Cubicin
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use CUBICIN safely and effectively. See full prescribing information for CUBICIN. CUBICIN (daptomycin for injection) for Intravenous UseInitial U.S. Approval: 2003MicrobiologyTo reduce the development of drug-resistant bacteria and maintain the effectiveness of CUBICIN and other antibacterial drugs, CUBICIN should be used to treat infections that are proven or strongly suspected to be caused by bacteria.INDICATIONS AND USAGECUBICIN is a lipopeptide antibacterial indicated for the treatment of: Complicated skin and skin structure infections (cSSSI) (1.1) Staphylococcus aureus bloodstream infections (bacteremia), including those with right-sided infective endocarditis (1.2) CUBICIN is not indicated for the treatment of pneumonia. (1.3)DOSAGE AND ADMINISTRATION Recommended dosage regimen for adult patients (2.2, 2.3, 2.4): Creatinine Clearance(CLCR) Dosage Regimen cSSSI For 7 to 14 days S. aureus Bacteremia For 2 to 6 weeks ≥30 mL/min 4 mg/kg once every 24 hours 6 mg/kg once every 24 hours
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 CUBICIN INDICATIONS AND USAGE
- 2 CUBICIN DOSAGE AND ADMINISTRATION
- 2.1 Administration Duration
- 2.2 Complicated Skin and Skin Structure Infections
- 2.3 Bloodstream Infections (Bacteremia), Including Those with Right-Sided Infective Endocarditis, Caused by Methicillin-Susceptible and Methicillin-Resistant Isolates
- 2.4 Patients with Renal Impairment
- 2.5 Preparation of CUBICIN for Administration
- 2.6 Compatible Intravenous Solutions
- 2.7 Incompatibilities
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CUBICIN CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Anaphylaxis/Hypersensitivity Reactions
- 5.2 Myopathy and Rhabdomyolysis
- 5.3 Eosinophilic Pneumonia
- 5.4 Peripheral Neuropathy
- 5.5 –Associated Diarrhea
- 5.6 Persisting or Relapsing Bacteremia/Endocarditis
- 5.7 Decreased Efficacy in Patients with Moderate Baseline Renal Impairment
- 5.8 Drug-Laboratory Test Interactions
- 5.9 Non-Susceptible Microorganisms
- 6 CUBICIN ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 CUBICIN DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL TRIALS
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
CUBICIN® (daptomycin for injection)
1 INDICATIONS AND USAGE
CUBICIN is indicated for the treatment of the infections listed below.
1.1 Complicated Skin and Skin Structure Infections
Complicated skin and skin structure infections (cSSSI) caused by susceptible isolates of the following Gram-positive bacteria: Staphylococcus aureus (including methicillin-resistant isolates), Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus dysgalactiae subsp. equisimilis, and Enterococcus faecalis (vancomycin-susceptible isolates only).
1.2 Bloodstream Infections (Bacteremia), Including Those with Right-Sided Infective Endocarditis, Caused by Methicillin-Susceptible and Methicillin-Resistant Isolates
Staphylococcus aureus bloodstream infections (bacteremia), including those with right-sided infective endocarditis, caused by methicillin-susceptible and methicillin-resistant isolates.
1.3 Limitations of Use
CUBICIN is not indicated for the treatment of pneumonia.
CUBICIN is not indicated for the treatment of left-sided infective endocarditis due to S. aureus. The clinical trial of CUBICIN in patients with S. aureus bloodstream infections included limited data from patients with left-sided infective endocarditis; outcomes in these patients were poor [see Clinical Trials (14.2) ]. CUBICIN has not been studied in patients with prosthetic valve endocarditis.
1.4 Usage
Appropriate specimens for microbiological examination should be obtained in order to isolate and identify the causative pathogens and to determine their susceptibility to daptomycin.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of CUBICIN and other antibacterial drugs, CUBICIN should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria.
When culture and susceptibility information is available, it should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy. Empiric therapy may be initiated while awaiting test results.
2 DOSAGE AND ADMINISTRATION
2.1 Administration Duration
CUBICIN should be administered intravenously either by injection over a two (2) minute period or by infusion over a thirty (30) minute period.
2.2 Complicated Skin and Skin Structure Infections
CUBICIN 4 mg/kg should be administered intravenously in 0.9% sodium chloride injection once every 24 hours for 7 to 14 days.
2.3 Bloodstream Infections (Bacteremia), Including Those with Right-Sided Infective Endocarditis, Caused by Methicillin-Susceptible and Methicillin-Resistant Isolates
CUBICIN 6 mg/kg should be administered intravenously in 0.9% sodium chloride injection once every 24 hours for 2 to 6 weeks. There are limited safety data for the use of CUBICIN for more than 28 days of therapy. In the Phase 3 trial, there were a total of 14 patients who were treated with CUBICIN for more than 28 days.
2.4 Patients with Renal Impairment
The recommended dosage regimen for patients with creatinine clearance (CLCR) <30 mL/min, including patients on hemodialysis or continuous ambulatory peritoneal dialysis (CAPD), is 4 mg/kg (cSSSI) or 6 mg/kg (S. aureus bloodstream infections) once every 48 hours (Table 1). When possible, CUBICIN should be administered following the completion of hemodialysis on hemodialysis days [see Warnings and Precautions (5.2, 5.7), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3) ].
| Creatinine Clearance (CLCR) |
Dosage Regimen | |
|---|---|---|
| cSSSI | S. aureus Bloodstream Infections | |
| ≥30 mL/min | 4 mg/kg once every 24 hours | 6 mg/kg once every 24 hours |
| <30 mL/min, including hemodialysis and CAPD | 4 mg/kg once every 48 hours |
6 mg/kg once every 48 hours |
2.5 Preparation of CUBICIN for Administration
CUBICIN is supplied in single-use vials, each containing 500 mg daptomycin as a sterile, lyophilized powder. The contents of a CUBICIN vial should be reconstituted, using aseptic technique, to 50 mg/mL as follows:
-
- Remove the polypropylene flip-off cap from the CUBICIN vial to expose the central portion of the rubber stopper.
- Slowly transfer 10 mL of 0.9% sodium chloride injection through the center of the rubber stopper into the CUBICIN vial, pointing the transfer needle toward the wall of the vial.
- Ensure that all of the CUBICIN powder is wetted by gently rotating the vial.
- Allow the wetted product to stand undisturbed for 10 minutes.
- Gently rotate or swirl the vial contents for a few minutes, as needed, to obtain a completely reconstituted solution.
For intravenous (IV) injection over a period of 2 minutes, administer the appropriate volume of the reconstituted CUBICIN (concentration of 50 mg/mL).
For IV infusion over a period of 30 minutes, the appropriate volume of the reconstituted CUBICIN (concentration of 50 mg/mL) should be further diluted, using aseptic technique, into a 50 mL IV infusion bag containing 0.9% sodium chloride injection.
Parenteral drug products should be inspected visually for particulate matter prior to administration.
No preservative or bacteriostatic agent is present in this product. Aseptic technique must be used in the preparation of final IV solution. Stability studies have shown that the reconstituted solution is stable in the vial for 12 hours at room temperature and up to 48 hours if stored under refrigeration at 2 to 8°C (36 to 46°F).
The diluted solution is stable in the infusion bag for 12 hours at room temperature and 48 hours if stored under refrigeration. The combined storage time (reconstituted solution in vial and diluted solution in infusion bag) should not exceed 12 hours at room temperature or 48 hours under refrigeration.
CUBICIN vials are for single use only.
2.6 Compatible Intravenous Solutions
CUBICIN is compatible with 0.9% sodium chloride injection and lactated Ringer's injection.
2.7 Incompatibilities
CUBICIN is not compatible with dextrose-containing diluents.
CUBICIN should not be used in conjunction with ReadyMED® elastomeric infusion pumps (Cardinal Health, Inc.). Stability studies of CUBICIN solutions stored in ReadyMED® elastomeric infusion pumps identified an impurity (2-mercaptobenzothiazole) leaching from this pump system into the CUBICIN solution.
Because only limited data are available on the compatibility of CUBICIN with other IV substances, additives and other medications should not be added to CUBICIN single-use vials or infusion bags, or infused simultaneously with CUBICIN through the same IV line. If the same IV line is used for sequential infusion of different drugs, the line should be flushed with a compatible intravenous solution before and after infusion with CUBICIN.
3 DOSAGE FORMS AND STRENGTHS
500 mg daptomycin as a sterile, pale yellow to light brown lyophilized powder for reconstitution in a single-use vial.
4 CONTRAINDICATIONS
CUBICIN is contraindicated in patients with known hypersensitivity to daptomycin.
