Follistim AQ
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Follistim AQ safely and effectively. See full prescribing information for Follistim AQ. Follistim AQ (follitropin beta injection) for subcutaneous or intramuscular use Initial U.S. Approval: 1997INDICATIONS AND USAGEFollistim AQ is a gonadotropin indicated: In Women for: Induction of ovulation and pregnancy in anovulatory infertile women in whom the cause of infertility is functional and not due to primary ovarian failure (1.1) Development of multiple follicles in ovulatory women participating in an Assisted Reproductive Technology (ART) program (1.2) In Men for: Induction of spermatogenesis in men with primary and secondary hypogonadotropic hypogonadism (HH) in whom the cause of infertility is not due to primary testicular failure (1.3) DOSAGE AND ADMINISTRATION Ovulation Induction in Women (2.2) Starting daily dose of 75 international units of Follistim AQ is administered subcutaneously or intramuscularly for at least the first 7 days. The dose is increased by 25 or 50 international units at weekly intervals until follicular growth and/or serum estradiol levels indicate an adequate response. When an acceptable pre-ovulatory state is achieved, final oocyte maturation is achieved with 5000 to 10,000 international units of human chorionic gonadotropin (hCG). The woman and her partner should have intercourse daily, beginning on the day prior to the administration of hCG and until ovulation becomes apparent. Assisted Reproductive Technology (ART) in Women (2.3) Starting dose of 150 to 225 international units of Follistim AQ is administered subcutaneously or intramuscularly for at least the first 4 days of treatment. Subsequent doses are adjusted based upon ovarian response as determined by ultrasound evaluation of follicular growth and serum estradiol levels. Final oocyte maturation is induced with a dose of 5000-10,000 international units of hCG. Oocyte (egg) retrieval is performed 34 to 36 hours later. Induction of Spermatogenesis in Men (2.4) Pretreatment with hCG alone (1500 international units twice weekly) is required. If serum testosterone levels have not normalized after 8 weeks of hCG treatment, the dose may be increased to 3000 international units twice a week. After normalization of serum testosterone levels, administer 450 international units per week (225 international units twice weekly or 150 international units three times weekly) of Follistim AQ subcutaneously (only) with the same pre-treatment hCG dose used to normalize testosterone levels. DOSAGE FORMS AND STRENGTHSSingle-Use Vial 75 international units per 0.5 mL (3)Single-Use Vial 150 international units per 0.5 mL (3)CONTRAINDICATIONS Women and men who exhibit: Prior hypersensitivity to recombinant hFSH products (4) High levels of FSH indicating primary gonadal failure (4) Presence of uncontrolled non-gonadal endocrinopathies (4) Hypersensitivity reactions related to streptomycin or neomycin (4) Tumor of the ovary, breast, uterus, testis, hypothalamus or pituitary gland (4) Women who exhibit: Pregnancy (4, 8.1) Heavy or irregular vaginal bleeding of undetermined origin (4) Ovarian cysts or enlargement not due to polycystic ovary syndrome (PCOS) (4) WARNINGS AND PRECAUTIONSTreatment with Follistim AQ may result in: Abnormal Ovarian Enlargement (5.1) Ovarian Hyperstimulation Syndrome (OHSS) (5.2) Pulmonary and Vascular Complications (5.3) Ovarian Torsion (5.4) Multi-fetal Gestation and Birth (5.5) Congenital Anomalies (5.6) Ectopic Pregnancy (5.7) Spontaneous Abortion (5.8) Ovarian Neoplasms (5.9) Side EffectsThe most common adverse reactions (≥2%) in women undergoing ovulation induction are: ovarian hyperstimulation syndrome, ovarian cyst, abdominal discomfort, abdominal pain and lower abdominal pain. (6.1)The most common adverse reactions (≥2%) in women receiving ART are ovarian hyperstimulation syndrome and abdominal pain. (6.1)The most common (≥2%) adverse reactions in men undergoing induction of spermatogenesis are headache, acne, injection site reaction, injection site pain, gynecomastia, rash and dermoid cyst. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONSNursing Mothers: It is not known whether this drug is excreted in human milk. (8.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 FOLLISTIM AQ INDICATIONS AND USAGE
- 1.1 Induction of ovulation and pregnancy in anovulatory infertile women in whom the cause of infertility is functional and not due to primary ovarian failure
- 1.2 Development of multiple follicles in ovulatory women participating in an Assisted Reproductive Technology (ART) program
- 1.3 Induction of spermatogenesis in men with primary and secondary hypogonadotropic hypogonadism (HH) in whom the cause of infertility is not due to primary testicular failure
- 2 FOLLISTIM AQ DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 FOLLISTIM AQ CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 FOLLISTIM AQ ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 FOLLISTIM AQ DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PATIENT INFORMATION LEAFLET
- PATIENT INSTRUCTIONS FOR USE
- PRINCIPAL DISPLAY PANEL - 75 IU/0.5 mL Vial Carton
- PRINCIPAL DISPLAY PANEL - 150 IU/0.5 mL Vial Carton
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Follistim® AQ (follitropin beta injection) is indicated:
In Women for:
1.1 Induction of ovulation and pregnancy in anovulatory infertile women in whom the cause of infertility is functional and not due to primary ovarian failure
Prior to initiation of treatment with Follistim AQ:
- Women should have a complete gynecologic and endocrinologic evaluation.
- Primary ovarian failure should be excluded.
- The possibility of pregnancy should be excluded.
- Tubal patency should be demonstrated.
- The fertility status of the male partner should be evaluated.
1.2 Development of multiple follicles in ovulatory women participating in an Assisted Reproductive Technology (ART) program
Prior to initiation of treatment with Follistim AQ:
- Women should have a complete gynecologic and endocrinologic evaluation and diagnosis of cause of infertility.
- The possibility of pregnancy should be excluded.
- The fertility status of the male partner should be evaluated.
In Men for:
1.3 Induction of spermatogenesis in men with primary and secondary hypogonadotropic hypogonadism (HH) in whom the cause of infertility is not due to primary testicular failure
Prior to initiation of treatment with Follistim AQ:
- Men should have a complete medical and endocrinologic evaluation.
- Hypogonadotropic hypogonadism should be confirmed and primary testicular failure should be excluded.
- Serum testosterone levels should be normalized with human chorionic gonadotropin (hCG) treatment.
- The fertility status of the female partner should be evaluated.
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If the solution is not clear and colorless or has particles in it, the solution should not be used.
- Do not mix Follistim AQ with any other medicines in the same vial or in the same syringe.
2.2 Recommended Dosing for Ovulation Induction
The dosing scheme is stepwise and is individualized for each woman [see Clinical Studies (14.1)].
- A starting daily dose of 75 international units of Follistim AQ is administered for at least the first 7 days.
- Subsequent dosage adjustments are made at weekly intervals based upon ovarian response. If an increase in dose is indicated by the ovarian response, the increase should be made by 25 or 50 international units of Follistim AQ at weekly intervals until follicular growth and/or serum estradiol levels indicate an adequate ovarian response.
The following should be considered when planning the woman's individualized dose:
-
- Appropriate Follistim AQ dose adjustment(s) should be used to prevent multiple follicular growth and cycle cancellation.
- The maximum, individualized, daily dose of Follistim AQ is 300 international units.
- Treatment should continue until ultrasonic visualizations and/or serum estradiol determinations approximate the pre-ovulatory conditions seen in normal individuals.
