Honey Bee hymenoptera venom Venomil Diagnostic
Jubilant HollisterStier LLC
Jubilant HollisterStier LLC
INSTRUCTIONS AND DOSAGE SCHEDULE FOR ALLERGENIC EXTRACTS HYMENOPTERA VENOM PRODUCTS (Honey Bee, Yellow Jacket, Yellow Hornet, White-Faced Hornet, Wasp, and Mixed Vespid) VENOMIL
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNINGS
- HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC DESCRIPTION
- CLINICAL PHARMACOLOGY
- HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC INDICATIONS AND USAGE
- HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC ADVERSE REACTIONS
- OVERDOSAGE
- HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- LIMITED WARRANTY
- REFERENCES
FULL PRESCRIBING INFORMATION
WARNINGS
This product is intended for use only by licensed medical personnel experienced in administering allergenic extracts and trained to provide immediate emergency treatment in the event of a life-threatening reaction.
Hymenoptera Venom extracts may potentially elicit a severe life-threatening systemic reaction, rarely resulting in death.(1) Therefore, emergency measures and personnel trained in their use must be available immediately in the event of such a reaction. Patients should be instructed to recognize adverse reaction symptoms, observed in the office for at least 30 minutes after skin testing or treatment, and cautioned to contact the physician's office if symptoms occur. See ADVERSE REACTION, Section 4, of this instruction for information regarding adverse event reporting.
All patients should have available an Emergency Anaphylaxis Kit containing epinephrine and be instructed in its use for emergency treatment of possible systemic reactions occurring at times after the patient has departed the testing or treatment premises. Patients with cardiovascular diseases and/or pulmonary diseases such as symptomatic unstable, steroid-dependent asthma, and/or those who are receiving cardiovascular drugs such as beta blockers, may be at higher risk for severe adverse reactions. These patients may also be more refractory to the normal allergy treatment regimen. Patients should be treated only if the benefit of treatment outweighs the risks.(1)
Patients on beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions.(2)
Immunotherapy for insect sting allergy should be given to those patients who have experienced significant systemic reactions (for detailed description of symptoms see INDICATIONS AND USAGE and ADVERSE REACTIONS) from insect stings and who demonstrate hypersensitivity by skin testing with these products. The only approved method for diagnosing insect sting allergic patients for immunization is by skin testing.
This product must never be injected intravenously.
Refer also to CONTRAINDICATIONS, WARNINGS, PRECAUTIONS, ADVERSE REACTIONS and OVERDOSAGE for further discussion.
HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC DESCRIPTION
Hymenoptera Venom Products available are sterile freeze-dried venom of Honey Bee (Apis mellifera) and venom protein of Yellow Jacket (Vespula sp.), Yellow Hornet (Dolichovespula arenaria), White-Faced Hornet (Dolichovespula maculata) and Wasp (Polistes sp.). Mixed Vespid venom protein (Yellow Jacket, Yellow Hornet and White-Faced Hornet) is also available.
The reconstituted single venom products are intended for subcutaneous injection for immunotherapy and percutaneous use for diagnosis. The Mixed Vespid venom protein is for immunotherapy only, not for diagnosis. Diagnosis should be based on individual venoms.
Because of the difficulty in collecting all species of Yellow Jacket and Wasp, the venom raw materials for these two insects may vary in species composition from lot to lot. A listing of the exact species content for any particular lot of Yellow Jacket or Wasp venom protein may be obtained by calling Technical Services at Jubilant HollisterStier, (800) 992-1120.
Final containers of sterile freeze-dried venom products are sealed under vacuum. This will result in the diluting fluid being forcibly drawn into the sealed vial when the syringe needle penetrates the seal during reconstitution. See PRECAUTIONS.
