Didanosine
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use didanosine delayed-release capsules safely and effectively. See full prescribing information for didanosine delayed-release capsules. Didanosine Delayed-Release Capsules (Enteric-Coated Beadlets) Initial U.S. Approval: 1991 RECENT MAJOR CHANGES(5.7)BOXED WARNINGWARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS See full prescribing information for complete boxed warning. Fatal and nonfatal pancreatitis. Didanosine delayed-release capsules should be suspended in patients with suspected pancreatitis and discontinued in patients with confirmed pancreatitis. (5.1) Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases. Fatal lactic acidosis has been reported in pregnant women who received the combination of didanosine and stavudine. (5.2) INDICATIONS AND USAGE(1)DOSAGE AND ADMINISTRATION Adult patients: Administered on an empty stomach. Dosing is based on body weight. (2.1) Pediatric patients: Ages 6 to 18 years, can safely swallow capsules and body weight at least 20 kg. Administered on an empty stomach, dosing is based on body weight. (2.1) Body Weight Dose 20 kg to less than 25 kg 200 mg once daily 25 kg to less than 60 kg 250 mg once daily at least 60 kg 400 mg once daily Renal impairment: Dose reduction is recommended. (2.2) Coadministration with tenofovir: Dose reduction is recommended. Patients should be monitored closely for didanosine-associated adverse reactions. (2.3, 7.1) DOSAGE FORMS AND STRENGTHS(3)CONTRAINDICATIONSCoadministration with allopurinol or ribavirin is contraindicated. (4.1 and 4.2) WARNINGS AND PRECAUTIONS Pancreatitis: Suspension or discontinuation of didanosine may be necessary. (5.1) Lactic acidosis and severe hepatomegaly with steatosis: Suspend didanosine in patients who develop clinical symptoms or signs with or without laboratory findings. (5.2) Hepatic toxicity: Interruption or discontinuation of didanosine must be considered upon worsening of liver disease. (5.3) Non-cirrhotic portal hypertension: Discontinue didanosine in patients with evidence of non-cirrhotic portal hypertension. (5.4) Patients may develop peripheral neuropathy (5.5), retinal changes and optic neuritis (5.6), immune reconstitution syndrome (5.7), and redistribution/accumulation of body fat. (5.8) Side Effects In adults, the most common adverse reactions (greater than 10%, all grades) are diarrhea, peripheral neurologic symptoms/neuropathy, nausea, headache, rash, and vomiting. (6.1) Adverse reactions in pediatric patients were consistent with those in adults. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Aurobindo Pharma USA, Inc. at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatchDRUG INTERACTIONSCoadministration of didanosine delayed-release capsules can alter the concentration of other drugs and other drugs may alter the concentration of didanosine. The potential drug-drug interactions must be considered prior to and during therapy. (4, 7, 12.3) USE IN SPECIFIC POPULATIONS5.28.1
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
- 1 DIDANOSINE INDICATIONS AND USAGE
- 2 DIDANOSINE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 DIDANOSINE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 DIDANOSINE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 DIDANOSINE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- Medication Guide
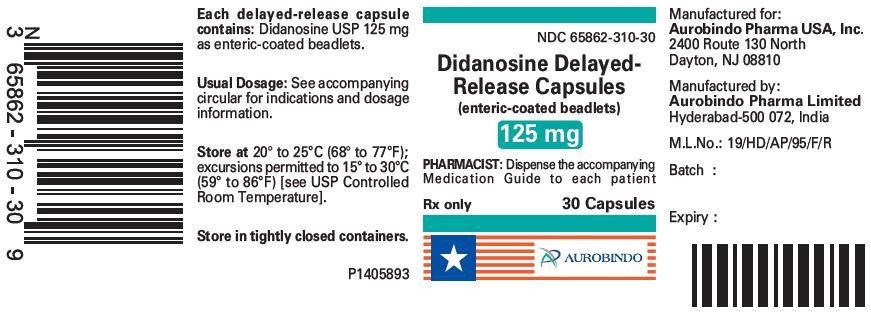
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 125 mg (30 Capsule Bottle)
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 125 mg Blister Carton (10 x 14 Unit-dose)
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 200 mg (30 Capsule Bottle)
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 200 mg Blister Carton (10 x 10 Unit-dose)
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 250 mg (30 Capsule Bottle)
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 250 mg Blister Carton (10 x 10 Unit-dose)
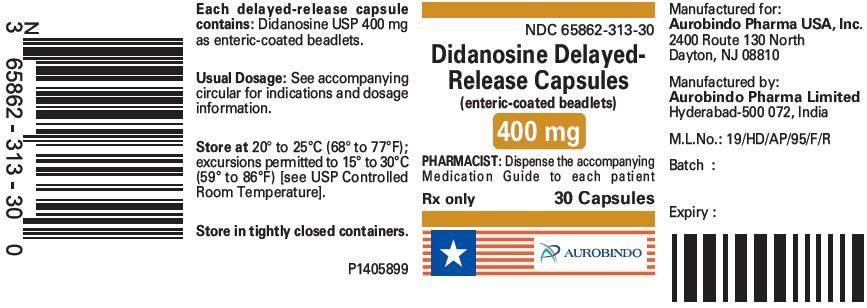
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 400 mg (30 Capsule Bottle)
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 400 mg Blister Carton (10 x 5 Unit-dose)
FULL PRESCRIBING INFORMATION
WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. Didanosine delayed-release capsules should be suspended in patients with suspected pancreatitis and discontinued in patients with confirmed pancreatitis [see Warnings and Precautions (5.1)].
