Dalbavancin
HIGHLIGHTS OF PRESCRIBING INFORMATION INDICATIONS AND USAGEDALVANCE is indicated for acute bacterial skin and skin structure infections (ABSSSI) caused by designated susceptible strains of Gram-positive microorganisms. (1) To reduce the development of drug-resistant bacteria and maintain the effectiveness of DALVANCE and other antibacterial drugs, DALVANCE should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria.DOSAGE AND ADMINISTRATION Two-dose regimen: 1000 mg followed one week later by 500 mg (2.1) Dosage adjustment for patients with creatinine clearance less than 30 mL/min and not receiving regularly scheduled hemodialysis: 750 mg followed one week later by 375 mg (2.2) Administer by intravenous infusion over 30 minutes (2.3) DOSAGE FORMS AND STRENGTHSFor injection: 500 mg of lyophilized powder in a single-use vial for reconstitution (3)CONTRAINDICATIONSHypersensitivity to dalbavancin (4)WARNINGS AND PRECAUTIONS Serious hypersensitivity (anaphylactic) and skin reactions have been reported with glycopeptide antibacterial agents, including DALVANCE; exercise caution in patients with known hypersensitivity to glycopeptides. (5.1) Rapid intravenous infusion of glycopeptide antibacterial agents can cause reactions. (5.2) ALT elevations with DALVANCE treatment were reported in clinical trials. (5.3) Clostridium difficile-associated diarrhea (CDAD) has been reported with nearly all systemic antibacterial agents, including DALVANCE. Evaluate if diarrhea occurs. (5.4) Side EffectsThe most common adverse reactions in patients treated with DALVANCE were nausea (5.5%), headache (4.7%), and diarrhea (4.4%). To report SUSPECTED ADVERSE REACTIONS, contact Durata Therapeutics, Inc. at 1-855-387-2825 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONSDosage adjustment is required in patients whose creatinine clearance is less than 30 mL/min and who are not receiving regularly scheduled hemodialysis. (8.6)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 DALBAVANCIN INDICATIONS AND USAGE
- 2 DALBAVANCIN DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 DALBAVANCIN CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 DALBAVANCIN ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 DALBAVANCIN DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Acute Bacterial Skin and Skin Structure Infections
DALVANCE™ (dalbavancin) for injection is indicated for the treatment of adult patients with acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible isolates of the following Gram-positive microorganisms: Staphylococcus aureus (including methicillin-susceptible and methicillin-resistant strains), Streptococcus pyogenes, Streptococcus agalactiae and Streptococcus anginosus group (including S. anginosus, S. intermedius, S. constellatus).
1.2 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of DALVANCE and other antibacterial agents, DALVANCE should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose Regimen
For treatment of adults with ABSSSI, the recommended two-dose regimen of DALVANCE is 1000 mg followed one week later by 500 mg. DALVANCE should be administered over 30 minutes by intravenous infusion [see Dosage and Administration (2.3)].
2.2 Patients with Renal Impairment
In patients with renal impairment whose known creatinine clearance is less than 30 mL/min and who are not receiving regularly scheduled hemodialysis, the recommended two-dose regimen of DALVANCE is 750 mg followed one week later by 375 mg. No dosage adjustment is recommended for patients receiving regularly scheduled hemodialysis, and DALVANCE can be administered without regard to the timing of hemodialysis [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.3)].
2.3 Preparation and Administration
DALVANCE(dalbavancin) for injection must be reconstituted with Sterile Water for Injection, USP, and subsequently diluted only with 5% Dextrose Injection, USP, to a final concentration of 1 mg/mL to 5 mg/mL.
Reconstitution: DALVANCE must be reconstituted under aseptic conditions, using 25 mL of Sterile Water for Injection, USP, for each 500 mg vial. To avoid foaming, alternate between gentle swirling and inversion of the vial until its contents are completely dissolved. Do not shake. The reconstituted vial contains 20 mg/mL dalbavancin as a clear, colorless to yellow solution.
Reconstituted vials may be stored either refrigerated at 2 to 8 °C (36 to 46 °F), or at controlled room temperature 20 to 25 °C (68 to 77 °F). Do not freeze.
Dilution: Aseptically transfer the required dose of reconstituted dalbavancin solution from the vial(s) to an intravenous bag or bottle containing 5% Dextrose Injection, USP. The diluted solution must have a final dalbavancin concentration of 1 mg/mL to 5 mg/mL. Discard any unused portion of the reconstituted solution.
Once diluted into an intravenous bag or bottle as described above, DALVANCE may be stored either refrigerated at 2 to 8 °C (36 to 46 °F) or at a controlled room temperature of 20 to 25 °C (68 to 77 °F). Do not freeze.
The total time from reconstitution to dilution to administration should not exceed 48 hours.
Like all parenteral drug products, diluted DALVANCE should be inspected visually for particulate matter prior to infusion. If particulate matter is identified, do not use.
After reconstitution and dilution, DALVANCE is to be administered via intravenous infusion, using a total infusion time of 30 minutes.