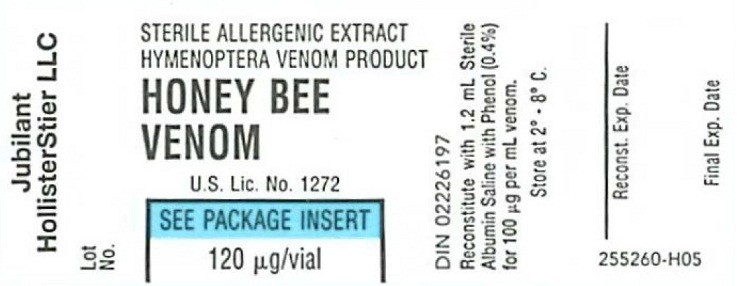
Venom or venom protein is supplied in 2 mL diagnostic vials and in 2 mL vials for treatment maintenance. The chart below lists for each vial size the content of lyophilized venom or venom protein and reconstituted product, (mannitol and venom concentrations). Trace amounts of sodium chloride, potassium chloride, acetic acid and beta-alanine, as well as the constituents of the reconstituting fluid, will also be present.
|
|
Vial Size |
µg Venom or Venom Protein |
Reconstitution | mg/mL Mannitol | Venom Concentration |
| Single Venom |
2 mL |
120 |
1.2 mL |
7.7 mg/mL |
100µg/mL |
| Mixed Vespid |
2 mL |
360 |
1.2 mL |
23.1 mg/mL |
300 µg/mL |
DOSAGE AND ADMINISTRATION
PRECAUTIONS
CLINICAL PHARMACOLOGY
DiagnosisTreatment
(3, 4)
(3, 4)
(4)(5)(3, 4)
DOSAGE AND ADMINISTRATION)(4)
(4)(4)
(4)(4)
DOSAGE AND ADMINISTRATION)(4)
(4)
HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC INDICATIONS AND USAGE
Insect stings may induce a wide range of allergic symptoms in sensitive patients. A normal sting response is initial burning or stinging pain that may be intense and last several minutes to an hour or more. There is usually some local swelling coming on immediately and persisting for several days. The location of the sting has considerable influence on the intensity of the pain and extent of swelling. Stings on the fingers or feet produce much pain, but less swelling; whereas a sting on the head or face produces extensive swelling with variable pain.
Local reactions coming on rapidly and larger than the usual local reaction, particularly if the swelling spans both adjacent joints on the extremities, can indicate hypersensitivity. Systemic symptoms come on shortly after the sting, often within seconds to minutes. Symptoms may range from generalized flushing, itching, redness, diffuse swelling of the skin or urticarial wheals, abdominal cramps, nausea, vomiting, or incontinence of urine or stool, to faintness, blurring or loss of vision, unconsciousness, seizures, respiratory or cardiac arrest, or death. Later reactions may consist of fever, achiness, malaise, joint swelling, urticaria or other signs of vascular damage typical of serum sickness, a Type III reaction. Typical delayed Type IV reactions may also occur.(6) Rarely, other types of severe reactions to insect stings have been reported.(6)These include serum sickness, hematologic abnormalities, and neurological disorders commencing some time after a sting, and not associated with anaphylactoid reactions. These patients are not candidates for immunotherapy using insect venoms.
(1) Diagnosis
Skin testing with insect venoms is useful to demonstrate the presence of IgE antibodies which account for the patient's symptoms.(3)Patients are seldom able to identify the insect which stung them, so skin testing is used to determine the insect culprit. Dilutions of these venom products will help judge the sensitivity of the patient and whether the patient should be treated.(7)
It is not absolutely known what levels (micrograms) of venom, that elicit positive skin tests, are diagnostic of clinical sensitivity. However, patients with a history of reactions (any of three types: generalized urticaria or angioedema; respiratory difficulty due either to laryngeal edema or to bronchospasm; or vascular collapse, with or without loss of consciousness) to previous stings and a positive skin test to a venom intradermal injection of approximately 1 µg/mL had about a 60% chance of reacting again when stung by the same insect. These patients should receive venom immunotherapy.(3)
Patients with a history of reaction (any of the three reaction types described above) to previous stings, but who did not demonstrate a positive skin test reaction to venom, were considered in a previous study not to be clinically sensitive, and were not treated.(3) We cannot recommend treatment for such patients.
Another study demonstrated false positive reactions when skin testing with venom concentrations of 10 µg/mL and 100 µg/mL was carried out.(8) Thus there can be a nonspecific skin test reaction potentially due to the pharmacological action of the venom at higher concentrations.