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. Fatal lactic acidosis has been reported in pregnant women who received the combination of didanosine and stavudine with other antiretroviral agents. The combination of didanosine and stavudine should be used with caution during pregnancy and is recommended only if the potential benefit clearly outweighs the potential risk [see Warnings and Precautions (5.2)].
1 INDICATIONS AND USAGE
[see Clinical Studies (14) ]
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage (Adult and Pediatric Patients)
| Body Weight | Dose |
|---|---|
| 20 kg to less than 25 kg |
200 mg once daily |
| 25 kg to less than 60 kg |
250 mg once daily |
| at least 60 kg |
400 mg once daily |
2.2 Renal Impairment
Adult Patients
| Creatinine Clearance (mL/min) |
Dosage (mg) | |
|---|---|---|
| at least 60 kg | less than 60 kg | |
|
a Based on studies using a buffered formulation of didanosine. b Not suitable for use in patients less than 60 kg with CLcr less than 10 mL/min. An alternate formulation of didanosine should be used. |
||
| at least 60 30-59 10-29 less than 10 |
400 once daily 200 once daily 125 once daily 125 once daily |
250 once daily 125 once daily 125 once daily b |
Pediatric Patients
Patients Requiring Continuous Ambulatory Peritoneal Dialysis (CAPD) or Hemodialysis
2.3 Dose Adjustment
Concomitant Therapy with Tenofovir Disoproxil Fumarate
[see Drug Interactions (7) and Clinical Pharmacology (12.3)].
Hepatic Impairment
[see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)].
3 DOSAGE FORMS AND STRENGTHS
- 125 mg are white / white size ‘3’ hard gelatin capsules imprinted with ‘D’ on white cap and ‘70’ on white body with black edible ink filled with white to off-white beadlets.
- 200 mg are white / white size ‘1’ hard gelatin capsules imprinted with ‘D’ on white cap and ‘69’ on white body with black edible ink filled with white to off-white beadlets.
- 250 mg are white / white size ‘0’ hard gelatin capsules imprinted with ‘D’ on white cap and ‘10’ on white body with black edible ink filled with white to off-white beadlets.
- 400 mg are white / white size ‘00’ hard gelatin capsules imprinted with ‘D’ on white cap and ‘09’ on white body with black edible ink filled with white to off-white beadlets.
4 CONTRAINDICATIONS
4.1 Allopurinol
[see Clinical Pharmacology (12.3)]
4.2 Ribavirin
5 WARNINGS AND PRECAUTIONS
5.1 Pancreatitis
Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. Didanosine delayed-release capsules should be suspended in patients with signs or symptoms of pancreatitis and discontinued in patients with confirmed pancreatitis. Patients treated with didanosine delayed-release capsules in combination with stavudine may be at increased risk for pancreatitis.
[See Adverse Reactions (6).]
5.2 Lactic Acidosis/Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals.[see Use in Specific Populations (8.1)].
5.3 Hepatic Toxicity
[See Adverse Reactions (6).]
5.4 Non-cirrhotic Portal Hypertension
5.5 Peripheral Neuropathy
[See Adverse Reactions (6).]
5.6 Retinal Changes and Optic Neuritis
[see Adverse Reactions (6)].
