CEFACLOR
PD-Rx Pharmaceuticals, Inc.
PD-Rx Pharmaceuticals, Inc.
CEFACLOR CAPSULES, USP Rx only
FULL PRESCRIBING INFORMATION: CONTENTS*
- CEFACLOR DESCRIPTION
- CLINICAL PHARMACOLOGY
- CEFACLOR INDICATIONS AND USAGE
- CEFACLOR CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- CEFACLOR ADVERSE REACTIONS
- OVERDOSAGE
- CEFACLOR DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- REFERENCES
- Principal Display Panel
FULL PRESCRIBING INFORMATION
To reduce the development of drug-resistant bacteria and maintain the effectiveness of cefaclor and other antibacterial drugs, cefaclor should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
CEFACLOR DESCRIPTION
Cefaclor is a semisynthetic cephalosporin antibiotic for oral administration. It is chemically designated as 3-chloro-7-D-(2-phenylglycinamido)-3-cephem-4-carboxylic acid monohydrate. The molecular formula for cefaclor is C15H14ClN3O4S•H2O and the molecular weight is 385.82.

Each capsule contains cefaclor monohydrate equivalent to 250 mg (0.68 mmol) or 500 mg (1.36 mmol) anhydrous cefaclor. The capsules also contain black iron oxide, croscarmellose sodium, FD&C Red No. 3, FD&C Blue No. 2, gelatin, magnesium stearate, corn starch, and titanium dioxide.
The color of the capsule powder is white to off white.
CLINICAL PHARMACOLOGY
Cefaclor is well absorbed after oral administration to fasting subjects. Total absorption is the same whether the drug is given with or without food; however, when it is taken with food, the peak concentration achieved is 50% to 75% of that observed when the drug is administered to fasting subjects and generally appears from three fourths to 1 hour later. Following administration of 250- mg, 500-mg, and 1-g doses to fasting subjects, average peak serum levels of approximately 7, 13, and 23 mcg/mL respectively were obtained within 30 to 60 minutes. Approximately 60% to 85% of the drug is excreted unchanged in the urine within 8 hours, the greater portion being excreted within the first 2 hours. During this 8-hour period, peak urine concentrations following the 250-mg, 500-mg, and 1-g doses were approximately 600, 900, and 1,900 mcg/mL, respectively. The serum half-life in normal subjects is 0.6 to 0.9 hour. In patients with reduced renal function, the serum half-life of cefaclor is slightly prolonged. In those with complete absence of renal function, the plasma half-life of the intact molecule is 2.3 to 2.8 hours. Excretion pathways in patients with markedly impaired renal function have not been determined. Hemodialysis shortens the half-life by 25% to 30%.
In vitro tests demonstrate that the bactericidal action of the cephalosporins results from inhibition of cell-wall synthesis. Cefaclor has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Aerobes, Gram-positive
Staphylococci, including coagulase-positive, coagulase-negative, and penicillinase-producing strains
Streptococcus pneumoniae
Streptococcus pyogenes (group A β-hemolytic streptococci)
Aerobes, Gram-negative
Escherichia coli
Haemophilus influenzae, excluding β-lactamase-negative, ampicillin-resistant strains
Klebsiella spp.
Proteus mirabilis
The following in vitro data are available, but their clinical significance is unknown.
Cefaclor exhibits in vitro minimal inhibitory concentrations (MICs) of < 8 mcg/mL against most (> 90%) strains of the following microorganisms; however, the safety and effectiveness of cefaclor in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobes, Gram-negative
Citrobacter diversus
Moraxella (Branhamella) catarrhalis
Neisseria gonorrhoeae
Anaerobes, Gram-positive
Bacteroides spp (excluding Bacteroides fragilis)
Peptococcus
Peptostreptococcus
Propionibacterium acnes
Note: Pseudomonas spp., Acinetobacter calcoaceticus and most strains of enterococci (Enterococcus faecalis, group D streptococci), Enterobacter spp., indole-positive Proteus, Morganella morganii (formerly Proteus morganii), Provendencia rettgeri (formerly Proteus rettgeri), and Serratia spp. are resistant to cefaclor. When tested by in vitro methods, staphylococci exhibit cross-resistance between cefaclor and methicillin-type antibiotics.