The best statement that can be made, at present, is that patients with significant positive history (reactions of the three types described above) following an insect sting, and who do react with a positive skin test to a venom concentration of 1 µg/mL or less, are recommended for treatment. Patients who have the history described above, but who do not react to a 1 µg/mL intradermal venom skin test, cannot be recommended for treatment. At present, the data does not exist, to determine whether a patient who might react to a higher concentration, e.g., 2-10 µg/mL, is at risk from a subsequent sting or not. Since it is not known if sting-sensitive patients who subsequently lose their IgE anti-venom antibody can be resensitized by further stings, it is advisable to retest these patients after any subsequent stings.(3) However, since the level of venom-specific IgE may fall to low levels briefly after a sting, patients should not be re-tested until 2 to 4 weeks after any sting.
(2) Treatment
Immunotherapy is indicated for those patients diagnosed as sensitive (see Diagnosis above) and is accomplished by using graduated dilutions of the appropriate insect venom or venoms to control the severity of the patient's symptoms from subsequent stings.
Increasing doses of venom are given at intervals, dependent on the patient's ability to tolerate the venoms, until a maintenance dosage (100 µg per venom is recommended - 300 µg in the case of the Mixed Vespid venom protein) is reached and maintained.
Venom sensitivity differs for individual patients, thus it is not possible to provide a dosage schedule that is universally suited to all patients. The dosage schedule shown under DOSAGE AND ADMINISTRATION is a summary of the schedule used in clinical trials of our product and found suitable for the majority of patients.
In highly sensitive patients, the physician may be required to use a modified dose schedule, based on the patient's sensitivity to and tolerance of the injections. Lower initial doses and smaller dosage increments than shown under DOSAGE AND ADMINISTRATION may be necessary.
HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC CONTRAINDICATIONS
There are no known absolute contraindications to immunotherapy using Hymenoptera Venom Products. See also PRECAUTIONS and WARNINGS.
Patients showing negative intradermal skin tests to specific venoms at 1 µg/mL are not recommended for venom treatment.
Any injections, including immunotherapy, should be avoided in patients with a bleeding tendency. Patients with cardiovascular diseases and/or pulmonary diseases such as symptomatic unstable, steroid-dependent asthma, and/or those who are receiving cardiovascular drugs such as beta blockers, may be at higher risk for severe adverse reactions. These patients may also be more refractory to the normal allergy treatment regimen. Patients should be treated only if the benefit of treatment outweighs the risks.(1)
Patients on beta blockers may be more reactive to allergens given for testing or treatment and maybe unresponsive to the usual doses of epinephrine used to treat systemic reactions.(2)
Since there are differences of opinion concerning the possibility of routine immunizations exacerbating autoimmune diseases, immunotherapy should be given cautiously to patients with other immunologic diseases and only if the risk from insect stings is greater than the risk of exacerbating the underlying disorder.
WARNINGS
WARNINGSPRECAUTIONS(9)(10)
(11)INDICATIONS AND USAGEADVERSE REACTIONS.PRECAUTIONSADVERSE REACTIONS
PRECAUTIONS
1. GENERAL
The presence of asthmatic signs and symptoms appear to be an indicator for severe reactions following allergy injections. An assessment of airway obstruction either by measurement of peak flow or an alternate procedure may provide a useful indicator as to the advisability of administering an allergy injection. (1, 12-16)
Concentrated extracts must not be injected unless tolerance has been established.
Diluting fluid should be forcibly drawn into the sealed vial when the syringe needle penetrates the seal during reconstitution. Failure of this to occur for a particular vial indicates possible loss of vacuum. Vials without vacuum should be returned to the manufacturer.
Record date of reconstitution and expiration date of reconstituted product in the space provided on the product label. Date of expiration after reconstitution must not exceed the Final Expiration Date indicated on the container label. (See table below for expiration dates, including dilutions).
