Aralast
ARALAST NP[alpha-proteinase inhibitor (human)]Solvent Detergent TreatedNanofiltered
FULL PRESCRIBING INFORMATION: CONTENTS*
- ARALAST DESCRIPTION
- CLINICAL PHARMACOLOGY
- ARALAST INDICATIONS AND USAGE
- ARALAST CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- ARALAST ADVERSE REACTIONS
- ARALAST DOSAGE AND ADMINISTRATION
- RECONSTITUTION
- HOW SUPPLIED
- STORAGE
- REFERENCES
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
ARALAST DESCRIPTION
ARALAST NP is a sterile, stable, lyophilized preparation of purified human alpha1–proteinase inhibitor (α1–PI), also known as alpha1–antitrypsin.1 ARALAST NP is a similar product to ARALAST, containing the same active components of plasma α1-PI with identical formulations.
ARALAST NP is prepared from large pools of human plasma by using the cold ethanol fractionation process, followed by purification steps including polyethylene glycol and zinc chloride precipitations and ion exchange chromatography. All U.S. licensed α1-PI plasma derived products contain chemical modifications which arise during manufacturing and occur in varying levels from product to product.11 ARALAST NP contains approximately 2% α1-PI with truncated C-terminal lysine (removal of Lys394), whereas ARALAST contains approximately 67% α1-PI with the C-terminal lysine truncation.12 No known data suggest influence of these structural modifications on the functional activity and immunogenicity of α1-PI.13
To reduce the risk of viral transmission, the manufacturing process includes treatment with a solvent detergent (S/D) mixture [tri–n–butyl phosphate and polysorbate 80] to inactivate enveloped viral agents such as human immunodeficiency virus (HIV), hepatitis B (HBV), and hepatitis C (HCV). In addition, a nanofiltration step is incorporated into the manufacturing process to reduce the risk of transmission of enveloped and non–enveloped viral agents. Based on in vitro studies, the process used to produce ARALAST NP has been shown to inactivate and/or partition various viruses as shown in Table 1 below.2
| Processing Step | Virus Log Reduction Factors | ||||
| HIV-1 | BVDV | PRV | HAV | MMV | |
| Cold ethanol fractionation | 4.6 | 1.4 | 2.1 | 1.4 |
< 1.0 |
| Solvent Detergent-treatment | > 5.8 | > 6.0 | > 5.5 |
N/A |
N/A |
| 15 N nanofiltration | > 5.3 | > 6.0 | > 5.6 | > 5.1 | 4.9 |
| Overall reduction factor | > 15.7 | > 13.4 | > 13.2 | > 6.5 | 4.9 |
| HIV-1: Human immunodeficiency virus-1, BVDV (Bovine Viral Diarrhea Virus, model for Hepatitis C Virus and other lipid enveloped RNA viruses), PRV (Pseudorabies Virus, model for lipid-enveloped DNA viruses, to wich also hepatitis B belongs): HAV: Hepatitus A Virus, MMV (Mice Minute Virus, model for small non-lipid enveloped DNA viruses) | |||||
The unreconstituted, lyophilized cake should be white or off-white to slightly yellow-green or yellow in color. When reconstituted as directed, the concentration of functionally active α1–PI is ≥16 mg/mL and the specific activity is ≥0.55 mg active α1–PI/mg total protein. The composition of the reconstituted product is as follows:
| Component | Quality/mL |
| Elastase Inhibitory Activity | ≥400 mg Active α1–PI/0.5 g vial* |
| ≥800 mg Active α1–PI/1.0 g vial** | |
| Albumin | ≤5 mg/mL |
| Polyethylene Glycol | ≤112 µg/mL |
| Polysorbate 80 | ≤50 µg/mL |
| Sodium | ≤230 mEq/L |
| Tri-n-buyl Phosphate | ≤1.0 µg/mL |
| Zinc | ≤3 ppm |
| * Reconstitution volume: 25mL/0.5 g vial
** Reconstitution volume: 50mL/1.0 g vial |
|
Each vial of ARALAST NP is labeled with the amount of functionally active α1–PI expressed in mg/vial. The formulation contains no preservative. The pH of the solution ranges from 7.2 to 7.8. Product must only be administered intravenously.
