FLUTICASONE PROPIONATE
FLUTICASONE PROPIONATE
FULL PRESCRIBING INFORMATION: CONTENTS*
- FLUTICASONE PROPIONATE DESCRIPTION SECTION
- CLINICAL PHARMACOLOGY SECTION
- INDICATIONS & USAGE SECTION
- FLUTICASONE PROPIONATE CONTRAINDICATIONS SECTION
- PRECAUTIONS SECTION
- FLUTICASONE PROPIONATE ADVERSE REACTIONS SECTION
- OVERDOSAGE SECTION
- DOSAGE & ADMINISTRATION SECTION
- CLINICAL STUDIES SECTION
- HOW SUPPLIED SECTION
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
DESCRIPTION SECTION
Fluticasone Propionate Cream 0.05% contains fluticasone propionate [(6α,11β,16α,17α)-6,9,-difluoro-11-hydroxy-16-methyl-3-oxo-17-(1-oxopropoxy)androsta-1,4-diene-17-carbothioic acid, S-fluoromethyl ester], a synthetic fluorinated cortico-steroid, for topical dermatologic use. The topical cortico-steroids constitute a class of primarily synthetic steroids used as anti-inflammatory and antipruritic agents.
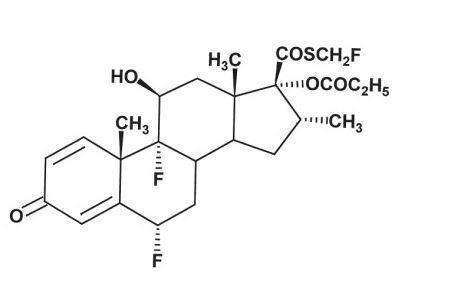
Chemically, fluticasone propionate is C25H3F3O5S. It has the following structural formula:
Fluticasone propionate has a molecular weight of 500.6. It is a white to off-white powder and is insoluble in water.
Each gram of Fluticasone Propionate Cream contains fluticasone propionate 0.5 mg in a base of propylene glycol, mineral oil, cetostearyl alcohol, Ceteth-20, isopropyl myristate, dibasic sodium phosphate, citric acid, purified water, and methylparaben as preservative.
CLINICAL PHARMACOLOGY SECTION
Like other topical corticosteroids, fluticasone propionate has anti-inflammatory, antipruritic, and vasoconstrictive properties. The mechanism of the anti-inflammatory activity of the topical steroids, in general, is unclear. However, corticosteroids are thought to act by the induction of phospholipase A2 inhibitory proteins, collectively called lipocortins. It is postulated that these proteins control the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes by inhibiting the release of their common precursor, arachidonic acid. Arachidonic acid is released from membrane phospholipids by phospholipase A2.
Fluticasone propionate is lipophilic and has a strong affinity for the glucocorticoid receptor. It has weak affinity for the progesterone receptor, and virtually no affinity for the mineralocorticoid, estrogen, or androgen receptors. The therapeutic potency of glucocorticoids is related to the half-life of the glucocorticoid-receptor complex. The half-life of the fluticasone propionate-glucocorticoid receptor complex is approximately 10 hours.
Studies performed with Fluticasone Propionate Cream indicate that it is in the medium range of potency as compared with other topical corticosteroids.
Pharmacokinetics: Absorption: The activity of Fluticasone Propionate Cream is due to the parent drug, fluticasone propionate. The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle and the integrity of the epidermal barrier. Occlusive dressing enhances penetration. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin increase percutaneous absorption.In a human study of 12 healthy males receiving 12.5 g of 0.05% fluticasone propionate cream twice daily for 3 weeks, plasma levels were generally below the level of quantification (0.05 ng/mL). In another study of 6 healthy males administered 25 g of 0.05% fluticasone propionate cream under occlusion for 5 days, plasma levels of fluticasone ranged from 0.07 to 0.39 ng/mL.
