Arcapta Neohaler
Novartis Pharmaceuticals Corporation
HIGHLIGHTS OF PRESCRIBING INFORMATION ARCAPTA™ NEOHALER™ (indacaterol inhalation powder) RECENT MAJOR CHANGESContraindications (4) 09/2012Warnings and Precautions, Immediate Hypersensitivity Reactions (5.4) 09/2012BOXED WARNING WARNING : ASTHMA-RELATED DEATH See full prescribing information for complete boxed warning L ong -acting beta 2 -adrenergic agonist s (LABA) increase the risk of asthma-related death (5.1) . A placebo-controlled study with another long-acting beta 2 -adrenergic agonist (salmeterol) showed an increase in asthma-related deaths in patients receiving salmeterol. (5.1) This finding of an increased risk of asthma-related death with salmeterol is considered a class effect of LABA, including indacaterol , the active ingredient in ARCAPTA NEOHALER . The safety and efficacy of ARCAPTA NEOHALER in patients with asthma have not been established . A RCAPTA NEOHALER is not indicated for the treatment of asthma. ( 4, 5.1) INDICATIONS AND USAGEARCAPTA NEOHALER is a long-acting beta2-adrenergic agonist indicated for: The long term, once-daily maintenance bronchodilator treatment of airflow obstruction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema. (1.1) Important limitations: ARCAPTA NEOHALER is NOT indicated to treat acute deteriorations of chronic obstructive pulmonary disease. (1.2) ARCAPTA NEOHALER is NOT indicated for asthma. (1.2) DOSAGE AND ADMINISTRATIONFor oral inhalation only. DO NOT swallow ARCAPTA capsule. ARCAPTA capsules should always be used with the NEOHALER inhaler only.75 mcg inhaled every day (once-daily). (2)DOSAGE FORMS AND STRENGTHSInhalation powder hard capsules: 75 mcg. (3) CONTRAINDICATIONS All LABA are contraindicated in patients with asthma without use of a long-term asthma control medication. (4) ARCAPTA NEOHALER is not indicated for the treatment of asthma. ARCAPTA NEOHALER is contraindicated in patients with a history of hypersensitivity to indacaterol or to any of the ingredients. (4) WARNINGS AND PRECAUTIONS Do not initiate in acutely deteriorating COPD patients (5.2) Do not use for relief of acute symptoms. Concomitant short-acting beta2-agonists can be used as needed for acute relief (5.2) Do not exceed the recommended dose. Excessive use or use in conjunction with other medications containing LABA can result in clinically significant cardiovascular effects and may be fatal (5.3) Immediate hypersensitivity reactions may occur. Discontinue immediately. (5.4) Life-threatening paradoxical bronchospasm can occur. Discontinue immediately. (5.5) Use with caution in patients with cardiovascular or convulsive disorders, thyrotoxicosis or sensitivity to sympathomimetic drugs. (5.6, 5.7) Side EffectsMost common adverse reactions (>2% and more common than placebo) are cough, oropharyngeal pain, nasopharyngitis, headache and nausea. (6) To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Other adrenergic drugs may potentiate effect: Use with caution. (5.3, 7.1) Xanthine derivatives, steroids, diuretics or non-potassium sparing diuretics may potentiate hypokalemia or ECG changes. Use with caution. (7.2, 7.3) MAO inhibitors, tricyclic antidepressants, and drugs that prolong QTc interval may potentiate effect on cardiovascular system. Use with extreme caution. (7.4) Beta-blockers may decrease effectiveness: Use with caution and only when medically necessary. (7.5)
FULL PRESCRIBING INFORMATION
L ong-acting beta 2 -adrenergic agonist s (LABA) increase the risk of asthma-related death. Data from a large placebo-controlled US study that compared the safety of another long-acting beta 2 -adrenergic agonist (salmeterol) or placebo added to usual asthma therapy showed an increase in asthma-related deaths in patients receiving salmeterol. This finding with salmeterol is considered a class effect of LABA, including indacaterol, the active ingredient in ARCAPTA NEOHALER . The safety and efficacy of ARCAPTA NEOHALER in patients with asthma have not been established. A RCAPTA NEOHALER is not indicated for the treatment of asthma. [See C ontraindications (4), W arnings and Precautions (5.1) ] .
1.1 Maintenance Treatment of COPD
ARCAPTA NEOHALER is a long-acting beta2-agonist indicated for long-term, once-daily maintenance bronchodilator treatment of airflow obstruction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema.
1.2 Important Limitations of Use
ARCAPTA NEOHALER is not indicated to treat acute deteriorations of chronic obstructive pulmonary disease [see W arnings and Precautions (5.2)].
ARCAPTA NEOHALER is not indicated to treat asthma. The safety and effectiveness of ARCAPTA NEOHALER in asthma have not been established.
DO NOT SWALLOW ARCAPTA CAPSULES
FOR USE WITH NEOHALER DEVICE ONLY
FOR ORAL INHALATION ONLY
ARCAPTA capsules must not be swallowed as the intended effects on the lungs will not be obtained. The contents of ARCAPTA capsules are only for oral inhalation and should only be used with the NEOHALER device.
The recommended dosage of ARCAPTA NEOHALER is the once-daily inhalation of the contents of one 75 mcg ARCAPTA capsule using the NEOHALER inhaler.
ARCAPTA NEOHALER should be administered once daily every day at the same time of the day by the orally inhaled route only. If a dose is missed, the next dose should be taken as soon as it is remembered. Do not use ARCAPTA NEOHALER more than one time every 24 hours.
ARCAPTA capsules must always be stored in the blister, and only removed IMMEDIATELY BEFORE USE.
No dosage adjustment is required for geriatric patients, patients with mild and moderate hepatic impairment, or renally impaired patients. No data are available for subjects with severe hepatic impairment [see Clinical Pharmacology (12.3)].
Inhalation powder:
75 mcg: hard gelatin capsule with black product code “IDL 75” above a bar printed on one side of the capsule and the logo “ ” printed on the other side.
” printed on the other side.
All LABA are contraindicated in patients with asthma without use of a long-term asthma control medication. [see W arnings and P recautions (5.1)]. ARCAPTA NEOHALER is not indicated for the treatment of asthma.
ARCAPTA NEOHALER is contraindicated in patients with a history of hypersensitivity to indacaterol or to any of the ingredients. [see Warnings and Precautions (5.4)].
5.1 Asthma-Related Death
-
Data from a large placebo-controlled study in asthma patients showed that long-acting beta
2
-adrenergic agonists may increase the risk of asthma-related death. Data are not available to determine whether the rate of death in patients with COPD is increased by long-acting beta
2
-adrenergic agonists.
-
A 28-week, placebo-controlled US study comparing the safety of another long-acting beta
2
-adrenergic agonist (
salmeterol
) with placebo, each added to usual asthma therapy, showed an increase in asthma-related deaths in patients receiving salmeterol (13/13,176 in patients treated with salmeterol vs. 3/13,179 in patients treated with placebo; RR 4.37, 95% CI 1.25, 15.34). The increased risk of asthma-related death is considered a class effect of the long-acting beta
2
-adrenergic agonists, including
ARCAPTA NEOHALER
. No study adequate to determine whether the rate of asthma-related death is increased in patients treated with
ARCAPTA NEOHALER
has been conducted. The safety and efficacy of
ARCAPTA NEOHALER
in patients with asthma have not been established.
ARCAPTA NEOHALER
is not indicated for the treatment of asthma. [
see Contraindications (4
)].
- Serious asthma-related events, including death, were reported in clinical studies with ARCAPTA NEOHALER. The sizes of these studies were not adequate to precisely quantify the differences in serious asthma exacerbation rates between treatment groups . [see Adverse Reactions ( 6.2 )] .
5.2 Deterioration of Disease and Acute Episodes
ARCAPTA NEOHALER should not be initiated in patients with acutely deteriorating COPD, which may be a life-threatening condition. ARCAPTA NEOHALER has not been studied in patients with acutely deteriorating COPD. The use of ARCAPTA NEOHALER in this setting is inappropriate.