Store freeze-dried and reconstituted venom product, stock solutions and venom dilutions constantly at 2 - 8 C.
| Venom Concentration |
Diluent |
Recommended Expiration Date* |
| 100 µg/mL |
Albumin Saline with Phenol (0.4%) |
6 Months |
| 10µg/mL |
Albumin Saline with Phenol (0.4%) |
1 month |
| 1 µg/mL |
Albumin Saline with Phenol (0.4%) |
1 month |
| 0.1 µg/mL |
Albumin Saline with Phenol (0.4%) |
14 days |
| Less than 0.1 µg/mL |
Albumin Saline with Phenol (0.4%) |
Prepare fresh daily |
*But not to exceed Final Expiration Date indicated on the container label.
Sterile solutions, vials, syringes, etc., should be used and aseptic precautions observed in making dilutions.
To avoid cross-contamination, do not use the same needle to withdraw materials from vials of more than one extract, or extract followed by diluent.
A sterile tuberculin syringe, with a needle at least 5/8" long and graduated in 0.01 mL units, should be used to measure carefully each dose from the appropriate dilution. Aseptic techniques should always be employed when injections are being administered.
A separate sterile syringe should be used for each patient to prevent transmission of hepatitis and other infectious agents from one person to another.
Patient reactions to previous injections should be reviewed before each new injection so that dose can be adjusted accordingly. See ADVERSE REACTIONS and WARNINGS.
Rarely, a patient is encountered who develops systemic reactions to minute doses of allergen and does not demonstrate increasing tolerance to injections after several months of treatment. It is suggested that if systemic reactions or excessive local responses occur persistently at very small doses, efforts at immunotherapy should be stopped.
PATIENTS SHOULD BE OBSERVED IN THE OFFICE FOR AT LEAST 30 MINUTES AFTER SKIN TESTING AND AFTER EACH TREATMENT INJECTION. Most severe reactions will occur within this time period, and rapid treatment measures should be instituted. See ADVERSE REACTIONS for such treatment measures.
2. INFORMATION FOR PATIENTS
Patients should be instructed in the recognition of adverse reactions to immunotherapy, and in particular, to the symptoms of shock. (See WARNINGS box at the beginning of this Instruction Sheet). Patients should be made to understand the importance of a 30 minute observation period following skin testing or therapeutic injections, and be cautioned to return to the office promptly if symptoms occur after leaving. Patients should be instructed in the use of, and have available, an Emergency Anaphylaxis Kit for self-administration of epinephrine.
Patients must be instructed to report any insect stings that have occurred, since a venom injection should not be given on the same day as the sting, nor during a time when the patient is still experiencing symptoms from the sting.
3. DRUG INTERACTIONS
Patients with cardiovascular diseases and/or pulmonary diseases such as symptomatic, unstable, steroid-dependent asthma, and/or those who are receiving cardiovascular drugs such as beta blockers, may be at higher risk for severe adverse reactions. These patients may also be more refractory to the normal allergy treatment regimen. Patients should be treated only if the benefit of treatment outweighs the risks.(1)
Patients on beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions.
See WARNINGS section regarding concurrent treatment with ACE inhibitors.
Certain medications may lessen the skin test wheal and erythema responses elicited by allergens and histamine for varying time periods. Conventional antihistamines should be discontinued at least 5 days before skin testing. Long acting antihistamines should be discontinued for at least 3 weeks prior to skin testing.(17) Topical steroids should be discontinued at the skin test site for at least 2-3 weeks before skin testing.(17, 18)
Tricyclic antidepressants such as doxepin, should be withheld for at least 7 days before skin testing.(19) Topical local anesthetics may suppress the flare responses and should be avoided on skin test sites.(20)
When using other drugs in patients receiving allergenic extracts, always consult the product labeling of the other drugs to determine any possible interaction with use of allergenic extracts, and specifically with stinging insect (Hymenoptera) venom extracts.
4. CARCINOGENESIS AND MUTAGENSIS AND IMPAIRMENT OF FERTILITY
Long-term studies in animals have not been conducted with allergenic extracts to determine their potential for carcinogenicity, mutagenicity, or impairment of fertility.
5. PREGNANCY
(12, 21)6. NURSING MOTHERS
There are no current studies on secretion of the allergenic extract components in human milk or effect on the nursing infant. Because many drugs are excreted in human milk, caution should be exercised when allergenic extracts are administered to a nursing woman.