Susceptibility Testing
Dilution Techniques — Quantitative methods that are used to determine minimum inhibitory concentrations (MIC) provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure that has been recommended for use with cefaclor powder uses a standardized dilution method1 (broth, agar, or microdilution). The MIC values obtained should be interpreted according to the following criteria:
| MIC (mcg/mL) | Interpretation* |
| < 8 | Susceptible (S) |
| 16 | Intermediate (I) |
| > 32 | Resistant (R) |
*When testing H. influenzae spp. these interpretive standards are applicable only to broth microdilution method using Haemophilus Test Medium (HTM)1
Note: β-lactamase-negative, ampicillin-resistant strains of H. influenzae should be considered resistant to cefaclor despite apparent in vitro susceptibility to this agent.
A report of “Susceptible” indicates that the pathogen is likely to be inhibited by usually achievable concentrations of the antimicrobial compound in blood. A report of “Intermediate” indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of “Resistant” indicates that usually achievable concentrations of the antimicrobial compound in the blood are unlikely to be inhibitory and that other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms. Standard cefaclor powder should provide the following MIC values:
| Microorganism | MIC (mcg/mL) |
| E. coli ATCC 25922 | 1 - 4 |
| E. faecalis ATCC 29212 | > 32 |
| S. aureus ATCC 29213 | 1 - 4 |
When testing H. influenzae*
| Microorganism | MIC (mcg/mL) |
| H. influenzae ATCC 49766 | 1 - 4 |
*Broth microdilution test performed using Haemophilus Test Medium (HTM)1
Diffusion Techniques— Quantitative methods that require measurement of zone diameters provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure2 that has been recommended for use with disks to test the susceptibility of microorganisms to cefaclor uses the 30 mcg cefaclor disk. Interpretation involves correlation of the diameter obtained in the disk test with the MIC for cefaclor. Reports from the laboratory providing results of the standard single-disk susceptibility test with a 30 mcg cefaclor disk should be interpreted according to the following criteria:
When Testing Organisms Other Than Haemophilus spp. and Streptococci
| Zone Diameter (mm) | Interpretation |
| > 18 | Susceptible (S) |
| 15 - 17 | Intermediate (I) |
| < 14 | Resistant (R) |
When testing H. influenzae*
| Zone Diameter (mm) | Interpretation |
| > 20 | Susceptible (S) |
| 17 - 19 | Intermediate (I) |
| < 16 | Resistant (R) |
*Disk susceptibility test performed using Haemophilus Test Medium (HTM)2
Note: β-lactamase-negative, ampicillin-resistant strains of H. influenzae should be considered resistant to cefaclor despite apparent in vitro susceptibility to this agent.
Interpretation should be as stated above for results using dilution techniques.
As with standard dilution techniques, diffusion methods require the use of laboratory control microorganisms. The 30 mcg cefaclor disk should provide the following zone diameters in these laboratory test quality control strains:
| Microorganisms | Zone Diameter (mm) |
| E. coli ATCC 25922 | 23 - 27 |
| S. aureus ATCC 25923 | 27 - 31 |
When testing H. influenzae*
| Microorganisms | Zone Diameter (mm) |
| H. influenzae ATCC 49766 | 25 - 31 |
*Disk susceptibility test performed using Haemophilus Test Medium (HTM)2
CEFACLOR INDICATIONS AND USAGE
Cefaclor is indicated in the treatment of the following infections when caused by susceptible strains of the designated microorganisms:
Otitis media caused by Streptococcus pneumoniae, Haemophilus influenzae, staphylococci, and Streptococcus pyogenes
Note: β-lactamase-negative, ampicillin-resistant (BLNAR) strains of Haemophilus influenzae should be considered resistant to cefaclor despite apparent in vitro susceptibility of some BLNAR strains.
Lower respiratory tract infections, including pneumonia caused by Streptococcus pneumoniae, Haemophilus influenzae, and Streptococcus pyogenes.