ARCAPTA NEOHALER should not be used for the relief of acute symptoms, i.e. as rescue therapy for the treatment of acute episodes of bronchospasm. ARCAPTA NEOHALER has not been studied in the relief of acute symptoms and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled short-acting beta2-agonist.
When beginning ARCAPTA NEOHALER, patients who have been taking inhaled, short-acting beta2-agonists on a regular basis (e.g., four times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms. When prescribing ARCAPTA NEOHALER, the healthcare provider should also prescribe an inhaled, short-acting beta2- agonist and instruct the patient on how it should be used. Increasing inhaled beta2-agonist use is a signal of deteriorating disease for which prompt medical attention is indicated.
COPD may deteriorate acutely over a period of hours or chronically over several days or longer. If ARCAPTA NEOHALER no longer controls the symptoms of bronchoconstriction, or the patient’s inhaled, short-acting beta2-agonist becomes less effective or the patient needs more inhalation of short-acting beta2-agonist than usual, these may be markers of deterioration of disease. In this setting, a re-evaluation of the patient and the COPD treatment regimen should be undertaken at once. Increasing the daily dosage of ARCAPTA NEOHALER beyond the recommended dose is not appropriate in this situation.
5.3 Excessive Use of ARCAPTA NEOHALER and Use with Other Long-Acting Beta-Agonists
As with other inhaled beta2-adrenergic drugs, ARCAPTA NEOHALER should not be used more often, at higher doses than recommended, or in conjunction with other medications containing long-acting beta2-agonists, as an overdose may result. Clinically significant cardiovascular effects and fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs.
5.4 Immediate Hypersensitivity Reactions
Immediate hypersensitivity reactions may occur after administration of ARCAPTA NEOHALER. If signs suggesting allergic reactions (in particular, difficulties in breathing or swallowing, swelling of tongue, lips and face, urticaria, skin rash) occur, ARCAPTA NEOHALER should be discontinued immediately and alternative therapy instituted.
5.5 Paradoxical Bronchospasm
As with other inhaled beta2-agonists, ARCAPTA NEOHALER may produce paradoxical bronchospasm that may be life-threatening. If paradoxical bronchospasm occurs, ARCAPTA NEOHALER should be discontinued immediately and alternative therapy instituted.
5.6 Cardiovascular Effects
ARCAPTA NEOHALER, like other beta2-agonists, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic or diastolic blood pressure, or symptoms. If such effects occur, ARCAPTA NEOHALER may need to be discontinued. In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression, although the clinical significance of these findings is unknown. Therefore, ARCAPTA NEOHALER, like other sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
5.7 Coexisting Conditions
ARCAPTA NEOHALER, like other sympathomimetic amines, should be used with caution in patients with convulsive disorders or thyrotoxicosis, and in patients who are unusually responsive to sympathomimetic amines. Doses of the related beta2-agonist albuterol, when administered intravenously, have been reported to aggravate pre-existing diabetes mellitus and ketoacidosis.
5.8 Hypokalemia and Hyperglycemia
Beta2-agonist medications may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects [see Clinical Pharmacology (12.2)]. The decrease in serum potassium is usually transient, not requiring supplementation. Inhalation of high doses of beta2-adrenergic agonists may produce increases in plasma glucose.
Clinically notable decreases in serum potassium or changes in blood glucose were infrequent during clinical studies with long-term administration of ARCAPTA NEOHALER with the rates similar to those for placebo controls. ARCAPTA NEOHALER has not been investigated in patients whose diabetes mellitus is not well controlled.
L ong - acting beta 2 -adrenergic agonists , such as A RCAPTA NEOHALER , increase the risk of asthma-related death . ARCAPTA NEOHALER is not indicated for the treatment of asthma [See B oxed Warning and W arning and Precautions (5.1) ].
6.1 Clinical Trials Experience in Chronic Obstructive Pulmonary Disease
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The ARCAPTA NEOHALER safety database reflects exposure of 2516 patients to ARCAPTA NEOHALER at doses of 75 mcg or greater for at least 12 weeks in six confirmatory randomized, double-blind, placebo and active-controlled clinical trials (see Section 14). In these trials, 449 patients were exposed to the recommended dose of 75 mcg for up to 3 months, and 144, 583 and 425 COPD patients were exposed to a dose of 150, 300 or 600 mcg for one year, respectively. Overall, patients had a mean pre-bronchodilator forced expiratory volume in one second (FEV1) percent predicted of 54%. The mean age of patients was 64 years, with 47% of patients aged 65 years or older, and the majority (88%) was Caucasian.
In these six clinical trials, 48% of patients treated with any dose of ARCAPTA NEOHALER reported an adverse reaction compared with 43% of patients treated with placebo. The proportion of patients who discontinued treatment due to adverse reaction was 5% for ARCAPTA NEOHALER-treated patients and 5% for placebo-treated patients. The most common adverse reactions that lead to discontinuation of ARCAPTA NEOHALER were COPD and dyspnea.
The most common serious adverse reactions were COPD exacerbation, pneumonia, angina pectoris, and atrial fibrillation, which occurred at similar rates across treatment groups.
Table 1 displays adverse drug reactions reported by at least 2% of patients (and higher than placebo) during a 3 month exposure at the recommended 75 mcg once daily dose. Adverse drug reactions are listed according to MedDRA (version 13.0) system organ class and sorted in descending order of frequency.
|
Indacaterol
75 mcg once daily |
Placebo | |
| n=449 | n= 445 | |
| n (%) | n (%) | |
| Respiratory, thoracic and mediastinal disorders | ||
| - Cough | 29 (6.5) | 20 (4.5) |
| - Oropharyngeal pain | 10 (2.2) | 3 (0.7) |
| Infections and infestations | ||
| - Nasopharyngitis | 24 (5.3) | 12 (2.7) |
| Nervous system disorders | ||
| - Headache | 23 (5.1) | 11 (2.5) |
| Gastrointestinal disorders | ||
| - Nausea | 11 (2.4) | 4 (0.9) |
In these trials the overall frequency of all cardiovascular adverse reactions was 2.5% for ARCAPTA NEOHALER 75 mcg and 1.6% for placebo during a 3 month exposure. There were no frequently occurring specific cardiovascular adverse reactions for ARCAPTA NEOHALER 75 mcg (frequency at least 1% and greater than placebo).
Additional adverse drug reactions reported in greater than 2% (and higher than on placebo) in patients dosed with 150, 300 or 600 mcg for up to 12 months were as follows:
- Musculoskeletal and connective tissue disorders: muscle spasm, musculoskeletal pain
- General disorders and administration site conditions: edema peripheral
- Metabolism and nutrition disorder: diabetes mellitus, hyperglycemia
- Infections and infestations: sinusitis, upper respiratory tract infection
C ough experienced p ost - inhalation
In the clinical trials, health care providers observed during clinic visits that an average of 24% of patients experienced a cough on at least 20% of visits following inhalation of the recommended 75 mcg dose of ARCAPTA NEOHALER compared to 7% of patients receiving placebo. The cough usually occurred within 15 seconds following inhalation and lasted for no more than 15 seconds. Cough following inhalation in clinical trials was not associated with bronchospasm, exacerbations, deteriorations of disease or loss of efficacy.
6.2 Clinical Trials Experience in Asthma
In a 6-month randomized, active controlled asthma safety trial, 805 adult patients with moderate to severe persistent asthma were treated with ARCAPTA NEOHALER 300 mcg (n=268), ARCAPTA NEOHALER 600 mcg (n=268), and salmeterol (n=269), all concomitant with inhaled corticosteroids, which were not co-randomized. Of these patients, there were 2 respiratory-related deaths in the ARCAPTA NEOHALER 300 mcg dose group. There were no deaths in the ARCAPTA NEOHALER 600 mcg dose group or in the salmeterol active control group. Serious adverse reactions related to asthma exacerbation were reported for 2 patients in the indacaterol 300 mcg group, 3 patients in the indacaterol 600 mcg group, and no patients in the salmeterol active control group.