7. PEDIATRIC USE
Since dosage for the pediatric population is the same as for adults, the larger volumes of solution may produce excessive discomfort. Therefore, in order to achieve the total dose required, the volume of the dose may need to be divided into more than one injection per visit. A study done in children ages 4 to 17 showed no special problems with venom immunotherapy in this population.(22)
8. GERIATRIC USE
The reactions from immunotherapy can be expected to be the same in elderly patients as in younger ones. Elderly patients may be more likely to be on medication that could block the effect of epinephrine which could be used to treat serious reactions, or they could be more sensitive to the cardiovascular side effect of epinephrine because of pre-existing cardiovascular disease.(23)
HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC ADVERSE REACTIONS
WARNINGS(1) Local Reactions
4
CLINICAL PHARMACOLOGYDOSAGE AND ADMINISTRATION
WARNINGSPRECAUTIONS
(2) Systemic Reactions
INDICATIONS AND USAGE
CLINICAL PHARMACOLOGY
If a systemic or anaphylactic reaction does occur, inject 1:1000 epinephrine-hydrochloride intramuscularly or subcutaneously.
WARNINGSPRECAUTIONSDOSAGE AND ADMINISTRATION
3. Adverse Event Reporting
OVERDOSAGE
See ADVERSE REACTIONS Section.
HONEY BEE HYMENOPTERA VENOM VENOMIL DIAGNOSTIC DOSAGE AND ADMINISTRATION
(1) General
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Reconstitute and dilute the freeze-dried venom as directed below. Sterile Albumin Saline with Phenol (0.4%) must be used to reconstitute and dilute the venoms for skin testing and treatment.
Reconstitute the freeze-dried venoms by adding 1.2 mL Sterile Albumin Saline with Phenol (0.4%) to the vial using a sterile syringe. Swirl or rock the container to dissolve the venom completely. DO NOT SHAKE, since shaking can cause foaming.
Dilutions (see table below) must be made in Sterile Albumin Saline with Phenol (0.4%). They must be made accurately and aseptically, using sterile solutions, vials, syringes, etc., and thoroughly mixed by rocking or swirling. DO NOT SHAKE. Maintain stock solutions and dilutions constantly at 2° - 8°C.
| Extract of Volume | Extract Concentration |
|
Diluent Volume |
|
Dilution Concentration |
| 1 part of |
100 µg/mL |
+ |
9 parts |
= |
10 µg/mL |
| 1 part of |
10 µg/mL |
+ |
9 parts |
= |
1 µg/mL |
| 1 part of |
1µg/mL |
+ |
9 parts |
= |
0.1µg/mL |
| 1 part of |
0.1 µg/mL |
+ |
9 parts |
= |
0.01 µg/mL |
| 1 part of |
0.01 µg/mL |
+ |
9 parts |
= |
0.001 µg/mL |
| 1 part of |
0.001 µg/mL |
+ |
9 parts |
= |
0.0001 µg/mL |
| Extract of Volume | Extract Concentration |
|
Diluent Volume |
|
Dilution Concentration |
| 0.2mL of |
100 µg/mL |
+ |
1.8mL |
= |
10 µg/mL |
| 0.2mL of |
10 µg/mL |
+ |
1.8mL |
= |
1 µg/mL |
| 0.2mL of |
1 µg/mL |
+ |
1.8mL |
= |
0.1 µg/mL |
| 0.2mL of |
0.1 µg/mL |
+ |
1.8mL |
= |
0.01 µg/mL |
| 0.2mL of |
0.01 µg/mL |
+ |
1.8mL |
= |
0.001 µg/mL |
| 0.2mL of |
0.001 µg/mL |
+ |
1.8mL |
= |
0.0001 µg/mL |
USE OF VENOMIL DIAGNOSTIC SETS
WARNINGSPRECAUTIONSCONTRAINDICATIONSADVERSE REACTIONS
At this point, you have completed the reconstitution of the freeze-dried venom. The reconstituted products contain 100 µg of venom or venom protein per mL. DO NOT USE THIS STRENGTH FOR INTRADERMAL SKIN TESTING. DISCARD AFTER THE DILUTIONS HAVE BEEN PREPARED.
