Feraheme
HIGHLIGHTS OF PRESCRIBING INFORMATION RECENT MAJOR CHANGES Dosage and Administration (2) 06/2013 INDICATIONS AND USAGEFeraheme is an iron replacement product indicated for the treatment of iron deficiency anemia in adult patients with chronic kidney disease (CKD). (1) DOSAGE AND ADMINISTRATION The recommended dose of Feraheme is an initial 510 mg dose intravenous injection or infusion followed by a second 510 mg dose 3 to 8 days later. Administer Feraheme as an undiluted intravenous injection delivered at a rate of up to 1 mL/sec (30 mg/sec), or as an intravenous infusion in 50-200 mL 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP for at least 15 minutes. The recommended Feraheme dose may be readministered to patients with persistent or recurrent iron deficiency anemia. DOSAGE FORMS AND STRENGTHSInjection: 510 mg iron / 17 mL in single use vials. (3)CONTRAINDICATIONSKnown hypersensitivity to Feraheme or any of its components. (4) WARNINGS AND PRECAUTIONS Hypersensitivity Reactions: Observe for signs and symptoms of hypersensitivity during and after Feraheme administration for at least 30 minutes and until clinically stable following completion of each administration. (5.1) Hypotension: Feraheme may cause hypotension. Monitor for signs and symptoms of hypotension following each administration of Feraheme. (5.2) Iron Overload: Regularly monitor hematologic responses during Feraheme therapy. Do not administer Feraheme to patients with iron overload. (5.3) Magnetic Resonance Imaging: Feraheme can alter magnetic resonance imaging (MRI) studies. (5.4) Side EffectsThe most common adverse reactions (≥ 2%) following the administration of Feraheme are diarrhea, nausea, dizziness, hypotension, constipation, and peripheral edema. (6.1) To report SUSPECTED ADVERSE REACTIONS with Feraheme, contact AMAG Pharmaceuticals, Inc. at 1-877-411-2510, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 FERAHEME INDICATIONS AND USAGE
- 2 FERAHEME DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 FERAHEME CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 FERAHEME ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 FERAHEME DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Feraheme is indicated for the treatment of iron deficiency anemia in adult patients with chronic kidney disease (CKD).
2 DOSAGE AND ADMINISTRATION
The recommended dose of Feraheme is an initial 510 mg dose followed by a second 510 mg dose 3 to 8 days later. Administer Feraheme intravenously, either as an undiluted slow intravenous injection or by infusion.
| Administration | Rate of delivery | Dilution |
| Undiluted intravenous injection |
1 mL/sec (30 mg/sec) At least 17 seconds |
No Dilution |
| Diluted intravenous infusion | At least 15 minutes | Dilute in 50 to 200 mL of 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP. |
Feraheme, when added to intravenous infusion bags containing either Sodium Chloride Injection, USP (normal saline), or 5% Dextrose Injection, USP, at concentrations of 2-8 mg elemental iron per mL, should be used immediately, but may be stored at controlled room temperature (25°C ± 2°C) for up to 4 hours.
The dosage is expressed in terms of mg of elemental iron, with each mL of Feraheme containing 30 mg of elemental iron. Evaluate the hematologic response (hemoglobin, ferritin, iron and transferrin saturation) at least one month following the second Feraheme injection. The recommended Feraheme dose may be readministered to patients with persistent or recurrent iron deficiency anemia.
For patients receiving hemodialysis, administer Feraheme once the blood pressure is stable and the patient has completed at least one hour of hemodialysis. Monitor for signs and symptoms of hypotension following each Feraheme injection.
The recommended Feraheme dose may be readministered to patients with persistent or recurrent iron deficiency anemia.
3 DOSAGE FORMS AND STRENGTHS
Feraheme Injection is available in single use vials. Each vial contains 510 mg of elemental iron in 17 mL.
