BUPRENORPHINE HYDROCHLORIDE
FULL PRESCRIBING INFORMATION: CONTENTS*
- SPL UNCLASSIFIED
- BUPRENORPHINE HYDROCHLORIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- SPECIFIC POPULATIONS
- CLINICAL STUDIES
- INDICATIONS & USAGE
- BUPRENORPHINE HYDROCHLORIDE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- DRUG INTERACTIONS
- INFORMATION FOR PATIENTS
- PREGNANCY
- NURSING MOTHERS
- PEDIATRIC USE
- BUPRENORPHINE HYDROCHLORIDE ADVERSE REACTIONS
- DRUG ABUSE AND DEPENDENCE
- OVERDOSAGE
- DOSAGE & ADMINISTRATION
- HOW SUPPLIED
- PATIENT INFORMATION
- PHYSICIAN INFORMATION
- INFORMATION FOR PHARMACISTS
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
FULL PRESCRIBING INFORMATION
SPL UNCLASSIFIED
BUPRENORPHINE HYDROCHLORIDE DESCRIPTION

CLINICAL PHARMACOLOGY
Comparisons of buprenorphine with full agonists such as methadone and hydromorphone suggest that sublingual buprenorphine produces typical opioid agonist effects, which are limited by a ceiling effect.
In non-dependent subjects, acute sublingual doses of buprenorphine and naloxone sublingual tablets produced opioid agonist effects, which reached a maximum between doses of 8 mg and 16 mg of buprenorphine HCl sublingual tablets. The effects of 16 mg buprenorphine and naloxone sublingual tablets were similar to those produced by 16 mg buprenorphine HCl sublingual tablets (buprenorphine alone).
Opioid agonist ceiling effects were also observed in a double-blind, parallel group, dose ranging comparison of single doses of buprenorphine sublingual solution (1, 2, 4, 8, 16, or 32 mg), placebo, and a full agonist control at various doses. The treatments were given in ascending dose order at intervals of at least one week to 16 opioid-experienced, nondependent subjects. Both drugs produced typical opioid agonist effects. For all the measures for which the drugs produced an effect, buprenorphine produced a dose-related response but, in each case, there was a dose that produced no further effect. In contrast, the highest dose of the full agonist control always produced the greatest effects. Agonist objective rating scores remained elevated for the higher doses of buprenorphine (8 to 32 mg) longer than for the lower doses and did not return to baseline until 48 hours after drug administrations. The onset of effects appeared more rapidly with buprenorphine than with the full agonist control, with most doses nearing peak effect after 100 minutes for buprenorphine compared to 150 minutes for the full agonist control.
Buprenorphine in intravenous (2 mg, 4 mg, 8 mg, 12 mg and 16 mg) and sublingual (12 mg) doses has been administered to non-dependent subjects to examine cardiovascular, respiratory and subjective effects at doses comparable to those used for treatment of opioid dependence. Compared with placebo, there were no statistically significant differences among any of the treatment conditions for blood pressure, heart rate, respiratory rate, O2 saturation or skin temperature across time. Systolic BP was higher in the 8 mg group than placebo (3 hour AUC values). Minimum and maximum effects were similar across all treatments. Subjects remained responsive to low voice and responded to computer prompts. Some subjects showed irritability, but no other changes were observed.
The respiratory effects of sublingual buprenorphine were compared with the effects of methadone in a double-blind, parallel group, dose ranging comparison of single doses of buprenorphine sublingual solution (1, 2, 4, 8, 16, or 32 mg) and oral methadone (15, 30, 45, or 60 mg) in non-dependent, opioid-experienced volunteers. In this study, hypoventilation not requiring medical intervention was reported more frequently after buprenorphine doses of 4 mg and higher than after methadone. Both drugs decreased O2 saturation to the same degree.
Physiologic and subjective effects following acute sublingual administration of buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets were similar at equivalent dose levels of buprenorphine. Naloxone, in the buprenorphine and naloxone sublingual tablets formulation, had no clinically significant effect when administered by the sublingual route, although blood levels of the drug were measurable.
Plasma levels of buprenorphine increased with the sublingual dose of buprenorphine HCl sublingual tablets and buprenorphine and naloxone sublingual tablets, and plasma levels of naloxone increased with the sublingual dose of buprenorphine and naloxone sublingual tablets (Table 1). There was a wide inter-patient variability in the sublingual absorption of buprenorphine and naloxone, but within subjects the variability was low. Both Cmax and AUC of buprenorphine increased in a linear fashion with the increase in dose (in the range of 4 to 16 mg), although the increase was not directly dose-proportional.
Naloxone did not affect the pharmacokinetics of buprenorphine and both buprenorphine HCl sublingual tablets and buprenorphine and naloxone sublingual tablets deliver similar plasma concentrations of buprenorphine. The levels of naloxone were too low to assess dose-proportionality. At the three naloxone doses of 1 mg, 2 mg, and 4 mg, levels above the limit of quantitation (0.05 ng/mL) were not detected beyond 2 hours in seven of eight subjects. In one individual, at the 4 mg dose, the last measurable concentration was at 8 hours. Within each subject (for most of the subjects), across the doses there was a trend toward an increase in naloxone concentrations with increase in dose. Mean peak naloxone levels ranged from 0.11 to 0.28 ng/mL in the dose range of 1-4 mg.
| Pharmacokinetic Parameter |
Buprenorphine
and Naloxone Sublingual Tablets 4 mg |
Buprenorphine and Naloxone Sublingual
Tablets |
Buprenorphine
and Naloxone Sublingual Tablets 16 mg |
Buprenorphine
Hydrochloride |
| Cmax, ng/mL | 1.84 (39) | 3.0 (51) | 5.95 (38) | 5.47 (23) |
|
AUC0-48, hour*ng/mL |
12.52 (35) | 20.22 (43) | 34.89 (33) | 32.63 (25) |
Buprenorphine is approximately 96% protein bound, primarily to alpha and beta globulin.
Naloxone is approximately 45% protein bound, primarily to albumin.
Buprenorphine undergoes both N-dealkylation to norbuprenorphine
and glucuronidation. The
N-dealkylation pathway is mediated by cytochrome
P-450 3A4 isozyme. Norbuprenorphine, an active metabolite, can further undergo
glucuronidation.
Naloxone undergoes direct glucuronidation to naloxone 3-glucuronide as well as N-dealkylation, and reduction of the 6-oxo group.
A mass balance study of buprenorphine showed complete recovery of radiolabel in urine (30%) and feces (69%) collected up to 11 days after dosing. Almost all of the dose was accounted for in terms of buprenorphine, norbuprenorphine, and two unidentified buprenorphine metabolites. In urine, most of buprenorphine and norbuprenorphine was conjugated (buprenorphine, 1% free and 9.4% conjugated; norbuprenorphine, 2.7% free and 11% conjugated). In feces, almost all of the buprenorphine and norbuprenorphine were free (buprenorphine, 33% free and 5% conjugated; norbuprenorphine, 21% free and 2% conjugated).
Buprenorphine has a mean elimination half-life from plasma of 37 h.
SPECIFIC POPULATIONS
The effect of hepatic impairment on the pharmacokinetics of buprenorphine and naloxone is unknown. Since both drugs are extensively metabolized, the plasma levels will be expected to be higher in patients with moderate and severe hepatic impairment. However, it is not known whether both drugs are affected to the same degree. Therefore, in patients with hepatic impairment dosage should be adjusted and patients should be observed for symptoms of precipitated opioid withdrawal.
No differences in buprenorphine pharmacokinetics were observed between 9 dialysis-dependent and 6 normal patients following intravenous administration of 0.3 mg buprenorphine.
A pharmacokinetic interaction study of ketoconazole (400 mg/day), a potent inhibitor of CYP 3A4, in 12 patients stabilized on buprenorphine and naloxone sublingual tablets [8 mg (n=1) or 12 mg (n=5) or 16 mg (n=6)] resulted in increases in buprenorphine mean Cmax values (from 4.3 to 9.8, 6.3 to 14.4 and 9.0 to 17.1) and mean AUC values (from 30.9 to 46.9, 41.9 to 83.2 and 52.3 to 120) respectively. Subjects receiving buprenorphine HCl sublingual tablets or buprenorphine and naloxone sublingual tablets should be closely monitored and may require dose-reduction if inhibitors of CYP 3A4 such as azole antifungal agents (e.g., ketoconazole), macrolide antibiotics (e.g., erythromycin) and HIV protease inhibitors (e.g., ritonavir, indinavir and saquinavir) are co-administered. The interaction of buprenorphine with CYP 3A4 inducers has not been investigated; therefore it is recommended that patients receiving buprenorphine HCl sublingual tablets or buprenorphine and naloxone sublingual tablets should be closely monitored if inducers of CYP 3A4 (e.g., phenobarbital, carbamazepine, phenytoin, rifampicin) are co-administered (see WARNINGS).
CLINICAL STUDIES
Clinical data on the safety and efficacy of buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets are derived from studies of buprenorphine sublingual tablet formulations, with and without naloxone, and from studies of sublingual administration of a more bioavailable ethanolic solution of buprenorphine.
Buprenorphine and naloxone sublingual tablets have been studied in 575 patients, buprenorphine HCl sublingual tablets in 1834 patients and buprenorphine sublingual solutions in 2470 patients. A total of 1270 females have received buprenorphine in clinical trials. Dosing recommendations are based on data from one trial of both tablet formulations and two trials of the ethanolic solution. All trials used buprenorphine in conjunction with psychosocial counseling as part of a comprehensive addiction treatment program. There have been no clinical studies conducted to assess the efficacy of buprenorphine as the only component of treatment.
In a double blind placebo- and active controlled study, 326 heroin-addicted subjects were randomly assigned to either buprenorphine and naloxone sublingual tablets 16 mg per day, 16 mg buprenorphine HCl sublingual tablets per day or placebo tablets. For subjects randomized to either active treatment, dosing began with one 8 mg tablet of buprenorphine HCl sublingual tablets on Day 1, followed by 16 mg (two 8 mg tablets) of buprenorphine HCl sublingual tablets on Day 2. On Day 3, those randomized to receive buprenorphine and naloxone sublingual tablets were switched to the combination tablet. Subjects randomized to placebo received one placebo tablet on Day 1 and two placebo tablets per day thereafter for four weeks. Subjects were seen daily in the clinic (Monday through Friday) for dosing and efficacy assessments. Take-home doses were provided for weekends. Subjects were instructed to hold the medication under the tongue for approximately 5 to 10 minutes until completely dissolved. Subjects received one hour of individual counseling per week and a single session of HIV education. The primary study comparison was to assess the efficacy of buprenorphine HCl sublingual tablets and buprenorphine and naloxone sublingual tablets individually against placebo. The percentage of thrice-weekly urine samples that were negative for non-study opioids was statistically higher for both buprenorphine HCl sublingual tablets and buprenorphine and naloxone sublingual tablets, than for placebo.