(2) Diagnosis
may(4)
beforeDOSAGE AND ADMINISTRATION
both
Prick Tests
Intradermal Tests:
(8)
(3) Immunotherapy
WARNINGSPRECAUTIONSADVERSE REACTIONS
CAUTION
(4)
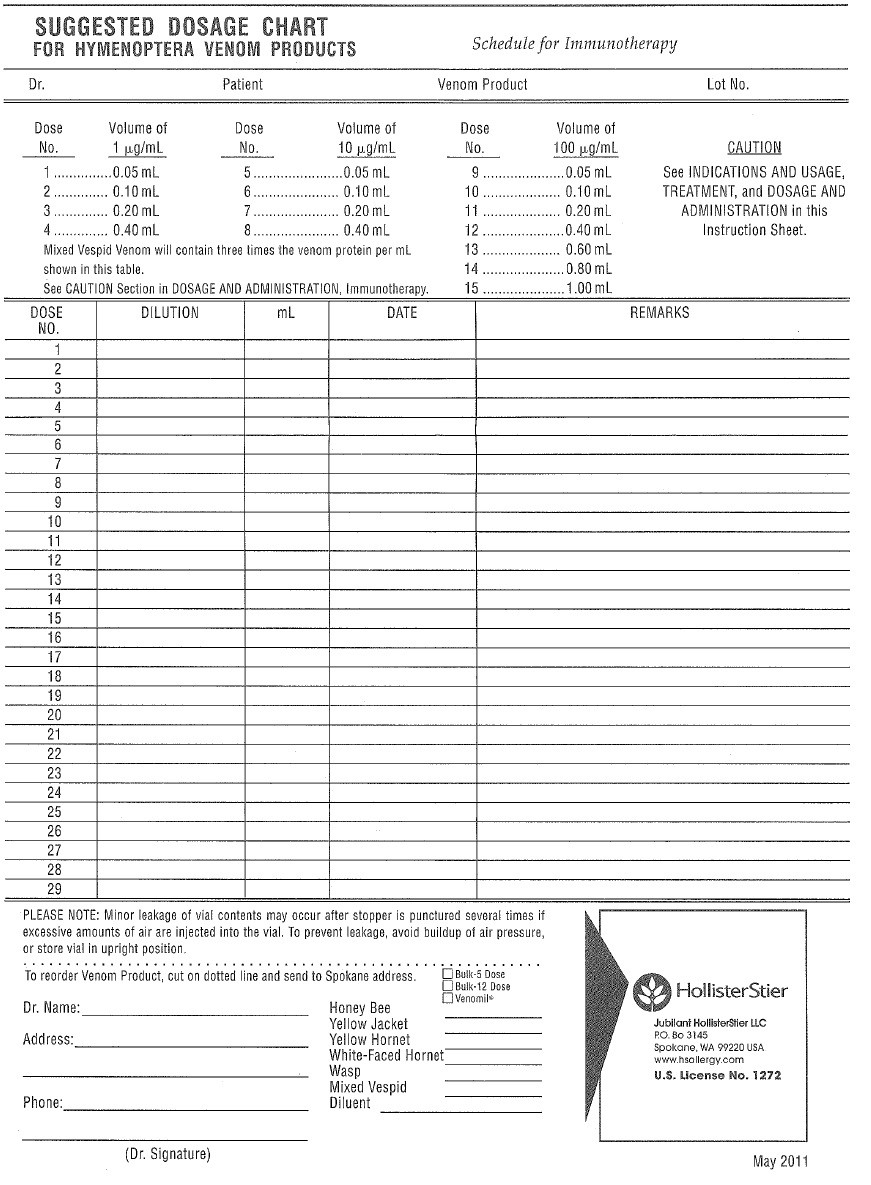
Suggested Dose Schedule for a Single Venom:
| Dose No. | *Volume of 1 µg/mL | Dose No. | Volume of 10 µg/mL | Dose No. | Volume of 100 µg/mL |
| 1..... | ...0.05 mL | 5..... | ...0.05 mL | 9..... | ...0.05mL |
| 2..... | ...0.10 mL | 6..... | ...0.10 mL | 10.... | ...0.10mL |
| 3..... | ...0.20 mL | 7..... | ...0.20 mL | 11.... | ...0.20mL |
| 4..... | ...0.40 mL | 8..... | ...0.40 mL | 12.... | ...0.40mL |
| 13.... | ...0.60mL | ||||
| 14.... | ...0.80mL | ||||
| 15.... | ...1.00mL |
CLINICAL PHARMACOLOGYINDICATIONS AND USAGE
(4)
CLINICAL PHARMACOLOGYINDICATIONS AND USAGE
PEDIATRIC USE
The dose for the pediatric population is the same as for adults. (See PRECAUTIONS).