4 CONTRAINDICATIONS
Feraheme is contraindicated in patients with:
Known hypersensitivity to Feraheme or any of its components
5 WARNINGS AND PRECAUTIONS
5.1 HYPERSENSITIVITY REACTIONS
Serious hypersensitivity reactions, including anaphylactic-type reactions, some of which have been life-threatening and fatal, have been reported in patients receiving Feraheme. Observe patients for signs and symptoms of hypersensitivity during and after Feraheme administration for at least 30 minutes and until clinically stable following completion of each administration. Only administer the drug when personnel and therapies are immediately available for the treatment of anaphylaxis and other hypersensitivity reactions [ see Adverse Reactions (6.1) ]. Anaphylactic type reactions presenting with cardiac/cardiorespiratory arrest, clinically significant hypotension, syncope, and unresponsiveness have been reported in the post-marketing experience [ see Adverse Reactions from Post-marketing Spontaneous Reports (6.2) ]. In clinical studies, serious hypersensitivity reactions were reported in 0.2% (3/1,726) of subjects receiving Feraheme. Other adverse reactions potentially associated with hypersensitivity (e.g., pruritus, rash, urticaria or wheezing) were reported in 3.7% (63/1,726) of these subjects.
5.2 HYPOTENSION
Severe adverse reactions of clinically significant hypotension have been reported. In clinical studies, hypotension was reported in 1.9% (33/1,726) of subjects, including three patients with serious hypotensive reactions. Hypotension has also been reported in the post-marketing experience [ see Adverse Reactions from Post-marketing Spontaneous Reports (6.2) ]. Monitor patients for signs and symptoms of hypotension following each Feraheme administration [ see Dosage and Administration (2) and Warnings and Precautions (5.1) ].
5.3 IRON OVERLOAD
Excessive therapy with parenteral iron can lead to excess storage of iron with the possibility of iatrogenic hemosiderosis. Regularly monitor the hematologic response during parenteral iron therapy [ see Dosage and Administration (2) ]. Do not administer Feraheme to patients with iron overload.
In the 24 hours following administration of Feraheme, laboratory assays may overestimate serum iron and transferrin bound iron by also measuring the iron in the Feraheme complex.
5.4 MAGNETIC RESONANCE (MR) IMAGING
Administration of Feraheme may transiently affect the diagnostic ability of MR imaging. Anticipated MR imaging studies should be conducted prior to the administration of Feraheme. Alteration of MR imaging studies may persist for up to 3 months following the last Feraheme dose. If MR imaging is required within 3 months after Feraheme administration, use T1- or proton density-weighted MR pulse sequences to minimize the Feraheme effects; MR imaging using T2-weighted pulse sequences should not be performed earlier than 4 weeks after the administration of Feraheme. Maximum alteration of vascular MR imaging is anticipated to be evident for 1 – 2 days following Feraheme administration [ see Clinical Pharmacology (12.3) ].
Feraheme will not interfere with X-ray, computed tomography (CT), positron emission tomography (PET), single photon emission computed tomography (SPECT), ultrasound or nuclear medicine imaging.
6 ADVERSE REACTIONS
Feraheme injection may cause serious hypersensitivity reactions and hypotension [ see Warnings and Precautions (5.1) (5.2) ].
In clinical studies, 1,726 subjects were exposed to Feraheme; 1,562 of these had CKD and 164 did not have CKD. Of these subjects 46% were male and the median age was 63 years (range of 18 to 96 years).
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug may not reflect the rates observed in practice.
6.1 ADVERSE REACTIONS IN CLINICAL STUDIES
Across the three randomized clinical trials [Trial 1, 2, and 3, see Clinical Studies (14) ], a total of 605 patients were exposed to two injections of 510 mg of Feraheme and a total of 280 patients were exposed to 200 mg/day of oral iron for 21 days. Most patients received their second Feraheme injection 3 to 8 days after the first injection.
Adverse reactions related to Feraheme and reported by ≥ 1% of Feraheme-treated patients in the randomized clinical trials are listed in Table 1. Diarrhea (4.0%), constipation (2.1%) and hypertension (1.0%) have also been reported in Feraheme-treated patients.
| Table 1: Adverse Reactions to Feraheme Reported in ≥1% of Patients with CKD | ||
| Adverse Reactions | Feraheme 2 x 510 mg (n = 605) |
Oral Iron (n = 280) |
| Nausea | 3.1% | 7.5% |
| Dizziness | 2.6% | 1.8% |
| Hypotension | 2.5% | 0.4% |
| Peripheral Edema | 2.0% | 3.2% |
| Headache | 1.8% | 2.1% |
| Edema | 1.5% | 1.4% |
| Vomiting | 1.5% | 5.0% |
| Abdominal Pain | 1.3% | 1.4% |
| Chest Pain | 1.3% | 0.7% |
| Cough | 1.3% | 1.4% |
| Pruritus | 1.2% | 0.4% |
| Pyrexia | 1.0% | 0.7% |
| Back Pain | 1.0% | 0% |
| Muscle Spasms | 1.0% | 1.4% |
| Dyspnea | 1.0% | 1.1% |
| Rash | 1.0% | 0.4% |
In clinical trials, adverse reactions leading to treatment discontinuation and occurring in ≥ 2 Feraheme-treated patients included hypotension, infusion site swelling, increased serum ferritin level, chest pain, diarrhea, dizziness, ecchymosis, pruritus, chronic renal failure, and urticaria.