In a double-blind, double-dummy, parallel-group study comparing buprenorphine ethanolic solution to a full agonist active control, 162 subjects were randomized to receive the ethanolic sublingual solution of buprenorphine at 8 mg/day (a dose which is roughly comparable to a dose of 12 mg/day of buprenorphine HCl sublingual tablets or buprenorphine and naloxone sublingual tablets), or two relatively low doses of active control, one of which was low enough to serve as an alternative to placebo, during a 3 to 10 day induction phase, a 16-week maintenance phase and a 7-week detoxification phase. Buprenorphine was titrated to maintenance dose by Day 3; active control doses were titrated more gradually.
Maintenance dosing continued through Week 17, and then medications were tapered by approximately 20 to 30% per week over Weeks 18 to 24, with placebo dosing for the last two weeks. Subjects received individual and/or group counseling weekly.
Based on retention in treatment and the percentage of thrice-weekly urine samples negative for non-study opioids, buprenorphine was more effective than the low dose of the control, in keeping heroin addicts in treatment and in reducing their use of opioids while in treatment. The effectiveness of buprenorphine, 8 mg per day was similar to that of the moderate active control dose, but equivalence was not demonstrated.
In a dose-controlled, double-blind, parallel-group, 16-week study, 731 subjects were randomized to receive one of four doses of buprenorphine ethanolic solution. Buprenorphine was titrated to maintenance doses over 1-4 days ( Table 2) and continued for 16 weeks. Subjects received at least one session of AIDS education and additional counseling ranging from one hour per month to one hour per week, depending on site.
|
|
||||
|
Target Dose of Buprenorphine * |
Induction Dose | Maintenance dose | ||
| Day 1 | Day 2 | Day 3 | ||
| 1 mg | 1 mg | 1 mg | 1 mg | 1 mg |
| 4 mg | 2 mg | 4 mg | 4 mg | 4 mg |
| 8 mg | 2 mg | 4 mg | 8 mg | 8 mg |
| 16 mg | 2 mg | 4 mg | 8 mg | 16 mg |
Based on retention in treatment and the percentage of thrice-weekly urine samples negative for non-study opioids, the three highest tested doses were superior to the 1 mg dose. Therefore, this study showed that a range of buprenorphine doses may be effective. The 1 mg dose of buprenorphine sublingual solution can be considered to be somewhat lower than a 2 mg tablet dose. The other doses used in the study encompass a range of tablet doses from approximately 6 mg to approximately 24 mg.
INDICATIONS & USAGE
BUPRENORPHINE HYDROCHLORIDE CONTRAINDICATIONS
WARNINGS
Significant respiratory depression has been associated with buprenorphine, particularly by the intravenous route. A number of deaths have occurred when addicts have intravenously misused buprenorphine, usually with benzodiazepines concomitantly. Deaths have also been reported in association with concomitant administration of buprenorphine with other depressants such as alcohol or other opioids. Patients should be warned of the potential danger of the self-administration of benzodiazepines or other depressants while under treatment with buprenorphine HCl sublingual tablets or buprenorphine and naloxone sublingual tablets.
IN THE CASE OF OVERDOSE, THE PRIMARY MANAGEMENT SHOULD BE THE RE-ESTABLISHMENT OF ADEQUATE VENTILATION WITH MECHANICAL ASSISTANCE OF RESPIRATION, IF REQUIRED. NALOXONE MAY NOT BE EFFECTIVE IN REVERSING ANY RESPIRATORY DEPRESSION PRODUCED BY BUPRENORPHINE.
Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets should be used with caution in patients with compromised respiratory function (e.g., chronic obstructive pulmonary disease, cor pulmonale, decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression).
Patients receiving buprenorphine in the presence of other narcotic analgesics, general anesthetics, benzodiazepines, phenothiazines, other tranquilizers, sedative/hypnotics or other CNS depressants (including alcohol) may exhibit increased CNS depression. When such combined therapy is contemplated, reduction of the dose of one or both agents should be considered.
Buprenorphine is a partial agonist at the mu-opiate receptor and chronic administration produces dependence of the opioid type, characterized by withdrawal upon abrupt discontinuation or rapid taper. The withdrawal syndrome is milder than seen with full agonists, and may be delayed in onset.
Cases of cytolytic hepatitis and hepatitis with jaundice have been observed in the addict population receiving buprenorphine both in clinical trials and in post-marketing adverse event reports. The spectrum of abnormalities ranges from transient asymptomatic elevations in hepatic transaminases to case reports of hepatic failure, hepatic necrosis, hepatorenal syndrome, and hepatic encephalopathy. In many cases, the presence of pre-existing liver enzyme abnormalities, infection with hepatitis B or hepatitis C virus, concomitant usage of other potentially hepatotoxic drugs, and ongoing injecting drug use may have played a causative or contributory role. In other cases, insufficient data were available to determine the etiology of the abnormality. The possibility exists that buprenorphine had a causative or contributory role in the development of the hepatic abnormality in some cases. Measurements of liver function tests prior to initiation of treatment is recommended to establish a baseline. Periodic monitoring of liver function tests during treatment is also recommended. A biological and etiological evaluation is recommended when a hepatic event is suspected. Depending on the case, the drug should be carefully discontinued to prevent withdrawal symptoms and a return to illicit drug use, and strict monitoring of the patient should be initiated.
Cases of acute and chronic hypersensitivity to buprenorphine have been reported both in clinical trials and in the post-marketing experience. The most common signs and symptoms include rashes, hives, and pruritus. Cases of bronchospasm, angioneurotic edema, and anaphylactic shock have been reported. A history of hypersensitivity to buprenorphine is a contraindication to buprenorphine HCl sublingual tablets or buprenorphine and naloxone sublingual tablets use. A history of hypersensitivity to naloxone is a contraindication to buprenorphine and naloxone sublingual tablets use.
Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving a car or operating machinery, especially during drug induction and dose adjustment. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that buprenorphine therapy does not adversely affect their ability to engage in such activities. Like other opioids, buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets may produce orthostatic hypotension in ambulatory patients.
Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets, like other potent opioids, may elevate cerebrospinal fluid pressure and should be used with caution in patients with head injury, intracranial lesions and other circumstances where cerebrospinal pressure may be increased. Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets can produce miosis and changes in the level of consciousness that may interfere with patient evaluation.
Because it contains naloxone, buprenorphine and naloxone sublingual tablets are highly likely to produce marked and intense withdrawal symptoms if misused parenterally by individuals dependent on opioid agonists such as heroin, morphine, or methadone. Sublingually, buprenorphine and naloxone sublingual tablets may cause opioid withdrawal symptoms in such persons if administered before the agonist effects of the opioid have subsided.
PRECAUTIONS
Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets should be administered with caution in elderly or debilitated patients and those with severe impairment of hepatic, pulmonary, or renal function; myxedema or hypothyroidism, adrenal cortical insufficiency (e.g., Addison's disease); CNS depression or coma; toxic psychoses; prostatic hypertrophy or urethral stricture; acute alcoholism; delirium tremens; or kyphoscoliosis.
The effect of hepatic impairment on the pharmacokinetics of buprenorphine and naloxone is unknown. Since both drugs are extensively metabolized, the plasma levels will be expected to be higher in patients with moderate and severe hepatic impairment. However, it is not known whether both drugs are affected to the same degree. Therefore, dosage should be adjusted and patients should be watched for symptoms of precipitated opioid withdrawal.
Buprenorphine has been shown to increase intracholedochal pressure, as do other opioids, and thus should be administered with caution to patients with dysfunction of the biliary tract.
As with other mu-opioid receptor agonists, the administration of buprenorphine and naloxone sublingual tablets or buprenorphine HCl sublingual tablets may obscure the diagnosis or clinical course of patients with acute abdominal conditions.
DRUG INTERACTIONS
Buprenorphine is metabolized to norbuprenorphine by cytochrome CYP 3A4. Because CYP 3A4 inhibitors may increase plasma concentrations of buprenorphine, patients already on CYP 3A4 inhibitors such as azole antifungals (e.g., ketoconazole), macrolide antibiotics (e.g., erythromycin), and HIV protease inhibitors (e.g., ritonavir, indinavir and saquinavir) should have their dose of buprenorphine HCl sublingual tablets, or buprenorphine and naloxone sublingual tablets adjusted.
Based on anecdotal reports, there may be an interaction between buprenorphine and benzodiazepines. There have been a number of reports in the post-marketing experience of coma and death associated with the concomitant intravenous misuse of buprenorphine and benzodiazepines by addicts. In many of these cases, buprenorphine was misused by self-injection of crushed buprenorphine HCl sublingual tablets. Buprenorphine HCl sublingual tablets and buprenorphine and naloxone sublingual tablets should be prescribed with caution to patients on benzodiazepines or other drugs that act on the central nervous system, regardless of whether these drugs are taken on the advice of a physician or are taken as drugs of abuse. Patients should be warned of the potential danger of the intravenous self-administration of benzodiazepines while under treatment with buprenorphine and naloxone sublingual tablets or buprenorphine HCl sublingual tablets.
INFORMATION FOR PATIENTS
Patients should inform their family members that, in the event of emergency, the treating physician or emergency room staff should be informed that the patient is physically dependent on narcotics and that the patient is being treated with buprenorphine and naloxone sublingual tablets or buprenorphine HCl sublingual tablets.
Patients should be cautioned that a serious overdose and death may occur if benzodiazepines, sedatives, tranquilizers, antidepressants, or alcohol are taken at the same time as buprenorphine and naloxone sublingual tablets or buprenorphine HCl sublingual tablets.
Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving a car or operating machinery, especially during drug induction and dose adjustment. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that buprenorphine therapy does not adversely affect their ability to engage in such activities. Like other opioids, buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets may produce orthostatic hypotension in ambulatory patients.
Patients should consult their physician if other prescription medications are currently being used or are prescribed for future use.
Carcinogenicity data on buprenorphine and naloxone sublingual tablets are not available. Carcinogenicity studies of buprenorphine were conducted in Sprague-Dawley rats and CD-1 mice. Buprenorphine was administered in the diet to rats at doses of 0.6, 5.5, and 56 mg/kg/day (estimated exposure was approximately 0.4, 3 and 35 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) for 27 months. Statistically significant dose-related increases in testicular interstitial (Leydig’s) cell tumors occurred, according to the trend test adjusted for survival. Pair-wise comparison of the high dose against control failed to show statistical significance. In an 86-week study in CD-1 mice, buprenorphine was not carcinogenic at dietary doses up to 100 mg/kg/day (estimated exposure was approximately 30 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
The 4:1 combination of buprenorphine and naloxone was not mutagenic in a bacterial mutation assay (Ames test) using four strains of S. typhimurium and two strains of E. coli. The combination was not clastogenic in an in vitro cytogenetic assay in human lymphocytes, or in an intravenous micronucleus test in the rat.
Buprenorphine was studied in a series of tests utilizing gene, chromosome, and DNA interactions in both prokaryotic and eukaryotic systems. Results were negative in yeast (Saccharomyces cerevisiae) for recombinant, gene convertant, or forward mutations; negative in Bacillus subtilis “rec” assay, negative for clastogenicity in CHO cells, Chinese hamster bone marrow and spermatogonia cells, and negative in the mouse lymphoma L5178Y assay. Results were equivocal in the Ames test: negative in studies in two laboratories, but positive for frame shift mutation at a high dose (5 mg/plate) in a third study. Results were positive in the Green-Tweets (E. coli) survival test, positive in a DNA synthesis inhibition (DSI) test with testicular tissue from mice, for both in vivo and in vitro incorporation of [3H] thymidine, and positive in unscheduled DNA synthesis (UDS) test using testicular cells from mice.
Dietary administration of buprenorphine and naloxone sublingual tablets in the rat at dose levels of 500 ppm or greater (equivalent to approximately 47 mg/kg/day or greater; estimated exposure was approximately 28 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) produced a reduction in fertility demonstrated by reduced female conception rates. A dietary dose of 100 ppm (equivalent to approximately 10 mg/kg/day; estimated exposure was approximately 6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) had no adverse effect on fertility.
Reproduction studies of buprenorphine in rats demonstrated no evidence of impaired fertility at daily oral doses up to 80mg/kg/day (estimated exposure was approximately 50 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) or up to 5 mg/kg/day im or sc (estimated exposure was approximately 3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
PREGNANCY
Buprenorphine was not teratogenic in rats or rabbits after im or sc doses up to 5 mg/kg/day (estimated exposure was approximately 3 and 6 times, respectively, the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), after iv doses up to 0.8 mg/kg/day (estimated exposure was approximately 0.5 times and equal to, respectively, the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), or after oral doses up to 160 mg/kg/day in rats (estimated exposure was approximately 95 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) and 25 mg/kg/day in rabbits (estimated exposure was approximately 30 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). Significant increases in skeletal abnormalities (e.g., extra thoracic vertebra or thoraco-lumbar ribs) were noted in rats after sc administration of 1 mg/kg/day and up (estimated exposure was approximately 0.6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), but were not observed at oral doses up to 160 mg/kg/day. Increases in skeletal abnormalities in rabbits after im administration of 5 mg/kg/day (estimated exposure was approximately 6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) or oral administration of 1 mg/kg/day or greater (estimated exposure was approximately equal to the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) were not statistically significant.
In rabbits, buprenorphine produced statistically significant pre-implantation losses at oral doses of 1 mg/kg/day or greater and post-implantation losses that were statistically significant at iv doses of 0.2 mg/kg/day or greater (estimated exposure was approximately 0.3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
There are no adequate and well-controlled studies of buprenorphine and naloxone sublingual tablets or buprenorphine HCl sublingual tablets in pregnant women. Buprenorphine and naloxone sublingual tablets or buprenorphine HCl sublingual tablets should only be used during pregnancy if the potential benefit justifies the potential risk to the fetus.
Dystocia was noted in pregnant rats treated im with buprenorphine 5 mg/kg/day (approximately 3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). Both fertility and peri- and postnatal development studies with buprenorphine in rats indicated increases in neonatal mortality after oral doses of 0.8 mg/kg/day and up (approximately 0.5 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), after im doses of 0.5 mg/kg/day and up (approximately 0.3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), and after sc doses of 0.1 mg/kg/day and up (approximately 0.06 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). Delays in the occurrence of righting reflex and startle response were noted in rat pups at an oral dose of 80 mg/kg/day (approximately 50 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
Neonatal withdrawal has been reported in the infants of women treated with buprenorphine HCl sublingual tablets during pregnancy. From post-marketing reports, the time to onset of neonatal withdrawal symptoms ranged from Day 1 to Day 8 of life with most occurring on Day 1. Adverse events associated with neonatal withdrawal syndrome included hypertonia, neonatal tremor, neonatal agitation, and myoclonus. There have been rare reports of convulsions and in one case, apnea and bradycardia were also reported.
NURSING MOTHERS
PEDIATRIC USE
BUPRENORPHINE HYDROCHLORIDE ADVERSE REACTIONS
The safety of buprenorphine and naloxone sublingual tablets has been evaluated in 497 opioid-dependent subjects. The prospective evaluation of buprenorphine and naloxone sublingual tablets was supported by clinical trials using buprenorphine HCl sublingual tablets (buprenorphine tablets without naloxone) and other trials using buprenorphine sublingual solutions. In total, safety data are available from 3214 opioid-dependent subjects exposed to buprenorphine at doses in the range used in treatment of opioid addiction.
Few differences in adverse event profile were noted between buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets, or buprenorphine administered as a sublingual solution.
In a comparative study, adverse event profiles were similar for subjects treated with 16 mg buprenorphine and naloxone sublingual tablets or 16 mg buprenorphine HCl sublingual tablets. The following adverse events were reported to occur by at least 5% of patients in a 4-week study ( Table 3).
|
|
N (%) | N (%) | N (%) |
|
Body System /Adverse Event (COSTART Terminology) |
Buprenorphine and Naloxone Sublingual
Tablets |
Buprenorphine
HCl Sublingual Tablets 16 mg/day N = 103 |
Placebo N = 107 |
| Body As A Whole |
|
|
|
| Asthenia | 7 (6.5%) | 5 (4.9%) | 7 (6.5%) |
| Chills | 8 (7.5%) | 8 (7.8%) | 8 (7.5%) |
| Headache | 39 (36.4%) | 30 (29.1%) | 24 (22.4%) |
| Infection | 6 (5.6%) | 12 (11.7%) | 7 (6.5%) |
| Pain | 24 (22.4%) | 19 (18.4%) | 20 (18.7%) |
| Pain Abdomen | 12 (11.2%) | 12 (11.7%) | 7 (6.5%) |
| Pain Back | 4 (3.7%) | 8 (7.8%) | 12 (11.2%) |
| Withdrawal Syndrome | 27 (25.2%) | 19 (18.4%) | 40 (37.4%) |
| Cardiovascular System |
|
|
|
| Vasodilation | 10 (9.3%) | 4 (3.9%) | 7 (6.5%) |
| Digestive System |
|
|
|
| Constipation | 13 (12.1%) | 8 (7.8%) | 3 (2.8%) |
| Diarrhea | 4 (3.7%) | 5 (4.9%) | 16 (15.0%) |
| Nausea | 16 (15.0%) | 14 (13.6%) | 12 (11.2%) |
| Vomiting | 8 (7.5%) | 8 (7.8%) | 5 (4.7%) |
| Nervous System |
|
|
|
| Insomnia | 15 (14.0%) | 22 (21.4%) | 17 (15.9%) |
| Respiratory System |
|
|
|
| Rhinitis | 5 (4.7%) | 10 (9.7%) | 14 (13.1%) |
| Skin And Appendages |
|
|
|
| Sweating | 15 (14.0%) | 13 (12.6%) | 11 (10.3%) |
The adverse event profile of buprenorphine was also characterized in the dose-controlled study of buprenorphine solution, over a range of doses in four months of treatment. Table 4 shows adverse events reported by at least 5% of subjects in any dose group in the dose-controlled study.