GERIATRIC USE
The dose for elderly patients is the same as for adult patients under 65.(23) (See PRECAUTIONS).
HOW SUPPLIED
DESCRIPTIONStorage:
Store freeze-dried and reconstituted venom product, and venom dilutions, at 2° - 8° C, and keep at this temperature range during office use.
LIMITED WARRANTY
REFERENCES
1. Lockey, Richard F., Linda M. Benedict, Paul C. Turkeltaub, Samuel C. Bukantz. Fatalities from immunotherapy (IT) and skin testing (ST). J. Allergy Clin. Immunol. 79 (4): 660-677, 1987.
2. Jacobs, Robert L., Goeffrey W. Rake, Jr., et. al. Potentiated anaphylaxis in patients with drug-induced beta-adrenergic blockade. J. Allergy Clin. Immunol. 68 (2): 125-127, August 1981.
3. Hunt, K. J., M. D. Valentine, A. K. Sobotka, A. W. Benton, F. J. Amodio, L. M. Lichtenstein. A controlled trial of immunotherapy in insect hypersensitivity. New Eng. J. Med. 299: 157-161, July 27, 1978.
4. Summary of data from BB-IND 1292 clinical studies, 1978-79, on Hollister-Stier products.
5. Amodio, F., L. Markley, M. D. Valentine, A. K. Sobotka, L. M. Lichtenstein. Maintenance immunotherapy for Hymenoptera sensitivity. J. Allergy Clin. Immunol. 61 (3): 134, 1978.
6. Reisman, R. E., Allergy Principles and Practice. E. Middleton, C. E. Reed, E. F. Ellis, ed. C. V. Mosby Co., 1978.
7. Sobotka, A. K., N. F. Adkinson, Jr., M. D. Valentine, L. M. Lichtenstein. Allergy to insect stings. IV. Diagnosis by R.A.S.T. J. Immunol. 121 (6): 2477-2484, 1978.
8. Hunt, K. J., M. D. Valentine, A. K. Sobotka, L. M. Lichtenstein. Diagnosis of allergy to stinging insects by skin testing with Hymenoptera venoms. Annals Int. Med. 85: 56-59, 1976.
9. Annals of Allergy, Asthma and Immunology. Inhibitors of angiotensin II: Potential hazards for patients at risk for anaphylaxis. Editorial. 78: 527-529, June 1997.
10. Pharm. Ind. (Germany). Anaphylactoid reactions in patients treated with ACE inhibitor treatment in combination with desensitization treatment or after insect bites. 56 (9): IX226-227, 1994.
11. Tunon-De-Lara, J. M., et al. ACE inhibitors and anaphylactoid reactions during venom immunotherapy. The Lancet (United Kingdom). 340 (8824): 908, Oct. 10, 1992.
12. Weinstien, A. M., B. D. Dubin, W. K. Podleski, S. L. Spector, R. S. Farr. Asthma and pregnancy. JAMA. 124 (11): 1161-1165, 1979.
13. Reid, M. J., R. F. Lockey, P. C. Turkletaub, T. A. E. Platts-Mills. Survey of fatalities from skin testing and immunotherapy. J. Allergy Clin. Immunol. 92 (1): 6-15, July 1993.