CLINICAL PHARMACOLOGY
ARALAST NP functions in the lungs to inhibit serine proteases such as neutrophil elastase (NE), which is capable of degrading protein components of the alveolar walls and which is chronically present in the lung. In the normal lung, α1–PI is thought to provide more than 90% of the anti–NE protection in the lower respiratory tract.3,4
α1–PI deficiency is an autosomal, co-dominant, hereditary disorder characterized by low serum and lung levels of α1–PI.1,3,5,6 Severe forms of the deficiency are frequently associated with slowly progressive, moderate-to-severe panacinar emphysema that most often manifests in the third to fourth decades of life, resulting in a significantly lower life expectancy.1,3,4,6,7 However, an unknown percentage of individuals with severe α1–PI deficiency are not diagnosed with or may never develop clinically evident emphysema during their lifetimes. Individuals with α1–PI deficiency have little protection against NE released by a chronic, low–level of neutrophils in their lower respiratory tract, resulting in a protease:protease inhibitor imbalance in the lung.3,8 The emphysema associated with severe α1–PI deficiency is typically worse in the lower lung zones.5 It is believed to develop because there are insufficient amounts of α1–PI in the lower respiratory tract to inhibit NE. This imbalance allows relatively unopposed destruction of the connective tissue framework of the lung parenchyma.8
There are a large number of phenotypic variants of this
disorder.1,3,4 Individuals with the PiZZ variant
typically have serum α1–PI levels less than 35% of the
average normal level.1,5 Individuals with the Pi(null)(null)
variant have undetectable α1–PI protein in their
serum.1,3 Individuals with these low serum
α1-PI levels, i.e., less than 11 µM, have an increased risk
of developing emphysema over their lifetimes. In addition, PiSZ
individuals, whose serum α1-PI levels range from
approximately 9 to 23 μΜ14, are considered to have moderately
increased risk for developing emphysema, regardless of whether their
serum α1-PI levels are above or below
11 μΜ. Two
Registry studies have shown 54% and 72% of α1-PI deficient
individuals had emphysema and pulmonary symptoms such as cough, phlegm,
wheeze, breathlessness, and chest colds, respectively.9,10
The risk of accelerated development and progression of emphysema in
individuals with severe α1–PI deficiency is higher in smokers
than in ex-smokers or non-smokers.3
Not all individuals with severe genetic variants of α1-PI deficiency have emphysema. Augmentation therapy with Alpha1-Proteinase Inhibitor (Human) is indicated only in patients with congenital α1-PI deficiency who have clinically evident emphysema.
Augmenting the levels of functional α1-proteinase inhibitor by intravenous infusion is an approach to therapy for patients with α1-PI deficiency. However, the efficacy of augmentation therapy in affecting the progression of emphysema has not been demonstrated in randomized, controlled clinical trials. The intended theoretical goal is to provide protection to the lower respiratory tract by correcting the imbalance between neutrophil elastase and protease inhibitors. Whether augmentation therapy with ARALAST NP actually protects the lower respiratory tract from progressive emphysematous changes has not been evaluated. Although the maintenance of blood serum levels of α1-PI (antigenically measured) above 11 µM has been historically postulated to provide therapeutically relevant anti-neutrophil elastase protection, this has not been proven. Individuals with severe α1-PI deficiency have been shown to have increased neutrophil and neutrophil elastase concentrations in lung epithelial lining fluid compared to normal PiMM individuals, and some PiSZ individuals with α1-PI above 11 µM have emphysema attributed to α1-PI deficiency. These observations underscore the uncertainty regarding the appropriate therapeutic target serum level of α1-PI during augmentation therapy. The clinical benefit of the increased blood levels of Alpha1-Proteinase Inhibitor at the recommended dose has not been established.
The clinical efficacy of ARALAST NP in influencing the course of pulmonary emphysema or the frequency, duration, or severity of pulmonary exacerbations has not been demonstrated in randomized, controlled clinical trials.
Pharmacokinetics
The pharmacokinetics of ARALAST NP were compared with ARALAST in a multicenter, single-dose, randomized, double-blind, crossover clinical study (Study 460501). Twenty-five subjects with congenital α1-PI deficiency received a single intravenous (IV) infusion of 60 mg/kg ARALAST NP or ARALAST. The 25 subjects in this study were between 20 and 75 years old, with a median age of 59. Plasma α1-PI concentrations were measured using an enzyme linked immunosorbent assay (ELISA). Figure 1 shows that the mean ± standard deviation (SD) plasma α1-PI concentration-time profiles after a single IV infusion of ARALAST NP and ARALAST at 60 mg/kg were comparable. Table 2 summarizes the pharmacokinetic parameters of ARALAST NP and ARALAST. The 90% confidence intervals for Cmax and AUC 0 inf/dose were well within the pre-defined acceptance limits of 80 to 125%.