Do not co-infuse DALVANCE with other medications or electrolytes. Saline-based infusion solutions may cause precipitation and should not be used. The compatibility of reconstituted DALVANCE with intravenous medications, additives, or substances other than 5% Dextrose Injection, USP has not been established.
If a common intravenous line is being used to administer other drugs in addition to DALVANCE, the line should be flushed before and after each DALVANCE infusion with 5% Dextrose Injection, USP.
3 DOSAGE FORMS AND STRENGTHS
DALVANCE is supplied in single-use, clear glass vials containing sterile powder (white/off-white to pale yellow) equivalent to 500 mg of anhydrous dalbavancin.
4 CONTRAINDICATIONS
DALVANCE is contraindicated in patients with known hypersensitivity to dalbavancin. No data are available on cross-reactivity between dalbavancin and other glycopeptides, including vancomycin.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
Serious hypersensitivity (anaphylactic) and skin reactions have been reported in patients treated with DALVANCE. If an allergic reaction occurs, treatment with DALVANCE should be discontinued. Before using DALVANCE, inquire carefully about previous hypersensitivity reactions to glycopeptides, and due to the possibility of cross-sensitivity, exercise caution in patients with a history of glycopeptide allergy [see Patient Counseling Information (17)].
5.2 Infusion-Related Reactions
DALVANCE is administered via intravenous infusion, using a total infusion time of 30 minutes to minimize the risk of infusion-related reactions. Rapid intravenous infusions of DALVANCE can cause reactions that resemble "Red-Man Syndrome," including flushing of the upper body, urticaria, pruritus, and/or rash. Stopping or slowing the infusion may result in cessation of these reactions.
5.3 Hepatic Effects
In Phase 2 and 3 clinical trials, more DALVANCE- than comparator-treated subjects with normal baseline transaminase levels had post-baseline alanine aminotransferase (ALT) elevation greater than 3 times the upper limit of normal (ULN). Overall, abnormalities in liver tests (ALT, AST, bilirubin) were reported with similar frequency in the DALVANCE and comparator arms [see Adverse Reactions (6.1)].
5.4 Clostridium difficile-Associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported in users of nearly all systemic antibacterial drugs, including DALVANCE, with severity ranging from mild diarrhea to fatal colitis. Treatment with antibacterial agents can alter the normal flora of the colon, and may permit overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antibacterial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary because CDAD has been reported to occur more than 2 months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile should be discontinued, if possible. Appropriate measures such as fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.5 Development of Drug-Resistant Bacteria
Prescribing DALVANCE in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of DALVANCE cannot be directly compared to rates in the clinical trials of another drug and may not reflect rates observed in practice.
6.1 Side Effects in Clinical Trials
Adverse reactions were evaluated for 1778 patients treated with DALVANCE and 1224 patients treated with comparator antibacterial drugs in seven Phase 2 and Phase 3 clinical trials. A causal relationship between study drug and adverse reactions was not always established. The median age of patients treated with DALVANCE was 47 years, ranging between 16 and 93 years old. Patients treated with DALVANCE were predominantly male (60%) and Caucasian (78%).
Serious Adverse Reactions and Adverse Reactions Leading to Discontinuation
Serious adverse reactions occurred in 109/1778 (6.1%) of patients treated with DALVANCE and in 80/1224 (6.5%) of patients treated with comparator. DALVANCE was discontinued due to an adverse reaction in 53/1778 (3%) patients and the comparator was discontinued due to an adverse reaction in 35/1224 (2.8%) patients.
Most Common Adverse Reactions
The most common adverse reactions in patients treated with DALVANCE were nausea (5.5%), headache (4.7%), and diarrhea (4.4%). The median duration of adverse reactions was 4.0 days in both treatment groups.
Table 1 lists selected adverse reactions occurring in more than 2% of patients treated with DALVANCE in clinical trials.