In an animal study using radiolabeled 0.05% fluticasone propionate cream and ointment preparations, rats received a topical dose of 1 g/kg for a 24-hour period. Total recovery of radioactivity was approximately 80% at the end of 7 days. The majority of the dose (73%) was recovered from the surface of the application site. Less than 1% of the dose was recovered in the skin at the application site. Approximately 5% of the dose was absorbed systemically through the skin. Absorption from the skin continued for the duration of the study (7 days), indicating a long retention time at the application site.
Distribution: Following intravenous administration of 1 mg fluticasone propionate in healthy volunteers, the initial disposition phase for fluticasone propionate was rapid and consistent with its high lipid solubility and tissue binding. The apparent volume of distribution averaged 4.2 L/kg (range, 2.3 to 16.7 L/kg). The percentage of fluticasone propionate bound to human plasma proteins averaged 91%. Fluticasone propionate is weakly and reversibly bound to erythrocytes. Fluticasone propionate is not significantly bound to human transcortin.
Metabolism: No metabolites of fluticasone propionate were detected in an in vitro study of radiolabeled fluticasone propionate incubated in a human skin homogenate. The total blood clearance of systemically absorbed fluticasone propionate averages 1,093 mL/min (range, 618 to 1,702 mL/min) after a 1-mg intravenous dose, with renal clearance accounting for less than 0.02% of the total. Fluticasone propionate is metabolized in the liver by cytochrome P450 3A4-mediated hydrolysis of the 5-fluoromethyl carbothioate grouping. This transformation occurs in 1 metabolic step to produce the inactive 17-b-carboxylic acid metabolite, the only known metabolite detected in man. This metabolite has approximately 2,000 times less affinity than the parent drug for the glucocorticoid receptor of human lung cytosol in vitro and negligible pharmacological activity in animal studies. Other metabolites detected in vitro using cultured human hepatoma cells have not been detected in man.
Excretion: Following intravenous dose of 1 mg in healthy volunteers, fluticasone propionate showed polyexponential kinetics and had an average terminal half-life of 7.2 hours (range, 3.2 to 11.2 hours).
INDICATIONS & USAGE SECTION
Fluticasone Propionate Cream is a medium potency corticosteroid indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses. Fluticasone Propionate Cream may be used with caution in pediatric patients 3 months of age or older. The safety and efficacy of drug use for longer than 4 weeks in this population have not been established. The safety and efficacy of Fluticasone Propionate Cream in pediatric patients below 3 months of age have not been established.
CONTRAINDICATIONS SECTION
Fluticasone Propionate Cream is contraindicated in those patients with a history of hypersensitivity to any of the components in the preparation.
PRECAUTIONS SECTION
General: Systemic absorption of topical corticosteroids can produce reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal from treatment. Manifestations of Cushing's syndrome, hyperglycemia, and glucosuria can also be produced in some patients by systemic absorption of topical corticosteroids while on treatment.
Patients applying a potent topical steroid to a large surface area or to areas under occlusion should be evaluated periodically for evidence of HPA axis suppression. This may be done by using the ACTH stimulation, A.M. plasma cortisol, and urinary free cortisol tests.
If HPA axis suppression is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent steroid. Recovery of HPA axis function is generally prompt upon discontinuation of topical corticosteroids. Infrequently, signs and symptoms of glucocorticosteroid insufficiency may occur requiring supplemental systemic corticosteroids. For information on systemic supplementation, see prescribing information for those products.
Fluticasone Propionate Cream, 0.05% caused depression of A.M. plasma cortisol levels in 1 of 6 adult patients when used daily for 7 days in patients with psoriasis or eczema involving at least 30% of the body surface. After 2 days of treatment, this patient developed a 60% decrease from pretreatment values in the A.M. plasma cortisol level.
There was some evidence of corresponding decrease in the 24-hour urinary free cortisol levels. The A.M. plasma cortisol level remained slightly depressed for 48 hours but recovered by day 6 of treatment.