| Parameters | Units | Aralast NP | Aralast |
| Cmax | mg/mL | 1.6 ± 0.3 | 1.7 ± 0.3 |
| AUC0-inf/dose | days*kg/mL | 0.0868 ± 0.0253 | 0.0920 ± 0.0238 |
| Half-life | days | 4.7 ± 2.7 | 4.8 ± 2.0 |
| Clearance | mL/day | 940 ± 275 | 862 ± 206 |
| Vss | mL | 5632 ± 2006 | 5618 ± 1618 |
| Cmax = Maximum increase in plasma
α1-PI concentration following
infusion; AUC0-inf/dose = Area under the curve from time 0 to infinity divided by dose; Half life = terminal phase half-life determined using non-compartmental method; Vss = Volume of distribution at steady state. |
|||
A clinical study (ATC 97-01) was conducted to compare ARALAST to a commercially available preparation of α1–PI (Prolastin®, manufactured by Bayer Corporation). All subjects were to have been diagnosed as having congenital α1–PI deficiency and emphysema but no α1–PI augmentation therapy within the preceding six months.
Twenty-eight subjects were randomized to receive either ARALAST or Prolastin®, 60 mg/kg intravenously per week, for 10 consecutive weeks. Two subjects withdrew from the study prematurely: 1 subject receiving ARALAST withdrew consent after 6 infusions; 1 subject receiving Prolastin® withdrew after 1 infusion due to pneumonia following unscheduled bronchoscopy to remove a foreign body. Trough levels of α1–PI (antigenic determination) and anti–NE capacity (functional determination) were measured prior to treatment at Weeks 8 through 11. Following their first 10 weekly infusions, the subjects who were receiving Prolastin® were switched to ARALAST while those who already were receiving ARALAST continued to receive it. Maintenance of mean serum α1–PI trough levels was assessed prior to treatments at Weeks 12 through 24. Bronchoalveolar lavages (BALs) were performed on subjects at baseline and prior to treatment at Week 7. The epithelial lining fluid (ELF) from each BAL meeting acceptance criteria was analyzed for the α1–PI level and anti–NE capacity.
With weekly augmentation therapy with ARALAST or Prolastin®, a gradual increase in peak and trough serum α1–PI levels was noted, with stabilization after several weeks. The metabolic half–life of ARALAST was 5.9 days. Serum anti–NE capacity trough levels rose substantially in all subjects by Week 2, and by Week 3, serum anti–NE capacity trough levels exceeded 11 µM in the majority of subjects. With few exceptions, levels remained above this recommended threshold level in individual subjects for the duration of the period Weeks 3 through 24 on study. Although only five of fourteen subjects (35.7%) receiving ARALAST had BALs meeting acceptance criteria for analysis at both baseline and Week 7, a statistically significant increase in the antigenic level of α1–PI in the ELF was observed. No statistically significant increase in the anti-NE capacity in the ELF was detected.
Viral serology of all subjects was determined periodically throughout the study, including testing for antibodies to hepatitis A (HAV) and C (HCV), presence of circulating HBsAg, and presence of antibodies to HIV–1, HIV–2, and Parvovirus B–19. Subjects who were seronegative to parvovirus B–19 at enrollment were retested by PCR at Week 2. There were no seroconversions in subjects treated with ARALAST through Week 24. None of the subjects became HBsAg positive during the study, although five of 13 (38%) evaluable subjects treated with ARALAST and eight of 13 (62%) treated with Prolastin® had not been vaccinated to hepatitis B. No patient developed antibodies against α1–PI.
It was concluded that at a dose of 60 mg/kg administered intravenously once weekly, ARALAST and Prolastin® had similar effects in maintaining target serum α1–PI trough levels and increasing antigenic levels of α1–PI in epithelial lining fluid (ELF) with maintenance augmentation therapy.
