Amiodarone Hydrochloride
Amiodarone Hydrochloride Injection, 50 mg/mL
FULL PRESCRIBING INFORMATION: CONTENTS*
- AMIODARONE HYDROCHLORIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- INDICATIONS AND USAGE
- AMIODARONE HYDROCHLORIDE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- AMIODARONE HYDROCHLORIDE ADVERSE REACTIONS
- OVERDOSAGE
- DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
FULL PRESCRIBING INFORMATION
AMIODARONE HYDROCHLORIDE DESCRIPTION
Amiodarone HCl Injection contains amiodarone HCl (C25H29I2NO3•HCl), a class III antiarrhythmic drug. Amiodarone HCl is (2-butyl-3-benzofuranyl) [4-[2-(diethylamino)ethoxy]-3,5-diiodophenyl] methanone hydrochloride. Amiodarone HCl has the following structural formula:
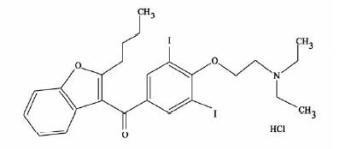
Amiodarone HCl is a white to slightly yellow crystalline powder, and is very slightly soluble in water. It has a molecular weight of 681.78 and contains 37.3% iodine by weight. Amiodarone HCl injection is a sterile clear, pale-yellow micellar solution visually free from particulates. Each milliliter of the amiodarone HCl injection formulation contains 50 mg of amiodarone HCl, 20.2 mg of benzyl alcohol NF, 100 mg of polysorbate 80 NF, and Water for Injection USP.
Intravenous amiodarone contains polysorbate 80, which is known to leach di-(2-ethylhexyl)phthalate (DEHP) from polyvinylchloride (PVC) (see DOSAGE AND ADMINISTRATION).
CLINICAL PHARMACOLOGY
Amiodarone is generally considered a class III antiarrhythmic drug, but it possesses electrophysiologic characteristics of all four Vaughan Williams classes. Like class I drugs, amiodarone blocks sodium channels at rapid pacing frequencies, and like class II drugs, it exerts a noncompetitive antisympathetic action. One of its main effects, with prolonged administration, is to lengthen the cardiac action potential, a class III effect. The negative chronotropic effect of amiodarone in nodal tissues is similar to the effect of class IV drugs. In addition to blocking sodium channels, amiodarone blocks myocardial potassium channels, which contributes to slowing of conduction and prolongation of refractoriness. The antisympathetic action and the block of calcium and potassium channels are responsible for the negative dromotropic effects on the sinus node and for the slowing of conduction and prolongation of refractoriness in the atrioventricular (AV) node. Its vasodilatory action can decrease cardiac workload and consequently myocardial oxygen consumption.
Intravenous amiodarone administration prolongs intranodal conduction (Atrial-His, AH) and refractoriness of the atrioventricular node (ERP AVN), but has little or no effect on sinus cycle length (SCL), refractoriness of the right atrium and right ventricle (ERP RA and ERP RV), repolarization (QTc), intraventricular conduction (QRS), and infranodal conduction (His-ventricular, HV). A comparison of the electrophysiologic effects of intravenous amiodarone and oral amiodarone is shown in the table below.
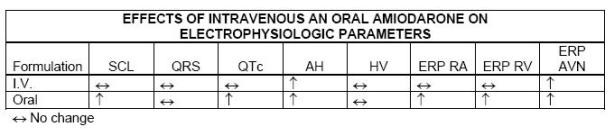
At higher doses (>10 mg/kg) of amiodarone HCl injection, prolongation of the ERP RV and modest prolongation of the QRS have been seen. These differences between oral and intravenous administration suggest that the initial acute effects of amiodarone injection may be predominantly focused on the AV node, causing an intranodal conduction delay and increased nodal refractoriness due to slow channel blockade (class IV activity) and noncompetitive adrenergic antagonism (class II activity).
Amiodarone exhibits complex disposition characteristics after intravenous administration. Peak serum concentrations after single 5 mg/kg 15-minute intravenous infusions in healthy subjects range between 5 and 41 mg/L. Peak concentrations after 10-minute infusions of 150 mg intravenous amiodarone in patients with ventricular fibrillation (VF) or hemodynamically unstable ventricular tachycardia (VT) range between 7 and 26 mg/L. Due to rapid distribution, serum concentrations decline to 10% of peak values within 30 to 45 minutes after the end of the infusion. In clinical trials, after 48 hours of continued infusions (125, 500, or 1000 mg/day) plus supplemental (150 mg) infusions (for recurrent arrhythmias), amiodarone mean serum concentrations between 0.7 to 1.4 mg/L were observed (n=260).
N-desethylamiodarone (DEA) is the major active metabolite of amiodarone in humans. DEA serum concentrations above 0.05 mg/L are not usually seen until after several days of continuous infusion but with prolonged therapy reach approximately the same concentration as amiodarone. Amiodarone is metabolized to desethylamiodarone by the cytochrome P450 (CYP450) enzyme group, specifically cytochrome P450 3A4 (CYP3A4) and CYP2C8. The CYP3A4 isoenzyme is present in both the liver and intestines. The highly variable systemic availability of oral amiodarone may be attributed potentially to large interindividual variability in CYP3A4 activity.