|
|
|||||
|
Body System /Adverse Event (COSTART Terminology) |
Buprenorphine Dose * | ||||
|
Very Low * (N=184) |
Low * (N=180) |
Moderate * (N=186) |
High * (N=181) |
Total * (N=731) |
|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Body as a Whole |
|
|
|
|
|
| Abscess | 9 (5%) | 2 (1%) | 3 (2%) | 2 (1%) | 16 (2%) |
| Asthenia | 26 (14%) | 28 (16%) | 26 (14%) | 24 (13%) | 104 (14%) |
| Chills | 11 (6%) | 12 (7%) | 9 (5%) | 10 (6%) | 42 (6%) |
| Fever | 7 (4%) | 2 (1%) | 2 (1%) | 10 (6%) | 21 (3%) |
| Flu Syndrome | 4 (2%) | 13 (7%) | 19 (10%) | 8 (4%) | 44 (6%) |
| Headache | 51 (28%) | 62 (34%) | 54 (29%) | 53 (29%) | 220 (30%) |
| Infection | 32 (17%) | 39 (22%) | 38 (20%) | 40 (22%) | 149 (20%) |
| Injury Accidental | 5 (3%) | 10 (6%) | 5 (3%) | 5 (3%) | 25 (3%) |
| Pain | 47 (26%) | 37 (21%) | 49 (26%) | 44 (24%) | 177 (24%) |
| Pain Back | 18 (10%) | 29 (16%) | 28 (15%) | 27 (15%) | 102 (14%) |
| Withdrawal Syndrome | 45 (24%) | 40 (22%) | 41 (22%) | 36 (20%) | 162 (22%) |
| Digestive System |
|
|
|
|
|
| Constipation | 10 (5%) | 23 (13%) | 23 (12%) | 26 (14%) | 82 (11%) |
| Diarrhea | 19 (10%) | 8 (4%) | 9 (5%) | 4 (2%) | 40 (5%) |
| Dyspepsia | 6 (3%) | 10 (6%) | 4 (2%) | 4 (2%) | 24 (3%) |
| Nausea | 12 (7%) | 22 (12%) | 23 (12%) | 18 (10%) | 75 (10%) |
| Vomiting | 8 (4%) | 6 (3%) | 10 (5%) | 14 (8%) | 38 (5%) |
| Nervous System |
|
|
|
|
|
| Anxiety | 22 (12%) | 24 (13%) | 20 (11%) | 25 (14%) | 91 (12%) |
| Depression | 24 (13%) | 16 (9%) | 25 (13%) | 18 (10%) | 83 (11%) |
| Dizziness | 4 (2%) | 9 (5%) | 7 (4%) | 11 (6%) | 31 (4%) |
| Insomnia | 42 (23%) | 50 (28%) | 43 (23%) | 51 (28%) | 186 (25%) |
| Nervousness | 12 (7%) | 11 (6%) | 10 (5%) | 13 (7%) | 46 (6%) |
| Somnolence | 5 (3%) | 13 (7%) | 9 (5%) | 11 (6%) | 38 (5%) |
| Respiratory System |
|
|
|
|
|
| Cough Increase | 5 (3%) | 11 (6%) | 6 (3%) | 4 (2%) | 26 (4%) |
| Pharyngitis | 6 (3%) | 7 (4%) | 6 (3%) | 9 (5%) | 28 (4%) |
| Rhinitis | 27 (15%) | 16 (9%) | 15 (8%) | 21 (12%) | 79 (11%) |
| Skin and Appendages |
|
|
|
|
|
| Sweat | 23 (13%) | 21 (12%) | 20 (11%) | 23 (13%) | 87 (12%) |
| Special Senses |
|
|
|
|
|
| Runny Eyes | 13 (7%) | 9 (5%) | 6 (3%) | 6 (3%) | 34 (5%) |
DRUG ABUSE AND DEPENDENCE
Buprenorphine and naloxone sublingual tablets and buprenorphine HCl sublingual tablets are controlled as Schedule III narcotics under the Controlled Substances Act.
Buprenorphine is a partial agonist at the mu-opioid receptor and chronic administration produces dependence of the opioid type, characterized by moderate withdrawal upon abrupt discontinuation or rapid taper. The withdrawal syndrome is milder than seen with full agonists, and may be delayed in onset (see WARNINGS).
Neonatal withdrawal has been reported in the infants of women treated with buprenorphine HCl sublingual tablets during pregnancy (see PRECAUTIONS).
Buprenorphine and naloxone sublingual tablets contains naloxone and if misused parenterally, is highly likely to produce marked and intense withdrawal symptoms in subjects dependent on other opioid agonists.
OVERDOSAGE
Manifestations of acute overdose include pinpoint pupils, sedation, hypotension, respiratory depression and death.
The respiratory and cardiac status of the patient should be monitored carefully. In the event of depression of respiratory or cardiac function, primary attention should be given to the re-establishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. Oxygen, intravenous fluids, vasopressors, and other supportive measures should be employed as indicated.
IN THE CASE OF OVERDOSE, THE PRIMARY MANAGEMENT SHOULD BE THE RE-ESTABLISHMENT OF ADEQUATE VENTILATION WITH MECHANICAL ASSISTANCE OF RESPIRATION, IF REQUIRED. NALOXONE MAY NOT BE EFFECTIVE IN REVERSING ANY RESPIRATORY DEPRESSION PRODUCED BY BUPRENORPHINE.
High doses of naloxone hydrochloride, 10 to 35 mg/70 kg may be of limited value in the management of buprenorphine overdose. Doxapram (a respiratory stimulant) also has been used.
DOSAGE & ADMINISTRATION
Buprenorphine HCl Sublingual Tablets and Buprenorphine and Naloxone Sublingual Tablets are administered sublingually as a single daily dose in the range of 12 to 16 mg/day. When taken sublingually, Buprenorphine and Naloxone Sublingual Tablets and Buprenorphine HCl Sublingual Tablets have similar clinical effects and are interchangeable. There are no adequate and well-controlled studies using Buprenorphine and Naloxone Sublingual Tablets as initial medication. Buprenorphine HCl Sublingual Tablets contains no naloxone and is preferred for use during induction. Following induction, Buprenorphine and Naloxone Sublingual Tablets, due to the presence of naloxone, is preferred when clinical use includes unsupervised administration. The use of Buprenorphine HCl Sublingual Tablets for unsupervised administration should be limited to those patients who cannot tolerate Buprenorphine and Naloxone Sublingual Tablets, for example those patients who have been shown to be hypersensitive to naloxone.
Buprenorphine and Naloxone Sublingual Tablets and Buprenorphine HCl Sublingual Tablets should be placed under the tongue until they are dissolved. For doses requiring the use of more than two tablets, patients are advised to either place all the tablets at once or alternatively (if they cannot fit in more than two tablets comfortably) place two tablets at a time under the tongue. Either way, the patients should continue to hold the tablets under the tongue until they dissolve; swallowing the tablets reduces the bioavailability of the drug. To ensure consistency in bioavailability, patients should follow the same manner of dosing with continued use of the product.
Prior to induction, consideration should be given to the type of opioid dependence (i.e., long- or short-acting opioid), the time since last opioid use, and the degree or level of opioid dependence. To avoid precipitating withdrawal, induction with Buprenorphine HCl Sublingual Tablets should be undertaken when objective and clear signs of withdrawal are evident.
In a one-month study of Buprenorphine and Naloxone Sublingual Tablets induction was conducted with Buprenorphine HCl Sublingual Tablets. Patients received 8 mg of Buprenorphine HCl Sublingual Tablets on day 1 and 16 mg Buprenorphine HCl Sublingual Tablets on day 2. From day 3 onward, patients received Buprenorphine and Naloxone Sublingual Tablets at the same buprenorphine dose as day 2. Induction in the studies of buprenorphine solution was accomplished over 3 to 4 days, depending on the target dose. In some studies, gradual induction over several days led to a high rate of drop-out of buprenorphine patients during the induction period. Therefore it is recommended that an adequate maintenance dose, titrated to clinical effectiveness, should be achieved as rapidly as possible to prevent undue opioid withdrawal symptoms.
At treatment initiation, the dose of Buprenorphine HCl Sublingual Tablets should be administered at least 4 hours after the patient last used opioids or preferably when early signs of opioid withdrawal appear.
There is little controlled experience with the transfer of methadone-maintained patients to buprenorphine. Available evidence suggests that withdrawal symptoms are possible during induction to buprenorphine treatment. Withdrawal appears more likely in patients maintained on higher doses of methadone (>30mg) and when the first buprenorphine dose is administered shortly after the last methadone dose.
Buprenorphine and Naloxone Sublingual Tablets are preferred for maintenance treatment due to the presence of naloxone in the formulation.
The recommended target dose of Buprenorphine and Naloxone Sublingual Tablets is 16 mg/day. Clinical studies have shown that 16 mg of Buprenorphine HCl Sublingual Tablets or Buprenorphine and Naloxone Sublingual Tablets are a clinically effective dose compared with placebo and indicate that doses as low as 12 mg may be effective in some patients. The dosage of Buprenorphine and Naloxone Sublingual Tablets should be progressively adjusted in increments/decrements of 2 mg or 4 mg to a level that holds the patient in treatment and suppresses opioid withdrawal effects. This is likely to be in the range of 4 mg to 24 mg per day depending on the individual.
The decision to discontinue therapy with Buprenorphine and Naloxone Sublingual Tablets or Buprenorphine HCl Sublingual Tablets after a period of maintenance or brief stabilization should be made as part of a comprehensive treatment plan. Both gradual and abrupt discontinuation have been used, but no controlled trials have been undertaken to determine the best method of dose taper at the end of treatment.
HOW SUPPLIED
Buprenorphine Hydrochloride Sublingual Tablets are available as:
| 2 mg: |
White, oval, flat-faced, unscored tablet. Debossed with 798 on one side and stylized b on the other side. Each tablet contains 2.16 mg of buprenorphine HCl, equivalent to 2 mg of buprenorphine base. |
| Available in bottles of: | |
| 30 Tablets NDC 0093-5378-56 | |
| 100 Tablets NDC 0093-5378-01 | |
| 8 mg: |
White, oval, flat-faced, unscored tablet. Debossed with 799 on one side and stylized b on the other side. Each tablet contains 8.64 mg of buprenorphine HCl, equivalent to 8 mg of buprenorphine base. |
| Available in bottles of: | |
| 30 Tablets NDC 0093-5379-56 | |
| 100 Tablets NDC 0093-5379-01 |
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure as required.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
PATIENT INFORMATION
BUPRENORPHINE HYDROCHLORIDE CIII
Sublingual Tablets
Rx only
Read this information carefully before you take buprenorphine HCl sublingual tablets and each time you get more buprenorphine HCl sublingual tablets. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment. Only you and your doctor can decide if buprenorphine HCl sublingual tablets are right for you. Share the important information in this leaflet with members of your household.
What is the most important information I should know about buprenorphine HCl sublingual tablets?
- Buprenorphine HCl sublingual tablets can cause death from overdose, especially if you inject them with tranquilizers. Use buprenorphine hydrochloride sublingual tablets exactly the way your doctor tells you to with medicines used to treat depression or anxiety.
- Use buprenorphine HCl sublingual tablets only for the condition for which it was prescribed.
- Buprenorphine HCl sublingual tablets can cause drug dependence. This means that you can get withdrawal symptoms if you stop using the medicine too quickly. Buprenorphine HCl sublingual tablets are not for occasional (“as needed”) use.
- Prevent theft and misuse. Buprenorphine HCl sublingual tablets contain a narcotic painkiller that can be a target for people who abuse prescription medicines or street drugs. Therefore, keep your tablets in a safe place, to protect them from theft. Never give them to anyone else. Selling or giving away this medicine is against the law.
- In an emergency, have family members tell emergency room staff that you are dependent on opioids (narcotic painkillers) and are being treated with buprenorphine HCl sublingual tablets.
What are buprenorphine HCl sublingual tablets?
