estrogens are not indicated for the prevention of postpartum breast engorgement. Caution should be exercised when Alora is administered to a nursing woman.
H. Pediatric Use
Estrogen replacement therapy has been used for the induction of puberty in adolescents with some forms of pubertal delay. Safety and effectiveness in pediatric patients have not otherwise been established.
Large and repeated doses of estrogen over an extended time period have been shown to accelerate epiphyseal closure, which could result in short adult stature if treatment is initiated before the completion of physiologic puberty in normally developing children. If estrogen is administered to patients whose bone growth is not complete, periodic monitoring of bone maturation and effects on epiphyseal centers is recommended during estrogen administration.
Estrogen treatment of prepubertal girls also induces premature breast development and vaginal cornification, and may induce gynecomastia [see INDICATIONS and DOSAGE AND ADMINISTRATION ].
I. Geriatric Use
In the Women’s Health Initiative Memory Study, including 4,532 women 65 years of age and older, followed for an average of 4 years, 82% (n=3,729) were 65 to 74 while 18% (n=803) were 75 and over. Most women (80%) had no prior hormone therapy use. Women treated with conjugated estrogens plus medroxyprogesterone acetate were reported to have a 2-fold increase in the risk of developing probable dementia. Alzheimer’s disease was the most common classification of probable dementia in both the conjugated estrogens plus medroxyprogesterone acetate group and the placebo group. Ninety percent of the cases of probable dementia occurred in the 54% of women that were older than 70 [see BOXED WARNINGS and WARNINGS, Dementia ].
With respect to efficacy in the approved indications, there have not been sufficient numbers of geriatric patients involved in studies utilizing Alora to determine whether those over 65 years of age differ from younger subjects in their response to Alora.
ALORA ADVERSE REACTIONS
See BOXED WARNINGS, WARNINGS and PRECAUTIONS.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Incidence of adverse events > 2% of each treatment group is given in Table 5.
| Placeboa | Alora a | Alora a | Alora a | Alora b | ||
| Body System | 0.025 mg/day | 0.05 mg/day | 0.075 mg/day | 0.1 mg/day | ||
| (N=87) | (N=89) | (N=90) | (N=89) | (N=174) | ||
|
Preferred Term |
||||||
| a - Adverse events for the three lower Alora doses and placebo were obtained from the 2-year prevention of osteoporosis study | ||||||
| b - Adverse events for the highest Alora doses were obtained from two 12-week studies of the treatment of menopausal symptoms | ||||||
| c - Data reported for women with partially or fully intact uteri in the menopausal symptom study only (N=31 for Placebo; N=69 for Alora 0.05 mg/day and N=87 for Alora 0.1 mg/day) | ||||||
| NA – data not available | ||||||
| Body As A Whole | ||||||
| Accidental Injury | 4 (4.6) | 6 (6.7) | 8 (8.9) | 4 (4.5) | 9 (5.2) | |
| Allergic Reaction | 2 (2.3) | 4 (4.5) | 4 (4.4) | 2 (2.2) | 1 (0.6) | |
| Asthenia | 4 (4.6) | 7 (7.9) | 4 (4.4) | 0 (0) | 4 (2.3) | |
| Cyst | 3 (3.4) | 0 (0) | 6 (6.7) | 3 (3.4) | 0 (0) | |