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylaxis/Hypersensitivity Reactions
Anaphylaxis/hypersensitivity reactions have been reported with the use of antibacterial agents, including CUBICIN, and may be life-threatening. If an allergic reaction to CUBICIN occurs, discontinue the drug and institute appropriate therapy [see Adverse Reactions (6.2) ].
5.2 Myopathy and Rhabdomyolysis
Myopathy, defined as muscle aching or muscle weakness in conjunction with increases in creatine phosphokinase (CPK) values to greater than 10 times the upper limit of normal (ULN), has been reported with the use of CUBICIN. Rhabdomyolysis, with or without acute renal failure, has been reported [see Adverse Reactions (6.2) ].
Patients receiving CUBICIN should be monitored for the development of muscle pain or weakness, particularly of the distal extremities. In patients who receive CUBICIN, CPK levels should be monitored weekly, and more frequently in patients who received recent prior or concomitant therapy with an HMG-CoA reductase inhibitor or in whom elevations in CPK occur during treatment with CUBICIN.
In patients with renal impairment, both renal function and CPK should be monitored more frequently than once weekly [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3) ].
In Phase 1 studies and Phase 2 clinical trials, CPK elevations appeared to be more frequent when CUBICIN was dosed more than once daily. Therefore, CUBICIN should not be dosed more frequently than once a day.
CUBICIN should be discontinued in patients with unexplained signs and symptoms of myopathy in conjunction with CPK elevations to levels >1,000 U/L (~5× ULN), and in patients without reported symptoms who have marked elevations in CPK, with levels >2,000 U/L (≥10× ULN). In addition, consideration should be given to suspending agents associated with rhabdomyolysis, such as HMG-CoA reductase inhibitors, temporarily in patients receiving CUBICIN [see Drug Interactions (7.1) ].
5.3 Eosinophilic Pneumonia
Eosinophilic pneumonia has been reported in patients receiving CUBICIN [see Adverse Reactions (6.2) ]. In reported cases associated with CUBICIN, patients developed fever, dyspnea with hypoxic respiratory insufficiency, and diffuse pulmonary infiltrates. In general, patients developed eosinophilic pneumonia 2 to 4 weeks after starting CUBICIN and improved when CUBICIN was discontinued and steroid therapy was initiated. Recurrence of eosinophilic pneumonia upon re-exposure has been reported. Patients who develop these signs and symptoms while receiving CUBICIN should undergo prompt medical evaluation, and CUBICIN should be discontinued immediately. Treatment with systemic steroids is recommended.
5.4 Peripheral Neuropathy
Cases of peripheral neuropathy have been reported during the CUBICIN postmarketing experience [see Adverse Reactions (6.2) ]. Therefore, physicians should be alert to signs and symptoms of peripheral neuropathy in patients receiving CUBICIN.
5.5 –Associated Diarrhea
Clostridium difficile–associated diarrhea (CDAD) has been reported with the use of nearly all systemic antibacterial agents, including CUBICIN, and may range in severity from mild diarrhea to fatal colitis [see Adverse Reactions (6.2) ]. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile.
C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, since these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary because CDAD has been reported to occur more than 2 months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.6 Persisting or Relapsing Bacteremia/Endocarditis
Patients with persisting or relapsing S. aureus bacteremia/endocarditis or poor clinical response should have repeat blood cultures. If a blood culture is positive for S. aureus, minimum inhibitory concentration (MIC) susceptibility testing of the isolate should be performed using a standardized procedure, and diagnostic evaluation of the patient should be performed to rule out sequestered foci of infection. Appropriate surgical intervention (e.g., debridement, removal of prosthetic devices, valve replacement surgery) and/or consideration of a change in antibacterial regimen may be required.
Failure of treatment due to persisting or relapsing S. aureus bacteremia/endocarditis may be due to reduced daptomycin susceptibility (as evidenced by increasing MIC of the S. aureus isolate) [see Clinical Trials (14.2) ].
5.7 Decreased Efficacy in Patients with Moderate Baseline Renal Impairment
Limited data are available from the two Phase 3 complicated skin and skin structure infection (cSSSI) trials regarding clinical efficacy of CUBICIN treatment in patients with creatinine clearance (CLCR) <50 mL/min; only 31/534 (6%) patients treated with CUBICIN in the intent-to-treat (ITT) population had a baseline CLCR <50 mL/min. Table 2 shows the number of patients by renal function and treatment group who were clinical successes in the Phase 3 cSSSI trials.
| CLCR | Success Rate n/N (%) |
|
|---|---|---|
| CUBICIN 4 mg/kg q24h |
Comparator | |
| 50–70 mL/min | 25/38 (66%) | 30/48 (63%) |
| 30–<50 mL/min | 7/15 (47%) | 20/35 (57%) |
In a subgroup analysis of the ITT population in the Phase 3 S. aureus bacteremia/endocarditis trial, clinical success rates, as determined by a treatment-blinded Adjudication Committee [see Clinical Trials (14.2) ], in the CUBICIN-treated patients were lower in patients with baseline CLCR <50 mL/min (see Table 3). A decrease of the magnitude shown in Table 3 was not observed in comparator-treated patients.
| Baseline CLCR | Success Rate n/N (%) |
|||
|---|---|---|---|---|
| CUBICIN 6 mg/kg q24h |
Comparator | |||
| Bacteremia | Right-Sided Infective Endocarditis |
Bacteremia | Right-Sided Infective Endocarditis |
|
| >80 mL/min | 30/50 (60%) | 7/14 (50%) | 19/42 (45%) | 5/11 (46%) |
| 50–80 mL/min | 12/26 (46%) | 1/4 (25%) | 13/31 (42%) | 1/2 (50%) |
| 30–<50 mL/min | 2/14 (14%) | 0/1 (0%) | 7/17 (41%) | 1/1 (100%) |
Consider these data when selecting antibacterial therapy for use in patients with baseline moderate to severe renal impairment.
5.8 Drug-Laboratory Test Interactions
Clinically relevant plasma concentrations of daptomycin have been observed to cause a significant concentration-dependent false prolongation of prothrombin time (PT) and elevation of International Normalized Ratio (INR) when certain recombinant thromboplastin reagents are utilized for the assay [see Drug-Laboratory Interactions (7.2) ].
5.9 Non-Susceptible Microorganisms
The use of antibacterials may promote the overgrowth of non-susceptible microorganisms. If superinfection occurs during therapy, appropriate measures should be taken.
Prescribing CUBICIN in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
6 ADVERSE REACTIONS
The following adverse reactions are described, or described in greater detail, in other sections:
-
- Anaphylaxis/hypersensitivity reactions [see Warnings and Precautions (5.1) ] -
- Myopathy and rhabdomyolysis [see Warnings and Precautions (5.2) ] -
- Eosinophilic pneumonia [see Warnings and Precautions (5.3) ] -
- Peripheral neuropathy [see Warnings and Precautions (5.4) ] -
- Increased International Normalized Ratio (INR)/prolonged prothrombin time [see Warnings and Precautions (5.8) and Drug-Laboratory Test Interactions (7.2) ]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1 Clinical Trials Experience
Clinical trials enrolled 1,864 patients treated with CUBICIN and 1,416 treated with comparator.
Complicated Skin and Skin Structure Infection Trials
In Phase 3 complicated skin and skin structure infection (cSSSI) trials, CUBICIN was discontinued in 15/534 (2.8%) patients due to an adverse reaction, while comparator was discontinued in 17/558 (3.0%) patients.
The rates of the most common adverse reactions, organized by body system, observed in cSSSI (4 mg/kg CUBICIN) patients are displayed in Table 4.
| Adverse Reaction | Patients (%) | |
|---|---|---|
| CUBICIN 4 mg/kg (N=534) |
Comparator (N=558) |
|
| Gastrointestinal disorders | ||
| Diarrhea | 5.2 | 4.3 |
| Nervous system disorders | ||
| Headache | 5.4 | 5.4 |
| Dizziness | 2.2 | 2.0 |
| Skin/subcutaneous disorders | ||
| Rash | 4.3 | 3.8 |
| Diagnostic investigations | ||
| Abnormal liver function tests | 3.0 | 1.6 |
| Elevated CPK | 2.8 | 1.8 |
| Infections | ||
| Urinary tract infections | 2.4 | 0.5 |
| Vascular disorders | ||
| Hypotension | 2.4 | 1.4 |
| Respiratory disorders | ||
| Dyspnea | 2.1 | 1.6 |
Drug-related adverse reactions (possibly or probably drug-related) that occurred in <1% of patients receiving CUBICIN in the cSSSI trials are as follows:
Body as a Whole: fatigue, weakness, rigors, flushing, hypersensitivity
Blood/Lymphatic System: leukocytosis, thrombocytopenia, thrombocytosis, eosinophilia, increased International Normalized Ratio (INR)
Cardiovascular System: supraventricular arrhythmia
Dermatologic System: eczema
Digestive System: abdominal distension, stomatitis, jaundice, increased serum lactate dehydrogenase
Metabolic/Nutritional System: hypomagnesemia, increased serum bicarbonate, electrolyte disturbance
Musculoskeletal System: myalgia, muscle cramps, muscle weakness, arthralgia
Nervous System: vertigo, mental status change, paresthesia
Special Senses: taste disturbance, eye irritation
S. aureus Bacteremia/Endocarditis Trial
In the S. aureus bacteremia/endocarditis trial, CUBICIN was discontinued in 20/120 (16.7%) patients due to an adverse reaction, while comparator was discontinued in 21/116 (18.1%) patients.
