Lamisil
Novartis Pharmaceuticals Corporation
HIGHLIGHTS OF PRESCRIBING INFORMATION INDICATIONS AND USAGELamisil Oral Granules are an allylamine antifungal indicated for the treatment of tinea capitis in patients 4 years of age and older. (1)DOSAGE AND ADMINISTRATIONTake once a day with food for 6 weeks (dose based on body weight). The entire contents of each packet of granules should be sprinkled on a spoonful of non-acidic food (for example, pudding or mashed potatoes) and swallowed in its entirety. (2) Table 1: Dosage by Body Weight 35 kg 250 mg/day DOSAGE FORMS AND STRENGTHSOral Granules, 125 mg or 187.5 mg (terbinafine base equivalent) per packet. (3)CONTRAINDICATIONSLamisil Oral Granules are contraindicated in individuals with a history of allergic reaction to oral terbinafine because of the risk of anaphylaxis. (4)WARNINGS AND PRECAUTIONS Liver failure, sometimes leading to death or liver transplant, has occurred with the use of oral terbinafine. Obtain pretreatment serum transaminases. Discontinue Lamisil Oral Granules if liver injury develops. (5.1, 5.8) Taste disturbance, including taste loss, has been reported with oral terbinafine use. Taste disturbance can be severe, may be prolonged, or may be permanent. Discontinue Lamisil Oral Granules if taste disturbance occurs. (5.2) Smell disturbance, including loss of smell, has been reported with the use of oral terbinafine. Smell disturbance may be prolonged or may be permanent. Discontinue Lamisil Oral Granules if smell disturbance occurs. (5.3) Depressive symptoms have been reported with oral terbinafine use. Prescribers should be alert to the development of depressive symptoms. (5.4) Severe neutropenia has been reported. If the neutrophil count is 3% in patients treated with Lamisil Oral Granules) reported adverse events include: nasopharyngitis, headache, pyrexia, cough, vomiting, upper respiratory tract infection, nausea, upper abdominal pain, and diarrhea. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSTerbinafine is an inhibitor of CYP450 2D6 isozyme and has an effect on metabolism of desipramine. Drug interactions have also been noted with cimetidine, fluconazole, cyclosporine, rifampin, and caffeine. (7.1)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 LAMISIL INDICATIONS AND USAGE
- 2 LAMISIL DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 LAMISIL CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 LAMISIL ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 LAMISIL DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Lamisil (terbinafine hydrochloride) Oral Granules are indicated for the treatment of tinea capitis in patients 4 years of age and older.
2 DOSAGE AND ADMINISTRATION
Lamisil (terbinafine hydrochloride) Oral Granules should be taken once a day for 6 weeks based upon body weight (See Table 1). Sprinkle the contents of each packet on a spoonful of pudding or other soft, nonacidic food such as mashed potatoes and swallow the entire spoonful (without chewing); do not use applesauce or fruit-based foods. Take with food. If 2 packets (250 mg) are required with each dose, either the content of both packets may be sprinkled on 1 spoonful, or the contents of both packets may be sprinkled on 2 spoonfuls of nonacidic food as directed above.
| <25 kg | 125 mg/day |
| 25-35 kg | 187.5 mg/day |
| >35 kg | 250 mg/day |
3 DOSAGE FORMS AND STRENGTHS
Oral Granules, 125 mg or 187.5 mg (terbinafine base equivalent) per packet. The film-coated granules are off-white to yellowish, round, biconvex, each having a diameter of approximately 2.1 mm.
4 CONTRAINDICATIONS
Lamisil (terbinafine hydrochloride) Oral Granules are contraindicated in individuals with a history of allergic reaction to oral terbinafine because of the risk of anaphylaxis.
5 WARNINGS AND PRECAUTIONS
5.1 Hepatotoxicity
Cases of liver failure, some leading to liver transplant or death, have occurred with the use of oral terbinafine during postmarketing experience in individuals with and without preexisting liver disease. In the majority of liver cases reported in association with oral terbinafine use, the patients had serious underlying systemic conditions. The severity of hepatic events and/or their outcome may be worse in patients with active or chronic liver disease. Treatment with Lamisil Oral Granules should be discontinued if biochemical or clinical evidence of liver injury develops.
