Hetastarch
Teva Parenteral Medicines, Inc
6% Hetastarch In 0.9% Sodium Chloride Injection
FULL PRESCRIBING INFORMATION: CONTENTS*
- HETASTARCH DESCRIPTION
- CLINICAL PHARMACOLOGY
- HETASTARCH INDICATIONS AND USAGE
- HETASTARCH CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- HETASTARCH ADVERSE REACTIONS
- HETASTARCH DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- References:
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
HETASTARCH DESCRIPTION
6% Hetastarch in 0.9% Sodium Chloride Injection (Hetastarch Injection) is a sterile, nonpyrogenic solution for intravenous administration.
The composition of each 100 mL is as follows:
| Hetastarch................................................................ | 6 g |
| Sodium Chloride, USP............................................. | 0.9 g |
| Water for Injection, USP.......................................... | qs |
|
pH adjusted with Sodium Hydroxide, NF if necessary |
|
| Concentration of Electrolytes (mEq/L): Sodium 154, Chloride 154 | |
|
pH: approximately 5.5 with negligible buffering capacity |
|
| Calculated Osmolarity: approximately 309 m0sM | |
Hetastarch is an artificial colloid derived from a waxy starch composed almost entirely of amylopectin. Hydroxyethyl ether groups are introduced into the glucose units of the starch, and the resultant material is hydrolyzed to yield a product with a molecular weight suitable for use as a plasma volume expander and erythrocyte sedimenting agent. Hetastarch is characterized by its molar substitution and also by its molecular weight. The molar substitution is approximately 0.75 which means hetastarch has an average of approximately 75 hydroxyethyl groups for every 100 glucose units. The weight average molecular weight is approximately 600,000 with a range of 450,000 to 800,000 and with at least 80% of the polymers falling within the range of 20,000 to 2,500,000. Hydroxyethyl groups are attached by either linkage primarily at C-2 of the glucose unit and to a lesser extent at C-3 and C-6. The polymer resembles glycogen, and the polymerized D-glucose units are joined primarily by α-1,4 linkages with occasional α-1,6 branching linkages. The degree of branching is approximately 1:20 which means that there is an average of approximately one α-1,6 branch for every 20 glucose monomer units.
The chemical name for hetastarch is hydroxyethyl starch.
The structural formula is as follows:
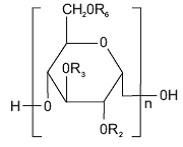
Amylopectin derivative in which R2 and R3 are H or CH2CH2OH and R6 is H, CH2CH2OH, or a branching point in the starch polymer connected through an α-1,6 link to additional D-glucopyranosyl units.
Hetastarch injection is a clear, pale yellow to amber solution. Exposure to prolonged adverse storage conditions may result in a change to a turbid deep brown or the formation of a crystalline precipitate. Do not use the solution if these conditions are evident.
The flexible plastic container is fabricated from a specially formulated polyvinylchloride. Solutions in contact with the plastic container may leach out certain chemical components from the plastic in very small amounts; however, biological testing was supportive of the safety of the plastic container materials. The container solution unit is a closed system and is not dependent upon entry of external air during administration. The container is overwrapped to provide protection from the physical environment and to provide an additional moisture barrier when necessary.
The closure system has two ports; the one for the administration set has a tamper evident plastic protector.
CLINICAL PHARMACOLOGY
The plasma volume expansion produced by hetastarch injection approximates that of 5% Albumin (Human). Intravenous infusion of hetastarch injection results in expansion of plasma volume that decreases over the succeeding 24 to 36 hours. The degree of plasma volume expansion and improvement in hemodynamic state depend upon the patient's intravascular status.
Hetastarch molecules below 50,000 molecular weight are rapidly eliminated by renal excretion. A single dose of approximately 500 mL of hetastarch injection (approximately 30 g) results in elimination in the urine of approximately 33% of the dose within 24 hours. This is a variable process but generally results in an intravascular hetastarch concentration of less than 10% of the total dose injected by two weeks. A study of the biliary excretion of hetastarch in 10 healthy males accounted for less than 1% of the dose over a 14 day period. The hydroxyethyl group is not cleaved by the body but remains intact and attached to glucose units when excreted. Significant quantities of glucose are not produced as hydroxyethylation prevents complete metabolism of the smaller polymers.
The addition of hetastarch to whole blood increases the erythrocyte sedimentation rate. Therefore hetastarch injection is used to improve the efficiency of granulocyte collection by centrifugal means.