Serious Gram-negative infections (including bloodstream infections) were reported in 10/120 (8.3%) CUBICIN-treated patients and 0/115 comparator-treated patients. Comparator-treated patients received dual therapy that included initial gentamicin for 4 days. Infections were reported during treatment and during early and late follow-up. Gram-negative infections included cholangitis, alcoholic pancreatitis, sternal osteomyelitis/mediastinitis, bowel infarction, recurrent Crohn's disease, recurrent line sepsis, and recurrent urosepsis caused by a number of different Gram-negative bacteria.
The rates of the most common adverse reactions, organized by System Organ Class (SOC), observed in S. aureus bacteremia/endocarditis (6 mg/kg CUBICIN) patients are displayed in Table 5.
| Adverse Reaction |
Patients n (%) |
|
|---|---|---|
| CUBICIN 6 mg/kg (N=120) |
Comparator (N=116) |
|
| Infections and infestations | ||
| Sepsis NOS | 6 (5%) | 3 (3%) |
| Bacteremia | 6 (5%) | 0 (0%) |
| Gastrointestinal disorders | ||
| Abdominal pain NOS | 7 (6%) | 4 (3%) |
| General disorders and administration site conditions | ||
| Chest pain | 8 (7%) | 7 (6%) |
| Edema NOS | 8 (7%) | 5 (4%) |
| Respiratory, thoracic and mediastinal disorders | ||
| Pharyngolaryngeal pain | 10 (8%) | 2 (2%) |
| Skin and subcutaneous tissue disorders | ||
| Pruritus | 7 (6%) | 6 (5%) |
| Sweating increased | 6 (5%) | 0 (0%) |
| Psychiatric disorders | ||
| Insomnia | 11 (9%) | 8 (7%) |
| Investigations | ||
| Blood creatine phosphokinase increased | 8 (7%) | 1 (1%) |
| Vascular disorders | ||
| Hypertension NOS | 7 (6%) | 3 (3%) |
The following reactions, not included above, were reported as possibly or probably drug-related in the CUBICIN-treated group:
Blood and Lymphatic System Disorders: eosinophilia, lymphadenopathy, thrombocythemia, thrombocytopenia
Cardiac Disorders: atrial fibrillation, atrial flutter, cardiac arrest
Ear and Labyrinth Disorders: tinnitus
Eye Disorders: vision blurred
Gastrointestinal Disorders: dry mouth, epigastric discomfort, gingival pain, hypoesthesia oral
Infections and Infestations: candidal infection NOS, vaginal candidiasis, fungemia, oral candidiasis, urinary tract infection fungal
Investigations: blood phosphorous increased, blood alkaline phosphatase increased, INR increased, liver function test abnormal, alanine aminotransferase increased, aspartate aminotransferase increased, prothrombin time prolonged
Metabolism and Nutrition Disorders: appetite decreased NOS
Musculoskeletal and Connective Tissue Disorders: myalgia
Nervous System Disorders: dyskinesia, paresthesia
Psychiatric Disorders: hallucination NOS
Renal and Urinary Disorders: proteinuria, renal impairment NOS
Skin and Subcutaneous Tissue Disorders: pruritus generalized, rash vesicular
Other Trials
In Phase 3 trials of community-acquired pneumonia (CAP), the death rate and rates of serious cardiorespiratory adverse events were higher in CUBICIN-treated patients than in comparator-treated patients. These differences were due to lack of therapeutic effectiveness of CUBICIN in the treatment of CAP in patients experiencing these adverse events [see Indications and Usage (1.3) ].
Laboratory Changes
Complicated Skin and Skin Structure Infection Trials
In Phase 3 cSSSI trials of CUBICIN at a dose of 4 mg/kg, elevations in CPK were reported as clinical adverse events in 15/534 (2.8%) CUBICIN-treated patients, compared with 10/558 (1.8%) comparator-treated patients. Of the 534 patients treated with CUBICIN, 1 (0.2%) had symptoms of muscle pain or weakness associated with CPK elevations to greater than 4 times the upper limit of normal (ULN). The symptoms resolved within 3 days and CPK returned to normal within 7 to 10 days after treatment was discontinued [see Warnings and Precautions (5.2) ]. Table 6 summarizes the CPK shifts from Baseline through End of Therapy in the cSSSI trials.
| Change in CPK | All Patients | Patients with Normal CPK at Baseline |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| CUBICIN 4 mg/kg (N=430) |
Comparator (N=459) |
CUBICIN 4 mg/kg (N=374) |
Comparator (N=392) |
||||||
| % | n | % | n | % | n | % | n | ||
| Note: Elevations in CPK observed in patients treated with CUBICIN or comparator were not clinically or statistically significantly different. | |||||||||
| No Increase | 90.7 | 390 | 91.1 | 418 | 91.2 | 341 | 91.1 | 357 | |
| Maximum Value | >1× ULN |
9.3 | 40 | 8.9 | 41 | 8.8 | 33 | 8.9 | 35 |
| >2× ULN | 4.9 | 21 | 4.8 | 22 | 3.7 | 14 | 3.1 | 12 | |
| >4× ULN | 1.4 | 6 | 1.5 | 7 | 1.1 | 4 | 1.0 | 4 | |
| >5× ULN | 1.4 | 6 | 0.4 | 2 | 1.1 | 4 | 0.0 | 0 | |
| >10× ULN | 0.5 | 2 | 0.2 | 1 | 0.2 | 1 | 0.0 | 0 | |
S. aureus Bacteremia/Endocarditis Trial
In the S. aureus bacteremia/endocarditis trial, at a dose of 6 mg/kg, 11/120 (9.2%) CUBICIN-treated patients, including two patients with baseline CPK levels >500 U/L, had CPK elevations to levels >500 U/L, compared with 1/116 (0.9%) comparator-treated patients. Of the 11 CUBICIN-treated patients, 4 had prior or concomitant treatment with an HMG-CoA reductase inhibitor. Three of these 11 CUBICIN-treated patients discontinued therapy due to CPK elevation, while the one comparator-treated patient did not discontinue therapy [see Warnings and Precautions (5.2) ].
6.2 Post-Marketing Experience
The following adverse reactions have been identified during postapproval use of CUBICIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency reliably or establish a causal relationship to drug exposure.
Immune System Disorders: anaphylaxis; hypersensitivity reactions, including angioedema, drug rash with eosinophilia and systemic symptoms (DRESS), pruritus, hives, shortness of breath, difficulty swallowing, truncal erythema, and pulmonary eosinophilia [see Contraindications (4), Warnings and Precautions (5.1) ]
Infections and Infestations: Clostridium difficile–associated diarrhea [see Warnings and Precautions (5.5) ]
Musculoskeletal Disorders: myoglobin increased; rhabdomyolysis (some reports involved patients treated concurrently with CUBICIN and HMG-CoA reductase inhibitors) [see Warnings and Precautions (5.2), Drug Interactions (7.1), and Clinical Pharmacology (12.3) ]
Respiratory, Thoracic, and Mediastinal Disorders: cough, eosinophilic pneumonia [see Warnings and Precautions (5.3) ]
Nervous System Disorders: peripheral neuropathy [see Warnings and Precautions (5.4) ]
Skin and Subcutaneous Tissue Disorders: serious skin reactions, including Stevens-Johnson syndrome and vesiculobullous rash (with or without mucous membrane involvement)
Gastrointestinal Disorders: nausea, vomiting
7 DRUG INTERACTIONS
7.1 HMG-CoA Reductase Inhibitors
In healthy subjects, concomitant administration of CUBICIN and simvastatin had no effect on plasma trough concentrations of simvastatin, and there were no reports of skeletal myopathy [see Clinical Pharmacology (12.3) ].
However, inhibitors of HMG-CoA reductase may cause myopathy, which is manifested as muscle pain or weakness associated with elevated levels of creatine phosphokinase (CPK). In the Phase 3 S. aureus bacteremia/endocarditis trial, some patients who received prior or concomitant treatment with an HMG-CoA reductase inhibitor developed elevated CPK [see Adverse Reactions (6.1) ]. Experience with the coadministration of HMG-CoA reductase inhibitors and CUBICIN in patients is limited; therefore, consideration should be given to suspending use of HMG-CoA reductase inhibitors temporarily in patients receiving CUBICIN.