5.7 Immune Reconstitution Syndrome
Mycobacterium avium Pneumocystis jiroveci
5.8 Fat Redistribution
6 ADVERSE REACTIONS
- Pancreatitis [see Boxed Warning, Warnings and Precautions (5.1)]
- Lactic acidosis/severe hepatomegaly with steatosis [see Boxed Warning, Warnings and Precautions (5.2)]
- Hepatic toxicity [see Warnings and Precautions (5.3)]
- Non-cirrhotic portal hypertension [see Warnings and Precautions (5.4)]
- Peripheral neuropathy [see Warnings and Precautions (5.5)]
- Retinal changes and optic neuritis [see Warnings and Precautions (5.6)]
6.1 Clinical Trials Experience
Adults
| Adverse Reactions | Percent of Patientsb,c | |
|---|---|---|
| didanosine delayed-release capsules + stavudine + nelfinavir n=258 |
zidovudine/lamivudined + nelfinavir n=253 |
|
|
a Median duration of treatment was 62 weeks in the didanosine delayed-release capsules + stavudine + nelfinavir group and 61 weeks in the zidovudine/lamivudine + nelfinavir group. b Percentages based on treated patients. c The incidences reported included all severity grades and all reactions regardless of causality. d Zidovudine/lamivudine combination tablet. * This event was not observed in this study arm. |
||
| Diarrhea Peripheral Neurologic Symptoms/Neuropathy Nausea Headache Rash Vomiting Pancreatitis (see below) |
57 25 24 22 14 14 less than 1 |
58 11 36 17 12 19 * |
[see Warnings and Precautions (5)]
| Percent of Patientsb | ||||
|---|---|---|---|---|
| didanosine delayed-release capsules + stavudine + nelfinavir n=258 |
zidovudine/lamivudinec
+ nelfinavir n=253 |
|||
| Parameter | Grades 3 to 4d | All Grades | Grades 3 to 4d | All Grades |
|
a Median duration of treatment was 62 weeks in the didanosine delayed-release capsules + stavudine + nelfinavir group and 61 weeks in the zidovudine/lamivudine + nelfinavir group. b Percentages based on treated patients. c Zidovudine/lamivudine combination tablet. d Greater than 5 x ULN for SGOT and SGPT, at least 2.1 x ULN for lipase, and at least 2.6 x ULN for bilirubin (ULN = upper limit of normal). |
||||
| SGOT (AST) SGPT (ALT) Lipase Bilirubin |
5 6 5 less than 1 |
46 44 23 9 |
5 5 2 less than 1 |
19 22 13 3 |
Pediatric Patients
22 2[see Clinical Studies (14)].
6.2 Postmarketing Experience
Blood and Lymphatic System Disorders
Body as a Whole [see Warnings and Precautions (5.8) ].
Digestive Disorders
Exocrine Gland Disorders [see Warnings and Precautions (5.1) ]
Hepatobiliary Disorders [see Warnings and Precautions (5.2)]; [see Warnings and Precautions (5.4)];
Metabolic Disorders
Musculoskeletal Disorders
Ophthalmologic Disorders [see Warnings and Precautions (5.6) ].
Use with Stavudine- and Hydroxyurea-Based Regimens
[see Warnings and Precautions (5)]
7 DRUG INTERACTIONS
7.1 Established Drug Interactions
[see Contraindications (4.1 and 4.2), Clinical Pharmacology (12.3)].
| Drug | Effect | Clinical Comment |
|---|---|---|
| ↑ Indicates increase. ↓ Indicates decrease. a Coadministration of didanosine with food decreases didanosine concentrations. Thus, although not studied, it is possible that coadministration with heavier meals could reduce didanosine concentrations further. |
||
|
ganciclovir |
↑ didanosine concentration |
If there is no suitable alternative to ganciclovir, then use in combination with didanosine delayed-release capsules with caution. Monitor for didanosine- associated toxicity. |
|
methadone |
↓ didanosine concentration |
If coadministration of methadone and didanosine is necessary, the recommended formulation of didanosine is didanosine delayed-release capsules. Patients should be closely monitored for adequate clinical response when didanosine delayed-release capsules is coadministered with methadone, including monitoring for changes in HIV RNA viral load. Do not coadminister methadone with didanosine pediatric powder due to significant decreases in didanosine concentrations. |
|
nelfinavir |
No interaction 1 hour after didanosine |
Administer nelfinavir 1 hour after didanosine delayed-release capsules. |
|
tenofovir disoproxil fumarate |
↑ didanosine concentration |
A dose reduction of didanosine delayed-release capsules to the following dosage once daily taken together with tenofovir disoproxil fumarate and a light meal (400 kcalories or less and 20% fat or less) or in the fasted state is recommended.a
|
see Clinical Pharmacokinetics (12.3, Tables 9 and 10) [see Dosage and Administration (2.3), Warnings and Precautions (5)]
7.2 Predicted Drug Interactions
| Drug or Drug Class | Effect | Clinical Comment |
|---|---|---|
| ↑ Indicates increase. a Only if other drugs are not available and if clearly indicated. If treatment with life-sustaining drugs that cause pancreatic toxicity is required, suspension of didanosine delayed-release capsules is recommended [see Warnings and Precautions (5.1)]. b [See Warnings and Precautions (5.6).] |
||
|
Drugs that may cause pancreatic toxicity |
↑ risk of pancreatitis |
Use only with extreme caution.a |
|
Neurotoxic drugs |
↑ risk of neuropathy |
Use with caution.b |
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category B
p
[see Warnings and Precautions (5.2)]. The combination of didanosine and stavudine should be used with caution during pregnancy and is recommended only if the potential benefit clearly outweighs the potential risk.
