Exforge
HIGHLIGHTS OF PRESCRIBING INFORMATION BOXED WARNING WARNING: AVOID USE IN PREGNANCY See full prescribing information for complete boxed warning . When pregnancy is detected, discontinue Exforge as soon as possible. D rugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus. (5.1) INDICATIONS AND USAGEExforge is the combination tablet of amlodipine, a dihydropyridine calcium channel blocker (DHP CCB), and valsartan, an angiotensin II receptor blocker (ARB). Exforge is indicated for the treatment of hypertension: In patients not adequately controlled on monotherapy (1) As initial therapy in patients likely to need multiple drugs to achieve their blood pressure goals (1). DOSAGE AND ADMINISTRATIONGeneral Considerations Majority of effect attained within 2 weeks (2.1) May be administered with other antihypertensive agents (2.1) Hypertension May be used as add-on therapy for patients not controlled on monotherapy (2.2) Patients who experience dose-limiting adverse reactions on monotherapy may be switched to Exforge containing a lower dose of that component (2.2) May be substituted for titrated components (2.3) When used as initial therapy: Initiate with 5/160 mg, then titrate upwards as necessary to a maximum of 10/320 mg once daily (2.4) DOSAGE FORMS AND STRENGTHS3WARNINGS AND PRECAUTIONS Avoid fetal or neonatal exposure (5.1) Assess for hypotension. (5.2) Warn patients with severe obstructive coronary artery disease about the risk of myocardial infarction or increased angina (5.3) Titrate slowly in patients with impaired hepatic (5.4) or severely impaired renal (5.5) function Side EffectsIn placebo-controlled clinical trials, discontinuation due to side effects occurred in 1.8% of patients in the Exforge-treated patients and 2.1% in the placebo-treated group. The most common reasons for discontinuation of therapy with Exforge were peripheral edema and vertigo. The adverse experiences that occurred in clinical trials (≥2% of patients) at a higher incidence than placebo included peripheral edema, nasopharyngitis, upper respiratory tract infection and dizziness. (6) To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS If simvastatin is co-administered with amlodipine, do not exceed doses greater than 20 mg daily of simvastatin (7) NSAIDS use may lead to increased risk of renal impairment and loss of anti-hypertensive effect (7) USE IN SPECIFIC POPULATIONS8.5 Nursing Mothers: Choose breastfeeding or Exforge therapy, but not both. (8.3)
FULL PRESCRIBING INFORMATION
When pregnancy is detected, discontinue Exforge as soon as possible . Drugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus . [ See W arnings and P recautions (5.1) ]
Exforge (amlodipine and valsartan) is indicated for the treatment of hypertension.
Exforge may be used in patients whose blood pressure is not adequately controlled on either monotherapy.
Exforge may also be used as initial therapy in patients who are likely to need multiple drugs to achieve their blood pressure goals.
The choice of Exforge as initial therapy for hypertension should be based on an assessment of potential benefits and risks including whether the patient is likely to tolerate the lowest dose of Exforge.
Patients with stage 2 hypertension (moderate or severe) are at a relatively higher risk for cardiovascular events (such as strokes, heart attacks, and heart failure), kidney failure and vision problems, so prompt treatment is clinically relevant. The decision to use a combination as initial therapy should be individualized and should be shaped by considerations such as baseline blood pressure, the target goal and the incremental likelihood of achieving goal with a combination compared to monotherapy. Individual blood pressure goals may vary based upon the patient’s risk.
Data from the high-dose multifactorial study [see Clinical Studies (14)] provide estimates of the probability of reaching a blood pressure goal with Exforge compared to amlodipine or valsartan monotherapy. The figures below provide estimates of the likelihood of achieving systolic or diastolic blood pressure control with Exforge 10/320 mg, based upon baseline systolic or diastolic blood pressure. The curve of each treatment group was estimated by logistic regression modeling. The estimated likelihood at the right tail of each curve is less reliable due to small numbers of subjects with high baseline blood pressures.

Figure 1: Probability of Achieving Systolic Blood Pressure <140 mmHg at Week 8 |
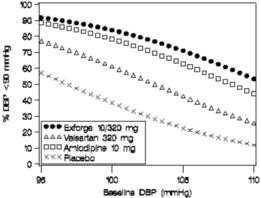
Figure 2: Probability of Achieving Diastolic Blood Pressure <90 mmHg at Week 8 |

Figure 3: Probability of Achieving Systolic Blood Pressure <130 mmHg at Week 8 |

Figure 4: Probability of Achieving Diastolic Blood Pressure <80 mmHg at Week 8 |
For example, a patient with a baseline blood pressure of 160/100 mmHg has about a 67% likelihood of achieving a goal of <140 mmHg (systolic) and 80% likelihood of achieving <90 mmHg (diastolic) on amlodipine alone, and the likelihood of achieving these goals on valsartan alone is about 47% (systolic) or 62% (diastolic). The likelihood of achieving these goals on Exforge rises to about 80% (systolic) or 85% (diastolic). The likelihood of achieving these goals on placebo is about 28% (systolic) or 37% (diastolic).
Amlodipine is an effective treatment of hypertension in once daily doses of 2.5 mg to 10 mg while valsartan is effective in doses of 80 mg to 320 mg. In clinical trials with once daily Exforge (amlodipine and valsartan) using amlodipine doses of 5 mg to 10 mg and valsartan doses of 160 mg to 320 mg, the antihypertensive effects increased with increasing doses.
The hazards [see W arnings and Precautions(5)] of valsartan are generally independent of dose; those of amlodipine are a mixture of dose-dependent phenomena (primarily peripheral edema) and dose-independent phenomena, the former much more common than the latter [s ee Adverse Reactions (6)].
The majority of the antihypertensive effect is attained within 2 weeks after initiation of therapy or a change in dose. The dosage can be increased after 1 to 2 weeks of therapy to a maximum of one 10/320 mg tablet once daily as needed to control blood pressure [s ee Clinical Studies (14)].
Exforge may be administered with or without food.
Exforge may be administered with other antihypertensive agents.
Elderly patients: Because of decreased clearance of amlodipine, therapy should usually be initiated at 2.5 mg.
Renal Impairment: No initial dosage adjustment is required for patients with mild or moderate renal impairment. Titrate slowly in patients with severe renal impairment.
Hepatic Impairment: No initial dosage adjustment is required for patients with mild or moderate liver insufficiency. Titrate slowly in patients with hepatic impairment.
A patient whose blood pressure is not adequately controlled with amlodipine (or another dihydropyridine calcium-channel blocker) alone or with valsartan (or another angiotensin II receptor blocker) alone may be switched to combination therapy with Exforge.
A patient who experiences dose-limiting adverse reactions on either component alone may be switched to Exforge containing a lower dose of that component in combination with the other to achieve similar blood pressure reductions. The clinical response to Exforge should be subsequently evaluated and if blood pressure remains uncontrolled after 3 to 4 weeks of therapy, the dose may be titrated up to a maximum of 10/320 mg.
For convenience, patients receiving amlodipine and valsartan from separate tablets may instead wish to receive tablets of Exforge containing the same component doses.
A patient may be initiated on Exforge if it is unlikely that control of blood pressure would be achieved with a single agent. The usual starting dose is Exforge 5/160 mg once daily in patients who are not volume-depleted.
5/160 mg tablets, debossed with NVR/ECE (side 1/side 2)
10/160 mg tablets, debossed with NVR/UIC
5/320 mg tablets, debossed with NVR/CSF
10/320 mg tablets, debossed with NVR/LUF
None.
Exforge can cause fetal harm when administered to a pregnant woman. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Drugs that act on the renin angiotensin system can cause fetal and neonatal morbidity and mortality when used in pregnancy. In several dozen published cases, ACE inhibitor use during the second and third trimesters of pregnancy was associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death [s ee Use in Specific Populations (8.1)].