Fluticasone Propionate Cream, 0.05%, caused HPA axis suppression in 2 of 43 pediatric patients, ages 2 and 5 years old, who were treated for 4 weeks covering at least 35% of the body surface area. Follow-up testing 12 days after treatment discontinuation, available for 1 of the 2 subjects, demonstrated a normally responsive HPA axis (see PRECAUTIONS: Pediatric Use).
Pediatric patients may be more susceptible to systemic toxicity from equivalent doses due to their larger skin surface to body mass ratios (see PRECAUTIONS: Pediatric Use).
Fluticasone Propionate Cream, 0.05% may cause local cutaneous adverse reactions (see ADVERSE REACTIONS).
If irritation develops, Fluticasone Propionate Cream should be discontinued and appropriate therapy instituted. Allergic contact dermatitis with corticosteroids is usually diagnosed by observing failure to healrather than noting a clinical exacerbation as with most topical products not containing corticosteroids. Such an observation should be corroborated with appropriate diagnostic patch testing.
If concomitant skin infections are present or develop, an appropriate antifungal or antibacterial agent should be used. If a favorable response does not occur promptly, use of Fluticasone Propionate Cream should be discontinued until the infection has been adequately controlled.
Fluticasone Propionate Cream should not be used in the presence of preexisting skin atrophy and should not be used where infection is present at the treatment site. Fluticasone Propionate Cream should not be used in the treatment of rosacea and perioral dermatitis.
Information for Patients: Patients using topical corticosteroids should receive the following information and instructions:
- This medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes.
- This medication should not be used for any disorder other than that for which it was prescribed.
- The treated skin area should not be bandaged or otherwise covered or wrapped so as to be occlusive unless directed by the physician.
- Patients should report to their physician any signs of local adverse reactions.
- Parents of pediatric patients should be advised not to use this medication in the treatment of diaper dermatitis. Fluticasone Propionate Cream should not be applied in the diaper areas as diapers or plastic pants may constitute occlusive dressing (see DOSAGE AND ADMINISTRATION).
- This medication should not be used on the face, underarms, or groin areas unless directed by a physician.
- As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, contact the physician.
Laboratory Tests: The following tests may be helpful in evaluating patients for HPA axis suppression:
ACTH stimulation test
A.M. plasma cortisol test
Urinary free cortisol test
Carcinogenesis, Mutagenesis, and Impairment of Fertility: Two 18-month studies were performed in mice to evaluate the carcinogenic potential of fluticasone propionate when given topically (as an 0.05% ointment) and orally. No evidence of carcinogenicity was found in either study.
Fluticasone propionate was not mutagenic in the standard Ames test, E. coli fluctuation test, S. cerevisiae gene conversion test, or Chinese Hamster ovarian cell assay. It was not clastogenic in mouse micronucleus or cultured human lymphocyte tests.
In a fertility and general reproductive performance study in rats, fluticasone propionate administered subcutaneously to females at up to 50 mcg/kg per day and to males at up to 100 mcg/kg per day (later reduced to 50 mcg/kg per day) had no effect upon mating performance or fertility. These doses are approximately 15 and 30 times, respectively, the human systemic exposure following use of the recommended human topical dose of fluticasone propionate cream, 0.05%, assuming human percutaneous absorption of approximately 3% and the use in a 70-kg person of 15 g/day.
Pregnancy: Teratogenic Effects: Pregnancy Category C.Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals. Teratology studies in the mouse demonstrated fluticasone propionate to be teratogenic (cleft palate) when administered subcutaneously in doses of 45 mcg/kg per day and 150 mcg/kg per day. This dose is approximately 14 and 45 times, respectively, the human topical dose of fluticasone propionate cream, 0.05%. There are no adequate and well-controlled studies in pregnant women. Fluticasone Propionate Cream should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers: Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when Fluticasone Propionate Cream is administered to a nursing woman.