Note: β-lactamase-negative, ampicillin-resistant (BLNAR) strains of Haemophilus influenzae should be considered resistant to cefaclor despite apparent in vitro susceptibility of some BLNAR strains.
Pharyngitis and Tonsillitis, caused by Streptococcus pyogenes
Note: Penicillin is the usual drug of choice in the treatment and prevention of streptococcal infections, including the prophylaxis of rheumatic fever. Cefaclor is generally effective in the eradication of streptococci from the nasopharynx; however, substantial data establishing the efficacy of cefaclor in the subsequent prevention of rheumatic fever are not available at present.
Urinary tract infections, including pyelonephritis and cystitis, caused by Escherichia coli, Proteus mirabilis, Klebsiella spp., and coagulase-negative staphylococci
Skin and skin structure infections caused by Staphylococcus aureus and Streptococcus pyogenes
Appropriate culture and susceptibility studies should be performed to determine susceptibility of the causative organism to cefaclor.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of cefaclor and other antibacterial drugs, cefaclor should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
CEFACLOR CONTRAINDICATIONS
Cefaclor is contraindicated in patients with known allergy to the cephalosporin group of antibiotics.
WARNINGS
BEFORE THERAPY WITH CEFACLOR IS INSTITUTED, CAREFUL INQUIRY SHOULD BE MADE TO DETERMINE WHETHER THE PATIENT HAS HAD PREVIOUS HYPERSENSITIVITY REACTIONS TO CEFACLOR, CEPHALOSPORINS, PENICILLINS, OR OTHER DRUGS. IF THIS PRODUCT IS TO BE GIVEN TO PENICILLIN-SENSITIVE PATIENTS, CAUTION SHOULD BE EXERCISED BECAUSE CROSS-HYPERSENSITIVITY AMONG β-LACTAM ANTIBIOTICS HAS BEEN CLEARLY DOCUMENTED AND MAY OCCUR IN UP TO 10% OF PATIENTS WITH A HISTORY OF PENICILLIN ALLERGY.
IF AN ALLERGIC REACTION TO CEFACLOR OCCURS, DISCONTINUE THE DRUG. SERIOUS ACUTE HYPERSENSITIVITY REACTIONS MAY REQUIRE TREATMENT WITH EPINEPHRINE AND OTHER EMERGENCY MEASURES, INCLUDING OXYGEN, INTRAVENOUS FLUIDS, INTRAVENOUS ANTIHISTAMINES, CORTICOSTEROIDS, PRESSOR AMINES, AND AIRWAY MANAGEMENT, AS CLINICALLY INDICATED.
Antibiotics, including cefaclor, should be administered cautiously to any patient who has demonstrated some form of allergy, particularly to drugs.
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including cefaclor, and has ranged in severity from mild to life-threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents.
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowthof clostridia. Studies indicate that a toxin produced by Clostridium difficile is one primary cause of antibiotic-associated colitis.
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to drug discontinuation alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation and treatment with an antibacterial drug effective against C. difficile.
PRECAUTIONS
General
Prescribing cefaclor in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Prolonged use of cefaclor may result in the overgrowth of nonsusceptible organisms. Careful observation of the patient is essential. If superinfection occurs during therapy, appropriate measures should be taken.
Positive direct Coombs’ tests have been reported during treatment with the cephalosporin antibiotics. It should be recognized that a positive Coombs’ test may be due to the drug, e.g., in hematologic studies or in transfusion cross-matching procedures when antiglobulin tests are performed on the minor side or in Coombs’ testing of newborns whose mothers have received cephalosporin antibiotics before parturition.
Cefaclor should be administered with caution in the presence of markedly impaired renal function. Since the half-life of cefaclor in anuria is 2.3 to 2.8 hours, dosage adjustments for patients with moderate or severe renal impairment are usually not required. Clinical experience with cefaclor under such conditions is limited; therefore, careful clinical observation and laboratory studies should be made.
As with other β-lactam antibiotics, the renal excretion of cefaclor is inhibited by probenecid. Antibiotics, including cephalosporins, should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
Information for Patients
Patients should be counseled that antibacterial drugs including cefaclor should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When cefaclor is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by cefaclor or other antibacterial drugs in the future.