Excessive hypotension was seen in 0.4% of patients with uncomplicated hypertension treated with Exforge in placebo-controlled studies. In patients with an activated renin-angiotensin system, such as volume-and/or salt-depleted patients receiving high doses of diuretics, symptomatic hypotension may occur in patients receiving angiotensin receptor blockers. Volume depletion should be corrected prior to administration of Exforge. Treatment with Exforge should start under close medical supervision.
Initiate therapy cautiously in patients with heart failure or recent myocardial infarction and in patients undergoing surgery or dialysis. Patients with heart failure or post-myocardial infarction patients given valsartan commonly have some reduction in blood pressure, but discontinuation of therapy because of continuing symptomatic hypotension usually is not necessary when dosing instructions are followed. In controlled trials in heart failure patients, the incidence of hypotension in valsartan-treated patients was 5.5% compared to 1.8% in placebo-treated patients. In the Valsartan in Acute Myocardial Infarction Trial (VALIANT), hypotension in post-myocardial infarction patients led to permanent discontinuation of therapy in 1.4% of valsartan-treated patients and 0.8% of captopril-treated patients.
Since the vasodilation induced by amlodipine is gradual in onset, acute hypotension has rarely been reported after oral administration. Nonetheless, caution, as with any other peripheral vasodilator, should be exercised when administering amlodipine, particularly in patients with severe aortic stenosis.
If excessive hypotension occurs with Exforge, the patient should be placed in a supine position and, if necessary, given an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
Rarely, patients, particularly those with severe obstructive coronary artery disease, have developed documented increased frequency, duration or severity of angina or acute myocardial infarction on starting calcium channel blocker therapy or at the time of dosage increase. The mechanism of this effect has not been elucidated.
Studies with A mlodipine: Amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t½) is 56 hours in patients with impaired hepatic function, therefore, caution should be exercised when administering amlodipine to patients with severe hepatic impairment.
Studies with V alsartan: As the majority of valsartan is eliminated in the bile, patients with mild-to-moderate hepatic impairment, including patients with biliary obstructive disorders, showed lower valsartan clearance (higher AUCs). Care should be exercised in administering valsartan to these patients.
In studies of ACE inhibitors in hypertensive patients with unilateral or bilateral renal artery stenosis, increases in serum creatinine or blood urea nitrogen have been reported. In a 4-day trial of valsartan in 12 hypertensive patients with unilateral renal artery stenosis, no significant increases in serum creatinine or blood urea nitrogen were observed. There has been no long-term use of valsartan in patients with unilateral or bilateral renal artery stenosis, but an effect similar to that seen with ACE inhibitors should be anticipated.
As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function may occur particularly in volume depleted patients. In patients with severe heart failure whose renal function may depend on the activity of the renin-angiotensin-aldosterone system, treatment with angiotensin-converting enzyme inhibitors and angiotensin receptor antagonists has been associated with oliguria and/or progressive azotemia and (rarely) with acute renal failure and/or death. Similar outcomes have been reported with valsartan.
Studies with A mlodipine: In general, calcium channel blockers should be used with caution in patients with heart failure. Amlodipine (5-10 mg per day) has been studied in a placebo-controlled trial of 1,153 patients with NYHA Class III or IV heart failure on stable doses of ACE inhibitor, digoxin, and diuretics. Follow-up was at least 6 months, with a mean of about 14 months. There was no overall adverse effect on survival or cardiac morbidity (as defined by life-threatening arrhythmia, acute myocardial infarction, or hospitalization for worsened heart failure). Amlodipine has been compared to placebo in four 8-12 week studies of patients with NYHA class II/III heart failure, involving a total of 697 patients. In these studies, there was no evidence of worsened heart failure based on measures of exercise tolerance, NYHA classification, symptoms, or LVEF.
Studies with V alsartan: Some patients with heart failure have developed increases in blood urea nitrogen, serum creatinine, and potassium on valsartan. These effects are usually minor and transient, and they are more likely to occur in patients with pre-existing renal impairment. Dosage reduction and/or discontinuation of the diuretic and/or valsartan may be required. In the Valsartan Heart Failure Trial, in which 93% of patients were on concomitant ACE inhibitors, treatment was discontinued for elevations in creatinine or potassium (total of 1.0% on valsartan vs. 0.2% on placebo). In the Valsartan in Acute Myocardial Infarction Trial (VALIANT), discontinuation due to various types of renal dysfunction occurred in 1.1% of valsartan-treated patients and 0.8% of captopril-treated patients. Evaluation of patients with heart failure or post-myocardial infarction should always include assessment of renal function.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Studies with Exforge :
Exforge has been evaluated for safety in over 2,600 patients with hypertension; over 1,440 of these patients were treated for at least 6 months and over 540 of these patients were treated for at least one year. Adverse reactions have generally been mild and transient in nature and have only infrequently required discontinuation of therapy.
The overall frequency of adverse reactions was neither dose-related nor related to gender, age, or race. In placebo-controlled clinical trials, discontinuation due to side effects occurred in 1.8% of patients in the Exforge-treated patients and 2.1% in the placebo-treated group. The most common reasons for discontinuation of therapy with Exforge were peripheral edema (0.4%), and vertigo (0.2%).
The adverse reactions that occurred in placebo-controlled clinical trials in at least 2% of patients treated with Exforge but at a higher incidence in amlodipine/valsartan patients (n=1,437) than placebo (n=337) included peripheral edema (5.4% vs. 3.0%), nasopharyngitis (4.3% vs. 1.8%), upper respiratory tract infection (2.9% vs 2.1%) and dizziness (2.1% vs 0.9%).
Orthostatic events (orthostatic hypotension and postural dizziness) were seen in less than 1% of patients.
Other adverse reactions that occurred in placebo-controlled clinical trials with Exforge (≥ 0.2%) are listed below. It cannot be determined whether these events were causally related to Exforge.
Blood and Lymphatic System Disorders: Lymphadenopathy
Cardiac Disorders: Palpitations, tachycardia
Ear and Labyrinth Disorders: Ear pain
Gastrointestinal Disorders: Diarrhea, nausea, constipation, dyspepsia, abdominal pain, abdominal pain upper, gastritis, vomiting, abdominal discomfort, abdominal distention, dry mouth, colitis
General Disorders and Administration Site Conditions: Fatigue, chest pain, asthenia, pitting edema, pyrexia, edema
Immune System Disorders: Seasonal allergies
Infections and Infestations: Nasopharyngitis, sinusitis, bronchitis, pharyngitis, gastroenteritis, pharyngotonsillitis, bronchitis acute, tonsillitis
Injury and Poisoning: Epicondylitis, joint sprain, limb injury
Metabolism and Nutrition Disorders: Gout, non-insulin dependent diabetes mellitus, hypercholesterolemia
Musculoskeletal and Connective Tissue Disorders: Arthralgia, back pain, muscle spasms, pain in extremity, myalgia, osteoarthritis, joint swelling, musculoskeletal chest pain
Nervous System Disorders: Headache, sciatica, paresthesia, cervicobrachial syndrome, carpal tunnel syndrome, hypoesthesia, sinus headache, somnolence
Psychiatric Disorders: Insomnia, anxiety, depression
Renal and Urinary Disorders: Hematuria, nephrolithiasis, pollakiuria
Reproductive System and Breast Disorders: Erectile dysfunction
Respiratory, Thoracic and Mediastinal Disorders: Cough, pharyngolaryngeal pain, sinus congestion, dyspnea, epistaxis, productive cough, dysphonia, nasal congestion
Skin and Subcutaneous Tissue Disorders: Pruritus, rash, hyperhidrosis, eczema, erythema
Vascular Disorders: Flushing, hot flush
Isolated cases of the following clinically notable adverse reactions were also observed in clinical trials: exanthema, syncope, visual disturbance, hypersensitivity, tinnitus, and hypotension.