Buprenorphine HCl sublingual tablets are prescription medicine used to treat adults addicted to opioid (narcotic painkillers) medicines and drugs, such as morphine and heroin. Buprenorphine HCl sublingual tablets take the place of these medicines and drugs and may help you stop using and abusing them. Buprenorphine HCl sublingual tablets are a part of a complete addiction treatment program that also includes counseling or behavioral therapy.
Buprenorphine HCl sublingual tablets have not been studied in children.
Buprenorphine HCl sublingual tablets are tablets that contain only the medicine buprenorphine. It is like painkiller medicines such as morphine, street drugs like heroin, and addiction treatment medicines like methadone. Buprenorphine may give you less of a “high” than these other prescription medicines and street drugs. Withdrawal or stopping buprenorphine may be easier than stopping other prescription medicines and street drugs. Buprenorphine tablets are usually used under a doctor’s direct supervision.
Who should not take Buprenorphine HCl sublingual tablets?
Do not take buprenorphine HCl sublingual tablets if
- your doctor did not prescribe buprenorphine HCl sublingual tablets for you.
- you are allergic to buprenorphine, or any of the inactive ingredients in the medicines. See the end of this leaflet for a complete list of ingredients.
Your doctor should know about all your medical conditions before deciding if buprenorphine HCl sublingual tablets are right for you or what dose is best. Tell your doctor about all of your medical problems, especially the ones listed below:
- trouble breathing or lung problems
- head injury or brain problem
- liver or kidney problems
- gallbladder problems
- adrenal gland problems, such as Addison’s disease
- low thyroid (hypothyroidism)
- enlarged prostate gland (men)
- problems urinating
- a curve in your spine that affects your breathing
- severe mental problems or hallucinations (seeing or hearing things that are not really there)
- alcoholism
If any of these conditions apply to you, make sure you tell your doctor about them before taking buprenorphine HCl sublingual tablets.
Tell your doctor:
- if you are pregnant or plan to become pregnant. Buprenorphine HCl sublingual tablets may not be right for you. It is not known whether buprenorphine HCl sublingual tablets could harm your baby.
- if you are breast-feeding. Buprenorphine HCl sublingual tablets will pass through your milk and may harm your baby.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. They may cause serious side effects when taken with buprenorphine HCl sublingual tablets. Sometimes, the doses of certain medicines and buprenorphine HCl sublingual tablets need to be reduced if used together.
Do not take any other medicine, herbal, or over-the-counter medicine while using buprenorphine HCl sublingual tablets unless your doctor has told you it is okay.
How should I take buprenorphine HCl sublingual tablets?
- Follow your doctor’s directions exactly. Your doctor may change your dose after seeing how the medicine affects you. Do not change your dose unless your doctor tells you to change it. Do not take buprenorphine HCl sublingual tablets more often than prescribed.
- Put the tablets under your tongue and let them melt. This will take 2 to 10 minutes. Do not chew or swallow the tablets. The medicine will not work this way and you may get withdrawal symptoms.
-
If your doctor tells you to take more than 1 tablet,
you will be told to:
- take all tablets at the same time together under your tongue, or
- take 2 tablets, put them under your tongue. After they melt, put the next tablet or tablets under your tongue right away.
- hold the tablets under your tongue until they melt completely. The medicine will not work if swallowed and you may get withdrawal symptoms.
- Do not change the way you are told to take your medicine or you may get too
little or too much medicine.
- Do not inject (“shoot-up”) buprenorphine HCl sublingual tablets. Shooting-up is dangerous and you may get bad withdrawal symptoms.
- Buprenorphine HCl sublingual tablets can cause withdrawal symptoms if you take them too soon after using drugs like heroin, morphine, or methadone.
- If you miss a dose of buprenorphine HCl sublingual tablets, take it as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take 2 doses at once unless your doctor tells you to.
- Before stopping buprenorphine HCl sublingual tablets, ask your doctor how to stop to avoid withdrawal symptoms.
- If you take too much buprenorphine HCl sublingual tablets or overdose, call your local emergency number or poison control center right away.
After you stop taking buprenorphine HCl sublingual tablets, flush the unused tablets down the toilet.
What should I avoid while taking buprenorphine HCl sublingual tablets?
- Do not drive, operate heavy machinery, or perform any other dangerous activities until you know if this medicine affects how alert you are.
- Do not drink alcohol or take tranquilizers or sedatives (medicines that help you sleep) while using buprenorphine HCl sublingual tablets. You can die when you use these products with buprenorphine HCl sublingual tablets.
- Do not take other medicines without talking to your doctor. Other medicines include prescription and non-prescription medicines, vitamins, and herbal supplements. Be especially careful about medicines that may make you sleepy.
What are the possible side effects of buprenorphine HCl sublingual tablets?
Call your doctor or get medical help right away if
- You feel faint, dizzy, confused, or have any other unusual symptoms.
- Your breathing gets much slower than is normal for you.
These can be signs of an overdose or serious problem.
Buprenorphine HCl sublingual tablets may cause liver problems. Call your doctor right away if:
- Your skin or the white part of your eyes turns yellow (jaundice).
- Your urine turns dark.
- Your bowel movements (stools) turn light in color.
- You don’t feel like eating much food for several days or longer.
- You feel sick to your stomach (nausea).
- You have lower stomach pain.
Your doctor will do blood tests while you are taking buprenorphine HCl sublingual tablets to make sure your liver is okay.
- Buprenorphine HCl sublingual tablets can cause your blood pressure to drop. This can make you feel dizzy if you get up too fast from sitting or lying down.
- Buprenorphine HCl sublingual tablets can cause allergic reactions that can make it hard for you to breathe. Other symptoms of a bad allergic reaction include hives, swelling of your face, asthma (wheezing) or shock (loss of blood pressure and consciousness). Call a doctor or get emergency help right away if you get any of these symptoms.
You may have withdrawal symptoms when you start treatment with buprenorphine HCl sublingual tablets.
You can develop dependence from taking buprenorphine HCl sublingual tablets, and so you may get withdrawal symptoms when you stop taking buprenorphine HCl sublingual tablets. There is also a chance that you may abuse or get addicted to buprenorphine HCl sublingual tablets because buprenorphine HCl sublingual tablets are treatments for other drug addictions.
Some of the common side effects of buprenorphine HCl sublingual tablets are headache, pain, problems sleeping, nausea, sweating, stomach pain, and constipation.
These are not all the possible side effects of buprenorphine HCl sublingual tablets. For a complete list, ask your doctor or pharmacist.
GENERAL INFORMATION ABOUT THE SAFE AND EFFECTIVE USE OF BUPRENORPHINE HCL SUBLINGUAL TABLETS.
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use buprenorphine HCl sublingual tablets for conditions for which they were not prescribed. Do not give buprenorphine HCl sublingual tablets to other people, even if they have the same symptoms you have. Sharing is illegal and may cause severe medical problems. Keep buprenorphine HCl sublingual tablets out of the reach of children. Accidental overdose in children is dangerous and can result in death.
This leaflet summarizes the most important information about buprenorphine HCl sublingual tablets. If you would like more information, talk with your doctor. Also, you can ask your pharmacist or doctor for information about buprenorphine HCl sublingual tablets that is written for health professionals. For more information call 1-800-227-7522.
What are the ingredients of buprenorphine hydrochloride sublingual tablets?
Active Ingredients: buprenorphine hydrochloride
Inactive Ingredients: anhydrous citric acid, corn starch, lactose monohydrate, magnesium stearate, mannitol, povidone and sodium citrate.
PHYSICIAN INFORMATION
Sublingual Tablets
Answers to Frequently Asked Questions
Who is qualified to prescribe buprenorphine HCl sublingual tablets?
Physicians who:
- Meet one or more of the following training requirements
- Hold a subspecialty board certification in addiction psychiatry from the American Board of Medical Specialities
- Hold an addiction certification from the American Society of Addiction Medicine
- Hold a subspecialty board certification in Addiction Medicine from the American Osteopathic Association
- Have completed not less than 8 hours of authorized training on the treatment or management of opioid-dependent patients. This training may include classroom situations, seminars at professional society meetings, electronic communications, or other media. The American Society of Addiction Medicine, The American Academy of Addiction Psychiatry, the American Medical Association, the American Osteopathic Association, and the American Psychiatric Association are all authorized to provide this training. Details and website addresses can be found in the section below.
- AND meet both of the following criteria:
- Have the capacity to provide or to refer patients for necessary ancillary services, such as psychosocial therapy.
- Agree to treat no more than 30 patients at any one time in their individual or group practice
When and where are training sessions being held?
Each of the above organizations has scheduled training sessions. You may contact them directly at the addresses below, or visit their web sites.
I am already qualified. What do I do next?
The Drug Addiction Treatment Act (DATA) requires that before you begin prescribing buprenorphine HCl sublingual tablets you must notify the Secretary of Health and Human Services of your intent to treat patients with these products. The agency within the Department of Health and Human Services to be notified is the Substance Abuse and Mental Health Services Administration (SAMHSA). Notification is handled within SAMHSA by the Division of Pharmacologic Therapies (DPT) within the Center for Substance Abuse Treatment (CSAT). For convenience CSAT has developed a form that may be used for your notification. You may complete the notification form online or download the form by visiting CSAT’s web site at www.dpt.samhsa.gov. If you prefer, you may also notify by letter if you include all of the required information. All forms (or letters) should be mailed or faxed to:
Call CSAT/DPT if you have any questions about the notification process or need help completing the form. They can be reached at (301) 443-7745.
What happens after my notification is sent to CSAT?
CSAT will communicate with the Drug Enforcement Administration (DEA), review your notification and then notify DEA that you are qualified as required by the DATA. The DATA allows 45 days for this review process. No later than at the end of that 45-day period, DEA will issue a unique identification number indicating that you are a qualifying physician under the DATA. DEA is developing regulations that will require this number along with your existing DEA registration number to be included on all prescriptions issued for the treatment of opioid dependence under the DATA; therefore it is strongly recommended that you include this number when you write prescriptions for buprenorphine HCl sublingual tablets for the treatment of opioid dependence. CSAT will send you a letter notifying you of the new DEA identification number that will be assigned. You will subsequently receive a revised DEA registration certificate (showing both numbers).
Do I have to wait 45 days before treating patients?
