Amlodipine Besylate and Benazepril Hydrochloride
HIGHLIGHTS OF PRESCRIBING INFORMATION BOXED WARNING WARNING: AVOID USE IN PREGNANCY See full prescribing information for complete boxed warning When pregnancy is detected, discontinue amlodipine besylate and benazepril hydrochloride as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus (5.4) INDICATIONS AND USAGEAmlodipine besylate and benazepril hydrochloride capsules is a combination capsule of amlodipine, a dihydropyridine calcium channel blocker (DHP CCB) and benazepril, an angiotensin converting enzyme (ACE) inhibitor. Amlodipine besylate and benazepril hydrochloride capsules are indicated for the treatment of hypertension (1) in patients not adequately controlled on monotherapy with either agentDOSAGE AND ADMINISTRATION Dose once-daily May be used as add-on therapy for patients not adequately controlled with either a dihydropyridine calcium channel blocker or an ACE inhibitor (2.2) Patients who experience edema with amlodipine may be switched to amlodipine besylate and benazepril hydrochloride capsules containing a lower dose of amlodipine (2.2) Start amlodipine besylate and benazepril hydrochloride capsules at 2.5/10 mg in patients ≥75 years old or in patients with hepatic impairment (2.1) DOSAGE FORMS AND STRENGTHSCapsules (amlodipine/benazepril mg): 5/40, 10/40 (3)CONTRAINDICATIONSAmlodipine besylate and benazepril hydrochloride capsules are contraindicated in patients with a history of angioedema, with or without previous ACE inhibitor treatment, or patients who are hypersensitive to benazepril, to any other ACE inhibitor, or to amlodipine. (4)WARNINGS AND PRECAUTIONS Watch for anaphylactoid reactions, including angioedema (head, neck or intestinal). Warn patients with severe obstructive coronary artery disease about the risk of myocardial infarction or increased angina (5.2) Assess for hypotension and hyperkalemia (5.3 and 5.7) Titrate slowly in patients with impaired hepatic (5.5) or severely impaired renal (5.6) function. Side EffectsDiscontinuation because of adverse reactions occurred in 4% of amlodipine besylate and benazepril hydrochloride-treated patients and 3% of placebo-treated patients. The most common reasons for discontinuation of therapy with amlodipine besylate and benazepril hydrochloride were cough and edema. (6) To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories Inc. at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch . DRUG INTERACTIONS Potassium supplements / Potassium-sparing diuretics: risk of hyperkalemia Lithium: Increased serum lithium levels; toxicity symptoms Injectable gold: facial flushing, nausea, vomiting, or hypotension may occur USE IN SPECIFIC POPULATIONS Nursing Mothers: It is not known whether amlodipine is excreted in human milk. Nursing or drug should be discontinued. (8.3) See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling
FULL PRESCRIBING INFORMATION: CONTENTS*
- BOXED WARNING
- 1 AMLODIPINE BESYLATE AND BENAZEPRIL HYDROCHLORIDE INDICATIONS AND USAGE
- 2 AMLODIPINE BESYLATE AND BENAZEPRIL HYDROCHLORIDE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 AMLODIPINE BESYLATE AND BENAZEPRIL HYDROCHLORIDE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 AMLODIPINE BESYLATE AND BENAZEPRIL HYDROCHLORIDE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 AMLODIPINE BESYLATE AND BENAZEPRIL HYDROCHLORIDE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- 17.2 FDA-Approved Patient Labeling
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
BOXED WARNING
WARNING: AVOID USE IN PREGNANCY
When pregnancy is detected, discontinue amlodipine besylate and benazepril hydrochloride as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus (5.4)
1 INDICATIONS AND USAGE
{template}
Amlodipine besylate and benazepril hydrochloride capsules are indicated for the treatment of hypertension in patients not adequately controlled on monotherapy with either agent.
2 DOSAGE AND ADMINISTRATION
Amlodipine is an effective treatment of hypertension in once-daily doses of 2.5 mg to 10 mg while benazepril is effective in doses of 10 mg to 80 mg. In clinical trials of amlodipine/benazepril combination therapy using amlodipine doses of 2.5 mg to 10 mg and benazepril doses of 10 mg to 40 mg, the antihypertensive effects increased with increasing dose of amlodipine in all patient groups, and the effects increased with increasing dose of benazepril in nonblack groups.
The antihypertensive effect of amlodipine besylate and benazepril hydrochloride capsules is largely attained within 2 weeks.
It is usually appropriate to begin therapy with amlodipine besylate and benazepril hydrochloride capsules only after a patient has either (a) failed to achieve the desired antihypertensive effect with one or the other monotherapy, or (b) demonstrated inability to achieve adequate antihypertensive effect with amlodipine therapy without developing edema.
Renal Impairment: Regimens of therapy with amlodipine besylate and benazepril hydrochloride capsules need not take account of renal function as long as the patient’s creatinine clearance is >30 mL/min/1.73 m2 (serum creatinine roughly ≤3 mg/dL or 265 μmol/L). Amlodipine besylate and benazepril hydrochloride capsules are not recommended in patients with more severe renal impairment.
Hepatic Impairment and Elderly Patients: The recommended initial dose of amlodipine, as monotherapy or as a component of combination therapy, is 2.5 mg.
A patient whose blood pressure is not adequately controlled with amlodipine (or another dihydropyridine) alone or with benazepril (or another ACE inhibitor) alone may be switched to combination therapy with amlodipine besylate and benazepril hydrochloride capsules .
In patients whose blood pressure is adequately controlled with amlodipine but who experience unacceptable edema, combination therapy may achieve similar (or better) blood pressure control with less edema.
Amlodipine besylate and benazepril hydrochloride capsules may be substituted for the titrated components.