|
Table 1. Selected Adverse Reactions in Phase 2/3 Trials (Number (%) of Patients) |
||
| Dalbavancin | Comparator* | |
| (N = 1778) | (N = 1224) | |
|
Nausea |
98 (5.5) |
78 (6.4) |
|
Vomiting |
50 (2.8) |
37 (3) |
|
Diarrhea |
79 (4.4) |
72 (5.9) |
|
Headache |
83 (4.7) |
59 (4.8) |
|
Rash |
48 (2.7) |
30 (2.4) |
|
Pruritus |
38 (2.1) |
41 (3.3) |
|
* Comparators included linezolid, cefazolin, cephalexin, and vancomycin. |
||
The following selected adverse reactions were reported in DALVANCE treated patients at a rate of less than 2% in these clinical trials:
Blood and lymphatic system disorders: anemia, hemorrhagic anemia, leucopenia, neutropenia, thrombocytopenia, petechiae, eosinophilia, thrombocytosis
Gastrointestinal disorders: gastrointestinal hemorrhage, melena, hematochezia, abdominal pain
General disorders and administration site conditions: infusion-related reactions
Hepatobiliary disorders: hepatotoxicity
Immune system disorders: anaphylactoid reaction
Infections and infestations: Clostridium difficile colitis, oral candidiasis, vulvovaginal mycotic infection
Investigations: hepatic transaminases increased, blood alkaline phosphatase increased, international normalized ratio increased
Metabolism and nutrition disorders: hypoglycemia
Nervous System disorders: dizziness
Respiratory, thoracic and mediastinal disorders: bronchospasm
Skin and Subcutaneous Tissue disorders: urticaria
Vascular disorders: flushing, phlebitis, wound hemorrhage, spontaneous hematoma
Alanine Aminotransferase (ALT) Elevations
Among patients with normal baseline ALT levels, more DALVANCE- than comparator-treated patients had post-baseline ALT elevations greater than 3 times the upper limit of normal (ULN), 12 (0.8%) vs. 2 (0.2%), respectively including three subjects with post-baseline ALT values greater than 10 times ULN. Eight of 12 patients treated with DALVANCE and one comparator patient had underlying conditions which could affect liver enzymes, including chronic viral hepatitis and a history of alcohol abuse. In addition, one DALVANCE-treated subject in a Phase 1 trial had post-baseline ALT elevations greater than 20 times ULN. ALT elevations were reversible in all subjects. No comparator-treated subject with normal baseline transaminases had post-baseline ALT elevation greater than 10 times ULN.
7 DRUG INTERACTIONS
7.1 Drug-Laboratory Test Interactions
Drug-laboratory test interactions have not been reported.
7.2 Drug-Drug Interactions
No clinical drug-drug interaction studies have been conducted with DALVANCE. There is minimal potential for drug-drug interactions between DALVANCE and cytochrome P450 (CYP450) substrates, inhibitors, or inducers [see Clinical Pharmacology (12.3)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy: Category C
There have been no adequate and well-controlled studies with dalbavancin in pregnant women. DALVANCE should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
No evidence of embryo or fetal toxicity was found in the rat or rabbit at a dose of 15 mg/kg/day (1.2 and 0.7 times the human dose on an exposure basis, respectively). Delayed fetal maturation was observed in the rat at a dose of 45 mg/kg/day (3.5 times the human dose on an exposure basis).
In a rat prenatal and postnatal development study, increased embryo lethality and increased offspring deaths during the first week post-partum were observed at a dose of 45 mg/kg/day (3.5 times the human dose on an exposure basis).
8.3 Nursing Mothers
Dalbavancin is excreted in the milk of lactating rats. It is not known whether dalbavancin or its metabolite is excreted in human milk; therefore, caution should be exercised when DALVANCE is administered to a nursing woman.
8.4 Pediatric Use
Safety and efficacy in pediatric patients have not been established.
8.5 Geriatric Use
Of the 1778 patients treated with DALVANCE in Phase 2 and 3 clinical trials, 313 patients (17.7%) were 65 years of age or older. The efficacy and tolerability of DALVANCE were similar to comparator regardless of age. The pharmacokinetics of dalbavancin were not significantly altered with age; therefore, no dosage adjustment is necessary based on age alone.
DALVANCE is substantially excreted by the kidney, and the risk of adverse reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection in this age group.
8.6 Renal Impairment
In patients with renal impairment whose known creatinine clearance is less than 30 mL/min and who are not receiving regularly scheduled hemodialysis, the recommended two-dose regimen for DALVANCE is 750 mg followed one week later by 375 mg. No dosage adjustment is recommended for patients receiving regularly scheduled hemodialysis, and DALVANCE can be administered without regard to the timing of hemodialysis [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dosage adjustment of DALVANCE is recommended for patients with mild hepatic impairment (Child-Pugh Class A). Caution should be exercised when prescribing dalbavancin to patients with moderate or severe hepatic impairment (Child-Pugh Class B or C) as no data are available to determine the appropriate dosing in these patients [see Clinical Pharmacology (12.3)].
10 OVERDOSAGE
Specific information is not available on the treatment of overdose with DALVANCE, as dose-limiting toxicity has not been observed in clinical studies. In Phase 1 studies, healthy volunteers have been administered single doses of up to 1500 mg, and cumulative doses of up to 4500 mg over a period of up to 8 weeks, with no signs of toxicity nor laboratory results of clinical concern.
Treatment of overdose with DALVANCE should consist of observation and general supportive measures. Although no information is available specifically regarding the use of hemodialysis to treat overdose, in a Phase 1 study in patients with renal impairment less than 6% of the recommended dalbavancin dose was removed [see Clinical Pharmacology (12.3)].
11 DESCRIPTION
DALVANCE (dalbavancin) for injection is a lipoglycopeptide synthesized from a fermentation product of Nonomuraea species.
Dalbavancin is a mixture of five closely related active homologs (A0, A1, B0, B1, and B2); the component B0 is the major component of dalbavancin. The homologues share the same core structure and differ in the fatty acid side chain of the N-acylaminoglucuronic acid moiety (R1) structure and/or the presence of an additional methyl group (R2) on the terminal amino group (shown in the figure and table below).