Drug /Laboratory Test Interactions
Patients receiving cefaclor may show a false-positive reaction for glucose in the urine with tests that use Benedict’s and Fehling’s solutions and also with Clinitest® tablets.
There have been reports of increased anticoagulant effect when cefaclor and oral anticoagulants were administered concomitantly.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies have not been performed to determine potential for carcinogenicity, mutagenicity, or impairment of fertility.
Pregnancy–Teratogenic Effects–Pregnancy Category B
Reproduction studies have been performed in mice and rats at doses up to 12 times the human dose and in ferrets given 3 times the maximum human dose and have revealed no harm to the fetus due to cefaclor. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Labor and Delivery
The effect of cefaclor on labor and delivery is unknown.
Nursing Mothers
Small amounts of cefaclor have been detected in mother’s milk following administration of single 500 mg doses. Average levels were 0.18, 0.20, 0.21, and 0.16 mcg/mL at 2, 3, 4, and 5 hours respectively. Trace amounts were detected at 1 hour. The effect on nursing infants is not known. Caution should be exercised when cefaclor is administered to a nursing woman.
Pediatric Use
Safety and effectiveness of this product for use in infants less than 1 month of age have not been established.
Geriatric Use
Of the 3703 patients in clinical studies of cefaclor, 594 (16.0%) were 65 and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
This drug is known to be substantially excreted by the kidney (see CLINICAL PHARMACOLOGY ), and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function (see DOSAGE AND ADMINISTRATION ).
CEFACLOR ADVERSE REACTIONS
Adverse effects considered to be related to therapy with cefaclor are listed below:
Hypersensitivity reactions have been reported in about 1.5% of patients and include morbilliform eruptions (1 in 100). Pruritus, urticaria, and positive Coombs’ tests each occur in less than 1 in 200 patients.
Cases of serum-sickness-like reactions have been reported with the use of cefaclor. These are characterized by findings of erythema multiforme, rashes, and other skin manifestations accompanied by arthritis/arthralgia, with or without fever, and differ from classic serum sickness in that there is infrequently associated lymphadenopathy and proteinuria, no circulating immune complexes, and no evidence to date of sequelae of the reaction. Occasionally, solitary symptoms may occur, but do not represent a serum-sickness-like reaction. While further investigation is ongoing, serum-sickness-like reactions appear to be due to hypersensitivity and more often occur during or following a second (or subsequent) course of therapy with cefaclor. Such reactions have been reported more frequently in pediatric ptients than in adults with an overall occurrence ranging from 1 in 200 (0.5%) in one focused trial to 2 in 8,346 (0.024%) in overall clinical trials (with an incidence in pediatric patients in clinical trials of 0.055%) to 1 in 38,000 (0.003%) in spontaneous event reports. Signs and symptoms usually occur a few days after initiation of therapy and subside within a few days after cessation of therapy; occasionally these reactions have resulted in hospitalization, usually of short duration (median hospitalization = 2 to 3 days, based on postmarketing surveillance studies). In those requiring hospitalization, the symptoms have ranged from mild to severe at the time of admission with more of the severe reactions occurring in pediatric patients. Antihistamines and glucocorticoids appear to enhance resolution of the signs and symptoms. No serious sequelae have been reported.
More severe hypersensitivity reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and anaphylaxis have been reported rarely. Anaphylactoid events may be manifested by solitary symptoms, including angioedema, asthenia, edema (including face and limbs), dyspnea, paresthesias, syncope, hypotension, or vasodilatation. Anaphylaxis may be more common in patients with a history of penicillin allergy.
Rarely, hypersensitivity symptoms may persist for several months.
Gastrointestinal symptoms occur in about 2.5% of patients and include diarrhea (1 in 70).
Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS ). Nausea and vomiting have been reported rarely. As with some penicillins and some other cephalosporins, transient hepatitis and cholestatic jaundice have been reported rarely.
Other effects considered related to therapy included eosinophilia (1 in 50 patients), genital pruritus , moniliasis or vaginitis (about 1 in 50 patients), and, rarely, thrombocytopenia or reversible interstitial nephritis.