7.2 Drug-Laboratory Test Interactions
Clinically relevant plasma concentrations of daptomycin have been observed to cause a significant concentration-dependent false prolongation of prothrombin time (PT) and elevation of International Normalized Ratio (INR) when certain recombinant thromboplastin reagents are utilized for the assay. The possibility of an erroneously elevated PT/INR result due to interaction with a recombinant thromboplastin reagent may be minimized by drawing specimens for PT or INR testing near the time of trough plasma concentrations of daptomycin. However, sufficient daptomycin concentrations may be present at trough to cause interaction.
If confronted with an abnormally high PT/INR result in a patient being treated with CUBICIN, it is recommended that clinicians:
- Repeat the assessment of PT/INR, requesting that the specimen be drawn just prior to the next CUBICIN dose (i.e., at trough concentration). If the PT/INR value obtained at trough remains substantially elevated above what would otherwise be expected, consider evaluating PT/INR utilizing an alternative method.
- Evaluate for other causes of abnormally elevated PT/INR results.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects: Pregnancy Category B
There are no adequate and well-controlled trials of CUBICIN in pregnant women. Embryofetal development studies performed in rats and rabbits at doses of up to 75 mg/kg (2 and 4 times the 6 mg/kg human dose, respectively, on a body surface area basis) revealed no evidence of harm to the fetus due to daptomycin. Because animal reproduction studies are not always predictive of human response, CUBICIN should be used during pregnancy only if the potential benefit outweighs the possible risk.
8.3 Nursing Mothers
Daptomycin is present in human milk but is poorly bioavailable orally. In a single case study, CUBICIN was administered daily for 28 days to a nursing mother at an IV dose of 6.7 mg/kg/day, and samples of the patient's breast milk were collected over a 24-hour period on day 27. The highest measured concentration of daptomycin in the breast milk was 0.045 mcg/mL1. The calculated maximum daily CUBICIN dose to the infant (assuming mean milk consumption of 150 mL/kg/day) was 0.1% of the maternal dose of 6.7 mg/kg/day. Caution should be exercised when CUBICIN is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness of CUBICIN in patients under the age of 18 years have not been established [see Nonclinical Toxicology (13.2) ].
8.5 Geriatric Use
Of the 534 patients treated with CUBICIN in Phase 3 controlled clinical trials of complicated skin and skin structure infections (cSSSI), 27% were 65 years of age or older and 12% were 75 years of age or older. Of the 120 patients treated with CUBICIN in the Phase 3 controlled clinical trial of S. aureus bacteremia/endocarditis, 25% were 65 years of age or older and 16% were 75 years of age or older. In Phase 3 clinical trials of cSSSI and S. aureus bacteremia/endocarditis, clinical success rates were lower in patients ≥65 years of age than in patients <65 years of age. In addition, treatment-emergent adverse events were more common in patients ≥65 years of age than in patients <65 years of age.
The exposure of daptomycin was higher in healthy elderly subjects than in healthy young subjects. However, no adjustment of CUBICIN dosage is warranted for elderly patients with creatinine clearance (CLCR) ≥30 mL/min [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3) ].
8.6 Patients with Renal Impairment
Daptomycin is eliminated primarily by the kidneys; therefore, a modification of CUBICIN dosage interval is recommended for patients with CLCR <30 mL/min, including patients receiving hemodialysis or continuous ambulatory peritoneal dialysis (CAPD). In patients with renal impairment, both renal function and creatine phosphokinase (CPK) should be monitored more frequently than once weekly [see Dosage and Administration (2.4) , Warnings and Precautions (5.2, 5.7), and Clinical Pharmacology (12.3) ].
10 OVERDOSAGE
In the event of overdosage, supportive care is advised with maintenance of glomerular filtration. Daptomycin is cleared slowly from the body by hemodialysis (approximately 15% of the administered dose is removed over 4 hours) and by peritoneal dialysis (approximately 11% of the administered dose is removed over 48 hours). The use of high-flux dialysis membranes during 4 hours of hemodialysis may increase the percentage of dose removed compared with that removed by low-flux membranes.
11 DESCRIPTION
CUBICIN contains daptomycin, a cyclic lipopeptide antibacterial agent derived from the fermentation of Streptomyces roseosporus. The chemical name is N-decanoyl-L-tryptophyl-D-asparaginyl-L-aspartyl-L-threonylglycyl-L-ornithyl-L-aspartyl-D-alanyl-L-aspartylglycyl-D-seryl-threo-3-methyl-L-glutamyl-3-anthraniloyl-L-alanine ε1-lactone. The chemical structure is:
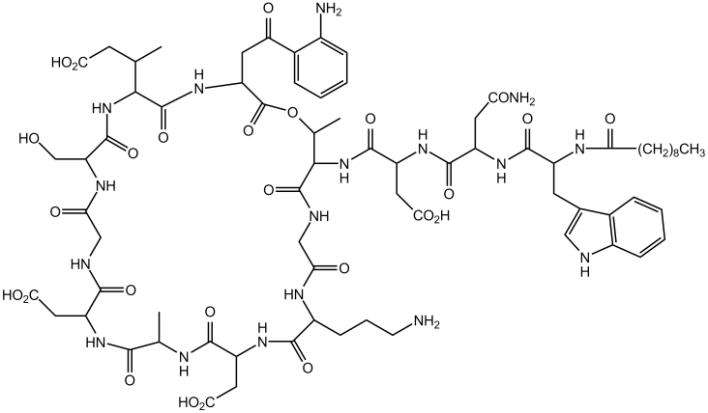
The empirical formula is C72H101N17O26; the molecular weight is 1620.67. CUBICIN is supplied in a single-use vial as a sterile, preservative-free, pale yellow to light brown, lyophilized cake containing approximately 500 mg of daptomycin for intravenous (IV) use following reconstitution with 0.9% sodium chloride injection [see Dosage and Administration (2.5) ]. The only inactive ingredient is sodium hydroxide, which is used in minimal quantities for pH adjustment. Freshly reconstituted solutions of CUBICIN range in color from pale yellow to light brown.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Daptomycin is an antibacterial drug [see Microbiology (12.4) ].
12.2 Pharmacodynamics
Based on animal models of infection, the antimicrobial activity of daptomycin appears to correlate with the AUC/MIC (area under the concentration-time curve/minimum inhibitory concentration) ratio for certain pathogens, including S. aureus. The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and microbiological cure has not been elucidated in clinical trials with CUBICIN.
12.3 Pharmacokinetics
CUBICIN Administered over a 30-Minute Period
The mean and standard deviation (SD) pharmacokinetic parameters of daptomycin at steady-state following intravenous (IV) administration of CUBICIN over a 30-minute period at 4 to 12 mg/kg q24h to healthy young adults are summarized in Table 7.
| Dose (mg/kg) |
Pharmacokinetic Parameters |
||||
|---|---|---|---|---|---|
| AUC0-24
(mcg•h/mL) |
t1/2
(h) |
Vss
(L/kg) |
CLT
(mL/h/kg) |
Cmax
(mcg/mL) |
|
| 4 (N=6) | 494 (75) | 8.1 (1.0) | 0.096 (0.009) | 8.3 (1.3) | 57.8 (3.0) |
| 6 (N=6) | 632 (78) | 7.9 (1.0) | 0.101 (0.007) | 9.1 (1.5) | 93.9 (6.0) |
| 8 (N=6) | 858 (213) | 8.3 (2.2) | 0.101 (0.013) | 9.0 (3.0) | 123.3 (16.0) |
| 10 (N=9) | 1039 (178) | 7.9 (0.6) | 0.098 (0.017) | 8.8 (2.2) | 141.1 (24.0) |
| 12 (N=9) | 1277 (253) | 7.7 (1.1) | 0.097 (0.018) | 9.0 (2.8) | 183.7 (25.0) |
Daptomycin pharmacokinetics were generally linear and time-independent at CUBICIN doses of 4 to 12 mg/kg q24h administered by IV infusion over a 30-minute period for up to 14 days. Steady-state trough concentrations were achieved by the third daily dose. The mean (SD) steady-state trough concentrations attained following the administration of 4, 6, 8, 10, and 12 mg/kg q24h were 5.9 (1.6), 6.7 (1.6), 10.3 (5.5), 12.9 (2.9), and 13.7 (5.2) mcg/mL, respectively.