Antiretroviral Pregnancy Registry
8.3 Nursing Mothers
The Centers for Disease Control and Prevention recommend that HIV-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV.mothers should be instructed not to breastfeed if they are receiving didanosine.
8.4 Pediatric Use
[see Dosage and Administration (2), Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)].
8.5 Geriatric Use
[see Warnings and Precautions (5.1)]. [see Dosage and Administration (2.2)].
8.6 Renal Impairment
[see Clinical Pharmacology (12.3)]. [see Dosage and Administration (2)].
10 OVERDOSAGE
[see Clinical Pharmacology (12.3)].
11 DESCRIPTION

101243
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
[see Clinical Pharmacology (12.4)].
12.3 Pharmacokinetics
in vitro in vitro
|
Parametera |
Pediatrics | Adults | ||
|---|---|---|---|---|
| 20 kg to less than 25 kg n=10 |
25 kg to less than 60 kg n=17 |
At least 60 kg n=7 |
At least 60 kg n=44 |
|
| a The pharmacokinetic parameters (mean ± standard deviation) of didanosine were determined by a population pharmacokinetic model based on combined clinical studies. |
||||
| Apparent clearance (L/h) Apparent volume of distribution (L) Elimination half-life (h) Steady-state AUC (mg•h/L) |
89.5 ± 21.6 98.1 ± 30.2 0.75 ± 0.13 2.38 ± 0.66 |
116.2 ± 38.6 154.7 ± 55 0.92 ± 0.09 2.36 ± 0.7 |
196 ± 55.8 363 ± 137.7 1.26 ± 0.19 2.25 ± 0.89 |
174.5 ± 69.7 308.3 ± 164.3 1.19 ± 0.21 2.65 ± 1.07 |
Comparison of Didanosine Formulations
maxmax
Effect of Food
max[see Dosage and Administration (2)].
Special Populations
Renal Insufficiency: [See Dosage and Administration (2.2).]
| Parameter | Creatinine Clearance (mL/min) | Dialysis Patients n=11 |
|||
|---|---|---|---|---|---|
| at least 90 n=12 |
60-90 n=6 |
30-59 n=6 |
10-29 n=3 |
||
| ND = not determined due to anuria. CLcr = creatinine clearance. CL/F = apparent oral clearance. CLR= renal clearance. |
|||||
| CLcr (mL/min) CL/F (mL/min) CLR (mL/min) T½ (h) |
112 ± 22 2164 ± 638 458 ± 164 1.42 ± 0.33 |
68 ± 8 1566 ± 833 247 ± 153 1.59 ± 0.13 |
46 ± 8 1023 ± 378 100 ± 44 1.75 ± 0.43 |
13 ± 5 628 ± 104 20 ± 8 2 ± 0.3 |
ND 543 ± 174 less than 10 4.1 ± 1.2 |
Hepatic Impairment:maxmax[See Dosage and Administration (2.3).]
Pediatric Patients:
[see Dosage and Administration (2)].
Geriatric Patients: [see Use in Specific Populations (8.5)].