Studies with Amlodipine:
Norvasc® * has been evaluated for safety in more than 11,000 patients in U.S. and foreign clinical trials. Other adverse events that have been reported <1% but >0.1% of patients in controlled clinical trials or under conditions of open trials or marketing experience where a causal relationship is uncertain were:
Cardiovascular: arrhythmia (including ventricular tachycardia and atrial fibrillation), bradycardia, chest pain, peripheral ischemia, syncope, postural hypotension, vasculitis
Central and Peripheral Nervous System: neuropathy peripheral, tremor
Gastrointestinal: anorexia, dysphagia, pancreatitis, gingival hyperplasia
General: allergic reaction, hot flushes, malaise, rigors, weight gain, weight loss
Musculoskeletal System: arthrosis, muscle cramps
Psychiatric: sexual dysfunction (male and female), nervousness, abnormal dreams, depersonalization
Respiratory System: dyspnea
Skin and Appendages: angioedema, erythema multiforme, rash erythematous, rash maculopapular
Special Senses: abnormal vision, conjunctivitis, diplopia, eye pain, tinnitus
Urinary System: micturition frequency, micturition disorder, nocturia
Autonomic Nervous System: sweating increased
Metabolic and Nutritional: hyperglycemia, thirst
Hemopoietic: leukopenia, purpura, thrombocytopenia
Other events reported with amlodipine at a frequency of ≤0.1% of patients include: cardiac failure, pulse irregularity, extrasystoles, skin discoloration, urticaria, skin dryness, alopecia, dermatitis, muscle weakness, twitching, ataxia, hypertonia, migraine, cold and clammy skin, apathy, agitation, amnesia, gastritis, increased appetite, loose stools, rhinitis, dysuria, polyuria, parosmia, taste perversion, abnormal visual accommodation, and xerophthalmia. Other reactions occurred sporadically and cannot be distinguished from medications or concurrent disease states such as myocardial infarction and angina.
Adverse reactions reported for amlodipine for indications other than hypertension may be found in the prescribing information for Norvasc.
Studies with Valsartan:
Diovan® has been evaluated for safety in more than 4,000 hypertensive patients in clinical trials. In trials in which valsartan was compared to an ACE inhibitor with or without placebo, the incidence of dry cough was significantly greater in the ACE inhibitor group (7.9%) than in the groups who received valsartan (2.6%) or placebo (1.5%). In a 129 patient trial limited to patients who had had dry cough when they had previously received ACE inhibitors, the incidences of cough in patients who received valsartan, HCTZ, or lisinopril were 20%, 19%, and 69% respectively (p<0.001).
Other adverse reactions, not listed above, occurring in >0.2% of patients in controlled clinical trials with valsartan are:
Body as a Whole: allergic reaction, asthenia
Musculoskeletal: muscle cramps
Neurologic and Psychiatric: paresthesia
Respiratory: sinusitis, pharyngitis
Urogenital: impotence
Other reported events seen less frequently in clinical trials were: angioedema.
Adverse reactions reported for valsartan for indications other than hypertension may be found in the prescribing information for Diovan.
Amlodipine: Gynecomastia has been reported infrequently and a causal relationship is uncertain. Jaundice and hepatic enzyme elevations (mostly consistent with cholestasis or hepatitis), in some cases severe enough to require hospitalization, have been reported in association with use of amlodipine.
Valsartan: The following additional adverse reactions have been reported in postmarketing experience with valsartan:
Blood and Lymphatic: There are very rare reports of thrombocytopenia.
Hypersensitivity: There are rare reports of angioedema.
Digestive: Elevated liver enzymes and very rare reports of hepatitis
Renal: Impaired renal function
Clinical Laboratory Tests: Hyperkalemia
Dermatologic: Alopecia
Vascular: Vasculitis
Rare cases of rhabdomyolysis have been reported in patients receiving angiotensin II receptor blockers.
No drug interaction studies have been conducted with Exforge and other drugs, although studies have been conducted with the individual amlodipine and valsartan components, as described below:
Studies with Amlodipine
In clinical trials, amlodipine has been safely administered with thiazide diuretics, beta-blockers, angiotensin-converting enzyme inhibitors, long-acting nitrates, sublingual nitroglycerin, digoxin, warfarin, non-steroidal anti-inflammatory drugs, antibiotics, and oral hypoglycemic drugs.
Cimetidine: Co-administration of amlodipine with cimetidine did not alter the pharmacokinetics of amlodipine.
Grapefruit juice: Co-administration of 240 mL of grapefruit juice with a single oral dose of amlodipine 10 mg in 20 healthy volunteers had no significant effect on the pharmacokinetics of amlodipine.
Maalox ® (antacid): Co-administration of the antacid Maalox with a single dose of amlodipine had no significant effect on the pharmacokinetics of amlodipine.
Sildenafil: A single 100 mg dose of sildenafil (Viagra®**) in subjects with essential hypertension had no effect on the pharmacokinetic parameters of amlodipine. When amlodipine and sildenafil were used in combination, each agent independently exerted its own blood pressure lowering effect.
Atorvastatin: Co-administration of multiple 10 mg doses of amlodipine with 80 mg of atorvastatin resulted in no significant change in the steady state pharmacokinetic parameters of atorvastatin.
Digoxin: Co-administration of amlodipine with digoxin did not change serum digoxin levels or digoxin renal clearance in normal volunteers.
Warfarin: Co-administration of amlodipine with warfarin did not change the warfarin prothrombin response time.
Simvastatin: Co-administration of multiple doses of 10 mg of amlodipine with 80 mg simvastatin resulted in a 77% increase in exposure to simvastatin compared to simvastatin alone. Limit the dose of simvastatin in patients on amlodipine to 20 mg daily.
Studies with Valsartan
No clinically significant pharmacokinetic interactions were observed when valsartan was co-administered with amlodipine, atenolol, cimetidine, digoxin, furosemide, glyburide, hydrochlorothiazide, or indomethacin. The valsartan-atenolol combination was more antihypertensive than either component, but it did not lower the heart rate more than atenolol alone.
Warfarin: Co-administration of valsartan and warfarin did not change the pharmacokinetics of valsartan or the time-course of the anticoagulant properties of warfarin.
Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors) : In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, co-administration of NSAIDs, including selective COX-2 inhibitors, with angiotensin II receptor antagonists, including valsartan, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically in patients receiving valsartan and NSAID therapy.
The antihypertensive effect of angiotensin II receptor antagonists, including valsartan may be attenuated by NSAIDs including selective COX-2 inhibitors.
In vitro metabolism studies indicate that CYP 450 mediated drug interactions between valsartan and co-administered drugs are unlikely because of low extent of metabolism [see Pharmacokinetics, Valsartan (12.3)]. As with other drugs that block angiotensin II or its effects, concomitant use of potassium sparing diuretics (e.g., spironolactone, triamterene, amiloride), potassium supplements, or salt substitutes containing potassium may lead to increases in serum potassium and in heart failure patients to increases in serum creatinine.
The results from an in vitro study with human liver tissue indicate that valsartan is a substrate of the hepatic uptake transporter OATP1B1 and the hepatic efflux transporter MRP2. Co-administration of inhibitors of the uptake transporter (rifampin, cyclosporine) or efflux transporter (ritonavir) may increase the systemic exposure to valsartan.
Creatinine : In hypertensive patients, greater than 50% increases in creatinine occurred in 0.4% of patients receiving Exforge and 0.6% receiving placebo. In heart failure patients, greater than 50% increases in creatinine were observed in 3.9% of valsartan-treated patients compared to 0.9% of placebo-treated patients. In post-myocardial infarction patients, doubling of serum creatinine was observed in 4.2% of valsartan-treated patients and 3.4% of captopril-treated patients.