3 DOSAGE FORMS AND STRENGTHS
Amlodipine besylate and benazepril hydrochloride capsules are available as follows:
5/40 mg, and 10/40 mg.
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
{template}
Presumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors (including amlodipine besylate and benazepril hydrochloride) may be subject to a variety of adverse reactions, some of them serious. These reactions usually occur after one of the first few doses of the ACE inhibitor, but they sometimes do not appear until after months of therapy. Black patients receiving ACE inhibitors have a higher incidence of angioedema compared to nonblacks.
Head and Neck Angioedema: Angioedema of the face, extremities, lips, tongue, glottis, and larynx has been reported in patients treated with ACE inhibitors. In U.S. clinical trials, symptoms consistent with angioedema were seen in none of the subjects who received placebo and in about 0.5% of the subjects who received benazepril. Angioedema associated with laryngeal edema can be fatal. If laryngeal stridor or angioedema of the face, tongue, or glottis occurs, discontinue treatment with amlodipine besylate and benazepril hydrochloride and treat immediately. When involvement of the tongue, glottis, or larynx appears likely to cause airway obstruction, appropriate therapy, e.g., administer subcutaneous epinephrine injection 1:1000 (0.3-0.5 mL), promptly. [see Adverse Reactions (6)].
Intestinal Angioedema: Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor. Intestinal angioedema should be included in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
Anaphylactoid Reactions During Desensitization: Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Anaphylactoid Reactions During Membrane Exposure: Anaphylactoid reactions have been reported in patients dialyzed with high-flux membranes and treated concomitantly with an ACE inhibitor. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
Rarely, patients, particularly those with severe obstructive coronary artery disease, have developed documented increased frequency, duration or severity of angina or acute myocardial infarction on starting calcium channel blocker therapy or at the time of dosage increase. The mechanism of this effect has not been elucidated.
Amlodipine besylate and benazepril hydrochloride can cause symptomatic hypotension. Symptomatic hypotension is most likely to occur in patients who have been volume or salt depleted as a result of prolonged diuretic therapy, dietary salt restriction, dialysis, diarrhea, or vomiting.
In patients with congestive heart failure, with or without associated renal insufficiency, ACE inhibitor therapy may cause excessive hypotension, which may be associated with oliguria, azotemia, and (rarely) with acute renal failure and death. In such patients, start amlodipine besylate and benazepril hydrochloride therapy under close medical supervision; follow closely for the first 2 weeks of treatment and whenever the dose of the benazepril component is increased or a diuretic is added or its dose increased.
Symptomatic hypotension is also possible in patients with severe aortic stenosis.
If hypotension occurs, place the patient in a supine position, and if necessary, treat with intravenous infusion of physiologic saline. Amlodipine besylate and benazepril hydrochloride treatment usually can be continued following restoration of blood pressure and volume.
Amlodipine besylate and benazepril hydrochloride can cause fetal harm when administered to a pregnant woman. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Drugs that act on the renin angiotensin system can cause fetal and neonatal morbidity and mortality when used in pregnancy. In several dozen published cases, ACE inhibitor use during the second and third trimesters of pregnancy was associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death [see Use in Specific Populations (8.1)].
Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis and, sometimes, death. The mechanism of this syndrome is not understood. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up.
In patients with hepatic dysfunction due to cirrhosis, levels of benazeprilat are essentially unaltered.
However, since amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t1/2) is 56 hours in patients with hepatic function, titrate amlodipine besylate and benazepril hydrochloride slowly in patients with severe hepatic impairment.
Amlodipine besylate and benazepril hydrochloride should not be used in patients with severe renal disease (Clearance creatinine < 30 mL/min), (Dosage and Administration, 2)
In patients with severe heart failure, whose renal function may depend on the activity of the renin-angiotensin-aldosterone system, treatment with benazepril may be associated with oliguria or progressive azotemia and (rarely) with acute renal failure and/or death.
In a small study of hypertensive patients with unilateral or bilateral renal artery stenosis, treatment with benazepril was associated with increases in blood urea nitrogen and serum creatinine; these increases were reversible upon discontinuation of benazepril therapy, concomitant diuretic therapy, or both. When such patients are treated with amlodipine besylate and benazepril hydrochloride, monitor renal function during the first few weeks of therapy.
Some benazepril-treated hypertensive patients with no apparent preexisting renal vascular disease have developed increases in blood urea nitrogen and serum creatinine, usually minor and transient, especially when benazepril has been given concomitantly with a diuretic. Dosage reduction of amlodipine besylate and benazepril hydrochloride may be required.
Renal function should be monitored periodically in patients receiving benazepril.
In U.S. placebo-controlled trials of amlodipine besylate and benazepril hydrochloride, hyperkalemia (serum potassium at least 0.5 mEq/L greater than the upper limit of normal) not present at baseline occurred in approximately 1.5% of hypertensive patients receiving amlodipine besylate and benazepril hydrochloride. Increases in serum potassium were generally reversible. Risk factors for the development of hyperkalemia include renal insufficiency, diabetes mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salt substitutes. Serum potassium should be monitored periodically in patients receiving benazepril.
Presumably due to the inhibition of the degradation of endogenous bradykinin, persistent nonproductive cough has been reported with all ACE inhibitors, generally resolving after discontinuation of therapy. Consider ACE inhibitor-induced cough in the differential diagnosis of cough.
In patients undergoing surgery or during anesthesia with agents that produce hypotension, benazepril will block the angiotensin II formation that could otherwise occur secondary to compensatory renin release. Hypotension that occurs as a result of this mechanism can be corrected by volume expansion.
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Amlodipine besylate and benazepril hydrochloride has been evaluated for safety in over 2,991 patients with hypertension; over 500 of these patients were treated for at least 6 months, and over 400 were treated for more than 1 year.