CUBICIN Administered over a 2-Minute Period
Following IV administration of CUBICIN over a 2-minute period to healthy volunteers at doses of 4 mg/kg (N=8) and 6 mg/kg (N=12), the mean (SD) steady-state systemic exposure (AUC) values were 475 (71) and 701 (82) mcg•h/mL, respectively. Values for maximum plasma concentration (Cmax) at the end of the 2-minute period could not be determined adequately in this study. However, using pharmacokinetic parameters from 14 healthy volunteers who received a single dose of CUBICIN 6 mg/kg IV administered over a 30-minute period in a separate study, steady-state Cmax values were simulated for CUBICIN 4 and 6 mg/kg IV administered over a 2-minute period. The simulated mean (SD) steady-state Cmax values were 77.7 (8.1) and 116.6 (12.2) mcg/mL, respectively.
Distribution
Daptomycin is reversibly bound to human plasma proteins, primarily to serum albumin, in a concentration-independent manner. The overall mean binding ranges from 90 to 93%.
In clinical studies, mean serum protein binding in subjects with creatinine clearance (CLCR) ≥30 mL/min was comparable to that observed in healthy subjects with normal renal function. However, there was a trend toward decreasing serum protein binding among subjects with CLCR <30 mL/min (88%), including those receiving hemodialysis (86%) and continuous ambulatory peritoneal dialysis (CAPD) (84%). The protein binding of daptomycin in subjects with moderate hepatic impairment (Child-Pugh Class B) was similar to that in healthy adult subjects.
The volume of distribution at steady-state (Vss) of daptomycin in healthy adult subjects was approximately 0.1 L/kg and was independent of dose.
Metabolism
In in vitro studies, daptomycin was not metabolized by human liver microsomes.
In 5 healthy adults after infusion of radiolabeled 14C-daptomycin, the plasma total radioactivity was similar to the concentration determined by microbiological assay. Inactive metabolites were detected in urine, as determined by the difference between total radioactive concentrations and microbiologically active concentrations. In a separate study, no metabolites were observed in plasma on Day 1 following the administration of CUBICIN at 6 mg/kg to subjects. Minor amounts of three oxidative metabolites and one unidentified compound were detected in urine. The site of metabolism has not been identified.
Excretion
Daptomycin is excreted primarily by the kidneys. In a mass balance study of 5 healthy subjects using radiolabeled daptomycin, approximately 78% of the administered dose was recovered from urine based on total radioactivity (approximately 52% of the dose based on microbiologically active concentrations), and 5.7% of the administered dose was recovered from feces (collected for up to 9 days) based on total radioactivity.
Specific Populations
Renal Impairment
Population-derived pharmacokinetic parameters were determined for infected patients (complicated skin and skin structure infections [cSSSI] and S. aureus bacteremia) and noninfected subjects with various degrees of renal function (Table 8). Total plasma clearance (CLT), elimination half-life (t1/2), and volume of distribution at steady-state (Vss) in patients with cSSSI were similar to those in patients with S. aureus bacteremia. Following administration of CUBICIN 4 mg/kg q24h by IV infusion over a 30-minute period, the mean CLT was 9%, 22%, and 46% lower among subjects and patients with mild (CLCR 50–80 mL/min), moderate (CLCR 30–<50 mL/min), and severe (CLCR <30 mL/min) renal impairment, respectively, than in those with normal renal function (CLCR >80 mL/min). The mean steady-state systemic exposure (AUC), t1/2, and Vss increased with decreasing renal function, although the mean AUC for patients with CLCR 30–80 mL/min was not markedly different from the mean AUC for patients with normal renal function. The mean AUC for patients with CLCR <30 mL/min and for patients on dialysis (CAPD and hemodialysis dosed post-dialysis) was approximately 2 and 3 times higher, respectively, than for patients with normal renal function. The mean Cmax ranged from 60 to 70 mcg/mL in patients with CLCR ≥30 mL/min, while the mean Cmax for patients with CLCR <30 mL/min ranged from 41 to 58 mcg/mL. After administration of CUBICIN 6 mg/kg q24h by IV infusion over a 30-minute period, the mean Cmax ranged from 80 to 114 mcg/mL in patients with mild to moderate renal impairment and was similar to that of patients with normal renal function.
| Renal Function | Pharmacokinetic Parameters |
|||||
|---|---|---|---|---|---|---|
t1/2
 (h) 4 mg/kg |
Vss
 (L/kg) 4 mg/kg |
CLT
 (mL/h/kg) 4 mg/kg |
AUC0-∞
 (mcg•h/mL) 4 mg/kg |
AUCss
(mcg•h/mL) 6 mg/kg |
Cmin,ss
 (mcg/mL) 6 mg/kg |
|
| Note: CUBICIN was administered over a 30-minute period. | ||||||
| Normal (CLCR >80 mL/min) |
9.39 (4.74) N=165 |
0.13 (0.05) N=165 |
10.9 (4.0) N=165 |
417 (155) N=165 |
545 (296) N=62 |
6.9 (3.5) N=61 |
| Mild Renal Impairment (CLCR 50–80 mL/min) |
10.75 (8.36) N=64 |
0.12 (0.05) N=64 |
9.9 (4.0) N=64 |
466 (177) N=64 |
637 (215) N=29 |
12.4 (5.6) N=29 |
| Moderate Renal Impairment (CLCR 30–<50 mL/min) |
14.70 (10.50) N=24 |
0.15 (0.06) N=24 |
8.5 (3.4) N=24 |
560 (258) N=24 |
868 (349) N=15 |
19.0 (9.0) N=14 |
| Severe Renal Impairment (CLCR <30 mL/min) |
27.83 (14.85) N=8 |
0.20 (0.15) N=8 |
5.9 (3.9) N=8 |
925 (467) N=8 |
1050, 892 N=2 |
24.4, 21.4 N=2 |
| Hemodialysis | 30.51 (6.51) N=16 |
0.16 (0.04) N=16 |
3.9 (2.1) N=16 |
1193 (399) N=16 |
NA | NA |
| CAPD | 27.56 (4.53) N=5 |
0.11 (0.02) N=5 |
2.9 (0.4) N=5 |
1409 (238) N=5 |
NA | NA |
Because renal excretion is the primary route of elimination, adjustment of CUBICIN dosage interval is necessary in patients with severe renal impairment (CLCR <30 mL/min) [see Dosage and Administration (2.4) ].
Hepatic Impairment
The pharmacokinetics of daptomycin were evaluated in 10 subjects with moderate hepatic impairment (Child-Pugh Class B) and compared with those in healthy volunteers (N=9) matched for gender, age, and weight. The pharmacokinetics of daptomycin were not altered in subjects with moderate hepatic impairment. No dosage adjustment is warranted when CUBICIN is administered to patients with mild to moderate hepatic impairment. The pharmacokinetics of daptomycin in patients with severe hepatic impairment (Child-Pugh Class C) have not been evaluated.
Gender
No clinically significant gender-related differences in daptomycin pharmacokinetics have been observed. No dosage adjustment is warranted based on gender when CUBICIN is administered.
Geriatric
The pharmacokinetics of daptomycin were evaluated in 12 healthy elderly subjects (≥75 years of age) and 11 healthy young controls (18 to 30 years of age). Following administration of a single 4 mg/kg dose of CUBICIN by IV infusion over a 30-minute period, the mean total clearance of daptomycin was approximately 35% lower and the mean AUC0- ∞ was approximately 58% higher in elderly subjects than in healthy young subjects. There were no differences in Cmax [see Use in Specific Populations (8.5) ].
Obesity
The pharmacokinetics of daptomycin were evaluated in 6 moderately obese (Body Mass Index [BMI] 25 to 39.9 kg/m2) and 6 extremely obese (BMI ≥40 kg/m2) subjects and controls matched for age, gender, and renal function. Following administration of CUBICIN by IV infusion over a 30-minute period as a single 4 mg/kg dose based on total body weight, the total plasma clearance of daptomycin normalized to total body weight was approximately 15% lower in moderately obese subjects and 23% lower in extremely obese subjects than in nonobese controls. The AUC0- ∞ of daptomycin was approximately 30% higher in moderately obese subjects and 31% higher in extremely obese subjects than in nonobese controls. The differences were most likely due to differences in the renal clearance of daptomycin. No adjustment of CUBICIN dosage is warranted in obese patients.
Pediatric
The pharmacokinetics of daptomycin in pediatric populations (<18 years of age) have not been established [see Nonclinical Toxicology (13.2) ].
Drug-Drug Interactions
In Vitro Studies
In vitro studies with human hepatocytes indicate that daptomycin does not inhibit or induce the activities of the following human cytochrome P450 isoforms: 1A2, 2A6, 2C9, 2C19, 2D6, 2E1, and 3A4. It is unlikely that daptomycin will inhibit or induce the metabolism of drugs metabolized by the P450 system.
