Didanosine
State of Florida DOH Central Pharmacy
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Didanosine Delayed-Release Capsules Enteric-Coated Pellets safely and effectively. See full prescribing information for Didanosine Delayed-Release Capsules Enteric-Coated Pellets. Initial U.S. Approval: 1991RECENT MAJOR CHANGESDosage and Administration (2) 09/2008Contraindications Allopurinol (4.1 ) 06/2009 Ribavirin (4.2 ) 06/2009BOXED WARNINGWARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS See full prescribing information for complete boxed warning Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. Didanosine delayed-release capsules should be suspended in patients with suspected pancreatitis and discontinued in patients with confirmed pancreatitis [see Warnings and Precautions (5.1 )]. Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. Fatal lactic acidosis has been reported in pregnant women who received the combination of didanosine and stavudine with other antiretroviral agents. The combination of didanosine and stavudine should be used with caution during pregnancy and is recommended only if the potential benefit clearly outweighs the potential risk [see Warnings and Precautions (5.2)]. INDICATIONS AND USAGEDidanosine delayed-release capsules are a nucleoside reverse transcriptase inhibitor for use in combination with other antiretroviral agents for the treatment of human immunodeficiency virus (HIV)-1 infection. (1)DOSAGE AND ADMINISTRATION Adult patients: Administered on an empty stomach. Dosing is based on body weight. (2.1) Pediatric patients: Ages 6 to 18 years, can safely swallow capsules and body weight at least 20 kg. Administered on an empty stomach, dosing is based on body weight. (2.1) Body Weight Dose 20 kg to less than 25 kg 200 mg once daily 25 kg to less than 60 kg 250 mg once daily at least 60 kg 400 mg once daily Renal impairment: Dose reduction is recommended. (2.2 ) Coadministration with tenofovir: Dose reduction is recommended. Patients should be monitored closely for didanosine-associated adverse reactions. (2.3 , 7.1) DOSAGE FORMS AND STRENGTHSCapsules: 200 mg, 250 mg, 400 mg (3 )CONTRAINDICATIONSCoadministration with allopurinol or ribavirin is contraindicated. (4.1 and 4.2 )WARNINGS AND PRECAUTIONS Pancreatitis: Suspension or discontinuation of didanosine may be necessary. (5.1 ) Lactic acidosis and severe hepatomegaly with steatosis: Suspend didanosine in patients who develop clinical symptoms or signs with or without laboratory findings. (5.2 ) Hepatic toxicity: Interruption or discontinuation or didanosine must be considered upon worsening of liver disease. (5.3) Patients may develop peripheral neuropathy (5.4), retinal changes and optic neuritis (5.5), immune reconstitution syndrome (5.6), and redistribution/accumulation of body fat (5.7) Side Effects In adults, the most common adverse reactions (greater than 10%, all grades) are diarrhea, peripheral neurologic symptoms/neuropathy, nausea, headache, rash and vomiting. (6.1) Adverse reactions in pediatric patients were consistent with those in adults. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-888-838-2872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONSCoadministration of didanosine delayed-release capsules can alter the concentration of other drugs and other drugs may alter the concentration of didanosine. The potential drug-drug interactions must be considered prior to and during therapy. (4, 7, 12.3)USE IN SPECIFIC POPULATIONSPregnancy: Fatal lactic acidosis has been reported in pregnant women who received both didanosine and stavudine with other agents. This combination should be used with caution during pregnancy and only if the potential benefit clearly outweighs the potential risk. (5.2, 8.1) Physicians are encouraged to register patients in the Antiretroviral Pregnancy Registry by calling 1-800-258-4263.
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
- 1 DIDANOSINE INDICATIONS AND USAGE
- 2 DIDANOSINE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 DIDANOSINE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 DIDANOSINE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 DIDANOSINE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- Image of 250 mg Label
- Image of 400 mg Label
FULL PRESCRIBING INFORMATION
WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. Didanosine delayed-release capsules should be suspended in patients with suspected pancreatitis and discontinued in patients with confirmed pancreatitis [see Warnings and Precautions (5.1 )].
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. Fatal lactic acidosis has been reported in pregnant women who received the combination of didanosine and stavudine with other antiretroviral agents. The combination of didanosine and stavudine should be used with caution during pregnancy and is recommended only if the potential benefit clearly outweighs the potential risk [see Warnings and Precautions (5.2)].
1 INDICATIONS AND USAGE
Didanosine delayed-release capsules, also known as ddI, in combination with other antiretroviral agents is indicated for the treatment of human immunodeficiency virus (HIV)-1 infection [see Clinical Studies (14)].
2 DOSAGE AND ADMINISTRATION
Didanosine delayed-release capsules should be administered on an empty stomach. Didanosine delayed-release capsules should be swallowed intact.
2.1 Recommended Dosage (Adult and Pediatric Patients)
The recommended total daily dose is based on body weight and is administered as one capsule given on a once-daily schedule as outlined in Table 1.
The recommended total daily dose to be administered once daily to pediatric patients weighing at least 20 kg who can swallow capsules is based on body weight (kg), consistent with the recommended adult dosing guidelines (see Table 1). Please consult the complete prescribing information for Didanosine Pediatric Powder for Oral Solution for dosage and administration of didanosine to pediatric patients weighing less than 20 kg or who can not swallow capsules.
| Body Weight | Dose |
| 20 kg to less than 25 kg | 200 mg once daily |
| 25 kg to less than 60 kg | 250 mg once daily |
| at least 60 kg | 400 mg once daily |
2.2 Renal Impairment
Dosing recommendations for didanosine delayed-release capsules and didanosine buffered formulations are different for patients with renal impairment. Please consult the complete prescribing information on administration of didanosine buffered formulations to patients with renal impairment.
Adult Patients
In adult patients with impaired renal function, the dose of didanosine should be adjusted to compensate for the slower rate of elimination. The recommended doses and dosing intervals of didanosine in adult patients with renal insufficiency are presented in Table 2.
|
Creatinine Clearance (mL/min) |
Dosage (mg) | |
| at least 60 kg | less than 60 kg | |
| at least 60 | 400 once daily | 250 once daily |
| 30 to 59 | 200 once daily | 125 once daily |
| 10 to 29 | 125 once daily | 125 once daily |
| less than 10 | 125 once daily |
 |
Pediatric Patients
Urinary excretion is also a major route of elimination of didanosine in pediatric patients, therefore the clearance of didanosine may be altered in pediatric patients with renal impairment. Although there are insufficient data to recommend a specific dose adjustment of didanosine in this patient population, a reduction in the dose should be considered (see Table 2).
Patients Requiring Continuous Ambulatory Peritoneal Dialysis (CAPD) or Hemodialysis
For patients requiring CAPD or hemodialysis, follow dosing recommendations for patients with creatinine clearance of less than 10 mL/min, shown in Table 2. It is not necessary to administer a supplemental dose of didanosine following hemodialysis.