In addition, a two-week dose-ranging trial was conducted in 511 adult patients with mild persistent asthma taking inhaled corticosteroids. No deaths, intubations, or serious adverse reactions related to asthma exacerbation were reported in this trial.
6.3 Postmarketing Experience
The following adverse reactions have been identified during worldwide post-approval use of indacaterol, the active ingredient in ARCAPTA NEOHALER. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These adverse reactions are: hypersensitivity reactions, paradoxical bronchospasm, tachycardia/heart rate increase/palpitations, pruritus/rash and dizziness.
7.1 Adrenergic Drugs
If additional adrenergic drugs are to be administered by any route, they should be used with caution because the sympathetic effects of ARCAPTA NEOHALER may be potentiated [see W arnings and Precautions (5.3, 5.6, 5.7, 5.8)].
7.2 Xanthine Derivatives, Steroids, or Diuretics
Concomitant treatment with xanthine derivatives, steroids, or diuretics may potentiate any hypokalemic effect of ARCAPTA NEOHALER [see W arnings and Precautions (5.8)].
7.3 Non-Potassium Sparing Diuretics
The ECG changes or hypokalemia that may result from the administration of non-potassium sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical relevance of these effects is not known, caution is advised in the co-administration of ARCAPTA NEOHALER with non-potassium-sparing diuretics.
7.4 Monoamine Oxidase Inhibitors, Tricyclic Antidepressants, QTc Prolonging Drugs
Indacaterol, as with other beta2-agonists, should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors, tricyclic antidepressants, or other drugs known to prolong the QTc interval because the action of adrenergic agonists on the cardiovascular system may be potentiated by these agents. Drugs that are known to prolong the QTc interval may have an increased risk of ventricular arrhythmias.
7.5 Beta-Blockers
Beta-adrenergic receptor antagonists (beta-blockers) and ARCAPTA NEOHALER may interfere with the effect of each other when administered concurrently. Beta-blockers not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers. However, under certain circumstances, e.g. as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
7.6 Inhibitors of Cytochrome P450 3A4 and P-gp Efflux Transporter
Drug interaction studies were carried out using potent and specific inhibitors of CYP3A4 and P-gp (i.e., ketoconazole, erythromycin, verapamil and ritonavir). The data suggest that systemic clearance is influenced by modulation of both P-gp and CYP3A4 activities and that the 1.9-fold AUC0-24 increase caused by the strong dual inhibitor ketoconazole reflects the impact of maximal combined inhibition. ARCAPTA NEOHALER was evaluated in clinical trials for up to one year at doses up to 600 mcg. No dose adjustment is warranted at the 75 mcg dose. [See Drug-drug Interaction (12.3)]
8.1 Pregnancy
Teratogenic Effects: Pregnancy Category C.
There are no adequate and well-controlled studies with ARCAPTA NEOHALER in pregnant women. ARCAPTA NEOHALER should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Indacaterol was not teratogenic following subcutaneous administration to rats and rabbits at doses up to 1 mg/kg, approximately 130 and 260 times, respectively, the 75 mcg dose on a mg/m2 basis.
8.2 Labor and Delivery
There are no adequate and well-controlled human studies that have investigated effects of ARCAPTA NEOHALER on preterm labor or labor at term. Because of the potential for beta-agonist interference with uterine contractility, use of ARCAPTA NEOHALER during labor should be restricted to those patients in whom the benefits clearly outweigh the risks.
8.3 Nursing Mothers
It is not known that the active component of ARCAPTA NEOHALER, indacaterol, is excreted in human milk. Because many drugs are excreted in human milk and because indacaterol has been detected in the milk of lactating rats, caution should be exercised when ARCAPTA NEOHALER is administered to nursing women.
8.4 Pediatric Use
ARCAPTA NEOHALER is not indicated for use in children. The safety and effectiveness of ARCAPTA NEOHALER in pediatric patients have not been established.
8.5 Geriatric Use
Based on available data, no adjustment of ARCAPTA NEOHALER dosage in geriatric patients is warranted. Of the total number of patients who received ARCAPTA NEOHALER at the recommended dose of 75 mcg once daily in the clinical studies from the pooled 3-month database, 239 were <65 years, 153 were 65–74 years and 57 were ≥75 years of age.
No overall differences in effectiveness were observed, and in the 3-month pooled data, the adverse drug reaction profile was similar in the older population compared to the patient population overall. When treated at higher doses (300 mcg and 600 mcg) over the course of a year, the adverse drug reaction profiles for patients >65 years was similar to that of the general patient population.
8.6 Hepatic Impairment
Patients with mild and moderate hepatic impairment showed no relevant changes in Cmax or AUC, nor did protein binding differ between mild and moderate hepatically impaired subjects and their healthy controls. Studies in subjects with severe hepatic impairment were not performed.
8.7 Renal Impairment
Due to the very low contribution of the urinary pathway to total body elimination, a study in renally impaired subjects was not performed.
10.1 Human Experience
In COPD patients single doses of 40 times the 75 mcg dose were associated with moderate increases in pulse rate, systolic blood pressure and QTc interval.
The expected signs and symptoms associated with overdosage of ARCAPTA NEOHALER are those of excessive beta-adrenergic stimulation and occurrence or exaggeration of any of the signs and symptoms, e.g., angina, hypertension or hypotension, tachycardia, with rates up to 200 bpm, arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, muscle cramps, nausea, dizziness, fatigue, malaise, hypokalemia, hyperglycemia, metabolic acidosis and insomnia. As with all inhaled sympathomimetic medications, cardiac arrest and even death may be associated with an overdose of ARCAPTA NEOHALER.
Treatment of overdosage consists of discontinuation of ARCAPTA NEOHALER together with institution of appropriate symptomatic and supportive therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of ARCAPTA NEOHALER. Cardiac monitoring is recommended in cases of overdosage.
ARCAPTA NEOHALER consists of a dry powder formulation of indacaterol maleate for oral inhalation only with the NEOHALER inhaler. The inhalation powder is packaged in clear gelatin capsules.
Each clear, hard gelatin capsule contains a dry powder blend of 75 mcg of indacaterol (equivalent to 97 mcg of indacaterol maleate) with approximately 25 mg of lactose monohydrate (which contains trace levels of milk protein) as the carrier.
The active component of ARCAPTA NEOHALER is indacaterol maleate, a (R) enantiomer. Indacaterol maleate is a selective beta2-adrenergic agonist. Its chemical name is (R)-5-[2-(5,6-Diethylindan-2-ylamino)-1-hydroxyethyl]-8-hydroxy-1H-quinolin-2-one maleate; its structural formula is
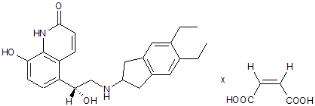
Indacaterol maleate has a molecular weight of 508.56, and its empirical formula is C24H28N2O3 • C4H4O4. Indacaterol maleate is a white to very slightly grayish or very slightly yellowish powder. Indacaterol maleate is freely soluble in N-methylpyrrolidone and dimethylformamide, slightly soluble in methanol, ethanol, propylene glycol and polyethylene glycol 400, very slightly soluble in water, isopropyl alcohol and practically insoluble in 0.9% sodium chloride in water, ethyl acetate and n-octanol.
The NEOHALER inhaler is a plastic device used for inhaling ARCAPTA. The amount of drug delivered to the lung will depend on patient factors, such as inspiratory flow rate and inspiratory time. Under standardized in vitro testing at a fixed flow rate of 60 L/min for 2 seconds, the NEOHALER inhaler delivered 57 mcg for the 75 mcg dose strength (equivalent to 73.9 mcg of indacaterol maleate) from the mouthpiece. Peak inspiratory flow rates (PIFR) achievable through the NEOHALER inhaler were evaluated in 26 adult patients with COPD of varying severity. Mean PIFR was 95 L/min (range 52-133 L/min) for adult patients. Approximately ninety-five percent of the population studied generated a PIFR through the device exceeding 60 L/min.