Gender:
Drug Interactions
max Dosage and Administration (2.3) Drug Interactions (7.1)
|
Drug |
Didanosine Dosage |
n |
% Change of Didanosine Pharmacokinetic Parametersa |
|
|---|---|---|---|---|
| AUC of Didanosine (90% CI) |
Cmax of Didanosine (90% CI) |
|||
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 90% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b All studies conducted in healthy volunteers at least 60 kg with creatinine clearance of at least 60 mL/min. c Tenofovir disoproxil fumarate. d 373 kcalories, 8.2 grams fat. e Compared with didanosine delayed-release capsules 250 mg administered alone under fasting conditions. f Compared with didanosine delayed-release capsules 400 mg administered alone under fasting conditions. g Comparisons are made to historical controls (n=148, pooled from 5 studies) conducted in healthy subjects. The number of subjects evaluated for AUC and Cmax is 15 and 16, respectively. |
||||
|
tenofovir,
b,c 300 mg once daily with a light meald |
400 mg single dose fasting 2 hours before tenofovir |
26 |
↑ 48% (31, 67%) |
↑ 48% (25, 76%) |
|
tenofovir,
b,c 300 mg once daily with a light meald |
400 mg single dose with tenofovir and a light meal |
25 |
↑ 60% (44, 79%) |
↑ 64% (41, 89%) |
|
tenofovir,
b,c 300 mg once daily with a light meald |
200 mg single dose with tenofovir and a light meal |
33 |
↑ 16% (6, 27%)e |
↓ 12% (-25, 3%)e |
| |
250 mg single dose with tenofovir and a light meal |
33 |
↔ (-13, 5%)f |
↓ 20% (-32, -7%)f |
| 325 mg single dose with tenofovir and a light meal |
33 |
↑ 13% (3, 24%)f |
↓ 11% (-24, 4%)f |
|
|
methadone, chronic maintenance dose |
400 mg single dose |
15, 16g
|
↓ 17% (-29, -2%) |
↓ 16% (-33, 4%) |
| Drug | Didanosine Dosage | n | % Change of Coadministered Drug Pharmacokinetic Parametersa,b |
|
|---|---|---|---|---|
| AUC of Coadministered Drug (90% CI) |
Cmax of Coadministered Drug (90% CI) |
|||
| ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 90% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b All studies conducted in healthy volunteers at least 60 kg with creatinine clearance of at least 60 mL/min. c Tenofovir disoproxil fumarate. d 373 kcalories, 8.2 grams fat. |
||||
| ciprofloxacin, 750 mg single dose |
400 mg single dose |
16 |
↔ |
↔ |
| indinavir, 800 mg single dose |
400 mg single dose |
23 |
↔ |
↔ |
| ketoconazole, 200 mg single dose |
400 mg single dose |
21 |
↔ |
↔ |
| tenofovir,c 300 mg once daily with a light meald |
400 mg single dose fasting 2 hours before tenofovir |
25 |
↔ |
↔ |
| tenofovir,c 300 mg once daily with a light meald |
400 mg single dose with tenofovir and a light meal |
25 |
↔ |
↔ |
Didanosine Buffered Formulations: max Dosage and Administration (2.3 for Concomitant Therapy with Tenofovir Disoproxil Fumarate), Contraindications (4.1), Drug Interactions (7.1)
| Drug | Didanosine Dosage | n | % Change of Didanosine Pharmacokinetic Parametersa |
|
|---|---|---|---|---|
| AUC of Didanosine (95% CI) |
Cmax of Didanosine (95% CI) |
|||
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. aThe 95% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b 90% CI. c HIV-infected patients. NA = Not available. |
||||
|
allopurinol, renally impaired, 300 mg/day |
200 mg single dose |
2 |
↑ 312% |
↑ 232% |
| healthy volunteer, 300 mg/day for 7 days |
400 mg single dose |
14 |
↑ 113% |
↑ 69% |
|
ganciclovir, 1000 mg every 8 hours, 2 hours after didanosine |
200 mg every 12 hours |
12 |
↑ 111% |
NA |
| ciprofloxacin, 750 mg every 12 hours for 3 days, 2 hours before didanosine |
200 mg every 12 hours for 3 days |
8c
|
↓ 16% |
↓ 28% |
| indinavir, 800 mg single dose simultaneous |
200 mg single dose |
16 |
↔ |
↔ |
| 1 hour before didanosine |
200 mg single dose |
16 |
↓ 17% (-27, -7%)b |
↓ 13% (-28, 5%)b |
| ketoconazole, 200 mg/day for 4 days, 2 hours before didanosine |