ARALAST INDICATIONS AND USAGE
Congenital Alpha–Proteinase Inhibitor deficiency
ARALAST NP is indicated for chronic augmentation therapy in patients having congenital deficiency of α1–PI with clinically evident emphysema. Clinical and biochemical studies have demonstrated that with such therapy, ARALAST is effective in maintaining target serum α1–PI trough levels and increasing α1–PI levels in epithelial lining fluid (ELF). ARALAST NP pharmacokinetics are comparable with the pharmacokinetics of ARALAST after single-dose administration in 25 subjects with congenital deficiency of α1–PI. Clinical data demonstrating the long–term effects of chronic augmentation or replacement therapy of individuals with ARALAST NP or ARALAST are not available.
The effect of augmentation therapy with ARALAST NP on pulmonary exacerbations and on the progression of emphysema in alpha1-antitrypsin deficiency has not been demonstrated in randomized, controlled clinical trials.
ARALAST NP is not indicated as therapy for lung disease patients in whom congenital α1–PI deficiency has not been established.
ARALAST CONTRAINDICATIONS
ARALAST NP is contraindicated in IgA deficient patients with antibodies against IgA, due to the risk of severe hypersensitivity.
WARNINGS
Because ARALAST NP is derived from pooled human plasma, it may carry a risk of transmitting infectious agents, e.g., viruses and theoretically, the Creutzfeldt–Jakob disease (CJD) agent. Stringent procedures designed to reduce the risk of adventitious agent transmission have been employed in the manufacture of this product, from the screening of plasma donors and the collection and testing of plasma through the application of viral elimination/reduction steps such as ethanol fractionation, PEG precipitation, solvent detergent treatment, and nanofiltration. Despite these measures, such products can still potentially transmit disease; therefore, the risk of infectious agents cannot be totally eliminated. ALL infections thought by a physician possibly to have been transmitted by this product should be reported to the manufacturer at 1-800-423-2090 (US). The physician should weigh the risks and benefits of the use of this product and should discuss these with the patient.
ARALAST NP may contain trace amounts of IgA. Patients with known antibodies to IgA, which can be present in patients with selective or severe IgA deficiency, have a greater risk of developing potentially severe hypersensitivity and anaphylactic reactions. ARALAST NP is contraindicated in patients with antibodies against IgA due to risk of severe hypersensitivity.
The rate of administration specified in DOSAGE AND ADMINISTRATION should be closely followed, at least until the physician has had sufficient experience with a given patient. Vital signs should be monitored continuously and the patient should be carefully observed throughout the infusion. IF ANAPHYLACTIC OR SEVERE ANAPHYLACTOID REACTIONS OCCUR, THE INFUSION SHOULD BE DISCONTINUED IMMEDIATELY. Epinephrine and other appropriate supportive therapy should be available for the treatment of any acute anaphylactic or anaphylactoid reaction.
PRECAUTIONS
General
ARALAST NP should be administered at room temperature within three (3) hours after reconstitution. Partially used vials should be discarded and not saved for future use. The solution contains no preservative.
ARALAST NP should be administered alone, without mixing with other agents or diluting solutions.
Pregnancy Category C
Animal reproduction studies have not been conducted with ARALAST NP. It is also not known whether ARALAST NP can cause fetal harm when administered to pregnant women or can affect reproductive capacity.
Nursing Mothers
It is not known whether alpha1-proteinase inhibitor is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ARALAST NP is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical studies of ARALAST NP did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. As for all patients, dosing for geriatric patients should be appropriate to their overall situation. Safety and effectiveness in patients over age 65 years of age have not been established.
Information for Patients
Inform patients that administration of ARALAST NP has been demonstrated to raise the plasma level of α1-PI, but that the effect of this augmentation on the frequency of pulmonary exacerbations and on the rate of progression of emphysema has not been established by clinical trials.