The DATA envisions physicians notifying CSAT as soon as they are qualified, but makes provision for those who find themselves in the position of being qualified and needing to treat a patient, but not having notified CSAT. In this case, you must first notify CSAT and DEA of your intent before treating the patient; this can be done electronically on the internet by checking the appropriate box, or by faxing in the form included in this package to CSAT at: (301) 443-3994.
During the training sessions, as well as in the product information and CSAT Guidelines, it is recommended that patients be given initial doses under supervision. It is not my normal practice to keep a stock of controlled substances in my office. How do I get buprenorphine HCl sublingual tablets for use in the office?
State laws vary regarding stocking of controlled substances. If you have a routine supplier of products such as vaccines, or injectable products that you use in your office, that supplier will be able to provide you with buprenorphine HCl sublingual tablets. If you do not have a normal supplier of such products we will facilitate the establishment of a relationship with a supplier. You may call our toll-free number 1-800-227-7522.
What storage and record-keeping requirements are associated with maintenance of a supply of buprenorphine HCl sublingual tablets in my office?
For a full listing of requirements for a specific State you may call our toll-free number 1-800-227-7522. Generally, you will be required to keep the medications in a secure environment. They should be kept in a locked compartment with limited access. You will also be required to maintain a written record of the disposition of all doses. Usually this can be done with the maintenance of a logbook in which you record all incoming doses and account for each dispensed dose as it is used. This record must be kept current at all times. Additional requirements may be in place in your State.
While I appreciate the convenience of maintaining a supply of buprenorphine HCl sublingual tablets in my office for induction purposes, the situation at our office precludes such an arrangement. How do I manage supervised induction doses without maintaining such a supply in my office?
For those physicians who do not wish to maintain a supply of buprenorphine HCl sublingual tablets in their offices, where State law and regulation allows, you would write a prescription only for the initial dose of buprenorphine HCl sublingual tablets. If pharmacy delivery services are available, you may choose to arrange to have the dose delivered to your office; if not give the prescription, to the patient (or, if available, to a trustworthy family member accompanying the patient) with instructions that the prescription is to be taken to the pharmacy, filled, and brought back to your office for dosing. It is recommended that you call or fax ahead to ensure availability of the medication and to reduce patient waiting time. You should instruct the patient that on his or her return to the office the induction dose will be administered, and that he or she will be monitored in your office. The pharmacist should reiterate this instruction upon filling the prescription. You may wish to limit the prescription to one days’ dose, and repeat this method for the first several days of treatment before providing a prescription for several days’ supply at one time.
Will prescriptions be valid at any pharmacy, or will I need to refer patients to a specific store?
Prescriptions will be valid at any pharmacy. However, prior to prescribing
buprenorphine HCl sublingual tablets, if you do not maintain a supply of tablets
for induction dosing in your office, it is essential that you establish a
relationship with one or more specific pharmacies in your area who will be in a
position to provide your patients with initial doses as well as instructions for
returning to your office for induction and the follow-up prescription. (Such a
relationship is also recommended if you intend to maintain initial dosing
supplies in your office.) Generally, a pharmacy near your office is recommended
for patient convenience. If possible, it is advisable to identify a pharmacy
that will deliver initial doses to your office, so that patients do not have to
leave and return for induction dosing. Alternatively, it is recommended that you
avail yourself of any call-in or fax-in prescription services provided, to
reduce patient waiting time.
Are there special confidentiality issues I should consider?
Remember that you may be communicating with the pharmacist to verify prescriptions for a particular patient. As you may know, there are special federal regulations concerning the confidentiality of substance abuse treatment, records (42 CFR Part 2) and the privacy of health records (HIPAA). To ensure that you will be able to communicate with the pharmacist to confirm the validity of a buprenorphine HCl sublingual tablets prescription, it is recommended that you have the patient sign a release of information at the time of the office visit. A sample consent form with all the elements required under 42 CFR Part 2 is included with this booklet as an attachment. It is particularly important to obtain the patient’s consent if you elect to phone or FAX in prescriptions, as this constitutes disclosure of the patient’s treatment. When the prescription is directly transmitted by the physician, there are also prohibitions on the further redisclosure of patient identifying information by the pharmacist. 42 CFR Part 2 does not apply when it is the patient who delivers the presciption to the pharmacist, without direct communication from the physician to the pharmacist.
To learn more about these regulations, visit the SAMHSA website www.hipaa.samhsa.gov, or call 1-866-BUP-CSAT.
I’m familiar with general principles of addiction treatment, but this is my first experience with office-based prescription of this type of medication. What precautions should I take in my practice to prevent diversion and abuse?
You should consider the following suggestions:
- Initiate treatment with supervised administration, progressing to unsupervised administration as your patient’s clinical stability permits.
- Limit the use of buprenorphine HCl sublingual tablets to supervised use, wherever possible. Recall that the buprenorphine and naloxone sublingual tablets product contains naloxone, which buprenorphine HCl sublingual tablets does not. The naloxone in buprenorphine and naloxone sublingual tablets is likely to precipitate withdrawal symptoms when injected by individuals dependent on heroin, morphine, or other full opiate agonists. Therefore, it is expected that buprenorphine and naloxone sublingual tablets will be less attractive to “street addicts” and less likely to be diverted. Therefore, it is strongly recommended that buprenorphine and naloxone sublingual tablets be used whenever unsupervised administration is planned.
- As your patients progress, and you consider prescribing buprenorphine and naloxone sublingual tablets for take-home use; when determining the size of the prescription you write, you should consider your patient’s level of stability, the security of his or her home situation, and other factors likely to affect the ability to manage supplies of take-home medication.
- Have plans in place to deal with patient requests for replacement of prescriptions or supplies of medication that are described as lost or stolen.
- Keep tight control of your prescription pads. Never leave them in the examination room, even inside a desk drawer. Never sign an incomplete prescription blank.
- Write all numbers (quantity and strength) in both numbers and letters –like you write your checks.
- Establish a relationship with the pharmacies you expect to be filling your prescriptions for buprenorphine HCl sublingual tablets and discuss potential diversion problems and controls with them.
- Request photo (or other) I.D. and Social Security number and maintain copies in patient’s record.
- If you suspect an attempt to divert prescription medications, call your local police department.
Where can I get more information on treating patients with buprenorphine HCl sublingual tablets?
- Refer to the physician package insert for prescribing information. Additional recommendations may be found in treatment guidelines available for free from the Center for Substance Abuse Treatment at the Substance Abuse and Mental Health Services Administration. Additional information is also available on the CSAT web site at www.dpt.samhsa.gov
- Refer to the package insert for full information on the adverse events seen during the clinical trials using buprenorphine for opiate addiction treatment. Note the important precautions and warnings to share with patients, such as the risk of fatal respiratory depression when buprenorphine is combined with other depressants. Also note other important safety issues such as the fact that buprenorphine should be administered with caution in the elderly or debilitated patient, and those with severe impairment of hepatic, pulmonary or renal function; and that buprenorphine may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving a car or operating machinery, especially during drug induction and dose adjustment.
- General information on the treatment of addiction is available through;
|
Notification of Intent to Use Schedule III, IV, or V Opioid Drugs for the Maintenance and Detoxification Treatment of Opiate Addiction under 21 USC § 823(g)(2) |
Form Approved: 0930- 0234 Expiration Date: 10/31/2002 See OMB Statement on Reverse |
|
|
DATE OF SUBMISSION |
|
Note: Notification is required by Sec. 303(g)(2), Controlled Substances Act (21 USC § 823(g)(2)). See instructions on reverse. |
|
|
1a. NAME OF PRACTITIONER b. State Medical License Number |
c. DEA Registration Number |
|
2. ADDRESS OF PRIMARY LOCATION (Include Zip Code) |
3. TELEPHONE NUMBER (Include Area Code) 4. FAX NUMBER (Include Area Code) 5. EMAIL ADDRESS (optional) |
|
6. NAME AND ADDRESS OF GROUP PRACTICE 7. GROUP PRACTICE EMPLOYER IDENTIFICATION NUMBER |
8. PURPOSE OF NOTIFICATION (Check all that apply) New Immediate |
|
9. GROUP PRACTITIONERS NAME _______________________________________________DEA Registration Number NAME _______________________________________________DEA Registration Number (Include additional pages as necessary to identify each group practice member.) |
|
|
10. CERTIFICATION OF USE OF NARCOTIC DRUGS UNDER THIS NOTIFICATION I certify that I will only use schedule III, IV, or V drugs or combinations of drugs that have been approved by the FDA for use in maintenance or detoxification treatment and that have not been the subject of an adverse determination. |
|
|
11. CERTIFICATION OF QUALIFYING CRITERIA (Check each appropriate source and provide documentation.) I certify that I meet at least one of the following criteria and am therefore a qualifying physician (check and provide documentation for all that apply): Subspecialty board certification in addiction psychiatry from the American Board of Medical Specialties Addiction certification from the American Society of Addiction Medicine Subspecialty board certification in addiction medicine from the American Osteopathic Association Completion of not less than eight hours of training for the treatment and management of opiate-dependent patients provided by the following organization(s): Date and location of training American Society of Addiction Medicine American Academy of Addiction Psychiatry American Medical Association American Osteopathic Association American Psychiatric Association Other (specify, include date and location) Participation as an investigator in one or more clinical trials leading to the approval of a schedule III, IV, or V narcotic drug for maintenance or detoxification treatment State medical licensing board-approved experience or training in the treatment and management of opiate-dependent patients. OTHER (Specify) |
|
|
12. CERTIFICATION OF CAPACITY I certify that I have the capacity to refer patients for appropriate counseling and other appropriate ancillary services. |
|
|
13. CERTIFICATION OF MAXIMUM PATIENT LOAD I certify that I, or my group practice will not exceed 30 patients for maintenance or detoxification treatment at one time. SMA-167 |
|
|
14. CONSENT TO RELEASE IDENTIFYING INFORMATION TO SAMHSA TREATMENT FACILITY LOCATOR I consent to the release of my name, address, and phone number to the SAMHSA Treatment Facility Locator. I do not consent to the release of my name, address, and phone number to the SAMHSA Treatment Facility Locator. |
|
|