375 mg every 12 hours for 4 days |
12c
|
↔ |
↓12% |
| loperamide, 4 mg every 6 hours for 1 day |
300 mg single dose |
12c
|
↔ |
↓23% |
| metoclopramide, 10 mg single dose |
300 mg single dose |
12c
|
↔ |
↑13% |
| ranitidine, 150 mg single dose, 2 hours before didanosine |
375 mg single dose |
12c
|
↑14% |
↑13% |
| rifabutin, 300 or 600 mg/day for 12 days |
167 or 250 mg every 12 hours for 12 days |
11 |
↑ 13% (-1, 27%) |
↑ 17% (-4, 38%) |
| ritonavir, 600 mg every 12 hours for 4 days |
200 mg every 12 hours for 4 days |
12 |
↓ 13% (0, 23%) |
↓ 16% (5, 26%) |
| stavudine, 40 mg every 12 hours for 4 days |
100 mg every 12 hours for 4 days |
10 |
↔ |
↔ |
| sulfamethoxazole, 1000 mg single dose |
200 mg single dose |
8c
|
↔ |
↔ |
| trimethoprim, 200 mg single dose |
200 mg single dose |
8c
|
↔ |
↑ 17% (-23, 77%) |
| zidovudine, 200 mg every 8 hours for 3 days |
200 mg every 12 hours for 3 days |
6c
|
↔ |
↔ |
| Drug | Didanosine Dosage | n | % Change of Coadministered Drug Pharmacokinetic Parametersa |
|
|---|---|---|---|---|
| AUC of Coadministered Drug (95% CI) |
Cmax of Coadministered Drug (95% CI) |
|||
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 95% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b HIV-infected patients. NA = Not available. |
||||
| dapsone, 100 mg single dose |
200 mg every 12 hours for 14 days |
6b
|
↔ |
↔ |
| ganciclovir, 1000 mg every 8 hours, 2 hours after didanosine |
200 mg every 12 hours |
12b
|
↓21% |
NA |
|
nelfinavir, 750 mg single dose, 1 hour after didanosine |
200 mg single dose |
10b
|
↑12% |
↔ |
| ranitidine, 150 mg single dose, 2 hours before didanosine |
375 mg single dose |
12b
|
↓16% |
↔ |
| ritonavir, 600 mg every 12 hours for 4 days |
200 mg every 12 hours for 4 days |
12 |
↔ |
↔ |
| stavudine, 40 mg every 12 hours for 4 days |
100 mg every 12 hours for 4 days |
10b
|
↔ |
↑17% |
| sulfamethoxazole, 1000 mg single dose |
200 mg single dose |
8b
|
↓ 11% (-17, -4%) |
↓ 12% (-28, 8%) |
| trimethoprim, 200 mg single dose |
200 mg single dose |
8b
|
↑ 10% (-9, 34%) |
↓ 22% (-59, 49%) |
| zidovudine, 200 mg every 8 hours for 3 days |
200 mg every 12 hours for 3 days |
6b
|
↓ 10% (-27, 11%) |
↓ 16.5% (-53, 47%) |
12.4 Microbiology
Mechanism of Action
Antiviral Activity in Cell Culture
50
Resistance
Cross-resistance
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Escherichia coli in vitro in vitro in vitro Salmonella in vivo
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Adult Patients
331010

| Outcome | Percent of Patients with HIV-1 RNA less than 400 copies/mL (less than 50 copies/mL) |
|
|---|---|---|
| didanosine delayed-release capsules + stavudine + nelfinavir n=258 |
zidovudine/lamivudinea
+ nelfinavir n=253 |
|
|
a Zidovudine/lamivudine combination tablet. b Corresponds to rates at Week 48 in Figure 1. c Subjects achieved and maintained confirmed HIV-1 RNA less than 400 copies/mL (less than 50 copies/mL) through Week 48. d Includes viral rebound at or before Week 48 and failure to achieve confirmed HIV-1 RNA less than 400 copies/mL (less than 50 copies/mL) through Week 48. e Includes lost to follow-up, subject’s withdrawal, discontinuation due to physician’s decision, never treated, and other reasons. |
||
| Responderb,c
|
55% (33%) |
56% (33%) |
| Virologic failured
|
22% (45%) |
21% (43%) |
| Death or discontinued due to disease progression |
1% (1%) |
2% (2%) |
| Discontinued due to adverse event |
6% (6%) |
7% (7%) |
| Discontinued due to other reasonse |
16% (16%) |
15% (16%) |
14.2 Pediatric Patients
22 22
16 HOW SUPPLIED/STORAGE AND HANDLING
Didanosine Delayed-Release Capsules, 125 mg
Didanosine Delayed-Release Capsules, 200 mg
Didanosine Delayed-Release Capsules, 250 mg
Didanosine Delayed-Release Capsules, 400 mg
Store at
17 PATIENT COUNSELING INFORMATION
See Medication Guide.