2.3 Dose Adjustment
Concomitant Therapy with Tenofovir Disoproxil Fumarate
In patients who are also taking tenofovir disoproxil fumarate, a dose reduction of didanosine delayed-release capsules to 250 mg (adults weighing at least 60 kg with creatinine clearance of at least 60 mL/min) or 200 mg (adults weighing less than 60 kg with creatinine clearance of at least 60 mL/min) once daily taken together with tenofovir disoproxil fumarate and a light meal (400 kcalories or less, 20% fat or less) or in the fasted state is recommended. The appropriate dose of didanosine delayed-release capsules coadministered with tenofovir disoproxil fumarate in patients with creatinine clearance of less than 60 mL/min has not been established [see Drug Interactions (7 ) and Clinical Pharmacology (12.3)].
Hepatic Impairment
No dose adjustment is required in patients with hepatic impairment [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)].
3 DOSAGE FORMS AND STRENGTHS
Didanosine Delayed-Release Capsules are available as:
200 mg: Two-piece hard gelatin capsule with green opaque cap and white opaque body filled with white pellets. Imprinted in black ink stylized barr 588 over 200 mg.
250 mg: Two-piece hard gelatin capsule with blue opaque cap and white opaque body filled with white pellets. Imprinted in black ink stylized barr 589 over 250 mg.
400 mg: Two-piece hard gelatin capsule with red opaque cap and white opaque body filled with white pellets. Imprinted in black ink stylized barr 590 over 400 mg.
4 CONTRAINDICATIONS
These recommendations are based on either drug interaction studies or observed clinical toxicities.
4.1 Allopurinol
Coadministration of didanosine and allopurinol is contraindicated because systemic exposures of didanosine are increased, which may increase didanosine-associated toxicity [see Clinical Pharmacology (12.3)].
4.2 Ribavirin
Coadministration of didanosine and ribavirin is contraindicated because exposures of the active metabolite of didanosine (dideoxyadenosine 5’-triphosphate) are increased. Fatal hepatic failure, as well as peripheral neuropathy, pancreatitis, and symptomatic hyperlactatemia/lactic acidosis have been reported in patients receiving both didanosine and ribavirin.
5 WARNINGS AND PRECAUTIONS
5.1 Pancreatitis
Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. Didanosine should be suspended in patients with signs or symptoms of pancreatitis and discontinued in patients with confirmed pancreatitis. Patients treated with didanosine in combination with stavudine may be at increased risk for pancreatitis.
When treatment with life-sustaining drugs known to cause pancreatic toxicity is required, suspension of didanosine therapy is recommended. In patients with risk factors for pancreatitis, didanosine should be used with extreme caution and only if clearly indicated. Patients with advanced HIV-1 infection, especially the elderly, are at increased risk of pancreatitis and should be followed closely. Patients with renal impairment may be at greater risk for pancreatitis if treated without dose adjustment. The frequency of pancreatitis is dose related [see Adverse Reactions (6)].
5.2 Lactic Acidosis/Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. A majority of these cases have been in women. Obesity and prolonged nucleoside exposure may be risk factors. Fatal lactic acidosis has been reported in pregnant women who received the combination of didanosine and stavudine with other antiretroviral agents. The combination of didanosine and stavudine should be used with caution during pregnancy and is recommended only if the potential benefit clearly outweighs the potential risk [see Use in Specific Populations (8.1)]. Particular caution should be exercised when administering didanosine to any patient with known risk factors for liver disease; however, cases have also been reported in patients with no known risk factors. Treatment with didanosine should be suspended in any patient who develops clinical signs or symptoms with or without laboratory findings consistent with symptomatic hyperlactatemia, lactic acidosis, or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
5.3 Hepatic Toxicity
The safety and efficacy of didanosine have not been established in HIV-infected patients with significant underlying liver disease. During combination antiretroviral therapy, patients with preexisting liver dysfunction, including chronic active hepatitis, have an increased frequency of liver function abnormalities, including severe and potentially fatal hepatic adverse events, and should be monitored according to standard practice. If there is evidence of worsening liver disease in such patients, interruption or discontinuation of treatment must be considered.
Hepatotoxicity and hepatic failure resulting in death were reported during postmarketing surveillance in HIV-infected patients treated with hydroxyurea and other antiretroviral agents. Fatal hepatic events were reported most often in patients treated with the combination of hydroxyurea, didanosine, and stavudine. This combination should be avoided [see Adverse Reactions (6 )].
5.4 Peripheral Neuropathy
Peripheral neuropathy, manifested by numbness, tingling, or pain in the hands or feet, has been reported in patients receiving didanosine therapy. Peripheral neuropathy has occurred more frequently in patients with advanced HIV disease, in patients with a history of neuropathy, or in patients being treated with neurotoxic drug therapy, including stavudine. Discontinuation of didanosine should be considered in patients who develop peripheral neuropathy [see Adverse Reactions (6)].
5.5 Retinal Changes and Optic Neuritis
Retinal changes and optic neuritis have been reported in patients taking didanosine. Periodic retinal examinations should be considered for patients receiving didanosine [see Adverse Reactions (6)].
5.6 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including didanosine. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jiroveci pneumonia [PCP], or tuberculosis), which may necessitate further evaluation and treatment.
5.7 Fat Redistribution
Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and “cushingoid appearance” have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections:
- Pancreatitis [see Boxed Warning, Warnings and Precautions (5.1)]
- Lactic acidosis/severe hepatomegaly with steatosis [see Boxed Warning, Warnings and Precautions (5.2)]
- Hepatic toxicity [see Warnings and Precautions (5.3)]
- Peripheral neuropathy [see Warnings and Precautions (5.4)]
- Retinal changes and optic neuritis [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults
Study AI454-152 was a 48-week, randomized, open-label study comparing didanosine (400 mg once daily) plus stavudine (40 mg twice daily) plus nelfinavir (750 mg three times daily) to zidovudine (300 mg) plus lamivudine (150 mg) combination tablets twice daily plus nelfinavir (750 mg three times daily) in 511 treatment-naive patients. Selected clinical adverse reactions that occurred in combination with other antiretroviral agents are provided in Table 3.
Percent of Patients  |
||
| Adverse Reactions |
didanosine + stavudine + nelfinavir n=258 |
zidovudine/ lamivudine  nelfinavir n=253 |
| Diarrhea | 57 | 58 |
| Peripheral Neurologic Symptoms/Neuropathy |
25 | 11 |
| Nausea | 24 | 36 |
| Headache | 22 | 17 |
| Rash | 14 | 12 |
| Vomiting | 14 | 19 |
| Pancreatitis (see below) | less than 1 |
 |
In clinical trials using a buffered formulation of didanosine, pancreatitis resulting in death was observed in one patient who received didanosine plus stavudine plus nelfinavir, one patient who received didanosine plus stavudine plus indinavir, and 2 of 68 patients who received didanosine plus stavudine plus indinavir plus hydroxyurea. In an early access program, pancreatitis resulting in death was observed in one patient who received didanosine plus stavudine plus hydroxyurea plus ritonavir plus indinavir plus efavirenz [see Warnings and Precautions (5)].
The frequency of pancreatitis is dose related. In phase 3 studies with buffered formulations of didanosine, incidence ranged from 1% to 10% with doses higher than are currently recommended and 1% to 7% with recommended dose.
Selected laboratory abnormalities that occurred in a study of didanosine in combination with other antiretroviral agents are shown in Table 4.