Causal Relationship Uncertain–
CNS–Rarely, reversible hyperactivity, agitation, nervousness, insomnia, confusion, hypertonia, dizziness, hallucinations, and somnolence have been reported.
Transitory abnormalities in clinical laboratory test results have been reported. Although they were of uncertain etiology, they are listed below to serve as alerting information for the physician.
Hepatic–Slight elevations of AST, ALT, or alkaline phosphatase values (1 in 40).
Hematopoietic–As has also been reported with other β-lactam antibiotics, transient lymphocytosis, leukopenia, and, rarely, hemolytic anemia, aplastic anemia, agranulocytosis, and reversible neutropenia of possible clinical significance.
There have been rare reports of increased prothrombin time with or without clinical bleeding in patients receiving cefaclor and warfarin concomitantly.
Renal– Slight elevations in BUN or serum creatinine (less than 1 in 500) or abnormal urinalysis (less than 1 in 200).
Cephalosporin-class Side Effects
In addition to the adverse reactions listed above that have been observed in patients treated with cefaclor, the following adverse reactions and altered laboratory tests have been reported for cephalosporin-class antibiotics: fever, abdominal pain, superinfection, renal dysfunction, toxic nephropathy, hemorrhage, false positive test for urinary glucose, elevated bilirubin, elevated LDH, and pancytopenia.
Several cephalosporins have been implicated in triggering seizures, particularly in patients with renal impairment when the dosage was not reduced. If seizures associated with drug therapy occur, the drug should be discontinued. Anticonvulsant therapy can be given if clinically indicated (see DOSAGE AND ADMINISTRATION and OVERDOSAGE sections).
OVERDOSAGE
Signs and Symptoms –The toxic symptoms following an overdose of cefaclor may include nausea, vomiting, epigastric distress, and diarrhea. The severity of the epigastric distress and the diarrhea are dose related. If other symptoms are present, it is probable that they are secondary to an underlying disease state, an allergic reaction, or the effects of other intoxication.
Treatment–To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison Control Center. Telephone numbers of certified poison control centers are listed in the Physicians’ Desk Reference (PDR). In managing overdosage, consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug kinetics in your patient.
Unless 5 times the normal dose of cefaclor has been ingested, gastrointestinal decontamination will not be necessary.
Protect the patient’s airway and support ventilation and perfusion. Meticulously monitor and maintain, within acceptable limits, the patient’s vital signs, blood gases, serum electrolytes, etc. Absorption of drugs from the gastrointestinal tract may be decreased by giving activated charcoal, which, in many cases, is more effective than emesis or lavage; consider charcoal instead of or in addition to gastric emptying. Repeated doses of charcoal over time may hasten elimination of some drugs that have been absorbed. Safeguard the patient’s airway when employing gastric emptying or charcoal.
Forced diuresis, peritoneal dialysis, hemodialysis, or charcoal hemoperfusion have not been established as beneficial for an overdose of cefaclor.
CEFACLOR DOSAGE AND ADMINISTRATION
Cefaclor is administered orally.
Adults –The usual adult dosage is 250 mg every 8 hours. For more severe infections (such as pneumonia) or those caused by less susceptible organisms, doses may be doubled.
Pediatric patients–The usual recommended daily dosage for pediatric patients is 20 mg/kg/day in divided doses every 8 hours. In more serious infections, otitis media, and infections caused by less susceptible organisms, 40 mg/kg/day are recommended, with a maximum dosage of 1 g/day.
Cefaclor may be administered in the presence of impaired renal function. Under such a condition, the dosage usually is unchanged (see PRECAUTIONS ).
In the treatment of β-hemolytic streptococcal infections, a therapeutic dosage of cefaclor should be administered for at least 10 days.
HOW SUPPLIED
Capsules:
Cefaclor Capsules, USP 250 mg: opaque purple and white hard gelatin capsules imprinted with "West Ward 985" in bottles of 15 and bottles of 100.
Cefaclor Capsules, USP 500 mg: opaque purple and gray hard gelatin capsules imprinted with "West Ward 986" in bottles of 15 and bottles of 100.
