Hydromorphone Hydrochloride
HIGHLIGHTS OF PRESCRIBING INFORMATION BOXED WARNING WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION ; and NEONATAL OPIOID WITHDRAWAL SYNDROME See full prescribing information for complete boxed warning . Hydromorphone hydrochloride extended-release tablets expose users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient’s risk before prescribing, and monitor regularly for development of these behaviors or conditions. (5.1) Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Instruct patients to swallow hydromorphone hydrochloride extended-release tablets whole to avoid exposure to a potentially fatal dose of hydromorphone. (5.2) Accidental ingestion of hydromorphone hydrochloride extended-release tablets, especially in children, can result in fatal overdose of hydromorphone. (5.2) Prolonged use of hydromorphone hydrochloride extended-release tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available (5.3). RECENT MAJOR CHANGESBoxed Warning 04/2014Indications and Usage (1) 04/2014Dosage and Administration (2) 04/2014Warnings and Precautions (5) 04/2014INDICATIONS AND USAGEHydromorphone hydrochloride extended-release tablets are opioid agonists indicated in opioid-tolerant patients for the management of pain severe enough to require daily, around-the clock, long-term opioid treatment and for which alternative treatment options are inadequate.Patients considered opioid tolerant are those who are taking, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day or an equianalgesic dose of another opioid. Limitations of Use Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death with extended-release opioid formulations, reserve hydromorphone hydrochloride extended-release tablets for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain. Hydromorphone hydrochloride extended-release tablets are not indicated as an as-needed (prn) analgesic. DOSAGE AND ADMINISTRATION For once daily administration (2.1) Instruct patients to swallow hydromorphone hydrochloride extended-release tablets intact. (2.6) Do not abruptly discontinue hydromorphone hydrochloride extended-release tablets. (2.3, 5.12) To convert to hydromorphone hydrochloride extended-release tablets from another opioid, use available conversion factors to obtain estimated dose. (2.1) Dose may be increased using increments of 4-8 mg every 3 to 4 days as needed to achieve adequate analgesia. (2.2) DOSAGE FORMS AND STRENGTHSExtended-release tablets: 8 mg, 12 mg, 16 mg (3)CONTRAINDICATIONS Opioid non-tolerant patients (4) Significant respiratory depression (4) Acute or severe bronchial asthma (4) Known or suspected paralytic ileus (4) Narrowed or obstructed gastrointestinal tract (4) Known hypersensitivity to any components including hydromorphone hydrochloride and sulfites (4, 5.10) WARNINGS AND PRECAUTIONS Interactions with CNS depressants: Concomitant use may cause profound sedation, respiratory depression, and death. If coadministration is required, consider dose reduction of one or both drugs because of additive pharmacological effects.(5.4) Elderly, cachectic, debilitated patients and those with chronic pulmonary disease: Monitor closely because of increased risk for life-threatening respiratory depression. (5.5, 5.6) Hypotensive effect: Monitor during dose initiation and titration (5.7) Patients with head injury or increased intracranial pressure: Monitor for sedation and respiratory depression. Avoid use of hydromorphone hydrochloride in patients with impaired consciousness or coma susceptible to intracranial effects of CO2 retention. (5.8) Side EffectsMost common adverse reactions (>10%) are: constipation, nausea, vomiting, somnolence, headache, and dizziness (6.1). To report SUSPECTED ADVERSE REACTIONS, contact Watson Laboratories, Inc. at 1-800-272-5525 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Mixed agonist/antagonist and partial agonist opioid analgesics: Avoid use with hydromorphone hydrochloride because they may reduce analgesic effect of hydromorphone hydrochloride or precipitate withdrawal symptoms. (5.12, 7.2) Monoamine oxidase inhibitors (MAOIs): Avoid use of hydromorphone hydrochloride in patients taking MAOIs or within 14 days of stopping such treatment. (7.3) USE IN SPECIFIC POPULATIONS Pregnancy: Hydromorphone hydrochloride is not recommended. Based on animal data, may cause fetal harm. (8.1) Nursing mothers: Hydromorphone hydrochloride is not recommended. Hydromorphone has been detected in human milk. Closely monitor infants of nursing women receiving hydromorphone hydrochloride. (8.3) Hepatic or renal impairment: Administer a reduced dose of hydromorphone hydrochloride in patients with moderate hepatic (8.7) and moderate renal impairment (8.8). Consider use of an alternate analgesic in patients with severe hepatic (8.6) and renal impairment. (8.7)
FULL PRESCRIBING INFORMATION: CONTENTS*
FULL PRESCRIBING INFORMATION
Addiction, Abuse, and Misuse
Hydromorphone hydrochloride extended-release tablets expose patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient’s risk prior to prescribing hydromorphone hydrochloride extended-release tablets, and monitor all patients regularly for the development of these behaviors or conditions [see Warnings and Precautions (5.1)].
Life-threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression may occur with use of hydromorphone hydrochloride extended-release tablets. Monitor for respiratory depression, especially during initiation of hydromorphone hydrochloride extended-release tablets or following a dose increase. Instruct patients to swallow hydromorphone hydrochloride extended-release tablets whole; crushing, chewing, or dissolving hydromorphone hydrochloride extended-release tablets can cause rapid release and absorption of a potentially fatal dose of hydromorphone [see Warnings and Precautions (5.2)].
Accidental Ingestion
Accidental ingestion of even one dose of hydromorphone hydrochloride extended-release tablets, especially by children, can result in a fatal overdose of hydromorphone [see Warnings and Precautions (5.2)].
Neonatal Opioid Withdrawal Syndrome
Prolonged use of hydromorphone hydrochloride extended-release tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Warnings and Precautions (5.3)].
RECENT MAJOR CHANGES
Hydromorphone hydrochloride extended-release tablets are indicated for the management of pain in opioid-tolerant patients severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
Patients considered opioid tolerant are those who are receiving, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day or an equianalgesic dose of another opioid.
Limitations of Use
- Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death with extended-release opioid formulations, reserve hydromorphone hydrochloride extended-release tablets for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain.
- Hydromorphone hydrochloride extended-release tablets are not indicated as an as-needed (prn) analgesic.
To avoid medication errors, prescribers and pharmacists must be aware that hydromorphone is available as both immediate-release 8 mg tablets and extended-release 8 mg tablets.
Hydromorphone hydrochloride extended-release tablets should be prescribed only by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain.
Due to the risk of respiratory depression, hydromorphone hydrochloride extended-release tablets are only indicated for use in patients who are already opioid-tolerant. Discontinue or taper all other extended-release opioids when beginning hydromorphone hydrochloride extended-release tablets therapy. As hydromorphone hydrochloride extended-release tablets are only for use in opioid-tolerant patients, do not begin any patient on hydromorphone hydrochloride extended-release tablets as the first opioid.
Patients considered opioid-tolerant are those who are taking at least 60 mg of morphine daily, or at least 30 mg of oral oxycodone daily, or at least 8 mg of oral hydromorphone daily or an equianalgesic dose of another opioid for a week or longer.
Initiate the dosing regimen for each patient individually, taking into account the patient"s prior analgesic treatment experience and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.1)]. Monitor patients closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy with hydromorphone hydrochloride extended-release tablets [see Warnings and Precautions (5.2)].
Hydromorphone hydrochloride extended-release tablets must be taken whole. Crushing, chewing, or dissolving hydromorphone hydrochloride extended-release tablets will result in uncontrolled delivery of hydromorphone and can lead to overdose or death [see Warnings and Precautions (5.2)].
Conversion from Other Oral Hydromorphone Formulations to Hydromorphone Hydrochloride Extended-release Tablets
Patients receiving oral immediate-release hydromorphone may be converted to hydromorphone hydrochloride extended-release tablets by administering a starting dose equivalent to the patient’s total daily oral hydromorphone dose, taken once daily.
Conversion from Other Oral Opioids to Hydromorphone Hydrochloride Extended-release Tabelts
Discontinue all other around-the-clock opioid drugs when hydromorphone hydrochloride extended-release tablets therapy is initiated.
While there are useful tables of opioid equivalents readily available, there is substantial inter-patient variability in the relative potency of different opioid drugs and products. As such, it is safer to underestimate a patient’s 24-hour oral hydromorphone requirements and provide rescue medication (e.g., immediate-release opioid) than to overestimate the 24-hour oral hydromorphone requirements, which could result in adverse reactions.