Percent of Patients |
||||
|
didanosine + stavudine + nelfinavir n=258 |
zidovudine/lamivudine n=253 |
|||
| Parameter |
Grades 3-4 |
All Grades |
Grades 3-4 |
All Grades |
| SGOT (AST) | 5 | 46 | 5 | 19 |
| SGPT (ALT) | 6 | 44 | 5 | 22 |
| Lipase | 5 | 23 | 2 | 13 |
| Bilirubin | less than 1 | 9 | less than 1 | 3 |
Pediatric Patients
In clinical trials, 743 pediatric patients between 2 weeks and 18 years of age have been treated with didanosine. Adverse reactions and laboratory abnormalities reported to occur in these patients were generally consistent with the safety profile of didanosine in adults.
In pediatric phase 1 studies, pancreatitis occurred in 2 of 60 (3%) patients treated at entry doses below 300 mg/m2/day and in 5 of 38 (13%) patients treated at higher doses. In study ACTG 152, pancreatitis occurred in none of the 281 pediatric patients who received didanosine 120 mg/m2 every 12 hours and in less than 1% of the 274 pediatric patients who received didanosine 90 mg/m2 every 12 hours in combination with zidovudine [see Clinical Studies (14)].
Retinal changes and optic neuritis have been reported in pediatric patients.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of didanosine. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These reactions have been chosen for inclusion due to their seriousness, frequency of reporting, causal connection to didanosine, or a combination of these factors.
Blood and Lymphatic System Disorders - anemia, leukopenia, and thrombocytopenia.
Body as a Whole - abdominal pain, alopecia, anaphylactoid reaction, asthenia, chills/fever, pain, and redistribution/accumulation of body fat [see Warnings and Precautions (5.7)].
Digestive Disorders - anorexia, dyspepsia, and flatulence.
Exocrine Gland Disorders - pancreatitis (including fatal cases) [see Warnings and Precautions
(5.1 )], sialoadenitis, parotid gland enlargement, dry mouth, and dry eyes.
Hepatobiliary Disorders - symptomatic hyperlactatemia/lactic acidosis and hepatic steatosis [see Warnings and Precautions (5.2)]; hepatitis and liver failure.
Metabolic Disorders - diabetes mellitus, elevated serum alkaline phosphatase level, elevated serum amylase level, elevated serum gamma-glutamyltransferase level, elevated serum uric acid level, hypoglycemia, and hyperglycemia.
Musculoskeletal Disorders - myalgia (with or without increases in creatine kinase), rhabdomyolysis including acute renal failure and hemodialysis, arthralgia, and myopathy.
Ophthalmologic Disorders - retinal depigmentation and optic neuritis [see Warnings and Precautions (5.5)].
Use with Stavudine- and Hydroxyurea-Based Regimens
When didanosine is used in combination with other agents with similar toxicities, the incidence of these toxicities may be higher than when didanosine is used alone. Thus, patients treated with didanosine in combination with stavudine, with or without hydroxyurea, may be at increased risk for pancreatitis and hepatotoxicity, which may be fatal, and severe peripheral neuropathy [see Warnings and Precautions (5)]. The combination of didanosine and hydroxyurea, with or without stavudine, should be avoided.
7 DRUG INTERACTIONS
7.1 Established Drug Interactions
Clinical recommendations based on the results of drug interaction studies are listed in Table 5. Pharmacokinetic results of drug interaction studies are shown in Tables 9 to12 [see Contraindications (4.1 and 4.2), Clinical Pharmacology (12.3)].
| ↑Indicates increase. ↓Indicates decrease. |
||
| Drug | Effect | Clinical Comment |
| ganciclovir | ↑didanosine concentration | If there is no suitable alternative to ganciclovir, then use in combination with didanosine with caution. Monitor for didanosine-associated toxicity. |
| methadone | ↓didanosine concentration | If coadministration of methadone and didanosine is necessary, the recommended formulation of didanosine is didanosine delayed-release capsules. Patients should be closely monitored for adequate clinical response when didanosine is coadministered with methadone, including monitoring for changes in HIV RNA viral load. Do not coadminister methadone with didanosine pediatric powder due to significant decreases in didanosine concentrations. |
| nelfinavir | No interaction 1 hour after didanosine | Administer nelfinavir 1 hour after didanosine. |
|
tenofovir disoproxil fumarate |
↑didanosine concentration |
A dose reduction of didanosine to the following dosage once daily taken together with tenofovir disoproxil fumarate and a light meal (400 kcalories or less and 20% fat or less ) or in the fasted state is recommended.
|
Exposure to didanosine is increased when coadministered with tenofovir disoproxil fumarate
[Table 5 and see Clinical Pharmacokinetics (12.3, Tables Table 9 and Table 11)]. Increased exposure may cause or worsen didanosine-related clinical toxicities, including pancreatitis, symptomatic hyperlactatemia/lactic acidosis, and peripheral neuropathy. Coadministration of tenofovir disoproxil fumarate with didanosine should be undertaken with caution, and patients should be monitored closely for didanosine-related toxicities and clinical response. Didanosine should be suspended if signs or symptoms of pancreatitis, symptomatic hyperlactatemia, or lactic acidosis develop [see Dosage and Administration (2.3), Warnings and Precautions (5)]. Suppression of CD4 cell counts has been observed in patients receiving tenofovir disoproxil fumarate with didanosine at a dose of 400 mg daily.
7.2 Predicted Drug Interactions
Predicted drug interactions with didanosine are listed in Table 6.
| ↑ Indicates increase. | ||
| Drug or Drug Class | Effect | Clinical Comment |
| Drugs that may cause pancreatic toxicity | ↑risk of pancreatitis | Use only with extreme caution. |
| Neurotoxic drugs | ↑risk of neuropathy | Use with caution. |
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
Reproduction studies have been performed in rats and rabbits at doses up to 12 and 14.2 times the estimated human exposure (based upon plasma levels), respectively, and have revealed no evidence of impaired fertility or harm to the fetus due to didanosine. At approximately 12 times the estimated human exposure, didanosine was slightly toxic to female rats and their pups during mid and late lactation. These rats showed reduced food intake and body weight gains but the physical and functional development of the offspring was not impaired and there were no major changes in the F2 generation. A study in rats showed that didanosine and/or its metabolites are transferred to the fetus through the placenta. Animal reproduction studies are not always predictive of human response.
There are no adequate and well-controlled studies of didanosine in pregnant women. Didanosine should be used during pregnancy only if the potential benefit justifies the potential risk.
Fatal lactic acidosis has been reported in pregnant women who received the combination of didanosine and stavudine with other antiretroviral agents. It is unclear if pregnancy augments the risk of lactic acidosis/hepatic steatosis syndrome reported in nonpregnant individuals receiving nucleoside analogues [see Warnings and Precautions (5.2)]. The combination of didanosine and stavudine should be used with caution during pregnancy and is recommended only if the potential benefit clearly outweighs the potential risk. Healthcare providers caring for HIV-infected pregnant women receiving didanosine should be alert for early diagnosis of lactic acidosis/hepatic steatosis syndrome.
Antiretroviral Pregnancy Registry
To monitor maternal-fetal outcomes of pregnant women exposed to didanosine and other antiretroviral agents, an Antiretroviral Pregnancy Registry has been established. Physicians are encouraged to register patients by calling 1-800-258-4263.