12.1 Mechanism of Action
Indacaterol is a long-acting beta2-adrenergic agonist.
When inhaled, indacaterol acts locally in the lung as a bronchodilator. Although beta2-receptors are the predominant adrenergic receptors in bronchial smooth muscle and beta1-receptors are the predominant receptors in the heart, there are also beta2-adrenergic receptors in the human heart comprising 10%-50% of the total adrenergic receptors. The precise function of these receptors is not known, but their presence raises the possibility that even highly selective beta2-adrenergic agonists may have cardiac effects.
The pharmacological effects of beta2-adrenoceptor agonist drugs, including indacaterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3’, 5’-adenosine monophosphate (cyclic monophosphate). Increased cyclic AMP levels cause relaxation of bronchial smooth muscle. In vitro studies have shown that indacaterol has more than 24-fold greater agonist activity at beta2-receptors compared to beta1-receptors and 20-fold greater agonist activity compared to beta3-receptors. This selectivity profile is similar to formoterol. The clinical significance of these findings is unknown.
12.2 Pharmacodynamics
Systemic Safety
The major adverse effects of inhaled beta2-adrenergic agonists occur as a result of excessive activation of systemic beta-adrenergic receptors. The most common adverse effects in adults include skeletal muscle tremor and cramps, insomnia, tachycardia, decreases in serum potassium and increases in plasma glucose.
Changes in serum potassium and plasma glucose were evaluated in COPD patients in double-blind Phase III studies. In pooled data, at the recommended 75 mcg dose, at 1 hour post-dose at week 12, there was no change compared to placebo in serum potassium, and change in mean plasma glucose was 0.07 mmol/L.
E lectrophysiology
The effect of ARCAPTA NEOHALER on the QT interval was evaluated in a double-blind, placebo- and active (moxifloxacin)-controlled study following multiple doses of indacaterol 150 mcg, 300 mcg or 600 mcg once-daily for 2 weeks in 404 healthy volunteers. Fridericia’s method for heart rate correction was employed to derive the corrected QT interval (QTcF). Maximum mean prolongation of QTcF intervals were <5 ms, and the upper limit of the 90% confidence interval was below 10 ms for all time-matched comparisons versus placebo. During these studies, there were no clinically meaningful QT-interval prolongations. There was no evidence of a clinically relevant concentration-delta QTc relationship in the range of doses evaluated.
The effect of 150 mcg and 300 mcg once daily of ARCAPTA NEOHALER on heart rate and rhythm was assessed using continuous 24-hour ECG recording (Holter monitoring) in a subset of 605 patients with COPD from a 26-week, double-blind, placebo-controlled Phase III study. Holter monitoring occurred once at baseline and up to 3 times during the 26-week treatment period (at weeks 2, 12 and 26). A comparison of the mean heart rate over 24 hours showed no increase from baseline. The hourly heart rate analysis was similar compared to placebo. The pattern of diurnal variation over 24 hours was maintained and was similar to placebo. No difference from placebo was seen in the rates of atrial fibrillation, time spent in atrial fibrillation and also the maximum ventricular rate of atrial fibrillation. No clear patterns in the rates of single ectopic beats, couplets or runs were seen across visits. Because the summary data on rates of ventricular ectopic beats can be difficult to interpret, specific pro-arrhythmic criteria were analyzed. In this analysis, baseline occurrence of ventricular ectopic beats was compared to change from baseline, setting certain parameters for the change to describe the pro-arrhythmic response. The number of patients with a documented pro-arrhythmic response was very similar compared to placebo. Overall, there was no clinically relevant difference in the development of arrhythmic events in patients receiving indacaterol treatment over those patients who received placebo.
Tachyphylaxis/Tolerance
Tolerance to the effects of inhaled beta-agonists can occur with regularly-scheduled, chronic use. In two 12-week clinical efficacy trials in 323 and 318 adult patients with COPD, ARCAPTA NEOHALER improvement in lung function (as measured by the forced expiratory volume in one second, FEV1) observed at Week 4 with ARCAPTA NEOHALER was consistently maintained over the 12-week treatment period in both trials.
12.3 Pharmacokinetics
Absorption
The median time to reach peak serum concentrations of indacaterol was approximately 15 minutes after single or repeated inhaled doses. Systemic exposure to indacaterol increased with increasing dose (150 mcg to 600 mcg) in a dose proportional manner, and was about dose-proportional in the dose range of 75 mcg to 150 mcg. Absolute bioavailability of indacaterol after an inhaled dose was on average 43-45%. Systemic exposure results from a composite of pulmonary and intestinal absorption.
Indacaterol serum concentrations increased with repeated once-daily administration. Steady-state was achieved within 12 to 15 days. The mean accumulation ratio of indacaterol, i.e. AUC over the 24-hour dosing interval on day 14 or day 15 compared to day 1, was in the range of 2.9 to 3.8 for once-daily inhaled doses between 75 mcg and 600 mcg.
Distribution
After intravenous infusion the volume of distribution (Vz) of indacaterol was 2,361 L to 2,557 L indicating an extensive distribution. The in vitro human serum and plasma protein binding was 94.1-95.3% and 95.1-96.2%, respectively.
Metabolism
After oral administration of radiolabeled indacaterol in the human ADME (absorption, distribution, metabolism, excretion) study unchanged indacaterol was the main component in serum, accounting for about one third of total drug-related AUC over 24 hours. A hydroxylated derivative was the most prominent metabolite in serum. Phenolic O-glucuronides of indacaterol and hydroxylated indacaterol were further prominent metabolites. A diastereomer of the hydroxylated derivative, a N-glucuronide of indacaterol, and C- and N-dealkylated products were further metabolites identified.
In vitro investigations indicated that UGT1A1 was the only UGT isoform that metabolized indacaterol to the phenolic O-glucuronide. The oxidative metabolites were found in incubations with recombinant CYP1A1, CYP2D6, and CYP3A4. CYP3A4 is concluded to be the predominant isoenzyme responsible for hydroxylation of indacaterol.
In vitro investigations indicated that indacaterol is a low affinity substrate for the efflux pump P-gp.
In vitro investigations indicated that indacaterol has negligible potential to cause metabolic interactions with medications (by inhibition or induction of cytochrome P450 enzymes, or induction of UGT1A1) at the systemic exposure levels achieved in clinical practice. In vitro investigation furthermore indicated that, in vivo, indacaterol is unlikely to significantly inhibit transporter proteins such as P-gp, MRP2, BCRP, the cationic substrate transporters hOCT1 and hOCT2, and the human multidrug and toxin extrusion transporters hMATE1 and hMATE2K, and that indacaterol has negligible potential to induce P-gp or MRP2.
Elimination
In clinical studies which included urine collection the amount of indacaterol excreted unchanged via urine was generally lower than 2% of the dose. Renal clearance of indacaterol was, on average, between 0.46 and 1.2 L/h. When compared with the serum clearance of indacaterol of 18.8 L/h to 23.3 L/h, it is evident that renal clearance plays a minor role (about 2 to 6% of systemic clearance) in the elimination of systemically available indacaterol.