In a hydromorphone hydrochloride extended-release tablets clinical trial with an open-label titration period, patients were converted from their prior opioid to hydromorphone hydrochloride extended-release tablets using the Table 1 as a guide for the initial hydromorphone hydrochloride extended-release tablets dose. The recommended starting dose of hydromorphone hydrochloride extended-release tablets is 50% of the calculated estimate of daily hydromorphone requirement. Calculate the estimated daily hydromorphone requirement using Table 1.
Consider the following when using the information in Table 1:
- This is not a table of equianalgesic doses.
- The conversion factors in this table are only for the conversion from one of the listed oral opioid analgesics to hydromorphone hydrochloride extended-release tablets.
- The table cannot be used to convert from hydromorphone hydrochloride extended-release tablets to another opioid. Doing so will result in an overestimation of the dose of the new opioid and may result in fatal overdose.
|
Prior Oral Opioid |
Approximate Oral |
|
H y dromorphone |
1 |
|
Codeine |
0.06 |
|
H y drocodone |
0.4 |
|
Methadone |
0.6 |
|
Morphine |
0.2 |
|
Oxycodone |
0.4 |
|
Oxymorphone |
0.6 |
To calculate the estimated hydromorphone hydrochloride extended-release tablets dose using Table 1:
- For patients on a single opioid, sum the current total daily dose of the opioid and then multiply the total daily dose by the conversion factor to calculate the approximate oral hydromorphone daily dose.
- For patients on a regimen of more than one opioid, calculate the approximate oral hydromorphone dose for each opioid and sum the totals to obtain the approximate total hydromorphone daily dose.
- For patients on a regimen of fixed-ratio opioid/non-opioid analgesic products, use only the opioid component of these products in the conversion.
Always round the dose down, if necessary, to the appropriate hydromorphone hydrochloride extended-release tablets strength(s) available. Example conversion from a single opioid to hydromorphone hydrochloride extended-release tablets:
Step 1: Sum the total daily dose of the opioid
- 30 mg of oxycodone 2 times daily = 60 mg total daily dose of oxycodone
Step 2: Calculate the approximate equivalent dose of oral hydromorphone based on the total daily dose of the current opioid using Table 1
- 60 mg total daily dose of oxycodone x Conversion Factor of 0.4 = 24 mg of oral hydromorphone daily
Step 3: Calculate the approximate starting dose of hydromorphone hydrochloride extended-release tablets to be given every 24 hours, which is 50% of the calculated oral hydromorphone dose. Round down, if necessary, to the appropriate hydromorphone hydrochloride extended-release tablet strengths available.
- 50% of 24 mg results in an initial dose of 12 mg of hydromorphone hydrochloride extended-release tablets once daily
- Adjust individually for each patient
Close observation and frequent titration are warranted until pain management is stable on the new opioid. Monitor patients for signs and symptoms of opioid withdrawal or for signs of over-sedation/toxicity after converting patients to hydromorphone hydrochloride extended-release tablets.
Conversion from Transdermal Fentanyl to Hydromorphone Hydrochloride Extended-release Tablets
Eighteen hours following the removal of the transdermal fentanyl patch, hydromorphone hydrochloride extended-release tablets treatment can be initiated. To calculate the 24-hour hydromorphone hydrochloride extended-release tablets dose, use a conversion factor of 25 mcg/hr fentanyl transdermal patch to 12 mg of hydromorphone hydrochloride extended-release tablets. Then reduce the hydromorphone hydrochloride extended-release tablets dose by 50%.
For example:
Step 1: Identify the dose of transdermal fentanyl.
- 75 mg of transdermal fentanyl
Step 2: Use the conversion factor of 25 mcg/hr fentanyl transdermal patch to 12 mg of hydromorphone hydrochloride extended-release tablets.
- 75 mg of transdermal fentanyl : 36 mg total daily dose of hydromorphone hydrochloride extended-release tablets
Step 3: Calculate the approximate starting dose of hydromorphone hydrochloride extended-release tablets to be given every 24 hours, which is 50% of the converted dose. Round down, if necessary, to the appropriate hydromorphone hydrochloride extended-release tablet strengths available.
- 50% of 36 mg results in an initial dose of 18 mg, which would be rounded down to 16 mg of hydromorphone hydrochloride extended-release tablets once daily
- Adjust individually for each patient
Conversion from Methadone to Hydromorphone Hydrochloride Extended-release Tablets
Close monitoring is of particular importance when converting from methadone to other opioid agonists. The ratio between methadone and other opioid agonists may vary widely as a function of previous dose exposure. Methadone has a long half-life and can accumulate in the plasma.
Individually titrate hydromorphone hydrochloride extended-release tablets to a dose that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving hydromorphone hydrochloride extended-release tablets to assess the maintenance of pain control and the relative incidence of adverse reactions, as well as monitoring for the development of addiction, abuse, or misuse. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration. During chronic therapy, periodically reassess the continued need for opioid analgesics.
Plasma levels of hydromorphone hydrochloride extended-release tablets are sustained for 18 to 24 hours. Dosage adjustments of hydromorphone hydrochloride extended-release tablets may be made in increments of 4-8 mg every 3 to 4 days as needed to achieve adequate analgesia.
Patients who experience breakthrough pain may require a dose increase of hydromorphone hydrochloride extended-release tablets, or may need rescue medication with an appropriate dose of an immediate-release analgesic. If the level of pain increases after dose stabilization, attempt to identify the source of increased pain before increasing the hydromorphone hydrochloride extended-release tablets dose.
If unacceptable opioid-related adverse reactions are observed, the subsequent doses may be reduced. Adjust the dose to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
When a patient no longer requires therapy with hydromorphone hydrochloride extended-release tablets, taper doses gradually, by 25% to 50% every 2 or 3 days down to a dose of 8 mg before discontinuation of therapy, to prevent signs and symptoms of withdrawal in the opioid-tolerant patient.
To dispose of unused hydromorphone hydrochloride extended-release tablets flush all remaining tablets down the toilet or remit to authorities at a certified drug take-back program.
Start patients with moderate hepatic impairment on 25% of the hydromorphone hydrochloride extended-release tablets dose that would be prescribed for patients with normal hepatic function. Closely monitor patients with moderate hepatic impairment for respiratory and central nervous system depression during initiation of therapy with hydromorphone hydrochloride extended-release tablets and during dose titration. Use of alternate analgesics is recommended for patients with severe hepatic impairment [see Use in Specific Populations (8.6)].
Start patients with moderate renal impairment on 50% and patients with severe renal impairment on 25% of the hydromorphone hydrochloride extended-release tablets dose that would be prescribed for patients with normal renal function. Closely monitor patients with renal impairment for respiratory and central nervous system depression during initiation of therapy with hydromorphone hydrochloride extended-release tablets and during dose titration. As hydromorphone hydrochloride extended-release tablets are only intended for once daily administration, consider use of an alternate analgesic that may permit more flexibility with the dosing interval in patients with severe renal impairment [see Use in Specific Populations (8.7)].
Instruct patients to swallow hydromorphone hydrochloride extended-release tablets intact. The tablets are not to be crushed, dissolved, or chewed due to the risk of rapid release and absorption of a potentially fatal dose of hydromorphone [see Warnings and Precautions (5.2)].
Hydromorphone hydrochloride extended-release tablets are available in 8 mg, 12 mg or 16 mg dosage strengths. The 8 mg tablets are reddish brown, round, film coated tablets with black imprint stating “WPI” and “3629” on one side and plain on the other side. The 12 mg tablets are dark yellow, round, film coated tablets with black imprint stating WPI and 3739 on one side and plain on the other side. The 16 mg tablets are beige to light yellow, round, film coated tablets with black imprint stating WPI and 3630 on one side and plain on the other side.
Hydromorphone hydrochloride is contraindicated in:
- Opioid non-tolerant patients. Fatal respiratory depression could occur in patients who are not opioid tolerant.
- Patients with significant respiratory depression
- Patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment
- Patients with known or suspected paralytic ileus
- Patients who have had surgical procedures and/or underlying disease resulting in narrowing of the gastrointestinal tract, or have “blind loops” of the gastrointestinal tract or gastrointestinal obstruction.