Amiodarone is eliminated primarily by hepatic metabolism and biliary excretion and there is negligible excretion of amiodarone or DEA in urine. Neither amiodarone nor DEA is dialyzable. Amiodarone and DEA cross the placenta and both appear in breast milk.
No data are available on the activity of DEA in humans, but in animals, it has significant electrophysiologic and antiarrhythmic effects generally similar to amiodarone itself. DEA’s precise role and contribution to the antiarrhythmic activity of oral amiodarone are not certain. The development of maximal ventricular class III effects after oral amiodarone administration in humans correlates more closely with DEA accumulation over time than with amiodarone accumulation. On the other hand (see Clinical Trials), after intravenous amiodarone administration, there is evidence of activity well before significant concentrations of DEA are attained.
The following table summarizes the mean ranges of pharmacokinetic parameters of amiodarone reported in single dose i.v. (5 mg/kg over 15 min) studies of healthy subjects.
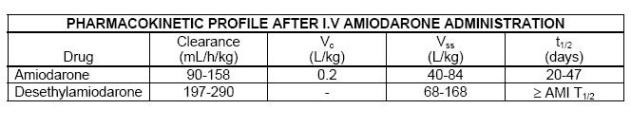
Notes VC and VSS denote the central and steady-state volumes of distribution from i.v. studies. “-” denotes not available.
Desethylamiodarone clearance and volume involve an unknown biotransformation factor.
The systemic availability of oral amiodarone in healthy subjects ranges between 33% and 65%. From in vitro studies, the protein binding of amiodarone is >96%.
In clinical studies of 2 to 7 days, clearance of amiodarone after intravenous administration in patients with VT and VF ranged between 220 and 440 mL/h/kg. Age, sex, renal disease, and hepatic disease (cirrhosis) do not have marked effects on the disposition of amiodarone or DEA. Renal impairment does not influence the pharmacokinetics of amiodarone. After a single dose of intravenous amiodarone in cirrhotic patients, significantly lower Cmax and average concentration values are seen for DEA, but mean amiodarone levels are unchanged. Normal subjects over 65 years of age show lower clearances (about 100 mL/hr/kg) than younger subjects (about 150 mL/hr/kg) and an increase in t1/2 from about 20 to 47 days. In patients with severe left ventricular dysfunction, the pharmacokinetics of amiodarone are not significantly altered but the terminal disposition t1/2 of DEA is prolonged. Although no dosage adjustment for patients with renal, hepatic, or cardiac abnormalities has been defined during chronic treatment with oral amiodarone, close clinical monitoring is prudent for elderly patients and those with severe left ventricular dysfunction.
There is no established relationship between drug concentration and therapeutic response for short-term intravenous use. Steady-state amiodarone concentrations of 1 to 2.5 mg/L have been associated with antiarrhythmic effects and acceptable toxicity following chronic oral amiodarone therapy.
Intravenous amiodarone has been reported to produce negative inotropic and vasodilatory effects in animals and humans. In clinical studies of patients with refractory VF or hemodynamically unstable VT, treatment-emergent, drug-related hypotension occurred in 288 of 1836 patients (16%) treated with amiodarone. No correlations were seen between the baseline ejection fraction and the occurrence of clinically significant hypotension during infusion of intravenous amiodarone.
Apart from studies in patients with VT or VF, described below, there are two other studies of amiodarone showing an antiarrhythmic effect before significant levels of DEA could have accumulated. A placebo-controlled study of i.v. amiodarone (300 mg over 2 hours followed by 1200 mg/day) in post-coronary artery bypass graft patients with supraventricular and 2- to 3-consecutive-beat ventricular arrhythmias showed a reduction in arrhythmias from 12 hours on. A baseline-controlled study using a similar i.v. regimen in patients with recurrent, refractory VT/VF also showed rapid onset of antiarrhythmic activity; amiodarone therapy reduced episodes of VT by 85% compared to baseline.
The acute effectiveness of amiodarone HCl injection in suppressing recurrent VF or hemodynamically unstable VT is supported by two randomized, parallel, dose-response studies of approximately 300 patients each. In these studies, patients with at least two episodes of VF or hemodynamically unstable VT in the preceding 24 hours were randomly assigned to receive doses of approximately 125 or 1000 mg over the first 24 hours, an 8-fold difference. In one study, a middle dose of approximately 500 mg was evaluated. The dose regimen consisted of an initial rapid loading infusion, followed by a slower 6-hour loading infusion, and then an 18-hour maintenance infusion. The maintenance infusion was continued up to hour 48. Additional 10-minute infusions of 150 mg intravenous amiodarone were given for “breakthrough” VT/VF more frequently to the 125 mg dose group, thereby considerably reducing the planned 8-fold differences in total dose to 1.8- and 2.6- fold, respectively, in the two studies.
The prospectively defined primary efficacy end point was the rate of VT/VF episodes per hour. For both studies, the median rate was 0.02 episodes per hour in patients receiving the high dose and 0.07 episodes per hour in patients receiving the low dose, or approximately 0.5 versus 1.7 episodes per day (p = 0.07, 2-sided, in both studies). In one study, the time to first episode of VT/VF was significantly prolonged (approximately 10 hours in patients receiving the low dose and 14 hours in patients receiving the high dose). In both studies, significantly fewer supplemental infusions were given to patients in the high-dose group. Mortality was not affected in these studies; at the end of double-blind therapy or after 48 hours, all patients were given open access to whatever treatment (including intravenous amiodarone) was deemed necessary.