In a human ADME study where indacaterol was given orally, the fecal route of excretion was dominant over the urinary route. Indacaterol was excreted into human feces primarily as unchanged parent drug (54% of the dose) and, to a lesser extent, hydroxylated indacaterol metabolites (23% of the dose). Mass balance was complete with ≥90% of the dose recovered in the excreta.
Indacaterol serum concentrations declined in a multi-phasic manner with an average terminal half-life ranging from 45.5 to 126 hours. The effective half-life, calculated from the accumulation of indacaterol after repeated dosing with once daily doses between 75 mcg and 600 mcg ranged from 40 to 56 hours which is consistent with the observed time-to-steady state of approximately 12-15 days.
Special Population s
A population pharmacokinetic analysis was performed for indacaterol utilizing data from 3 controlled clinical trials that included 1,844 patients with COPD aged 40 to 88 years who received treatment with ARCAPTA NEOHALER.
The population analysis showed that no dose adjustment is warranted based on the effect of age, gender and weight on systemic exposure in COPD patients after inhalation of ARCAPTA NEOHALER. The population pharmacokinetic analysis did not suggest any difference between ethnic subgroups in this population.
Hepatic Impairment
Patients with mild and moderate hepatic impairment showed no relevant changes in Cmax or AUC of indacaterol, nor did protein binding differ between mild and moderate hepatically impaired subjects and their healthy controls. Studies in subjects with severe hepatic impairment were not performed.
Renal Impairment
Due to the very low contribution of the urinary pathway to total body elimination, a study in renally impaired subjects was not performed.
Drug-drug Interaction
Drug interaction studies were carried out using potent and specific inhibitors of CYP3A4 and P-gp (i.e., ketoconazole, erythromycin, verapamil and ritonavir).
Verapamil: Co-administration of indacaterol 300 mcg (single dose) with verapamil (80 mg t.i.d for 4 days) showed 2-fold increase in indacaterol AUC0-24, and 1.5-fold increase in indacaterol Cmax.
Erythromycin: Co-administration of indacaterol inhalation powder 300 mcg (single dose) with erythromycin (400 mg q.i.d for 7 days) showed a 1.4-fold increase in indacaterol AUC0-24, and 1.2-fold increase in indacaterol Cmax
Ketoconazole: Co-administration of indacaterol inhalation powder 300 mcg (single dose) with ketoconazole (200 mg b.i.d for 7 days) caused a 1.9-fold increase in indacaterol AUC0-24, and 1.3-fold increase in indacaterol Cmax
Ritonavir: Co-administration of indacaterol 300 mcg (single dose) with ritonavir (300 mg b.i.d for 7.5 days) resulted in a 1.7-fold increase in indacaterol AUC0-24 whereas indacaterol Cmax was unaffected. [See Drug Interactions (7.6)].
12.4 Pharmacogenomics
The pharmacokinetics of indacaterol were prospectively investigated in subjects with the UGT1A1 (TA)7/(TA)7 genotype (low UGT1A1 expression; also referred to as *28) and the (TA)6, (TA)6 genotype. Steady-state AUC and Cmax of indacaterol were 1.2-fold higher in the [(TA)7, (TA)7] genotype, suggesting no relevant effect of UGT1A1 genotype of indacaterol exposure.
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies were conducted in transgenic mice using oral administration and in rats using inhalation administration to evaluate the carcinogenic potential of indacaterol maleate. Indacaterol did not show a statistically significant increase in tumor formation in mice or rats.
Lifetime treatment of rats resulted in increased incidences of benign ovarian leiomyoma and focal hyperplasia of ovarian smooth muscle in females at doses approximately 270-times the dose of 75 mcg once-daily for humans (on a mg/m2 basis).
A 26-week oral (gavage) study in CB6F1/TgrasH2 hemizygous mice with indacaterol did not show any evidence of tumorigenicity at doses approximately 39,000-times the dose of 75 mcg once-daily for humans (on a mg/m2 basis).
Increases in leiomyomas of the female rat genital tract have been similarly demonstrated with other beta2-adrenergic agonist drugs. The relevance of these findings to human use is unknown.
Indacaterol was not mutagenic or clastogenic in Ames test, chromosome aberration test in V79 Chinese hamster cells, and bone marrow micronucleus test in rats.
Indacaterol did not impair fertility of rats in reproduction studies.
The ARCAPTA NEOHALER COPD clinical development program included three dose-ranging trials and six confirmatory trials (Trial 3, a 26-week seamless adaptive design trial that included an initial 2 week dose ranging phase; Trials 4, 5, and 6, 12-week trials; Trial 7, a 26-week trial; and Trial 8, a 52 week trial).
Dose-ranging trials:
Dose selection for ARCAPTA NEOHALER for COPD was based on three dose-ranging trials (Trial 1, a 2-week dose- ranging trial in an asthma population; Trial 2, a 2-week dose-ranging trial in a COPD population; and Trial 3, a 26-week adaptive seamless design trial that included an initial 2-week dose ranging phase). Although ARCAPTA NEOHALER is not indicated for asthma, dose selection was primarily based upon the results from the dose-ranging trial in asthma patients (Trial 1) as an asthma population is the most responsive to beta-agonist bronchodilation and is most likely to demonstrate a dose response. Dose-ranging in COPD patients (Trials 2 and 3) provided supportive information.
Dose - ranging in asthma
ARCAPTA NEOHALER is not indicated for asthma.
Trial 1 was a 2-week, randomized, double-blinded, placebo-controlled design that enrolled 511 patients with persistent asthma 18 years of age and older. All enrolled patients were required to be taking inhaled corticosteroids, had a forced expiratory volume in one second (FEV1) of ≥ 50% and ≤ 90% predicted, and FEV1 reversibility after albuterol of at least 12% and at least 200 mL. Trial 1 included ARCAPTA NEOHALER doses of 18.75, 37.5, 75, and 150 mcg once daily, a salmeterol active control group, and placebo. The trial showed that the effect on FEV1 in patients treated with ARCAPTA NEOHALER 18.75 and 37.5 mcg doses was lower compared to patients treated with other ARCAPTA NEOHALER doses, particularly after the first dose. The effect did not clearly differ between the 75 and 150 mcg doses.
Results of the ARCAPTA NEOHALER and placebo treatment arms are as follows. After the first dose (Day 1), the peak (4 hour) FEV1 was 2.58L in the placebo group, with a treatment difference of 0.04L (95% CI -0.01, 0.09) in the 18.75 mcg ARCAPTA NEOHALER group, 0.04L (-0.01, 0.09) in the 37.5 mcg group, 0.12L (0.07, 0.17) in the 75 mcg group, and 0.15L (0.10, 0.20) in the 150 mcg group. The Day 2 trough FEV1 was 2.45L in the placebo group, with a treatment difference of 0.02L (95% CI -0.05, 0.08), 0.08L (0.01, 0.15), 0.09L (0.03, 0.16) and 0.16L (0.09, 0.22) in the ARCAPTA NEOHALER groups, respectively. At Day 14, the peak (4 hour) FEV1 was 2.55L in the placebo group, with a treatment difference of 0.12L (95% CI 0.05, 0.20) in the 18.75 mcg ARCAPTA NEOHALER group, 0.14L (0.06, 0.21) in the 37.5 mcg group, 0.23L (0.15, 0.30) in the 75 mcg group, and 0.20L (0.13, 0.27) in the 150 mcg group. The Day 15 FEV1 (primary endpoint) was 2.42L in the placebo group, with a treatment difference of 0.09L (95% CI 0.00, 0.17), 0.11L (0.02, 0.19), 0.17L (0.08, 0.26), and 0.12L (0.04, 0.21) in the ARCAPTA NEOHALER groups, respectively.
Dose - ranging in COPD
Trial 2 was a 2-week, randomized, double-blinded, placebo-controlled design that enrolled 552 patients with a clinical diagnosis of COPD, who were 40 years or older, had a smoking history of at least 10 pack years, had a post-bronchodilator FEV1 less than 80% and at least 30% of the predicated normal value and a post-bronchodilator ratio of FEV1 over forced vital capacity (FEV1/FVC) of less than 70%. Trial 2 included ARCAPTA NEOHALER doses of 18.75, 37.5, 75 and 150 mcg once daily, a salmeterol active control group, and placebo. Results of the ARCAPTA NEOHALER and placebo arms are shown in Figure 1. The trial showed that the effect on FEV1 in patients treated with ARCAPTA NEOHALER 18.75 mcg dose was lower compared to patients treated with other ARCAPTA NEOHALER doses. Although a dose-response relationship was observed at Day 1, the effect did not clearly differ among the 37.5, 75 and 150 mcg doses by Day 15.