| Flu Syndrome | 9 (10.3) | 8 (9) | 12 (13.3) | 9 (10.1) | 6 (3.4) | |
| Headache | 11 (12.6) | 10 (11.2) | 8 (8.9) | 5 (5.6) | 37 (21.3) | |
| Infection | 2 (2.3) | 2 (2.2) | 3 (3.3) | 3 (3.4) | 2 (1.1) | |
| Infection Fungal | 1 (1.1) | 3 (3.4) | 9 (10) | 4 (4.5) | 0 (0) | |
| Pain | 11 (12.6) | 9 (10.1) | 5 (5.6) | 6 (6.7) | 16 (9.2) | |
| Pain Abdominal | 4 (4.6) | 7 (7.9) | 5 (5.6) | 1 (1.1) | 5 (2.9) | |
| Pain Back | 5 (5.7) | 5 (5.6) | 3 (3.3) | 7 (7.9) | 11 (6.3) | |
| Pain Chest | 4 (4.6) | 4 (4.5) | 2 (2.2) | 1 (1.1) | 2 (1.1) | |
| Cardiovascular | ||||||
| Hypertension | 3 (3.4) | 3 (3.4) | 3 (3.3) | 6 (6.7) | 0 (0) | |
| Migraine | 2 (2.3) | 6 (6.7) | 2 (2.2) | 0 (0) | 2 (1.1) | |
| Vasodilation | 13 (14.9) | 6 (6.7) | 2 (2.2) | 1 (1.1) | 0 (0) | |
| Digestive | ||||||
| Constipation | 4 (4.6) | 3 (3.4) | 6 (6.7) | 1 (1.1) | 3 (1.7) | |
| Diarrhea | 2 (2.3) | 1 (1.1) | 3 (3.3) | 2 (2.2) | 5 (2.9) | |
| Dyspepsia | 1 (1.1) | 8 (9) | 4 (4.4) | 3 (3.4) | 2 (1.1) | |
| Flatulence | 5 (5.7) | 1 (1.1) | 2 (2.2) | 3 (3.4) | 8 (4.6) | |
| Gastroenteritis | 2 (2.3) | 3 (3.4) | 4 (4.4) | 3 (3.4) | 0 (0) | |
| Nausea | 3 (3.4) | 6 (6.7) | 5 (5.6) | 3 (3.4) | 7 (4) | |
| Metabolic And Nutritional | ||||||
| Edema Peripheral | 4 (4.6) | 3 (3.4) | 4 (4.4) | 3 (3.4) | 3 (1.7) | |
| Weight Increased | 4 (4.6) | 3 (3.4) | 2 (2.2) | 4 (4.5) | 1 (0.6) | |
| Musculoskeletal | ||||||
| Arthralgia | 12 (13.8) | 5 (5.6) | 10 (11.1) | 11 (12.4) | 2 (1.1) | |
| Bone Fracture Spontaneous | 7 (8) | 1 (1.1) | 3 (3.3) | 0 (0) | 0 (0) | |
| Joint Disorder | 2 (2.3) | 4 (4.5) | 4 (4.4) | 1 (1.1) | 0 (0) | |
| Myalgia | 4 (4.6) | 3 (3.4) | 2 (2.2) | 5 (5.6) | 3 (1.7) | |
| Nervous | ||||||
| Anxiety | 3 (3.4) | 0 (0) | 9 (10) | 2 (2.2) | 3 (1.7) | |
| Depression | 8 (9.2) | 1 (1.1) | 3 (3.3) | 1 (1.1) | 6 (3.4) | |
| Dizziness | 0 (0) | 1 (1.1) | 7 (7.8) | 4 (4.5) | 1 (0.6) | |
| Hypesthesia | 2 (2.3) | 3 (3.4) | 3 (3.3) | 0 (0) | 0 (0) | |
| Insomnia | 7 (8) | 4 (4.5) | 2 (2.2) | 1 (1.1) | 8 (4.6) | |
| Respiratory | ||||||
| Asthma | 1 (1.1) | 3 (3.4) | 3 (3.3) | 1 (1.1) | 2 (1.1) | |
| Bronchitis | 6 (6.9) | 7 (7.9) | 4 (4.4) | 4 (4.5) | 6 (3.4) | |
| Cough Increased | 2 (2.3) | 1 (1.1) | 4 (4.4) | 1 (1.1) | 6 (3.4) | |
| Infection Respiratory | 23 (26.4) | 22 (24.7) | 22 (24.4) | 19 (21.3) | 28 (16.1) | |
| Pharyngitis | 1 (1.1) | 4 (4.5) | 2 (2.2) | 2 (2.2) | 4 (2.3) | |
| Pneumonia | 4 (4.6) | 4 (4.5) | 4 (4.4) | 1 (1.1) | 1 (0.6) | |
| Sinusitis | 16 (18.4) | 9 (10.1) | 11 (12.2) | 6 (6.7) | 13 (7.5) | |
| Skin | ||||||
| Application Site Reaction | 51 (58.6) | 47 (52.8) | 51 (56.7) | 49 (55.1) | 10 (5.7) | |
| Hirsutism | 0 (0) | 2 (2.2) | 2 (2.2) | 4 (4.5) | 1 (0.6) | |
| Pruritus | 4 (4.6) | 2 (2.2) | 1 (1.1) | 6 (6.7) | 9 (5.2) | |
| Rash | 5 (5.7) | 6 (6.7) | 8 (8.9) | 4 (4.5) | 5 (2.9) | |
| Special Senses | ||||||
| Conjunctivitis | 2 (2.3) | 2 (2.2) | 3 (3.3) | 2 (2.2) | 0 (0) | |
| Otitis Media | 2 (2.3) | 3 (3.4) | 2 (2.2) | 1 (1.1) | 0 (0) | |
| Urogenital | ||||||
| Breast Enlargement | 3 (3.4) | 1 (1.1) | 2 (2.2) | 6 (6.7) | 4 (2.3) | |
| Infection Urinary Tract | 2 (2.3) | 5 (5.6) | 4 (4.4) | 2 (2.2) | 3 (1.7) | |
| Leukorrhea | 1 (1.1) | 3 (3.4) | 2 (2.2) | 4 (4.5) | 3 (1.7) | |