Pediatric Use: Fluticasone Propionate Cream may be used with caution in pediatric patients as young as 3 months of age. The safety and efficacy of drug use for longer than 4 weeks in this population have not been established. The safety and efficacy of Fluticasone Propionate Cream in pediatric patients below 3 months of age have not been established.
Fluticasone Propionate Cream, 0.05%, caused HPA axis suppression in 2 of 43 pediatric patients, ages 2 and 5 years old, who were treated for 4 weeks covering at least 35% of the body surface area. Follow-up testing 12 days after treatment discontinuation, available for 1 of the 2 subjects, demonstrated a normally responsive HPA axis (see ADVERSE REACTIONS). Adverse effects including striae have been reported with use of topical corticosteroids in pediatric patients.
HPA axis suppression, Cushing's syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in pediatric patients receiving topical corticosteroids. Manifestations of adrenal suppression in pediatric patients include low plasma cortisol levels to an absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
Geriatric Use: A limited number of patients above 65 years of age (n = 126) have been treated with Fluticasone Propionate Cream in US and non-US clinical trials. While the number of patients is too small to permit separate analysis of efficacy and safety, the adverse reactions reported in this population were similar to those reported by younger patients. Based on available data, no adjustment of dosage of Fluticasone Propionate in geriatric patients is warranted.
ADVERSE REACTIONS SECTION
In controlled clinical trials of twice-daily administration, the total incidence of adverse reactions associated with the use of Fluticasone Propionate Cream was approximately 4%. These adverse reactions were usually mild; self-limiting; and consisted primarily of pruritus, dryness, numbness of fingers, and burning. These events occurred in 2.9%, 1.2%, 1.0%, and 0.6% of patients, respectively.
Two clinical studies compared once- to twice-daily administration of Fluticasone Propionate Cream for the treatment of moderate to severe eczema. The local drug-related adverse events for the 491 patients enrolled in both studies are shown in Table 1. In the study enrolling both adult and pediatric patients, the incidence of local adverse events in the 119 pediatric patients ages 1 to 12 years was comparable to the 140 patients ages 13 to 62 years.
Fifty-one pediatric patients ages 3 months to 5 years, with moderate to severe eczema, were enrolled in an open-label HPA axis safety study. Fluticasone Propionate Cream was applied twice daily for 3 to 4 weeks over an arithmetic mean body surface area of 64% (range, 35% to 95%). The mean morning cortisol levels with standard deviations before treatment (prestimulation mean value = 13.76 ± 6.94 mcg/dL, poststimulation mean value = 30.53 ± 7.23 mcg/dL) and at end treatment (prestimulation mean value = 12.32 ± 6.92 mcg/dL, poststimulation mean value = 28.84 ± 7.16 mcg/dL) showed little change. In 2 of 43 (4.7%) patients with end-treatment results, peak cortisol levels following cosyntropin stimulation testing were <18 µg/dL, indicating adrenal suppression. Follow-up testing after treatment discontinuation, available for 1 of the 2 subjects, demonstrated a normally responsive HPA axis. Local drug-related adverse events were transient burning, resolving the same day it was reported; transient urticaria, resolving the same day it was reported; erythematous rash; dusky erythema, resolving within 1 month after cessation of Fluticasone Propionate Cream; and telangiectasia, resolving within 3 months after stopping Fluticasone Propionate Cream.