|
Dalbavancin |
R1 |
R2 |
Molecular Formula |
Molecular Weight* |
|
A0 |
CH(CH3)2 |
H |
C87H98N10O28Cl2 · 1.6 HCl |
1802.7 |
|
A1 |
CH2CH2CH3 |
H |
C87H98N10O28Cl2 · 1.6 HCl |
1802.7 |
|
B0 |
CH2CH(CH3)2 |
H |
C88H100N10O28Cl2 · 1.6 HCl |
1816.7 |
|
B1 |
CH2CH2CH2CH3 |
H |
C88H100N10O28Cl2 · 1.6 HCl |
1816.7 |
|
B2 |
CH2CH(CH3)2 |
CH3 |
C89H102N10O28Cl2 · 1.6 HCl |
1830.7 |
*Anhydrous free base
The B0 INN chemical name is: 5,31-dichloro-38-de(methoxycarbonyl)-7-demethyl-19-deoxy-56-O-[2-deoxy-2-[(10-methylundecanoyl)amino]-β-D-glucopyranuronosyl]-38-[[3-(dimethylamino)propyl] carbamoyl]-42-O-α-D-mannopyranosyl-15-N-methyl(ristomycin A aglycone) hydrochloride.
DALVANCE is supplied in clear glass vials as a sterile, lyophilized, preservative-free, white to off-white to pale yellow solid. Each vial contains dalbavancin HCl equivalent to 500 mg of anhydrous dalbavancin as the free base, plus lactose monohydrate (129 mg) and mannitol (129 mg) as excipients. Sodium hydroxide or hydrochloric acid may be added to adjust the pH at the time of manufacture. The powder is to be reconstituted and further diluted for IV infusion [see Dosage and Administration (2.3) and How Supplied/Storage and Handling (16)].
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Dalbavancin is an antibacterial drug [see Clinical Pharmacology (12.4)].
12.2 Pharmacodynamics
The antibacterial activity of dalbavancin appears to best correlate with the ratio of area under the concentration-time curve to minimal inhibitory concentration (AUC/MIC) for Staphylococcus aureus based on animal models of infection. An exposure-response analysis of a single study in patients with complicated skin and skin structure infections supports the two-dose regimen [see Dosage and Administration (2.1) and Clinical Pharmacology (12.3)].
Cardiac Electrophysiology: In a randomized, positive- and placebo-controlled, thorough QT/QTc study, 200 healthy subjects received dalbavancin 1000 mg IV, dalbavancin 1500 mg IV, oral moxifloxacin 400 mg, or placebo. Neither dalbavancin 1000 mg nor dalbavancin 1500 mg (supratherapeutic dose) had any clinically relevant adverse effect on cardiac repolarization.
12.3 Pharmacokinetics
Dalbavancin pharmacokinetic parameters have been characterized in healthy subjects, patients, and specific populations. Pharmacokinetic parameters following administration of a single intravenous 1000 mg dose were as shown in Table 3. The pharmacokinetics of dalbavancin can be described using a three-compartment model.
|
Parameter |
Single 1000 mg Dose |
|
Cmax (mg/L) |
287 (13.9)1 |
|
AUC0-24 (mg•h/L) |
3185 (12.8)1 |
|
AUC0-Day7 (mg•h/L) |
11160 (41.1)2 |
|
AUC0-inf (mg•h/L) |
23443 (40.9)2 |
|
Terminal t½ (h) |
346 (16.5)2,3 |
|
CL (L/h) |
0.0513 (46.8)2 |
|
All values are presented as mean (% coefficient of variation) |
|
In healthy subjects, dalbavancin AUC0-24h and Cmax both increased proportionally to dose following single IV dalbavancin doses ranging from 140 mg to 1500 mg, indicating linear pharmacokinetics.
The mean plasma concentration-time profile for dalbavancin at the recommended two-dose regimen of 1000 mg followed one week later by 500 mg is shown in Figure 2.

No apparent accumulation of dalbavancin was observed following multiple IV infusions administered once weekly for up to eight weeks, with 1000 mg on Day 1 followed by up to seven weekly 500 mg doses, in healthy adults with normal renal function.
Distribution: Dalbavancin is reversibly bound to human plasma proteins, primarily to albumin. The plasma protein binding of dalbavancin is approximately 93% and is not altered as a function of drug concentration, renal impairment, or hepatic impairment. The mean concentrations of dalbavancin achieved in skin blister fluid remain above 30 mg/L up to 7 days (approximately 146 hours) post dose, following 1000 mg IV dalbavancin. The mean ratio of the AUC0-144 hrs in skin blister fluid/AUC0-144 hrs in plasma is 0.60 (range 0.44 to 0.64).
Metabolism: In vitro studies using human microsomal enzymes and hepatocytes indicate that dalbavancin is not a substrate, inhibitor, or inducer of CYP450 isoenzymes. A minor metabolite of dalbavancin (hydroxy-dalbavancin) has been observed in the urine of healthy subjects. Quantifiable concentrations of the hydroxy-dalbavancin metabolite have not been observed in human plasma (lower limit of quantitation = 0.4 µg/mL) [see Drug Interactions (7.2)].