| Neoplasm Breast | 6 (6.9) | 3 (3.4) | 5 (5.6) | 1 (1.1) | 3 (1.7) | |
| Pain Breast | 7 (8) | 13 (14.6) | 16 (17.8) | 31 (34.8) | 12 (6.9) | |
| Vaginitis | 6 (6.9) | 0 (0) | 3 (3.3) | 0 (0) | 14 (8) | |
| Vaginal Bleedingc | 4 (12.9) | NA | 6 (8.7) | NA | 29 (33.3) | |
The following additional adverse reactions have been reported with estrogens and/or progestin therapy:
-
Genitourinary system. Changes in vaginal bleeding pattern and abnormal withdrawal bleeding or flow; breakthrough bleeding; spotting; dysmenorrhea; increase in size of uterine leiomyomata; vaginitis, including vaginal candidiasis; change in amount of cervical secretion; changes in cervical ectropion; ovarian cancer; endometrial hyperplasia; endometrial cancer.
-
Breasts. Tenderness, enlargement, pain, nipple discharge, galactorrhea; fibrocystic breast changes; breast cancer.
-
Cardiovascular. Deep and superficial venous thrombosis; pulmonary embolism; thrombophlebitis; myocardial infarction; stroke; increase in blood pressure.
-
Gastrointestinal. Nausea, vomiting; abdominal cramps, bloating; cholestatic jaundice; increased incidence of gall bladder disease; pancreatitis; enlargement of hepatic hemangiomas.
-
Skin. Chloasma or melasma, which may persist when drug is discontinued; erythema multiform; erythema nodosum; hemorrhagic eruption; loss of scalp hair; hirsutism; pruritus; rash.
-
Eyes. Retinal vascular thrombosis; intolerance to contact lenses.
-
Central nervous system. Headache; migraine; dizziness; mental depression; chorea; nervousness; mood disturbances; irritability; exacerbation of epilepsy; dementia.
-
Miscellaneous. Increase or decrease in weight; reduced carbohydrate tolerance; aggravation of porphyria; edema; arthalgias; leg cramps; changes in libido; anaphylactoid/anaphylactic reactions including urticaria and angioedema; hypocalcemia; exacerbation of asthma; increased triglycerides.
OVERDOSAGE
Serious ill effects have not been reported following acute ingestion of large doses of estrogen containing drug products by young children. Overdosage of estrogen may cause nausea and vomiting, and withdrawal bleeding may occur in females.
ALORA DOSAGE AND ADMINISTRATION
Alora should be administered twice weekly, as instructed. The adhesive side of the Alora system should be placed on a clean, dry area of skin. The recommended application site is the lower abdomen. In addition, the upper quadrant of the buttocks or outer aspect of the hip may be used. Alora should not be applied to the breasts. The sites of application should be rotated, with an interval of at least 1 week allowed between applications to a particular site. The area selected should not be oily, damaged, or irritated. The waistline should be avoided, since tight clothing may rub the system off. The system should be applied immediately after opening the pouch and removing the protective liner. The system should be pressed firmly in place with the palm of the hand for about 10 seconds, making sure there is good contact, especially around the edges.
In the event that a system should fall off, the same system may be reapplied. If necessary, a new system may be applied to another site. The original treatment schedule should be maintained.