Lamisil Oral Granules are not recommended for patients with chronic or active liver disease. Before prescribing Lamisil Oral Granules, liver function tests should be performed since hepatotoxicity may occur in patients with and without pre-existing liver disease. Periodic monitoring of liver function tests is recommended. Lamisil Oral Granules should be immediately discontinued in case of elevation of liver function tests. Patients prescribed Lamisil Oral Granules and/or their guardians should be warned to report immediately to their physician any symptoms of persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain or jaundice, dark urine, or pale stools. Patients with these symptoms should discontinue taking Lamisil Oral Granules, and the patient’s liver function should be immediately evaluated.
5.2 Taste Disturbance Including Loss of Taste
Taste disturbance, including taste loss, has been reported with the use of oral terbinafine. It can be severe enough to result in decreased food intake, weight loss, anxiety, and depressive symptoms. Taste disturbance may resolve within several weeks after discontinuation of treatment, but may be prolonged (greater than 1 year), or may be permanent. If symptoms of a taste disturbance occur, Lamisil Oral Granules should be discontinued.
5.3 Smell Disturbance Including Loss of Smell
Smell disturbance, including loss of smell, has been reported with the use of oral terbinafine. Smell disturbance may resolve after discontinuation of treatment, but may be prolonged (greater than one year), or may be permanent. If symptoms of a smell disturbance occur, Lamisil Oral Granules should be discontinued.
5.4 Depressive Symptoms
Depressive symptoms have occurred during postmarketing use of oral terbinafine. Prescribers should be alert to the development of depressive symptoms, and patients should be instructed to report depressive symptoms to their physician.
5.5 Hematologic Effects
Transient decreases in absolute lymphocyte counts (ALCs) have been observed in controlled clinical trials. In placebo-controlled trials, 8/465 subjects receiving Lamisil Tablets (1.7%) and 3/137 subjects receiving placebo (2.2%) had decreases in ALC to below 1000/mm3 on 2 or more occasions. In patients with known or suspected immunodeficiency, physicians should consider monitoring complete blood counts if treatment continues for more than 6 weeks. Cases of severe neutropenia have been reported. These were reversible upon discontinuation of oral terbinafine, with or without supportive therapy. If clinical signs and symptoms suggestive of secondary infection occur, a complete blood count should be obtained. If the neutrophil count is ≤1000 cells/mm3, Lamisil Oral Granules should be discontinued and supportive management started.
5.6 Serious Skin/Hypersensitivity Reactions
There have been postmarketing reports of serious skin/hypersensitivity reactions [e.g., Stevens-Johnson Syndrome, toxic epidermal necrolysis, erythema multiforme, exfoliative dermatitis, bullous dermatitis, and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome] with oral terbinafine. Manifestations of DRESS syndrome may include cutaneous reaction (such as rash or exfoliative dermatitis), eosinophilia, and one or more organ complications such as hepatitis, pneumonitis, nephritis, myocarditis, and pericarditis. If progressive skin rash or signs/symptoms of the above drug reactions occur, treatment with Lamisil Oral Granules should be discontinued.
5.7 Lupus Erythematosus
During postmarketing experience, precipitation and exacerbation of cutaneous and systemic lupus erythematosus have been reported in patients taking oral terbinafine. Therapy should be discontinued in patients with clinical signs and symptoms suggestive of lupus erythematosus.
5.8 Laboratory Monitoring
Measurement of serum transaminases (ALT and AST) is advised for all patients before taking Lamisil Oral Granules.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Lamisil (terbinafine hydrochloride) Oral Granules
The data described below reflect exposure to terbinafine including 1042 subjects exposed for a median of 42 days. Lamisil Oral Granules was studied in 2 active-controlled trials (n=1042). The population was children aged 4 to 12 years old, 64% male and 36% female, 21% Caucasian, 47% Black, 32% Other. Baseline disease (dermatophyte) characteristics of subjects included 49% having T. tonsurans, 15% T. violaceum, 15% M. canis, 2% M. audouinii, and 1% others. Subjects received once daily, for 6 weeks, oral doses of Lamisil Oral Granules based on body weight: <25 kg 125 mg/day, 25-35 kg 187.5 mg/day, and >35 kg 250 mg/day.