Aztreonam
In a study in which 15 healthy adult subjects received a single dose of CUBICIN 6 mg/kg IV and a combination dose of CUBICIN 6 mg/kg IV and aztreonam 1 g IV, administered over a 30-minute period, the Cmax and AUC0- ∞ of daptomycin were not significantly altered by aztreonam.
Tobramycin
In a study in which 6 healthy adult males received a single dose of CUBICIN 2 mg/kg IV, tobramycin 1 mg/kg IV, and both in combination, administered over a 30-minute period, the mean Cmax and AUC0- ∞ of daptomycin were 12.7% and 8.7% higher, respectively, when CUBICIN was coadministered with tobramycin. The mean Cmax and AUC0- ∞ of tobramycin were 10.7% and 6.6% lower, respectively, when tobramycin was coadministered with CUBICIN. These differences were not statistically significant. The interaction between daptomycin and tobramycin with a clinical dose of CUBICIN is unknown.
Warfarin
In 16 healthy subjects, administration of CUBICIN 6 mg/kg q24h by IV infusion over a 30-minute period for 5 days, with coadministration of a single oral dose of warfarin (25 mg) on the 5th day, had no significant effect on the pharmacokinetics of either drug and did not significantly alter the INR (International Normalized Ratio).
Simvastatin
In 20 healthy subjects on a stable daily dose of simvastatin 40 mg, administration of CUBICIN 4 mg/kg q24h by IV infusion over a 30-minute period for 14 days (N=10) had no effect on plasma trough concentrations of simvastatin and was not associated with a higher incidence of adverse events, including skeletal myopathy, than in subjects receiving placebo once daily (N=10) [see Warnings and Precautions (5.2) and Drug Interactions (7.1) ].
Probenecid
Concomitant administration of probenecid (500 mg 4 times daily) and a single dose of CUBICIN 4 mg/kg by IV infusion over a 30-minute period did not significantly alter the Cmax or AUC0- ∞ of daptomycin.
12.4 Microbiology
Daptomycin belongs to the cyclic lipopeptide class of antibacterials. Daptomycin has clinical utility in the treatment of infections caused by aerobic, Gram-positive bacteria. The in vitro spectrum of activity of daptomycin encompasses most clinically relevant Gram-positive pathogenic bacteria.
Daptomycin exhibits rapid, concentration-dependent bactericidal activity against Gram-positive bacteria in vitro. This has been demonstrated both by time-kill curves and by MBC/MIC (minimum bactericidal concentration/minimum inhibitory concentration) ratios using broth dilution methodology. Daptomycin maintained bactericidal activity in vitro against stationary phase S. aureus in simulated endocardial vegetations. The clinical significance of this is not known.
Mechanism of Action
The mechanism of action of daptomycin is distinct from that of any other antibacterial. Daptomycin binds to bacterial cell membranes and causes a rapid depolarization of membrane potential. This loss of membrane potential causes inhibition of DNA, RNA, and protein synthesis, which results in bacterial cell death.
Mechanism of Resistance
The mechanism(s) of daptomycin resistance is not fully understood. Currently, there are no known transferable elements that confer resistance to daptomycin.
Complicated Skin and Skin Structure Infection (cSSSI) Trials
The emergence of daptomycin non-susceptible isolates occurred in 2 infected patients across the set of Phase 2 and pivotal Phase 3 clinical trials of cSSSI. In one case, a non-susceptible S. aureus was isolated from a patient in a Phase 2 trial who received CUBICIN at less than the protocol-specified dose for the initial 5 days of therapy. In the second case, a non-susceptible Enterococcus faecalis was isolated from a patient with an infected chronic decubitus ulcer who was enrolled in a salvage trial.
S. aureus Bacteremia/Endocarditis and Other Post-Approval Trials
In subsequent clinical trials, non-susceptible isolates were recovered. S. aureus was isolated from a patient in a compassionate-use trial and from 7 patients in the S. aureus bacteremia/endocarditis trial [see Clinical Trials (14.2) ]. An E. faecium was isolated from a patient in a vancomycin-resistant enterococci trial.
Interactions with Other Antibacterials
In vitro studies have investigated daptomycin interactions with other antibacterials. Antagonism, as determined by kill curve studies, has not been observed. In vitro synergistic interactions of daptomycin with aminoglycosides, β-lactam antibacterials, and rifampin have been shown against some isolates of staphylococci (including some methicillin-resistant isolates) and enterococci (including some vancomycin-resistant isolates).
Activity In Vitro and In Vivo
Daptomycin has been shown to be active against most isolates of the following Gram-positive bacteria both in vitro and in clinical infections, as described in Indications and Usage (1) .
-
-
-
-
-
-
The following in vitro data are available, but their clinical significance is unknown. At least 90% of the following Gram-positive bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for daptomycin versus the bacterial genus (Table 9). However, the efficacy of CUBICIN in treating clinical infections due to these bacteria has not been established in adequate and well-controlled clinical trials.
-
-
-
-
-
-
Susceptibility Testing Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility tests for antimicrobial drug products used in resident hospitals to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting an antibacterial drug product for treatment.
Dilution Techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized broth test method2,3 with the broth adjusted to a calcium content of 50 mg/L. The use of the agar dilution method is not recommended with daptomycin3. The MICs should be interpreted according to the criteria listed in Table 9.
| Pathogen | Broth Dilution MIC (mcg/mL) |
||
|---|---|---|---|
| S | I | R | |
| Note: S, Susceptible; I, Intermediate; R, Resistant. | |||
|
Staphylococcus aureus
(methicillin-susceptible and methicillin-resistant) |
≤1 | ( |
( |
|
Streptococcus pyogenes, Streptococcus agalactiae, and Streptococcus dysgalactiae subsp. equisimilis |
≤1 | ( |
( |
|
Enterococcus faecalis
(vancomycin-susceptible only) |
≤4 | ( |
( |
A report of "Susceptible" indicates that the antimicrobial is likely to inhibit the growth of the pathogen if the antimicrobial compound reaches the concentration at the infection site necessary to inhibit growth of the pathogen.
Diffusion Technique
Quantitative methods that require measurement of zone diameters have not been shown to provide reproducible estimates of the susceptibility of bacteria to daptomycin. The use of the disk diffusion method is not recommended with daptomycin3,4.
Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay, and the techniques of the individuals performing the test2,3. Standard daptomycin powder should provide the ranges of MIC values noted in Table 10.
| Quality Control Strain | Broth Dilution MIC Range (mcg/mL) |
|---|---|
| Enterococcus faecalis ATCC 29212 | 1–4 |
| Staphylococcus aureus ATCC 29213 | 0.12–1 |
|
Streptococcus pneumoniae ATCC 49619 |
0.06–0.5 |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term carcinogenicity studies in animals have not been conducted to evaluate the carcinogenic potential of CUBICIN. However, neither mutagenic nor clastogenic potential was found in a battery of genotoxicity tests, including the Ames assay, a mammalian cell gene mutation assay, a test for chromosomal aberrations in Chinese hamster ovary cells, an in vivo micronucleus assay, an in vitro DNA repair assay, and an in vivo sister chromatid exchange assay in Chinese hamsters.
Daptomycin did not affect the fertility or reproductive performance of male and female rats when administered intravenously at doses up to 150 mg/kg/day, which is approximately 9 times the estimated human exposure level based upon AUCs.
13.2 Animal Toxicology and/or Pharmacology
Adult Animals
In animals, daptomycin administration has been associated with effects on skeletal muscle. However, there were no changes in cardiac or smooth muscle. Skeletal muscle effects were characterized by microscopic degenerative/regenerative changes and variable elevations in creatine phosphokinase (CPK). No fibrosis or rhabdomyolysis was evident in repeat-dose studies up to the highest doses tested in rats (150 mg/kg/day) and dogs (100 mg/kg/day). The degree of skeletal myopathy showed no increase when treatment was extended from 1 month to up to 6 months. Severity was dose-dependent. All muscle effects, including microscopic changes, were fully reversible within 30 days following the cessation of dosing.
In adult animals, effects on peripheral nerve (characterized by axonal degeneration and frequently accompanied by significant losses of patellar reflex, gag reflex, and pain perception) were observed at daptomycin doses higher than those associated with skeletal myopathy. Deficits in the dogs' patellar reflexes were seen within 2 weeks after the start of treatment at 40 mg/kg/day (9 times the human Cmax at the 6 mg/kg/day dose), with some clinical improvement noted within 2 weeks after the cessation of dosing. However, at 75 mg/kg/day for 1 month, 7 of 8 dogs failed to regain full patellar reflex responses within a 3-month recovery period. In a separate study in dogs receiving doses of 75 and 100 mg/kg/day for 2 weeks, minimal residual histological changes were noted at 6 months after the cessation of dosing. However, recovery of peripheral nerve function was evident.