INDICATIONS AND USAGE
Amiodarone HCl injection is indicated for initiation of treatment and prophylaxis of frequently recurring ventricular fibrillation and hemodynamically unstable ventricular tachycardia in patients refractory to other therapy. Intravenous amiodarone also can be used to treat patients with VT/VF for whom oral amiodarone is indicated, but who are unable to take oral medication. During or after treatment with intravenous amiodarone, patients may be transferred to oral amiodarone therapy(see DOSAGE AND ADMINISTRATION).
Intravenous amiodarone should be used for acute treatment until the patient’s ventricular arrhythmias are stabilized. Most patients will require this therapy for 48 to 96 hours, but intravenous amiodarone may be safely administered for longer periods if necessary.
AMIODARONE HYDROCHLORIDE CONTRAINDICATIONS
Amiodarone injection is contraindicated in patients with known hypersensitivity to any of the components of amiodarone injection, including iodine, or in patients with cardiogenic shock, marked sinus bradycardia, and second- or third-degree AV block unless a functioning pacemaker is available.
WARNINGS
Hypotension
Hypotension is the most common adverse effect seen with intravenous amiodarone. In clinical trials, treatment-emergent, drug-related hypotension was reported as an adverse effect in 288 (16%) of 1836 patients treated with intravenous amiodarone. Clinically significant hypotension during infusions was seen most often in the first several hours of treatment and was not dose related, but appeared to be related to the rate of infusion. Hypotension necessitating alterations in intravenous amiodarone therapy was reported in 3% of patients, with permanent discontinuation required in less than 2% of patients.
Hypotension should be treated initially by slowing the infusion; additional standard therapy may be needed, including the following: vasopressor drugs, positive inotropic agents, and volume expansion. The initial rate of infusion should be monitored closely and should not exceed that prescribed in DOSAGE AND ADMINISTRATION.
In some cases, hypotension may be refractory resulting in fatal outcome (see ADVERSE REACTIONS, Postmarketing Reports).
Bradycardia and AV Block
Drug-related bradycardia occurred in 90 (4.9%) of 1836 patients in clinical trials while they were receiving intravenous amiodarone for life-threatening VT/VF; it was not dose-related. Bradycardia should be treated by slowing the infusion rate or discontinuing amiodarone. In some patients, inserting a pacemaker is required. Despite such measures, bradycardia was progressive and terminal in 1 patient during the controlled trials. Patients with a known predisposition to bradycardia or AV block should be treated with intravenous amiodarone in a setting where a temporary pacemaker is available.
Long-Term Use
See labeling for oral amiodarone. There has been limited experience in patients receiving intravenous amiodarone for longer than 3 weeks.
Neonatal Hypo- or Hyperthyroidism
Although amiodarone use during pregnancy is uncommon, there have been a small number of published reports of congenital goiter/hypothyroidism and hyperthyroidism associated with its oral administration. If intravenous amiodarone is administered during pregnancy, the patient should be apprised of the potential hazard to the fetus.
PRECAUTIONS
Amiodarone injection should be administered only by physicians who are experienced in the treatment of life-threatening arrhythmias, who are thoroughly familiar with the risks and benefits of amiodarone therapy, and who have access to facilities adequate for monitoring the effectiveness and side effects of treatment.
Liver Enzyme Elevations
Elevations of blood hepatic enzyme values-alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyl transferase (GGT)-are seen commonly in patients with immediately life-threatening VT/VF. Interpreting elevated AST activity can be difficult because the values may be elevated in patients who have had recent myocardial infarction, congestive heart failure, or multiple electrical defibrillations. Approximately 54% of patients receiving intravenous amiodarone in clinical studies had baseline liver enzyme elevations, and 13% had clinically significant elevations. In 81% of patients with both baseline and on-therapy data available, the liver enzyme elevations either improved during therapy or remained at baseline levels. Baseline abnormalities in hepatic enzymes are not a contraindication to treatment.
Acute, centrolobular confluent hepatocellular necrosis leading to hepatic coma, acute renal failure, and death has been associated with the administration of intravenous amiodarone at a much higher loading dose concentration and much faster rate of infusion than recommended in DOSAGE AND ADMINISTRATION. Therefore, the initial concentration and rate of infusion should be monitored closely and should not exceed that prescribed in DOSAGE AND ADMINISTRATION (see DOSAGE AND ADMINISTRATION).
In patients with life-threatening arrhythmias, the potential risk of hepatic injury should be weighed against the potential benefit of intravenous amiodarone therapy, but patients receiving intravenous amiodarone should be monitored carefully for evidence of progressive hepatic injury. Consideration should be given to reducing the rate of administration or withdrawing intravenous amiodarone in such cases.