Liver Function Tests : Occasional elevations (greater than 150%) of liver chemistries occurred in Exforge-treated patients.
Serum Potassium : In hypertensive patients, greater than 20% increases in serum potassium were observed in 2.8% of Exforge-treated patients compared to 3.4% of placebo-treated patients. In heart failure patients, greater than 20% increases in serum potassium were observed in 10% of valsartan-treated patients compared to 5.1% of placebo-treated patients.
Blood Urea Nitrogen (BUN) : In hypertensive patients, greater than 50% increases in BUN were observed in 5.5% of Exforge-treated patients compared to 4.7% of placebo-treated patients. In heart failure patients, greater than 50% increases in BUN were observed in 16.6% of valsartan-treated patients compared to 6.3% of placebo-treated patients.
Neutropenia: Neutropenia was observed in 1.9% of patients treated with Diovan and 0.8% of patients treated with placebo.
Pregnancy Category D [see W arnings and P recautions (5.1)]
Exforge, like other drugs that act on the renin angiotensin system, can cause fetal and neonatal morbidity and death when used during the second or third trimester of pregnancy. Exforge can cause fetal harm when administered to a pregnant woman. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Angiotensin II receptor antagonists, like valsartan, and angiotensin converting enzyme (ACE) inhibitors exert similar effects on the renin-angiotensin system. In several dozen published cases, ACE inhibitor use during the second and third trimesters of pregnancy was associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios was also reported, presumably from decreased fetal renal function. In this setting, oligohydramnios was associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus were also reported, although it is not clear whether these occurrences were due to exposure to the drug. In a retrospective study, first trimester use of ACE inhibitors, a specific class of drugs acting on the renin angiotensin system, was associated with a potential risk of birth defects.
When pregnancy occurs in a patient using Exforge, the physician should discontinue Exforge treatment as soon as possible. The physician should inform the patient about potential risks to the fetus based on the time of gestational exposure to Exforge (first trimester only or later). If exposure occurs beyond the first trimester, an ultrasound examination should be done.
In rare cases when another antihypertensive agent cannot be used to treat the pregnant patient, serial ultrasound examinations should be performed to assess the intraamniotic environment. Routine fetal testing with non-stress tests, biophysical profiles, and/or contraction stress tests may be appropriate based on gestational age and standards of care in the community. If oligohydramnios occurs in these situations, individualized decisions about continuing or discontinuing Exforge treatment and about pregnancy management should be made by the patient, her physician, and experts in the management of high risk pregnancy. Patients and physicians should be aware that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Infants with histories of in utero exposure to Exforge should be closely observed for hypotension, oliguria, and hyperkalemia. If oliguria occurs, these infants may require blood pressure and renal perfusion support. Exchange transfusion or dialysis may be required to reverse hypotension and/or support decreased renal function.
Healthcare professionals who prescribe drugs acting directly on the renin angiotensin system should counsel women of childbearing potential about the risks of these agents during pregnancy [see Nonclincial Toxicology (13.2)].
The effect of Exforge on labor and delivery has not been studied.
It is not known whether amlodipine is excreted in human milk. In the absence of this information, it is recommended that nursing be discontinued while amlodipine is administered.
It is not known whether valsartan is excreted in human milk. Valsartan was excreted into the milk of lactating rats; however, animal breast milk drug levels may not accurately reflect human breast milk levels. Because many drugs are excreted into human milk and because of the potential for adverse reactions in nursing infants from Exforge, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Safety and effectiveness of Exforge in pediatric patients have not been established.
In controlled clinical trials, 323 (22.5%) hypertensive patients treated with Exforge were ≥65 years and 79 (5.5%) were ≥75 years. No overall differences in the efficacy or safety of Exforge was observed in this patient population, but greater sensitivity of some older individuals cannot be ruled out.
Amlodipine: Clinical studies of amlodipine besylate tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased clearance of amlodipine with a resulting increase of AUC of approximately 40-60%, and a lower initial dose may be required [see Dosage and Administration (2.1)].
Valsartan: In the controlled clinical trials of valsartan, 1,214 (36.2%) of hypertensive patients treated with valsartan were ≥65 years and 265 (7.9%) were ≥75 years. No overall difference in the efficacy or safety of valsartan was observed in this patient population, but greater sensitivity of some older individuals cannot be ruled out.
Information on Amlodipine
Single oral doses of amlodipine maleate equivalent to 40 mg/kg and 100 mg/kg amlodipine in mice and rats, respectively, caused deaths. Single oral doses equivalent to 4 or more mg/kg amlodipine in dogs (11 or more times the maximum recommended human dose on a mg/m2 basis) caused a marked peripheral vasodilation and hypotension.
Overdosage might be expected to cause excessive peripheral vasodilation with marked hypotension. In humans, experience with intentional overdosage of amlodipine is limited. Reports of intentional overdosage include a patient who ingested 250 mg and was asymptomatic and was not hospitalized; another (120 mg) who was hospitalized underwent gastric lavage and remained normotensive; the third (105 mg) was hospitalized and had hypotension (90/50 mmHg) which normalized following plasma expansion. A case of accidental drug overdose has been documented in a 19-month-old male who ingested 30 mg amlodipine (about 2 mg/kg). During the emergency room presentation, vital signs were stable with no evidence of hypotension, but a heart rate of 180 bpm. Ipecac was administered 3.5 hours after ingestion and on subsequent observation (overnight) no sequelae was noted.
If massive overdose should occur, active cardiac and respiratory monitoring should be instituted. Frequent blood pressure measurements are essential. Should hypotension occur, cardiovascular support including elevation of the extremities and the judicious administration of fluids should be initiated. If hypotension remains unresponsive to these conservative measures, administration of vasopressors (such as phenylephrine) should be considered with attention to circulating volume and urine output. Intravenous calcium gluconate may help to reverse the effects of calcium entry blockade. As amlodipine is highly protein bound, hemodialysis is not likely to be of benefit.
Information on Valsartan
Limited data are available related to overdosage in humans. The most likely effect of overdose with valsartan would be peripheral vasodilation, hypotension and tachycardia; bradycardia could occur from parasympathetic (vagal) stimulation. Depressed level of consciousness, circulatory collapse and shock have been reported. If symptomatic hypotension should occur, supportive treatment should be instituted.
Valsartan is not removed from the plasma by hemodialysis.
Valsartan was without grossly observable adverse effects at single oral doses up to 2000 mg/kg in rats and up to 1000 mg/kg in marmosets, except for the salivation and diarrhea in the rat and vomiting in the marmoset at the highest dose (60 and 37 times, respectively, the maximum recommended human dose on a mg/m2 basis). (Calculations assume an oral dose of 320 mg/day and a 60-kg patient.)
Exforge is a fixed combination of amlodipine and valsartan.
Exforge contains the besylate salt of amlodipine, a dihydropyridine calcium-channel blocker (CCB). Amlodipine besylate is a white to pale yellow crystalline powder, slightly soluble in water and sparingly soluble in ethanol. Amlodipine besylate’s chemical name is 3-Ethyl-5-methyl(4RS)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-6-methyl-1,4-dihydropyridine-3,5-dicarboxylate benzenesulphonate; its structural formula is

Its empirical formula is C20H25ClN2O5•C6H6O3S and its molecular weight is 567.1.