8.3 Nursing Mothers
The Centers for Disease Control and Prevention recommend that HIV-infected mothers not breast-feed their infants to avoid risking postnatal transmission of HIV. A study in rats showed that following oral administration, didanosine and/or its metabolites were excreted into the milk of lactating rats. It is not known if didanosine is excreted in human milk. Because of both the potential for HIV transmission and the potential for serious adverse reactions in nursing infants, mothers should be instructed not to breast-feed if they are receiving didanosine.
8.4 Pediatric Use
Use of didanosine in pediatric patients from 2 weeks of age through adolescence is supported by evidence from adequate and well-controlled studies of didanosine in adult and pediatric patients [see Dosage and Administration (2), Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)]. Additional pharmacokinetic studies in pediatric patients support use of didanosine in pediatric patients who weigh at least 20 kg.
8.5 Geriatric Use
In an Expanded Access Program using a buffered formulation of didanosine for the treatment of advanced HIV infection, patients aged 65 years and older had a higher frequency of pancreatitis (10%) than younger patients (5%) [see Warnings and Precautions (5.1)]. Clinical studies of didanosine, including those for didanosine delayed-release capsules, did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently than younger subjects. Didanosine is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection. In addition, renal function should be monitored and dosage adjustments should be made accordingly [see Dosage and Administration (2.2)].
8.6 Renal Impairment
Patients with renal impairment (creatinine clearance of less than 60 mL/min) may be at greater risk of toxicity from didanosine due to decreased drug clearance [see Clinical Pharmacology (12.3)]. A dose reduction is recommended for these patients [see Dosage and Administration (2)].
10 OVERDOSAGE
There is no known antidote for didanosine overdosage. In phase 1 studies, in which buffered formulations of didanosine were initially administered at doses ten times the currently recommended dose, toxicities included: pancreatitis, peripheral neuropathy, diarrhea, hyperuricemia, and hepatic dysfunction. Didanosine is not dialyzable by peritoneal dialysis, although there is some clearance by hemodialysis [see Clinical Pharmacology (12.3)].
11 DESCRIPTION
Didanosine delayed-release capsules are an enteric-coated formulation of didanosine, (ddl), a synthetic purine nucleoside analogue active against HIV-1. Didanosine delayed-release capsules, containing enteric-coated pellets, are available for oral administration in the strengths of 200, 250, and 400 mg of didanosine. The inactive ingredients include croscarmellose sodium, hydroxypropyl cellulose, hypromellose, methacrylic acid copolymer dispersion, microcrystalline cellulose, polydextrose, polyethylene glycol, silicon dioxide, sodium hydroxide, talc, titanium dioxide, triacetin and triethyl citrate.The capsule shell contains FD&C blue no.1, gelatin, and titanium dioxide.The 200 mg capsule shell also contains D&C red no. 33, and FD&C yellow no. 6. The 250 mg capsule shell also contains D&C red no. 28. The 400 mg capsule shell also contains D&C red no.33, and FD&C yellow no. 6. The edible imprinting ink contains D&C yellow no. 10 aluminum lake, FD&C blue no. 1 aluminum lake, FD&C blue no. 2 aluminum lake, FD&C red no. 40 aluminum lake, iron oxide, propylene glycol and shellac glaze.
The chemical name for didanosine is 2', 3'-dideoxyinosine. The structural formula is:
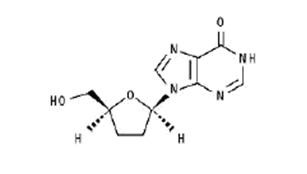
Didanosine is a white crystalline powder with the molecular formula C10H12N4O3 and a molecular weight of 236.2. The aqueous solubility of didanosine at 25° C and pH of approximately 6 is 27.3 mg/mL. Didanosine is unstable in acidic solutions. For example, at pH less than 3 and 37° C, 10% of didanosine decomposes to hypoxanthine in less than 2 minutes. In didanosine delayed-release capsules, an enteric coating is used to protect didanosine from degradation by stomach acid.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Didanosine is an antiviral agent [see Clinical Pharmacology (12.4)].
12.3 Pharmacokinetics
The pharmacokinetic parameters of didanosine in HIV-infected adult and pediatric patients are summarized in Table 7, by weight ranges that correspond to recommended doses (Table 1). Didanosine is rapidly absorbed, with peak plasma concentrations generally observed from 0.25 to 1.50 hours following oral dosing with a buffered formulation. Increases in plasma didanosine concentrations were dose proportional over the range of 50 to 400 mg. In adults, the mean (± standard deviation) oral bioavailability following single oral dosing with a buffered formulation is 42 (±12)%. After oral administration, the urinary recovery of didanosine is approximately 18 (±8)% of the dose. The CSF-plasma ratio following IV administration is 21 (±0.03)%. Steady-state pharmacokinetic parameters did not differ significantly from values obtained after a single dose. Binding of didanosine to plasma proteins in vitro was low (less than 5%). Based on data from in vitro and animal studies, it is presumed that the metabolism of didanosine in man occurs by the same pathways responsible for the elimination of endogenous purines.
| Pediatrics | Adults | |||
Parameter |
20 kg to less than 25 kg n = 10 | 25 kg to less than 60 kg n = 17 | At least 60 kg n= 7 |
At least 60 kg n= 44 |
| Apparent clearance (L/h) | 89.5 + 21.6 | 116.2 + 38.6 | 196 + 55.8 | 174.5 + 69.7 |
| Apparent volume of distribution (L) | 98.1 + 30.2 | 154.7 + 55 | 363 + 137.7 | 308.3 + 164.3 |
| Elimination half-life (h) | 0.75 + 0.13 | 0.92 + 0.09 | 1.26 + 0.19 | 1.19 + 0.21 |
| Steady-state (AUC) (mg•h/L) |
2.38 + 0.66 | 2.36 + 0.70 | 2.25 + 0.89 | 2.65 + 1.07 |
Comparison of Didanosine Formulations
In didanosine delayed-release capsules, the active ingredient, didanosine, is protected against degradation by stomach acid by the use of an enteric coating on the pellets in the capsule. The enteric coating dissolves when the pellets empty into the small intestine, the site of drug absorption. With buffered formulations of didanosine, administration with antacid provides protection from degradation by stomach acid.
In healthy volunteers, as well as subjects infected with HIV-1, the AUC is equivalent for didanosine administered as the didanosine delayed-release capsules formulation relative to a buffered tablet formulation. The peak plasma concentration (Cmax) of didanosine, administered as didanosine delayed-release capsules, is reduced approximately 40% relative to didanosine buffered tablets. The time to the peak concentration (Tmax) increases from approximately 0.67 hours for didanosine buffered tablets to 2 hours for didanosine delayed-release capsules.
Effect of Food
In the presence of food, the Cmax and AUC for didanosine were reduced by approximately 46% and 19%, respectively, compared to the fasting state [see Dosage and Administration (2)]. Didanosine delayed-release capsules should be taken on an empty stomach.