Initiation of Therapy
For treatment of moderate-to-severe vasomotor symptoms, vulvar and vaginal atrophy associated with the menopause, hypogonadism, castration, or primary ovarian failure, treatment is usually initiated with Alora 0.05 mg/day applied to the skin twice weekly. The lowest dose and regimen that will control symptoms should be chosen and medication should be discontinued as promptly as possible. Attempts to discontinue or taper medication should be made at 3-month to 6-month intervals.
For the prevention of postmenopausal osteoporosis, the minimum dose of Alora that has been studied and shown to be effective is 0.025 mg/day applied to the skin twice weekly. Bone mineral density measurements should be repeated to monitor treatment efficacy. The dosage may be increased as necessary, depending on bone mineral density and adverse events.
In women who are not currently taking oral estrogens or in women switching from topical therapy or another transdermal estradiol therapy, treatment with Alora can be initiated at once. In women who are currently taking oral estrogens, treatment with Alora should be initiated 1 week after withdrawal of oral therapy or sooner if menopausal symptoms reappear in less than 1 week.
When estrogen is prescribed for a postmenopausal woman with a uterus, progestin should also be initiated to reduce the risk of endometrial cancer. A woman without a uterus does not need progestin. Use of estrogen, alone or in combination with a progestin, should be limited to the shortest duration consistent with treatment goals and risks for the individual woman. Patients should be reevaluated periodically as clinically appropriate (e.g., 3-month to 6-month intervals) to determine if treatment is still necessary (see BOXED WARNINGS and WARNINGS). For women who have a uterus, adequate diagnostic measures, such as endometrial sampling, when indicated, should be undertaken to rule out malignancy in cases of undiagnosed persistent or recurring abnormal vaginal bleeding.
Therapeutic Regimen
Alora may be administered in a continuous regimen in patients who do not possess an intact uterus. In those patients with an intact uterus who are not using concomitant progestin therapy, Alora can be administered on a cyclic schedule (e.g., 3 weeks of therapy followed by 1 week without) for the treatment of postmenopausal symptoms. However, no studies have been conducted using this intermittent regimen for the prevention of postmenopausal osteoporosis.
HOW SUPPLIED
Alora (Estradiol Transdermal System, USP) 0.025 mg/day. Each 9 cm2 system contains 0.77 mg of estradiol, USP for nominal delivery of 0.025 mg of estradiol per day when dosed in a twice weekly regimen.
NDC 52544-884-08 Patient Calendar Box of 8 Systems
Alora (Estradiol Transdermal System, USP) 0.05 mg/day. Each 18 cm2 system contains 1.5 mg of estradiol, USP for nominal delivery of 0.05 mg of estradiol per day when dosed in a twice weekly regimen.
NDC 52544-471-08 Patient Calendar Box of 8 Systems
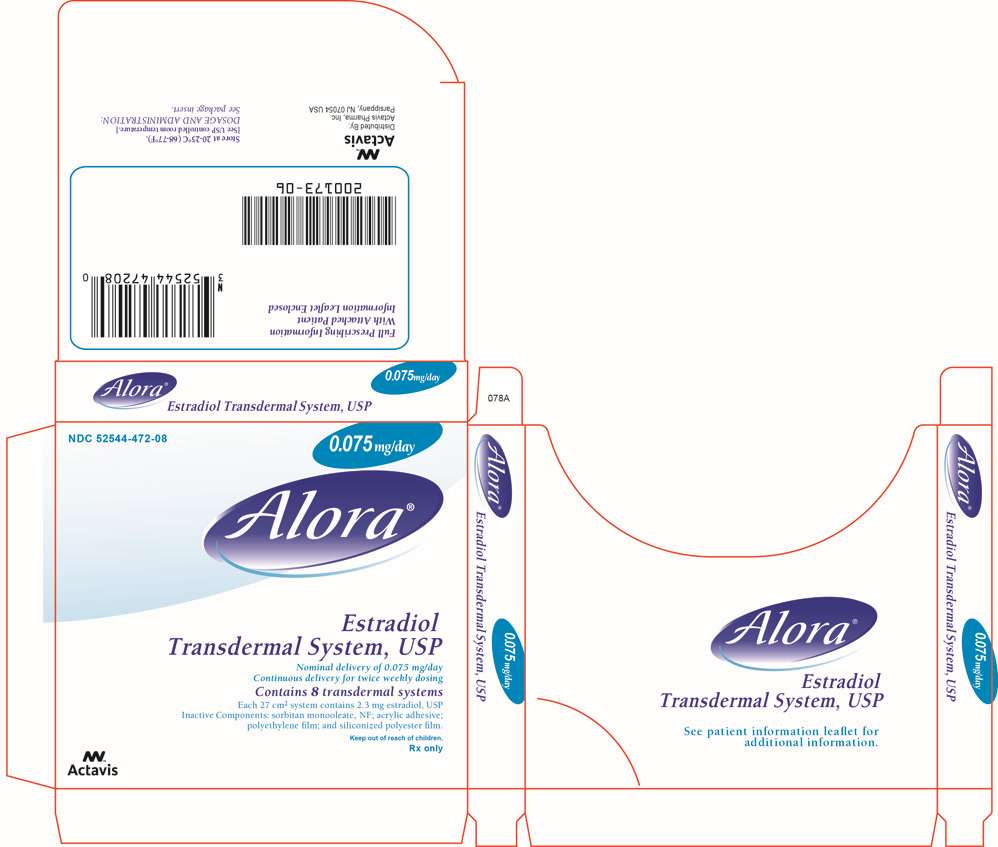
Alora (Estradiol Transdermal System, USP) 0.075 mg/day. Each 27 cm2 system contains 2.3 mg of estradiol, USP for nominal delivery of 0.075 mg of estradiol per day when dosed in a twice weekly regimen.