15. I certify that the information presented above is true and correct to the best of my knowledge. I certify that I will notify SAMHSA at the address below if any of the information contained on this form changes. Note: Any false, fictitious, or fraudulent statements or information presented above or misrepresentations relative thereto may violate Federal laws and could subject you to prosecution, and/or monetary penalties, and or denial, revocation or suspension of DEA registration (See 18 U.S.C.§1001; 31 U.S.C.§§3801-3812; 21 U.S.C.§824.) Signature Date |
|
|
Please send the completed form to: Substance Abuse and Mental Health Services Administration Office of Pharmacologic and Alternative Therapies Attention: Opioid Treatment Waiver Program CSAT, Rockwall II Building, Suite 74 0 5600 Fishers Lane Rockville, MD 20857 Fax 301-443-3994 Phone 301-443-7745 |
|
|
This form is intended to facilitate the implementation of the provisions of 21 USC § 823 (g)(2). The Secretary of DHHS will use the information provided to determine whether practitioners meet the qualifications for waivers from the separate registration requirements under the Controlled Substances Act (21 USC § 823 (g)(1)). The Drug Enforcement Administration will assign an identification number to qualifying practitioners and the number will be included in the practitioner’s registration under 21 USC § 823 (f). This form may be completed and submitted electronically (including facsimile) to facilitate processing. |
|
| 1. The practitioner must identify the DEA registration number issued under 21 USC§ 823(f) to prescribe substances controlled in Schedules III, IV, or V. | 2. The address should be the primary address listed in the practitioner’s registration under § 823(f). Only one address should be specified. If the narcotic drugs or combinations to be used under this notification are to be dispensed by the practitioner then the address must reflect the site where the medication will be dispensed. |
|
6. Group practice is defined under section 1877(h)(4) of the Social Security Act. 14. The SAMHSA Treatment Facility Locator is freely accessible on the World Wide Web (http://findtreatment.samhsa.gov) and is widely used by the members of the treatment seeking public and referring professionals. It lists more than 11,000 facilities that offer specialized drug and alcohol abuse treatment programs and provides links to many other sources of information on substance abuse. The information on physicians will be retrieved by a geographical search of a separate category within the locator. No disclosures to the SAMHSA Treatment Facility Locator will be made in the absence of express consent. |
8. Purpose of notification: New - an initial notification for a waiver submitted for the purpose of obtaining an identification number from DEA for inclusion in the registration under 21 U.S.C. §823(f). Immediate - a notification submitted for the purpose of notifying the Secretary and the Attorney General of the intent to immediately facilitate the treatment of an individual (one) patient. Note: It is permissible to submit a new and immediate notification simultaneously. |
|
PRIVACY ACT INFORMATION Authority: Section 303 of the Controlled Substances Act of 1970 (21 U.S.C §823(g)(2)). Purpose: To obtain information required to determine whether a practitioner meets the requirements of 21 U.S.C §823(g)(2). Routine Uses: Disclosures of information from this system are made to the following categories of users for the purposes stated: A. Medical specialty societies to verify practitioner qualifications. B. Other federal law enforcement and regulatory agencies for law enforcement and regulatory purposes. C. State and local law enforcement and regulatory agencies for law enforcement and regulatory purposes. D. Persons registered under the Controlled Substance Act (PL 91-513) for the purpose of verifying the registration of customers and practitioners. Effect: This form was created to facilitate the submission and review of waivers under 21 U.S.C. §823(g)(2). This does not preclude other forms of notification. Paperwork Reduction Act Statement Public reporting burden for completing this form is estimated to average 5 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the completed form. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. The OMB control number for this project is (0930-0234). |
SMA-167
Attachment to Physician’s Brochure:
SAMPLE 42 CFR Part 2.31 Consent Form
- I (name of patient)
________________________________{time}
Authorize: - Dr.______________________________________________________________________
- To disclose: (kind and amount of information to be disclosed)
Any information needed to confirm the validity of my prescription and for submission for payment for the prescription.
_________________________________________________________________________ - To: (name or title of the person or organization to which disclosure is to
be made)
The dispensing pharmacy to whom I present my prescription or to whom my prescription is called/sent/faxed, as well as to third party payors. - For (purpose of the disclosure)
Assuring the pharmacy of the validity of the prescription, so it can be legally dispensed, and for payment purposes.
__________________________________________________________________________ - Date (on which this consent is signed)___________________________________________
- Signature of patient _________________________________________________________
- Signature of parent or guardian (where
required)
__________________________________________________________________________ - Signature of person authorized to sign in lieu of the patient (where
required)
__________________________________________________________________________ - This consent is subject to revocation at any time except to the extent that the program which is to make the disclosure has already taken action in reliance on it. If not previously revoked, this consent will terminate upon: (specific date, event, or condition)
Termination of treatment
(c) Expired, deficient, or false consent. A disclosure may not be made on the basis of a consent which: (1) Has expired; (2) On its face substantially fails to conform to any of the requirements set forth in paragraph (a) of this section; (3) Is known to have been revoked; or (4) Is known, or through a reasonable effort could be known, by the person holding the records to be materially false. (Approved by the Office of Management and Budget under control number 0930-0099)
Notice to accompany disclosure:
Each disclosure made with the patient's written consent must be accompanied by the following written statement: This information has been disclosed to you from records protected by Federal confidentiality rules (42 CFR part 2). The Federal rules prohibit you from making any further disclosure of this information unless further disclosure is expressly permitted by the written consent of the person to whom it pertains or as otherwise permitted by 42 CFR part 2. A general authorization for the release of medical or other information is NOT sufficient for this purpose.
INFORMATION FOR PHARMACISTS
BUPRENORPHINE HYDROCHLORIDE CIII
Sublingual Tablets
Rx only
What are buprenorphine HCl sublingual tablets?
Buprenorphine HCl sublingual tablets are sublingual tablets indicated for the treatment of opioid dependence. Buprenorphine tablets contain buprenorphine (a partial agonist at the mu-opioid receptor and an antagonist at the kappa-opioid receptor). Buprenorphine HCl sublingual tablets contain buprenorphine only.
Why is it important for all pharmacists to learn about buprenorphine HCl sublingual tablets?
For the first time, pharmacists will play a role in the delivery of opiate addiction treatment. Buprenorphine HCl sublingual tablets are the first medications approved for office-based treatment of opioid dependence under the Drug Addiction Treatment Act of 2000 (DATA). Prior to the passage of this law, it was illegal for a doctor to prescribe narcotic drugs for the treatment of narcotic dependence. Opioid dependence treatment of this type could only be provided at specially registered clinics. Under the new law, only opiate addiction treatment drugs under Schedule II are confined to use in the clinic setting. Less tightly controlled drugs (Schedules III-V) may be prescribed for opiate addiction treatment by specially qualified doctors who treat patients in their private offices.
Why are there two formulations?
Buprenorphine and naloxone sublingual tablets is the preferred medication for maintenance treatment due to the presence of naloxone in the formulation, which is intended to deter intravenous abuse by persons dependent on other opiates.
Buprenorphine HCl sublingual tablets, which does not contain naloxone, may be better tolerated by patients in the first several days of treatment and is generally preferred for induction. “Induction” refers to the initial period of treatment, during which time the patient should receive medication under the doctor’s supervision in the office. Patients or their family members may need to come and pick up induction doses each day for the first several days of treatment (or you may be asked to arrange delivery to the doctor’s office, if your pharmacy provides this service). Therefore, while you may see prescriptions for small amounts of buprenorphine HCl sublingual tablets presented for induction doses, you should expect the majority of prescriptions to be for buprenorphine and naloxone sublingual tablets. Buprenorphine HCl sublingual tablets are controlled as Schedule III narcotics under the Controlled Substances Act.
How are they supplied?
| 2 mg: |
White, oval, flat-faced, unscored tablet. Debossed with 798 on one side and stylized b on the other side. Each tablet contains 2.16 mg of buprenorphine HCl, equivalent to 2 mg of buprenorphine base. |
| Available in bottles of: | |
| 30 Tablets NDC 0093-5378-56 | |
| 100 Tablets NDC 0093-5378-01 |
|
| 8 mg: |
White, oval, flat-faced, unscored tablet. Debossed with 799 on one side and stylized b on the other side. Each tablet contains 8.64 mg of buprenorphine HCl, equivalent to 8 mg of buprenorphine base. |
| Available in bottles of: | |
| 30 Tablets NDC 0093-5379-56 | |
| 100 Tablets NDC 0093-5379-01 |
I’ve heard that buprenorphine is safer than methadone. Can these drugs be dangerous?
Significant respiratory depression has been associated with buprenorphine, particularly when administered intravenously. A number of deaths have occurred when addicts have intravenously misused buprenorphine, usually with benzodiazepines concomitantly. Deaths have also been reported in association with concomitant administration of buprenorphine and other depressants such as alcohol or other opioids.
Chronic administration of buprenorphine HCl sublingual tablets produces dependence of the opiate type, characterized by withdrawal upon abrupt discontinuation or rapid taper. The withdrawal syndrome is milder than seen with full agonists, and may be delayed in onset.
Be sure to read the full Prescribing Information for complete WARNINGS and PRECAUTIONS.
What other information should I relay to patients?
It’s important that you make sure patients understand their physicians’ instructions, and that you answer any questions they may have.
When counseling patients, be sure to discuss any relevant precautions as listed in the Prescribing Information, including but not limited to the following:
- Patients should inform their family members that, in the event of emergency, the treating physician or emergency room staff should be informed that the patient is physically dependent on opioids and that the patient is being treated with buprenorphine HCl sublingual tablets.
- Patients should be cautioned that a serious overdose may occur if benzodiazepines, sedatives, tranquilizers, antidepressants, or alcohol are taken at the same time as buprenorphine HCl sublingual tablets.
- Patients should be cautioned that buprenorphine HCl sublingual tablets may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving a car or operating machinery. Patients should be cautioned not to drive or operate complex machinery until they know how buprenorphine HCl sublingual tablets affects their ability to function in these circumstances, such as driving a car.
- Patients should consult their physician if other prescription medications are currently being used or are prescribed for future use.
What are the possible side effects of buprenorphine HCl sublingual tablets?
The most common adverse events reported in clinical trials with buprenorphine HCl sublingual tablets were headache, withdrawal syndrome, pain, nausea, insomnia, sweating, abdominal pain, back pain, constipation, infection, asthenia, rhinitis, anxiety, and depression.
What is the role of the pharmacist in ensuring safe use of buprenorphine HCl sublingual tablets?