In both COPD clinical trials including the 75 mcg dose (Trials 4 and 5), patients treated with ARCAPTA NEOHALER used less daily rescue albuterol during the trial compared to patients treated with placebo.
Health-related quality of life was measured using the St. George’s Respiratory Questionnaire (SGRQ) in all six confirmatory COPD clinical trials. SGRQ is a disease-specific patient reported instrument which measures symptoms, activities, and its impact on daily life. At week 12, pooled data from these trials demonstrated an improvement over placebo in SGRQ total score of -3.8 with a 95% CI of (-5.3, -2.3) for the ARCAPTA NEOHALER 75 mcg dose, -4.6 with a 95% CI of (-5.5, -3.6) for 150 mcg, and -3.8 with a 95% CI of (-4.9, -2.8) for 300 mcg. The confidence intervals for this change are widely overlapping with no dose ordering. Results from individual studies were variable, but are generally consistent with the pooled data results.
16.1 How Supplied
75 mcg ARCAPTA NEOHALER contains ARCAPTA (indacaterol inhalation powder) capsules packaged in aluminum blister cards, one NEOHALER inhaler, and an FDA approved Medication Guide.
Unit Dose (blister pack), Box of 30 (5 blister cards with 6 capsules each) NDC 0078-0619-15
The NEOHALER inhaler consists of a white protective cap and a base with mouthpiece, capsule chamber and two translucent red push buttons.
16.2 Storage and Handling
Store in a dry place at 25°C (77°F); excursions permitted to 15-30°C (59-86° F) [see USP Controlled Room Temperature].
75 mcg: Protect capsule from light and moisture.
- ARCAPTA capsules should be used with the NEOHALER inhaler only. The NEOHALER inhaler should not be used with any other capsules.
- Capsules should always be stored in the blister and only removed from the blister immediately before use.
- Always use the new NEOHALER inhaler provided with each new prescription.
Keep out of the reach of children.
See FDA-approved patient labeling (Medication Guide)
17.1 Asthma-Related Death
Patients should be informed that LABA, such as ARCAPTA NEOHALER, increase the risk of asthma-related death. ARCAPTA NEOHALER is not indicated for the treatment of asthma.
17.2 Instructions for Administering ARCAPTA NEOHALER
It is important for patients to understand how to correctly administer ARCAPTA capsules using the NEOHALER device [see Instructions for Use at the end of the Medication Guide]. Patients should be instructed that ARCAPTA capsules should only be administered via the NEOHALER device and the NEOHALER device should not be used for administering other medications. The contents of ARCAPTA capsules are for oral inhalation only and must not be swallowed.
ARCAPTA capsules should always be stored in sealed blisters. Only one ARCAPTA capsule should be removed immediately before use, or its effectiveness may be reduced. Additional ARCAPTA capsules that are exposed to air (i.e. not intended for immediate use) should be discarded.
17.3 Not for Acute Symptoms
ARCAPTA NEOHALER is not meant to relieve acute symptoms or exacerbations of COPD and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, short-acting beta2-agonist such as albuterol. (The healthcare provider should provide the patient with such medication and instruct the patient in how it should be used.)
Patients should be instructed to notify their physician immediately if they experience any of the following:
- Worsening of symptoms
- Decreasing effectiveness of inhaled, short-acting beta2-agonists
- Need for more inhalations than usual of inhaled, short-acting beta2-agonists
- Significant decrease in lung function as outlined by the physician.
Patients should not stop therapy with ARCAPTA NEOHALER without physician/provider guidance since symptoms may recur after discontinuation.
17.4 Do Not Use Additional Long-Acting Beta-Agonists
Patients who have been taking inhaled, short-acting beta2-agonists on a regular basis should be instructed to discontinue the regular use of these products and use them only for the symptomatic relief of acute symptoms.
When patients are prescribed ARCAPTA NEOHALER, other inhaled medications containing long-acting beta2-agonists should not be used. Patients should not use more than the recommended once daily dose of ARCAPTA NEOHALER. Excessive use of sympathomimetics may cause significant cardiovascular effects, and may be fatal.
17.5 Risks Associated With Beta-Agonist Therapy
Patients should be informed of adverse effects associated with beta2-agonists, such as palpitations, chest pain, rapid heart rate, tremor, or nervousness.
T2012-174
September 2012
Medication Guide
A RCAPTA TM (ar- CAP -ta) N EOHALER TM
(indacaterol inhalation powder)
| Important: Do not swallow ARCAPTA capsules. ARCAPTA c apsules are used only with the NEOHALER i nhaler that comes with ARCAPTA NEOHALER . Never place a capsule in the mouthpiece of the NEOHALER inhaler. |
Read the Medication Guide that comes with ARCAPTA NEOHALER before you start using it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your health care provider about your medical condition or treatment.
What is the most important information I should know about ARCAPTA NEOHALER ?
ARCAPTA NEOHALER has been approved for COPD only. Therefore, ARCAPTA NEOHALER is NOT to be used in asthma.
ARCAPTA NEOHALER can cause serious side effects, including:
-
People with asthma who take long-acting beta
2
adrenergic
-agonist (LABA) medicines
, such as ARCAPTA NEOHALER,
have an increased risk of death from asthma problems.
-
It is not known if LABA med
i
cines, such as
ARCAPTA NEOHALER
, increase the risk of death in people with chronic obstructive pulmonary disease (COPD).
- Get emergency medical care if:
- breathing problems worsen quickly
- you use your rescue inhaler medicine, but it does not relieve your breathing problems.
- breathing problems worsen quickly
What is ARCAPTA NEOHALER ?
ARCAPTA NEOHALER is used long term, 1 time each day, in controlling symptoms of chronic obstructive pulmonary disease (COPD) in adults with COPD.
LABA medicines such as ARCAPTA NEOHALER help the muscles around the airways in your lungs stay relaxed to prevent symptoms, such as wheezing, cough, chest tightness and shortness of breath.