Valsartan is a nonpeptide, orally active, and specific angiotensin II antagonist acting on the AT1 receptor subtype. Valsartan is a white to practically white fine powder, soluble in ethanol and methanol and slightly soluble in water. Valsartan’s chemical name is N-(1-oxopentyl)-N-[[2’-(1H-tetrazol-5-yl) [1,1’-biphenyl]-4-yl]methyl]-L-valine; its structural formula is

Its empirical formula is C24H29N5O3 and its molecular weight is 435.5.
Exforge tablets are formulated in four strengths for oral administration with a combination of amlodipine besylate, equivalent to 5 mg or 10 mg of amlodipine free-base, with 160 mg, or 320 mg of valsartan providing for the following available combinations: 5/160 mg, 10/160 mg, 5/320 mg, and 10/320 mg.
The inactive ingredients for all strengths of the tablets are colloidal silicon dioxide, crospovidone, magnesium stearate and microcrystalline cellulose. Additionally the 5/320 mg and 10/320 mg strengths contain iron oxide yellow and sodium starch glycolate. The film coating contains hypromellose, iron oxides, polyethylene glycol, talc and titanium dioxide.
Amlodipine
Amlodipine is a dihydropyridine calcium channel blocker that inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac muscle. Experimental data suggest that amlodipine binds to both dihydropyridine and nondihydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic effects can be detected in vitro but such effects have not been seen in intact animals at therapeutic doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range, amlodipine is an ionized compound (pKa=8.6), and its kinetic interaction with the calcium channel receptor is characterized by a gradual rate of association and dissociation with the receptor binding site, resulting in a gradual onset of effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause a reduction in peripheral vascular resistance and reduction in blood pressure.
Valsartan
Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin-converting enzyme (ACE, kininase II). Angiotensin II is the principal pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation, and renal reabsorption of sodium. Valsartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT1 receptor in many tissues, such as vascular smooth muscle and the adrenal gland. Its action is therefore independent of the pathways for angiotensin II synthesis.
There is also an AT2 receptor found in many tissues, but AT2 is not known to be associated with cardiovascular homeostasis. Valsartan has much greater affinity (about 20,000-fold) for the AT1 receptor than for the AT2 receptor. The increased plasma levels of angiotensin following AT1 receptor blockade with valsartan may stimulate the unblocked AT2 receptor. The primary metabolite of valsartan is essentially inactive with an affinity for the AT1 receptor about one-200th that of valsartan itself.
Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is widely used in the treatment of hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction also catalyzed by ACE. Because valsartan does not inhibit ACE (kininase II), it does not affect the response to bradykinin. Whether this difference has clinical relevance is not yet known. Valsartan does not bind to or block other hormone receptors or ion channels known to be important in cardiovascular regulation.
Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and angiotensin II circulating levels do not overcome the effect of valsartan on blood pressure.
Amlodipine
Following administration of therapeutic doses to patients with hypertension, amlodipine produces vasodilation resulting in a reduction of supine and standing blood pressures. These decreases in blood pressure are not accompanied by a significant change in heart rate or plasma catecholamine levels with chronic dosing. Although the acute intravenous administration of amlodipine decreases arterial blood pressure and increases heart rate in hemodynamic studies of patients with chronic stable angina, chronic oral administration of amlodipine in clinical trials did not lead to clinically significant changes in heart rate or blood pressures in normotensive patients with angina.
With chronic once daily administration, antihypertensive effectiveness is maintained for at least 24 hours. Plasma concentrations correlate with effect in both young and elderly patients. The magnitude of reduction in blood pressure with amlodipine is also correlated with the height of pretreatment elevation; thus, individuals with moderate hypertension (diastolic pressure 105-114 mmHg) had about a 50% greater response than patients with mild hypertension (diastolic pressure 90-104 mmHg). Normotensive subjects experienced no clinically significant change in blood pressure (+1/-2 mmHg).
In hypertensive patients with normal renal function, therapeutic doses of amlodipine resulted in a decrease in renal vascular resistance and an increase in glomerular filtration rate and effective renal plasma flow without change in filtration fraction or proteinuria.
As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine have generally demonstrated a small increase in cardiac index without significant influence on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine has not been associated with a negative inotropic effect when administered in the therapeutic dose range to intact animals and man, even when co-administered with beta-blockers to man. Similar findings, however, have been observed in normals or well-compensated patients with heart failure with agents possessing significant negative inotropic effects.
Amlodipine does not change sinoatrial nodal function or atrioventricular conduction in intact animals or man. In patients with chronic stable angina, intravenous administration of 10 mg did not significantly alter A-H and H-V conduction and sinus node recovery time after pacing. Similar results were obtained in patients receiving amlodipine and concomitant beta-blockers. In clinical studies in which amlodipine was administered in combination with beta-blockers to patients with either hypertension or angina, no adverse effects of electrocardiographic parameters were observed. In clinical trials with angina patients alone, amlodipine therapy did not alter electrocardiographic intervals or produce higher degrees of AV blocks.
Amlodipine has indications other than hypertension which can be found in the Norvasc* package insert.
Valsartan
Valsartan inhibits the pressor effect of angiotensin II infusions. An oral dose of 80 mg inhibits the pressor effect by about 80% at peak with approximately 30% inhibition persisting for 24 hours. No information on the effect of larger doses is available.
Removal of the negative feedback of angiotensin II causes a 2- to 3-fold rise in plasma renin and consequent rise in angiotensin II plasma concentration in hypertensive patients. Minimal decreases in plasma aldosterone were observed after administration of valsartan; very little effect on serum potassium was observed.
In multiple dose studies in hypertensive patients with stable renal insufficiency and patients with renovascular hypertension, valsartan had no clinically significant effects on glomerular filtration rate, filtration fraction, creatinine clearance, or renal plasma flow.
Administration of valsartan to patients with essential hypertension results in a significant reduction of sitting, supine, and standing systolic blood pressure, usually with little or no orthostatic change. Valsartan has indications other than hypertension which can be found in the Diovan package insert.
Exforge
Exforge has been shown to be effective in lowering blood pressure. Both amlodipine and valsartan lower blood pressure by reducing peripheral resistance, but calcium influx blockade and reduction of angiotensin II vasoconstriction are complementary mechanisms.
Amlodipine
Peak plasma concentrations of amlodipine are reached 6-12 hours after administration of amlodipine alone. Absolute bioavailability has been estimated to be between 64% and 90%. The bioavailability of amlodipine is not altered by the presence of food.
The apparent volume of distribution of amlodipine is 21 L/kg. Approximately 93% of circulating amlodipine is bound to plasma proteins in hypertensive patients.
Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism with 10% of the parent compound and 60% of the metabolites excreted in the urine.
Elimination of amlodipine from the plasma is biphasic with a terminal elimination half-life of about 30-50 hours. Steady state plasma levels of amlodipine are reached after 7-8 days of consecutive daily dosing.
Valsartan
Following oral administration of valsartan alone peak plasma concentrations of valsartan are reached in 2-4 hours. Absolute bioavailability is about 25% (range 10%-35%). Food decreases the exposure (as measured by AUC) to valsartan by about 40% and peak plasma concentration (Cmax) by about 50%.
The steady state volume of distribution of valsartan after intravenous administration is 17 L indicating that valsartan does not distribute into tissues extensively. Valsartan is highly bound to serum proteins (95%), mainly serum albumin.
Valsartan shows bi-exponential decay kinetics following intravenous administration with an average elimination half-life of about 6 hours. The recovery is mainly as unchanged drug, with only about 20% of dose recovered as metabolites. The primary metabolite, accounting for about 9% of dose, is valeryl 4-hydroxy valsartan. In vitro metabolism studies involving recombinant CYP 450 enzymes indicated that the CYP 2C9 isoenzyme is responsible for the formation of valeryl-4-hydroxy valsartan. Valsartan does not inhibit CYP 450 isozymes at clinically relevant concentrations. CYP 450 mediated drug interaction between valsartan and co-administered drugs are unlikely because of the low extent of metabolism.