Adverse events reported in the 2 trials are listed in the table below.
| Lamisil Oral Granules (%) N=1042 |
Griseofulvin Oral Suspension (%) N=507 |
|
| Nasopharyngitis | 10 | 11 |
| Headache | 7 | 8 |
| Pyrexia | 7 | 6 |
| Cough | 6 | 5 |
| Vomiting | 5 | 5 |
| Upper respiratory tract infection | 5 | 5 |
| Upper abdominal pain | 4 | 4 |
| Diarrhea | 3 | 4 |
| Influenza | 2 | 1 |
| Abdominal pain | 2 | 1 |
| Pharyngolaryngeal pain | 2 | 2 |
| Nausea | 2 | 2 |
| Rash | 2 | 2 |
| Rhinorrhea | 2 | 0 |
| Nasal congestion | 2 | 1 |
| Pruritus | 1 | 1 |
| Toothache | 1 | 1 |
In the pooled pivotal trials, 2% (17/1042) of subjects in the terbinafine group and 2% (6/507) in the griseofulvin group experienced discontinuation of study drug due to adverse events. The most common categories of adverse events causing discontinuation in those exposed to terbinafine included gastrointestinal disorders, skin and subcutaneous disorders, and infections and infestations.
No ophthalmologic safety signal was identified in the pooled pivotal trials. Ophthalmologic assessments included dilated fundoscopy to assess for refractile bodies in the retina, visual acuity assessment, and color vision testing. Of the 940 subjects in the terbinafine group and 471 subjects in the griseofulvin group who completed dilated fundoscopy at posttreatment visits, none of the subjects were found to have refractile bodies of the retina at baseline or end of treatment. For visual acuity, 1% (11/837) of subjects treated with terbinafine and 2% (7/426) of subjects treated with griseofulvin showed a doubling of visual angle after 6 weeks of treatment, while 2% (15/837) treated with terbinafine and 3% (12/426) treated with griseofulvin showed a halving of the visual angle after 6 weeks of treatment. Of subjects who completed yellow-blue color vision assessment for acquired defects, 5% (13/262) of subjects treated with terbinafine and 6% (8/129) of subjects treated with griseofulvin had color confusion on more than 1 symbol at week 6 than at baseline, while 13% (33/262) of subjects treated with terbinafine and 13% (17/129) of subjects treated with griseofulvin identified more symbols correctly at week 6 than at baseline.
Lamisil (terbinafine hydrochloride) Tablets
Adverse events reported in three US/Canadian placebo-controlled trials included diarrhea (6%), rashes (6%), dyspepsia (4%), nausea (3%), liver abnormalities (3%), pruritus (3%), taste disturbances (3%), abdominal pain (2%), and urticaria (1%).
Changes in the ocular lens and retina have been reported following the use of Lamisil Tablets in clinical trials in adult subjects with onychomycosis. The clinical significance of these changes is unknown.
6.2 Postmarketing Experience
The following adverse events have been identified during postapproval use of oral terbinafine. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: Pancytopenia, agranulocytosis, severe neutropenia, thrombocytopenia, anemia [see Warnings and Precautions (5.5)]
Immune system disorders: Serious hypersensitivity reactions e.g., angioedema and allergic reactions (including anaphylaxis), precipitation and exacerbation of cutaneous and systemic lupus erythematosus [see Warnings and Precautions (5.7)], serum sickness-like reaction
Psychiatric disorders: Anxiety and depressive symptoms independent of taste disturbance have been reported with oral terbinafine use. In some cases, depressive symptoms have been reported to subside with discontinuance of therapy and to recur with reinstitution of therapy [see Warnings and Precautions (5.4)].
Nervous system disorders: Cases of taste disturbance, including taste loss, have been reported with the use of oral terbinafine. It can be severe enough to result in decreased food intake, weight loss, anxiety, and depressive symptoms. Cases of smell disturbance, including smell loss, have been reported with the use of oral terbinafine [see Warnings and Precautions (5.2, 5.3)]. Cases of paresthesia and hypoesthesia have been reported with the use of oral terbinafine.