Tissue distribution studies in rats showed that daptomycin is retained in the kidney but appears to penetrate the blood-brain barrier only minimally following single and multiple doses.
Juvenile Animals
Target organs of daptomycin-related effects in 7-week-old juvenile dogs were skeletal muscle and nerve, the same target organs as in adult dogs. In juvenile dogs, nerve effects were noted at lower daptomycin blood concentrations than in adult dogs following 28 days of dosing. In contrast to adult dogs, juvenile dogs also showed evidence of effects in nerves of the spinal cord as well as peripheral nerves after 28 days of dosing. No nerve effects were noted in juvenile dogs following 14 days of dosing at doses up to 75 mg/kg/day.
Administration of daptomycin to 7-week-old juvenile dogs for 28 days at doses of 50 mg/kg/day produced minimal degenerative effects on the peripheral nerve and spinal cord in several animals, with no corresponding clinical signs. A dose of 150 mg/kg/day for 28 days produced minimal degeneration in the peripheral nerve and spinal cord as well as minimal to mild degeneration of the skeletal muscle in a majority of animals, accompanied by slight to severe muscle weakness evident in most dogs. Following a 28-day recovery phase, microscopic examination revealed recovery of the skeletal muscle and the ulnar nerve effects, but nerve degeneration in the sciatic nerve and spinal cord was still observed in all 150 mg/kg/day dogs.
Following once-daily administration of daptomycin to juvenile dogs for 28 days, microscopic effects in nerve tissue were noted at a Cmax value of 417 mcg/mL, which is approximately 3-fold less than the Cmax value associated with nerve effects in adult dogs treated once daily with daptomycin for 28 days (1308 mcg/mL).
14 CLINICAL TRIALS
14.1 Complicated Skin and Skin Structure Infections
Adult patients with clinically documented complicated skin and skin structure infections (cSSSI) (Table 11) were enrolled in two randomized, multinational, multicenter, investigator-blinded trials comparing CUBICIN (4 mg/kg IV q24h) with either vancomycin (1 g IV q12h) or an anti-staphylococcal semi-synthetic penicillin (i.e., nafcillin, oxacillin, cloxacillin, or flucloxacillin; 4 to 12 g IV per day). Patients could switch to oral therapy after a minimum of 4 days of IV treatment if clinical improvement was demonstrated. Patients known to have bacteremia at baseline were excluded. Patients with creatinine clearance (CLCR) between 30 and 70 mL/min were to receive a lower dose of CUBICIN as specified in the protocol; however, the majority of patients in this subpopulation did not have the dose of CUBICIN adjusted.
| Primary Diagnosis | Patients (CUBICIN / Comparator |
||
|---|---|---|---|
| Study 9801 N=264 / N=266 |
Study 9901 N=270 / N=292 |
Pooled N=534 / N=558 |
|
| Wound Infection | 99 (38%) / 116 (44%) | 102 (38%) / 108 (37%) | 201 (38%) / 224 (40%) |
| Major Abscess | 55 (21%) / 43 (16%) | 59 (22%) / 65 (22%) | 114 (21%) / 108 (19%) |
| Ulcer Infection | 71 (27%) / 75 (28%) | 53 (20%) / 68 (23%) | 124 (23%) / 143 (26%) |
| Other Infection |
39 (15%) / 32 (12%) | 56 (21%) / 51 (18%) | 95 (18%) / 83 (15%) |
One trial was conducted primarily in the United States and South Africa (study 9801), and the second was conducted at non-US sites only (study 9901). The two trials were similar in design but differed in patient characteristics, including history of diabetes and peripheral vascular disease. There were a total of 534 patients treated with CUBICIN and 558 treated with comparator in the two trials. The majority (89.7%) of patients received IV medication exclusively.
The efficacy endpoints in both trials were the clinical success rates in the intent-to-treat (ITT) population and in the clinically evaluable (CE) population. In study 9801, clinical success rates in the ITT population were 62.5% (165/264) in patients treated with CUBICIN and 60.9% (162/266) in patients treated with comparator drugs. Clinical success rates in the CE population were 76.0% (158/208) in patients treated with CUBICIN and 76.7% (158/206) in patients treated with comparator drugs. In study 9901, clinical success rates in the ITT population were 80.4% (217/270) in patients treated with CUBICIN and 80.5% (235/292) in patients treated with comparator drugs. Clinical success rates in the CE population were 89.9% (214/238) in patients treated with CUBICIN and 90.4% (226/250) in patients treated with comparator drugs.
The success rates by pathogen for microbiologically evaluable patients are presented in Table 12.
| Pathogen | Success Rate n/N (%) |
|
|---|---|---|
| CUBICIN | Comparator |
|
Methicillin-susceptible Staphylococcus aureus (MSSA) |
170/198 (86%) | 180/207 (87%) |
Methicillin-resistant Staphylococcus aureus (MRSA) |
21/28 (75%) | 25/36 (69%) |
| Streptococcus pyogenes | 79/84 (94%) | 80/88 (91%) |
| Streptococcus agalactiae | 23/27 (85%) | 22/29 (76%) |
| Streptococcus dysgalactiae subsp. equisimilis | 8/8 (100%) | 9/11 (82%) |
| Enterococcus faecalis (vancomycin-susceptible only) | 27/37 (73%) | 40/53 (76%) |
14.2 Bacteremia/Endocarditis
The efficacy of CUBICIN in the treatment of patients with S. aureus bacteremia was demonstrated in a randomized, controlled, multinational, multicenter, open-label trial. In this trial, adult patients with at least one positive blood culture for S. aureus obtained within 2 calendar days prior to the first dose of study drug and irrespective of source were enrolled and randomized to either CUBICIN (6 mg/kg IV q24h) or standard of care [an anti-staphylococcal semi-synthetic penicillin 2 g IV q4h (nafcillin, oxacillin, cloxacillin, or flucloxacillin) or vancomycin 1 g IV q12h, each with initial gentamicin 1 mg/kg IV every 8 hours for first 4 days]. Of the patients in the comparator group, 93% received initial gentamicin for a median of 4 days, compared with 1 patient (<1%) in the CUBICIN group. Patients with prosthetic heart valves, intravascular foreign material that was not planned for removal within 4 days after the first dose of study medication, severe neutropenia, known osteomyelitis, polymicrobial bloodstream infections, creatinine clearance <30 mL/min, and pneumonia were excluded.
Upon entry, patients were classified for likelihood of endocarditis using the modified Duke criteria (Possible, Definite, or Not Endocarditis). Echocardiography, including a transesophageal echocardiogram (TEE), was performed within 5 days following study enrollment. The choice of comparator agent was based on the oxacillin susceptibility of the S. aureus isolate. The duration of study treatment was based on the investigator's clinical diagnosis. Final diagnoses and outcome assessments at Test of Cure (6 weeks after the last treatment dose) were made by a treatment-blinded Adjudication Committee, using protocol-specified clinical definitions and a composite primary efficacy endpoint (clinical and microbiological success) at the Test of Cure visit.
A total of 246 patients ≥18 years of age (124 CUBICIN, 122 comparator) with S. aureus bacteremia were randomized from 48 centers in the US and Europe. In the ITT population, 120 patients received CUBICIN and 115 received comparator (62 received an anti-staphylococcal semi-synthetic penicillin and 53 received vancomycin). Thirty-five patients treated with an anti-staphylococcal semi-synthetic penicillin received vancomycin initially for 1 to 3 days, pending final susceptibility results for the S. aureus isolates. The median age among the 235 patients in the ITT population was 53 years (range: 21 to 91 years); 30/120 (25%) in the CUBICIN group and 37/115 (32%) in the comparator group were ≥65 years of age. Of the 235 ITT patients, there were 141 (60%) males and 156 (66%) Caucasians across the two treatment groups. In addition, 176 (75%) of the ITT population had systemic inflammatory response syndrome (SIRS) at baseline and 85 (36%) had surgical procedures within 30 days prior to onset of the S. aureus bacteremia. Eighty-nine patients (38%) had bacteremia caused by methicillin-resistant S. aureus (MRSA). Entry diagnosis was based on the modified Duke criteria and comprised 37 (16%) Definite, 144 (61%) Possible, and 54 (23%) Not Endocarditis. Of the 37 patients with an entry diagnosis of Definite Endocarditis, all (100%) had a final diagnosis of infective endocarditis, and of the 144 patients with an entry diagnosis of Possible Endocarditis, 15 (10%) had a final diagnosis of infective endocarditis as assessed by the Adjudication Committee. Of the 54 patients with an entry diagnosis of Not Endocarditis, 1 (2%) had a final diagnosis of infective endocarditis as assessed by the Adjudication Committee.