Valsartan, when administered as an oral solution, is primarily recovered in feces (about 83% of dose) and urine (about 13% of dose). Following intravenous administration, plasma clearance of valsartan is about 2 L/h and its renal clearance is 0.62 L/h (about 30% of total clearance).
Exforge
Following oral administration of Exforge in normal healthy adults, peak plasma concentrations of valsartan and amlodipine are reached in 3 and 6-8 hours, respectively. The rate and extent of absorption of valsartan and amlodipine from Exforge are the same as when administered as individual tablets. The bioavailabilities of amlodipine and valsartan are not altered by the co-administration of food.
Special Populations
Geriatric
Studies with Amlodipine : Elderly patients have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40%-60%; therefore a lower initial dose of amlodipine may be required.
Studies with Valsartan : Exposure (measured by AUC) to valsartan is higher by 70% and the half-life is longer by 35% in the elderly than in the young. No dosage adjustment is necessary.
Gender
Studies with Valsartan: Pharmacokinetics of valsartan does not differ significantly between males and females.
Renal Insufficiency
Studies with Amlodipine: The pharmacokinetics of amlodipine is not significantly influenced by renal impairment. Patients with renal failure may therefore receive the usual initial dose.
Studies with Valsartan: There is no apparent correlation between renal function (measured by creatinine clearance) and exposure (measured by AUC) to valsartan in patients with different degrees of renal impairment. Consequently, dose adjustment is not required in patients with mild-to-moderate renal dysfunction. No studies have been performed in patients with severe impairment of renal function (creatinine clearance <10 mL/min). Valsartan is not removed from the plasma by hemodialysis. In the case of severe renal disease, exercise care with dosing of valsartan.
Hepatic Insufficiency
Studies with Amlodipine: Patients with hepatic insufficiency have decreased clearance of amlodipine with resulting increase in AUC of approximately 40%-60%; therefore, a lower initial dose of amlodipine may be required.
Studies with Valsartan: On average, patients with mild-to-moderate chronic liver disease have twice the exposure (measured by AUC values) to valsartan of healthy volunteers (matched by age, sex and weight). In general, no dosage adjustment is needed in patients with mild-to-moderate liver disease. Care should be exercised in patients with liver disease.
Studies with A mlodipine
Rats and mice treated with amlodipine maleate in the diet for up to two years, at concentrations calculated to provide daily dosage levels of 0.5, 1.25, and 2.5 mg amlodipine/kg/day, showed no evidence of a carcinogenic effect of the drug. For the mouse, the highest dose was, on mg/m2 basis, similar to the maximum recommended human dose [MRHD] of 10 mg amlodipine/day. For the rat, the highest dose was, on a mg/m2 basis, about two and a half times the MRHD. (Calculations based on a 60 kg patient.)
Mutagenicity studies conducted with amlodipine maleate revealed no drug-related effects at either the gene or chromosome level.
There was no effect on the fertility of rats treated orally with amlodipine maleate (males for 64 days and females for 14 days prior to mating) at doses of up to 10 mg amlodipine/kg/day (about 10 times the MRHD of 10 mg/day on a mg/m2 basis).
Studies with V alsartan
There was no evidence of carcinogenicity when valsartan was administered in the diet to mice and rats for up to 2 years at concentrations calculated to provide doses of up to 160 and 200 mg/kg/day, respectively. These doses in mice and rats are about 2.4 and 6 times, respectively, the MRHD of 320 mg/day on a mg/m2 basis. (Calculations based on a 60 kg patient.)
Mutagenicity assays did not reveal any valsartan-related effects at either the gene or chromosome level. These assays included bacterial mutagenicity tests with Salmonella and E. coli, a gene mutation test with Chinese hamster V79 cells, a cytogenetic test with Chinese hamster ovary cells, and a rat micronucleus test.
Valsartan had no adverse effects on the reproductive performance of male or female rats at oral doses of up to 200 mg/kg/day. This dose is about 6 times the maximum recommended human dose on a mg/m2 basis.
Studies with A mlodipine
No evidence of teratogenicity or other embryo/fetal toxicity was found when pregnant rats and rabbits were treated orally with amlodipine maleate at doses of up to 10 mg amlodipine/kg/day (respectively, about 10 and 20 times the maximum recommended human dose [MRHD] of 10 mg amlodipine on a mg/m2 basis) during their respective periods of major organogenesis. (Calculations based on a patient weight of 60 kg.) However, litter size was significantly decreased (by about 50%) and the number of intrauterine deaths was significantly increased (about 5-fold) for rats receiving amlodipine maleate at a dose equivalent to 10 mg amlodipine/kg/day for 14 days before mating and throughout mating and gestation. Amlodipine maleate has been shown to prolong both the gestation period and the duration of labor in rats at this dose. There are no adequate and well-controlled studies in pregnant women. Amlodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Studies with V alsartan
No teratogenic effects were observed when valsartan was administered to pregnant mice and rats at oral doses of up to 600 mg/kg/day and to pregnant rabbits at oral doses of up to 10 mg/kg/day. However, significant decreases in fetal weight, pup birth weight, pup survival rate, and slight delays in developmental milestones were observed in studies in which parental rats were treated with valsartan at oral, maternally toxic (reduction in body weight gain and food consumption) doses of 600 mg/kg/day during organogenesis or late gestation and lactation. In rabbits, fetotoxicity (i.e., resorptions, litter loss, abortions, and low body weight) associated with maternal toxicity (mortality) was observed at doses of 5 and 10 mg/kg/day. The no observed adverse effect doses of 600, 200 and 2 mg/kg/day in mice, rats and rabbits, respectively, are about 9, 6 and 0.1 times the MRHD of 320 mg/day on a mg/m2 basis. (Calculations based on a patient weight of 60 kg.)
Studies with A mlodipine B esylate and V alsartan
In the oral embryo-fetal development study in rats using amlodipine besylate plus valsartan at doses equivalent to 5 mg/kg/day amlodipine plus 80 mg/kg/day valsartan, 10 mg/kg/day amlodipine plus 160 mg/kg/day valsartan, and 20 mg/kg/day amlodipine plus 320 mg/kg/day valsartan, treatment-related maternal and fetal effects (developmental delays and alterations noted in the presence of significant maternal toxicity) were noted with the high dose combination. The no-observed-adverse-effect level (NOAEL) for embryo-fetal effects was 10 mg/kg/day amlodipine plus 160 mg/kg/day valsartan. On a systemic exposure [AUC(0-∞)] basis, these doses are, respectively, 4.3 and 2.7 times the systemic exposure [AUC(0-∞)] in humans receiving the MRHD (10/320 mg/60 kg).
Exforge was studied in 2 placebo-controlled and 4 active-controlled trials in hypertensive patients. In a double-blind, placebo controlled study, a total of 1,012 patients with mild-to-moderate hypertension received treatments of three combinations of amlodipine and valsartan (5/80, 5/160, 5/320 mg) or amlodipine alone (5 mg), valsartan alone (80, 160, or 320 mg) or placebo. All doses with the exception of the 5/320 mg dose were initiated at the randomized dose. The high dose was titrated to that dose after a week at a dose of 5/160 mg. At week 8, the combination treatments were statistically significantly superior to their monotherapy components in reduction of diastolic and systolic blood pressures.
| Amlodipine dosage | Valsartan dosage | |||||||
| 0 mg | 80 mg | 160 mg | 320 mg | |||||
| Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | |
| 0 mg | -6.4 | --- | -9.5 | -3.1 | -10.9 | -4.5 | -13.2 | -6.7 |
| 5 mg | -11.1 | -4.7 | -14.2 | -7.8 | -14.0 | -7.6 | -15.7 | -9.3 |
*Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Diastolic Blood Pressure. Mean baseline diastolic BP was 99.3 mmHg.
| Amlodipine dosage | Valsartan dosage | |||||||
| 0 mg | 80 mg | 160 mg | 320 mg | |||||
| Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | |
| 0 mg | -6.2 | --- | -12.9 | -6.8 | -14.3 | -8.2 | -16.3 | -10.1 |
| 5 mg | -14.8 | -8.6 | -20.7 | -14.5 | -19.4 | -13.2 | -22.4 | -16.2 |
*Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Systolic Blood Pressure. Mean baseline systolic BP was 152.8 mmHg.