In a pooled analysis of 5 placebo-controlled trials involving amlodipine besylate and benazepril hydrochloride doses up to 5/20, the reported side effects were generally mild and transient, and there was no relationship between side effects and age, sex, race, or duration of therapy. Discontinuation of therapy due to side effects was required in approximately 4% of patients treated with amlodipine besylate and benazepril hydrochloride and in 3% of patients treated with placebo.
The most common reasons for discontinuation of therapy with amlodipine besylate and benazepril hydrochloride in these studies were cough and edema (including angioedema).
The peripheral edema associated with amlodipine use is dose-dependent. When benazepril is added to a regimen of amlodipine, the incidence of edema is substantially reduced.
The addition of benazepril to a regimen of amlodipine should not be expected to provide additional antihypertensive effect in African-Americans. However, all patient groups benefit from the reduction in amlodipine-induced edema.
The side effects considered possibly or probably related to study drug that occurred in these trials in more than 1% of patients treated with amlodipine besylate and benazepril hydrochloride are shown in the table below. Cough was the only adverse event with at least possible relationship to treatment that was more common on amlodipine besylate and benazepril hydrochloride (3.3%) than on placebo (0.2%).
PERCENT INCIDENCE IN U.S. PLACEBO-CONTROLLED TRIALS
| Benazepril/ Amlodipine N=760 |
Benazepril N=554 |
Amlodipine N=475 |
Placebo N=408 |
|
| Cough | 3.3 | 1.8 | 0.4 | 0.2 |
| Headache | 2.2 | 3.8 | 2.9 | 5.6 |
| Dizziness | 1.3 | 1.6 | 2.3 | 1.5 |
| Edema* | 2.1 | 0.9 | 5.1 | 2.2 |
*Edema refers to all edema, such as dependent edema, angioedema, facial edema.
The incidence of edema was greater in patients treated with amlodipine monotherapy (5.1%) than in patients treated with amlodipine besylate and benazepril hydrochloride (2.1%) or placebo (2.2%).
Other side effects considered possibly or probably related to study drug that occurred in U.S. placebo-controlled trials of patients treated with amlodipine besylate and benazepril hydrochloride or in postmarketing experience were the following:
Body as a Whole: Asthenia and fatigue.
CNS: Insomnia, nervousness, anxiety, tremor, and decreased libido.
Dermatologic: Flushing, hot flashes, rash, skin nodule, and dermatitis.
Digestive: Dry mouth, nausea, abdominal pain, constipation, diarrhea, dyspepsia, and esophagitis.
Hematologic: Neutropenia
Metabolic and Nutritional: Hypokalemia.
Musculoskeletal: Back pain, musculoskeletal pain, cramps, and muscle cramps.
Respiratory: Pharyngitis.
Urogenital: Sexual problems such as impotence, and polyuria.
Monotherapies of benazepril and amlodipine have been evaluated for safety in clinical trials in over 6,000 and 11,000 patients, respectively. The observed adverse reactions to the monotherapies in these trials were similar to those seen in trials of amlodipine besylate and benazepril hydrochloride.
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
In postmarketing experience with benazepril, there have been rare reports of Stevens-Johnson syndrome, pancreatitis, hemolytic anemia, pemphigus, and thrombocytopenia. Gingival hyperplasia, tachycardia, jaundice and hepatic enzyme elevations (mostly consistent with cholestasis severe enough to require hospitalization) have been reported in association with use of amlodipine. Other potentially important adverse experiences attributed to other ACE inhibitors and calcium channel blockers include: eosinophilic pneumonitis (ACE inhibitors) and gynecomastia (CCBs). Other infrequently reported events included chest pain, ventricular extrasystole, gout, neuritis, tinnitus, alopecia, upper respiratory tract infection, palpitations and somnolence.
7 DRUG INTERACTIONS
{template}
Diuretics: Patients on diuretics, especially those in whom diuretic therapy was recently instituted, may occasionally experience an excessive reduction of blood pressure after initiation of therapy with amlodipine besylate and benazepril hydrochloride. The possibility of hypotensive effects with amlodipine besylate and benazepril hydrochloride can be minimized by either discontinuing the diuretic or increasing the salt intake prior to initiation of treatment with amlodipine besylate and benazepril hydrochloride.
Potassium Supplements and Potassium-Sparing Diuretics: Benazepril can attenuate potassium loss caused by thiazide diuretics. Potassium-sparing diuretics (spironolactone, amiloride, triamterene, and others) or potassium supplements can increase the risk of hyperkalemia. If concomitant use of such agents is indicated, the patient’s serum potassium should be monitored frequently.
Lithium: Increased serum lithium levels and symptoms of lithium toxicity have been reported in patients receiving ACE inhibitors during therapy with lithium. When coadministering amlodipine besylate and benazepril hydrochloride and lithium, frequent monitoring of serum lithium levels is recommended.
Gold: Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy.
Other: Benazepril has been used concomitantly with oral anticoagulants, beta-adrenergic-blocking agents, calcium-blocking agents, cimetidine, diuretics, digoxin, hydralazine, and naproxen without evidence of clinically important adverse interactions.
In clinical trials, amlodipine has been safely administered with thiazide diuretics, beta-blockers, ACE inhibitors, long-acting nitrates, sublingual nitroglycerin, digoxin, warfarin, nonsteroidal anti-inflammatory drugs, antibiotics, and oral hypoglycemic drugs.
In vitro data in human plasma indicate that amlodipine has no effect on the protein binding of drugs tested (digoxin, phenytoin, warfarin, and indomethacin). Special studies have indicated that the coadministration of amlodipine with digoxin did not change serum digoxin levels or digoxin renal clearance in normal volunteers; that coadministration with cimetidine did not alter the pharmacokinetics of amlodipine; and that coadministration with warfarin did not change thewarfarin-induced prothrombin response time.
Serum Electrolytes: [See Warnings and Precautions (5)].