Following completion of the controlled phase of the trials, 69 patients received two additional 510 mg intravenous injections of Feraheme (for a total cumulative dose of 2.04 g). Adverse reactions following this repeat Feraheme dosing were similar in character and frequency to those observed following the first two intravenous injections.
In a placebo-controlled, cross-over trial, 713 patients with CKD received a single 510 mg dose of Feraheme. Adverse reactions reported by these patients were similar in character and frequency to those observed in other clinical trials.
6.2 ADVERSE REACTIONS FROM POST-MARKETING SPONTANEOUS REPORTS
The following adverse reactions have been identified during post-approval use of Feraheme. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following serious adverse reactions have been reported from the post-marketing spontaneous reports with Feraheme: life-threatening anaphylactic-type reactions, cardiac/cardiorespiratory arrest, clinically significant hypotension, syncope, unresponsiveness, loss of consciousness, tachycardia/rhythm abnormalities, angioedema, ischemic myocardial events, congestive heart failure, pulse absent, and cyanosis. These adverse reactions have occurred up to 30 minutes after the administration of Feraheme injection. Reactions have occurred following the first dose or subsequent doses of Feraheme.
7 DRUG INTERACTIONS
Drug-drug interaction studies with Feraheme were not conducted. Feraheme may reduce the absorption of concomitantly administered oral iron preparations.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no studies of Feraheme in pregnant women. In animal studies, ferumoxytol caused fetal malformations and decreased fetal weights at maternally toxic doses of 6 times the estimated human daily dose. Use Feraheme during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Administration of ferumoxytol during organogenesis, at doses of 31.6 mg Fe/kg/day in rats and 16.5 mg Fe/kg/day in rabbits, did not result in maternal or fetal effects. These doses are approximately 2 times the estimated human daily dose based on body surface area. In rats, administration of ferumoxytol during organogenesis at a maternally toxic dose of 100 mg Fe/kg/day, approximately 6 times the estimated human daily dose based on body surface area, caused a decrease in fetal weights. In rabbits, administration of ferumoxytol during organogenesis at a maternally toxic dose of 45 mg Fe/kg/day, approximately 6 times the estimated human daily dose based on body surface area, was associated with external and/or soft tissue fetal malformations and decreased fetal weights.
8.3 Nursing Mothers
It is not known whether Feraheme is present in human milk. Because many drugs are excreted in human milk and because of the potential for adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to avoid Feraheme, taking into account the importance of Feraheme to the mother and the known benefits of nursing.
8.4 Pediatric Use
The safety and effectiveness of Feraheme in pediatric patients have not been established.
8.5 Geriatric Use
In controlled clinical trials, 330 patients ≥ 65 years of age were treated with Feraheme. No overall differences in safety and efficacy were observed between older and younger patients in these trials, but greater sensitivity of older individuals cannot be ruled out. In general, dose administration to an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy [ see Dosage and Administration (2) and Clinical Studies (14) ].
10 OVERDOSAGE
No data are available regarding overdosage of Feraheme in humans. Excessive dosages of Feraheme may lead to accumulation of iron in storage sites potentially leading to hemosiderosis. Do not administer Feraheme to patients with iron overload [ Warnings and Precautions (5.3) ].
11 DESCRIPTION
Feraheme, an iron replacement product, is a non-stoichiometric magnetite (superparamagnetic iron oxide) coated with polyglucose sorbitol carboxymethylether. The overall colloidal particle size is 17-31 nm in diameter. The chemical formula of Feraheme is Fe5874O8752-C11719H18682O9933Na414 with an apparent molecular weight of 750 kDa.