14. Reid, M. J., G. Gurka. Deaths associated with skin testing and immunotherapy. J. Allergy Clin. Immunol. 97 (1) Part 3:231, Abstract 195, January 1996.
15. Thompson, R. A. et al. Report of a WHO/IUIS working group. The current status of allergen immunotherapy (hyposensitization). Allergy. 44: 369-379, 1989.
16. Malling, H.J., B. Weeke, et al. The European Academy of Allergology and Clinical Immunology. Position Papers. Allergy. 48 (Supplement 14): 9-82, 1993.
17. Pipkorn, Ulf. Pharmacological influence of anti-allergic medication on In Vivo allergen testing. Allergy. 43: 81-86, 1988.
18. Andersson, M. U. Pipkorn. Inhibition of the dermal immediate allergic reaction through prolonged treatment with topical glucocorticosteroids. J. Allergy Clin. Immunol. 79 (2): 345-349, February 1987.
19. Rao, Kamineni S., et al. Duration of suppressive effect of tricyclic anti-depressants on histamine induced wheal and flare reactions on human skin. J. Allergy Clin. Immunol. 82: 752-757, November 1988.
20. Pipkorn, Ulf, M. Andersson. Topical dermal anesthesia inhibits the flare but not the wheal response to allergen and histamine in the skin prick test. Clinical Allergy. 17: 307-311, 1987.
21. DuBuske, L. M., C. J. Ling, A. L. Sheffer. Special problems regarding allergy immunotherapy. Immunol. Allergy Clin. North Am. (USA). 12 (1): 145-175, 1992.
22. Graft, D., K. Schuberth, A. Kagey-Sobotka, K. Kwiterovich, Y. Niv, L. Lichtenstein, M. Valentine. Assessment of prolonged venom immunotherapy in children. J. Allergy Clin. Immunol. 80 (2): 162-169, August 1987.
23. Peebles, Ray Stokes, Jr., B. Bochner, Howard J. Zeitz, ed. Anaphylaxis in the elderly. Immunol. Allergy Clin. of North Am. 13 (3): 627-646, August 1993.
Honey Bee hymenoptera venom Venomil DiagnosticHoney Bee hymenoptera venom Venomil Diagnostic KIT
| ||||||||||||||||||||||||||||||||||||||||
Honey Bee hymenoptera venom Venomil MaintenanceHoney Bee hymenoptera venom Venomil Maintenance KIT
| ||||||||||||||||||||||||||||||||||||||||
White Faced Hornet hymenoptera venom Venomil DiagnosticWhite Faced Hornet hymenoptera venom Venomil Diagnostic KIT
| ||||||||||||||||||||||||||||||||||||||||
White Faced Hornet hymenoptera venom Venomil MaintenanceWhite Faced Hornet hymenoptera venom Venomil Maintenance KIT
| ||||||||||||||||||||||||||||||||||||||||
Yellow Hornet hymenoptera venom Venomil DiagnosticYellow Hornet hymenoptera venom Venomil Diagnostic KIT
| ||||||||||||||||||||||||||||||||||||||||
Yellow Hornet hymenoptera venom Venomil MaintenanceYellow Hornet hymenoptera venom Venomil Maintenance KIT
| ||||||||||||||||||||||||||||||||||||||||
Wasp hymenoptera venom Venomil DiagnosticWasp hymenoptera venom Venomil Diagnostic KIT
| ||||||||||||||||||||||||||||||||||||||||
Wasp hymenoptera venom Venomil MaintenanceWasp hymenoptera venom Venomil Maintenance KIT
| ||||||||||||||||||||||||||||||||||||||||
Yellow Jacket hymenoptera venom Venomil DiagnosticYellow Jacket hymenoptera venom Venomil Diagnostic KIT
| ||||||||||||||||||||||||||||||||||||||||
Yellow Jacket hymenoptera venom Venomil MaintenanceYellow Jacket hymenoptera venom Venomil Maintenance KIT
| ||||||||||||||||||||||||||||||||||||||||
Mixed Vespid hymenoptera venom Venomil MaintenanceMixed Vespid hymenoptera venom Venomil Maintenance KIT
| ||||||||||||||||||||||||||||||||||||||||