Creatinine: Minor reversible increases in serum creatinine were observed in patients with essential hypertension treated with amlodipine besylate and benazepril hydrochloride. Increases in creatinine are more likely to occur in patients with renal insufficiency or those pretreated with a diuretic and, based on experience with other ACE inhibitors, would be expected to be especially likely in patients with renal artery stenosis [see Warnings and Precautions (5)].
Other (causal relationships unknown): Clinically important changes in standard laboratory tests were rarely associated with amlodipine besylate and benazepril hydrochloride administration. Elevations of serum bilirubin and uric acid have been reported as have scattered incidents of elevations of liver enzymes.
8 USE IN SPECIFIC POPULATIONS
{template}
8.1 Pregnancy
Pregnancy Category D [see Warnings and Precautions (5.4)]
The use of ACE inhibitors during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal renal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were due to the ACE inhibitor exposure.
In addition, use of ACE inhibitors during the first trimester of pregnancy has been associated with a potentially increased risk of birth defects. In women planning to become pregnant, ACE inhibitors (including benazepril) should not be used.
Make women of child-bearing age aware of the potential risk and give amlodipine besylate and benazepril hydrochloride only after careful counseling and consideration of individual risks and benefits.
Rarely (probably less often than once in every thousand pregnancies), no alternative to ACE inhibitors will be found. In these rare cases, apprise the mothers of the potential hazards to their fetuses, and perform serial ultrasound examinations to assess the intra-amniotic environment.
If oligohydramnios is observed, discontinue amlodipine besylate and benazepril hydrochloride unless it is considered life-saving for the mother. Contraction stress testing (CST), a nonstress test (NST), or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Closely observe infants with histories of in utero exposure to ACE inhibitors for hypotension, oliguria, and hyperkalemia. If oliguria occurs, direct attention toward support of blood pressure and renal perfusion. Exchange transfusion or peritoneal dialysis may be required as means of reversing hypotension or substituting for disordered renal function. Benazepril, which crosses the placenta, can theoretically be removed from the neonatal circulation by these means; there are occasional reports of benefit from these maneuvers, but experience is limited.
8.2 Labor and Delivery
The effect of amlodipine besylate and benazepril hydrochloride on labor and delivery has not been studied.
8.3 Nursing Mothers
Minimal amounts of unchanged benazepril and of benazeprilat are excreted into the breast milk of lactating women treated with benazepril, so that a newborn child ingesting nothing but breast milk would receive less than 0.1% of the maternal doses of benazepril and benazeprilat.
It is not known whether amlodipine is excreted in human milk. Nursing or drug should be discontinued.
8.4 Pediatric Use
Safety and effectiveness of amlodipine besylate and benazepril hydrochloride in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of patients who received amlodipine besylate and benazepril hydrochloride in U.S. clinical studies of amlodipine besylate and benazepril hydrochloride, over 19% were 65 or older while about 2% were 75 or older. Overall differences in effectiveness or safety were not observed between these patients and younger patients. Clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Benazepril and benazeprilat are substantially excreted by the kidney. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Amlodipine is extensively metabolized in the liver. In the elderly, clearance of amlodipine is decreased with resulting increases in peak plasma levels, elimination half-life and area-under-the-plasma-concentration curve. Thus a lower starting dose may be required in older patients [see Dosage and Administration (2)].
10 OVERDOSAGE
Only a few cases of human overdose with amlodipine have been reported. One patient was asymptomatic after a 250 mg ingestion; another, who combined 70 mg of amlodipine with an unknown large quantity of a benzodiazepine, developed refractory shock and died.
Human overdoses with any combination of amlodipine and benazepril have not been reported. In scattered reports of human overdoses with benazepril and other ACE inhibitors, there are no reports of death.
Treatment: To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison-Control Center. Telephone numbers of certified poison-control centers are listed in the Physicians’ Desk Reference (PDR). In managing overdose, consider the possibilities of multiple-drug overdoses, drug-drug interactions, and unusual drug kinetics in your patient.
The most likely effect of overdose with amlodipine besylate and benazepril hydrochloride is vasodilation, with consequent hypotension and tachycardia. Simple repletion of central fluid volume (Trendelenburg positioning, infusion of crystalloids) may be sufficient therapy, but pressor agents (norepinephrine or high-dose dopamine) may be required. With abrupt return of peripheral vascular tone, overdoses of other dihydropyridine calcium channel blockers have sometimes progressed to pulmonary edema, andpatients must be monitored for this complication.
Analyses of bodily fluids for concentrations of amlodipine, benazepril, or their metabolites are not widely available. Such analyses are, in any event, not known to be of value in therapy or prognosis.
No data are available to suggest physiologic maneuvers (e.g., maneuvers to change the pH of the urine) that might accelerate elimination of amlodipine, benazepril, or their metabolites. Benazeprilat is only slightly dialyzable; attempted clearance of amlodipine by hemodialysis or hemo-perfusion has not been reported, but amlodipine’s high protein binding makes it unlikely that these interventions will be of value.
Angiotensin II could presumably serve as a specific antagonist-antidote to benazepril, but angiotensin II is essentially unavailable outside of scattered research laboratories.
11 DESCRIPTION
Amlodipine besylate and benazepril hydrochloride capsules is a combination of amlodipine besylate and benazepril hydrochloride. Benazepril hydrochloride is a white to off-white crystalline powder, soluble (>100 mg/mL) in water, in ethanol, and in methanol. Benazepril hydrochloride’s chemical name is 3-[[1-(ethoxycarbonyl)-3-phenyl-(1S)- propyl]amino]-2,3,4,5-tetrahydro-2-oxo-1H-1-(3S)-benzazepine-1-acetic acid monohydrochloride; its structural formula is
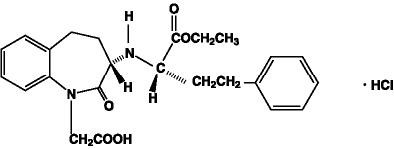
Its molecular formula is C24H28N2O5•HCl, and its molecular weight is 460.96.