| Adverse Event | Fluticasone Once Daily (n = 210) |
Fluticasone Twice Daily (n = 203) |
Vehicle Twice Daily (n = 78) |
|---|---|---|---|
| Skin Infection | 1 (0.5%) | 0 | 0 |
| Infected eczema | 1 (0.5%) | 2 (1.0%) | 0 |
| Viral warts | 0 | 1 (0.5%) | 0 |
| Herpes simplex | 0 | 1 (0.5%) | 0 |
| Impetigo | 1 (0.5%) | 0 | 0 |
| Atopic dermatitis | 1 (0.5%) | 0 | 0 |
| Eczema | 1 (0.5%) | 0 | 0 |
| Exacerbation of eczema | 4 (1.9%) | 1 (0.5%) | 1 (1.3%) |
| Erythema | 0 | 2 (1.0%) | 0 |
| Burning | 2 (1.0%) | 2 (1.0%) | 2 (2.6%) |
| Stinging | 0 | 2 (1.0%) | 1 (1.3%) |
| Skin irritation | 6 (2.9%) | 2 (1.0%) | 0 |
| Pruritis | 2 (1.0%) | 4 (1.9%) | 4 (5.1%) |
| Exacerbation of pruritis | 4 (1.9%) | 1 (0.5%) | 1 (1.3%) |
| Folliculitis | 1 (0.5%) | 1 (0.5%) | 0 |
| Blisters | 0 | 1 (0.5%) | 0 |
| Dryness of skin | 3 (1.4%) | 1 (0.5%) | 0 |
| Adverse Events | Fluticasone Twice Daily |
|---|---|
|
* See text for additional detail. † n = 41 |
|
| Burning | 1 (2.0%) |
| Dusky erythema | 1 (2.0%) |
| Erythematous rash | 1 (2.0%) |
| Facial teleangiectasia† | 2 (4.9%) |
| Non-facial teleangiectasia | 1 (2.0%) |
| Urticaria | 1 (2.0%) |
The following local adverse reactions have been reported infrequently with topical corticosteroids, and they may occur more frequently with the use of occlusive dressings and higher potency corticosteroids. These reactions are listed in an approximately decreasing order of occurrence: irritation, folliculitis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, skin atrophy, striae, and miliaria. Also, there are reports of the development of pustular psoriasis from chronic plaque psoriasis following reduction or discontinuation of potent topical corticosteroid products.
OVERDOSAGE SECTION
Topically applied Fluticasone Propionate Cream can be absorbed in sufficient amounts to produce systemic effects (see PRECAUTIONS).
DOSAGE & ADMINISTRATION SECTION
Fluticasone Propionate Cream may be used in adult and pediatric patients 3 months of age or older. Safety and efficacy of Fluticasone Propionate Cream in pediatric patients for more than 4 weeks of use have not been established (see PRECAUTIONS: Pediatric Use). The safety and efficacy of Fluticasone Propionate Cream in pediatric patients below 3 months of age have not been established.
Atopic Dermatitis: Apply a thin film of Fluticasone Propionate Cream to the affected skin areas once or twice daily. Rub in gently.
Other Corticosteroid-Responsive Dermatoses: Apply a thin film of Fluticasone Propionate Cream to the affected skin areas twice daily. Rub in gently.
As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, reassessment of diagnosis may be necessary.
Fluticasone Propionate Cream should not be used with occlusive dressings. Fluticasone Propionate Cream should not be applied in the diaper area, as diapers or plastic pants may constitute occlusive dressings.
Geriatric Use: In studies where geriatric patients (65 years of age or older, see PRECAUTIONS) have been treated with Fluticasone Propionate Cream, safety did not differ from that in younger patients; therefore, no dosage adjustment is recommended.
CLINICAL STUDIES SECTION
Psoriasis Studies: In 2 vehicle-controlled studies, Fluticasone Propionate Cream applied twice daily was significantly more effective than the vehicle in the treatment of moderate to severe psoriasis. The investigator’s global evaluation after 28 days of treatment is shown in Table 3
| Fluticasone Propionate Cream |
Vehicle | |||
|
Study 1 (n = 59) |
Study 2 (n = 74) |
Study 1 (n = 66) |
Study 2 (n = 75) |
|
| Cleared | 8% | 1% | 3% | 1% |
| Excellent | 29% | 28% | 11% | 17% |
| Good | 27% | 34% | 20% | 28% |
| Fair | 27% | 15% | 33% | 25% |
| Poor | 7% | 22% | 24% | 27% |
| Worse | 2% | 0 | 9% | 1% |
The clinical signs of psoriasis were scored on a scale of 0 = absent, 1 = mild, 2 = moderate, and 3 = severe. The mean improvements over baseline in the clinical signs at the end of treatment are shown in Table 4.