- Patients with hypersensitivity (e.g., anaphylaxis) to hydromorphone or sulfite-containing medications [see Warnings and Precautions (5.10)]
Hydromorphone hydrochloride contains hydromorphone, a Schedule II controlled substance. As an opioid, hydromorphone hydrochloride exposes users to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence (9)]. As modified- release products such as hydromorphone hydrochloride deliver the opioid over an extended period of time, there is a greater risk for overdose and death due to the larger amount of hydromorphone present.
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed hydromorphone hydrochloride and in those who obtain the drug illicitly. Addiction can occur at recommended doses and if the drug is misused or abused.
Assess each patient’s risk for opioid addiction, abuse, or misuse prior to prescribing hydromorphone hydrochloride, and monitor all patients receiving hydromorphone hydrochloride for the development of these behaviors or conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol addiction or abuse) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the prescribing of hydromorphone hydrochloride for the proper management of pain in any given patient.
Patients at increased risk may be prescribed modified-release opioid formulations such as hydromorphone hydrochloride, but use in such patients necessitates intensive counseling about the risks and proper use of hydromorphone hydrochloride along with intensive monitoring for signs of addiction, abuse, and misuse.
Abuse or misuse of hydromorphone hydrochloride by crushing, chewing, snorting, or injecting the dissolved product will result in the uncontrolled delivery of hydromorphone and can result in overdose and death [see Overdosage (10)].
Opioid agonists such as hydromorphone hydrochloride are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing hydromorphone hydrochloride. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on the proper disposal of unused drug [see Patient Counseling Information (17)]. Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
Serious, life-threatening, or fatal respiratory depression has been reported with the use of modified- release opioids, even when used as recommended. Respiratory depression from opioid use, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status [see Overdosage (10)]. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of hydromorphone hydrochloride, the risk is greatest during the initiation of therapy or following a dose increase. Closely monitor patients for respiratory depression when initiating therapy with hydromorphone hydrochloride and following dose increases.
To reduce the risk of respiratory depression, proper dosing and titration of hydromorphone hydrochloride are essential [see Dosage and Administration (2)]. Overestimating the hydromorphone hydrochloride dose when converting patients from another opioid product can result in fatal overdose with the first dose.
Accidental ingestion of even one dose of hydromorphone hydrochloride, especially by children, can result in respiratory depression and death due to an overdose of hydromorphone.
Prolonged use of hydromorphone hydrochloride during pregnancy can result in withdrawal signs in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. The onset, duration, and severity of neonatal opioid withdrawal syndrome vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination of the drug by the newborn.
Hypotension, profound sedation, coma, respiratory depression, and death may result if hydromorphone hydrochloride is used concomitantly with alcohol or other central nervous system (CNS) depressants (e.g., sedatives, anxiolytics, hypnotics, neuroleptics, other opioids).
When considering the use of hydromorphone hydrochloride in a patient taking a CNS depressant, assess the duration of use of the CNS depressant and the patient’s response, including the degree of tolerance that has developed to CNS depression. Additionally, evaluate the patient’s use of alcohol or illicit drugs that cause CNS depression. If the decision to begin hydromorphone hydrochloride is made, start with one third to one half the calculated starting dose, monitor patients for signs of sedation and respiratory depression, and consider using a lower dose of the concomitant CNS depressant [see Drug Interactions (7.1)].
Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients. Monitor such patients closely, particularly when initiating and titrating hydromorphone hydrochloride and when hydromorphone hydrochloride is given concomitantly with other drugs that depress respiration [see Warnings and Precautions (5.2)].
Monitor patients with significant chronic obstructive pulmonary disease or cor pulmonale, and patients having a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression for respiratory depression, particularly when initiating therapy and titrating with hydromorphone hydrochloride, as in these patients, even usual therapeutic doses of hydromorphone hydrochloride may decrease respiratory drive to the point of apnea [see Warnings and Precautions (5.2)]. Consider the use of alternative non-opioid analgesics in these patients if possible.
Hydromorphone hydrochloride may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is an increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g. phenothiazines or general anesthetics) [see Drug Interactions (7.1)]. Monitor these patients for signs of hypotension after initiating or titrating the dose of hydromorphone hydrochloride.
Monitor patients taking hydromorphone hydrochloride who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors) for signs of sedation and respiratory depression, particularly when initiating therapy with hydromorphone hydrochloride. Hydromorphone hydrochloride may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of hydromorphone hydrochloride in patients with impaired consciousness or coma.
Hydromorphone hydrochloride is contraindicated in patients with paralytic ileus. Avoid the use of hydromorphone hydrochloride in patients with other GI obstruction.
Because the hydromorphone hydrochloride extended-release tablet is nondeformable and does not appreciably change in shape in the GI tract, hydromorphone hydrochloride is contraindicated in patients with preexisting severe gastrointestinal narrowing (pathologic or iatrogenic, for example: esophageal motility disorders, small bowel inflammatory disease, “short gut” syndrome due to adhesions or decreased transit time, past history of peritonitis, cystic fibrosis, chronic intestinal pseudoobstruction, or Meckel’s diverticulum). There have been reports of obstructive symptoms in patients with known strictures or risk of strictures, such as previous GI surgery, in association with the ingestion of drugs in nondeformable extended-release formulations.
It is possible that hydromorphone hydrochloride extended-release tablets may be visible on abdominal x-rays under certain circumstances, especially when digital enhancing techniques are utilized.
The hydromorphone in hydromorphone hydrochloride may cause spasm of the sphincter of Oddi. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
Hydromorphone hydrochloride contains sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
The hydromorphone in hydromorphone hydrochloride may aggravate convulsions in patients with convulsive disorders, and may induce or aggravate seizures in some clinical settings. Monitor patients with a history of seizure disorders for worsened seizure control during hydromorphone hydrochloride therapy.
Avoid the use of mixed agonist/antagonist (i.e., pentazocine, nalbuphine, and butorphanol) or partial agonist (buprenorphine) analgesics in patients who have received or are receiving a course of therapy with a full opioid agonist analgesic, including hydromorphone hydrochloride. In these patients, mixed agonist/antagonist and partial agonist analgesics may reduce the analgesic effect and/or may precipitate withdrawal symptoms [see Drug Interactions (7.2)].
When discontinuing hydromorphone hydrochloride, gradually taper the dose [see Dosage and Administration (2.3)]. Do not abruptly discontinue hydromorphone hydrochloride.
Hydromorphone hydrochloride may impair the mental and/or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of hydromorphone hydrochloride and know how they will react to the medication.
The following serious adverse reactions are discussed elsewhere in the labeling:
- Addiction, Abuse, and Misuse [see Warnings and Precautions (5.1)]
- Life Threatening Respiratory Depression [see Warnings and Precautions (5.2)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.3)]
- Interactions with Other CNS Depressants [see Warnings and Precautions (5.4)]
- Hypotensive Effect [see Warnings and Precautions (5.7)]
- Gastrointestinal Effects [see Warnings and Precautions (5.9)]
- Seizures [see Warnings and Precautions (5.11)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Hydromorphone hydrochloride was administered to a total of 2,524 patients in 15 controlled and uncontrolled clinical studies. Of these, 423 patients were exposed to hydromorphone hydrochloride for greater than 6 months and 141 exposed for greater than one year.
The most common adverse reactions leading to study discontinuation were nausea, vomiting, constipation, somnolence, and dizziness. The most common treatment-related serious adverse reactions from controlled and uncontrolled chronic pain studies were drug withdrawal syndrome, overdose, confusional state, and constipation.
The overall incidence of adverse reactions in patients greater than 65 years of age was higher, with a greater than 5% difference in rates for constipation and nausea when compared with younger patients. The overall incidence of adverse reactions in female patients was higher, with a greater than 5% difference in rates for nausea, vomiting, constipation and somnolence when compared with male patients.