- When pre-ovulatory conditions are reached, 5000 to 10,000 international units of hCG are used to induce final oocyte maturation and ovulation.
The administration of hCG must be withheld in cases where the ovarian monitoring suggests an increased risk of OHSS on the last day of Follistim AQ therapy [see Warnings and Precautions (5.1, 5.2, 5.10)]. - The woman and her partner should be encouraged to have intercourse daily, beginning on the day prior to the administration of hCG and until ovulation becomes apparent [see Warnings and Precautions (5.10) ].
- During treatment with Follistim AQ and during a two-week post-treatment period, the woman should be assessed at least every other day for signs of excessive ovarian stimulation.
It is recommended that Follistim AQ administration be stopped if the ovarian monitoring suggests an increased risk of OHSS or abdominal pain occurs. Most OHSS occurs after treatment has been discontinued and reaches its maximum at about seven to ten days post-ovulation.
2.3 Recommended Dosing for ART
The dosing scheme follows a stepwise approach and is individualized for each woman.
- A starting dose of 150 to 225 international units of Follistim AQ is administered subcutaneously or intramuscularly daily for at least the first 4 days of treatment.
- Subsequent dosing beyond the first 4 days of treatment is adjusted based upon the woman's ovarian response as determined by ultrasound evaluation of follicular growth and serum estradiol levels.
The following should be considered when planning the woman's individualized dose:- For most normal responding women, the daily starting dose can be continued until pre-ovulatory conditions are achieved (six to twelve days).
- For low or poor responding women, the daily dose should be increased according to the ovarian response. The maximum, individualized, daily dose of Follistim AQ is 600 international units.
- For high responding women [those at particular risk of abnormal ovarian enlargement and/or ovarian hyperstimulation syndrome (OHSS)], decrease or temporarily stop the daily dose, or discontinue the cycle according to individual response [see Warnings and Precautions (5.1, 5.2, 5.10)].
- When a sufficient number of follicles of adequate size are present, dosing of Follistim AQ is stopped and final maturation of the oocytes is induced by administering hCG at a dose of 5000 to 10,000 international units. The administration of hCG should be withheld in cases where the ovarian monitoring suggests an increased risk of OHSS on the last day of Follistim AQ therapy [see Warnings and Precautions (5.1, 5.2, 5.10)].
- Oocyte (egg) retrieval should be performed 34 to 36 hours following the administration of hCG.
2.4 Recommended Dosing for Induction of Spermatogenesis in Men
- Pretreatment with hCG is required prior to concomitant therapy with Follistim AQ and hCG. An initial dosage of 1500 international units of hCG should be administered at twice weekly intervals to normalize serum testosterone levels. If serum testosterone levels have not normalized after 8 weeks of hCG treatment, the hCG dose can be increased to 3000 international units twice weekly [see Clinical Studies (14.3)].
- After normal serum testosterone levels have been reached, Follistim AQ should be administered by subcutaneous injection concomitantly with hCG treatment. Follistim AQ should be given at a dosage of 450 international units per week, as either 225 international units twice weekly or 150 international units three times per week, in combination with the same hCG dose used to normalize testosterone levels.
The concomitant therapy should be continued for at least 3 to 4 months before any improvement in spermatogenesis can be expected. If a man has not responded after this period, the combination therapy may be continued. Treatment response has been noted at up to 12 months.
3 DOSAGE FORMS AND STRENGTHS
Follistim AQ Single-Use Vial 75 international units per 0.5 mL
Follistim AQ Single-Use Vial 150 international units per 0.5 mL
4 CONTRAINDICATIONS
Follistim AQ is contraindicated in women and men who exhibit:
- Prior hypersensitivity to recombinant hFSH products
- High levels of FSH indicating primary gonadal failure
- Presence of uncontrolled non-gonadal endocrinopathies (e.g., thyroid, adrenal, or pituitary disorders) [see Indications and Usage (1.1, 1.2, 1.3)]
- Hypersensitivity reactions to streptomycin or neomycin. Follistim AQ may contain traces of these antibiotics
- Tumor of the ovary, breast, uterus, testis, hypothalamus or pituitary gland
Follistim AQ is also contraindicated in women who exhibit:
- Pregnancy [see Use in Specific Populations (8.1)]
- Heavy or irregular vaginal bleeding of undetermined origin
- Ovarian cysts or enlargement not due to polycystic ovary syndrome (PCOS)
5 WARNINGS AND PRECAUTIONS
Follistim AQ should be used only by physicians who are experienced in infertility treatment. Follistim AQ is a potent gonadotropic substance capable of causing Ovarian Hyperstimulation Syndrome (OHSS) [see Warnings and Precautions (5.2)] with or without pulmonary or vascular complications [see Warnings and Precautions (5.3)] and multiple births [see Warnings and Precautions (5.5)]. Gonadotropin therapy requires the availability of appropriate monitoring facilities [see Warnings and Precautions (5.10)].
Careful attention should be given to the diagnosis of infertility and in the selection of candidates for Follistim AQ therapy [see Indications and Usage (1.1, 1.2, 1.3) and Dosage and Administration (2.2, 2.3, 2.4)].
5.1 Abnormal Ovarian Enlargement
In order to minimize the hazards associated with abnormal ovarian enlargement that may occur with Follistim AQ therapy, treatment should be individualized and the lowest effective dose should be used [see Dosage and Administration (2.2, 2.3)]. Use of ultrasound monitoring of ovarian response and/or measurement of serum estradiol levels is important to minimize the risk of overstimulation [see Warnings and Precautions (5.8)].
If the ovaries are abnormally enlarged on the last day of Follistim AQ therapy, hCG should not be administered in order to reduce the chances of developing Ovarian Hyperstimulation Syndrome (OHSS). Intercourse should be prohibited in patients with significant ovarian enlargement after ovulation because of the danger of hemoperitoneum resulting from ruptured ovarian cysts [see Warnings and Precautions (5.3)].
5.2 Ovarian Hyperstimulation Syndrome (OHSS)
OHSS is a medical entity distinct from uncomplicated ovarian enlargement and may progress rapidly to become a serious medical condition. OHSS is characterized by a dramatic increase in vascular permeability, which can result in a rapid accumulation of fluid in the peritoneal cavity, thorax, and potentially, the pericardium. The early warning signs of OHSS developing are severe pelvic pain, nausea, vomiting, and weight gain. Abdominal pain, abdominal distension, gastrointestinal symptoms including nausea, vomiting and diarrhea, severe ovarian enlargement, weight gain, dyspnea, and oliguria have been reported with OHSS. Clinical evaluation may reveal hypovolemia, hemoconcentration, electrolyte imbalances, ascites, hemoperitoneum, pleural effusions, hydrothorax, acute pulmonary distress, and thromboembolic reactions [see Warnings and Precautions (5.3)]. Transient liver function test abnormalities suggestive of hepatic dysfunction with or without morphologic changes on liver biopsy have also been reported in association with OHSS.
OHSS occurs after gonadotropin treatment has been discontinued and it can develop rapidly, reaching its maximum about seven to ten days following treatment. Usually, OHSS resolves spontaneously with the onset of menses. If there is evidence that OHSS may be developing prior to hCG administration [see Warnings and Precautions (5.1)], the hCG must be withheld. Cases of OHSS are more common, more severe, and more protracted if pregnancy occurs; therefore, women should be assessed for the development of OHSS for at least two weeks after hCG administration.