Benazeprilat, the active metabolite of benazepril, is a nonsulfhydryl angiotensin-converting enzyme (ACE) inhibitor. Benazepril is converted to benazeprilat by hepatic cleavage of the ester group. Amlodipine besylate is a white to pale yellow crystalline powder, slightly soluble in water and sparingly soluble in ethanol. Its chemical name is (R,S)3-ethyl-5-methyl-2-(2-aminoethoxymethyl)-4-(2-chlorophenyl)-1,4- dihydro-6-methyl-3,5-pyridinedicarboxylate benzenesulfonate; its structural formula is
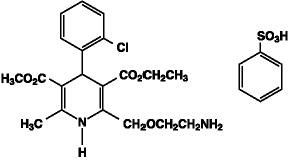
Its molecular formula is C20H25ClN2O5•C6H6O3S, and its molecular weight is 567.1.
Amlodipine besylate is the besylate salt of amlodipine, a dihydropyridine calcium channel blocker. Amlodipine besylate and benazepril hydrochloride capsules are formulated in four different strengths for oral administration with a combination of amlodipine besylate equivalent to 5 mg or 10 mg of amlodipine, with 40 mg of benazepril hydrochloride providing for the following available combinations:5 mg/40 mg and 10 mg/40 mg.
The inactive ingredients of the capsules are colloidal silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium starch glycolate and talc. Each hard gelatin capsule contains D & C Yellow 10, D & C Red 28 (only for 10 mg/40 mg), FD & C Blue 1, FD & C Red 40, FD & C Yellow 6 (only for 5 mg/40 mg), gelatin, sodium lauryl sulfate, titanium dioxide.
12 CLINICAL PHARMACOLOGY
{template}
12.1 Mechanism of Action
Benazepril
Benazepril and benazeprilat inhibit angiotensin-converting enzyme (ACE) in human subjects and in animals. ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex.
Inhibition of ACE results in decreased plasma angiotensin II, which leads to decreased vasopressor activity and to decreased aldosterone secretion. The latter decrease may result in a small increase of serum potassium. Hypertensive patients treated with benazepril and amlodipine for up to 56 weeks had elevations of serum potassium up to 0.2 mEq/L [see Warnings and Precautions (5)].
Removal of angiotensin II negative feedback on renin secretion leads to increased plasma renin activity. In animal studies, benazepril had no inhibitory effect on the vasopressor response to angiotensin II and did not interfere with the hemodynamic effects of the autonomic neurotransmitters acetylcholine, epinephrine, and norepinephrine.
ACE is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasodepressor peptide, play a role in the therapeutic effects of amlodipine besylate and benazepril hydrochloride remains to be elucidated.
While the mechanism through which benazepril lowers blood pressure is believed to be primarily suppression of the renin-angiotensin-aldosterone system, benazepril has an antihypertensive effect even in patients with low-renin hypertension.
Amlodipine
Amlodipine is a dihydropyridine calcium antagonist (calcium ion antagonist or slow channel blocker) that inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac muscle. Experimental data suggest that amlodipine binds to both dihydropyridine and nondihydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic effects can be detected in vitro but such effects have not been seen in intact animals at therapeutic doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range, amlodipine is an ionized compound (pKa=8.6), and its kinetic interaction with the calcium channel receptor is characterized by a gradual rate of association and dissociation with the receptor binding site, resulting in a gradual onset of effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause a reduction in peripheral vascular resistance and reduction in blood pressure.
12.2 Pharmacodynamics
Benazepril
Single and multiple doses of 10 mg or more of benazepril cause inhibition of plasma ACE activity by at least 80%-90% for at least 24 hours after dosing. For up to 4 hours after a 10 mg dose, pressor responses to exogenous angiotensin I were inhibited by 60%-90%.
Administration of benazepril to patients with mild-to-moderate hypertension results in a reduction of both supine and standing blood pressure to about the same extent, with no compensatory tachycardia. Symptomatic postural hypotension is infrequent, although it can occur in patients who are salt and/or volume depleted [see Warnings and Precautions (5)].
The antihypertensive effects of benazepril were not appreciably different in patients receiving high- or low-sodium diets.
In normal human volunteers, single doses of benazepril caused an increase in renal blood flow but had no effect on glomerular filtration rate.
Amlodipine
Following administration of therapeutic doses to patients with hypertension, amlodipine produces vasodilation resulting in a reduction of supine and standing blood pressures. These decreases in blood pressure are not accompanied by a significant change in heart rate or plasma catecholamine levels with chronic dosing. Plasma concentrations correlate with effect in both young and elderly patients.
As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine have generally demonstrated a small increase in cardiac index without significant influence on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine has not been associated with a negative inotropic effect when administered in the therapeutic dose range to intact animals and humans, even when coadministered with beta blockers to humans.
Amlodipine does not change sinoatrial (SA) nodal function or atrioventricular (AV) conduction in intact animals or humans. In clinical studies in which amlodipine was administered in combination with beta blockers to patients with either hypertension or angina, no adverse effects on electrocardiographic parameters were observed.
12.3 Pharmacokinetics
The rate and extent of absorption of benazepril and amlodipine from amlodipine besylate and benazepril hydrochloride are not significantly different, respectively, from the rate and extent of absorption of benazepril and amlodipine from individual tablet formulations. Absorption from the individual tablets is not influenced by the presence of food in the gastrointestinal tract; food effects on absorption from amlodipine besylate and benazepril hydrochloride have not been studied.