17.1 Pancreatitis
17.2 Peripheral Neuropathy
17.3 Lactic Acidosis and Severe Hepatomegaly with Steatosis
17.4 Hepatic Toxicity
17.5 Non-cirrhotic Portal Hypertension
17.6 Retinal Changes and Optic Neuritis
17.7 Fat Redistribution
17.8 Concomitant Therapy
17.9 General Information
- Do not share needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
- Do not have any kind of sex without protection. Always practice safe sex by using a latex or polyurethane condom or other barrier method to lower the chance of sexual contact with semen, vaginal secretions, or blood.
- Do not breastfeed. It is not known if didanosine can be passed to your baby in your breast milk and whether it could harm your baby. Also, mothers with HIV-1 should not breastfeed because HIV-1 can be passed to the baby in breast milk.
Aurobindo Pharma USA, Inc.
Aurobindo Pharma Limited
Medication Guide
Didanosine Delayed-Release Capsules
(didanosine, also known as ddI)
Enteric-Coated Beadlets
What is the most important information I should know about didanosine delayed-release capsules?
Didanosine delayed-release capsules may cause serious side effects, including:
Swelling of your pancreas (pancreatitis) that may cause death. Pancreatitis can happen at any time during your treatment with didanosine delayed-release capsules.
- have had pancreatitis
- have advanced HIV (human immunodeficiency virus) infection
- have kidney problems
- drink alcoholic beverages
- take a medicine called ZERIT® (stavudine)
It is important to call your healthcare provider right away if you have:
- stomach pain
- swelling of your stomach
- nausea and vomiting
- fever
Build-up of acid in your blood (lactic acidosis). Lactic acidosis must be treated in the hospital as it may cause death.
- have liver problems
- are pregnant. There have been deaths reported in pregnant women who get lactic acidosis after taking didanosine delayed-release capsules and ZERIT (stavudine).
- are overweight
- have been treated for a long time with other medicines to treat HIV
It is important to call your healthcare provider right away if you:
- feel weak or tired
- have unusual (not normal) muscle pain
- have trouble breathing
- have stomach pain with nausea and vomiting
- feel cold, especially in your arms and legs
- feel dizzy or light-headed
- have a fast or irregular heartbeat
Liver problems.
It is important to call your healthcare provider right away if you have:
- yellowing of your skin or the white of your eyes (jaundice)
- dark urine
- pain on the right side of your stomach
- swelling of your stomach
- easy bruising or bleeding
- loss of appetite
- nausea or vomiting
- vomiting blood or dark colored stools (bowel movements)
What are didanosine delayed-release capsules?
Who should not take didanosine delayed-release capsules?
Do not take didanosine delayed-release capsules if you take:
- ZYLOPRIM®, LOPURIN®, ALOPRIM® (allopurinol)
- COPEGUS®, REBETOL®, RIBASPHERE®, RIBAVIRIN®, VIRAZOLE® (ribavirin)
What should I tell my healthcare provider before taking didanosine delayed-release capsules?
- have or had kidney problems
- have or had liver problems (such as hepatitis)
- have or had persistent numbness, tingling, or pain in the hands or feet (neuropathy)
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if didanosine delayed-release capsules will harm your unborn baby. Tell your healthcare provider right away if you become pregnant while taking didanosine delayed-release capsules. You and your healthcare provider will decide if you should take didanosine delayed-release capsules while you are pregnant.
Pregnancy Registry: There is a pregnancy registry for women who take antiviral medicines during pregnancy. The purpose of the registry is to collect information about the health of you and your baby. Talk to your doctor about how you can take part in this registry. - are breastfeeding or plan to breastfeed. Do not breastfeed. It is not known if didanosine can be passed to your baby in your breast milk and whether it could harm your baby. Also, mothers with HIV-1 should not breastfeed because HIV-1 can be passed to the baby in the breast milk.
Tell your healthcare provider about all the medicines you take
Especially tell your healthcare provider if you take:
- CYTOVENE®, VALCYTE® (ganciclovir)
- DOLOPHINE® HYDROCHLORIDE, METHADOSE® (methadone)
- VIRACEPT® (nelfinavir)
- VIREAD® (tenofovir disoproxil fumarate)
- alcoholic beverages
How should I take didanosine delayed-release capsules?
- Take didanosine delayed-release capsules exactly as your healthcare provider tells you to take them.
- Your healthcare provider will tell you how much didanosine delayed-release capsules to take and when to take them.
- Your healthcare provider may change your dose. Do not change your dose of didanosine delayed-release capsules without talking to your healthcare provider.
- Do not take didanosine delayed-release capsules with food. Take didanosine delayed-release capsules on an empty stomach.