In a double-blind, placebo controlled study, a total of 1,246 patients with mild to moderate hypertension received treatments of two combinations of amlodipine and valsartan (10/160, 10/320 mg) or amlodipine alone (10 mg), valsartan alone (160 or 320 mg) or placebo. With the exception of the 10/320 mg dose, treatment was initiated at the randomized dose. The high dose was initiated at a dose of 5/160 mg and titrated to the randomized dose after 1 week. At week 8, the combination treatments were statistically significantly superior to their monotherapy components in reduction of diastolic and systolic blood pressures.
| Amlodipine dosage | Valsartan dosage | |||||
| 0 mg | 160 mg | 320 mg | ||||
| Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | |
| 0 mg | -8.2 | --- | -12.8 | - 4.5 | -12.8 | -4.5 |
| 10 mg | -15.0 | -6.7 | - 17.2 | - 9.0 | -18.1 | -9.9 |
*Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Diastolic Blood Pressure. Mean baseline diastolic BP was 99.1 mmHg.
| Amlodipine dosage | Valsartan dosage | |||||
| 0 mg | 160 mg | 320 mg | ||||
| Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | Mean Change* | Placebo-subtracted | |
| 0 mg | -11.0 | --- | -18.1 | -7.0 | -18.5 | -7.5 |
| 10 mg | -22.2 | -11.2 | -26.6 | -15.5 | -26.9 | -15.9 |
*Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Systolic Blood Pressure. Mean baseline systolic BP was 156.7 mmHg.
In a double-blind, active-controlled study, a total of 947 patients with mild to moderate hypertension who were not adequately controlled on valsartan 160 mg received treatments of two combinations of amlodipine and valsartan (10/160, 5/160 mg), or valsartan alone (160 mg). At week 8, the combination treatments were statistically significantly superior to the monotherapy component in reduction of diastolic and systolic blood pressures.
| Treatment Group | Diastolic BP | Systolic BP | ||
| Mean change* | Treatment Difference** | Mean change* | Treatment Difference** | |
| Exforge 10/160 mg |
-11.4 | -4.8 | -13.9 | -5.7 |
| Exforge 5/160 mg |
-9.6 | -3.1 | -12.0 | -3.9 |
| Valsartan 160 mg | -6.6 | --- | -8.2 | --- |
*Mean Change from Baseline at Week 8 in Sitting Diastolic/Systolic Blood Pressure. Mean baseline BP was 149.5/96.5 (systolic/diastolic) mmHg
**Treatment Difference = difference in mean BP reduction between Exforge and the control group (Valsartan 160 mg)
In a double-blind, active-controlled study, a total of 944 patients with mild to moderate hypertension who were not adequately controlled on amlodipine 10 mg received a combination of amlodipine and valsartan (10/160 mg), or amlodipine alone (10 mg). At week 8, the combination treatment was statistically significantly superior to the monotherapy component in reduction of diastolic and systolic blood pressures.
| Treatment Group | Diastolic BP | Systolic BP | ||
| Mean change* | Treatment Difference** | Mean change* | Treatment Difference** | |
| Exforge 10/160 mg |
-11.8 | -1.8 | -12.7 | -1.9 |
| Amlodipine 10 mg | -10.0 | --- | -10.8 | --- |
*Mean Change from Baseline at Week 8 in Sitting Diastolic/Systolic Blood Pressure. Mean baseline BP was 147.0/95.1 (systolic/diastolic) mmHg
**Treatment Difference = difference in mean BP reduction between Exforge and the control group (Amlodipine 10 mg)
Exforge was also evaluated for safety in a 6-week, double-blind, active-controlled trial of 130 hypertensive patients with severe hypertension (mean baseline BP of 171/113 mmHg). Adverse events were similar in patients with severe hypertension and mild/moderate hypertension treated with Exforge.
A wide age range of the adult population, including the elderly was studied (range 19-92 years, mean 54.7 years). Women comprised almost half of the studied population (47.3%). Of the patients in the studied Exforge group, 87.6% were Caucasian. Black and Asian patients each represented approximately 4% of the population in the studied Exforge group.
Two additional double-blind, active-controlled studies were conducted in which Exforge was administered as initial therapy. In one study, a total of 572 Black patients with moderate to severe hypertension were randomized to receive either combination amlodipine/valsartan or amlodipine monotherapy for 12 weeks. The initial dose of amlodipine/valsartan was 5/160 mg for 2 weeks with forced titration to 10/160 mg for 2 weeks, followed by optional titration to 10/320 mg for 4 weeks and optional addition of HCTZ 12.5 mg for 4 weeks. The initial dose of amlodipine was 5 mg for 2 weeks with forced titration to 10 mg for 2 weeks, followed by optional titration to 10 mg for 4 weeks and optional addition of HCTZ 12.5 mg for 4 weeks. At the primary endpoint of 8 weeks, the treatment difference between amlodipine/valsartan and amlodipine was 6.7/2.8 mmHg.
In the other study of similar design, a total of 646 patients with moderate to severe hypertension (MSSBP of ≥ 160 mmHg and <200 mmHg) were randomized to receive either combination amlodipine/valsartan or amlodipine monotherapy for 8 weeks. The initial dose of amlodipine/valsartan was 5/160 mg for 2 weeks with forced titration to 10/160 mg for 2 weeks, followed by the optional addition of HCTZ 12.5 mg for 4 weeks. The initial dose of amlodipine was 5 mg for 2 weeks with forced titration to 10 mg for 2 weeks, followed by the optional addition of HCTZ 12.5 mg for 4 weeks. At the primary endpoint of 4 weeks, the treatment difference between amlodipine/valsartan and amlodipine was 6.6/3.9 mmHg.
There are no trials of the Exforge combination tablet demonstrating reductions in cardiovascular risk in patients with hypertension, but the amlodipine component and several ARBs, which are the same pharmacological class as the valsartan component, have demonstrated such benefits.
Exforge is available as non-scored tablets containing amlodipine besylate equivalent to 5 mg, or 10 mg of amlodipine free-base with valsartan 160 mg or 320 mg, providing for the following available combinations: 5/160 mg, 10/160 mg, 5/320 mg and 10/320 mg.
5/160 mg Tablets - dark yellow, ovaloid shaped, film coated tablet with beveled edge, debossed with “NVR” on one side and “ECE” on the other side.
| Bottles of 30 |
NDC 54868-5997-0 |
| Bottles of 90 |
NDC 54868-5997-1 |
10/160 mg Tablets - light yellow, ovaloid shaped, film coated tablet with beveled edge, debossed with “NVR” on one side and “UIC” on the other side.
| Bottles of 30 |
NDC 54868-5804-0 |
5/320 mg Tablets - very dark yellow, ovaloid shaped, film coated tablet with beveled edge, debossed with “NVR” on one side and “CSF” on the other side.
| Bottles of 30 |
NDC 54868-5996-0 |
| Bottles of 90 |
NDC 54868-5996-1 |
10/320 mg Tablets - dark yellow, ovaloid shaped, film coated tablet with beveled edge, debossed with “NVR” on one side and “LUF” on the other side.
| Bottles of 30 |
NDC 54868-5983-0 |
| Bottles of 90 |
NDC 54868-5983-1 |
Store at 25oC (77oF); excursions permitted to 15-30oC (59-86oF). [See USP Controlled Room Temperature.] Protect from moisture.