Feraheme injection is an aqueous colloidal product that is formulated with mannitol. It is a black to reddish brown liquid, and is provided in single use vials containing 510 mg of elemental iron. Each mL of the sterile colloidal solution of Feraheme injection contains 30 mg of elemental iron and 44 mg of mannitol, and has low bleomycin-detectable iron. The formulation is isotonic with an osmolality of 270-330 mOsm/kg. The product contains no preservatives, and has a pH of 6 to 8.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Feraheme consists of a superparamagnetic iron oxide that is coated with a carbohydrate shell, which helps to isolate the bioactive iron from plasma components until the iron-carbohydrate complex enters the reticuloendothelial system macrophages of the liver, spleen and bone marrow. The iron is released from the iron-carbohydrate complex within vesicles in the macrophages. Iron then either enters the intracellular storage iron pool (e.g., ferritin) or is transferred to plasma transferrin for transport to erythroid precursor cells for incorporation into hemoglobin.
12.2 Pharmacodynamics
Cardiac Electrophysiology
In a randomized, positive- and placebo-controlled, parallel-group study, healthy subjects received a supratherapeutic regimen of Feraheme (1.02 g given as two 510 mg doses within 24 hours), placebo or a single dose of 400 mg moxifloxacin (positive control). Results demonstrated no effect of Feraheme on QT interval durations. No clinically meaningful effect of Feraheme on heart rate was observed.
12.3 Pharmacokinetics
The pharmacokinetic (PK) behavior of Feraheme has been examined in healthy subjects and in patients with CKD stage 5D on hemodialysis. Feraheme exhibited dose-dependent, capacity-limited elimination from plasma with a half life of approximately 15 hours in humans. The clearance (CL) was decreased by increasing the dose of Feraheme. Volume of distribution (Vd) was consistent with plasma volume, and the mean maximum observed plasma concentration (Cmax) and terminal half-life (t1/2) values increased with dose. The estimated values of CL and Vd following two 510 mg doses of Feraheme administered intravenously within 24 hours were 69.1 mL/hr and 3.16 L, respectively. The Cmax and time of maximum concentration (tmax) were 206 mcg/mL and 0.32 hr, respectively. Rate of infusion had no influence on Feraheme PK parameters. No gender differences in Feraheme PK parameters were observed. Feraheme is not removed by hemodialysis.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Ferumoxytol was not tested for carcinogenic effects. In standard genotoxicity tests, ferumoxytol showed no evidence of mutagenic activity in an in vitro Ames test or clastogenic activity in either an in vitro chromosomal aberration assay or an in vivo micronucleus assay.
No adverse effects on fertility or general reproductive performance were noted in animal studies. Ferumoxytol had no effect on male or female fertility or general reproductive function in rats.
14 CLINICAL STUDIES
The safety and efficacy of Feraheme for the episodic treatment of iron deficiency anemia in patients with CKD were assessed in three randomized, open-label, controlled clinical trials (Trial 1, 2 and 3). These trials also included an uncontrolled, follow-up phase in which patients with persistent iron deficiency anemia could receive two additional 510 mg intravenous injections of Feraheme. The major efficacy results from the controlled phase of each study are shown in Table 2.
In all three trials, patients with CKD and iron deficiency anemia were randomized to treatment with Feraheme or oral iron. Feraheme was administered as two 510 mg intravenous single doses and oral iron (ferrous fumarate) was administered as a total daily dose of 200 mg elemental iron daily for 21 days. The major trial outcomes assessed the change in hemoglobin from baseline to Day 35. Trial 1 and 2 enrolled patients with non-dialysis dependent CKD and Trial 3 enrolled patients who were undergoing hemodialysis.
In Trial 1, the mean age of patients was 66 years (range, 23 to 95); 60% were female; 65% were Caucasian, 32% were Black, and 2% were other races. In the Feraheme and oral iron groups, 42% and 44% of patients, respectively, were receiving erythropoiesis stimulating agents (ESAs) at baseline.
In Trial 2, the mean age of patients was 65 years (range, 31 to 96); 61% were female; 58% were Caucasian, 35% were Black, and 7% were other races. In the Feraheme and oral iron groups, 36% and 43% of patients, respectively, were receiving ESAs at baseline.
In Trial 3, the mean age of patients was 60 years (range, 24 to 87); 43% were female; 34% were Caucasian, 59% were Black, and 7% were other races. All patients were receiving ESAs.