NDC 52544-472-08 Patient Calendar Box of 8 Systems
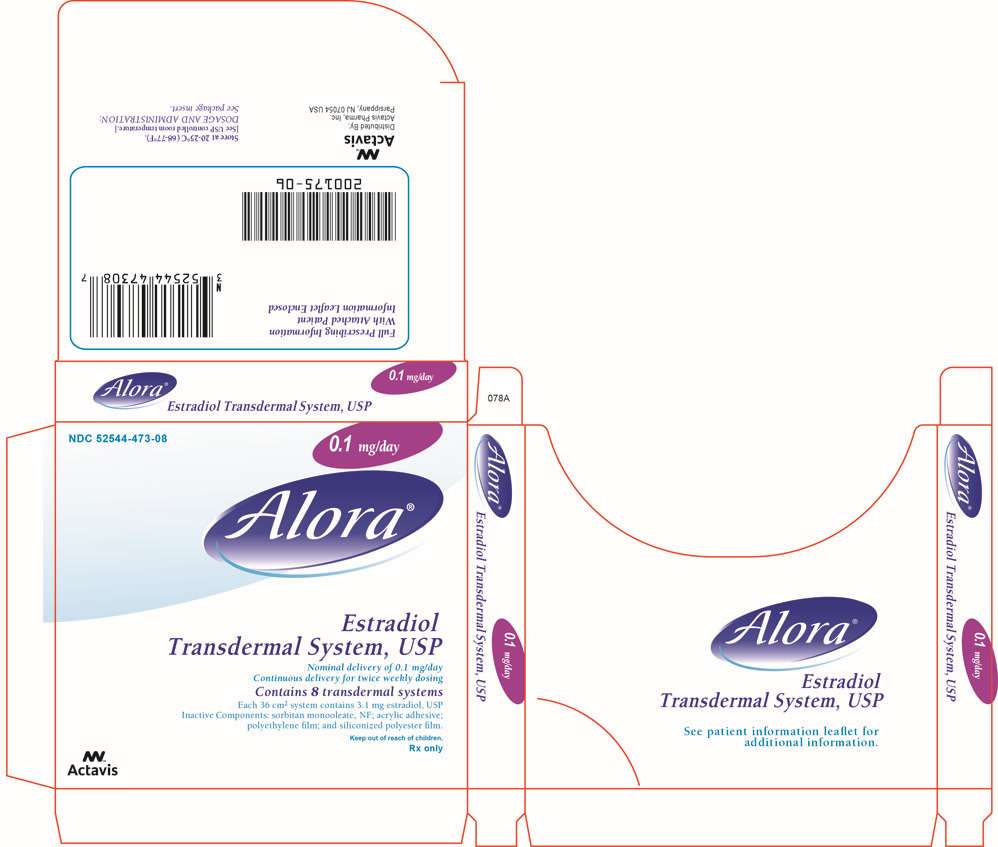
Alora (Estradiol Transdermal System, USP) 0.1 mg/day. Each 36 cm2 system contains 3.1 mg of estradiol, USP for nominal delivery of 0.1 mg of estradiol per day when dosed in a twice weekly regimen.