A 12-week double-blind, placebo-controlled, randomized withdrawal study was conducted in opioid tolerant patients with moderate to severe low back pain [see Clinical Studies (14)]. A total of 447 patients were enrolled into the open-label titration phase with 268 patients randomized into the double-blind treatment phase. The adverse reactions that were reported in at least 2% of the patients are contained in Table 2.
|
Preferred Term |
Open-Label |
Double-Blind Treatment Phase |
|
|
Hydromorphone Hydrochloride(N=134) |
Placebo (N=134) |
||
|
Constipation |
69 (15) |
10 (7) |
5 (4) |
|
Nausea |
53 (12) |
12 (9) |
10 (7) |
|
Somnolence |
39 (9) |
1 (1) |
0 (0) |
|
Headache |
35 (8) |
7 (5) |
10 (7) |
|
Vomiting |
29 (6) |
8 (6) |
6 (4) |
|
Pruritus |
21 (5) |
1 (1) |
0 (0) |
|
Dizziness |
17 (4) |
3 (2) |
2 (1) |
|
Insomnia |
13 (3) |
7 (5) |
5 (4) |
|
Dry Mouth |
13 (3) |
2 (1) |
0 (0) |
|
Edema Peripheral |
13 (3) |
3 (2) |
1 (1) |
|
H y perhidrosis |
13 (3) |
2 (1) |
2 (1) |
|
Anorexia/Decreased Appetite |
10 (2) |
2 (1) |
0 (0) |
|
Arthralgia |
9 (2) |
8 (6) |
3 (2) |
|
Abdominal Pain |
9 (2) |
4 (3) |
3 (2) |
|
Muscle Spasms |
5 (1) |
3 (2) |
1 (1) |
|
Weight Decreased |
3 (1) |
4 (3) |
3 (2) |
The adverse reactions that were reported in at least 2% of the total treated patients (N=2,474) in the 14 chronic clinical trials are contained in Table 3.
|
Preferred Term |
All Patients (N=2,474) |
|
Constipation |
765 (31) |
|
Nausea |
684 (28) |
|
Vomiting |
337 (14) |
|
Somnolence |
367 (15) |
|
Headache |
308 (12) |
|
Asthenia/Fatigue |
272 (11) |
|
Dizziness |
262 (11) |
|
Diarrhea |
201 (8) |
|
Pruritus |
193 (8) |
|
Insomnia |
161 (7) |
|
H y perhidrosis |
143 (6) |
|
Edema Peripheral |
135 (5) |
|
Anorexia/Decreased Appetite |
139 (6) |
|
Dry Mouth |
121 (5) |
|
Abdominal Pain |
115 (5) |
|
Anxiety |
95 (4) |
|
Back Pain |
95 (4) |
|
D y spepsia* |
88 (4) |
|
Depression |
81 (3) |
|
D y spnea |
76 (3) |
|
Muscle Spasms |
74 (3) |
|
Arthralgia |
72 (3) |
|
Rash |
64 (3) |
|
Pain in Extremity |
63 (3) |
|
Pain |
58 (2) |
|
Drug Withdrawal Syndrome |
55 (2) |
|
Pyrexia |
52 (2) |
|
Fall |
51 (2) |
|
Chest pain |
51 (2) |
* Reflux esophagitis, gastroesophageal reflux disease and Barrett’s esophagus were grouped and reported with dyspepsia
The following Adverse Reactions occurred in patients with an overall frequency of < 2% and are listed in descending order within each System Organ Class:
Cardiac disorders: palpitations, tachycardia, bradycardia, extrasystoles
Ear and labyrinth disorders: vertigo, tinnitus
Endocrine disorders: hypogonadism
Eye disorders: vision blurred, diplopia, dry eye, miosis
Gastrointestinal disorders: flatulence, dysphagia, hematochezia, abdominal distension, hemorrhoids, abnormal feces, intestinal obstruction, eructation, diverticulum, gastrointestinal motility disorder, large intestine perforation, anal fissure, bezoar, duodenitis, ileus, impaired gastric emptying, painful defecation
General disorders and administration site conditions: chills, malaise, feeling abnormal, feeling of body temperature change, feeling jittery, hangover, gait disturbance, feeling drunk, body temperature decreased
Infections and infestations: gastroenteritis, diverticulitis
Injury, poisoning and procedural complications: contusion, overdose
I nvestigations: weight decreased, hepatic enzyme increased, blood potassium decreased, blood amylase increased, blood testosterone decreased
Metabolism and nutrition disorders: dehydration, fluid retention, increased appetite, hyperuricemia
Musculoskeletal and connective tissue disorders: myalgia
Nervous system disorders: tremor, sedation, hypoesthesia, paresthesia, disturbance in attention, memory impairment, dysarthria, syncope, balance disorder, dysgeusia, depressed level of consciousness, coordination abnormal, hyperesthesia, myoclonus, dyskinesia, crying, hyperreflexia, encephalopathy, cognitive disorder, convulsion, psychomotor hyperactivity
Psychiatric disorders: confusional state, nervousness, restlessness, abnormal dreams, mood altered, hallucination, panic attack, euphoric mood, paranoia, dysphoria, listless, suicide ideation, libido decreased, aggression
Renal and urinary disorders: dysuria, urinary retention, urinary frequency, urinary hesitation, micturition disorder
Reproductive system and breast disorders: erectile dysfunction, sexual dysfunction
Respiratory, thoracic and mediastinal disorders: rhinorrhea, respiratory distress, hypoxia, bronchospasm, sneezing, hyperventilation, respiratory depression
Skin and subcutaneous tissue disorders: erythema
Vascular disorders: flushing, hypertension, hypotension
The following adverse reactions have been identified during post-approval use of hydromorphone hydrochloride:
Immune system disorders: hypersensitivity
Skin and subcutaneous tissue disorders: angioedema, urticarial
The concomitant use of hydromorphone hydrochloride with other CNS depressants including sedatives, hypnotics, tranquilizers, general anesthetics, phenothiazines, other opioids, and alcohol can increase the risk of respiratory depression, profound sedation, coma and death. Monitor patients receiving CNS depressants and hydromorphone hydrochloride for signs of respiratory depression, sedation and hypotension.
When combined therapy with any of the above medications is considered, the dose of one or both agents should be reduced [see Dosage and Administration (2.2) and Warnings and Precautions (5.4)].
Mixed agonist/antagonist (i.e., pentazocine, nalbuphine, and butorphanol) and partial agonist (buprenorphine) analgesics may reduce the analgesic effect of hydromorphone hydrochloride or precipitate withdrawal symptoms. Avoid the use of mixed agonist/antagonist and partial agonist analgesics in patients receiving hydromorphone hydrochloride.
The effects of opioid analgesics may be potentiated by MAOIs. Hydromorphone hydrochloride is not recommended for use in patients who have received MAOIs within 14 days. If concurrent therapy with an MAOI and hydromorphone hydrochloride is unavoidable, monitor patients for increased respiratory and central nervous system depression.
Anticholinergics or other medications with anticholinergic activity when used concurrently with hydromorphone hydrochloride may result in increased risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. Monitor patients for signs of urinary retention or reduced gastric motility when hydromorphone hydrochloride is used concurrently with anticholinergic drugs.
Clinical Considerations
Fetal/neonatal adverse reactions
Prolonged use of opioid analgesics during pregnancy for medical or nonmedical purposes can result in physical dependence in the neonate and neonatal opioid withdrawal syndrome shortly after birth. Observe newborns for symptoms of neonatal opioid withdrawal syndrome, such as poor feeding, diarrhea, irritability, tremor, rigidity, and seizures, and manage accordingly [see Warnings and Precautions (5.3)].
Teratogenic Effects
– Pregnancy Category C:
There are no adequate and well-controlled studies in pregnant women. Hydromorphone hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus [see Use in Specific Populations (8.2)].
Hydromorphone was not teratogenic in pregnant rats given oral doses up to 6.25 mg/kg/day or in pregnant rabbits administered oral doses up to 25 mg/kg/day during the period of organogenesis (~1.2 times the human exposure following 32 mg/day).