ARALAST ADVERSE REACTIONS
The safety of ARALAST NP was evaluated with ARALAST after a single dose IV infusion in a multicenter, randomized, double-blind, crossover clinical PK comparability study (Study 460501). The number of subjects with one or more adverse events, regardless of causality, was 23 of 25 (92%) when receiving ARALAST NP and 19 of 25 (76%) when receiving ARALAST. Treatment-related adverse events were reported in 8 of 25 subjects (32%) for ARALAST NP and 7 of 25 subjects (28%) for ARALAST. Of a total of 61 adverse events reported for ARALAST NP, 43 (70%) were mild, 16 (26%) moderate, and 2 (3%) severe. Seventeen of 61 (28%) adverse events were deemed possibly or probably related to ARALAST NP of which 14 (82%) were mild and 3 (18%) were moderate. Of a total of 60 adverse events reported for ARALAST, 45 (75%) were mild, 12 (20%) moderate, and 3 (5%) severe. Eleven of 60 (18%) adverse events were deemed possibly or probably related to ARALAST of which 8 (73%) were mild and 3 (27%) were moderate. No serious adverse events or deaths were reported in the study. No clinically significant changes in the peri-infusion vital signs (blood pressure, heart rate, or respiratory rate) were reported. The most common adverse events deemed related to ARALAST NP included: headache (4 of 61 [7%] events) and musculoskeletal discomfort (4 of 61 [7%] events). These adverse events, as well as most of the other adverse events, were also reported in subjects treated with ARALAST.
In Clinical Study ATC 97-01, ARALAST was evaluated for up to 96 weeks in 27 subjects with a congenital deficiency of α1–PI and clinically evident emphysema. The number of subjects with an adverse event, regardless of causality, was 22 of 27 (81.5%). The number of subjects with an adverse event deemed possibly, probably, or definitely related to study drug was 7 of 27 (25.9%).
The frequency of infusions associated with an adverse event, regardless of causality, was 108 of 1127 (9.6%) infusions administered per protocol. The most common symptoms were pharyngitis (1.6%), headache (0.7%), and increased cough (0.6%). Symptoms of bronchitis, sinusitis, pain, rash, back pain, viral infection, peripheral edema, bloating, dizziness, somnolence, asthma, and rhinitis were each associated with ≥0.2% but < 0.6% of infusions. All symptoms were mild to moderate in severity.
The overall frequency of adverse events deemed to be possibly, probably, or definitely related to study drug was 15 of 1127 (1.3%) infusions. The most common symptoms included headache (0.3%) and somnolence (0.3%). Symptoms of chills and fever, vasodilation, dizziness, pruritus, rash, abnormal vision, chest pain, increased cough, and dyspnea were each associated with one (0.1%) infusion. Five (5) of 27 (18.5%) subjects experienced eight (8) serious adverse reactions during the study. None of these serious adverse events were considered to be causally related to the administration of ARALAST.
Twenty-six (26) of 27 (96.3%) subjects experienced a total of 94 upper and lower respiratory-tract infections during the 96-week study (median: 3.0; range: 1 to 8; mean ± SD: 3.6 ± 2.3 infections). Twenty-eight (29.8%) of the respiratory infections occurred in 19 (70.4%) subjects during the first 24 weeks of the 96-week study suggesting that the risk of infection did not change with time on ARALAST. In a post-hoc analysis, subjects experienced a range of 0 to 8 exacerbations of COPD over the 96-week study with a median of less than one exacerbation per year (median: 0.61; mean ± SD: 0.83 ± 0.87 exacerbations per year).
Treatment-emergent elevations (> two times the upper limit of normal) in aminotransferases (ALT or AST), up to 3.7 times the upper limit of normal, were noted in 3 of 27 (11.1%) subjects. Elevations were transient lasting three months or less. No subject developed any evidence of viral hepatitis or hepatitis seroconversion while being treated with ARALAST, including 13 evaluable subjects who were not vaccinated against hepatitis B.
No clinically relevant alterations in blood pressure, heart rate, respiratory rate, or body temperature occurred during infusion of ARALAST. Mean hematology and laboratory parameters were little changed over the duration of the study, with individual variations not clinically meaningful.
During the initial 10 weeks of the study, subjects were randomized to receive either ARALAST or a commercially available preparation of α1-PI (Prolastin®). The overall frequency, severity and symptomatology of adverse reactions were similar in both the ARALAST and Prolastin® groups. There were two serious adverse events in the Prolastin® group, both of which were considered to be possibly related to Prolastin®. These included chest pain, dyspnea and bilateral pulmonary infiltrates in one individual that withdrew from the study prematurely following an unscheduled bronchoscopy to remove a foreign body and the other, a positive seroconversion to Parvovirus B-19. There were no serious adverse events or seroconversions reported for the ARALAST group during the 96 week study period. No subject developed an antibody to α1–PI.