Information for Patients
Pregnancy: Female patients of childbearing age should be told that use of drugs like valsartan that act on the renin-angiotensin system can cause serious problems in the fetus and infant including: low blood pressure, poor development of skull bones, kidney failure and death. Discuss other treatment options with female patients planning to become pregnant. Women using Exforge who become pregnant should notify their physicians as soon as possible.
FDA-APPROVED PATIENT LABELING
PATIENT INFORMATION
EXFORGE (X-phorj)
(amlodipine and valsartan)
Tablets
Read the Patient Information that comes with EXFORGE before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or treatment. If you have any questions about EXFORGE, ask your doctor or pharmacist.
|
What is the most important information I should know about EXFORGE?
If you become pregnant, stop taking EXFORGE and call your doctor right away. EXFORGE can harm an unborn baby causing injury and even death. If you plan to become pregnant, talk to your doctor about other treatment options to lower your blood pressure before taking EXFORGE. |
What is EXFORGE?
EXFORGE contains two prescription medicines:
- amlodipine, a calcium channel blocker
- valsartan, an angiotensin receptor blocker (ARB).
EXFORGE may be used to lower high blood pressure (hypertension) in adults
- when one medicine to lower your high blood pressure is not enough
- as the first medicine to lower high blood pressure if your doctor decides you are likely to need more than one medicine.
EXFORGE has not been studied in children under 18 years of age.
What should I tell my doctor before taking EXFORGE?
Tell your doctor about all of your medical conditions, including if you:
-
are pregnant or plan to become pregnant. See “What is the most important information I should know about EXFORGE?”
-
are breast-feeding or plan to breast-feed. EXFORGE may pass into your milk. Do not breast-feed while you are taking EXFORGE.
- have heart problems
- have liver problems
- have kidney problems
- are vomiting or having a lot of diarrhea
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Some of your other medicines and EXFORGE could affect each other, causing serious side effects.
Especially tell your doctor if you take:
- other medicines for high blood pressure or a heart problem
- water pills (diuretics)
- potassium supplements
- a salt substitute
- nonsteroidal anti-inflammatory drugs (like ibuprofen or naproxen)
Know the medicines you take. Keep a list of your medicines and show it to your doctor or pharmacist when you get a new medicine. Talk to your doctor or pharmacist before you start taking any new medicine. Your doctor or pharmacist will know what medicines are safe to take together.
How should I take EXFORGE?
- Take EXFORGE exactly as your doctor tells you.
- Take EXFORGE once each day.
- EXFORGE can be taken with or without food.
- If you miss a dose, take it as soon as you remember. If it is close to your next dose, do not take the missed dose. Just take the next dose at your regular time.
- If you take too much EXFORGE, call your doctor or Poison Control Center, or go to the emergency room.
- Tell all your doctors or dentist you are taking EXFORGE if you:
○ are going to have surgery
○ go for kidney dialysis
What should I avoid while taking Exforge?
You should not take Exforge during pregnancy. See “What is the most important information I should know about Exforge.”
What are the possible side effects of EXFORGE?
EXFORGE may cause serious side effects including:
-
harm to an unborn baby causing injury and even death
. See “What is the most important information I should know about EXFORGE?”
-
low blood pressure (hypotension). Low blood pressure is most likely to happen if you:
- take water pills
- are on a low salt diet
- get dialysis treatments
- have heart problems
- get sick with vomiting or diarrhea
- drink alcohol
Lie down if you feel faint or dizzy. Call your doctor right away.
-
more heart attacks and chest pain (angina) in people that already have severe heart problems. This may happen when you start EXFORGE or when there is an increase in your dose of EXFORGE. Get emergency help if you get worse chest pain or chest pain that does not go away.
-
kidney problems. Kidney problems may become worse in people that already have kidney disease. Some people will have changes in blood tests for kidney function and may need a lower dose of EXFORGE. Call your doctor if you have swelling in your feet, ankles, or hands or unexplained weight gain. If you have heart failure, your doctor should check your kidney function before prescribing EXFORGE.
- laboratory blood test changes in people with congestive heart failure. Some people with congestive heart failure who take valsartan, one of the medicines in EXFORGE, have changes in blood tests including increased potassium and decreased kidney function.
The most common side effects of EXFORGE include:
- swelling (edema) of the hands, ankles, or feet
- nasal congestion, sore throat and discomfort when swallowing
- upper respiratory tract infection (head or chest cold)
- dizziness
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of EXFORGE. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store EXFORGE?
- Store EXFORGE at room temperature between 59°F to 86°F (15°C to 30°C).
- Keep EXFORGE dry (protect it from moisture).
Keep EXFORGE and all medicines out of the reach of children.
General Information about EXFORGE
Medicines are sometimes prescribed for conditions that are not mentioned in the patient information leaflet. Do not use EXFORGE for a condition for which it was not prescribed. Do not give EXFORGE to other people, even if they have the same symptoms that you have. It may harm them.
This patient information leaflet summarizes the most important information about EXFORGE. If you would like more information about EXFORGE, talk with your doctor. You can ask your doctor or pharmacist for information about EXFORGE that is written for health professionals. For more information go to www.EXFORGE.com or call 1-888-839-3674.
What are the ingredients in EXFORGE?
Active ingredients: Amlodipine besylate and valsartan
The inactive ingredients of all strengths of the tablets are colloidal silicon dioxide, crospovidone, magnesium stearate and microcrystalline cellulose. Additionally, the 5/320 mg and 10/320 mg strengths contain iron oxide yellow and sodium starch glycolate. The film coating contains hypromellose, iron oxides, polyethylene glycol, talc and titanium dioxide.
What is high blood pressure (h ypertension)?
Blood pressure is the force of blood in your blood vessels when your heart beats and when your heart rests. You have high blood pressure when the force is too much. EXFORGE can help your blood vessels relax so your blood pressure is lower. Medicines that lower blood pressure lower your chance of having a stroke or heart attack.
High blood pressure makes the heart work harder to pump blood throughout the body and causes damage to blood vessels. If high blood pressure is not treated, it can lead to stroke, heart attack, heart failure, kidney failure and vision problems.
*Norvasc® is a registered trademark of Pfizer, Inc.
**Viagra® is a registered trademark of Pfizer, Inc.
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
©Novartis
T2011-133/T2011-69
October 2011/April 2011
Relabeling and Repackaging by:
Physicians Total Care, Inc.
Tulsa, Oklahoma 74146
PRINCIPAL DISPLAY PANEL
Package Label – 5 mg*/160 mg
Rx Only
EXFORGE® (amlodipine and valsartan) Tablets
*each tablet contains 6.9 mg of amlodipine besylate

PRINCIPAL DISPLAY PANEL
Package Label – 10 mg*/160 mg
Rx Only
EXFORGE® (amlodipine and valsartan) Tablets
*each tablet contains 13.9 mg of amlodipine besylate
PRINCIPAL DISPLAY PANEL
Package Label – 5 mg*/320 mg
Rx Only
EXFORGE® (amlodipine and valsartan) Tablets
*each tablet contains 6.9 mg of amlodipine besylate

PRINCIPAL DISPLAY PANEL
Package Label – 10 mg*/320 mg
Rx Only
EXFORGE® (amlodipine and valsartan) Tablets
*each tablet contains 13.9 mg of amlodipine besylate

Exforgeamlodipine besylate and valsartan TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Exforgeamlodipine besylate and valsartan TABLET, FILM COATED
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Exforgeamlodipine besylate and valsartan TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Exforgeamlodipine besylate and valsartan TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||