In randomized, controlled, comparative studies of hetastarch injection (n=92) and Albumin (n=85) in surgical patients, no patient in either treatment group had a bleeding complication and no significant difference was found in the amount of blood loss between the treatment groups.1-4
HETASTARCH INDICATIONS AND USAGE
Hetastarch injection is indicated in the treatment of hypovolemia when plasma volume expansion is desired. It is not a substitute for blood or plasma.
The adjunctive use of hetastarch injection in leukapheresis has also been shown to be safe and efficacious in improving the harvesting and increasing the yield of granulocytes by centrifugal means.
HETASTARCH CONTRAINDICATIONS
Hetastarch injection is contraindicated in patients with known hypersensitivity to hydroxyethyl starch or with bleeding disorders or with congestive heart failure where volume overload is a potential problem. Hetastarch injection should not be used in renal disease with oliguria or anuria not related to hypovolemia.
Patients with pre-existing coagulation or bleeding disorders should not be given hetastarch injection.
WARNINGS
Life-threatening anaphylactic/anaphylactoid reactions have been rarely reported with hetastarch injection; death has occurred, but a causal relationship has not been established. Patients who develop severe anaphylactic/anaphylactoid reactions may need continued supportive care until symptoms have resolved.
Hypersensitivity reactions can occur even after hetastarch injection has been discontinued.
Usage in Plasma Volume Expansion
Hetastarch injection has not been adequately evaluated to establish its safety in situations other than treatment of hypovolemia in elective surgery.
Large volumes of hetastarch injection may transiently alter the coagulation mechanism due to hemodilution and a mild direct inhibitory action on Factor VIII. Administration of volumes of hetastarch injection that are greater than 25% of the blood volume in less than 24 hours may cause significant hemodilution reflected by lower hematocrit and plasma protein values. Administration of packed red cells, platelets, or fresh frozen plasma should be considered if clinically indicated.
Hetastarch injection is not recommended for use as a cardiac bypass pump prime, while the patient is on cardiopulmonary bypass, or in the immediate period after the pump has been discontinued because of the risk of increasing coagulation abnormalities and bleeding in patients whose coagulation status is already impaired. However, this risk of bleeding diminished within hours.5-6
Hematocrit may be decreased and plasma proteins diluted excessively by administration of large volumes of hetastarch injection. Administration of packed red cells, platelets, and fresh frozen plasma should be considered if excessive dilution occurs.
Use over extended periods: Hetastarch injection has not been adequately evaluated to establish its safety in situations other than leukapheresis that require frequent use of colloidal solutions over extended periods. In some cases, hetastarch has been associated with coagulation abnormalities in conjunction with an acquired, reversible von Willebrand's-like syndrome and/or Factor VIII deficiency when used over a period of days. Replacement therapy should be considered if a severe Factor VIII deficiency is identified. If a coagulopathy develops, it may take several days to resolve. Certain conditions may affect the safe use of hetastarch injection on a chronic basis. For example, in patients with subarachnoid hemorrhage where hetastarch injection is used repeatedly over a period of days for the prevention of cerebral vasospasm, significant clinical bleeding may occur. Intracranial bleeding resulting in death has been reported.7
Usage in Leukapheresis
Slight declines in platelet counts and hemoglobin levels have been observed in donors undergoing repeated leukapheresis procedures using hetastarch injection due to the volume expanding effects of hetastarch and to the collection of platelets and erythrocytes. Hemoglobin levels usually return to normal within 24 hours. Hemodilution by hetastarch injection may also result in 24 hour declines of total protein, albumin, calcium, and fibrinogen levels. None of these decreases are to a degree recognized to be clinically significant risks to healthy donors.
PRECAUTIONS
General
If administration is by pressure infusion, all air should be withdrawn or expelled from the bag through the medication port prior to infusion.
Caution should be used when administering hetastarch injection to patients allergic to corn because such patients can also be allergic to hetastarch.
If hypersensitivity effect occurs, administration of the drug should be discontinued and appropriate treatment and supportive measures should be undertaken (see WARNINGS ).
When using hetastarch injection for plasma volume expansion, caution should be taken to avoid excessive hemodilution and circulatory overload especially in those patients at risk for developing congestive heart failure and pulmonary edema. Hetastarch injection is primarily excreted via the kidneys so caution should be exercised in patients who have impaired renal function. Although the risk of circulatory overload is largely dependent on the clinical circumstances, use of doses higher than 20 mL/kg/24h will increase the risk significantly. Increased risk of coagulation abnormalities and bleeding is also associated with higher doses. Patients vital signs and hemoglobin, hematocrit, platelet count, prothrombin time and partial thromboplastin time should be monitored closely.