Eye disorders: Visual field defects, reduced visual acuity
Ear and labyrinth disorders: Hearing impairment, vertigo, tinnitus
Vascular disorders: Vasculitis
Gastrointestinal disorders: Pancreatitis, vomiting
Hepatobiliary disorders: Cases of liver failure some leading to liver transplant or death [see Warnings and Precautions (5.1)], idiosyncratic and symptomatic hepatic injury. Cases of hepatitis, cholestasis, and increased hepatic enzymes [see Warnings and Precautions (5.1)] have been seen with the use of oral terbinafine.
Skin and subcutaneous tissue disorders: Serious skin reactions [e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, exfoliative dermatitis, bullous dermatitis, and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome] [see Warnings and Precautions (5.6)], acute generalized exanthematous pustulosis, psoriasiform eruptions or exacerbation of psoriasis, photosensitivity reactions, hair loss
Musculoskeletal and connective tissue disorders: Rhabdomyolysis, arthralgia, myalgia
General disorders and administration site conditions: Malaise, fatigue, influenza-like illness, pyrexia
Investigations: Altered prothrombin time (prolongation and reduction) in patients concomitantly treated with warfarin and increased blood creatine phosphokinase have been reported
7 DRUG INTERACTIONS
7.1 Drug-Drug Interactions
In vivo studies have shown that terbinafine is an inhibitor of the CYP450 2D6 isozyme. Drugs predominantly metabolized by the CYP450 2D6 isozyme include the following drug classes: tricyclic antidepressants, selective serotonin reuptake inhibitors, beta-blockers, antiarrhythmics class 1C (e.g., flecainide and propafenone) and monoamine oxidase inhibitors Type B. Coadministration of Lamisil (terbinafine hydrochloride) Oral Granules should be done with careful monitoring and may require a reduction in dose of the 2D6-metabolized drug. In a study to assess the effects of terbinafine on desipramine in healthy volunteers characterized as normal metabolizers, the administration of terbinafine resulted in a 2-fold increase in Cmax and a 5-fold increase in area under the curve (AUC). In this study, these effects were shown to persist at the last observation at 4 weeks after discontinuation of Lamisil. In studies in healthy subjects characterized as extensive metabolizers of dextromethorphan (antitussive drug and CYP2D6 probe substrate), terbinafine increases the dextromethorphan/dextrorphan metabolite ratio in urine by 16- to 97-fold, on average. Thus, terbinafine may convert extensive CYP2D6 metabolizers to poor metabolizer status.
In vitro studies with human liver microsomes showed that terbinafine does not inhibit the metabolism of tolbutamide, ethinylestradiol, ethoxycoumarin, cyclosporine, cisapride and fluvastatin.
In vivo drug-drug interaction studies conducted in healthy volunteer subjects showed that terbinafine does not affect the clearance of antipyrine or digoxin. Terbinafine decreases the clearance of caffeine by 19%. Terbinafine increases the clearance of cyclosporine by 15%.
The influence of terbinafine on the pharmacokinetics of fluconazole, cotrimoxazole (trimethoprim and sulfamethoxazole), zidovudine or theophylline was not considered to be clinically significant.
Coadministration of a single dose of fluconazole (100 mg) with a single dose of terbinafine resulted in a 52% and 69% increase in terbinafine Cmax and AUC, respectively. Fluconazole is an inhibitor of CYP2C9 and CYP3A enzymes. Based on this finding, it is likely that other inhibitors of both CYP2C9 and CYP3A4 (e.g., ketoconazole, amiodarone) may also lead to a substantial increase in the systemic exposure (Cmax and AUC) of terbinafine when concomitantly administered.
There have been spontaneous reports of increase or decrease in prothrombin times in patients concomitantly taking oral terbinafine and warfarin, however, a causal relationship between terbinafine and these changes has not been established.
Terbinafine clearance is increased 100% by rifampin, a CYP450 enzyme inducer, and decreased 33% by cimetidine, a CYP450 enzyme inhibitor. Terbinafine clearance is unaffected by cyclosporine. There is no information available from adequate drug-drug interaction studies with the following classes of drugs: oral contraceptives, hormone replacement therapies, hypoglycemics, phenytoins, thiazide diuretics, and calcium channel blockers.