Special Populations
Renal Insufficiency: Data from two studies using a buffered formulation of didanosine indicated that the apparent oral clearance of didanosine decreased and the terminal elimination half-life increased as creatinine clearance decreased (see Table 8). Following oral administration, didanosine was not detectable in peritoneal dialysate fluid (n=6); recovery in hemodialysate (n=5) ranged from 0.6% to 7.4% of the dose over a 3 to 4 hour dialysis period. The absolute bioavailability of didanosine was not affected in patients requiring dialysis. [See Dosage and Administration (2.2).]
| ND = not determined due to anuria. CLcr = creatinine clearance. CL/F= apparent oral clearance. CLR= renal clearance. |
|||||
| Creatinine Clearance (mL/min) | |||||
| Parameter | At least 90 n=12 |
60-90 n=6 |
30-59 n=6 |
10-29 n=3 |
Dialysis Patients n=11 |
| Clcr (mL/min) | 112 + 22 | 68 + 8 | 46 + 8 | 13 + 5 | ND |
| CL/F (mL/min) | 2164 + 638 | 1566 + 833 | 1023 + 378 | 628 + 104 | 543 + 174 |
| CLR (mL/min) | 458 + 164 | 247 + 153 | 100 + 44 | 20 + 8 | less than 10 |
| T1/2 (h) | 1.42 + 0.33 | 1.59 + 0.13 | 1.75 + 0.43 | 2 + 0.3 | 4.1 + 1.2 |
Hepatic Impairment: The pharmacokinetics of didanosine have been studied in 12 non-HIV infected subjects with moderate (n=8) to severe (n=4) hepatic impairment (Child-Pugh Class B or C). Mean AUC and Cmax values following a single 400 mg dose of didanosine were approximately 13% and 19% higher, respectively, in patients with hepatic impairment compared to matched healthy subjects. No dose adjustment is needed, because a similar range and distribution of AUC and Cmax values was observed for subjects with hepatic impairment and matched healthy controls. [See Dosage and Administration (2.3).]
Pediatric Patients: The pharmacokinetics of didanosine administered as didanosine delayed-release capsules have not been studied in pediatric patients.
A population pharmacokinetic analysis was conducted on pooled didanosine plasma concentration data from 9 clinical trials in 106 pediatric (neonate to 18 years of age) and 45 adult patients (greater than 18 years of age). Results showed that body weight is the primary factor associated with oral clearance. Based on the data analyzed, dosing schedule (once versus twice daily) and formulation (powder for oral solution, tablet, and delayed-release capsule) did not have an effect on oral clearance. Didanosine exposure similar to that at recommended adult doses can be achieved in pediatric patients with a weight-based dosing scheme [see Dosage and Administration (2)].
Geriatric Patients: Didanosine pharmacokinetics have not been studied in patients over 65 years of age [see Use in Specific Populations (8.5)].
Gender: The effects of gender on didanosine pharmacokinetics have not been studied.
Drug Interactions
Tables 9 and 10 summarize the effects on AUC and Cmax, with a 90% confidence interval (CI) when available, following coadministration of didanosine with a variety of drugs. For clinical recommendations based on drug interaction studies for drugs in bold font, see Dosage and Administration (2.3) and Drug Interactions (7.1).
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. |
||||
|
% Change of Didanosine Pharmacokinetic Parameters |
||||
| Drug Didanosine Dosage n |
AUC of Didanosine (90% CI) |
Cmax of Didanosine (90% CI) |
||
|
tenofovir, once daily with a light meal tenofovir, once daily with a light meal tenofovir, once daily with a light meal methadone, chronic maintenance dose |
400 mg single dose fasting 2 hours before tenofovir 400 mg single dose with tenofovir and a light meal 200 mg single dose with tenofovir and a light meal 250 mg single dose with tenofovir and a light meal 325 mg single dose with tenofovir and a light meal 400 mg single dose |
26 25 33 33 33 15, 16 |
↑ 48% (31, 67%) ↑ 60% (44, 79%) ↑ 16% (6, 27%) ↔ (-13, 5%) ↑ 13% (3, 24%) ↓ 17% (-29, -2%) |
↑ 48% (25, 76%) ↑ 64% (41, 89%) ↓ 12% (-25, 3%) ↓ 20% (-32, -7%) ↓ 11% (-24, 4%) ↓ 16% (-33, 4%) |
| ↔ Indicates no change, or mean increase or decrease of less than 10%. | ||||
% Change of Coadministered Drug Pharmacokinetic Parameters  |
||||
|
Drug Didanosine Dosage n |
AUC of Coadministered Drug (90% CI) |
Cmax of Coadministered Drug (90% CI) |
||
|
ciprofloxacin, 750 mg single dose indinavir, 800 mg single dose ketoconazole, 200 mg single dose tenofovir, once daily with a light meal tenofovir,  |
400 mg single dose 400 mg single dose 400 mg single dose 400 mg single dose fasting 2 hours before tenofovir 400 mg single dose with tenofovir and a light meal |
16 23 21 25 25 |
↔ ↔ ↔ ↔ ↔ |
↔ ↔ ↔ ↔ ↔ |
Didanosine Buffered Formulations: Tables 11 and 12 summarize the effects on AUC and Cmax, with a 90% or 95% CI when available, following coadministration of buffered formulations of didanosine with a variety of drugs. Except as noted in table footnotes, the results of these studies may be expected to apply to didanosine. For most of the listed drugs, no clinically significant pharmacokinetic interactions were noted. For clinical recommendations based on drug interaction studies for drugs in bold font, see Dosage and Administration (2.3 for Concomitant Therapy with Tenofovir Disoproxil Fumarate) and Drug Interactions (7.1).