| Fluticasone Propionate Cream |
Vehicle | |||
| Study 1 | Study 2 | Study 1 | Study 2 | |
| Erythema | 1.19 | 1.07 | 0.55 | 0.84 |
| Thickening | 1.22 | 1.17 | 0.81 | 0.97 |
| Scaling | 1.53 | 1.39 | 0.95 | 1.21 |
Atopic Dermatitis Studies: In 2 controlled 28-day studies, Fluticasone Propionate Cream once daily was equivalent to Fluticasone Propionate Cream twice daily in the treatment of moderate to severe eczema. The investigator’s global evaluation after 28 days of treatment is shown in Table 5.
|
Fluticasone |
Fluticasone Propionate Cream Twice Daily |
|||
|
Study 1 (n = 64) |
Study 2 (n = 106) |
Study 1 (n = 65) |
Study 2 (n = 100) |
|
| Cleared | 30% | 20% | 48% | 21% |
| Excellent | 42% | 32% | 32% | 50% |
| Good | 17% | 26% | 5% | 12% |
| Fair | 3% | 14% | 6% | 10% |
| Poor | 5% | 3% | 8% | 4% |
| Worse | 3% | 6% | 2% | 3% |
The clinical signs and symptoms of atopic dermatitis were scored on a scale of 0 = absent, 1 = mild, 2 = moderate, and 3 = severe. The mean improvements over baseline at the end of treatment are shown in Table 6.
| Fluticasone Propionate Cream Once Daily |
Fluticasone Propionate Cream Twice Daily |
|||
| Study 1 | Study 2 | Study 1 | Study 2 | |
| Erythema | 1.7 | 1.5 | 1.8 | 1.7 |
| Pruritis | 2.1 | 1.6 | 2.1 | 1.7 |
| Thickening | 1.6 | 1.3 | 1.6 | 1.5 |
| Lichenification | 1.2 | 1.2 | 1.2 | 1.3 |
| Vesiculation | 0.5 | 0.4 | 0.5 | 0.5 |
| Crusting | 0.6 | 0.7 | 0.8 | 0.8 |
HOW SUPPLIED SECTION
Fluticasone Propionate Cream, 0.05% is supplied in:
15-g tubes (NDC 0713-0631-15)
30-g tubes (NDC 0713-0631-31), and
60-g tubes (NDC 0713-0631-60)
STORAGE
Store between 2° and 30°C (36° and 86°F).
G&W Laboratories, Inc.
South Plainfield, NJ 07080
8-0631GW1
Issued 9/04
PACKAGE LABEL
G&W®
NDC 0713-0631-15
Fluticasone Propionate Cream, 0.05%
For dermatologic use only - Not for ophthalmic use.
Rx only
15g
Contains: Fluticasone propionate 0.05% in a cream base of propylene glycol, mineral oil, cetostearyl alcohol, Ceteth-20, isopropyl myristate, dibasic sodium phosphate, citric acid, purified water, and methylparaben as a preservative.
Usual Dosage: Apply a thin film of cream to the affected skin areas twice daily.
See package insert for full prescribing information.
Store between 2˚ and 30˚C (36˚ and 86˚F).
Manufactured by:
G&W Laboratories, Inc.
South Plainfield, NJ 07080
Visit our website @ www.gwlabs.com
Important: The opening of this product is covered by a metal tamper-resistant seal. If this seal has been punctured or is not visible, do not use and return product to place of purchase.
To Open: To puncture the seal, reverse the cap and place the puncture-top onto the tube. Push down firmly until seal is open. To close, screw the cap back onto the tube.
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL

FLUTICASONE PROPIONATEFLUTICASONE PROPIONATE CREAM
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||