ARCAPTA NEOHALER is not for use to treat sudden symptoms of COPD. Always have a short-acting beta2-agonist medicine with you to treat sudden symptoms. If you do not have an inhaled, short-acting bronchodilator, contact your healthcare provider to have one prescribed for you.
It is not known if ARCAPTA NEOHALER is safe and effective in people with asthma.
ARCAPTA NEOHALER should not be used in children. It is not known if ARCAPTA NEOHALER is safe and effective in children.
Who should not use ARCAPTA NEOHALER ?
Do not use ARCAPTA NEOHALER if you:
- have asthma.
- have had an allergic reaction to indacaterol or any of the ingredients in ARCAPTA NEOHALER. Ask your healthcare provider if you are not sure. See the end of the Medication Guide for a list of ingredients in ARCAPTA NEOHALER.
What should I tell my healthcare provider before using ARCAPTA NEOHALER ?
Tell your healthcare provider about all of your health conditions, including if you:
- have heart problems
- have high blood pressure
- have seizures
- have thyroid problems
- have diabetes
- are pregnant or planning to become pregnant. It is not known if ARCAPTA NEOHALER can harm your unborn baby.
- are breastfeeding. It is not known if ARCAPTA NEOHALER passes into your milk and if it can harm your baby.
- are allergic to ARCAPTA NEOHALER or any of its ingredients, any other medicines, or food products.
ARCAPTA NEOHALER contains lactose (milk sugar) and a small amount of milk proteins. It is possible that allergic reactions may happen in patients who have a severe milk protein allergy.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. ARCAPTA NEOHALER and certain other medicines may interact with each other. This may cause serious side effects.
Know the medicines you take. Keep a list of your medicines with you to show your healthcare provider and pharmacist each time you get a new medicine.
How should I use ARCAPTA NEOHALER ?
-
Read
the step-by-step instructions
for
using
ARCAPTA NEOHALER
at the end of th
is
Medication Guide
.
-
Use
ARCAPTA
NEOHALER
1
time
each
day
at the same time of the day.
- If you miss a dose of ARCAPTA NEOHALER, take it as soon as you remember. Do not take more than one dose in 24 hours.
-
Do not swallow
ARCAPTA
capsules. ARCAPTA capsules should always be used with the NEOHALER inhaler only.
- Always use the new NEOHALER inhaler that is provided with each new prescription.
-
ARCAPTA NEOHALER
does not relieve sudden symptoms of COPD. Always have a rescue inhaler medicine with you to treat sudden symptoms. If you do not have a rescue inhaler medicine, call your healthcare provider to have one prescribed for you.
- Do not stop using ARCAPTA NEOHALER or other medicines to control or treat your COPD unless told to do so by your healthcare provider because your symptoms might get worse. Your healthcare provider will change your medicines as needed.
-
Do not use
ARCAPTA NEOHALER:
- more often than prescribed
- more medicine than prescribed for you, or
- with other LABA medicines
- more often than prescribed
-
Call your health care provider or get emergency medical care right away if:
- your breathing problems worsen with ARCAPTA NEOHALER
- you need to use your rescue medicine more often than usual
- your rescue inhaler medicine does not work as well for you at relieving your symptoms
- your breathing problems worsen with ARCAPTA NEOHALER
What are the possible side effects with ARCAPTA NEOHALER ?
ARCAPTA NEOHALER can cause serious side effects, including:
-
See “What is the most important information I should know about
ARCAPTA NEOHALER
?”
- If your COPD symptoms worsen over time do not increase your dose of ARCAPTA NEOHALER, instead call your healthcare provider.
- serious allergic reactions including rash, hives, swelling of the tongue, lips and face, difficulties in breathing or swallowing. Call your healthcare provider or get emergency medical care if you get any symptoms of a serious allergic reaction.
- sudden shortness of breath that may be life-threatening
- fast or irregular heartbeat (palpitations)
- increased blood pressure
- chest pain
- low blood potassium (which may cause symptoms of muscle spasm, muscle weakness or abnormal heart rhythm)
- high blood sugar
Common side effects of ARCAPTA NEOHALER include:
- runny nose
- cough
- sore throat
- headache
- nausea
Tell your healthcare provider about any side effect that bothers you or that does not go away.
These are not all the side effects with ARCAPTA NEOHALER. Ask your healthcare provider or pharmacist for more information.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 .
How should I store ARCAPTA NEOHALER ?
- Store ARCAPTA NEOHALER (inhaler and blister-packaged capsules) in a dry place 59° F to 86° F (15°C to 30°C). Protect ARCAPTA NEOHALER (inhaler and blister-packaged capsules) from moisture.
- Do not remove ARCAPTA capsules from their foil package until just before use.
- Keep ARCAPTA capsules out of the light.
- Do not store ARCAPTA capsules in the NEOHALER inhaler.
- Keep ARCAPTA NEOHALER and all medicines out of the reach of children.
General Information about ARCAPTA NEOHALER
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ARCAPTA NEOHALER for a condition for which it was not prescribed. Do not give ARCAPTA NEOHALER to other people, even if they have the same condition. It may harm them.
This Medication Guide summarizes the most important information about ARCAPTA NEOHALER. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about ARCAPTA NEOHALER that was written for healthcare professionals.
For more information, go to www.arcapta.com or call 1-888-669-6682.
Active ingredient: indacaterol
Inactive ingredients: lactose monohydrate (contains trace levels of milk protein)
T2012-175
Revised September 2012
Instructions for Use
ARCAPTATM (ar-CAP-ta) NEOHALERTM
(indacaterol inhalation powder)
Do not swallow ARCAPTA capsules.
Follow the instructions below for using ARCAPTA NEOHALER. You will breathe-in (inhale) the medicine in the ARCAPTA capsules from the NEOHALER inhaler. If you have any questions, ask your healthcare provider or pharmacist.
ARCAPTA NEOHALER