If serious OHSS occurs, treatment should be stopped and the patient should be hospitalized. Treatment is primarily symptomatic and overall should consist of bed rest, fluid and electrolyte management, and analgesics (if needed). Because the use of diuretics can accentuate the diminished intravascular volume, diuretics should be avoided except in the late phase of resolution as described below. The management of OHSS may be divided into three phases as follows:
-
Acute Phase:
Management should be directed at preventing hemoconcentration due to loss of intravascular volume to the third space and minimizing the risk of thromboembolic phenomena and kidney damage. Fluid intake and output, weight, hematocrit, serum and urinary electrolytes, urine specific gravity, BUN and creatinine, total proteins with albumin: globulin ratio, coagulation studies, electrocardiogram to monitor for hyperkalemia, and abdominal girth should be thoroughly assessed daily or more often based on the clinical need. Treatment, consisting of limited intravenous fluids, electrolytes, human serum albumin, is intended to normalize electrolytes while maintaining an acceptable but somewhat reduced intravascular volume. Full correction of the intravascular volume deficit may lead to an unacceptable increase in the amount of third space fluid accumulation -
Chronic Phase:
After the acute phase is successfully managed as above, excessive fluid accumulation in the third space should be limited by instituting severe potassium, sodium, and fluid restriction -
Resolution Phase:
As third space fluid returns to the intravascular compartment, a fall in hematocrit and increasing urinary output are observed in the absence of any increase in intake. Peripheral and/or pulmonary edema may result if the kidneys are unable to excrete third space fluid as rapidly as it is mobilized. Diuretics may be indicated during the resolution phase, if necessary, to combat pulmonary edema
OHSS increases the risk of injury to the ovary. The ascitic, pleural, and pericardial fluid should not be removed unless there is the necessity to relieve symptoms such as pulmonary distress or cardiac tamponade. Pelvic examination may cause rupture of an ovarian cyst, which may result in hemoperitoneum, and should therefore be avoided. If bleeding occurs and requires surgical intervention, the clinical objective should be to control the bleeding and retain as much ovarian tissue as possible.
During clinical trials with Follistim therapy, OHSS occurred in 7.6% of 105 women (OI) and 5.2% of 591 women (ART) treated with Follistim.
5.3 Pulmonary and Vascular Complications
Serious pulmonary conditions (e.g., atelectasis, acute respiratory distress syndrome) have been reported in women treated with gonadotropins. In addition, thromboembolic reactions both in association with, and separate from, OHSS have been reported following gonadotropin therapy. Intravascular thrombosis, which may originate in venous or arterial vessels, can result in reduced blood flow to vital organs or the extremities. Women with generally recognized risk factors for thrombosis, such as a personal or family history, severe obesity, or thrombophilia, may have an increased risk of venous or arterial thromboembolic events, during or following treatment with gonadotropins. Sequelae of such reactions have included venous thrombophlebitis, pulmonary embolism, pulmonary infarction, cerebral vascular occlusion (stroke), and arterial occlusion resulting in loss of limb and rarely in myocardial infarction. In rare cases, pulmonary complications and/or thromboembolic reactions have resulted in death. In women with recognized risk factors, the benefits of ovulation induction or in vitro fertilization (IVF) treatment need to be weighed against the risks. It should be noted that pregnancy itself also carries an increased risk of thrombosis.
5.4 Ovarian Torsion
Ovarian torsion has been reported after treatment with Follistim AQ and after intervention with other gonadotropins. This may be related to OHSS, pregnancy, previous abdominal surgery, past history of ovarian torsion, previous or current ovarian cyst and polycystic ovaries. Damage to the ovary due to reduced blood supply can be limited by early diagnosis and immediate detorsion.
5.5 Multi-fetal Gestation and Birth
Multi-fetal gestation and births have been reported with all gonadotropin treatments including Follistim AQ treatment. The woman and her partner should be advised of the potential risk of multi-fetal gestation and births before starting treatment.
5.6 Congenital Anomalies
The incidence of congenital malformations after ART may be slightly higher than after spontaneous conception. This slightly higher incidence is thought to be related to differences in parental characteristics (e.g., maternal age, sperm characteristics) and to the higher incidence of multi-fetal gestations after ART. There are no indications that the use of gonadotropins during ART is associated with an increased risk of congenital malformations.
5.7 Ectopic Pregnancy
Since infertile women undergoing ART, and particularly IVF, often have tubal abnormalities the incidence of ectopic pregnancies might be increased. Early confirmation of an intrauterine pregnancy should be determined by hCG testing and transvaginal ultrasound.
5.8 Spontaneous Abortion
The risk of spontaneous abortions (miscarriage) is increased with gonadotropin products. However, causality has not been established. The increased risk may be a factor of the underlying infertility.
5.9 Ovarian Neoplasms
There have been infrequent reports of ovarian neoplasms, both benign and malignant, in women who have undergone multiple drug regimens for ovulation induction; however, a causal relationship has not been established.
5.10 Laboratory Tests
For Women:
In most instances, treatment with Follistim AQ will result only in follicular growth and maturation. In order to complete the final phase of follicular maturation and to induce ovulation, hCG must be given following the administration of Follistim AQ or when clinical assessment indicates that sufficient follicular maturation has occurred. The degree of follicular maturation and the timing of hCG administration can both be determined with the use of sonographic visualization of the ovaries and endometrial lining in conjunction with measurement of serum estradiol levels. The combination of transvaginal ultrasonography and measurement of serum estradiol levels is also useful for minimizing the risk of OHSS and multi-fetal gestations.
The clinical confirmation of ovulation is obtained by the following direct or indirect indices of progesterone production as well as sonographic evidence of ovulation.
Direct or indirect indices of progesterone production are:
- Urinary or serum luteinizing hormone (LH) rise
- A rise in basal body temperature
- Increase in serum progesterone
- Menstruation following the shift in basal body temperature
The following provide sonographic evidence of ovulation:
- Collapsed follicle
- Fluid in the cul-de-sac
- Features consistent with corpus luteum formation
Sonographic evaluation of the early pregnancy is also important to rule out ectopic pregnancy.
For Men:
Clinical monitoring for spermatogenesis utilizes the following indirect or direct measures:
- Serum testosterone level
- Semen analysis
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed elsewhere in the labeling:
- Ovarian Hyperstimulation Syndrome [see Warnings and Precautions (5.2)]
- Atelectasis [see Warnings and Precautions (5.3)]
- Thromboembolism [see Warnings and Precautions (5.3)]
- Ovarian Torsion [see Warnings and Precautions (5.4)]
- Multi-fetal Gestation and Birth [see Warnings and Precautions (5.5)]
- Congenital Anomalies [see Warnings and Precautions (5.6)]
- Ectopic Pregnancy [see Warnings and Precautions (5.7)]
- Spontaneous Abortion [see Warnings and Precautions (5.8)]
6.1 Clinical Study Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Ovulation Induction
In a single cycle, multi-center, assessor-blind, parallel group, comparative study, a total of 172 chronic anovulatory women who had failed to ovulate and/or conceive with clomiphene citrate therapy, were randomized and treated with Follistim (105) or a urofollitropin comparator. Adverse reactions with an incidence of greater than 2% in either treatment group are listed in Table 1.
| System Organ Class/Adverse Reactions | Treatment Number (%) of Women |
|
|---|---|---|
| Follistim N=105 n (%) |
Comparator N=67 n (%) |
|
| Gastrointestinal disorders | ||
| Abdominal discomfort | 3 (2.9) | 1 (1.5) |
| Abdominal pain | 3 (2.9) | 2 (3.0) |
| Abdominal pain lower | 3 (2.9) | 1 (1.5) |
| Reproductive system and breast disorders | ||
| Ovarian cyst | 3 (2.9) | 2 (3.0) |
| Ovarian hyperstimulation syndrome | 8 (7.6) | 3 (4.5) |
| General disorders and administration site conditions | ||
| Pyrexia | 0 (0.0) | 2 (3.0) |
Adverse reactions reported commonly (greater than or equal to 2% of women treated with Follistim) in other ovulation induction clinical trials were headache, abdominal distension, constipation, diarrhea, nausea, pelvic pain, uterine enlargement, vaginal hemorrhage and injection site reaction.