- Take didanosine delayed-release capsules whole. Do not break, crush, dissolve, or chew didanosine delayed-release capsules before swallowing. If you cannot swallow didanosine delayed-release capsules whole, tell your healthcare provider. You may need a different medicine.
- Try not to miss a dose, but if you do, take it as soon as possible. If it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule.
- Some medicines should not be taken at the same time of day that you take didanosine delayed-release capsules. Check with your healthcare provider.
- If your kidneys are not working well, your healthcare provider will need to do regular blood and urine tests to check how they are working while you take didanosine delayed-release capsules. Your healthcare provider may also lower your dosage of didanosine delayed-release capsules if your kidneys are not working well.
- If you take too much didanosine delayed-release capsules, contact a poison control center or emergency room right away.
What should I avoid while taking didanosine delayed-release capsules?
- Alcohol. Do not drink alcohol while taking didanosine delayed-release capsules. Alcohol may increase your risk of getting pain and swelling of your pancreas (pancreatitis) or may damage your liver.
What are the possible side effects of didanosine delayed-release capsules?
“What is the most important information I should know about didanosine delayed-release capsules?”
- Vision changes. You should have regular eye exams while taking didanosine delayed-release capsules.
- Peripheral neuropathy. Symptoms include: numbness, tingling, or pain in your hands or feet. This condition is more likely to happen in people who have had it before, in patients taking medicines that affect the nerves, and in people with advanced HIV disease. A child may not notice these symptoms. Ask the child’s healthcare provider for the signs and symptoms of peripheral neuropathy in children.
- Changes in your immune system (immune reconstitution syndrome). Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Tell your healthcare provider if you start having new or worse symptoms of infection after you start taking HIV medicine.
-
Changes in body fat (fat redistribution). Changes in body fat have been seen in people who take antiretroviral medicines. These changes may include:
- more fat in or around your
- less fat in your
- diarrhea
- stomach pain
- nausea
- vomiting
- headache
- rash
How should I store didanosine delayed-release capsules?
- Store didanosine delayed-release capsules in a tightly closed container between 15º to 30ºC (59º to 86ºF).
- Safely throw away any unused didanosine delayed-release capsules.
Keep didanosine delayed-release capsules and all medicines out of the reach of children and pets.
General information about the safe and effective use of didanosine delayed-release capsules
- Do not share needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
- Do not have any kind of sex without protection. Always practice safe sex by using a latex or polyurethane condom or other barrier method to lower the chance of sexual contact with semen, vaginal secretions, or blood.
What are the ingredients in didanosine delayed-release capsules?
Active Ingredient:
Inactive Ingredients:
Aurobindo Pharma USA, Inc.
Aurobindo Pharma Limited
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 125 mg (30 Capsule Bottle)
NDC 65862-310-30
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
125 mg
PHARMACIST:
Rx only 30 Capsules
AUROBINDO
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 125 mg Blister Carton (10 x 14 Unit-dose)
NDC 65862-310-14
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
125 mg
PHARMACIST:
Rx only 140 Unit-dose Capsules (10 x 14s)
AUROBINDO

PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 200 mg (30 Capsule Bottle)
NDC 65862-311-30
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
200 mg
PHARMACIST:
Rx only 30 Capsules
AUROBINDO

PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 200 mg Blister Carton (10 x 10 Unit-dose)
NDC 65862-311-10
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
200 mg
PHARMACIST:
Rx only 100 Unit-dose Capsules (10 x 10s)
AUROBINDO

PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 250 mg (30 Capsule Bottle)
NDC 65862-312-30
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
250 mg
PHARMACIST:
Rx only 30 Capsules
AUROBINDO

PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 250 mg Blister Carton (10 x 10 Unit-dose)
NDC 65862-312-10
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
250 mg
PHARMACIST:
Rx only 100 Unit-dose Capsules (10 x 10s)
AUROBINDO

PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 400 mg (30 Capsule Bottle)
NDC 65862-313-30
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
400 mg
PHARMACIST:
Rx only 30 Capsules
AUROBINDO
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 400 mg Blister Carton (10 x 5 Unit-dose)
NDC 65862-313-50
Didanosine Delayed-Release Capsules
(enteric-coated beadlets)
400 mg
PHARMACIST:
Rx only 50 Unit-dose Capsules (10 x 5s)
AUROBINDO

DidanosineDidanosine CAPSULE, DELAYED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
DidanosineDidanosine CAPSULE, DELAYED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
DidanosineDidanosine CAPSULE, DELAYED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
DidanosineDidanosine CAPSULE, DELAYED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
PLEASE, BE CAREFUL!
Be sure to consult your doctor before taking any medication!