|
% Change of Didanosine Pharmacokinetic Parameters |
||||
| Drug Didanosine Dosage n |
AUC of Didanosine (95% CI) |
Cmax of Didanosine (95% CI) |
||
|
allopurinol, renally impaired, 300 mg/day healthy volunteer, 300 mg/day for 7 days ganciclovir, 1000 mg every ciprofloxacin, 750 mg every didanosine indinavir, 800 mg single dose simultaneous 1 hour before didanosine ketoconazole, 200 mg/day for loperamide, 4 mg every 6 hours for 1 day metoclopramide, 10 mg single dose ranitidine, 150 mg single dose, rifabutin, 300 or 600 mg/day for ritonavir, 600 mg every 12 hours for 4 days stavudine, 40 mg every 12 hours for 4 days sulfamethoxazole, 1000 mg single dose trimethoprim, 200 mg single dose zidovudine, 200 mg every 8 hours for 3 days |
200 mg single dose 400 mg single dose 200 mg every 12 hours 200 mg every 12 hours for 3 days 200 mg single dose 200 mg single dose 375 mg every 12 hours for 4 days 300 mg single dose 300 mg single dose 375 mg single dose 167 or 250 mg every 12 hours for 12 days 200 mg every 12 hours for 4 days 100 mg every 12 hours for 4 days 200 mg single dose 200 mg single dose 200 mg every 12 hours for 3 days |
2 14 12 8 16 16 12 12 12 12 11 12 10 8 8  |
↑ 312% ↑ 113% ↑ 111% ↓ 16% ↔ ↓ 17% (-27, -7%) ↔ ↔ ↔ ↑ 14% ↑ 13% (-1, 27%) ↓ 13% (0, 23%) ↔ ↔ ↔ ↔ |
↑ 232% ↑ 69% NA ↓ 28% ↔ ↓ 13% (-28, 5%) ↓ 12% ↓ 23% ↑ 13% ↑ 13% ↑ 17% (-4, 38%) ↓ 16% (5, 26%) ↔ ↔ ↑ 17% (-23, 77%) ↔ |
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. NA = Not available. |
||||
% Change of Coadministered Drug Pharmacokinetic Parameters |
||||
|
Drug Didanosine Dosage n |
AUC of Coadministered Drug (95% CI) |
Cmax of Coadministered Drug (95% CI) |
||
|
dapsone, 100 mg single dose ganciclovir, 1000 mg every 8 hours, 2 hours after didanosine nelfinavir, 750 mg single dose, 1 hour after didanosine ranitidine, 150 mg single dose, 2 hours before didanosine ritonavir, 600 mg every 12 hours for 4 days stavudine, 40 mg every 12 hours for 4 days sulfamethoxazole, 1000 mg single dose trimethoprim, 200 mg single dose zidovudine, 200 mg every 8 hours for 3 days |
200 mg every 12 hours for 14 days 200 mg every 12 hours 200 mg single dose 375 mg single dose 200 mg every 12 hours for 4 days 100 mg every 12 hours for 4 days 200 mg single dose 200 mg single dose 200 mg every 12 hours for 3 days |
6 12 10 12 12 10 8 8  |
↔ ↓ 21% ↑ 12% ↓ 16% ↔ ↔ ↓ 11% (-17, -4%) ↑ 10% (-9, 34%) ↓ 10% (-27, 11%) |
↔ NA ↔ ↔ ↔ ↑ 17% ↓ 12% (-28, 8%) ↓ 22% (-59, 49%) ↓ 16.5% (-53, 47%) |
12.4 Microbiology
Mechanism of Action
Didanosine is a synthetic nucleoside analogue of the naturally occurring nucleoside deoxyadenosine in which the 3’-hydroxyl group is replaced by hydrogen. Intracellularly, didanosine is converted by cellular enzymes to the active metabolite, dideoxyadenosine 5’-triphosphate. Dideoxyadenosine 5’-triphosphate inhibits the activity of HIV-1 reverse transcriptase both by competing with the natural substrate, deoxyadenosine 5’-triphosphate, and by its incorporation into viral DNA causing termination of viral DNA chain elongation.
Antiviral Activity in Cell Culture
The anti-HIV-1 activity of didanosine was evaluated in a variety of HIV-1 infected lymphoblastic cell lines and monocyte/macrophage cell cultures. The concentration of drug necessary to inhibit viral replication by 50% (EC50) ranged from 2.5 to 10 μM
(1 μM=0.24 μg/mL) in lymphoblastic cell lines and 0.01 to 0.1 μM in monocyte/macrophage cell cultures.
Resistance
HIV-1 isolates with reduced sensitivity to didanosine have been selected in cell culture and were also obtained from patients treated with didanosine. Genetic analysis of isolates from didanosine-treated patients showed mutations in the reverse transcriptase gene that resulted in the amino acid substitutions K65R, L74V, and M184V. The L74V substitution was most frequently observed in clinical isolates. Phenotypic analysis of HIV-1 isolates from 60 patients (some with prior zidovudine treatment) receiving 6 to 24 months of didanosine monotherapy showed that isolates from 10 of 60 patients exhibited an average of a 10-fold decrease in susceptibility to didanosine in cell culture compared to baseline isolates. Clinical isolates that exhibited a decrease in didanosine susceptibility harbored one or more didanosine resistance-associated substitutions.
Cross-resistance
HIV-1 isolates from 2 of 39 patients receiving combination therapy for up to 2 years with didanosine and zidovudine exhibited decreased susceptibility to didanosine, lamivudine, stavudine, zalcitabine, and zidovudine in cell culture. These isolates harbored five substitutions (A62V, V75I, F77L, F116Y, and Q151M) in the reverse transcriptase gene. In data from clinical studies, the presence of thymidine analogue mutations (M41L, D67N, L210W, T215Y, K219Q) has been shown to decrease the response to didanosine.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime carcinogenicity studies were conducted in mice and rats for 22 and 24 months, respectively. In the mouse study, initial doses of 120, 800, and 1200 mg/kg/day for each sex were lowered after 8 months to 120, 210, and 210 mg/kg/day for females and 120, 300, and 600 mg/kg/day for males. The two higher doses exceeded the maximally tolerated dose in females and the high dose exceeded the maximally tolerated dose in males. The low dose in females represented 0.68-fold maximum human exposure and the intermediate dose in males represented 1.7-fold maximum human exposure based on relative AUC comparisons. In the rat study, initial doses were 100, 250, and 1000 mg/kg/day, and the high dose was lowered to 500 mg/kg/day after 18 months. The upper dose in male and female rats represented 3-fold maximum human exposure.
Didanosine induced no significant increase in neoplastic lesions in mice or rats at maximally tolerated doses.
Didanosine was positive in the following genetic toxicology assays: 1) the Escherichia coli tester strain WP2 uvrA bacterial mutagenicity assay; 2) the L5178Y/TK+/- mouse lymphoma mammalian cell gene mutation assay; 3) the in vitro chromosomal aberrations assay in cultured human peripheral lymphocytes; 4) the in vitro chromosomal aberrations assay in Chinese Hamster Lung cells; and 5) the BALB/c 3T3 in vitro transformation assay. No evidence of mutagenicity was observed in an Ames Salmonella bacterial mutagenicity assay or in rat and mouse in vivo micronucleus assays.
13.2 Animal Toxicology and/or Pharmacology
Evidence of a dose-limiting skeletal muscle toxicity has been observed in mice and rats (but not in dogs) following long-term (greater than 90 days) dosing with didanosine at doses that were approximately 1.2 to 12 times the estimated human exposure. The relationship of this finding to the potential of didanosine to cause myopathy in humans is unclear. However, human myopathy has been associated with administration of didanosine and other nucleoside analogues.
14 CLINICAL STUDIES
14.1 Adult Patients
Study AI454-152 was a 48-week, randomized, open-label study comparing didanosine (400 mg once daily) plus stavudine (40 mg twice daily) plus nelfinavir (750 mg three times daily) to zidovudine (300 mg) plus lamivudine (150 mg) combination tablets twice daily plus nelfinavir (750 mg three times daily) in 511 treatment-naive patients, with a mean CD4 cell count of 411 cells/mm3(range 39 to 1105 cells/mm3) and a mean plasma HIV-1 RNA of 4.71 log10 copies/mL (range 2.8 to 5.9 log10 copies/mL) at baseline. Patients were primarily males (72%) and Caucasian (53%) with a mean age of 35 years (range 18 to 73 years). The percentages of patients with HIV-1 RNA less than 400 and less than 50 copies/mL and outcomes of patients through 48 weeks are summarized in Figure 1 and Table 13, respectively.