The following medical events have been reported subsequent to pregnancies resulting from Follistim AQ therapy:
- Ectopic pregnancy [see Warnings and Precautions (5.7)]
- Spontaneous abortion [see Warnings and Precautions (5.8)]
ART
In a multiple cycle, multi-center, assessor-blind, parallel group, comparative study, after pituitary suppression with a gonadotropin release hormone (GnRH) agonist, a total of 989 women were randomized and treated with Follistim (N=591) or a urofollitropin comparator as part of in vitro fertilization therapy (IVF). Adverse reactions with an incidence of greater than 2% in either treatment group are listed in Table 2.
| System Organ Class/Adverse Reactions | Treatment Number (%) of Women |
|
|---|---|---|
| Follistim N=591 n (%) |
Comparator N=398 n (%) |
|
| Gastrointestinal disorders | ||
| Abdominal pain | 13 (2.2) | 4 (1.0) |
| Reproductive system and breast disorders | ||
| Ovarian hyperstimulation syndrome | 31 (5.2) | 17 (4.3) |
Adverse reactions reported commonly (greater than or equal to 2% of women treated with Follistim) in other IVF clinical trials were headache, abdominal distension, constipation, diarrhea, nausea, pelvic pain, breast tenderness, metrorrhagia, ovarian enlargement, vaginal hemorrhage, injection site reaction and rash.
The following medical events have been reported subsequent to pregnancies resulting from Follistim AQ therapy:
- Ectopic pregnancy [see Warnings and Precautions (5.7)]
- Spontaneous abortion [see Warnings and Precautions (5.8)]
Induction of Spermatogenesis
In an open-label, non-comparative clinical trial, 49 men with hypogonadotropic hypogonadism were enrolled to received pretreatment with hCG, followed by combination therapy with hCG and Follistim for induction of spermatogenesis. Of the 49 men, 30 received weekly Follistim doses of 450 international units; 24 of these 30 men received a total of 48 weeks of treatment with Follistim. Adverse reactions occurring with an incidence of greater than 2% in the 30 men treated with Follistim are listed in Table 3.
| System Organ Class/Adverse Reactions | Follistim Treatment N=30 n (%) |
|---|---|
| Nervous system disorders | |
| Headache | 2 (6.7) |
| General disorders and administration site disorders | |
| Injection site reaction | 2 (6.7) |
| Injection site pain | 2 (6.7) |
| Skin and subcutaneous tissue disorders | |
| Acne | 2 (6.7) |
| Rash | 1 (3.3) |
| Reproductive system and breast disorders | |
| Gynecomastia | 1 (3.3) |
| Neoplasms benign, malignant and unspecified | |
| Dermoid cyst | 1 (3.3) |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of Follistim and/or Follistim AQ. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Vascular disorders:
Thromboembolism [see Warnings and Precautions (5.3)]
7 DRUG INTERACTIONS
No drug-drug interaction studies have been performed.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category X: Follistim AQ should not be used during pregnancy [see Contraindications (4)].
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in the nursing infant from Follistim AQ, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Clinical studies of Follistim did not include subjects aged 65 and over.
10 OVERDOSAGE
Aside from the possibility of Ovarian Hyperstimulation Syndrome [see Warnings and Precautions (5.2, 5.3)] and multiple gestations [see Warnings and Precautions (5.5)], there is no additional information concerning the consequences of acute overdosage with Follistim AQ.
11 DESCRIPTION
Follistim AQ contains human follicle-stimulating hormone (hFSH), a glycoprotein hormone which is manufactured by recombinant DNA (rDNA) technology. The active drug substance, follitropin beta, has a dimeric structure containing two glycoprotein subunits (alpha and beta). Both the 92 amino acid alpha-chain and the 111 amino acid beta-chain have complex heterogeneous structures arising from two N-linked oligosaccharide chains. Follitropin beta is synthesized in a Chinese hamster ovary (CHO) cell line that has been transfected with a plasmid containing the two subunit DNA sequences encoding for hFSH. The purification process results in a highly purified preparation with a consistent hFSH isoform profile and high specific activity [as determined by the Ph. Eur. test for FSH in vivo bioactivity and on the basis of the molar extinction coefficient at 277 nm (εs:mg-1cm-1)=1.066].
The biological activity is determined by measuring the increase in ovary weight in female rats. The intrinsic luteinizing hormone (LH) activity in follitropin beta is less than 1 international unit per 40,000 international units FSH. The compound is considered to contain no LH activity.
The amino acid sequence and tertiary structure of the product are indistinguishable from that of hFSH of urinary source. Also, based on available data derived from physico-chemical tests and bioassay, follitropin beta and follitropin alfa, another recombinant follicle-stimulating hormone product, are indistinguishable.
Follistim AQ is presented as a sterile aqueous solution intended for subcutaneous (in men and women) or intramuscular (women only) administration. Each single-use vial of Follistim AQ contains the following per 0.5 mL: 75 international units or 150 international units of FSH activity; 25 mg sucrose NF; 7.35 mg sodium citrate (dihydrate) USP; 0.25 mg L-methionine USP; 0.1 mg polysorbate 20 NF; and water for injection USP. Hydrochloric acid NF and/or sodium hydroxide NF are used to adjust the pH to 7.
The recombinant protein in Follistim AQ has been standardized for FSH in vivo bioactivity in terms of the WHO International Standard for Follicle Stimulating Hormone (FSH) Recombinant, Human for Bioassay (code 92/642), issued by the World Health Organization Expert Committee on Biological Standardization (1995). Under current storage conditions, Follistim AQ may contain up to 11% of oxidized follitropin beta.
In clinical trials with Follistim, serum antibodies to FSH or anti-CHO cell derived proteins were not detected in any of the treated patients after exposure to Follistim for up to three cycles.
Therapeutic Class: Infertility.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Women:
Follicle-stimulating hormone (FSH), the active component in Follistim AQ, is required for normal follicular growth, maturation, and gonadal steroid production.
In women, the level of FSH is critical for the onset and duration of follicular development, and consequently for the timing and number of follicles reaching maturity. Follistim AQ stimulates ovarian follicular growth in women who do not have primary ovarian failure. In order to effect the final phase of follicle maturation, resumption of meiosis and rupture of the follicle in the absence of an endogenous LH surge, human chorionic gonadotropin (hCG) must be given following treatment with Follistim AQ when patient monitoring indicates appropriate follicular development parameters have been reached.