Table 2 shows the Baseline and mean change to Day 35 in hemoglobin (Hgb, g/dL), transferrin saturation (TSAT, %) and ferritin (ng/mL) in each treatment group for Trial 1, 2, and 3.
| * p≤0.001 for main efficacy endpoint | ||||||
| Table 2: Changes from Baseline to Day 35 in Hemoglobin, Transferrin Saturation and Ferritin (Intent to Treat Population) | ||||||
| ENDPOINT | Trial 1 Non-Dialysis CKD |
Trial 2 Non-Dialysis CKD |
Trial 3 CKD on Dialysis |
|||
| Feraheme n = 226 |
Oral Iron n = 77 |
Feraheme n = 228 |
Oral Iron n = 76 |
Feraheme n = 114 |
Oral Iron n = 116 |
|
| Baseline Hgb (mean ± SD, g/dL) |
9.9
± 0.8 |
9.9
± 0.7 |
10.0
± 0.7 |
10.0
± 0.8 |
10.6
± 0.7 |
10.7
± 0.6 |
| Hgb change from Baseline at Day 35 (mean ± SD, g/dL) |
1.2*
± 1.3 |
0.5
± 1.0 |
0.8*
± 1.2 |
0.2
± 1.0 |
1.0*
± 1.1 |
0.5
± 1.1 |
| Baseline TSAT (mean ± SD, %) |
9.8
± 5.4 |
10.4
± 5.2 |
11.3
± 6.1 |
10.1
± 5.5 |
15.7
± 7.2 |
15.9
± 6.3 |
| TSAT change from Baseline at Day 35 (mean ± SD, %) |
9.2
± 9.4 |
0.3
± 4.7 |
9.8
± 9.2 |
1.3
± 6.4 |
6.4
± 12.6 |
0.6
± 8.3 |
| Baseline ferritin (mean ± SD, ng/mL) |
123.7
± 125.4 |
146.2
± 136.3 |
146.1
± 173.6 |
143.5
± 144.9 |
340.5
± 159.1 |
357.6
± 171.7 |
| Ferritin change from Baseline at Day 35 (mean ± SD, ng/mL) |
300.7
± 214.9 |
0.3
± 82.0 |
381.7
± 278.6 |
6.9
± 60.1 |
233.9
± 207.0 |
-59.2
± 106.2 |
Following completion of the controlled phase of each of the Phase 3 trials, patients who were iron deficient and anemic could receive two additional 510 mg intravenous injections of Feraheme for a total cumulative dose of 2.04 g. Overall, 69 patients received two additional 510 mg intravenous injections of Feraheme, and on Day 35 following these additional injections, the majority of these patients (70%) experienced an increase in hemoglobin and iron parameters (TSAT and ferritin). The mean change (±SD) in hemoglobin level from the retreatment baseline for patients with an increase in hemoglobin was 0.86 (± 0.68) g/dL and was 0.5 (± 0.8) g/dL for all patients.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Feraheme is available in single use vials in the following package sizes (Table 3).
| Table 3: Feraheme Packaging Description | ||
| NDC Code | Dose / Total volume per vial | Vials / Carton |
| NDC 59338-775-01 | 510 mg/ 17 mL | 1 |
| NDC 59338-775-10 | 510 mg/ 17 mL | 10 |
16.2 Stability and Storage
Store at 20° to 25°C (68° to 77°F). Excursions permitted to 15° – 30°C (59° – 86°F) [see USP controlled room temperature].
17 PATIENT COUNSELING INFORMATION
Prior to Feraheme administration:
- Question patients regarding any prior history of reactions to parenteral iron products.
- Advise patients of the risks associated with Feraheme.
- Advise patient to report any signs and symptoms of hypersensitivity that may develop during and following Feraheme administration, such as rash, itching, dizziness, lightheadedness, swelling and breathing problems [ see Warnings and Precautions (5) ].