NDC 52544-473-08 Patient Calendar Box of 8 Systems
Store at 20-25°C (68-77°F). [See USP controlled room temperature.]
Do not store unpouched. Apply immediately upon removal from the protective pouch.
Discard used Alora in household trash in a manner that prevents accidental application or ingestion by children, pets, or others.
Keep out of reach of children.
For all medical inquiries contact:
ACTAVIS
Medical Communications
Parsippany, NJ 07054
1-800-272-5525
Distributed By:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
Content Updated: November 2013
200178-12
PATIENT INFORMATION
Read this PATIENT INFORMATION before you start using Alora (ah-LORE-ah) and read what you get each time you refill Alora. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
|
What is Alora?
Alora is a patch that contains the estrogen hormone estradiol. When applied to the skin as directed below, the Alora patch releases estrogen through the skin into the abdomen.
What is Alora used for?
Alora is used after menopause to:
-
Reduce moderate or severe hot flashes.
Estrogens are hormones made by a woman’s ovaries. Between ages 45 and 55, the ovaries normally stop making estrogens. This drop in body estrogen levels causes the “change of life” or menopause (the end of monthly menstrual periods). Sometimes, both ovaries are removed during an operation before natural menopause takes place. The sudden drop in estrogen levels causes “surgical menopause.”
When estrogen levels begin dropping, some women develop very uncomfortable symptoms, such as feelings of warmth in the face, neck, and chest, or sudden intense episodes of heat and sweating (“hot flashes” or “hot flushes”). In some women the symptoms are mild and they will not need estrogens. In other women, symptoms can be more severe. You and your healthcare provider should talk regularly about whether you still need treatment with Alora.
-
Treat moderate to severe dryness, itching and burning in and around the vagina.
You and your healthcare provider should talk regularly about whether you still need treatment with Alora to control these problems. If you use Alora only to treat your dryness, itching, and burning in and around your vagina, talk with your healthcare provider about whether a topical vaginal product would be better for you. -
Treat certain conditions in which a young woman’s ovaries do not produce enough estrogen naturally.
-
Help reduce your chances of getting osteoporosis (thin weak bones).
Osteoporosis from menopause is a thinning of the bones that makes them weaker and allows them to break more easily. If you use Alora only to prevent osteoporosis from menopause, talk with your healthcare provider about whether a different treatment or medicine without estrogens might be better for you.
Weight-bearing exercise like walking and running, and taking calcium and vitamin D supplements may lower your chances of getting postmenopausal osteoporosis. It is important to talk about exercise and supplements with your healthcare provider before starting them.
Who Should Not Use Alora
Do not use Alora if you:
-
Have unusual vaginal bleeding.
-
Currently have or have had certain cancers.
Estrogens may increase the risk of certain types of cancer, including cancer of the breast or uterus. If you have or have had cancer, talk to your healthcare provider about whether you should use Alora. -
Had a stroke or heart attack in the past year.
-
Currently have or have had blood clots.
-
Currently have or have had liver problems.
-
Are allergic to Alora or any of the ingredients in it. See the end of this leaflet for a list of ingredients in Alora.
-
Think you may be pregnant.
Tell your healthcare provider:
-
If you are breastfeeding. The hormone in Alora may pass into your milk.
-
About all of your medical problems. Your healthcare provider may need to check you more carefully if you have certain conditions, such as asthma (wheezing); epilepsy (seizures); migraine; endometriosis; lupus; problems with your heart; liver; thyroid; kidneys; or have high calcium levels in your blood.
-
About all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Some medicines may affect how Alora works. Alora may also affect how your other medicines work.
-
If you are going to have surgery or will be on bed rest. You may need to stop estrogens.
What Are the Possible Side Effects of Alora?
Less common but serious side effects include:
-
Breast cancer
-
Cancer of the uterus
-
Stroke
-
Heart attack
-
Blood clots
-
Gallbladder disease
-
Ovarian cancer
-
Dementia
These are some of the warning signs of serious side effects:
-
Breast lumps
-
Unusual vaginal bleeding
-
Dizziness and faintness
-
Changes in speech
-
Severe headaches
-
Chest pain
-
Shortness of breath
-
Pains in your legs
-
Changes in vision
-
Vomiting
Call your healthcare provider right away if you get any of these warning signs, or any other unusual symptom that concerns you.