Hydromorphone administration to pregnant Syrian hamsters and CF-1 mice during major organ development revealed teratogenicity likely the result of maternal toxicity associated with sedation and hypoxia. In Syrian hamsters given single subcutaneous doses from 14 to 258 mg/kg during organogenesis (gestation days 8 to 10), doses ≥ 19 mg/kg hydromorphone produced skull malformations (exencephaly and cranioschisis). Continuous infusion of hydromorphone (5 mg/kg, s.c.) via implanted osmotic mini pumps during organogenesis (gestation days 7 to 10) produced soft tissue malformations (cryptorchidism, cleft palate, malformed ventricals and retina), and skeletal variations (supraoccipital, checkerboard and split sternebrae, delayed ossification of the paws and ectopic ossification sites). The malformations and variations observed in the hamsters and mice were at doses approximately three-fold higher and < one-fold lower, respectively, than a 32 mg human daily oral dose on a body surface area basis.
Nonteratogenic Effects
In the pre- and postnatal effects study in rats, neonatal viability was reduced at 6.25 mg/kg/day (~1.2 times the human exposure following 32 mg/day).
Opioids cross the placenta and may produce respiratory depression in neonates. Hydromorphone hydrochloride is not for use in women during and immediately prior to labor, when shorter acting analgesics or other analgesic techniques are more appropriate. Opioid analgesics can prolong labor through actions that temporarily reduce the strength, duration, and frequency of uterine contractions. However this effect is not consistent and may be offset by an increased rate of cervical dilatation, which tends to shorten labor.
Low concentrations of hydromorphone have been detected in human milk in clinical trials. Withdrawal symptoms can occur in breastfeeding infants when maternal administration of an opioid analgesic is stopped. Nursing should not be undertaken while a patient is receiving hydromorphone hydrochloride since hydromorphone is excreted in the milk.
The safety and effectiveness of hydromorphone hydrochloride in patients 17 years of age and younger have not been established.
Elderly patients have been shown to be more sensitive to the adverse effects of opioids compared to the younger population. Therefore, closely monitor elderly patients for respiratory and central nervous system depression when prescribing hydromorphone hydrochloride, particularly during initiation and titration.
In a study that used a single 4 mg oral dose of immediate-release hydromorphone tablets, four-fold increases in plasma levels of hydromorphone (Cmax and AUC0-∞) were observed in patients with moderate hepatic impairment (Child-Pugh Group B). Start patients with moderate hepatic impairment on 25% of the hydromorphone hydrochloride dose that would be used in patients with normal hepatic function. Closely monitor patients with moderate hepatic impairment for respiratory and central nervous system depression during initiation of therapy with hydromorphone hydrochloride and during dose titration. The pharmacokinetics of hydromorphone in severe hepatic impairment patients have not been studied. As further increases in Cmax and AUC0-∞ of hydromorphone in this group are expected, use of alternate analgesics is recommended [see Dosage and Administration (2.4)].
Administration of a single 4 mg dose of immediate-release hydromorphone tablets resulted in two-fold and four-fold increases in plasma levels of hydromorphone (Cmax and AUC0-48h) in moderate (CLcr = 40 to 60 mL/min) and severe (CLcr < 30 mL/min) impairment, respectively. In addition, in patients with severe renal impairment hydromorphone appeared to be more slowly eliminated with longer terminal elimination half-life (40 hours) compared to subjects with normal renal function (15 hours). Start patients with moderate renal impairment on 50% and patients with severe renal impairment on 25% of the hydromorphone hydrochloride dose that would be prescribed for patients with normal renal function. Closely monitor patients with renal impairment for respiratory and central nervous system depression during initiation of therapy with hydromorphone hydrochloride and during dose titration. As hydromorphone hydrochloride is only intended for once daily administration, consider use of an alternate analgesic that may permit more flexibility with the dosing interval in patients with severe renal impairment [see Dosage and Administration (2.5)].
Hydromorphone hydrochloride contains hydromorphone, a Schedule II controlled substance with a high potential for abuse similar to fentanyl, methadone, morphine, oxycodone, and oxymorphone. Hydromorphone hydrochloride can be abused and is subject to misuse, abuse, addiction, and criminal diversion [see Warnings and Precautions (5.1)].
All patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Drug abuse is the intentional non-therapeutic use of an over-the-counter or prescription drug, even once, for its rewarding psychological or physiological effects. Drug abuse includes, but is not limited to the following examples: the use of a prescription or over-the-counter drug to get “high”, or the use of steroids for performance enhancement and muscle build up.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and include: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal.
'Drug-seeking' behavior is very common to addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated claims of loss of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” (visiting multiple prescribers) to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction. Preoccupation with achieving pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction.
Hydromorphone hydrochloride, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful recordkeeping of prescribing information, including quantity, frequency, and renewal requests, as required by law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of Hydromorphone Hydrochloride
Hydromorphone hydrochloride is intended for oral use only. Abuse of hydromorphone hydrochloride poses a risk of overdose and death. This risk is increased with concurrent abuse of hydromorphone hydrochloride with alcohol and other substances.
Taking cut, broken, chewed, crushed, or dissolved hydromorphone hydrochloride poses a hazard of overdose and death.
With intravenous abuse, the tablet excipients, especially polyethylene oxide, can be expected to result in necrosis and inflammation of cardiac tissues. In addition, parenteral drug abuse is commonly associated with transmission of infectious disease such as hepatitis and HIV.
Healthcare professionals should contact their State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dose reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity, e.g., naloxone, nalmefene, mixed agonist/antagonist analgesics (pentazocine, butorphanol, nalbuphine), or partial agonists (buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
Hydromorphone hydrochloride should not be abruptly discontinued [see Dosage and Administration (2.3)]. If hydromorphone hydrochloride is abruptly discontinued in a physically-dependent patient, an abstinence syndrome may occur. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, piloerection, myalgia, mydriasis, irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, increased blood pressure, respiratory rate, or heart rate.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms [see Use in Specific Populations (8.1, 8.2)].
Clinical Presentation
Acute overdosage with opioids can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and sometimes pulmonary edema, bradycardia, hypotension and death. Marked mydriasis rather than miosis may be seen due to severe hypoxia in overdose situations.
Treatment of Overdose
In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation if needed. Employ other supportive measures (including oxygen, vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life support techniques.
The opioid antagonists, such as naloxone and naltrexone, are specific antidotes to respiratory depression resulting from opioid overdose. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to hydromorphone overdose. Such agents should be administered cautiously to patients who are known, or suspected to be, physically dependent on hydromorphone hydrochloride. In such cases, an abrupt or complete reversal of opioid effects may precipitate an acute withdrawal syndrome.
Because the duration of reversal would be expected to be less than the duration of action of hydromorphone in hydromorphone hydrochloride, carefully monitor the patient until spontaneous respiration is reliably reestablished. Hydromorphone hydrochloride will continue to release hydromorphone adding to the hydromorphone load for up to 24 hours after administration, necessitating prolonged monitoring for at least 24 to 48 hours beyond the overdose. If the response to opioid antagonists is suboptimal or not sustained, additional antagonist should be given as directed in the product’s prescribing information.
In an individual physically dependent on opioids, administration of an opioid receptor antagonist may precipitate an acute withdrawal. The severity of the withdrawal syndrome produced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be begun with care and by titration with smaller than usual doses of the antagonist.
Hydromorphone hydrochloride extended-release tablets are for oral use and contain hydromorphone hydrochloride, a mu- opioid agonist.
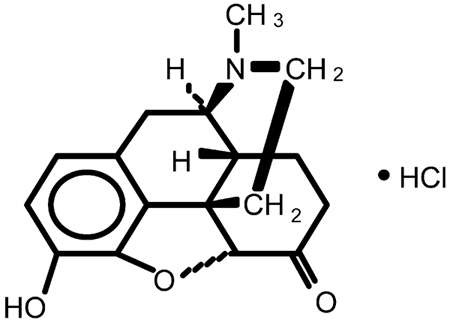
Hydromorphone hydrochloride USP is 4,5α-epoxy-3-hydroxy-17-methlymorphinan-6-one hydrochloride. Hydromorphone hydrochloride is a white or almost white crystalline powder that is freely soluble in water, very slightly soluble in ethanol (96%), and practically insoluble in methylene chloride. Its molecular formula is C17H19NO3•HCl. The compound has the following structural formula:
Hydromorphone hydrochloride extended-release tablets also contain the following inactive ingredients: cellulose acetate, copovidone, hypromellose, iron oxide black, iron oxide red (8 mg and 16 mg only), iron oxide yellow (12 mg and 16 mg only), lactose monohydrate, magnesium stearate, polyethylene glycol, polyvinyl alcohol (8 mg and 16 mg only), propylene glycol, sodium chloride, talc and titanium dioxide.