Men:
Follistim when administered with hCG stimulates spermatogenesis in men with hypogonadotropic hypogonadism. FSH, the active component of Follistim, is the pituitary hormone responsible for spermatogenesis.
12.3 Pharmacokinetics
Exposures of follitropin beta from Follistim AQ and Follistim are expected to be equivalent. The following information is based on studies conducted with Follistim.
Absorption:
Women:
The bioavailability of Follistim following subcutaneous and intramuscular administration was investigated in healthy, pituitary-suppressed, women given a single 300 international units dose. In these women, the area under the curve (AUC), expressed as the mean ± SD, was equivalent between the subcutaneous (455.6 ± 141.4 IU*h/L) and intramuscular (445.7 ± 135.7 IU*h/L) routes of administration. However, equivalence could not be established with respect to the peak serum FSH levels (Cmax). The Cmax achieved after subcutaneous administration and intramuscular administration was 5.41 ± 0.72 international units/L and 6.86 ± 2.90 international units/L, respectively. After subcutaneous or intramuscular injection the apparent dose absorbed was 77.8% and 76.4%, respectively.
The pharmacokinetics and pharmacodynamics of a single, intramuscular dose (300 international units) of Follistim were also investigated in a group (n=8) of gonadotropin-deficient, but otherwise healthy women. In these women, FSH (mean ± SD) AUC was 339 ± 105 international units*h/L, Cmax was 4.3 ± 1.7 international units/L. Cmax occurred at approximately 27 ± 5.4 hours after intramuscular administration.
A multiple dose, dose proportionality, pharmacokinetic study of Follistim was completed in healthy, pituitary-suppressed, women given subcutaneous doses of 75, 150, or 225 international units for 7 days. Steady-state blood concentrations of FSH were reached with all doses after 5 days of treatment based on the trough concentrations of FSH just prior to dosing (Ctrough). Peak blood concentrations with the 75, 150, and 225 international units dose were 4.30 ± 0.60 international units/L, 8.51 ± 1.16 international units/L and 13.92 ± 1.81 international units/L, respectively.
A multiple dose, dose proportionality, pharmacokinetic study of Follistim was completed in healthy, pituitary-suppressed, women given intramuscular doses of 75, 150, or 225 international units for 7 days. Steady-state blood concentrations of FSH were reached with all doses after 4 days of treatment based on the minimum concentrations of FSH just prior to dosing (Cmin). Peak blood concentrations with the 75, 150, and 225 international units dose were 4.65 ± 1.49 international units/L, 9.46 ± 2.57 international units/L and 11.30 ± 1.77 international units/L, respectively.
Men:
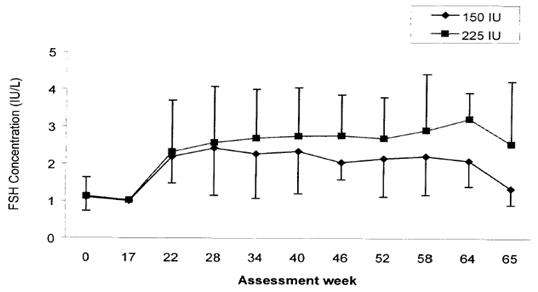
Serum levels of FSH were measured in a clinical study that compared the effects of two different dosing schedules of Follistim (150 international units three times a week or 225 international units twice a week) administered by subcutaneous injection concurrently with chorionic gonadotropin for injection for induction of spermatogenesis in hypogonadotropic hypogonadal men. Administration of Follistim was started at Week 17. Mean serum trough concentrations of FSH remained fairly constant over the treatment period. At the end of treatment (Week 64), the mean serum trough concentrations of FSH were 2.09 international units/L in the 150 international units group and 3.22 international units/L in the 225 international units group. Serum trough concentrations of FSH measured prior to the first Follistim injection on the Mondays of active treatment period (Weeks 17 to 64) and one week after the end of treatment period are presented in Figure 1.
Distribution:
The volume of distribution of Follistim in healthy, pituitary-suppressed, women following intravenous administration of a 300 international units dose was approximately 8 L.
Metabolism:
The recombinant FSH in Follistim AQ is biochemically very similar to urinary FSH and it is therefore anticipated that it is metabolized in the same manner.
Elimination:
The elimination half-life (t1/2) following a single intramuscular dose (300 international units) of Follistim in women was 43.9 ± 14.1 hours (mean ± SD). The elimination half-life following a 7-day intramuscular treatment of women with 75, 150, or 225 international units was 26.9 ± 7.8 hours (mean ± SD), 30.1 ± 6.2 and 28.9 ± 6.5, respectively.
Use in Specific Populations:
Body weight: The effect of body weight on the pharmacokinetics of Follistim was evaluated in a group of European and Japanese women who were significantly different in terms of body weight. The European women had a body weight of (mean ± SD) 67.4 ± 13.5 kg and the Japanese subjects were 46.8 ± 11.6 kg. Following a single intramuscular dose of 300 international units of Follistim, the AUC was significantly smaller in European women (339 ± 105 international units*h/L) than in Japanese women (544 ± 201 international units*h/L). However, clearance per kg of body weight was essentially the same for the respective groups (0.014 and 0.013 L/hr/kg).
Geriatric Use: The pharmacokinetics of Follistim has not been studied in geriatric subjects.
Pediatric Use: The pharmacokinetics of Follistim has not been studied in pediatric subjects.
Renal Impairment: The effect of renal impairment on the pharmacokinetics of Follistim has not been studied.
Hepatic Impairment: The effect of hepatic impairment on the pharmacokinetics of Follistim has not been studied.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term toxicity studies in animals have not been performed with Follistim to evaluate the carcinogenic potential of the drug. Follistim was not mutagenic in the Ames test using S. typhimurium and E. coli tester strains and did not produce chromosomal aberrations in an in vitro assay using human lymphocytes.
14 CLINICAL STUDIES
14.1 Ovulation Induction
The efficacy of Follistim for Ovulation Induction was evaluated in a randomized, assessor-blind, parallel-group comparative, multicenter safety and efficacy study of 172 chronic anovulatory women (105 subjects on Follistim) who had previously failed to ovulate and/or conceive during clomiphene citrate treatment. The study results for ovulation rates are summarized in Table 4 and those for pregnancy rates are summarized in Table 5.
| Cycle | Follistim (n=105) |
|---|---|
| First treatment cycle | 72% |
| Second treatment cycle | 82% |
| Third treatment cycle | 85% |
| Cycle | Follistim (n=105) |
|---|---|
| First treatment cycle | 14% |
| Second treatment cycle | 19% |
| Third treatment cycle | 23% |
14.2 Assisted Reproductive Technology (ART)
The efficacy of Follistim as part of an Assisted Reproductive Technology (ART) program was established in three studies, two of which are described below.