Following oral administration of amlodipine besylate and benazepril hydrochloride, peak plasma concentrations of benazepril are reached in 0.5-2 hours. Cleavage of the ester group (primarily in the liver) converts benazepril to its active metabolite, benazeprilat, which reaches peak plasma concentrations in 1.5-4 hours. The extent of absorption of benazepril is at least 37%.
Peak plasma concentrations of amlodipine are reached 6-12 hours after administration of amlodipine besylate and benazepril hydrochloride; the extent of absorption is 64%-90%.
The apparent volumes of distribution of amlodipine and benazeprilat are about 21 L/kg and 0.7 L/kg, respectively. Approximately 93% of circulating amlodipine is bound to plasma proteins, and the bound fraction of benazeprilat is slightly higher. On the basis of in vitro studies, benazeprilat’s degree of protein binding should be unaffected by age, by hepatic dysfunction, or—over the therapeutic concentration range—by concentration.
Benazeprilat has much greater ACE-inhibitory activity than benazepril, and the metabolism of benazepril to benazeprilat is almost complete. Only trace amounts of an administered dose of benazepril can be recovered unchanged in the urine; about 20% of the dose is excreted as benazeprilat, 8% as benazeprilat glucuronide, and 4% as benazepril glucuronide.
Amlodipine is extensively metabolized in the liver, with 10% of the parent compound and 60% of the metabolites excreted in the urine. In patients with hepatic dysfunction, decreased clearance of amlodipine may increase the area-under-the-plasma-concentration curve by 40%-60%, and dosage reduction may be required (see DOSAGE AND ADMINISTRATION). In patients with renal impairment, the pharmacokinetics of amlodipine are essentially unaffected.
Benazeprilat’s effective elimination half-life is 10-11 hours, while that of amlodipine is about 2 days, so steady-state levels of the two components are achieved after about a week of once-daily dosing. The clearance of benazeprilat from the plasma is primarily renal, but biliary excretion accounts for 11%-12% of benazepril elimination in normal subjects. In patients with severe renal insufficiency (creatinine clearance less than 30 mL/min), peak benazeprilat levels and the time to steady state may be increased (see DOSAGE AND ADMINISTRATION). In patients with hepatic impairment, on the other hand, the pharmacokinetics of benazeprilat are essentially unaffected.
Although the pharmacokinetics of benazepril and benazeprilat are unaffected by age, clearance of amlodipine is decreased in the elderly, with resulting increases of 35%-70% in peak plasma levels, elimination half-life, and area-under-the-plasma-concentration curve. Dose adjustment may be required.
13 NONCLINICAL TOXICOLOGY
{template}
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Carcinogenicity and mutagenicity studies have not been conducted with this combination. However, these studies have been conducted with amlodipine and benazepril alone (see below). No adverse effects on fertility occurred when the benazepril:amlodipine combination was given orally to rats of either sex at doses up to 15:7.5 mg (benazepril:amlodipine)/kg/day, prior to mating and throughout gestation.
Benazepril
No evidence of carcinogenicity was found when benazepril was administered to rats and mice for up to two years at doses of up to 150 mg/kg/day. When compared on the basis of body surface area, this dose is 18 and 9 times (rats and mice, respectively) the maximum recommended human dose (calculations assume a patient weight of 60 kg). No mutagenic activity was detected in the Ames test in bacteria, in an in vitro test for forward mutations in cultured mammalian cells, or in a nucleus anomaly test. At doses of 50 mg/kg/day to 500 mg/kg/day (6-60 times the maximum recommended human dose on a body surface area basis), benazepril had no adverse effect on the reproductive performance of male and female rats.
Amlodipine
Rats and mice treated with amlodipine maleate in the diet for up to two years, at concentrations calculated to provide daily dosage levels of 0.5 mg, 1.25 mg, and 2.5 mg amlodipine/kg/day, showed no evidence of a carcinogenic effect of the drug. For the mouse, the highest dose was, on a body surface area basis, similar to the maximum recommended human dose [MRHD] of 10 mg amlodipine/day. For the rat, the highest dose was, on a body surface area basis, about two and a half times the MRHD. (Calculations based on a 60 kg patient.) Mutagenicity studies conducted with amlodipine maleate revealed no drug-related effects at either the gene or chromosome level. There was no effect on the fertility of rats treated orally with amlodipine maleate (males for 64 days and females for 14 days prior to mating) at doses of up to 10 mg amlodipine/kg/day (about 10 times the MRHD of 10 mg/day on a body surface area basis).
When rats received benazepril:amlodipine at doses ranging from 5:2.5 mg/kg/day to 50:25 mg/kg/day, dystocia was observed at an increasing dose-related incidence at all doses tested. On a body surface area basis, the 2.5 mg/kg/day dose of amlodipine is 3.6 times the amlodipine dose delivered when the maximum recommended dose of amlodipine besylate and benazepril hydrochloride is given to a 50 kg woman. Similarly, the 5 mg/kg/day dose of benazepril is approximately twice the benazepril dose delivered when the maximum recommended dose of amlodipine besylate and benazepril hydrochloride is given to a 50 kg woman. No teratogenic effects were seen when benazepril and amlodipine were administered in combination to pregnant rats or rabbits. Rats received doses of up to 50:25 mg (benazepril:amlodipine)/kg/day (24 times the maximum recommended human dose on a body surface area basis, assuming a 50 kg woman). Rabbits received doses of up to 1.5:0.75 mg/kg/day (equivalent to the maximum recommended dose of amlodipine besylate and benazepril hydrochloride given to a 50 kg woman).
Benazepril
No teratogenic effects of benazepril were seen in studies of pregnant rats, mice, and rabbits. On a body surface area basis, the maximum doses used in these studies were 60 times (in rats), 9 times (in mice), and about equivalent to (in rabbits) the maximum recommended human dose (assuming a 50 kg woman).