7.2 Food Interactions
An evaluation of the effect of food on Lamisil (terbinafine hydrochloride) Oral Granules was not conducted. However, in the clinical trials, Lamisil (terbinafine hydrochloride) Oral Granules was administered with food [see Dosage and Administration (2)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, and because treatment of tinea capitis can be postponed until after pregnancy is completed, it is recommended that Lamisil (terbinafine hydrochloride) Oral Granules not be initiated during pregnancy.
Oral reproduction studies have been performed in rabbits and rats at doses up to 300 mg/kg/day [12x to 23x the Maximum Recommended Human Dose (MRHD), in rabbits and rats, respectively, based on body surface area (BSA) comparisons] and have revealed no evidence of impaired fertility or harm to the fetus due to terbinafine.
8.3 Nursing Mothers
After oral administration, terbinafine is present in breast milk of nursing mothers. The ratio of terbinafine in milk to plasma is 7:1. Treatment with Lamisil Oral Granules is not recommended in women who are nursing.
8.4 Pediatric Use
Lamisil Oral Granules was studied in 2 randomized, active-controlled trials in which 1021 subjects, 4 to 12 years old, having a clinical diagnosis of tinea capitis confirmed by potassium hydroxide (KOH) microscopy were treated with Lamisil Oral Granules at the labeled dose for up to 6 weeks. The most common adverse events were nasopharyngitis, headache, pyrexia, cough, vomiting, and upper respiratory tract infection [see Adverse Reactions (6.1)].
8.5 Geriatric Use
Lamisil Oral Granules has not been studied in geriatric patients.
8.6 Renal Impairment
In patients with renal impairment (creatinine clearance less than or equal to 50 mL/min) the use of Lamisil Oral Granules has not been adequately studied.
10 OVERDOSAGE
Clinical experience regarding overdose with oral terbinafine is limited. Doses up to 5 grams in adults (20 times the therapeutic daily adult dose) have been reported without inducing serious adverse reactions. The symptoms of overdose included nausea, vomiting, abdominal pain, dizziness, rash, frequent urination, and headache.
11 DESCRIPTION
Lamisil (terbinafine hydrochloride) Oral Granules 125 mg and 187.5 mg contain the synthetic allylamine antifungal compound, terbinafine hydrochloride.
Chemically, terbinafine hydrochloride is (E)-N-(6,6-dimethyl-2-hepten-4-ynyl)-N-methyl-1-naphthalenemethanamine hydrochloride. It has the empirical formula C21H26ClN with a molecular weight of 327.90, and the following structural formula:
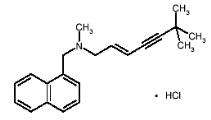
Terbinafine hydrochloride is a white to off-white fine crystalline powder. It is freely soluble in methanol and methylene chloride, soluble in ethanol, and slightly soluble in water.
Each packet of Lamisil Oral Granules contains:
Active Ingredients: terbinafine hydrochloride (equivalent to 125 mg or 187.5 mg terbinafine base)
Inactive Ingredients: basic butylated methacrylate copolymer, colloidal silicon dioxide NF, dibutyl sebacate NF, hypromellose USP, magnesium stearate NF, microcrystalline cellulose NF, nitrogen NF (filling gas), polyethylene glycol NF, sodium lauryl sulfate NF, and sodium starch glycolate NF.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Terbinafine is an allylamine antifungal [see Clinical Pharmacology (12.4)].
12.2 Pharmacodynamics
The pharmacodynamics of Lamisil (terbinafine hydrochloride) Oral Granules is unknown.
12.3 Pharmacokinetics
The pharmacokinetics in children 4 to 8 years of age with tinea capitis was investigated in a pharmacokinetic study after single and repeated (for 42 days) oral administration of Lamisil Oral Granules (N=16), once daily, using the body weight groups and doses described in Section 2. The systemic exposure (Cmax and AUC0-24) of terbinafine in children had a relatively high interindividual variability (ranging from 36% to 64%). At steady state the AUC0-24 increased by a mean factor of 1.9 to 2.1 across doses. The mean (SD) effective half-life obtained from the observed accumulation was 26.7 (13.8) hours and 30.5 (9.3) hours for the 125 mg and 187.5 mg doses, respectively.