Hetastarch injection should be used with caution in patients who have been anticoagulated with other drugs that negatively influence the coagulation system.
Regular and frequent clinical evaluation and complete blood counts (CBC) are necessary for proper monitoring of hetastarch injection use during leukapheresis. If the frequency of leukapheresis is to exceed the guidelines for whole blood donation, you may wish to consider the following additional tests: total leukocyte and platelet counts, leukocyte differential count, hemoglobin and hematocrit, prothrombin time (PT), and partial thromboplastin time (PTT).
Indirect bilirubin levels of 8.3 mg/L (normal 0.0-7.0 mg/L) have been reported in 2 out of 20 normal subjects who received multiple infusions of hetastarch injection. Total bilirubin was within normal limits at all times; indirect bilirubin retuned to normal by 96 hours following the final infusion. The significance, if any, of these elevations is not known; however, caution should be observed before administering hetastarch injection to patients with a history of liver disease.
Elevated serum amylase levels may be observed temporarily following administration of hetastarch injection, although no association with pancreatitis has been demonstrated. Serum amylase levels cannot be used to assess or to evaluate for pancreatitis for 3-5 days after administration of hetastarch injection. Elevated serum amylase levels persist for longer periods of time in patients with renal impairment. Hetastarch has not been shown to increase serum lipase.
One report suggests that in the presence of renal glomerular damage, larger molecules of hetastarch can leak into the urine and elevate the specific gravity. The elevation of specific gravity can obscure the diagnosis of renal failure.
Hetastarch is not eliminated by hemodialysis. The utility of other extracorporeal elimination techniques has not been evaluated.
The flexible plastic container has a natural gum rubber/latex-containing injection port. Unless medication addition occurs a diaphragm prevents the latex from coming in contact with the hetastarch injection solution. In patients with latex hypersensitivity, caution should be exercised when adding medication through the port of the flexible plastic container.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long –term studies of animals have not been performed to evaluate the carcinogenic potential of hetastarch.
Pregnancy Category C
Hetastarch has been shown to have an embryocidal effect on New Zealand rabbits when given intravenously over the entire organogenesis period in a daily dose 1/2 times the maximum recommended therapeutic human dose (1500 mL) and on BD rats when given intraperitoneally, from the 16th to the 21st day of pregnancy, in a daily dose 2.3 times the maximum recommended therapeutic human dose. When hetastarch was administered to New Zealand rabbits, BD rats, and Swiss mice with intravenous daily doses of 2 times, 1/3 times, and 1 time the maximum recommended therapeutic human dose respectively over several days during the period of gestation, no evidence of teratogenicity was evident. There were no adequate and well controlled studies in pregnant women. Hetastarch injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is not known whether hetastarch is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when hetastarch injection is administered to a nursing woman.
Pediatric Use
The safety and effectiveness of hetastarch in pediatric patients have not been established. Adequate, well-controlled clinical trials to establish the safety and effectiveness of hetastarch injection in pediatric patients have not been conducted. However, in one small double-blind study, 47 infants, children, and adolescents (ages 1 year to 15.5 years) scheduled for repair of congenital heart disease with moderate hypothermia were randomized to receive either hetastarch injection or Albumin as a postoperative volume expander during the first 24 hours after surgery. Thirty-eight children required colloid replacement therapy, of which 20 children received hetastarch injection. No differences were found in the coagulation parameters or in the amount of replacement fluids required in the children receiving 20 mL/kg or less of either colloid replacement therapy. In children who received greater than 20 mL/kg of hetastarch injection, an increase in prothrombin time was demonstrated (p=0.006).8 There were no neonates included in this study.
HETASTARCH ADVERSE REACTIONS
Reported adverse reactions associated with hetastarch include:
General
Hypersensitivity (see WARNINGS ).
Death, life-threatening anaphylactic/anaphylactoid reactions, cardiac arrest, ventricular fibrillation, severe hypotension, non-cardiac pulmonary edema, laryngeal edema, bronchospasm, angioedema, wheezing, restlessness, tachypnea, stridor, fever, chest pain, bradycardia, tachycardia, shortness of breath, chills, urticaria, pruritus, facial and periorbital edema, coughing, sneezing, flushing, erythema multiforme, and rash.
Cardiovascular
Circulatory overload, congestive heart failure, and pulmonary edema (see PRECAUTIONS ).
Hematologic
Intracranial bleeding, bleeding and/or anemia due to hemodilution (see WARNINGS ) and/or Factor VIII deficiency, acquired von Willebrand's-like syndrome, and coagulopathy including rare cases of disseminated intravascular coagulopathy and hemolysis.