Follistim was evaluated in a randomized, assessor-blind, parallel-group, comparative, multicenter safety and efficacy study of 981 healthy normal ovulatory infertile women (mean age 32) treated for multiple cycles with in vitro fertilization and controlled ovarian stimulation with Follistim (n=585) or urofollitropin (n=396) after pituitary suppression with a GnRH agonist. The first cycle results with Follistim are summarized in Table 6.
| Parameter | Follistim (n=585) |
|---|---|
| Total number of oocytes recovered | 10.9 |
Ongoing  |
22.2% |
Ongoing   |
26.0% |
Follistim was also evaluated in a randomized, assessor-blind, parallel-group, comparative, single center safety and efficacy study in 89 infertile healthy normal ovulatory women (mean age 32) treated for one cycle with in vitro fertilization and controlled ovarian stimulation with Follistim (n=54) or menotropins (n=35) without pituitary suppression with a GnRH agonist. The results with Follistim are summarized in Table 7.
| Parameter | Follistim (n=54) |
|---|---|
| Total number of oocytes recovered | 9.9 |
Ongoing  |
22.2% |
Ongoing   |
30.8% |
14.3 Induction of Spermatogenesis
The safety and efficacy of Follistim administered by subcutaneous injection concomitantly with chorionic gonadotropin for injection (hCG) has been examined in a multicenter, open-label, non-comparator clinical study for induction of spermatogenesis in hypogonadotropic hypogonadal men. The study compared the effects of two different Follistim dosing schedules on semen parameters and serum levels of follicle stimulating hormone (FSH). The multicenter study involved a 16-week pretreatment phase with hCG at a dosage of 1500 international units twice a week to normalize serum testosterone levels. If serum testosterone levels did not normalize after 8 weeks of hCG treatment, the hCG dose could have been increased to 3000 international units twice a week. This phase was followed by a 48-week treatment phase. Men who were still azoospermic after the pretreatment phase were randomized to receive either 225 international units Follistim together with 1500 international units hCG twice a week or 150 international units Follistim three times a week together with 1500 international units hCG twice weekly. Men who required 3000 international units of hCG twice a week in the pretreatment phase were continued on that dosage during the treatment phase. The mean age of patients in both treatment groups was approximately 30 years (range 18 to 47 years). At baseline, mean left and right testis volumes were 4.61 ± 2.94 mL and 4.57 ± 3.00 mL, respectively, in the group receiving three weekly injections of Follistim. For the group receiving two weekly injections of Follistim, the mean left and right testis volumes were 6.54 ± 2.45 mL and 7.21 ± 2.94 mL, respectively, at baseline. The primary efficacy endpoint was the percentage of patients with a mean sperm density of ≥1 x 106/mL on their last two treatment assessments. The outcomes of treatment in the 30 men enrolled in the treatment phase are summarized in Table 8.
| Follistim 150 international units three times a week (n=15) |
Follistim 225 international units twice a week (n=15) |
Overall (n=30) |
||||
|---|---|---|---|---|---|---|
| Sperm Density of ≥106/mL | n | % | n | % | n | % |
| Yes | 6 | 40 | 7 | 47 | 13 | 43 |
| No | 9 | 60 | 8 | 53 | 17 | 57 |
Overall, the median time to reach a sperm concentration of 106 per mL was 165 days (range 25 to 327 days) in patients who demonstrated a sperm concentration of at least 106 per mL. The median time to reach a sperm concentration of at least 106 per mL was 186 days (range 25 to 327 days) for the 150 international units group and 141 days (range 43 to 204 days) for the 225 international units group. No pregnancy data were collected during the trial.
The local tolerance data were comparable between the two treatment groups. The mean percentage of days without pain calculated for all subjects in the treatment period was 91.3% for patients in the 150 international units (three times a week) and 76.0% for patients in the 225 international units (two times a week) Follistim treatment groups. In the 225 international units (twice per week) group, local symptoms judged as severe by the investigator were: itching in 1 patient (7%), pain in 2 patients (13%), bruising in 2 patients (13%), swelling in 2 patients (13%), and redness in 1 patient (7%). In the 150 international units (three times per week) group, 1 event in 1 patient (bruising, 7%) was judged as severe. No patient discontinued treatment due to injection site reaction or injection site pain.
16 HOW SUPPLIED/STORAGE AND HANDLING
Follistim AQ (follitropin beta injection) is supplied as a sterile aqueous solution in a 2-mL vial to deliver 0.5 mL of the drug in the following concentrations and packaging:
Follistim AQ Single-Use Vial 75 international units per 0.5 mL
| Box of 1 | NDC 0052-0308-02 |
Follistim AQ Single-Use Vial 150 international units per 0.5 mL
| Box of 1 | NDC 0052-0309-02 |
Store refrigerated, 2° - 8°C (36° - 46°F) until dispensed. Upon dispensing, the product may be stored by the patient at 2° - 8°C (36° - 46°F) until the expiration date, or at or below 25°C (77°F) for 3 months or until expiration date, whichever occurs first. Protect from light, keep container in carton. Do not freeze.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling
17.1 Therapy Duration and Necessary Monitoring in Women and Men Undergoing Treatment
Prior to beginning therapy with Follistim AQ, inform women and men about the time commitment and monitoring procedures necessary to undergo treatment [see Dosage and Administration (2), Warnings and Precautions (5.10)].
17.2 Instructions on a Missed Dose
Inform women and men that if they miss or forget to take a dose of Follistim AQ, the next dose should not be doubled and they should call the healthcare provider for further dosing instructions.
17.3 Ovarian Hyperstimulation Syndrome
Inform women regarding the risks with use of Follistim AQ of Ovarian Hyperstimulation Syndrome [see Warnings and Precautions (5.2)] and associated symptoms including lung and blood vessel problems [see Warnings and Precautions (5.3)] and ovarian torsion [see Warnings and Precautions (5.4)].
17.4 Multi-fetal Gestation and Birth
Inform women regarding the risk of multi-fetal gestations with the use of Follistim AQ [see Warnings and Precautions (5.5)].
Manufactured for: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USA
Manufactured by: N.V. Organon, Oss, The Netherlands, a subsidiary of
Merck & Co., Inc., Whitehouse Station, NJ 08889, USA
For patent information: www.merck.com/product/patent/home.html
Copyright © 2005, 2010 Merck Sharp & Dohme B.V., a subsidiary of Merck & Co., Inc. All rights reserved.
Revised: 12/2013
uspi-mk8328-SOi-1312R006
PATIENT INFORMATION LEAFLET
Follistim® (Fol´-lis-tim) AQ
(follitropin beta injection)
Single-Use Vial
Read the Patient Information that comes with Follistim® AQ before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment.
What is Follistim AQ?
Follistim AQ is a prescription medicine that contains follicle-stimulating hormone (FSH).
Follistim AQ is used:
In women:
- to help healthy ovaries to develop (mature) and release eggs
- as part of an Assisted Reproductive Technology (ART) program to help the ovaries produce more mature eggs
In men:
- to help bring about the production and development of sperm
Who should not take Follistim AQ?
Do not take Follistim AQ if you are a Woman or Man who:
- is allergic to recombinant human FSH products
- has a high level of FSH in your blood indicating that your ovaries (women only) or testes (men only) may be permanently damaged and do not work at all
- has uncontrolled thyroid, pituitary, or adrenal gland problems
- is allergic to streptomycin or neomycin (types of antibiotics)
- has a tumor of the hypothalamus, pituitary gland, breast, uterus (women only), ovary (women only), or testis (men only)
Do not take Follistim AQ if you are a Woman who:
- is pregnant or think you may be pregnant
- has heavy or irregular vaginal bleeding and the cause is not known
- has ovarian cysts or enlarged ovaries, not due to polycystic ovary syndrome (PCOS)
Talk to your healthcare provider before taking this medicine if you have any of the conditions listed above.
What should I tell my healthcare provider before taking Follistim AQ?