Common side effects include:
-
Headache
-
Breast pain
-
Irregular vaginal bleeding or spotting
-
Stomach/abdominal cramps, bloating
-
Nausea and vomiting
-
Hair loss
Other side effects include:
-
High blood pressure
-
Liver problems
-
High blood sugar
-
Fluid retention
-
Enlargement of benign tumors of the uterus (“fibroids”)
-
Vaginal yeast infection
These are not all the possible side effects of Alora. For more information, ask your healthcare provider or pharmacist.
What Can I Do to Lower My Chances of Getting a Serious Side Effect with Alora?
-
Talk with your healthcare provider regularly about whether you should continue using Alora.
-
If you have a uterus, talk to your healthcare provider right away about whether the addition of a progestin is right for you. In general, the addition of a progestin is recommended for women with a uterus to reduce the chance of getting cancer of the uterus.
-
See your healthcare provider right away if you get vaginal bleeding while using Alora.
-
Have a breast exam and mammogram (breast X-ray) every year unless your healthcare provider tells you something else. If members of your family have had breast cancer or if you have ever had breast lumps or an abnormal mammogram, you may need to have breast exams more often.
-
If you have high blood pressure, high cholesterol (fat in the blood), diabetes, are overweight, or if you use tobacco, you may have higher chances for getting heart disease. Ask your healthcare provider for ways to lower your chances for getting heart disease.
How should I use Alora?
Before you begin, read all the information in these 5 steps.
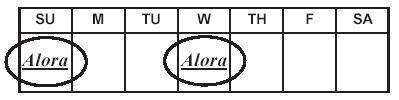
Step 1. Choose your schedule for twice-a-week application.

Put on a new patch twice a week. Use one of the schedules on the inside flap of the patch box.
For example, if you apply your first patch on Sunday, take that patch off on Wednesday and put on a new one. Stay on this schedule as long as you use Alora. To help remind yourself, mark the schedule on the inside flap of the patch box. Put a check next to the first day you apply the patch. When you change your patch, don’t put the new one in the same place. To help reduce the chance of skin redness or irritation, wait at least one week before you reuse a spot.
Step 2. Before you apply the patch make sure the skin at the spot is:
-
Freshly washed, but dry and cool (wait a few minutes after taking a hot bath or shower).
-
Free of body powder or lotion.
-
Free of cuts, rashes, or any other skin problem.
Step 3. Choose a spot for the patch
-
Place the patch on the lower abdomen (below the panty line) when you first start using Alora.
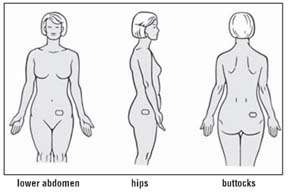
-
As you get used to applying Alora, you may want to try the hips or buttocks to see which area works best for you.
-
Do not apply Alora to your breasts or any other parts of your body.
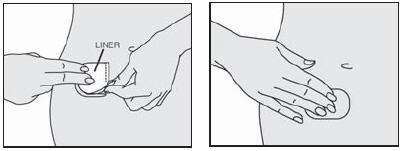
Step 4. How to apply the patch
-
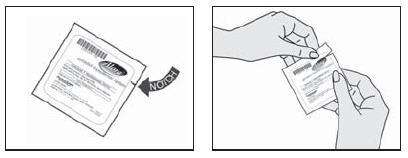
Open the pouch that contains the patch.
-
Locate the notch on the top left or right corner of the pouch.
-
Hold the pouch at the notch and tear off the top edge. Do not cut the pouch with scissors, which might damage the patch inside.
-
Pull the patch out.
-
Apply one half of the patch to your skin.
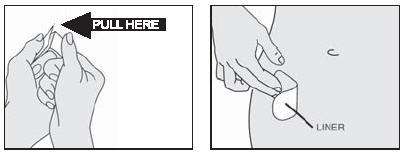
-
Remove half of the liner, which covers the sticky surface of the patch. To find the liner, bend the patch in half. Then grab the clear straight edge of the liner and pull that piece off.
-
Without touching the sticky surface, press the sticky half of the patch onto your skin. (If you touch the sticky surface, the patch may not stay on as well.)
-
Rub the sticky half firmly to ensure full contact with your skin.
-
Apply the second half of the patch to your skin.