Proarrhythmia
Like all antiarrhythmic agents, intravenous amiodarone may cause a worsening of existing arrhythmias or precipitate a new arrhythmia. Proarrhythmia, primarily torsades de pointes (TdP), has been associated with prolongation by intravenous amiodarone of the QTc interval to 500 ms or greater. Although QTc prolongation occurred frequently in patients receiving intravenous amiodarone, torsades de pointes or new-onset VF occurred infrequently (less than 2%). Patients should be monitored for QTc prolongation during infusion with intravenous amiodarone. Combination of amiodarone with other antiarrhythmic therapy that prolongs the QTc should be reserved for patients with life-threatening ventricular arrhythmias who are incompletely responsive to a single agent.
Fluoroquinolones, macrolide antibiotics, and azoles are known to cause QTc prolongation. There have been reports of QTc prolongation, with or without TdP, in patients taking amiodarone when fluoroquinolones, macrolide antibiotics, or azoles were administered concomitantly. (See Drug Interactions, Other reported interactions with amiodarone.)
The need to coadminister amiodarone with any other drug known to prolong the QTc interval must be based on a careful assessment of the potential risks and benefits of doing so for each patient.
A careful assessment of the potential risks and benefits of administering intravenous amiodarone must be made in patients with thyroid dysfunction due to the possibility of arrhythmia breakthrough or exacerbation of arrhythmia, which may result in death, in these patients.
Pulmonary Disorders
Early-onset pulmonary toxicity
There have been postmarketing reports of acute-onset (days to weeks) pulmonary injury in patients treated with intravenous amiodarone. Findings have included pulmonary infiltrates on X-ray, bronchospasm, wheezing, fever, dyspnea, cough, hemoptysis, and hypoxia. Some cases have progressed to respiratory failure and/or death.
ARDS
Two percent (2%) of patients were reported to have adult respiratory distress syndrome (ARDS) during clinical studies involving 48 hours of therapy. ARDS is a disorder characterized by bilateral, diffuse pulmonary infiltrates with pulmonary edema and varying degrees of respiratory insufficiency. The clinical and radiographic picture can arise after a variety of lung injuries, such as those resulting from trauma, shock, prolonged cardiopulmonary resuscitation, and aspiration pneumonia, conditions present in many of the patients enrolled in the clinical studies. There have been postmarketing reports of ARDS in intravenous amiodarone patients. Intravenous amiodarone may play a role in causing or exacerbating pulmonary disorders in those patients.
Postoperatively, occurrences of ARDS have been reported in patients receiving oral amiodarone therapy who have undergone either cardiac or noncardiac surgery. Although patients usually respond well to vigorous respiratory therapy, in rare instances the outcome has been fatal. Until further studies have been performed, it is recommended that FiO2 and the determinants of oxygen delivery to the tissues (e.g., SaO2, PaO2) be closely monitored in patients on amiodarone.
Pulmonary fibrosis
Only 1 of more than 1000 patients treated with intravenous amiodarone in clinical studies developed pulmonary fibrosis. In that patient, the condition was diagnosed 3 months after treatment with intravenous amiodarone, during which time she received oral amiodarone. Pulmonary toxicity is a well-recognized complication of long-term amiodarone use (see labeling for oral amiodarone).
Surgery
Close perioperative monitoring is recommended in patients undergoing general anesthesia who are on amiodarone therapy as they may be more sensitive to the myocardial depressant and conduction defects of halogenated inhalational anesthetics.
Drug Interactions
Amiodarone is metabolized to desethylamiodarone by the cytochrome P450 (CYP450) enzyme group, specifically cytochromes P450 3A4 (CYP3A4) and CYP2C8. The CYP3A4 isoenzyme is present in both the liver and intestines (see CLINICAL PHARMACOLOGY, Pharmacokinetics and Metabolism). Amiodarone is an inhibitor of CYP3A4 and p-glycoprotein. Therefore, amiodarone has the potential for interactions with drugs or substances that may be substrates, inhibitors or inducers of CYP3A4 and substrates of p-glycoprotein. While only a limited number of in vivo drug-drug interactions with amiodarone have been reported, chiefly with the oral formulation, the potential for other interactions should be anticipated. This is especially important for drugs associated with serious toxicity, such as other antiarrhythmics. If such drugs are needed, their dose should be reassessed and, where appropriate, plasma concentration measured. In view of the long and variable half-life of amiodarone, potential for drug interactions exists not only with concomitant medication but also with drugs administered after discontinuation of amiodarone.
Since amiodarone is a substrate for CYP3A4 and CYP2C8, drugs/substances that inhibit these isoenzymes may decrease the metabolism and increase serum concentration of amiodarone. Reported examples include the following:
Protease Inhibitors
Protease inhibitors are known to inhibit CYP3A4 to varying degrees. A case report of one patient taking amiodarone 200 mg and indinavir 800 mg three times a day resulted in increases in amiodarone concentrations from 0.9 mg/L to 1.3 mg/L. DEA concentrations were not affected. There was no evidence of toxicity. Monitoring for amiodarone toxicity and serial measurement of amiodarone serum concentration during concomitant protease inhibitor therapy should be considered.
Histamine H2 antagonists
Cimetidine inhibits CYP3A4 and can increase serum amiodarone levels.
Other substances
Grapefruit juice given to healthy volunteers increased amiodarone AUC by 50% and Cmax by 84%, resulting in increased plasma levels of amiodarone. Grapefruit juice should not be taken during treatment with oral amiodarone. This information should be considered when changing from intravenous amiodarone to oral amiodarone (see DOSAGE AND ADMINISTRATION, Intravenous to Oral Transition).