Excretion: Following administration of a single 1000 mg dose in healthy subjects, 20% of the dose was excreted in feces through 70 days post dose. An average of 33% of the administered dalbavancin dose was excreted in urine as unchanged dalbavancin and approximately 12% of the administered dose was excreted in urine as the metabolite hydroxy-dalbavancin through 42 days post dose.
Specific Populations
Renal Impairment:The pharmacokinetics of dalbavancin were evaluated in 28 subjects with varying degrees of renal impairment and in 15 matched control subjects with normal renal function. Following a single dose of 500 mg or 1000 mg dalbavancin, the mean plasma clearance (CLT) was reduced 11%, 35%, and 47% in subjects with mild (CLCR 50 to 79 mL/min), moderate (CLCR 30 to 49 mL/min), and severe (CLCR less than 30 mL/min), renal impairment, respectively, compared to subjects with normal renal function. The clinical significance of the decrease in mean plasma CLT, and the associated increase in AUC0-∞ noted in these pharmacokinetic studies of dalbavancin in subjects with severe renal impairment has not been established [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
No dosage adjustment is necessary for patients with CLCR greater than 30 mL/min or patients receiving hemodialysis. The recommended two-dose regimen for dalbavancin in patients with severe renal impairment who are not receiving regularly scheduled hemodialysis is 750 mg followed one week later by 375 mg.
Dalbavancin pharmacokinetic parameters in subjects with end-stage renal disease receiving regularly scheduled hemodialysis (three times/week) are similar to those observed in subjects with mild to moderate renal impairment, and less than 6% of an administered dose is removed after three hours of hemodialysis. Therefore, no dosage adjustment is recommended for patients receiving regularly scheduled hemodialysis, and dalbavancin may be administered without regard to the timing of hemodialysis in such patients [see Dosage and Administration (2.1) and Overdosage (10)].
Hepatic Impairment: The pharmacokinetics of dalbavancin were evaluated in 17 subjects with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B or C) and compared to those in nine matched healthy subjects with normal hepatic function. The mean AUC0-336 hrs was unchanged in subjects with mild hepatic impairment compared to subjects with normal hepatic function; however, the mean AUC0-336 hrs decreased 28% and 31% in subjects with moderate and severe hepatic impairment respectively, compared to subjects with normal hepatic function. The clinical significance of the decreased AUC0-336 hrs in subjects with moderate and severe hepatic function is unknown.
No dosage adjustment is recommended for patients with mild hepatic impairment. Caution should be exercised when prescribing dalbavancin to patients with moderate or severe hepatic impairment as no data are available to determine the appropriate dosing.
Gender: Clinically significant gender-related differences in dalbavancin pharmacokinetics have not been observed either in healthy subjects or in patients with infections. No dosage adjustment is recommended based on gender.
Geriatric Patients: Clinically significant age-related differences in dalbavancin pharmacokinetics have not been observed in patients with infections. No dosage adjustment is recommended based solely on age.
Pediatric Patients: The pharmacokinetics of dalbavancin in pediatric populations <12 years of age have not been established.
Drug Interactions
Nonclinical studies demonstrated that dalbavancin is not a substrate, inhibitor, or inducer of CYP450 isoenzymes. In a population pharmacokinetic analysis, dalbavancin pharmacokinetics were not affected by co‑administration with known CYP450 substrates, inducers or inhibitors, nor by individual medications including acetaminophen, aztreonam, fentanyl, metronidazole, furosemide, proton pump inhibitors (omeprazole, esomeprazole, pantoprazole, lansoprazole), midazolam, and simvastatin.
12.4 Microbiology
Mechanism of Action
Dalbavancin, a semisynthetic lipoglycopeptide, interferes with cell wall synthesis by binding to the D‑alanyl-D-alanine terminus of the stem pentapeptide in nascent cell wall peptidoglycan, thus preventing cross-linking. Dalbavancin is bactericidal in vitro against Staphylococcus aureus and Streptococcus pyogenes at concentrations similar to those sustained throughout treatment in humans treated according to the recommended dosage regimen.
Mechanism of Resistance
The development of bacterial isolates resistant to dalbavancin has not been observed, either in vitro, in studies using serial passage, or in animal infection experiments.
Interaction with Other Antimicrobials
When tested in vitro, dalbavancin demonstrated synergistic interactions with oxacillin and did not demonstrate antagonistic or synergistic interactions with any of the following antibacterial agents of various classes: gentamicin, vancomycin, levofloxacin, clindamycin, quinupristin/dalfopristin, linezolid, aztreonam, rifampin or daptomycin. The clinical significance of these in vitro findings is unknown.
Dalbavancin has been shown to be active against the following microorganisms, both in vitro and in clinical infections [see Indications and Usage (1)].
Gram-positive bacteria
Staphylococcus aureus (including methicillin-resistant isolates)
Streptococcus pyogenes
Streptococcus agalactiae
Streptococcus anginosus group (including S. anginosus, S. intermedius, S. constellatus)
The following in vitro data are available, but their clinical significance is unknown. In addition, at least 90% of organisms in the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the dalbavancin susceptible breakpoint of 0.12 mcg/mL. However, the safety and efficacy of dalbavancin in treating clinical infections due to these bacteria have not been established in adequate well-controlled clinical trials.