Store bottles at 20° to 25°C (68° to 77° F). [See USP Controlled Room Temperature]
REFERENCES
1. National Committee for Clinical Laboratory Standards. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically - Fourth Edition. Approved Standard NCCLS Document M7-A4, Vol. 17, No. 2, NCCLS, Wayne, PA, January 1997.
2. National Committee for Clinical Laboratory Standards. Performance Standards for Antimicrobial Disk Susceptibility Test - Sixth Edition, Approved Standard NCCLS Document M2-A6, Vol. 17, No. 1, NCCLS, Wayne, PA, January 1997.
West-ward Pharmaceutical Corp.
Eatontown, NJ 07724 - USA
Distributor
Manufactured by:
Jazeera Pharmaceutical Industries (JPI)
Al- Kharj Road
P.O. Box 106229
Riyadh 11666
Saudi Arabia
An Affiliate of:
Hikma Pharmaceuticals
P.O. Box 182400
Amman 11118
Jordan
Rev.: July 2006
Principal Display Panel
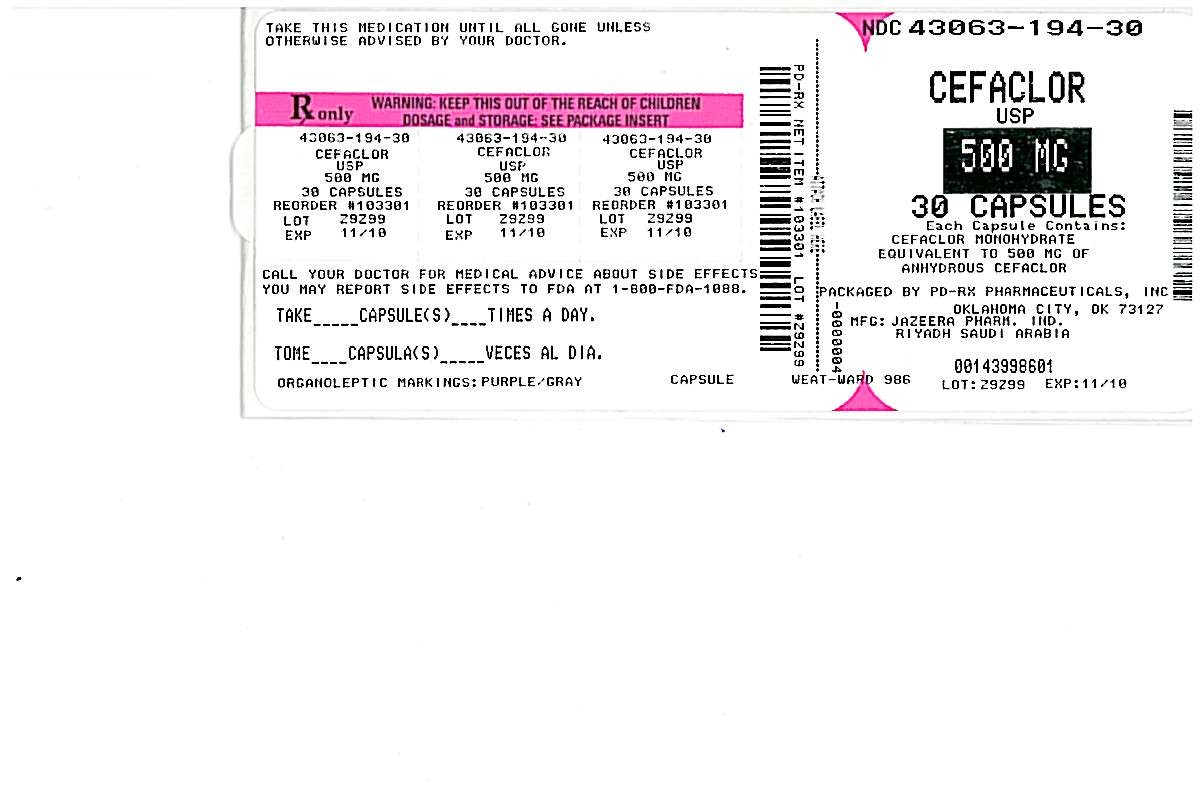
CEFACLORCEFACLOR CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||