In the ITT population, there were 182 patients with bacteremia and 53 patients with infective endocarditis as assessed by the Adjudication Committee, including 35 with right-sided endocarditis and 18 with left-sided endocarditis. The 182 patients with bacteremia comprised 121 with complicated S. aureus bacteremia and 61 with uncomplicated S. aureus bacteremia.
Complicated bacteremia was defined as S. aureus isolated from blood cultures obtained on at least 2 different calendar days, and/or metastatic foci of infection (deep tissue involvement), and classification of the patient as not having endocarditis according to the modified Duke criteria. Uncomplicated bacteremia was defined as S. aureus isolated from blood culture(s) obtained on a single calendar day, no metastatic foci of infection, no infection of prosthetic material, and classification of the patient as not having endocarditis according to the modified Duke criteria. The definition of right-sided infective endocarditis (RIE) used in the clinical trial was Definite or Possible Endocarditis according to the modified Duke criteria and no echocardiographic evidence of predisposing pathology or active involvement of either the mitral or aortic valve. Complicated RIE comprised patients who were not intravenous drug users, had a positive blood culture for MRSA, serum creatinine ≥2.5 mg/dL, or evidence of extrapulmonary sites of infection. Patients who were intravenous drug users, had a positive blood culture for methicillin-susceptible S. aureus (MSSA), had serum creatinine <2.5 mg/dL, and were without evidence of extrapulmonary sites of infection were considered to have uncomplicated RIE.
The coprimary efficacy endpoints in the trial were the Adjudication Committee success rates at the Test of Cure visit (6 weeks after the last treatment dose) in the ITT and Per Protocol (PP) populations. The overall Adjudication Committee success rates in the ITT population were 44.2% (53/120) in patients treated with CUBICIN and 41.7% (48/115) in patients treated with comparator (difference = 2.4% [95% CI −10.2, 15.1]). The success rates in the PP population were 54.4% (43/79) in patients treated with CUBICIN and 53.3% (32/60) in patients treated with comparator (difference = 1.1% [95% CI −15.6, 17.8]).
Adjudication Committee success rates are shown in Table 13.
| Population | Success Rate n/N (%) |
Difference: CUBICIN – Comparator (Confidence Interval) |
|
|---|---|---|---|
| CUBICIN 6 mg/kg | Comparator |
||
| Overall | 53/120 (44%) | 48/115 (42%) | 2.4% (−10.2, 15.1) |
| Baseline Pathogen | |||
| Methicillin-susceptible S. aureus | 33/74 (45%) | 34/70 (49%) | −4.0% (−22.6, 14.6) |
| Methicillin-resistant S. aureus | 20/45 (44%) | 14/44 (32%) | 12.6% (−10.2, 35.5) |
| Entry Diagnosis |
|||
| Definite or Possible Infective Endocarditis |
41/90 (46%) | 37/91 (41%) | 4.9% (−11.6, 21.4) |
| Not Infective Endocarditis | 12/30 (40%) | 11/24 (46%) | −5.8% (−36.2, 24.5) |
| Final Diagnosis | |||
| Uncomplicated Bacteremia | 18/32 (56%) | 16/29 (55%) | 1.1% (−31.7, 33.9) |
| Complicated Bacteremia | 26/60 (43%) | 23/61 (38%) | 5.6% (−17.3, 28.6) |
| Right-Sided Infective Endocarditis |
8/19 (42%) | 7/16 (44%) | −1.6% (−44.9, 41.6) |
| Uncomplicated Right-Sided Infective Endocarditis |
3/6 (50%) | 1/4 (25%) | 25.0% (−51.6, 100.0) |
| Complicated Right-Sided Infective Endocarditis |
5/13 (39%) | 6/12 (50%) | −11.5% (−62.4, 39.4) |
| Left-Sided Infective Endocarditis | 1/9 (11%) | 2/9 (22%) | −11.1% (−55.9, 33.6) |
Eighteen (18/120) patients in the CUBICIN arm and 19/116 patients in the comparator arm died during the trial. These comprise 3/28 CUBICIN-treated patients and 8/26 comparator-treated patients with endocarditis, as well as 15/92 CUBICIN-treated patients and 11/90 comparator-treated patients with bacteremia. Among patients with persisting or relapsing S. aureus infections, 8/19 CUBICIN-treated patients and 7/11 comparator-treated patients died.
Overall, there was no difference in time to clearance of S. aureus bacteremia between CUBICIN and comparator. The median time to clearance in patients with MSSA was 4 days and in patients with MRSA was 8 days.
Failure of treatment due to persisting or relapsing S. aureus infections was assessed by the Adjudication Committee in 19/120 (16%) CUBICIN-treated patients (12 with MRSA and 7 with MSSA) and 11/115 (10%) comparator-treated patients (9 with MRSA treated with vancomycin and 2 with MSSA treated with an anti-staphylococcal semi-synthetic penicillin). Among all failures, isolates from 6 CUBICIN-treated patients and 1 vancomycin-treated patient developed increasing MICs (reduced susceptibility) by central laboratory testing during or following therapy. Most patients who failed due to persisting or relapsing S. aureus infection had deep-seated infection and did not receive necessary surgical intervention [see Warnings and Precautions (5.6) ].
15 REFERENCES
- Buitrago MI, Crompton JA, Bertolami S, North DS, Nathan RA. Extremely low excretion of daptomycin into breast milk of a nursing mother with methicillin-resistant Staphylococcus aureus pelvic inflammatory disease. Pharmacotherapy 2009;29(3):347–351.
- Clinical and Laboratory Standards Institute (CLSI). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard—ninth edition. CLSI Document M07-A9; Wayne, PA. 2012.
- Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; twenty-second informational supplement. CLSI Document M100-S22; Wayne, PA. 2012.
- Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial disk susceptibility tests; approved standard—eleventh edition. CLSI Document M02-A11; Wayne, PA. 2012.
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633–638.
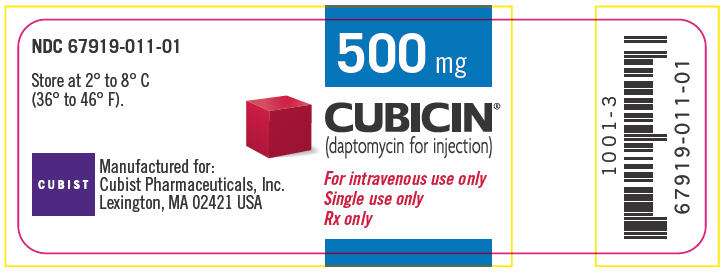
16 HOW SUPPLIED/STORAGE AND HANDLING
CUBICIN (daptomycin for injection) is supplied as a sterile pale yellow to light brown lyophilized cake in a single-use 10 mL vial containing 500 mg of daptomycin: Package of 1 (NDC 67919-011-01).
Store original packages at refrigerated temperatures, 2 to 8°C (36 to 46°F); avoid excessive heat.
17 PATIENT COUNSELING INFORMATION
Patients should be advised that allergic reactions, including serious allergic reactions, could occur and that serious reactions require immediate treatment. Patients should report any previous allergic reactions to CUBICIN. See Warnings and Precautions (5.1) .
Patients should be advised to report muscle pain or weakness, especially in the forearms and lower legs, as well as tingling or numbness. See Warnings and Precautions (5.2, 5.4) .
Patients should be advised to report any symptoms of cough, breathlessness, or fever. See Warnings and Precautions (5.3).
Diarrhea is a common problem caused by antibacterials that usually ends when the antibacterial is discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery and bloody stools (with or without stomach cramps and fever), even as late as 2 or more months after having received the last dose of the antibacterial. If this occurs, patients should contact their physician as soon as possible. See Warnings and Precautions (5.5) .
Patients should be counseled that antibacterial drugs, including CUBICIN, should be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When CUBICIN is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be administered exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by CUBICIN or other antibacterial drugs in the future.
CUBICIN is a registered trademark of Cubist Pharmaceuticals, Inc. All other trademarks are property of their respective owners.
Manufactured for:
Cubist Pharmaceuticals, Inc.
Lexington, MA 02421 USA
April 2013 (1004-12)
PRINCIPAL DISPLAY PANEL - 500 mg Vial
500 mg
CUBICIN
®
(daptomycin for injection)
For intravenous use only
Single use only
Rx only
PRINCIPAL DISPLAY PANEL - 1 Vial Carton
NDC 67919-011-01
One single-use vial
500 mg
CUBICIN
®
(daptomycin for injection)
For intravenous
use only
Rx only
CUBIST
Cubist Pharmaceuticals, Inc.
Lexington, MA 02421 USA
CubicinDaptomycin INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||