Gram-positive bacteria
Enterococcus
faecium (vancomycin-susceptible isolates only)
Enterococcus
faecalis (vancomycin-susceptible isolates only)
Susceptibility Test Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antimicrobial drug products used in resident hospitals to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting an antibacterial drug for treatment.
Dilution Techniques
Quantitative methods are used to determine minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized test method.1,2 When determining dalbavancin MICs, polysorbate-80 (P-80), should be added at a final concentration of 0.002% to freshly prepared or frozen microtiter trays. The MIC values should be interpreted according to the criteria provided in Table 4.
Diffusion Techniques
Dalbavancin disks for diffusion susceptibility testing are not available. Disk diffusion is not a reliable method for determining the in vitro activity of dalbavancin.
|
Pathogen |
MIC (mcg/mL)a | Zone Diameter (mm) | ||||
|
S |
I |
R |
S |
I |
R |
|
|
Staphylococcus aureus |
≤ 0.12 |
-- |
-- |
-- |
-- |
-- |
|
Streptococcus pyogenes, |
≤ 0.12 |
-- |
-- |
-- |
-- |
-- |
| a The current absence of data on resistant isolates precludes defining any category other than "Susceptible". If isolates yield MIC results other than susceptible, they should be submitted to a reference laboratory for additional testing. | ||||||
A report of "Susceptible" indicates that the antibacterial agent is likely to inhibit growth of the pathogen if the antibacterial compound reaches the concentrations at the infection site necessary to inhibit growth of the pathogen.
Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay, and the techniques of the individuals performing the test.1, 2 Standard dalbavancin powder should provide the following range of MIC values noted in Table 5.
|
Quality Control Strain |
MIC Range (µg/mL) |
|
Staphylococcus aureus ATCC ®29213 |
0.03-0.12 |
|
Streptococcus pneumoniae ATCC ®49619a |
0.008-0.03 |
|
Enterococcus faecalis ATCC®29212 |
0.03‑0.12 |
|
ATCC® = American Type Culture Collection |
|
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals to determine the carcinogenic potential of dalbavancin have not been conducted.
Dalbavancin was not genotoxic in a mammalian HGPRT gene mutation assay, an in vitro chromosome aberration assay in Chinese Hamster Ovary cells, or an in vivo mouse micronucleus assay.
Impaired fertility in the rat was not observed at a dose of 15 mg/kg/day (1.2 times the human dose on an exposure basis). Reductions in male and female fertility and increased embryo resorptions occurred at a dose of 45 mg/kg/day (3.5 times the human dose on an exposure basis), at which signs of parental toxicity were also observed.
13.2 Animal Toxicology and/or Pharmacology
Increases in serum levels of liver enzymes (ALT, AST), associated with microscopic findings in the liver were noted in toxicology studies in rats and dogs where dalbavancin was administered daily for 28 to 90 days. Hepatocellular necrosis was observed in dogs dosed at ≥10 mg/kg/day for longer than 2 months, i.e., at approximately 5 to 7 times the expected human dose on an exposure basis. Histiocytic vacuolation and hepatocyte necrosis were observed in rats dosed daily at 40 and 80 mg/kg/day, respectively, for 4 weeks, (approximately 3 and 6 times the expected human dose on an exposure basis, respectively). In addition, renal toxicity characterized by increases in serum BUN and creatinine and microscopic kidney findings was observed in rats and dogs at doses 5 to 7 times the expected human dose on an exposure basis. The relationship between these findings in the animal toxicology studies after 28 and 90 consecutive days of dosing to the indicated clinical dosing of 2 doses 7 days apart are unclear.
14 CLINICAL STUDIES
Acute Bacterial Skin and Skin Structure Infections: Adult patients with ABSSSI were enrolled in two Phase 3, randomized, double-blind, double-dummy clinical trials of similar design (Trial 1 and Trial 2). The Intent-to-Treat (ITT) population included 1,312 randomized patients. Patients were treated for two weeks with either a two-dose regimen of intravenous DALVANCE (1000 mg followed one week later by 500 mg) or intravenous vancomycin (1000 mg or 15 mg/kg every 12 hours, with the option to switch to oral linezolid after 3 days). DALVANCE-treated patients with creatinine clearance of less than 30 mL/min received 750 mg followed one week later by 375 mg. Approximately 5% of patients also received a protocol-specified empiric course of treatment with intravenous aztreonam for coverage of Gram-negative pathogens.