|
|

|
ARCAPTA NEOHALER consists of both the inhaler and the blister-packaged capsules. Each package contains ARCAPTA capsules and a NEOHALER inhaler.
- ARCAPTA capsules come in blister cards (see figure above).
- NEOHALER inhaler consists of a cap and a base (see figure above).
Your inhaler is made to give you the medicine contained in the capsules.
Do not use ARCAPTA capsules with any other capsule inhaler, and do not use NEOHALER inhaler to take any other capsule medicine.
| How to use your inhaler | |
Figure A

|
Step 1. Pull off cap. See Figure A. |
Figure B

|
Step 2.
Open inhaler:
See Figure B
Hold the base of the inhaler firmly and tilt the mouthpiece to open the inhaler. |
Figure C

|
Step 3.
Prepare capsule:
See Figure C
Separate one of the blisters from the blister card by tearing along the perforation. Take one blister and peel away the protective backing to expose the foil. |
Figure D

|
Step 4.
Remove an
ARCAPTA
capsule:
See Figure D
Capsules should always be stored in the blister and only removed immediately before use. With dry hands, remove one capsule from the blister by pushing the ARCAPTA capsule through the foil. Do not swallow ARCAPTA capsule. |
Figure E

|
Step 5.
Insert capsule:
See Figure E
Place the capsule into the capsule chamber. Do not place a capsule directly into the mouthpiece. |
Figure F

|
Step 6.
Close the inhaler:
See Figure F
Close the inhaler fully. You should hear a ‘click’ as it fully closes. |
Figure G

|
Step 7.
Pierce the capsule:
See Figure G
Hold the inhaler upright. Press both buttons fully one time. You should hear a ‘click’ as the capsule is being pierced. Do not press the piercing buttons more than one time. |
Figure H
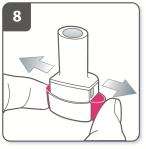
|
Step 8. Release the buttons fully. See Figure H |
Figure I

|
Step 9.
Breathe out:
See Figure I
Before placing the mouthpiece in your mouth, breathe out fully. Never blow into the mouthpiece. |
Figure J

|
Step 10.
Inhale the medicine:
See Figure J
Before breathing in, place the mouthpiece in your mouth and close your lips around the mouthpiece. Hold the inhaler with the buttons to the left and right (not up and down). Breathe in rapidly and steadily, as deeply as you can. Do not press the piercing buttons. |
Figure
K

|
Note:
See Figure K
As you breathe in through the inhaler, the capsule spins around in the chamber and you should hear a whirring noise. If you do not hear a whirring noise, the capsule may be stuck in the capsule cavity. If this occurs, open the inhaler and carefully loosen the capsule by tapping the base of the device. Do not press the piercing buttons to loosen the capsule. (Repeat steps 9 and 10 if needed). |
Figure
L

|
Step 1
1
.
Hold breath:
See Figure L
Continue to hold your breath as long as comfortably possible while removing the inhaler from your mouth. Then breathe out. Open the inhaler to see if any powder is left in the capsule. If there is powder left in the capsule, close the inhaler and repeat steps 9 to 12. Most people are able to empty the capsule in one or two inhalations. Some people may cough soon after inhaling the medicine. If you do, don’t worry, as long as the capsule is empty, you have received the full dose. |
Figure
M

|
Step 12.
Remove capsule:
See Figure M
After you have finished taking your daily dose of the ARCAPTA NEOHALER, open the mouthpiece again, remove the empty capsule by tipping it out, and discard it. Close the inhaler and replace the cap. Do not store the capsules in the NEOHALER device. |
Additional Information
Occasionally, very small pieces of the capsule can get past the screen and enter your mouth. If this happens, you may be able to feel these pieces on your tongue. It is not harmful if these pieces are swallowed or inhaled. The chances of the capsule shattering will be increased if the capsule is pierced more than once (Step 7). Therefore it is recommended that you follow the storage directions, remove the capsule from the blister immediately before use and pierce each capsule only once.
How to clean your inhaler
Cleaning the device is not necessary, however, if desired, a clean, dry lint-free cloth, or a clean, dry soft brush may be used to wipe the inhaler between uses.
Remember:
- ARCAPTA capsules should be stored in the blister, and only removed immediately before use.
- Do not breathe into the NEOHALER inhaler.
- Do not place the ARCAPTA capsule directly into the mouthpiece of the NEOHALER inhaler.
- Do not store the ARCAPTA capsule in the NEOHALER inhaler chamber.
- Always release the push buttons prior to inhalation
- Do not wash the NEOHALER inhaler. Keep it dry.
- Always keep the NEOHALER inhaler and ARCAPTA capsules in a dry place.
- Always use the new NEOHALER inhaler that comes with your refill.
- Do not use ARCAPTA capsules with inhalers from other medicines.
- Keep this and all drugs out of the reach of children.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Novartis Pharma Stein AG
Stein, Switzerland
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
© Novartis
T2012-179
Revised September 2012
PRINCIPAL DISPLAY PANEL
Package Label – 75 mcg
Rx Only NDC 0078-0619-15
Arcapta™
Neohaler™
(indacaterol inhalation powder)
75 mcg per capsule
30 capsules
FOR ORAL INHALATION ONLY
Do not swallow the Arcapta ™ capsules
PHARMACIST: Dispense with Medication Guide enclosed.
Contents:
30 capsules (5 blister cards of 6 capsules)
1 Neohaler™ Inhaler
Prescribing Information and Medication Guide

Arcapta NeohalerIndacaterol maleate CAPSULE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||