ARALAST DOSAGE AND ADMINISTRATION
Dose ranging studies using efficacy endpoints have not been performed.
Chronic Augmentation Therapy
FOR INTRAVENOUS USE ONLY. The recommended dosage of ARALAST NP is 60 mg/kg body weight administered once weekly by intravenous infusion. Each vial of ARALAST NP has the functional activity, as determined by inhibition of porcine pancreatic elastase, stated on the label. Administration of ARALAST NP within three hours after reconstitution is recommended to avoid the potential ill effect of any inadvertent microbial contamination occurring during reconstitution. Discard any unused contents.
Infusion Rate
ARALAST NP should be administered at a rate not exceeding 0.08 mL/kg body weight/minute. If adverse events occur, the rate should be reduced or the infusion interrupted until the symptoms subside. The infusion may then be resumed at a rate tolerated by the subject.
RECONSTITUTION
Use Aseptic Technique
1. ARALAST NP and diluent should be at room temperature before reconstitution.
2. Remove caps from the diluent and product vials.
3. Swab the exposed stopper surfaces with alcohol.
4. Remove cover from one end of the double–ended transfer needle. Insert the exposed end of the needle through the center of the stopper in the DILUENT vial.
5. Remove plastic cap from the other end of the double–ended transfer needle now seated in the stopper of the diluent vial. To reduce any foaming, invert the vial of diluent and insert the exposed end of the needle through the center of the stopper in the PRODUCT vial at an angle, making certain that the diluent vial is always above the product vial. The angle of insertion directs the flow of diluent against the side of the product vial. Refer to Figure below. The vacuum in the vial is sufficient to allow transfer of all of the diluent.

6. Disconnect the two vials by removing the transfer needle from the diluent vial stopper. Remove the double–ended transfer needle from the product vial and discard the needle into the appropriate safety container.
7. Let the vial stand until most of the contents is in solution, then GENTLY swirl until the powder is completely dissolved. Reconstitution requires no more than five minutes for a 0.5 gram vial and no more than 10 minutes for a 1.0 gram vial.
8. DO NOT SHAKE THE CONTENTS OF THE VIAL. DO NOT INVERT THE VIAL UNTIL READY TO WITHDRAW CONTENTS.
9. Use within three hours of reconstitution.
10. Inspect parenteral drug products visually for particulate matter and discoloration prior to administration. The reconstituted product should be a colorless or slightly yellow to yellowish-green solution. When reconstitution procedure is strictly followed, a few small visible particles may occasionally remain. These will be removed by the microaggregate filter.
11. Reconstituted product from several vials may be pooled into an empty, sterile IV solution container by using aseptic technique. A sterile 20 micron filter is provided for this purpose.
HOW SUPPLIED
ARALAST NP is supplied as a sterile, non-pyrogenic, lyophilized powder in single–dose vials. The following product packages are available: 0.5 g (NDC 0944-2802-01) and 1 g (NDC 0944-2802-02). A suitable volume of Sterile Water for Injection, USP diluent is provided (25 mL/0.5 g vial; 50 mL/1 g vial). Each vial is labeled with the total α1–PI functional activity in mg. ARALAST NP is packaged with a sterile double–ended transfer needle and a sterile 20-micron filter.
STORAGE
ARALAST NP should be stored at temperatures not to exceed 25°C (77°F). Do not freeze. Do not use after the expiration date printed on the label.
Rx only
REFERENCES
- Brantly M, Nukiwa T, Crystal RG. Molecular basis of alpha–1–antitrypsin deficiency. Am J Med 1988 (Suppl 6A);84:13–31.
- Data on file at Baxter Healthcare Corporation.
- Crystal RG, Brantly ML, Hubbard RC, Curiel DT, et al. The alpha1–antitrypsin gene and its mutations: Clinical consequences and strategies for therapy. Chest 1989;95:196–208.
- Crystal RG. α1–Antitrypsin deficiency: pathogenesis and treatment. Hospital Practice 1991;Feb.15:81–94.
- Hutchison DCS. Natural history of alpha–1–protease inhibitor deficiency. Am J Med 1988;84(Suppl 6A):3–12.
- Hubbard RC, Crystal RG. Alpha–1–antitrypsin augmentation therapy for alpha–1– antitrypsin deficiency. Am J Med 1988;84(Suppl 6A):52–62.