Before you take Follistim AQ, tell your healthcare provider if you:
- have an increased risk of blood clots (thrombosis)
- have ever had a blood clot (thrombosis), or anyone in your immediate family has ever had a blood clot (thrombosis)
- had stomach (abdominal) surgery
- had twisting of your ovary (ovarian torsion)
- had or have a cyst in your ovary
- have polycystic ovary disease
- have any other medical conditions
- are breastfeeding or plan to breastfeed. It is not known if Follistim AQ passes into your breast milk. You and your healthcare provider should decide if you will take Follistim AQ or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of them and show your healthcare provider and pharmacist when you get a new medicine.
How should I use Follistim AQ?
- Be sure that you read, understand, and follow the "Patient Instructions for Use" that come with Follistim AQ.
- Use Follistim AQ exactly as your healthcare provider tells you to.
- Your healthcare provider will tell you how much Follistim AQ to use, how to inject it, and how often it should be injected.
- Do not inject Follistim AQ at home until your healthcare provider has taught you the right way.
- Do not mix Follistim AQ with any other medicines in the same vial or in the same syringe.
- Do not change your dose of Follistim AQ unless your healthcare provider tells you to.
- Call your healthcare provider immediately if you use too much Follistim AQ.
- If you miss or forget to take a dose, do not double your next dose. Ask your healthcare provider for instructions.
- Your healthcare provider will do blood and urine hormone tests while you are taking Follistim AQ. Make sure you follow-up with your healthcare provider to have your blood and urine tested when told to do so.
Women:
- Your healthcare provider may do ultrasound scans of your ovaries. Make sure you follow-up with your healthcare provider to have your ultrasound scans.
Men:
- Your healthcare provider may test your semen while you are taking Follistim AQ. Make sure you follow-up with your healthcare provider to give a semen sample for testing.
What are the possible side effects of Follistim AQ?
Follistim AQ may cause serious side effects.
Serious side effects in women include:
- Ovarian enlargement
-
Ovarian hyperstimulation syndrome (OHSS). OHSS is a serious medical problem that can happen when the ovaries are over stimulated. In rare cases it has caused death. OHSS causes fluid to build up suddenly in your stomach and chest areas and can cause blood clots to form. Call you healthcare provider right away if you have:
- pain in your lower stomach area
- nausea
- vomiting
- weight gain
- diarrhea
- decreased urine output
- trouble breathing
- Lung problems. Follistim AQ can cause you to have fluid in your lungs (atelectasis) and trouble breathing (acute respiratory distress syndrome).
-
Blood clots. Follistim AQ may increase your chance of having blood clots in your blood vessels. Blood clots can cause:
- blood vessel problems (thrombophlebitis)
- stroke
- loss of your arm or leg
- blood clot in your lungs (pulmonary embolus)
- heart attack
- Ovarian torsion. Follistim AQ may increase the chance of twisting of the ovaries in women with certain conditions such as OHSS, pregnancy and previous abdominal surgery. Twisting of the ovary could cause the blood flow to the ovary to be cut off.
- Pregnancy and birth of multiple babies. Having a pregnancy with more than one baby at a time increases the health risk for you and your babies. Discuss your chances of multiple births with your healthcare provider.
- Birth defects. A woman's age, certain sperm problems, genetic background of both parents and a pregnancy with multiple babies can increase the chance that your baby might have birth defects.
- Ectopic pregnancy (pregnancy outside of the womb). The chance of a pregnancy outside of the womb is increased in women with damaged fallopian tubes.
- Miscarriage. The chance of loss of an early pregnancy may be increased in women who have difficulty with becoming pregnant at all.
The most common side effects of Follistim AQ include:
In women:
- cyst in the ovary
- stomach pain
In men:
- headache
- pain at the injection site
- bruising, swelling or redness at the injection site
- breast enlargement
- acne
These are not all the possible side effects of Follistim AQ. For more information, ask your healthcare provider or pharmacist.
Call your healthcare provider immediately if you get worsening or strong abdominal pain. Also, call your healthcare provider immediately if this happens some days after the last injection has been given.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Follistim AQ?
- Store Follistim AQ in the refrigerator between 2° - 8°C (36° - 46°F) until the expiration date.
- Follistim AQ can be stored at or below 25°C (77°F) for 3 months or until the expiration date, whichever comes first.
- Keep Follistim AQ away from light.
- Do not freeze.
Keep Follistim AQ and all medicines out of the reach of children.
General information about Follistim AQ
Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. Do not use Follistim AQ for a condition for which it was not prescribed. Do not give Follistim AQ to other people, even if they have the same condition that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about Follistim AQ. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for more information about Follistim AQ that is written for healthcare professionals.
For more information, go to www.follistim.com or call 1-866-836-5633.
What are the ingredients in Follistim AQ?
Active ingredient: follitropin beta
Inactive ingredients: sucrose, sodium citrate, L-methionine, polysorbate 20, water for injection, hydrochloric acid, and/or sodium hydroxide.
Manufactured for: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USA
Manufactured by: N.V. Organon, Oss, The Netherlands, a subsidiary of
Merck & Co., Inc., Whitehouse Station, NJ 08889, USA
For patent information: www.merck.com/product/patent/home.html
Copyright © 2005, 2010 Merck Sharp & Dohme B.V., a subsidiary of Merck & Co., Inc. All rights reserved.
Revised: 12/2013
usppi-mk8328-SOi-1312R006
PATIENT INSTRUCTIONS FOR USE
Follistim® (Fol´-lis-tim) AQ
(follitropin beta injection)
Single-Use Vial
Read the Patient Instructions for Use that comes with Follistim® AQ before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment.
A. Getting Ready
- Remove the vial from the refrigerator.
- Check the liquid in the vial. It should appear clear and colorless. If the solution is not clear and colorless or has particles in it, do not use it.
-
Gather the supplies you will need for your injection. You will need:
- a clean dry surface
- alcohol
- cotton balls or alcohol pads
- sterile gauze
- a puncture-proof container to throw away the used syringe and needle
- Wash your hands and dry them.
B. Preparing your Follistim AQ Injection
- Flip off the protective cap on the top of the vial. Do not remove the rubber stopper. Wipe the top of the rubber stopper with an alcohol wipe.
- Use a syringe and needle that has been recommended by your healthcare provider, attach a needle to the syringe.
C. Draw up your Dose
- Carefully remove the needle cover (cap) from the needle (See Figure 1).
- Pull back on the plunger to draw the amount of air into the syringe equal to the dose needed.
- With the vial on a flat work surface, insert the needle straight down through the rubber stopper of the Follistim AQ vial.
- Push the plunger of the syringe down to inject the air from the syringe into the vial of Follistim AQ. The air injected into the vial will allow Follistim AQ to be easily withdrawn into the syringe.
- Keep the needle inside the vial. Turn the vial and syringe upside down. Be sure that the tip of the Follistim AQ needle is in the liquid. Slowly pull back on the plunger to fill the syringe with Follistim AQ liquid to the number (mL or cc) that matches the dose your healthcare provider prescribed (See Figure 2).
D. Remove the Air
- Hold the syringe with the needle pointed up. Check for air bubbles in the syringe. A small amount of air will not hurt you. If you see large air bubbles, gently tap the side of the syringe with your finger until the air bubbles rise to the top of the syringe.
- Slowly push the plunger to force the air bubbles out of the syringe. You will see a drop of liquid on the tip of the needle (See Figure 3).