|
|
DALVANCE n/N (%) |
Vancomycin/Linezolid n/N (%) |
Difference (95%CI)3 |
|
Trial 1 |
240/288 (83.3%) |
233/285 (81.8%) |
1.5% (-4.6, 7.9) |
|
Trial 2 |
285/371 (76.8%) |
288/368 (78.3%) |
-1.5% (-7.4, 4.6) |
|
1 There were 7 patients who did not receive treatment and were counted as non-responders: 6 dalbavancin patients (3 in each trial) and one vancomycin/linezolid patient in Trial 2. 2 Patients who died or used non-study antibacterial therapy or had missing measurements were classified as non-responders. 3 The 95% Confidence Interval (CI) is computed using the Miettinen and Nurminen approach, stratified by baseline fever status. |
|||
The specific infections in these trials included cellulitis (approximately 50% of patients across treatment groups), major abscess (approximately 30%), and wound infection (approximately 20%). The median lesion area at baseline was 341 cm2. In addition to local signs and symptoms of infection, patients were also required to have at least one systemic sign of disease at baseline, defined as temperature 38°C or higher (approximately 85% of patients), white blood cell count greater than 12,000 cells/mm3 (approximately 40%), or 10% or more band forms on white blood cell differential (approximately 23%). Across both trials, 59% of patients were from Eastern Europe and 36% of patients were from North America. Approximately 89% of patients were Caucasian and 58% were males. The mean age was 50 years and the mean body mass index was 29.1 kg/m2.
The primary endpoint of these two ABSSSI trials was the clinical response rate where responders were defined as patients who had no increase from baseline in lesion area 48 to 72 hours after initiation of therapy, and had a temperature consistently at or below 37.6° C upon repeated measurement. Table 6 summarizes overall clinical response rates in these two ABSSSI trials using the pre‑specified primary efficacy endpoint in the ITT population.
|
DALVANCE
n/N (%) |
Vancomycin/Linezolid
n/N (%) |
Difference (95%CI)3 |
|
|
Trial 1 |
259/288 (89.9%) |
259/285 (90.9%) |
-1.0% (-5.7, 4.0) |
|
Trial 2 |
325/371 (87.6%) |
316/368 (85.9%) |
1.7% (-3.2, 6.7) |
|
1 There were 7 patients (as described in Table 6) who did not receive treatment and were counted as non-responders. 2 Patients who died or used non-study antibacterial therapy or had missing measurements were classified as non-responders. 3 The 95% CI is computed using the Miettinen and Nurminen approach, stratified by baseline fever status. |
|||
Another secondary endpoint in these two ABSSSI trials was the clinical success rate assessed at a follow-up visit occurring between Days 26 to 30. Clinical Success at this visit was defined as having a decrease in lesion size (both length and width measurements), a temperature of 37.6° C or lower, and meeting pre-specified criteria for local signs: purulent discharge and drainage absent or mild and improved from baseline, heat/warmth & fluctuance absent, swelling/induration & tenderness to palpation absent or mild. Table 8 summarizes clinical success rates at a follow-up visit for the ITT and clinically evaluable population in these two ABSSSI trials. Note that there are insufficient historical data to establish the magnitude of drug effect for antibacterial drugs compared with placebo at the follow-up visits. Therefore, comparisons of DALVANCE to vancomycin/linezolid based on clinical success rates at these visits cannot be utilized to establish non-inferiority.
|
DALVANCE n/N (%) |
Vancomycin/Linezolid n/N (%) |
Difference (95%CI)3 |
|
|
Trial 1 |
|||
|
ITT |
241/288 (83.7%) |
251/285 (88.1%) |
-4.4% (-10.1, 1.4) |
|
CE |
212/226 (93.8%) |
220/229 (96.1%) |
-2.3% (-6.6, 2.0) |
|
Trial 2 |
|||
|
ITT |
327/371 (88.1%) |
311/368 (84.5%) |
3.6% (-1.3, 8.7) |
|
CE |
283/294 (96.3%) |
257/272 (94.5%) |
1.8% (-1.8, 5.6) |
|
1 There were 7 patients (as described in Table 6) who did not receive treatment and were counted as failures in the ITT analysis. 2 Patients who died, used non-study antibacterial therapy, or had an unplanned surgical intervention 72 hours after the start of therapy were classified as Clinical Failures. 3 The 95% CI is computed using the Miettinen and Nurminen approach, stratified by baseline fever status. |
|||
Table 9 shows outcomes in patients with an identified baseline pathogen, using pooled data from Trials 1 and 2 in the microbiological ITT (microITT) population. The outcomes shown in the table are clinical response rates at 48 to 72 hours and clinical success rates at follow-up (Day 26 to 30), as defined above.
| Early Clinical Response at 48-72 hours | ||||||
| Early Responder2 | ≥ 20% reduction in lesion size | Clinical Success at Day 26 to 30 | ||||
|
Pathogen |
DALVANCE n/N (%) |
Comparator n/N (%) |
DALVANCE n/N (%) |
Comparator n/N (%) |
DALVANCE n/N (%) |
Comparator n/N (%) |
|
Staphylococcus aureus |
206/257 (80.2) |
219/256 (85.5) |
239/257 (93.0) |
232/256 (90.6) |
217/257 (84.4) |
229/256 (89.5) |
|
Streptococcus agalactiae |
6/12 (50.0) |
11/14 (78.6) |
10/12 (83.3) |
10/14 (71.4) |
10/12 (83.3) |
11/14 (78.6) |
|
Streptococcus pyogenes |
28/37 (75.7) |
24/36 (66.7) |
32/37 (86.5) |
27/36 (75.0) |
33/37 (89.2) |
32/36 (88.9) |
|
Streptococcus anginosus group |
18/22 (81.8) |
23/ 25 (92.0) |
21/22 (95.5) |
25/25 (100.0) |
21/22 (95.5) |
23/25 (92.0) |
|
1 There were 2 patients in the dalbavancin arm with methicillin-susceptible S. aureus at baselinewho did not receive treatment and were counted as non-responders/failures. |
||||||
15 REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antibiotic Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard—Ninth Edition. CLSI document M07-A9. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2012.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Third Informational Supplement. CLSI document M100-S23 Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2013.