As a pharmacist, you will play an important role in ensuring that buprenorphine HCl sublingual tablets are used safely and appropriately. Each time you fill a prescription for buprenorphine HCl sublingual tablets, make sure to:
- Verify that the prescriptions you receive are from physicians who are in compliance with the provisions of the DATA (see below).
- Remind patients who are picking up induction doses to return as directed to the doctor’s office so that they can be supervised while taking the medication.
- Be vigilant in detecting fraudulent prescriptions or simultaneous prescriptions for the same patient from multiple suppliers.
Who is qualified to prescribe buprenorphine HCl sublingual tablets?
The DATA limits office-based use of buprenorphine HCl sublingual tablets to physicians who meet special training criteria and can provide appropriate services. To be qualified, physicians must:
- Meet one or more of the following training requirements
- Hold a subspecialty board certification in addiction psychiatry from the American Board of Medical Specialties
- Hold a subspecialty board certification in Addiction Medicine from the American Osteopathic Association
- Hold an addiction certification from the American Society of Addiction Medicine
- Have completed not less than 8 hours of authorized training on the treatment or management of opioid-dependent patients. This training may include classroom situations, seminars at professional society meetings, electronic communications, or other media. The American Society of Addiction Medicine, The American Academy of Addiction Psychiatry, the American Medical Association, the American Osteopathic Association, and the American Psychiatric Association are all authorized to provide this training.
- AND meet both of the following criteria:
- Have the capacity to provide or to refer patients for necessary ancillary services, such as psychosocial therapy.
-
How can I be sure a physician is qualified to prescribe buprenorphine HCl sublingual tablets.
Physicians who meet the qualification criteria listed in the previous section must also notify the Secretary of Health and Human Services of their intent to prescribe buprenorphine HCl sublingual tablets before doing so. Once all relevant criteria are verified, DEA will issue the physician a unique identification number indicating that he or she is a qualifying physician under the DATA.
The Center for Substance Abuse Treatment (CSAT, a component of the Substance Abuse and Mental Health Services Administration) will send a letter informing the physician of the new DEA identification number. The physicians will subsequently receive a revised DEA registration certificate (showing both numbers).
What if I get a prescription from a doctor who does not have a special DEA identification number?
Call that physician for clarification that the physician has made the appropriate notification to DHHS. DEA is developing regulations that will require this number along with the physician’s existing DEA registration number to be included on all prescriptions issued for the treatment of opioid dependence; therefore physicians are being strongly urged to include this number on prescriptions.
Most physicians will make arrangements to obtain the identification number before prescribing buprenorphine HCl sublingual tablets, but in rare cases a physician may need to write a prescription before the number has been issued. This is allowed under the DATA provided the physician has notified the Department of Health and Human Services of his/her intention to begin treating a patient right away; the notification form includes a check box for this situation.
Agree to treat no more than 30 patients at any one time in their individual or group practice
Are there confidentiality issues I should be aware of related to substance abuse treatment?
There are special federal regulations concerning the confidentiality of substance abuse treatment records (42 CFR Part 2) and the privacy of health records (HIPAA), which may come into play in your interactions with physicians to verify prescriptions for buprenorphine HCl sublingual tablets. To ensure that physicians will be able to communicate with you to confirm the validity of a buprenorphine HCl prescription, it is recommended that the physician have the patient sign a release of information at the time of the office visit. A sample consent form with all the elements required under 42 CFR Part 2 is included. It is particularly important to obtain the patient's consent if the physician elects to phone or FAX in prescriptions, as this constitutes disclosure of the patient's treatment. When the prescription is directly transmitted by the physician, there are also prohibitions on the further redisclosure of patient identifying information by the pharmacist. 42CFR Part 2 does not apply when it is the patient who delivers the prescription to the pharmacist, without direct communication from the physician to the pharmacist.
To learn more about these regulations, visit the SAMHSA website www.hipaa.samhsa.gov, or call 1-866-BUP-CSAT for information.
Again, Pharmacists who seek information to verify whether or not physicians have valid waivers may contact 1-866-BUP-CSAT, or by email at info@buprenorphine.samhsa.gov
How will physicians obtain supplies of medication for induction?
Because induction doses of buprenorphine HCl sublingual tablets should be given in the physician’s office, many physicians will maintain a supply of each medication in their office. Most physicians will get this supply through their normal supplier or the manufacturer. Some physicians, however, will write prescriptions for individual patients’ induction doses at the time of the patient appointment. The prescribing physician may call or fax ahead to your pharmacy to request delivery (if you provide this service), or to ensure the medication will be ready in advance of the patient’s arrival. (Recall that the patient is likely to be in mild withdrawal while awaiting the prescription.) Some physicians may send a patient’s family member to the pharmacy to pick up the induction dose.
What should I do when a patient presents a prescription for an induction dose?
Physicians who choose not to maintain supplies of buprenorphine HCl sublingual tablets in their offices may give their patients a prescription for their induction doses with instructions to return to the office for supervision while the dose is administered. Fill the prescription as you normally would, then make sure the patient understands that he or she must return to the doctor’s office to take the medication. It may take several days of supervised administration to complete the induction process, therefore, some patients may be visiting your pharmacy repeatedly at the beginning of treatment.
Are there any special storage, record-keeping, or other requirements associated with buprenorphine HCl sublingual tablets?
As Schedule III controlled substances, buprenorphine HCl sublingual tablets are subject to certain federal regulations covering areas such as record-keeping, inventory, proper dispensing and disposal. These are explained in the Drug Enforcement Administration’s Pharmacist’s Manual, which can be found at www.deadiversion.usdoj.gov/pubs/manuals/pharm2/index.htm.
Many states have their own, additional requirements for pharmacists dispensing controlled substances. Be sure to check with the appropriate authority in your state. For more information, visit the website of the National Association of Boards of Pharmacy at www.nabp.org for links to individual state boards of pharmacy.
In addition, since drug addiction is a sensitive topic, you should make sure you have access to a private area in which to counsel patients about buprenorphine HCl sublingual tablets therapy. When speaking with these patients, it is important to keep in mind that addicts in withdrawal may be irritable and short on patience.
What else can I do to help safeguard against diversion?
According to federal law, pharmacists and prescribers jointly share legal responsibility for the legitimacy of a prescription. Communication between you and the prescriber is vital to ensure the validity of each prescription you’re asked to fill.
However, even if you determine that an individual prescription is legal, you should still be aware of other means by which addicts may attempt to divert their prescriptions. For example, an opioid user may present to 2 or more qualified prescribers, and therefore receive multiple prescriptions for buprenorphine HCl sublingual tablets. If a patient brings you more than 1 prescription covering the same therapeutic period, you have a legal duty to recognize that they are probably not for therapeutic use. You should refuse to fill the second prescription, and notify both prescribing physicians.
In addition, you should be aware that the DATA allows each physician to treat no more than 30 patients with buprenorphine at any one time. Obviously, as patients enter and leave treatment, more than 30 patients will be cared for by a particular physician over the course of time. However, if you notice an extraordinary number of new prescriptions from a single physician, you may wish to check with the prescriber to determine whether the prescriptions might be fraudulent.
Where can I get more information on treating opioid addiction with buprenorphine HCl sublingual tablets?
- Refer to the package insert for full information on the adverse events seen during the clinical trials using buprenorphine for opiate addiction treatment.
- Clinical guidelines for buprenorphine treatment and general information on the treatment of addiction is available through numerous sources such as the following: Substance Abuse and Mental Health Services (SAMHSA) Center for Substance Abuse Treatment (CSAT) Web site at www.dpt.samhsa.gov American Society of Addiction Medicine Web site at www.asam.org/ and the American Academy of Addiction Psychiatry website at www.aaap.org/
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
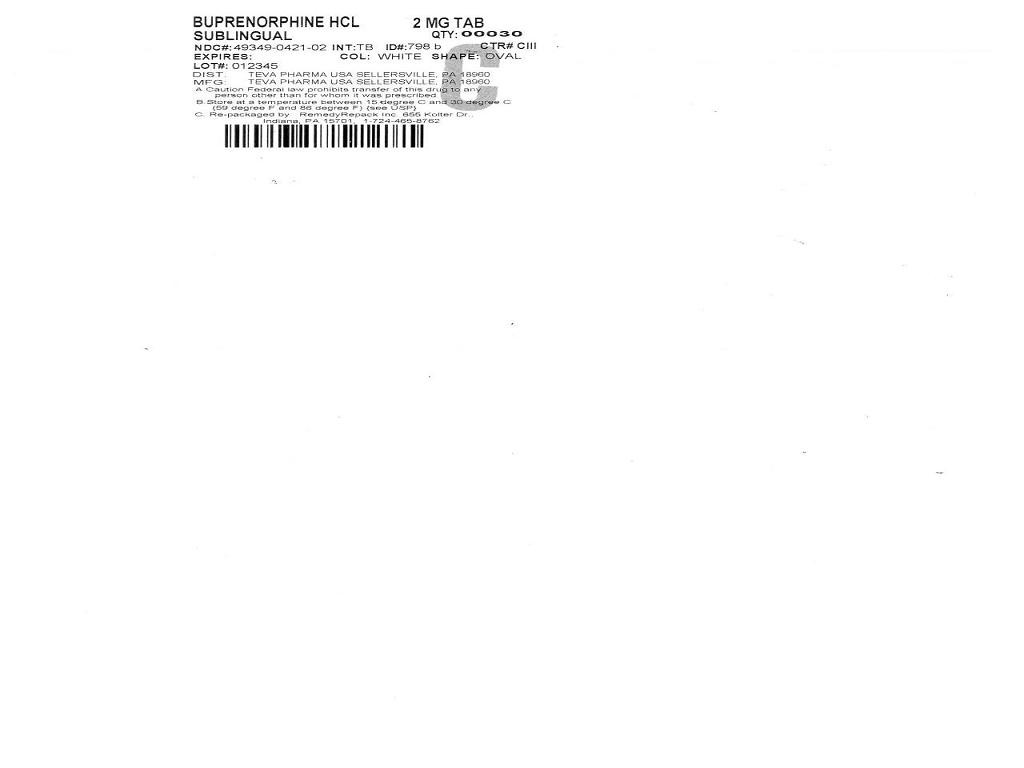

BUPRENORPHINE HYDROCHLORIDEBUPRENORPHINE HYDROCHLORIDE TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||