Amlodipine
No evidence of teratogenicity or other embryo/fetal toxicity was found when pregnant rats and rabbits were treated orally with amlodipine maleate at doses of up to 10 mg amlodipine/kg/day (respectively, about 10 and 20 times the maximum recommended human dose [MRHD] of 10 mg amlodipine on a body surface area basis) during their respective periods of major organogenesis. (Calculations based on a patient weight of 60 kg.) However, litter size was significantly decreased (by about 50%) and the number of intrauterine deaths was significantly increased (about 5-fold) for rats receiving amlodipine maleate at a dose equivalent to 10 mg amlodipine/kg/day for 14 days before mating and throughout mating and gestation. Amlodipine maleate has been shown to prolong both the gestation period and the duration of labor in rats at this dose. There are no adequate and well-controlled studies in pregnant women. Amlodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
14 CLINICAL STUDIES
Over 950 patients received amlodipine besylate and benazepril hydrochloride once daily in six double-blind, placebo-controlled studies. The antihypertensive effect of a single dose persisted for 24 hours, with peak reductions achieved 2-8 hours after dosing.
Once-daily doses of benazepril/amlodipine using benazepril doses of 10 mg to 20 mg and amlodipine doses of 2.5 mg to 10 mg decreased seated pressure (systolic/diastolic) 24 hours after dosing by about 10-25/6-13 mmHg.
In two studies in patients not adequately controlled on either benazepril 40 mg alone (n=329) or amlodipine 10 mg alone (n=812) once daily doses of amlodipine besylate and benazepril hydrochloride 10/40 mg further decreased seated blood pressure compared to the respective monotherapy alone.
Combination therapy was effective in blacks and nonblacks. Both components contributed to the antihypertensive efficacy in nonblacks, but virtually all of the antihypertensive effect in blacks could be attributed to the amlodipine component. Among nonblack patients in placebo-controlled trials comparing amlodipine besylate and benazepril hydrochloride to the individual components, the blood pressure lowering effects of the combination were shown to be additive and in some cases synergistic.
During chronic therapy with amlodipine besylate and benazepril hydrochloride, the maximum reduction in blood pressure with any given dose is generally achieved after 1-2 weeks. The antihypertensive effects of amlodipine besylate and benazepril hydrochloride have continued during therapy for at least 1 year. Abrupt withdrawal of amlodipine besylate and benazepril hydrochloride has not been associated with a rapid increase in blood pressure.
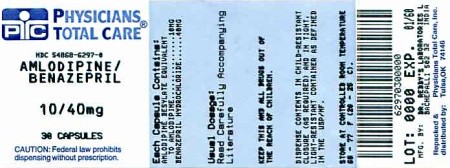
16 HOW SUPPLIED/STORAGE AND HANDLING
Amlodipine besylate and benazepril hydrochloride is available as capsules containing amlodipine besylate equivalent to 10 mg of amlodipine, with 40 mg of benazepril hydrochloride providing for the following available combinations: 10 mg/40 mg.
Amlodipine besylate and benazepril hydrochloride capsules, 10 mg/40 mg contain white to off-white powder and size “4” hard gelatin capsules of white opaque color cap and white opaque color body, filled in size “1” hard gelatin capsule with purple opaque color cap and ivory opaque color body, imprinted “RDY” on cap and “586” on body with black ink and are supplied in bottles of 30, 100 and 500.
| Bottles of 30 |
NDC 54868-6297-0 |
Storage: Store at 20°-25°C (68°-77°F); [See USP Controlled Room Temperature.]Protect from moisture. Dispense in tight container (USP).
17 PATIENT COUNSELING INFORMATION
{template}
Pregnancy: Tell female patients of childbearing age that use of drugs like benazepril that act on the renin-angiotensin system can cause serious problems in the fetus and infant including: low blood pressure, poor development of skull bones, kidney failure and death. Discuss other treatment options with female patients planning to become pregnant. Tell women using amlodipine besylate and benazepril hydrochloride who become pregnant to notify their physicians as soon as possible.
17.2 FDA-Approved Patient Labeling
Patient Information
Amlodipine Besylate and Benazepril Hydrochloride Capsules, 5 mg/40 mg, 10 mg/40 mg
Read this Patient Information leaflet before you start taking amlodipine besylate and benazepril hydrochloride capsules and each time you get a refill. There may be new information. This leaflet does not replace talking with your doctor. If you have any questions, ask your doctor or pharmacist.
What is the most important information I should know about amlodipine besylate and benazepril hydrochloride capsules?
Amlodipine besylate and benazepril hydrochloride capsules can harm an unborn baby and even cause death. If you get pregnant, stop taking amlodipine besylate and benazepril hydrochloride capsules. Call your doctor right away. Talk to your doctor about other ways to lower your blood pressure if you plan to become pregnant.
What is amlodipine besylate and benazepril hydrochloride capsules?
Amlodipine besylate and benazepril hydrochloride capsules contains two prescription medicines that work together to lower blood pressure: amlodipine besylate (the active ingredient found in Norvasc®), a calcium channel blocker, and benazepril hydrochloride (Lotensin®), an ACE inhibitor. Your doctor will prescribe amlodipine besylate and benazepril hydrochloride capsules only after other medicines haven’t worked.
High Blood Pressure (hypertension). Blood pressure is the force of blood in your blood vessels. You have high blood pressure when the force is too much. Amlodipine besylate and benazepril hydrochloride capsules can help your blood vessels relax so your blood pressure is lower.
Amlodipine besylate and benazepril hydrochloride capsules has not been studied in children.
Who should not take amlodipine besylate and benazepril hydrochloride capsules?
Don’t take amlodipine besylate and benazepril hydrochloride capsules if you are allergic to any of the ingredients. There is a complete list at the end of this leaflet.
What should I tell my Doctor before taking amlodipine besylate and benazepril hydrochloride capsules?