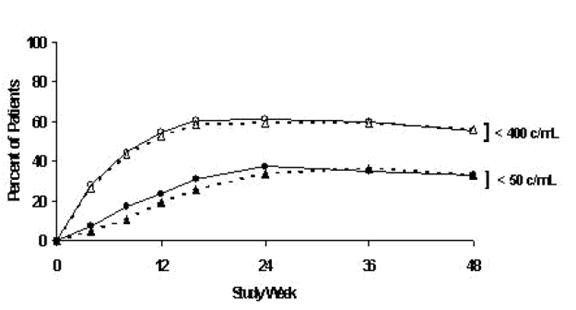
○● didanosine + stavudine + nelfinavir, n= 258
∆▲ zidovudine/lamivudine + nelfinavir, n= 253
*Percent of patients at each time point who have HIV RNA <400 or <50 copies/mL and do not meet any criteria for treatment failure (eg, virologic failure or discontinuation for any reason).
| Outcome |
Percent of Patients with HIV-1 RNA less than 400 copies/mL (less than 50 copies/mL) |
|
|
didanosine + stavudine |
zidovudine/lamivudine |
|
|
Responder Virologic failure Death or discontinued due to disease progression Discontinued due to adverse event Discontinued due to other reasons |
55% (33%) 22% (45%) 1% (1%) 6% (6%) 16% (16%) |
56% (33%) 21% (43%) 2% (2%) 7% (7%) 15% (16%) |
14.2 Pediatric Patients
Efficacy in pediatric patients was demonstrated in a randomized, double-blind, controlled study (ACTG 152, conducted 1991-1995) involving 831 patients 3 months to 18 years of age treated for more than 1.5 years with zidovudine (180 mg/m2 every 6 hours), didanosine (120 mg/m2 every 12 hours), or zidovudine (120 mg/m2 every 6 hours) plus didanosine (90 mg/m2 every 12 hours). Patients treated with didanosine or didanosine plus zidovudine had lower rates of HIV-1 disease progression or death compared with those treated with zidovudine alone.
16 HOW SUPPLIED/STORAGE AND HANDLING
Didanosine Delayed-Release Capsules are available as:
200 mg: Two-piece hard gelatin capsule with green opaque cap and white opaque body filled with white pellets. Imprinted in black ink stylized barr 588 over 200 mg.
250 mg: Two-piece hard gelatin capsule with blue opaque cap and white opaque body filled with white pellets. Imprinted in black ink stylized barr 589 over 250 mg.
400 mg: Two-piece hard gelatin capsule with red opaque cap and white opaque body filled with white pellets. Imprinted in black ink stylized barr 590 over 400 mg.
They are supplied by State of Florida DOH Central Pharmacy as follows:
| NDC | Strength | Quantity/Form | Color | Source Prod. Code |
| 53808-0236-1 | 250 mg | 30 Capsules in a Blister Pack | opaque | 0555-0589 |
| 53808-0353-1 | 400 mg | 30 Capsules in a Blister Pack | opaque | 0555-0590 |
Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Keep container tightly closed.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
17 PATIENT COUNSELING INFORMATION
See FDA-approved Patient Labeling (17.9)
17.1 Pancreatitis
Patients should be informed that a serious toxicity of didanosine, used alone and in combination regimens, is pancreatitis, which may be fatal.
17.2 Peripheral Neuropathy
Patients should be informed that peripheral neuropathy, manifested by numbness, tingling, or pain in hands or feet, may develop during therapy with didanosine. Patients should be counseled that peripheral neuropathy occurs with greatest frequency in patients with advanced HIV-1 disease or a history of peripheral neuropathy, and discontinuation of didanosine may be required if toxicity develops.
17.3 Lactic Acidosis and Severe Hepatomegaly with Steatosis
Patients should be informed that lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals.
17.4 Hepatic Toxicity
Patients should be informed that hepatotoxicity including fatal hepatic adverse events were reported in patients with preexisting liver dysfunction. The safety and efficacy of didanosine has not been established in HIV-infected patients with significant underlying liver disease.
17.5 Retinal Changes and Optic Neuritis
Patients should be informed that retinal changes and optic neuritis have been reported in adult and pediatric patients.
17.6 Fat Redistribution
Patients should be informed that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy and that the cause and long-term health effects of these conditions are not known at this time.
17.7 Concomitant Therapy
Patients should be informed that when didanosine is used in combination with other agents with similar toxicities, the incidence of adverse events may be higher than when didanosine is used alone. These patients should be followed closely.
Patients should be cautioned about the use of medications or other substances, including alcohol, which may exacerbate didanosine toxicities.
17.8 General Information
Didanosine is not a cure for HIV-1 infection, and patients may continue to develop HIV-associated illnesses, including opportunistic infection. Therefore, patients should remain under the care of a physician when using didanosine. Patients should be advised that didanosine therapy has not been shown to reduce the risk of transmission of HIV to others through sexual contact or blood contamination. Patients should be informed that the long-term effects of didanosine are unknown at this time.
17.9 FDA-Approved Patient Labeling
Didanosine Delayed-Release Capsules
Enteric-Coated Pellets
What is didanosine?
Didanosine is a prescription medicine used in combination with other drugs to treat children and adults who are infected with HIV (the human immunodeficiency virus, the virus that causes AIDS). Didanosine belongs to a class of drugs called nucleoside analogues. By reducing the growth of HIV, didanosine helps your body maintain its supply of CD4 cells, which are important for fighting HIV and other infections.
Didanosine will not cure your HIV infection. At present there is no cure for HIV infection. Even while taking didanosine, you may continue to have HIV-related illnesses, including infections with other disease-producing organisms. Continue to see your doctor regularly and report any medical problems that occur.
Didanosine does not prevent a patient infected with HIV from passing the virus to other people. To protect others, you must continue to practice safe sex and take precautions to prevent others from coming in contact with your blood and other body fluids.
There is limited information on the antiviral response of long-term use of didanosine.
In didanosine, an enteric coating is used to protect the medicine while it is in your stomach since stomach acids can break it down. The enteric coating dissolves when the medicine reaches your small intestine.
Who should not take didanosine?
Do not take didanosine if you are allergic to any of its ingredients, including its active ingredient, didanosine, and the inactive ingredients. (See Inactive Ingredients at the end of this leaflet.) Tell your doctor if you think you have had an allergic reaction to any of these ingredients.
How should I take didanosine? How should I store it?
Didanosine should only be taken once daily. Your doctor will determine your dose based on your body weight, kidney and liver function, other medicines you are taking, and any side effects that you may have had with didanosine or other medicines. Take didanosine on an empty stomach. Do not take didanosine with food. Swallow the capsule whole; do not open it. Try not to miss a dose, but if you do, take it as soon as possible. If it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule.
Store capsules in a tightly closed container at room temperature away from heat and out of the reach of children and pets.
If you have kidney disease: If your kidneys are not working properly, your doctor will need to do regular tests to check how they are working while you take didanosine. Your doctor may also lower your dosage of didanosine.
What should I do if someone takes an overdose of didanosine?
If someone may have taken an overdose of didanosine, get medical help right away. Contact their doctor or a poison control center.
What should I avoid while taking didanosine?
Alcohol. Do not drink alcohol while taking didanosine since alcohol may increase your risk of pancreatitis (pain and inflammation of the pancreas) or liver damage.
Allopurinol, also known as ZYLOPRIM®, ALOPRIM®, or others. Do not take allopurinol while taking didanosine because the risk of side-effects of didanosine are increased.