Amiodarone inhibits p-glycoprotein and certain CYP450 enzymes, including CYP1A2, CYP2C9, CYP2D6, and CYP3A4. This inhibition can result in unexpectedly high plasma levels of other drugs which are metabolized by those CYP450 enzymes or are substrates of p-glycoprotein. Reported examples of this interaction include the following:
Immunosuppressives
Cyclosporine (CYP3A4 substrate) administered in combination with oral amiodarone has been reported to produce persistently elevated plasma concentrations of cyclosporine resulting in elevated creatinine, despite reduction in dose of cyclosporine.
HMG-CoA Reductase Inhibitors
Simvastatin (CYP3A4 substrate) in combination with amiodarone has been associated with reports of myopathy/rhabdomyolysis.
Cardiovasculars
Cardiac glycosides
In patients receiving digoxin therapy, administration of oral amiodarone regularly results in an increase in serum digoxin concentration that may reach toxic levels with resultant clinical toxicity. Amiodarone taken concomitantly with digoxin increases the serum digoxin concentration by 70% after one day. On administration of oral amiodarone, the need for digitalis therapy should be reviewed and the dose reduced by approximately 50% or discontinued. If digitalis treatment is continued, serum levels should be closely monitored and patients observed for clinical evidence of toxicity. These precautions probably should apply to digitoxin administration as well.
Antiarrhythmics
Other antiarrhythmic drugs, such as quinidine, procainamide, disopyramide, and phenytoin, have been used concurrently with amiodarone. There have been case reports of increased steady-state levels of quinidine, procainamide, and phenytoin during concomitant therapy with amiodarone. Phenytoin decreases serum amiodarone levels. Amiodarone taken concomitantly with quinidine increases quinidine serum concentration by 33% after two days. Amiodarone taken concomitantly with procainamide for less than seven days increases plasma concentrations of procainamide and n-acetyl procainamide by 55% and 33%, respectively. Quinidine and procainamide doses should be reduced by one-third when either is administered with amiodarone. Plasma levels of flecainide have been reported to increase in the presence of oral amiodarone; because of this, the dosage of flecainide should be adjusted when these drugs are administered concomitantly. In general, any added antiarrhythmic drug should be initiated at a lower than usual dose with careful monitoring. Combination of amiodarone with other antiarrhythmic therapy should be reserved for patients with life-threatening ventricular arrhythmias who are incompletely responsive to a single agent or incompletely responsive to amiodarone. During transfer to oral amiodarone, the dose levels of previously administered agents should be reduced by 30 to 50% several days after the addition of oral amiodarone (see DOSAGE AND ADMINISTRATION, Intravenous to Oral Transition). The continued need for the other antiarrhythmic agent should be reviewed after the effects of amiodarone have been established, and discontinuation ordinarily should be attempted. If the treatment is continued, these patients should be particularly carefully monitored for adverse effects, especially conduction disturbances and exacerbation of tachyarrhythmias, as amiodarone is continued. In amiodarone-treated patients who require additional antiarrhythmic therapy, the initial dose of such agents should be approximately half of the usual recommended dose.
Antihypertensives
Amiodarone should be used with caution in patients receiving ß-receptor blocking agents (e.g., propranolol, a CYP3A4 inhibitor) or calcium channel antagonists (e.g., verapamil, a CYP3A4 substrate, and diltiazem, a CYP3A4 inhibitor) because of the possible potentiation of bradycardia, sinus arrest, and AV block; if necessary, amiodarone can continue to be used after insertion of a pacemaker in patients with severe bradycardia or sinus arrest.
Anticoagulants
Potentiation of warfarin-type (CYP2C9 and CYP3A4 substrate) anticoagulant response is almost always seen in patients receiving amiodarone and can result in serious or fatal bleeding. Since the concomitant administration of warfarin with amiodarone increases the prothrombin time by 100% after 3 to 4 days, the dose of the anticoagulant should be reduced by one-third to one-half, and prothrombin times should be monitored closely.
Some drugs/substances are known to accelerate the metabolism of amiodarone by stimulating the synthesis of CYP3A4 (enzyme induction). This may lead to low amiodarone serum levels and potential decrease in efficacy. Reported examples of this interaction include the following:
Antibiotics
Rifampin is a potent inducer of CYP3A4. Administration of rifampin concomitantly with oral amiodarone has been shown to result in decreases in serum concentrations of amiodarone and desethylamiodarone.
Other substances, including herbal preparations
St. John’s Wort (Hypericum perforatum) induces CYP3A4. Since amiodarone is a substrate for CYP3A4, there is the potential that the use of St. John’s Wort in patients receiving amiodarone could result in reduced amiodarone levels.
Other reported interactions with amiodarone
Fentanyl (CYP3A4 substrate) in combination with amiodarone may cause hypotension, bradycardia, and decreased cardiac output.
Sinus bradycardia has been reported with oral amiodarone in combination with lidocaine (CYP3A4 substrate) given for local anesthesia. Seizure, associated with increased lidocaine concentrations, has been reported with concomitant administration of intravenous amiodarone.
Dextromethorphan is a substrate for both CYP2D6 and CYP3A4. Amiodarone inhibits CYP2D6.