Metabolic
Metabolic acidosis.
Other
Vomiting, peripheral edema of the lower extremities, submaxillary and parotid glandular enlargement, mild influenza-like symptoms, headaches, and muscle pains.
Hydroxyethyl starch-associated pruritus has been reported in some patients with deposits of hydroxyethyl starch in peripheral nerves.
HETASTARCH DOSAGE AND ADMINISTRATION
Dosage for Acute Use in Plasma Volume Expansion
Hetastarch injection is administered by intravenous infusion only. Total dosage and rate of infusion depend upon the amount of blood or plasma lost and the resultant hemoconcentration.
Adults: The amount usually administered is 500 to 1000 mL. Doses of more than 1500 mL per day for the typical 70 kg patient (approximately 20 mL per kg of body weight) are usually not required although higher doses have been reported in postoperative and trauma patients where severe blood loss has occurred (see WARNINGS and PRECAUTIONS ).
Pediatric patients: Adequate, well-controlled clinical trials to establish the safety and effectiveness of hetastarch injection in pediatric patients have not been conducted (see PRECAUTIONS, Pediatric Use ).
Dosage in Leukapheresis
250 to 700 mL of hetastarch injection to which citrate anticoagulant has been added is typically administered by aseptic addition to the input line of the centrifugation apparatus at a ratio of 1:8 to 1:13 to venous whole blood. The hetastarch injection and citrate should be thoroughly mixed to assure effective anticoagulation of blood as it flows through the leukapheresis machine.
When stored at room temperature, hetastarch injection admixtures of 500-560 mL with citrate concentrations up to 2.5% were compatible for 24 hours. The safety and compatibility of additives other than citrate have not been established.
General Recommendations
Do not use plastic container in series connection.
If administration is controlled by a pumping device, care must be taken to discontinue pumping action before the container runs dry or air embolism may result.
This solution is intended for intravenous administration using sterile equipment. It is recommended that intravenous administration apparatus be replaced at least once every 24 hours.
Use only if solution is clear and container and seals are intact.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
If administration is by pressure infusion, all air should be withdrawn or expelled from the bag through the medication port prior to infusion.
The safety and compatibility of other additives have not been established.
Directions for Use (Plastic Container)
Caution: Before administering to the patient, review these directions:
Visual Checking
- Do not remove the plastic infusion container from its overwrap until immediately before use.
- While the overwrap is intact, identify the solution as 6% Hetastarch in 0.9% Sodium Chloride Injection, the lot number, and the expiration date.
- Check that the solution is clear.
- Inspect the intact unit for signs of obvious damage. If present, the unit should not be used.
Removal of Overwrap
To open overwrap, tear at any notch located at either end of unit. After removing overwrap, check for any leakage by squeezing container firmly. If leaks are found, discard unit as sterility may be impaired.
Preparation for Administration (Use aseptic technique)
- Close flow control clamp of administration set.
- Twist off plug from port designated "Delivery Set Port."
- Insert spike of infusion set into port with a twisting motion until the set is firmly seated.
- Suspend container from hanger.
- Follow manufacturer's recommended procedures for the administration set.
- Discontinue administration and notify physician immediately if patient exhibits signs of adverse reactions.
HOW SUPPLIED
6% Hetastarch in 0.9% Sodium Chloride Injection is supplied sterile and nonpyrogenic in 500 mL intravenous plastic infusion containers.
| NDC 0703-5079-37 | 12-Pack | 500 mL bags |
Exposure of pharmaceutical products to heat should be minimized. Avoid excessive heat. Protect from freezing. It is recommended that the product be stored at room temperature (25ºC); however, brief exposure up to 40ºC does not adversely affect the product.
Rx only
References:
- Diehl J. et al., Clinical Comparison of Hetastarch and Albumin in Postoperative Cardiac Patients. The Annals of Thoracic Surgery, 1982;34(6):674-679.
- Gold M. et al., Comparison of Hetastarch to Albumin for Perioperative Bleeding In Patients Undergoing Abdominal Aortic Aneurysm Surgery, Annals of Surgery, 1990;211(4):482-485.
- Kiklin J. et al., Hydroxyethyl Starch versus Albumin for Colloid Infusion Following Cardiopulmonary Bypass in Patients Undergoing Myocardial Revascularization, The Annals of Thoracic Surgery, 1984;37(1):40-46.