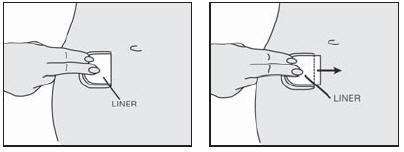
-
Bend the patch back over itself. Press down on the liner firmly.
-
Push the liner forward a little to loosen the edge.
-
Grab the loose edge at either corner and peel off the second piece of the liner. Try not to touch the sticky surface of the patch.
-
Press the entire patch firmly onto the skin with your finger tips.
Press for at least 10 seconds to make sure the patch will stay in place. Be sure all of it sticks to your skin, even around the edges.
To help the patch stay in place:
-
Try not to disturb the patch while putting on and removing clothes. It may help to place the patch where your underwear will cover it at all times.
-
Be careful while changing clothes, washing or drying off, so that you do not catch the patch with your clothes or the towel.
-
Try different sites on the lower abdomen, hips, or buttocks area to see what works well with your body and your clothing.
-
If the patch starts to lift, simply press it back in place.
Step 5. Removing the patch
-
Take off the old patch.
-
Fold it in half (sticky sides together) and throw it away out of the reach of children and pets.
The skin under the old patch may look pink, but the color should fade away soon. In some cases, the skin may itch or look red; this may last from a couple of hours to a couple of days. Most of the time this is minor, and goes away by itself. But if it bothers you a lot or lasts longer than a few days, call your healthcare provider.
For Best Results, Stay with Your Patch Program
-
Replace your patch twice each week, on the 2 days you have chosen. Until it becomes a habit, try
- Marking your schedule on the inside flap of the patch box;
- Marking the days on your calendar;
-
Linking the days you change your patch to other things that always happen on those days (e.g., an exercise class, meetings, etc.)
-
Handle each patch with care.
-
Make sure the skin is clean, dry, and free of lotion and powder.
-
Try to avoid touching the sticky surface when applying the patch.
-
Be careful while changing clothes, washing or drying off, so that you do not catch the patch with your clothes or the towel.
-
If the patch starts to lift, simply press it back in place.
-
-
Keep working with your healthcare provider, pharmacist, or other healthcare professional. Ask questions. If you have concerns, talk them over - don’t just stop using the patch on your own. Remember, it may take a little time and some experience to get accustomed to using a patch. Estrogens should be used only as long as needed. Start with the lowest dose and talk to your healthcare provider about how well that dose is working for you. You and your healthcare provider should talk regularly (for example, every 3 to 6 months) about whether you still need treatment with Alora.
-
Get your refills of the Alora patch before your supply runs out.
How should I store Alora?
Store at 20-25°C (68-77°F). [See USP controlled room temperature.] Do not store patches outside of their pouches. Apply the patch as soon as you take it out of the protective pouch.
Discard used Alora in household trash in a manner that prevents accidental application or ingestion by children, pets, or others.
General Information about the safe and effective use of Alora
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not take Alora for conditions for which it was not prescribed. Your healthcare provider has prescribed this drug for you and you alone. Do not give the drug to anyone else. It may harm them. Keep Alora out of the reach of children.
This leaflet provides a summary of the most important information about Alora. If you would like more information, talk with your healthcare provider. You can ask for information about Alora that is written for health professionals.
What are the ingredients in Alora?
Each patch contains estradiol, USP as the active component. Inactive components of each patch include sorbitan monooleate, NF; acrylic adhesive; polyethylene film; and siliconized polyester film.
Keep out of reach of children.
For all medical inquiries contact:
ACTAVIS
Medical Communications
Parsippany, NJ 07054 USA
1-800-272-5525
Distributed By:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
Content Updated: November 2013
200178-12
Alora®
Estradiol Transdermal System, USP
NDC 52544-884-08
Carton of 8 systems 0.025 mg/day
Alora®
Estradiol Transdermal System, USP
NDC 52544-471-08
Carton of 8 systems 0.05 mg/day
Alora®
Estradiol Transdermal System, USP
NDC 52544-472-08
Carton of 8 systems 0.075 mg/day
Alora®
Estradiol Transdermal System, USP
NDC 52544-473-08
Carton of 8 systems 0.1 mg/day
AloraEstradiol Transdermal System PATCH
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
AloraEstradiol Transdermal System PATCH
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
AloraEstradiol Transdermal System PATCH
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
AloraEstradiol Transdermal System PATCH
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||