Cholestyramine increases enterohepatic elimination of amiodarone and may reduce its serum levels and t1/2.
Disopyramide increases QT prolongation which could cause arrhythmia.
Fluoroquinolones, macrolide antibiotics, and azoles are known to cause QTc prolongation. There have been reports of QTc prolongation, with or without TdP, in patients taking amiodarone when fluoroquinolones, macrolide antibiotics, or azoles were administered concomitantly. (See PRECAUTIONS, Proarrhythmia).
Hemodynamic and electrophysiologic interactions have also been observed after concomitant administration with propranolol, diltiazem, and verapamil.
Volatile Anesthetic Agents: (see PRECAUTIONS, Surgery).
In addition to the interactions noted above, chronic (> 2 weeks) oral amiodarone administration impairs metabolism of phenytoin, dextromethorphan, and methotrexate.
Electrolyte Disturbances
Patients with hypokalemia or hypomagnesemia should have the condition corrected whenever possible before being treated with intravenous amiodarone, as these disorders can exaggerate the degree of QTc prolongation and increase the potential for torsades de pointes (TdP). Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or in patients receiving concomitant diuretics.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity studies were conducted with intravenous amiodarone. However, oral amiodarone caused a statistically significant, dose-related increase in the incidence of thyroid tumors (follicular adenoma and/or carcinoma) in rats. The incidence of thyroid tumors in rats was greater than the incidence in controls even at the lowest dose level tested i.e., 5 mg/kg/day (approximately 0.08 times the maximum recommended human maintenance dose*).
Mutagenicity studies conducted with amiodarone HCl (Ames, micronucleus, and lysogenic induction tests) were negative.
No fertility studies were conducted with intravenous amiodarone. However, in a study in which amiodarone HCl was orally administered to male and female rats, beginning 9 weeks prior to mating, reduced fertility was observed at a dose level of 90 mg/kg/day (approximately 1.4 times the maximum recommended human maintenance dose*).
*600 mg in a 50 kg patient (dose compared on a body surface area basis)
Category D. See WARNINGS, Neonatal Hypo- or Hyperthyroidism. In addition to causing infrequent congenital goiter/hypothyroidism and hyperthyroidism, amiodarone has caused a variety of adverse effects in animals.
In a reproductive study in which amiodarone was given intravenously to rabbits at dosages of 5, 10, or 25 mg/kg per day (about 0.1, 0.3, and 0.7 times the maximum recommended human dose [MRHD] on a body surface area basis), maternal deaths occurred in all groups, including controls. Embryotoxicity (as manifested by fewer full-term fetuses and increased resorptions with concomitantly lower litter weights) occurred at dosages of 10 mg/kg and above. No evidence of embryotoxicity was observed at 5 mg/kg and no teratogenicity was observed at any dosages.
In a teratology study in which amiodarone was administered by continuous i.v. infusion to rats at dosages of 25, 50, or 100 mg/kg per day (about 0.4, 0.7, and 1.4 times the MRHD when compared on a body surface area basis), maternal toxicity (as evidenced by reduced weight gain and food consumption) and embryotoxicity (as evidenced by increased resorptions, decreased live litter size, reduced body weights, and retarded sternum and metacarpal ossification) were observed in the 100 mg/kg group.
Intravenous amiodarone should be used during pregnancy only if the potential benefit to the mother justifies the risk to the fetus.
Nursing Mothers
Amiodarone and one of its major metabolites, desethylamiodarone (DEA), are excreted in human milk, suggesting that breast-feeding could expose the nursing infant to a significant dose of the drug. Nursing offspring of lactating rats administered amiodarone have demonstrated reduced viability and reduced body weight gains. The risk of exposing the infant to amiodarone should be weighed against the potential benefit of arrhythmia suppression in the mother. The mother should be advised to discontinue nursing.
Labor and Delivery
It is not known whether the use of amiodarone during labor or delivery has any immediate or delayed adverse effects. Preclinical studies in rodents have not shown any effect on the duration of gestation or on parturition.
Pediatric Use
The safety and efficacy of amiodarone in the pediatric population have not been established; therefore, its use in pediatric patients is not recommended. In a pediatric trial of 61 patients, aged 30 days to 15 years, hypotension (36%), bradycardia (20%), and atrio-ventricular block (15%) were common dose-related adverse events and were severe or life-threatening in some cases. Injection site reactions were seen in 5 (25%) of the 20 patients receiving amiodarone HCI injection through a peripheral vein irrespective of dose regimen.
Amiodarone HCl injection contains the preservative benzyl alcohol (see DESCRIPTION). There have been reports of fatal “gasping syndrome” in neonates (children less than one month of age) following the administration of intravenous solutions containing the preservative benzyl alcohol. Symptoms include a striking onset of gasping respiration, hypotension, bradycardia, and cardiovascular collapse.
Geriatric Use
Clinical studies of intravenous amiodarone did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
AMIODARONE HYDROCHLORIDE ADVERSE REACTIONS
In a total of 1836 patients in controlled and uncontrolled clinical trials, 14% of patients received intravenous amiodarone for at least 1 week, 5% received it for at least 2 weeks, 2% received it for at least 3 weeks, and 1% received it for more than 3 weeks, without an increased incidence of severe adverse reactions. The mean duration of therapy in these studies was 5.6 days; median exposure was 3.7 days.