- Moggio RA. et al., Hemodynamic Comparison of Albumin and Hydroxyethyl Starch in Postoperative Cardiac Surgery Patients, Critical Care Medicine, 1983;11(12):943-945.
- Knutson JE., et al., Does Intraoperative Hetastarch Administration Increase Blood Loss and Transfusion Requirements After Cardiac Surgery? Anesthesia Analg., 2000;90:801-7.
- Cope JT., et al., Intraoperative Hetastarch Infusion Impairs Hemostasis After Cardiac Operations. The Annals of Thoracic Surgery, 1997;63:78-83.
- Damon L., Intracranial Bleeding During Treatment with Hydroxyethyl Starch, New England Journal of Medicine, 1987;317(15):964-965.
- Brutocao D., et al., Comparison of Hetastarch with Albumin for Postoperative Volume Expansion in Children After Cardiopulmonary Bypass, Journal of Cardiothoracic and Vascular Anesthesia, 1996;10(3):348-351.
TEVA
Manufactured for Teva Parenteral Medicines Inc., Irvine, CA 92618, USA by Fresenius Kabi Norge AS, NO-1753, Halden, Norway
To report SUSPECTED ADVERSE REACTIONS contact TEVA USA, PHARMACOVIGILANCE at 1-888-838-2872 xt 6351 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Revised: October 2008
01-58-08-001-B
PRINCIPAL DISPLAY PANEL
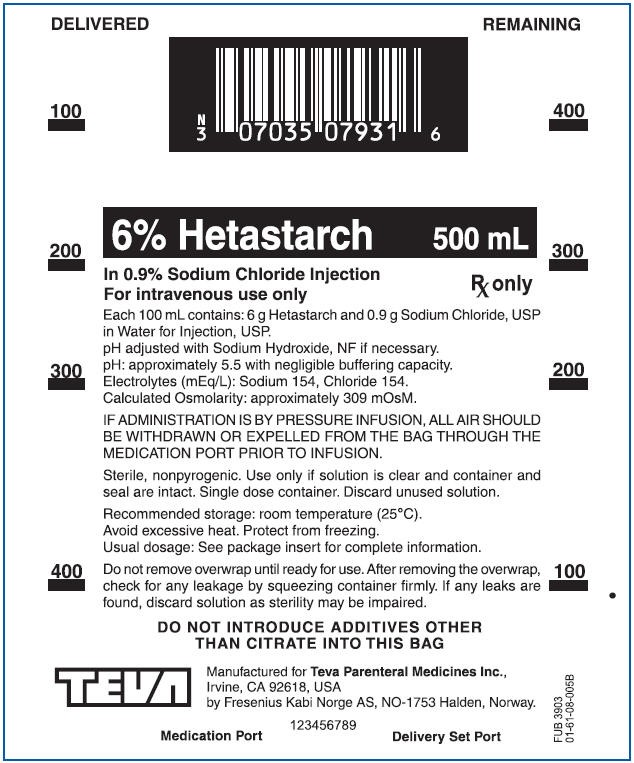
6% Hetastarch 500 mL Label Text
DELIVERED REMAINING
6% Hetastarch 500 mL
In 0.9% Sodium Chloride Injection
For intravenous use only
Rx only
Each 100 mL contains: 6 g Hetastarch and 0.9 g Sodium Chloride, USP
in Water for Injection, USP.
pH adjusted with Sodium Hydroxide, NF if necessary.
pH: approximately 5.5 with negligible buffering capacity.
Electrolytes (mEq/L): Sodium 154, Chloride 154.
Calculated Osmolarity: approximately 309 mOsM.
IF ADMINISTRATION IS BY PRESSURE INFUSION, ALL AIR SHOULD
BE WITHDRAWN OR EXPELLED FROM THE BAG THROUGH THE
MEDICATION PORT PRIOR TO INFUSION.
Sterile, nonpyrogenic. Use only if solution is clear and container and
seal are intact. Single dose container. Discard unused solution.
Recommended storage: room temperature (25°C).
Avoid excessive heat. Protect from freezing.
Usual dosage: See package insert for complete information.
Do not remove overwrap until ready for use. After removing the overwrap,
check for any leakage by squeezing container firmly. If any leaks are
found, discard solution as sterility may be impaired.
DO NOT INTRODUCE ADDITIVES OTHER
THAN CITRATE INTO THIS BAG
TEVA
Manufactured for Teva Parental Medicines Inc.,
Irvine, CA 92618, USA
by Fresenius Kabi Norge AS, NO-1753 Halden, Norway
123456789
Medication Port
Delivery Set Port
HetastarchHetastarch INJECTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||