Systemic exposure to terbinafine in the children did not exceed the highest values of the systemic exposure in adults receiving repeated once daily doses of 250 mg Lamisil (terbinafine hydrochloride) Tablets. A population pharmacokinetic evaluation of oral terbinafine that included children 4-12 years of age and adults 18-45 years of age (N=113) found that clearance (CL/F) of terbinafine is dependent on body weight in a nonlinear manner. For a typical child of 25 kg CL/F was predicted to be 19 L/h and for a typical adult of 70 kg body weight it was predicted to be 27 L/h. Over the weight range for pediatric patients included in the analysis (14.1 kg-68 kg), the predicted CL/F ranged between 15.6-26.7 L/hr. In plasma, terbinafine is >99% bound to plasma proteins. Prior to excretion, terbinafine is rapidly and extensively metabolized by at least 7 CYP isoenzymes with major contributions from CYP2C9, CYP1A2, CYP3A4, CYP2C8, and CYP2C19. No metabolites have been identified that have antifungal activity similar to terbinafine. Approximately 70% of the administered dose is eliminated in the urine. In adult patients with renal impairment (creatinine clearance ≤50 mL/min) or hepatic cirrhosis, the clearance of terbinafine is decreased by approximately 50% compared to normal volunteers.
12.4 Microbiology
Terbinafine, an allylamine antifungal, inhibits biosysnthesis of ergosterol, an essential component of fungal cell membrane, via inhibition of squalene epoxidase enzyme. This results in fungal cell death primarily due to the increased membrane permeability mediated by the accumulation of high concentrations of squalene but not due to ergosterol deficiency. Depending on the concentration of the drug and the fungal species tested in vitro, terbinafine may be fungicidal. However, the clinical significance of in vitro data is unknown.
Lamisil Oral Granules has been studied in tinea capitis [see Clinical Studies (14)].
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 28-month oral carcinogenicity study in rats, an increase in the incidence of liver tumors was observed in males at the highest dose tested, 69 mg/kg/day (2x the MRHD based on AUC comparisons of the parent terbinafine); however, even though dose-limiting toxicity was not achieved at the highest tested dose, higher doses were not tested.
The results of a variety of in vitro (mutations in E. coli and S. typhimurium, DNA repair in rat hepatocytes, mutagenicity in Chinese hamster fibroblasts, chromosome aberration and sister chromatid exchanges in Chinese hamster lung cells), and in vivo (chromosome aberration in Chinese hamsters, micronucleus test in mice) genotoxicity tests gave no evidence of a mutagenic or clastogenic potential.
Oral reproduction studies in rats at doses up to 300 mg/kg/day (approximately 12x the MRHD based on BSA comparisons) did not reveal any specific effects on fertility or other reproductive parameters. Intravaginal application of terbinafine hydrochloride at 150 mg/day in pregnant rabbits did not increase the incidence of abortions or premature deliveries nor affect fetal parameters.
13.2 Animal Toxicology and/or Pharmacology
A wide range of in vivo studies in mice, rats, dogs, and monkeys, and in vitro studies using rat, monkey, and human hepatocytes suggest that peroxisome proliferation in the liver is a rat-specific finding. However, other effects, including increased liver weights and APTT, occurred in dogs and monkeys at doses giving Css trough levels of the parent terbinafine 2-3x those seen in humans at the MRHD. Higher doses were not tested.
In a 52-week oral toxicology study conducted in juvenile maturing dogs, increased heart and liver weights were noted in males and signs of CNS disturbance including 3 cases of single episodes of seizures were noted in females at the highest dose tested, 100 mg/kg/day [19x (males) and 10x (females) the MRHD based on AUC comparisons of the parent terbinafine]. No treatment related findings were noted at 30 mg/kg/day [1.6x (males) and 1.9x (females) the MRHD based on AUC comparisons of the parent terbinafine] in this study.
14 CLINICAL STUDIES
Two randomized, multinational trials were conducted to investigate the safety and efficacy of Lamisil (terbinafine hydrochloride) Oral Granules in the treatment of subjects 4 to 12 years old with tinea capitis. Lamisil Oral Granules was dosed based on body weight. Griseofulvin dosed at 10-20 mg/kg was used as a comparator. Subjects were dosed for 6 weeks and followed for an additional 4 weeks.