The most important treatment-emergent adverse effects were hypotension, asystole/cardiac arrest/electromechanical dissociation (EMD), cardiogenic shock, congestive heart failure, bradycardia, liver function test abnormalities, VT, and AV block. Overall, treatment was discontinued for about 9% of the patients because of adverse effects. The most common adverse effects leading to discontinuation of intravenous amiodarone therapy were hypotension (1.6%), asystole/cardiac arrest/EMD (1.2%), VT (1.1%), and cardiogenic shock (1%).
The following table lists the most common (incidence ≥ 2%) treatment-emergent adverse events during intravenous amiodarone therapy considered at least possibly drug-related. These data were collected from the Wyeth-Ayerst clinical trials involving 1836 patients with life-threatening VT/VF. Data from all assigned treatment groups are pooled because none of the adverse events appeared to be dose-related.
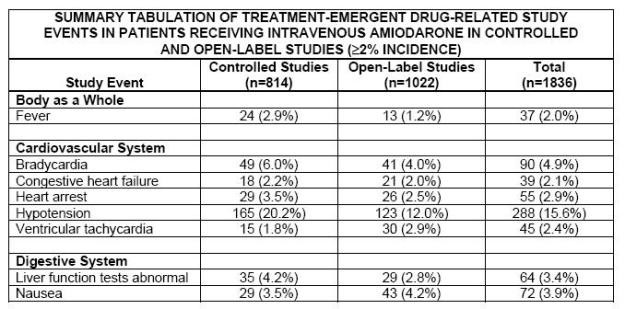
Other treatment-emergent possibly drug-related adverse events reported in less than 2% of patients receiving intravenous amiodarone in controlled and uncontrolled studies included the following: abnormal kidney function, atrial fibrillation, diarrhea, increased ALT, increased AST, lung edema, nodal arrhythmia, prolonged QT interval, respiratory disorder, shock, sinus bradycardia, Stevens-Johnson syndrome, thrombocytopenia, VF, and vomiting.
Postmarketing Reports
In postmarketing surveillance, hypotension (sometimes fatal), sinus arrest, pseudotumor cerebri, syndrome of inappropriate antidiuretic hormone secretion (SIADH), toxic epidermal necrolysis (sometimes fatal), exfoliative dermatitis, pancytopenia, neutropenia, erythema multiforme, angioedema, renal impairment, renal insufficiency, acute renal failure, bronchospasm, possibly fatal respiratory disorders (including distress, failure, arrest, and ARDS), fever, dyspnea, cough, hemoptysis, wheezing, hypoxia, pulmonary infiltrates and anaphylactic/anaphylactoid reaction (including shock), agranulocytosis, hallucination, confusional state, disorientation, and delirium also have been reported with amiodarone therapy.
Also, in patients receiving recommended dosages, there have been postmarketing reports of the following injection site reactions: pain, erythema, edema, pigment changes, venous thrombosis, phlebitis, thrombophlebitis, cellulitis, necrosis, and skin sloughing (see DOSAGE AND ADMINISTRATION).
OVERDOSAGE
There have been cases, some fatal, of amiodarone overdose. Effects of an inadvertent overdose of intravenous amiodarone include hypotension, cardiogenic shock, bradycardia, AV block, and hepatotoxicity. Hypotension and cardiogenic shock should be treated by slowing the infusion rate or with standard therapy: vasopressor drugs, positive inotropic agents, and volume expansion. Bradycardia and AV block may require temporary pacing. Hepatic enzyme concentrations should be monitored closely. Amiodarone is not dialyzable.
DOSAGE AND ADMINISTRATION
Amiodarone shows considerable interindividual variation in response. Thus, although a starting dose adequate to suppress life-threatening arrhythmias is needed, close monitoring with adjustment of dose as needed is essential. The recommended starting dose of intravenous amiodarone is about 1000 mg over the first 24 hours of therapy, delivered by the following infusion regimen:
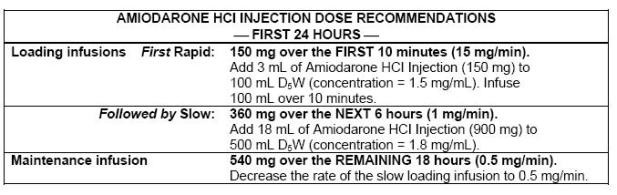
After the first 24 hours, the maintenance infusion rate of 0.5 mg/min (720 mg/24 hours) should be continued utilizing a concentration of 1 to 6 mg/mL (amiodarone HCl injection concentrations greater than 2 mg/mL should be administered via a central venous catheter). In the event of breakthrough episodes of VF or hemodynamically unstable VT, 150 mg supplemental infusions of amiodarone HCl injection mixed in 100 mL of D5W may be administered. Such infusions should be administered over 10 minutes to minimize the potential for hypotension. The rate of the maintenance infusion may be increased to achieve effective arrhythmia suppression.
The first 24-hour dose may be individualized for each patient; however, in controlled clinical trials, mean daily doses above 2100 mg were associated with an increased risk of hypotension. The initial infusion rate should not exceed 30 mg/min.