U.S Patents: 6,599,498 B1; 7,553,479 B2; 7,871,597 B2; 8,501,158 B2
Distributed by: AMAG Pharmaceuticals, Inc. Waltham, MA 02451
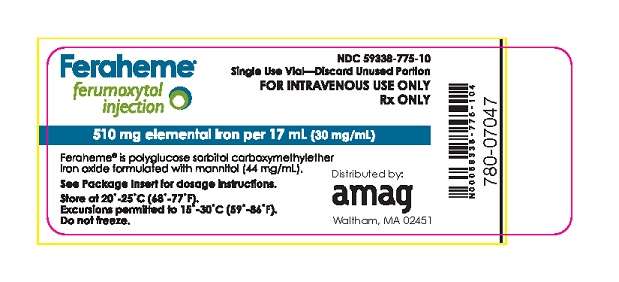
Package Label - Principal Display Panel – 17 mL Vial, Feraheme Injection
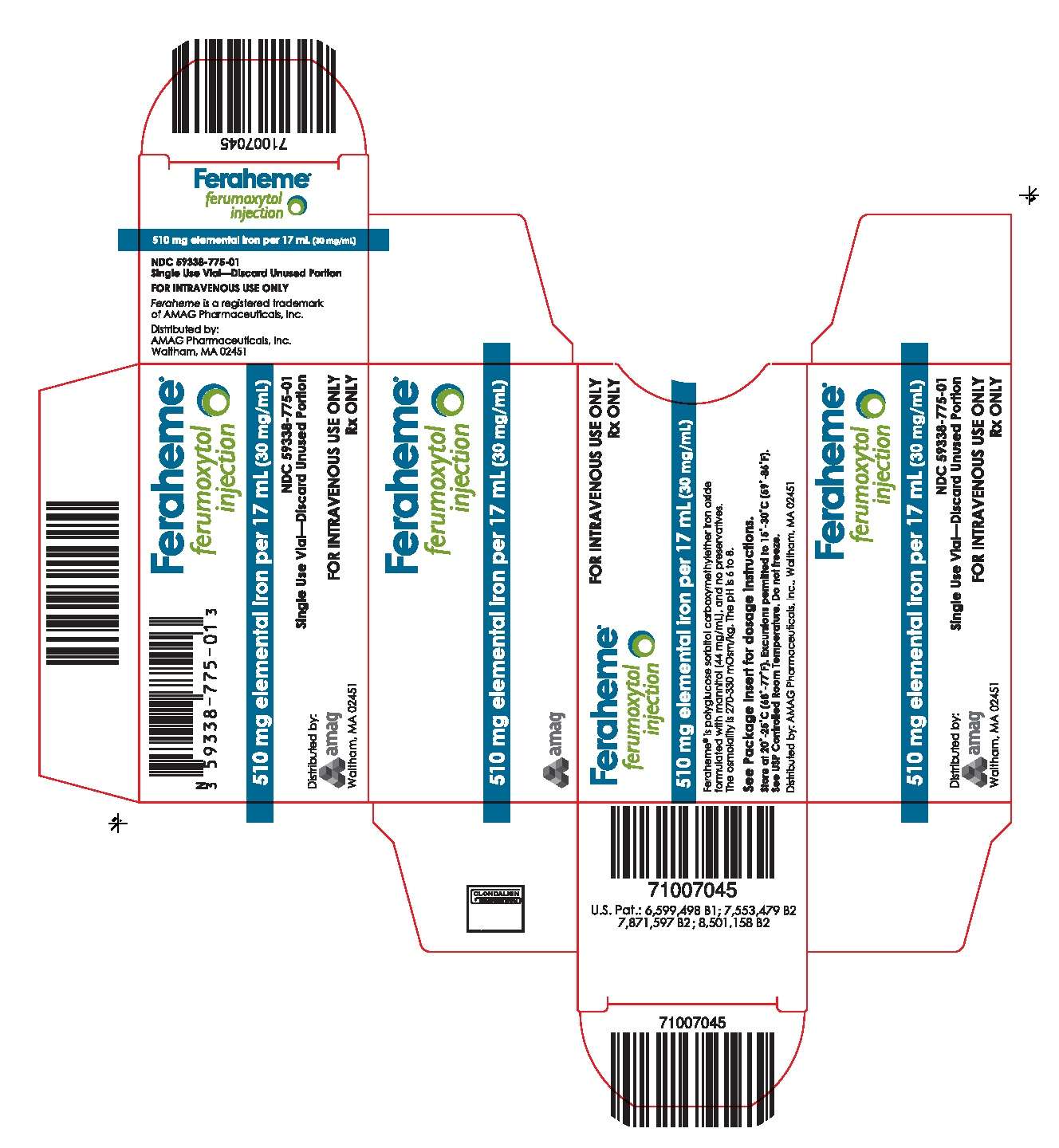
Package Label - Principal Display Panel – Carton for Single Use Vial, Feraheme Injection
Ferahemeferumoxytol INJECTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||