- Double-check that you have the right dose in the syringe. Lay the syringe down on its side until you have selected and prepared your injection site.
E. Selecting and Preparing the Injection Site
- Follistim AQ can be injected into your body using two different ways (routes) as described below. Follow your healthcare provider's instructions about how you should inject Follistim AQ.
-
1. Subcutaneous Route:
For women and men:- Follistim AQ can be injected directly into a layer of fat under your skin (subcutaneously).
- When giving a subcutaneous injection, follow your healthcare provider's instructions about changing the site for each injection. This will help lower your chances of having a skin reaction.
- Do not inject Follistim AQ into an area that is tender, red, bruised, or hard.
- Recommended sites for injecting Follistim AQ subcutaneously are:
- Just below your belly button (navel) (See Figure 4)
- The upper outer area of your thigh (See Figure 4)
Figure 4
- Clean the skin with an alcohol wipe where the injection is to be made. Be careful not to touch the skin that has been wiped clean.
- Pick up the prepared syringe and needle and hold it in the hand that you will use to inject the medicine.
- Use the other hand to pinch a fold of skin at the cleaned injection site. Do not touch the cleaned area of skin.
- Hold the syringe like you would a pencil. Use a quick "dart-like" motion to insert the needle either straight up and down (90-degree angle) or at a slight angle (45-degree angle) (See Figure 5).
Figure 5
- Let go of the syringe and slowly pull back on the plunger. If blood comes into the syringe, Do not inject Follistim AQ because the needle might have entered a blood vessel.
- If no blood is seen and the needle is properly placed, push the plunger slowly and steadily to inject the Follistim AQ solution.
- Once you have injected the entire content of the syringe, pull the needle out of your skin and press a cotton ball or gauze over the injection site and hold it there for several seconds (See Figure 6).
- Gently massage the site while still maintaining pressure. This will help disperse the Follistim AQ solution and may relieve any discomfort.
-
Do not put the needle cover (cap) back on the needle.
Figure 6
- Throw away the used needle and syringe in your puncture-proof container. (See "How Do I Throw Away Used Syringes and Needles?")
- For each injection, prepare a new syringe of Follistim AQ using the instructions above. Clean a new area of skin. In this new area of clean skin, again insert a new needle (as you did before), and again pull the plunger back slightly. If blood does not enter the syringe, inject the Follistim AQ by slowly pushing the plunger all the way down.
- Pull the needle out of your skin and press a cotton ball or gauze over the injection site and hold it there for several seconds. Do not put the needle cover (cap) back on the needle.
- Throw away the used needle and syringe in your puncture-proof container. (See "How Do I Throw Away Used Syringes and Needles?")
-
2. Intramuscular Route:
For women only:- You will need to ask another person to give you your Follistim AQ injection intramuscularly (IM).
- Follistim AQ can be injected directly into your muscle (intramuscularly).
- When giving an intramuscular injection, follow your healthcare provider's instructions about changing the site for each injection. This will help lower your chances of having a skin reaction.
- Do not inject Follistim AQ into an area that is tender, red, bruised, or hard.
- Recommended site for injecting Follistim AQ intramuscularly is:
- The upper outer area of the buttock (See Figure 7).
Figure 7
- The upper outer area of the buttock (See Figure 7).
- Relax the muscle first by shifting your weight to the leg opposite of the side that the medicine will be injected into.
- Clean the skin with an alcohol wipe where the injection is to be made. Be careful not to touch the skin that has been wiped clean.
- Pick up the prepared syringe and needle and hold it in the hand that you will use to inject the medicine.
- Use the other hand to stretch a fold of skin at the cleaned injection site. Stretching the skin helps the needle to go in more easily and pushes the tissue beneath the skin out of the way. Do not touch the cleaned area of skin (See Figure 8).
- Hold the syringe like you would a pencil. Use a quick "dart-like" motion to insert the needle straight up and down (90-degree angle) (See Figure 8).
Figure 8 - Let go of the syringe and slowly pull back on the plunger. If blood comes into the syringe, Do not inject Follistim AQ because the needle might have entered a blood vessel.
- Pull the needle out of your skin and press a cotton ball or gauze over the injection site and hold it there for several seconds (See Figure 6).
- Gently massage the site while still maintaining pressure. This will help disperse the Follistim AQ solution and may relieve any discomfort.
- Do not put the needle cover (cap) back on the needle.
- Throw away the used needle and syringe in your puncture-proof container. (See "How Do I Throw Away Used Syringes and Needles?")
- For each injection, prepare a new syringe of Follistim AQ using the instructions above. Clean a new area of skin. In this new area of clean skin, again insert a new needle (as you did before), and again pull the plunger back slightly. If blood does not enter the syringe, inject the Follistim AQ by slowly pushing the plunger all the way down.
- Pull the needle out of your skin and press a cotton ball or gauze over the injection site and hold it there for several seconds.
- Do not put the needle cover (cap) back on the needle.
- Throw away the used needle and syringe in your puncture-proof container. (See "How Do I Throw Away Used Syringes and Needles?")
How Do I Throw Away Used Syringes and Needles?
Check with your healthcare provider or pharmacist for instructions about the right way to throw away used syringes and needles. There may be special local or state laws about how to throw away used syringes and needles.
- Do not throw away used syringes and needles in the household trash and do not recycle them.
- Put used and empty Follistim AQ syringes, needles, and vials in a closeable, puncture-resistant container. You may use a sharps container (such as a red bio-hazard container), a hard plastic container with a screw-on cap (such as an empty detergent bottle) or in a metal container with a plastic lid, (such as a coffee can).
- When the container is full, tape around the cap or lid to make sure the cap or lid does not come off.
- When your injection is given by another person, this person must also be careful when removing the syringe and needle and disposing of the syringe and needle to prevent accidental needle stick injury and passing infection.
- Store Follistim AQ in the refrigerator at 2° - 8°C (36° - 46°F) until the expiration date.
- Follistim AQ can be stored at or below 25°C (77°F) for 3 months or until the expiration date, whichever comes first.
- Keep Follistim AQ away from light.
- Do not freeze.
- You will need to ask another person to give you your Follistim AQ injection intramuscularly (IM).
Manufactured for: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USA
Manufactured by: N.V. Organon, Oss, The Netherlands, a subsidiary of
Merck & Co., Inc., Whitehouse Station, NJ 08889, USA
For patent information: www.merck.com/product/patent/home.html
Copyright © 2005, 2010 Merck Sharp & Dohme B.V., a subsidiary of Merck & Co., Inc. All rights reserved.
Revised: 12/2013
usppi-mk8328-SOi-1312R006
PRINCIPAL DISPLAY PANEL - 75 IU/0.5 mL Vial Carton
NDC 0052-0308-02
One Single-Use Vial
contains 75 IU/0.5 mL
Discard Unused Portion.
Follistim
®
AQ
(follitropin beta injection)
75
IU
For Subcutaneous or
Intramuscular Injection
Rx only

PRINCIPAL DISPLAY PANEL - 150 IU/0.5 mL Vial Carton
NDC 0052-0309-02
One Single-Use Vial
contains 150 IU/0.5 mL
Discard Unused Portion.
Follistim
®
AQ
(follitropin beta injection)
150
IU
For Subcutaneous or
Intramuscular Injection
Rx only

Follistim AQfollitropin INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Follistim AQfollitropin INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||