Tell your doctor about all your medical conditions, including if:
• you are pregnant or plan to become pregnant. See “What is the most important information I should know about amlodipine besylate and benazepril hydrochloride capsules?”
• you are breastfeeding. Amlodipine besylate and benazepril hydrochloride capsules may pass into your milk. Don’t breastfeed while you are taking amlodipine besylate and benazepril hydrochloride capsules.
• you have a heart condition
• you have liver problems
• you have kidney problems
• you have diabetes (high blood sugar)
• you have systemic lupus erythematosus (SLE), scleroderma or a collagen vascular disease. Ask your doctor if you are not sure.
Keep a list of your medicines with you, including vitamins and natural or herbal remedies, to show your doctor or pharmacist. Some of your other medicines and amlodipine besylate and benazepril hydrochloride capsules could affect each other, causing serious side effects. Tell your doctor about all your medicines, especially:
• medicines for high blood pressure or heart failure
• water pills, extra potassium or a salt substitute
• Lithium (Eskalith®, Lithobid®)
How do I take amlodipine besylate and benazepril hydrochloride capsules?
• Take amlodipine besylate and benazepril hydrochloride capsules exactly as your doctor tells you.
• Take amlodipine besylate and benazepril hydrochloride capsules at the same time each day, with or without food.
• If you miss a dose, take it as soon as you remember. If it is more than 12 hours, just take your next dose at the regular time.
• Your doctor may test for kidney problems or check your blood potassium level.
• If you take too much amlodipine besylate and benazepril hydrochloride capsules, call your doctor or Poison Control Center, or go to the emergency room.
• Tell all your doctors or dentist you are taking amlodipine besylate and benazepril hydrochloride capsules if you:
- are going to have surgery
- are getting allergy shots for bee stings
- go for kidney dialysis
What are the possible side effects of amlodipine besylate and benazepril hydrochloride capsules?
Amlodipine besylate and benazepril hydrochloride capsules can cause serious side effects including:
• serious allergic reactions that can be life threatening.
Stop amlodipine besylate and benazepril hydrochloride capsules and get emergency help right away if you get:
- swelling of your face, eyelids, lips, tongue or throat
- have trouble swallowing
- asthma (wheezing) or other breathing problems
These allergic reactions are rare but happen more times in people who are African-American.
• low blood pressure (hypotension). Low blood pressure is most likely to happen if you also take water pills, are on a low salt diet, get dialysis treatments, have heart problems or get sick with vomiting or diarrhea. Lie down if you feel faint or dizzy.
• liver problems. Call your doctor if:
• you have nausea
• you feel more tired or weaker than usual
• you have itching
• your skin or eyes look yellow
• you have pain in your upper right stomach
• you have flu-like symptoms
• low white blood cells. Low white blood cells happen more in people who have kidney problems and collagen vascular diseases. Low white blood cells can give you a higher chance for getting infections. Call your doctor if you get a fever, sore throat, or other signs of infection that do not go away.
• kidney problems. Kidney problems may get worse in people that already have kidney disease. Some people will have changes on blood tests for kidney function and need a lower dose of amlodipine besylate and benazepril hydrochloride capsules. Call your doctor if you get swelling in your feet, ankles, or hands or unexplained weight gain.
• more chest pain and heart attacks in people that already have severe heart problems. Get emergency help if you get worse chest pain or chest pain that does not go away.
The more common side effects of amlodipine besylate and benazepril hydrochloride capsules are:
• Cough
• Dizziness
• Headache
• Swelling of the feet, ankles, and hands
These are not all the side effects of amlodipine besylate and benazepril hydrochloride capsules. For a complete list, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA 1088 or by visiting www.fda.gov/medwatch.
How do I store amlodipine besylate and benazepril hydrochloride capsules?
• Store amlodipine besylate and benazepril hydrochloride capsules at 20°-25°C (68°-77°F); [See USP Controlled Room Temperature.]
• Keep amlodipine besylate and benazepril hydrochloride capsules in a closed container in a dry place.
• Keep amlodipine besylate and benazepril hydrochloride capsules and all medicines out of the reach of children.
General Information about amlodipine besylate and benazepril hydrochloride capsules
Doctors can also use medicine for a condition that is not in the patient information leaflet. Take amlodipine besylate and benazepril hydrochloride capsules the way your doctor tells you. Do not share it with other people. It may harm them.
For more information, ask your doctor or pharmacist, or call 1-888-375-3784.
What are the ingredients in amlodipine besylate and benazepril hydrochloride capsules?
Active ingredients: amlodipine besylate, benazepril hydrochloride USP.
Inactive ingredients: colloidal silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium starch glycolate and talc. Each hard gelatin capsule contains gelatin, titanium dioxide, sodium lauryl sulfate, D & C Yellow 10, FD & C Blue 1, FD & C Red 40, FD & C Yellow 6 (only for 5 mg/40 mg), D & C Red 28 (only for 10 mg/40 mg).
Norvasc® is a registered trademark of Pfizer, Inc..
Lotensin® is a registered trademark of Novartis Corp.
Eskalith® and Lithobid® are registered trademarks of Noven Therapeutics, LLC..
To reorder additional Patient Information Leaflets, please contact Dr. Reddy’s Customer Service at1-866-733-3952.
Manufactured by:
Dr. Reddy’s Laboratories Limited
Bachepalli – 502 325 INDIA
Issued: 0111
Relabeling and Repackaging by:
Physicians Total Care, Inc.
Tulsa, OK 74146
PRINCIPAL DISPLAY PANEL
Amlodipine Besylate and Benazepril Hydrochloride Capsules
10 mg/40 mg
Amlodipine Besylate and Benazepril HydrochlorideAmlodipine Besylate and Benazepril Hydrochloride CAPSULE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||