16 HOW SUPPLIED/STORAGE AND HANDLING
DALVANCE (dalbavancin) for injection is supplied in the following packaging configuration:
500 mg/vial: package of 1 (NDC 57970-100-01)
Unreconstituted DALVANCE (dalbavancin) for injection should be stored at 25ºC (77ºF); excursions permitted to 15 to 30ºC (59 to 86ºF) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
Patients should be advised that allergic reactions, including serious allergic reactions, could occur, and that serious allergic reactions require immediate treatment. Patients should inform their healthcare provider about any previous hypersensitivity reactions to DALVANCE, or other glycopeptides.
Patients should be counseled that antibacterial drugs including DALVANCE should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When DALVANCE is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of treatment, and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by DALVANCE and other antibacterial drugs in the future.
Patients should be advised that diarrhea is a common problem caused by antibacterial drugs and usually resolves when the drug is discontinued. Sometimes, frequent watery or bloody diarrhea may occur and may be a sign of a more serious intestinal infection. If severe watery or bloody diarrhea develops, patients should contact their healthcare provider.
Rx only
Manufactured for: Durata Therapeutics U.S. Limited
Chicago, IL 60606
US Patent Numbers: Available online at http://www.duratatherapeutics.com/products/product-patents
DALVANCETM is a trademark of Durata Therapeutics Holding C.V.
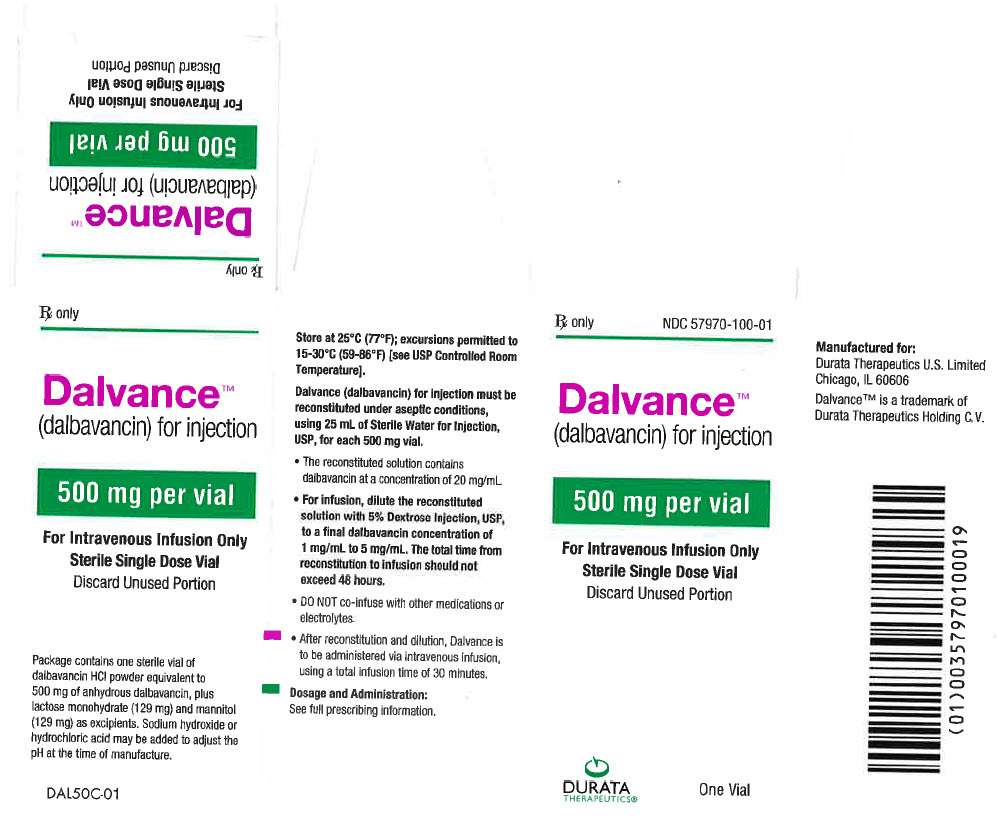
Principal Display Panel
NDC 57970-100-01
Dalvance
(dalbavancin) for injection
500 mg per vial
For Intravenous Infusion Only
Sterile Single Dose Vial
Dalbavancinanhydrous dalbavancin INJECTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||