- Buist SA, Burrows B, Cohen A, et al. Guidelines for the approach to the patient with severe hereditary alpha–1–antitrypsin deficiency. Am Rev Respir Dis 1989;140:1494–1497.
- Gadek JE, Fells GA, Zimmerman RL, et al. Antielastases of the human alveolar structures: Implications for the protease-antiprotease theory of emphysema. J Clin Invest 1981;68:889-898.
- Stoller JK, Brantly M, Fleming LE, et al. Formation and current results of a patient-organized registry for α1–antitrypsin deficiency. Chest 2000; 118(3):843-848.
- McElvaney NG, Stoller JK, Buist AS, et al. Baseline characteristics of enrollees in the National Heart, Lung and Blood Institute Registry of α1-antitrypsin deficiency. Chest 1997;111:394-403.
- FDA/CBER “Heterogeneity of Alpha-1-Proteinase Inhibitor Products”
27 Mar 2006
- Kolarich D, et al. Biochemical, molecular characterization, and glycoproteomic analyses of α1-proteinase inhibitor products used for replacement therapy. Transfusion 2006;46:1959-1977.
- Transcript of Blood Products Advisory Committee (BPAC) 85th Meeting; 3-4 Nov 2005.
- Turino GM, Barker AF, Brantly ML, et al: Clinical features of individuals with Pi*SZ phenotype of α1-antitrypsin deficiency. Am J Respir Crit Care Med 154: 1718-25, 1996.
BAXTER and ARALAST NP are trademarks of Baxter International Inc.
U.S. Patent No.: 5,616,693; 5,981,715 Other U.S. Patents Pending
DATE OF REVISION: Apr 2010
Baxter Healthcare Corporation
Westlake Village, CA 91362
U.S. License No. 140
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
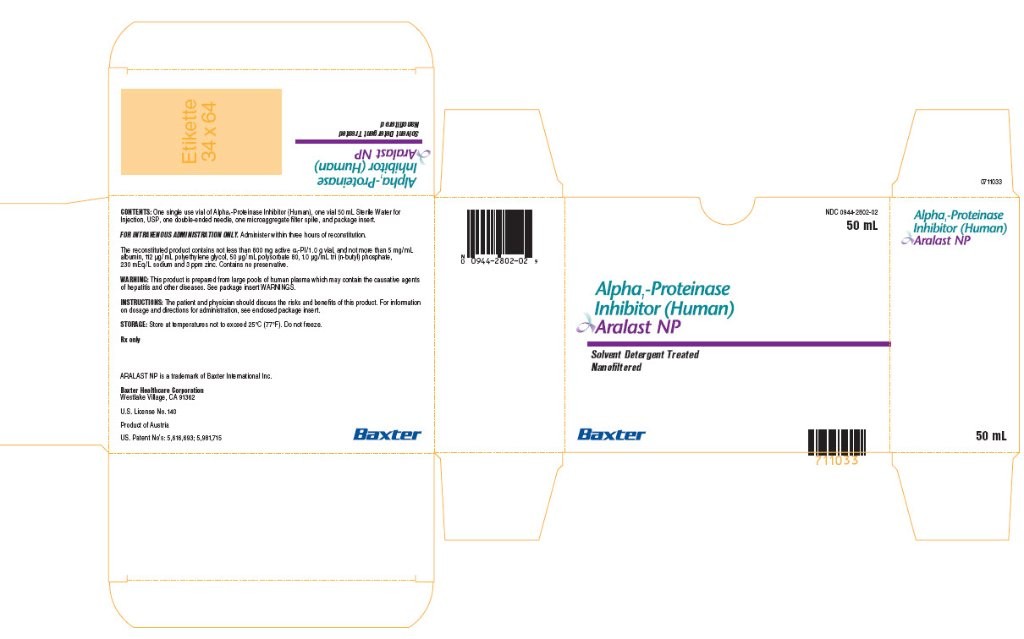
NDC 0944-2802-04
50 mL
Alpha1-Proteinase Inhibitor (Human)
Aralast NP
Solvent Detergent Treated
Nanofiltered
ARALAST NP is a trademark of Baxter International Inc.
Baxter (logo)
Aralastalpha-1 proteinase inhibitor human KIT
| ||||||||||||||||||||||||||||||||||||||||