Based on the experience from clinical studies of amiodarone injection, a maintenance infusion of up to 0.5 mg/min can be cautiously continued for 2 to 3 weeks regardless of the patient’s age, renal function, or left ventricular function. There has been limited experience in patients receiving amiodarone injection for longer than 3 weeks.
The surface properties of solutions containing injectable amiodarone are altered such that the drop size may be reduced. This reduction may lead to underdosage of the patient by up to 30% if drop counter infusion sets are used. Amiodarone injection must be delivered by a volumetric infusion pump.
Amiodarone injection should, whenever possible, be administered through a central venous catheter dedicated to that purpose. An in-line filter should be used during administration.
Amiodarone injection loading infusions at much higher concentrations and rates of infusion much faster than recommended have resulted in hepatocellular necrosis and acute renal failure, leading to death (see PRECAUTIONS, Liver Enzymes Elevations).
Amiodarone HCl injection concentrations greater than 3 mg/mL in D5W have been associated with a high incidence of peripheral vein phlebitis; however, concentrations of 2.5 mg/mL or less appear to be less irritating. Therefore, for infusions longer than 1 hour, amiodarone HCl injection concentrations should not exceed 2 mg/mL unless a central venous catheter is used (See ADVERSE REACTIONS Postmarketing Reports).
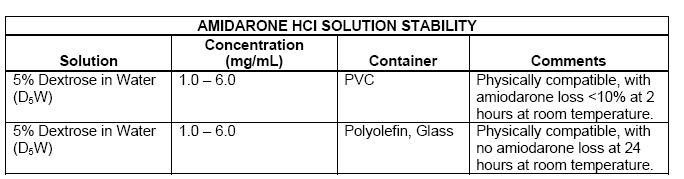
Amiodarone HCl injection infusions exceeding 2 hours must be administered in glass or polyolefin bottles containing D5W. Use of evacuated glass containers for admixing amiodarone HCl injection is not recommended as incompatibility with a buffer in the container may cause precipitation.
It is well known that amiodarone adsorbs to polyvinyl chloride (PVC) tubing and the clinical trial dose administration schedule was designed to account for this adsorption. All of the clinical trials were conducted using PVC tubing and its use is therefore recommended. The concentrations and rates of infusion provided in DOSAGE AND ADMINISTRATION reflect doses identified in these studies. Intravenous amiodarone has been found to leach out plasticizers, including DEHP [di-(2-ethylhexyl) phthalate] from intravenous tubing (including PVC tubing). The degree of leaching increases when infusing intravenous amiodarone at higher concentrations and lower flow rates than provided in DOSAGE AND ADMINISTRATION. In addition, polysorbate 80, a component of intravenous amiodarone, is also known to leach DEHP from PVC (see DESCRIPTION). Therefore, it is important that the recommendations in DOSAGE AND ADMINISTRATION be followed closely.
Intravenous amiodarone does not need to be protected from light during administration.
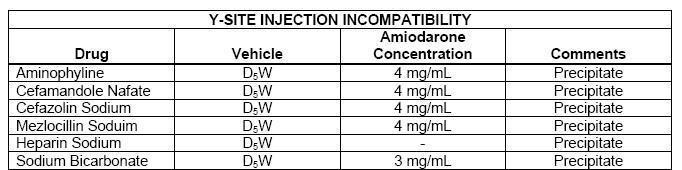
Admixture Incompatibility
Amiodarone HCI injection in D5W is incompatible with the drugs shown below.
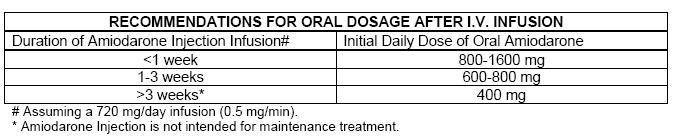
Intravenous to Oral Transition
Patients whose arrhythmias have been suppressed by intravenous amiodarone may be switched to oral amiodarone. The optimal dose for changing from intravenous to oral administration of amiodarone will depend on the dose of intravenous amiodarone already administered, as well as the bioavailability of oral amiodarone. When changing to oral amiodarone therapy, clinical monitoring is recommended, particularly for elderly patients.
Since there are some differences between the safety and efficacy profiles of the intravenous and oral formulations, the prescriber is advised to review the package insert for oral amiodarone when switching from intravenous to oral amiodarone therapy.
Since grapefruit juice is known to inhibit CYP3A4-mediated metabolism of oral amiodarone in the intestinal mucosa, resulting in increased plasma levels of amiodarone, grapefruit juice should not be taken during treatment with oral amiodarone (see PRECAUTIONS, Drug Interactions).
The following table provides suggested doses of oral amiodarone to be initiated after varying durations of intravenous amiodarone administration. These recommendations are made on the basis of a comparable total body amount of amiodarone delivered by the intravenous and oral routes, based on 50% bioavailability of oral amiodarone.
HOW SUPPLIED
Amiodarone Hydrochloride Injection, 50 mg/mL is supplied in:
3 mL (150 mg) 10 Single-dose vials per carton (NDC 60505-0722-0).
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Protect from light. Avoid excessive heat.
Use carton to protect contents from light until used.
Manufactured by:
Apotex Inc.
Toronto, Ontario
Canada M9L 1T9
Revised January 2006
225664
Amiodarone HydrochlorideAmiodarone Hydrochloride INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||