Hydromorphone, a semi-synthetic morphine derivative, is a hydrogenated ketone of morphine. Hydromorphone is principally an agonist of mu-receptors, showing a weak affinity for κ-receptors. Comparing relative binding affinity for mu- and κ-opioid receptors, hydromorphone binds more specifically to mu- receptors than structurally related morphine. As an opioid agonist, the principle therapeutic action of hydromorphone is analgesia. The precise mechanism of action of opioid analgesics is not known but the effects are thought to be mediated through opioid-specific receptors located predominantly in the central nervous system (CNS). Interaction with the mu-opioid receptor subtype is believed to be responsible for most of hydromorphone’s clinical effects. There is no intrinsic limit to the analgesic effect of hydromorphone. Clinically, however, dosage limitations are imposed by the adverse effects, primarily respiratory depression, sedation, nausea, and vomiting, which can result from high doses.
CNS Depressant/Alcohol Interaction
Additive pharmacodynamic effects may be expected when hydromorphone hydrochloride is used in conjunction with alcohol, other opioids, legal or illicit drugs that cause central nervous system depression.
Effects on the Central Nervous System
Hydromorphone produces dose-related respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to increases in carbon dioxide tension and to electrical stimulation.
Hydromorphone depresses the cough reflex by direct effect on the cough center in the medulla.
Hydromorphone causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomic. Marked mydriasis, rather than miosis, may be seen due to severe hypoxia in overdose situations.
Effects on the Gastrointestinal Tract and Other Smooth Muscle
Gastric, biliary and pancreatic secretions are decreased by hydromorphone. Hydromorphone causes a reduction in motility associated with an increase in tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm. The end result is constipation. Hydromorphone also can cause an increase in biliary tract pressure as a result of spasm of the sphincter of Oddi.
Effects on the Cardiovascular System
Hydromorphone produces peripheral vasodilation which may result in orthostatic hypotension or syncope. Release of histamine may be induced by hydromorphone and can contribute to opioid-induced hypotension. Manifestations of histamine release or peripheral vasodilation may include pruritus, flushing, red eyes, and sweating.
Effects on the Endocrine System
Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Absorption
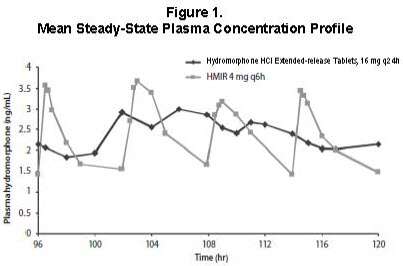
Hydromorphone hydrochloride is an extended-release formulation of hydromorphone that produces a gradual increase in hydromorphone concentrations. Following a single-dose administration of hydromorphone hydrochloride, plasma concentrations gradually increase over 6 to 8 hours, and thereafter concentrations are sustained for approximately 18 to 24 hours post-dose. The median Tmax values ranged from 12 to 16 hours. The mean half-life was approximately 11 hours, ranging from 8 to 15 hours in most individual subjects. Linear pharmacokinetics has been demonstrated for hydromorphone hydrochloride over the dose range 8 to 64 mg, with a dose-proportional increase in Cmax and overall exposure (AUC0-∞) (see
Table 4). Steady-state plasma concentrations are approximately twice those observed following the first dose, and steady state is reached after 3 to 4 days of once-daily dosing of hydromorphone hydrochloride. At steady state, hydromorphone hydrochloride given once daily maintained hydromorphone plasma concentrations within the same concentration range as the immediate-release tablet given 4 times daily at the same total daily dose and diminished the fluctuations between peak and trough concentrations seen with the immediate-release tablet (see
Figure 1). The bioavailability of hydromorphone hydrochloride once daily and immediate-release hydromorphone four times daily in adults is comparable, as presented in Table 4.
|
Regimen |
Dosage |
T max * (hrs) |
C max (ng/mL) |
AUC (ng·hr/mL) |
T ½ (hr) |
|
Single Dose |
8 mg |
12 (4-30) |
0.93 (1.01) |
18.1 (5.8) |
10.6 (4.3) |
|
(N = 31) |
16 mg |
16 (6-30) |
1.69 (0.78) |
36.5 (11.3) |
10.3 (2.4) |
|
32 mg |
16 (4-24) |
3.25 (1.37) |
72.2 (24.3) |
11.0 (3.2) |
|
|
64 mg |
16 (6-30) |
6.61 (1.75) |
156.0 (30.6) |
10.9 (3.8) |
|
|
Multiple Dose† (N = 29) |
16 mg q24h |
12 (6-24) |
3.54 (0.96)‡ |
57.6 (16.3) |
NA |
|
IR 4 mg q6h |
0.75 (0.5-2) |
5.28 (1.37)§ |
54.8 (14.8) |
NA |
NA = not applicable
* Median (range) reported for Tmax
† Steady-state results on Day 5 (0-24 hours)
‡Cmin 2.15 (0.87) ng/mL
§Cmin 1.47 (0.42) ng/mL
Food Effect
The pharmacokinetics of hydromorphone hydrochloride are not affected by food as indicated by bioequivalence when administered under fed and fasting conditions. Therefore, hydromorphone hydrochloride may be administered without regard to meals. When a 16 mg dose of hydromorphone hydrochloride was administered to healthy volunteers immediately following a high-fat meal, the median time to Cmax (Tmax) was minimally affected by the high-fat meal occurring at 16 hours compared to 18 hours while fasting.
Distribution
Following intravenous administration of hydromorphone to healthy volunteers, the mean volume of distribution was 2.9 (±1.3) L/kg, suggesting extensive tissue distribution. The mean extent of binding of hydromorphone to human plasma proteins was determined to be 27% in an in vitro study.
Metabolism
After oral administration of an immediate-release formulation, hydromorphone undergoes extensive first-pass metabolism and is metabolized primarily in the liver by glucuronidation to hydromorphone-3glucuronide, which follows a similar time course to hydromorphone in plasma. Exposure to the glucuronide metabolite is 35 to 40 times higher than exposure to the parent drug. In vitro data suggest that hydromorphone in clinically relevant concentrations has minimal potential to inhibit the activity of human hepatic CYP450 enzymes including CYP1A2, 2C9, 2C19, 2D6, 3A4, and 4A11.
Excretion
Approximately 75% of the administered dose is excreted in urine. Most of the administered hydromorphone dose is excreted as metabolites. Approximately 7% and 1% of the dose are excreted as unchanged hydromorphone in urine and feces, respectively.
Specific Populations
Geriatric Patients
Based on data obtained from a study using immediate-release hydromorphone, the pharmacokinetics of hydromorphone in healthy elderly subjects (65 to 74 years old) are similar to the pharmacokinetics in healthy young subjects.
Pediatric Patients
The pharmacokinetics of hydromorphone hydrochloride were not evaluated in a pediatric population.
Gender
Females appeared to have approximately 10% higher mean systemic exposure in terms of Cmax and AUC values.
R
a
ce
The effect of race on hydromorphone hydrochloride pharmacokinetics has not been studied.
Hepatic Impairment
In a study that used a single 4 mg oral dose of immediate-release hydromorphone tablets, four-fold increases in plasma levels of hydromorphone (Cmax and AUC0-∞) were observed in patients with moderate hepatic impairment (Child-Pugh Group B). Pharmacokinetics of hydromorphone in severe hepatic impairment patients has not been studied. Further increase in Cmax and AUC0-∞ of hydromorphone in this group is expected. Start patients with moderate hepatic impairment on 25% of the usual dose of hydromorphone hydrochloride and closely monitor for respiratory and central nervous system depression during dose titration. Consider alternate analgesic therapy for patients with severe hepatic impairment [see Dosage and Administration (2.4) and Specific Populations (8.6)].