Ribavirin, also known as COPEGUS®, REBETOL®, or others. Do not take ribavirin while taking didanosine because pancreatitis, peripheral neuropathy, lactic acidosis and fatal liver damage have been reported. (See "What are the possible side effects of didanosine?")
Other medicines. Other medicines, including those you can buy without a prescription, may interfere with the actions of didanosine or may increase the possibility or severity of side effects. Do not take any medicine, vitamin supplement, or other health preparation without first checking with your doctor.
Pregnancy. It is not known if didanosine can harm a human fetus. Also, pregnant women have experienced serious side effects when taking didanosine in combination with ZERIT (stavudine), also known as d4T, and other HIV medicines. Didanosine should be used during pregnancy only after discussion with your doctor. Tell your doctor if you become pregnant or plan to become pregnant while taking didanosine.
Nursing. Studies have shown didanosine is in the breast milk of animals getting the drug. It may also be in human breast milk. The Centers for Disease Control and Prevention (CDC) recommends that HIV-infected mothers not breast-feed. This should reduce the risk of passing HIV infection to their babies and the potential for serious adverse reactions in nursing infants. Therefore, do not nurse a baby while taking didanosine.
What are the possible side effects of didanosine?
Pancreatitis. Pancreatitis is a dangerous inflammation of the pancreas that may cause death. Tell your doctor right away if you or a child taking didanosine develop stomach pain, nausea, or vomiting. These can be signs of pancreatitis. Before starting didanosine therapy, let your doctor know if you or a child for whom it has been prescribed have ever had pancreatitis. This condition is more likely to happen in people who have had it before. It is also more likely in people with advanced HIV disease. However, it can occur at any stage of HIV disease. It may be more common in patients with kidney problems, those who drink alcohol, and those who are also treated with stavudine. If you get pancreatitis, your doctor will tell you to stop taking didanosine.
Lactic acidosis, severe liver enlargement, and liver failure, including deaths, have been reported among patients taking didanosine (including pregnant women). Symptoms that may indicate a liver problem are:
• feeling very weak, tired, or uncomfortable
• unusual or unexpected stomach discomfort
• feeling cold
• feeling dizzy or lightheaded
• suddenly developing a slow or irregular heartbeat
Lactic acidosis is a medical emergency that must be treated in a hospital.
If you notice any of these symptoms or if your medical condition changes, stop taking didanosine and call your doctor right away. Women, overweight patients, and those who have been treated for a long time with other medicines used to treat HIV infection are more likely to develop lactic acidosis. Your doctor should check your liver function periodically while you are taking didanosine. You should be especially careful if you have a history of heavy alcohol use or a liver problem.
Vision changes. Didanosine may affect the nerves in your eyes. Because of this, you should have regular eye examinations. You should also report any changes in vision to your doctor right away. This includes, for example, seeing colors abnormally or blurred vision.
Peripheral neuropathy. This is a problem with the nerves in your hands or feet. The nerve problem may be serious. Tell your doctor right away if you or a child taking didanosine have continuing numbness, tingling, or pain in the feet or hands. A child may not recognize these symptoms or know to tell you that his or her feet or hands are numb, burning, tingling, or painful. Ask your child’s doctor how to find out if your child is developing peripheral neuropathy.
Before starting didanosine therapy, let your doctor know if you or a child for whom it has been prescribed have ever had peripheral neuropathy. This condition is more likely to happen in people who have had it before. It is also more likely in patients taking medicines that affect the nerves and in people with advanced HIV disease. However, it can occur at any stage of HIV disease. If you get peripheral neuropathy, your doctor will tell you to stop taking didanosine. After stopping didanosine, the symptoms may get worse for a short time and then get better. Once symptoms of peripheral neuropathy go away completely, you and your doctor should decide if starting didanosine again is right for you.
Special note about other medicines. If you take didanosine along with other medicines with similar side effects, you may increase the chance of having these side effects. For example, using didanosine in combination with other medicines that may cause pancreatitis, peripheral neuropathy, or liver problems (including stavudine) may increase your chance of having these side effects.
Other side effects: The most common side effects in adults taking didanosine in combination with other HIV drugs included diarrhea, nausea, headache, vomiting, and rash. Children may have similar side effects as adults.
Changes in body fat have been seen in some patients taking antiretroviral therapy. These changes may include an increased amount of fat in the upper back and neck (“buffalo hump”), breast, and around the trunk. Loss of fat from the legs, arms, and face may also happen. The cause and long term health effects of these conditions are not known at this time.
Inactive Ingredients:
Croscarmellose sodium, hydroxypropyl cellulose, hypromellose, methacrylic acid copolymer dispersion, microcrystalline cellulose, polydextrose, polyethylene glycol, silicon dioxide, sodium hydroxide, talc, titanium dioxide, triacetin and triethyl citrate. The capsule shell contains FD&C blue no. 1, gelatin, and titanium dioxide. The 200 mg capsule shell also contains D&C red no. 33, and FD&C yellow no. 6. The 250 mg capsule shell also contains D&C red no. 28. The 400 mg capsule shell also contains D&C red no. 33, and FD&C yellow no. 6. The edible imprinting ink contains D&C yellow no. 10 aluminum lake, FD&C blue no. 1 aluminum lake, FD&C blue no. 2 aluminum lake, FD&C red no. 40 aluminum lake, iron oxide, propylene glycol and shellac glaze.
This medicine was prescribed for your particular condition. Do not use didanosine for another condition or give it to others. Keep all medicines out of the reach of children and pets at all times. Do not keep medicine that is out of date or that you no longer need. Dispose of unused medicines through community take-back disposal programs when available or place didanosine in an unrecognizable closed container in the household trash.
This summary does not include everything there is to know about didanosine. Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. If you have questions or concerns, or want more information about didanosine, your physician and pharmacist have the complete prescribing information upon which this leaflet is based. You may want to read it and discuss it with your doctor or other healthcare professional. Remember, no written summary can replace careful discussion with your doctor.
This Patient Information Leaflet has been approved by the U.S. Food and Drug Administration.
Zerit® is a registered trademark of Bristol-Myers Squibb Company.
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
This Product was Repackaged By:
State of Florida DOH Central Pharmacy
104-2 Hamilton Park Drive
Tallahassee, FL 32304
United States
Image of 250 mg Label
_c9891a49.jpg)
NDC 53808-0236-1
DIDANOSINE
Delayed-Release
Capsules (enteric-coated pellets)
250 mg
PHARMACIST: PLEASE DISPENSE WITH
ATTACHED PATIENT INFORMATION LEAFLET
Rx only
30 CAPSULES (Unit-of-Use)
TEVA
Image of 400 mg Label
_c9891a49.jpg)
NDC 53808-0353-1
DIDANOSINE
Delayed-Release
Capsules (enteric-coated pellets)
400 mg
PHARMACIST: PLEASE DISPENSE WITH
ATTACHED PATIENT INFORMATION LEAFLET
Rx only
30 CAPSULES (Unit-of-Use)
TEVA
DidanosineDidanosine CAPSULE, DELAYED RELEASE PELLETS
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
DidanosineDidanosine CAPSULE, DELAYED RELEASE PELLETS
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||