Renal Impairment
Renal impairment affected the pharmacokinetics of hydromorphone and its metabolites following administration of a single 4 mg dose of immediate-release tablets. The effects of renal impairment on hydromorphone pharmacokinetics were two-fold and four-fold increases in plasma levels of hydromorphone (Cmax and AUC0-48h) in moderate (CLcr = 40 to 60 mL/min) and severe (CLcr < 30 mL/min) impairment, respectively. In addition, in patients with severe renal impairment hydromorphone appeared to be more slowly eliminated with longer terminal elimination half-life (40 hr) compared to subjects with normal renal function (15 hr). Start patients with moderate renal impairment on 50% of the usual hydromorphone hydrochloride dose for patients with normal renal function and closely monitor for respiratory and central nervous system depression during dose titration. As hydromorphone hydrochloride is only intended for once-daily administration, consider use of an alternate analgesic that may permit more flexibility with the dosing interval in patients with severe renal impairment [see Dosage and Administration (2.5) and Use in Specific Populations (8.7)].
Drug Interaction/Alcohol Interaction
An in vivo study examined the effect of alcohol (40%, 20%, 4% and 0%) on the bioavailability of a single dose of 16 mg of hydromorphone hydrochloride in healthy, fasted or fed volunteers. The results showed that the hydromorphone mean AUC0-∞ was 5% higher and 4% lower (not statistically significant) in the fasted and fed groups respectively after co-administration of 240 mL of 40% alcohol. The AUC0-∞ was similarly unaffected in subjects following the co-administration of hydromorphone hydrochloride and alcohol (240 mL of 20% or 4% alcohol).
The change in geometric mean Cmax with concomitant administration of alcohol and hydromorphone hydrochloride ranged from an increase of 10% to 31% across all conditions studied. The change in mean Cmax was greater in the fasted group of subjects. Following concomitant administration of 240 mL of 40% alcohol while fasting, the mean Cmax increased by 37% and up to 151% in an individual subject. Following the concomitant administration of 240 mL of 20% alcohol while fasting, the mean Cmax increased by 35% and up to 139% in an individual subject. Following the concomitant administration of 240 mL of 4
Carcinogenesis
Long-term studies to evaluate the carcinogenic potential of hydromorphone hydrochloride were completed in both Han-Wistar rats and Crl:CD1®(ICR) mice. Hydromorphone HCl was administered to Han-Wistar rats (2, 5, and 15 mg/kg/day for males, and 8, 25 and 75 mg/kg/day for females) for 2 years by oral gavage. In female rats, incidences of hibernoma (tumor of brown fat) were increased at 10.5 times the maximum recommended daily exposure based on AUC at the mid dose (2 tumor, 25 mg/kg/day) and 53.7 times the maximum recommended human daily exposure based on AUC at the maximum dose (4 tumors, 75 mg/kg/day). The clinical relevance of this finding to humans has not been established. There was no evidence of carcinogenicity in male rats. The systemic drug exposure (AUC, ng·h/mL) at the 15 mg/kg/day in male rats was 7.6 times greater than the human exposure at a single dose of32 mg/day of hydromorphone hydrochloride. There was no evidence of carcinogenic potential in Crl:CD1®(ICR) mice administered hydromorphone HCl at doses up to 15 mg/kg/day for 2 years by oral gavage. The systemic drug exposure (AUC, ng•h/mL) at the 15 mg/kg/day in mice was 1.1 (in males) and 1.2 (in females) times greater than the human exposure at a single dose of 32 mg/day of hydromorphone hydrochloride.
Mutagenesis
Hydromorphone was not mutagenic in the in vitro bacterial reverse mutation assay (Ames assay). Hydromorphone was not clastogenic in either the in vitro human lymphocyte chromosome aberration assay or the in vivo mouse micronucleus assay.
Impairment of Fertility
Hydromorphone given orally to rats during the mating period caused a slight but statistically significant reduction in implantations at 6.25 mg/kg/day (~1.2 times the human exposure following to 32 mg/day).
Hydromorphone hydrochloride was investigated in a double-blind, placebo-controlled, randomized withdrawal study in opioid tolerant patients with moderate-to-severe low back pain. Patients were considered opioid tolerant if they were currently on opioid therapy that was ≥ 60 mg/day of oral morphine equivalent for at least 2 months prior to screening. Patients entered an open-label conversion and titration phase with hydromorphone hydrochloride, were converted to a starting dose that was approximately 75% of their total daily morphine equivalent dose, and were dosed once daily until adequate pain control was achieved while exhibiting tolerable side effects. Supplemental immediate-release hydromorphone tablets were allowed throughout the study. Patients who achieved a stable dose entered a 12-week, double-blind, placebo-controlled, randomized treatment phase. Mean daily dose at randomization was 37.8 mg/day (range of 12 mg/day to 64 mg/day). Fifty-eight (58) percent of patients were successfully titrated to a stable dose of hydromorphone hydrochloride during the open-label conversion and titration phase.
During the double-blind treatment phase, patients randomized to hydromorphone hydrochloride continued with the stable dose achieved in the conversion and titration phase of the study. Patients randomized to placebo received, in a blinded manner, hydromorphone hydrochloride and matching placebo in doses tapering from the stable dose achieved in conversion and titration. During the taper down period, patients were allowed immediate-release hydromorphone tablets as supplemental analgesia to minimize opioid withdrawal symptoms in placebo patients. After the taper period, the number of immediate-release hydromorphone tablets was limited to two tablets per day. Forty-nine (49) percent of patients treated with hydromorphone hydrochloride and 33% of patients treated with placebo completed the 12-week treatment period.
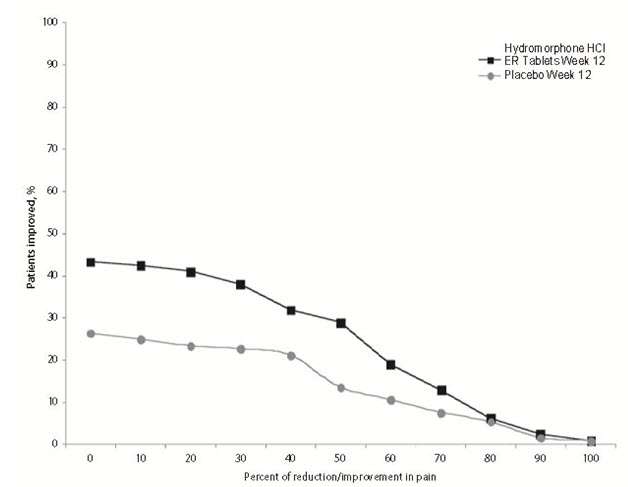
Hydromorphone hydrochloride provided superior analgesia compared to placebo. There was a significant difference between the mean changes from Baseline to Week 12 or Final Visit in average weekly pain intensity Numeric Rating Scale (NRS) scores obtained from patient diaries between the two groups. The proportion of patients with various degrees of improvement from screening to Week 12 or Final Visit is shown in Figure 2. For this analysis, patients who discontinued treatment for any reason prior to Week 12 were assigned a value of zero improvement.
How Supplied
Hydromorphone Hydrochloride Extended-Release Tablet Strengths
|
Strength |
Color |
Table t Description |
Bo
t
t
le |
NDC |
|
8 mg |
Reddish brown |
Round, film-coated tablets with black imprint stating WPI and 3629 on one side and plain on the other side |
30 |
0591-3629-30 |
|
100 |
0591-3629-01 |
|||
|
1000 |
0591-3629-10 |
|||
|
12 mg |
Dark yellow |
Round, film-coated tablets with black imprint stating WPI and 3739 on one side and plain on the other side |
30 |
0591-3739-30 |
|
100 |
0591-3739-01 |
|||
|
1000 |
0591-3739-10 |
|||
|
16 mg |
Beige to light yellow |
Round, film coated tablets with black imprint stating WPI and 3630 on one side and plain on the other side |
30 |
0591-3630-30 |
|
100 |
0591-3630-01 |
|||
|
1000 |
0591-3630-10 |
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Advise the patient to read the FDA-approved patient labeling (Medication Guide)
Addiction, Abuse, and Misuse
Inform patients that the use of hydromorphone hydrochloride extended-release tablets, even when taken as recommended, can result in addiction, abuse, and misuse, which can lead to overdose or death [see Warnings and Precautions (5.1)]. Instruct patients not to share hydromorphone hydrochloride extended-release tablets with others and to take steps to protect hydromorphone hydrochloride extended-release tablets from theft or misuse.
Life-threatening Respiratory Depression
Inform patients of the risk of life-threatening respiratory depression, including information that the risk is greatest when starting hydromorphone hydrochloride extended-release tablets or when the dose is increased, and that it can occur even at recommended doses [see Warnings and Precautions (5.2)]. Advise patients how to recognize respiratory depression and to seek medical attention if breathing difficulties develop.
Accidental Ingestion
Inform patients that accidental Ingestion, especially in children, may result in respiratory depression or death [see Warnings and Precautions (5.2)]. Instruct patients to take steps to store hydromorphone hydrochloride extended-release tablets securely and to dispose of unused hydromorphone hydrochloride extended-release tablets by flushing the tablets down the toilet.
Neonatal Opioid Withdrawal Syndrome
Inform female patients of reproductive potential that prolonged use of hydromorphone hydrochloride extended-release tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated [see Warnings and Precautions (5.3)].
Interactions with Alcohol and other CNS Depressants
Inform patients that potentially serious additive effects may occur if hydromorphone hydrochloride extended-release tablets are used with alcohol or other CNS depressants, and not to use such drugs unless supervised by a health care provider.
Important Administration Instructions
Instruct patients how to properly take hydromorphone hydrochloride extended-release tablets, including the following:
- Swallowing hydromorphone hydrochloride extended-release tablets whole
- Not crushing, chewing, splitting or dissolving the tablets
- Using hydromorphone hydrochloride extended-release tablets exactly as prescribed to reduce the risk of life-threatening adverse reactions (e.g., respiratory depression)
- Not discontinuing hydromorphone hydrochloride extended-release tablets without first discussing the need for a tapering regimen with the prescriber
Gastrointestinal Blockage
Advise patients that people with certain stomach or intestinal problems such as narrowing of the intestines or previous surgery may be at higher risk of developing a blockage. Symptoms include abdominal distension, abdominal pain, severe constipation, or vomiting. Instruct patients to contact their healthcare provider immediately if they develop these symptoms.
Hypotension
Inform patients that hydromorphone hydrochloride extended-release tablets may cause orthostatic hypotension and syncope. Instruct patients how to recognize symptoms of low blood pressure and how to reduce the risk of serious consequences should hypotension occur (e.g., sit or lie down, carefully rise from a sitting or lying position).
Driving or Operating Heavy Machinery
Inform patients that hydromorphone hydrochloride extended-release tablets may impair the ability to perform potentially hazardous activities such as driving a car or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication.
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention.
Anaphylaxis
Inform patients that anaphylaxis has been reported with ingredients contained in hydromorphone hydrochloride extended-release tablets. Advise patients how to recognize such a reaction and when to seek medical attention.
Pregnancy
Advise female patients that hydromorphone hydrochloride extended-release tablets can cause fetal harm and to inform the prescriber if they are pregnant or plan to become pregnant.
Disposal
Advise patients to flush the unused tablets down the toilet when hydromorphone hydrochloride extended-release tablets are no longer needed.
|
Medication Guide |
|
Hydromorphone hydrochloride extended-release tablets are:
|
|
Important information about hydromorphone hydrochloride extended-release tablets:
|
|
Do not take hydromorphone hydrochloride extended-release tablets if you have:
|
|
Before taking hydromorphone hydrochloride extended-release tablets, tell your healthcare provider if you have a history of:
|
|
Tell your healthcare provider if you are:
|
|
When taking hydromorphone hydrochloride extended-release tablets:
|
|
While taking hydromorphone hydrochloride extended-release tablets, DO NOT:
|
|
The possible side effects of hydromorphone hydrochloride extended-release tablets are:
Get emergency medical help if you have:
These are not all the possible side effects of hydromorphone hydrochloride extended-release tablets. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to dailymed.nlm.nih.gov Manufactured by: Distributed by: |
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: April 2014
NDC 0591-3629-01
Hydromorphone
Hydrochloride
Extended-release Tablets
Once-daily
8 mg
CII
For opiod-tolerant patients only
PHARMACIST: PLEASE DISPENSE IN THIS UNIT-OF-USE, CHILD
RESISTANT CONTAINER WITH MEDICATION GUIDE PROVIDED.
Watson®
100 Tablets
Rx Only
Each tablet contains: Hydromorphone
Hydrochloride USP, 8 mg.
Swallow tablets whole. Do not break, crush
or chew tablet.
See package insert for dosing information.
Store at 20º to 25º C (68º to 77º F) [See USP
Controlled Room Temperature].
Manufactured by:
Watson Laboratories, Inc.
Corona, CA 92880 USA
220444
Distributed by: Watson Pharma, Inc.
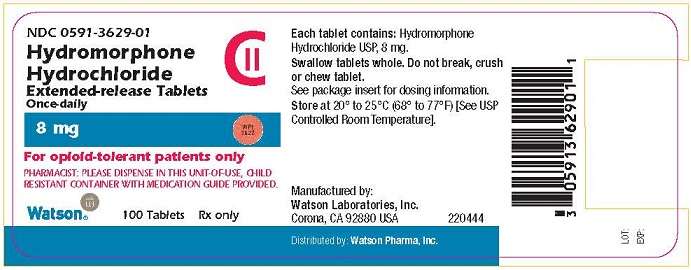
NDC 0591-3739-01
Hydromorphone
Hydrochloride
Extended-release Tablets
Once-daily
12 mg
CII
For opiod-tolerant patients only
PHARMACIST: PLEASE DISPENSE IN THIS UNIT-OF-USE, CHILD
RESISTANT CONTAINER WITH MEDICATION GUIDE PROVIDED.
Watson®
100 Tablets
Rx Only
Each tablet contains: Hydromorphone
Hydrochloride USP, 12 mg.
Swallow tablets whole. Do not break, crush
or chew tablet.
See package insert for dosing information.
Store at 20º to 25º C (68º to 77º F) [See USP
Controlled Room Temperature].
Manufactured by:
Watson Laboratories, Inc.
Corona, CA 92880 USA
220447
Distributed by: Watson Pharma, Inc.
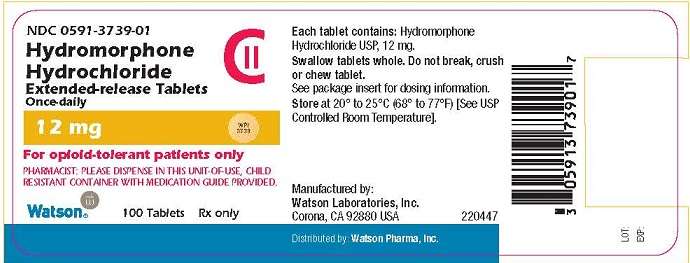
NDC 0591-3630-01
Hydromorphone
Hydrochloride
Extended-release Tablets
Once-daily
16 mg
CII
For opiod-tolerant patients only
PHARMACIST: PLEASE DISPENSE IN THIS UNIT-OF-USE, CHILD
RESISTANT CONTAINER WITH MEDICATION GUIDE PROVIDED.
Watson®
100 Tablets
Rx Only
Each tablet contains: Hydromorphone
Hydrochloride USP, 16 mg.
Swallow tablets whole. Do not break, crush
or chew tablet.
See package insert for dosing information.
Store at 20º to 25º C (68º to 77º F) [See USP
Controlled Room Temperature].
Manufactured by:
Watson Laboratories, Inc.
Corona, CA 92880 USA
220450
Distributed by: Watson Pharma, Inc.
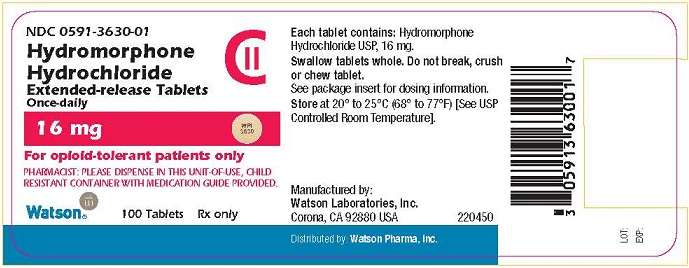
Hydromorphone HydrochlorideHydromorphone Hydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Hydromorphone HydrochlorideHydromorphone Hydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Hydromorphone HydrochlorideHydromorphone Hydrochloride TABLET, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||