The 2 trials enrolled 50% of subjects from the U.S. Additionally, among those with positive cultures, 65% and 54% of infections were due to T. tonsurans, and 19% and 17% due to M. canis in Studies 1 and 2, respectively.
The primary efficacy endpoint was the proportion of subjects with complete cure (negative KOH, negative culture, and absence of clinical signs of infection) at week 10. Table 3 below lists the efficacy results for Studies 1 and 2 overall and according to the dermatophyte species (T. tonsurans , M. canis , or Other).
| * T. violaceum, M. audouinii, T. mentagrophytes, T. rubrum, M. gypseum, and M. vanbreuseghemii. | |||||
| Study 1 | Study 2 | ||||
| Terbinafine | Griseofulvin | Terbinafine | Griseofulvin | ||
| All Dermatophytes | (N=411) | (N=197) | (N=441) | (N=237) | |
| Complete Cure | 190 (46.2%) | 67 (34.0%) | 194 (44.0%) | 103 (43.5%) | |
| T. tonsurans | (N=264) | (N=131) | (N=243) | (N=126) | |
| Complete Cure | 148 (56.1%) | 45 (34.4%) | 116 (47.7%) | 46 (36.5%) | |
| M. canis | (N=80) | (N=37) | (N=72) | (N=45) | |
| Complete Cure | 19 (23.8%) | 13 (35.1%) | 22 (30.6%) | 23 (51.1%) | |
| Other * | (N=67) | (N=29) | (N=126) | (N=66) | |
| Complete Cure | 23 (34.2%) | 9 (31.0%) | 56 (44.4%) | 34 (51.5%) | |
16 HOW SUPPLIED/STORAGE AND HANDLING
Lamisil ( terbinafine hydrochloride) Oral Granules 125 mg and 187.5 mg
Lamisil Oral Granules is supplied in cartons containing 14 laminated aluminum packets. Each packet contains approximately either 30 or 45 off-white to yellowish, round, biconvex, film-coated granules, corresponding to a single total dose of 125 mg or 187.5 mg (terbinafine base equivalent) per packet.
125 mg per packet
Carton of 14 packets………..………………………….………..NDC 0078-0499-58
Pack of 3 cartons each containing 14 packets (42 packets).........NDC 0078-0499-59
187.5 mg per packet
Carton of 14 packets………….………………………………....NDC 0078-0500-58
Pack of 3 cartons each containing 14 packets (42 packets)..........NDC 0078-0500-59
Storage conditions of Lamisil Oral Granules 125 mg and 187.5 mg: Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling (Patient Information)
Patients taking Lamisil (terbinafine hydrochloride) Oral Granules should receive the following information and instructions:
- Advise patients and/or their guardian to immediately report to their physician or get emergency help if they experience any of the following symptoms: hives, mouth sores, blistering and peeling of skin, swelling of face, lips, tongue, or throat, difficulty swallowing or breathing. Lamisil Oral Granules treatment should be discontinued.
- Advise patients prescribed Lamisil Oral Granules and/or their guardian to report immediately to their physician any symptoms of persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain, jaundice, dark urine, or pale stools. Lamisil Oral Granules treatment should be discontinued.
- Advise patients and/or their guardian to report to their physician any signs of taste disturbance, smell disturbance, and/or depressive symptoms, fever, skin eruption, lymph node enlargement, erythema, scaling, loss of pigment, and unusual photosensitivity that can result in a rash. Lamisil Oral Granules treatment should be discontinued.
- Advise patients and/or their guardian to minimize exposure to natural and artificial sunlight (tanning beds or UVA/B treatment) while using Lamisil Oral Granules.
- Advise patients and/or their guardian to call their physician if they take too many Lamisil Oral Granules.
T2013-97
October 2013
Patient Information
Lamisil (Lam-i-sil)
(terbinafine hydrochloride)
Oral Granules
What is Lamisil Oral Granules?
Lamisil Oral Granules is a prescription antifungal medicine used to treat an infection of the scalp (tinea capitis) in people 4 years of age and older.
Who should not take Lamisil Oral Granules?
Do not take Lamisil Oral Granules if you are allergic to terbinafine hydrochloride when taken by mouth.
What should I tell my doctor before taking Lamisil Oral Granules?
Before you take Lamisil Oral Granules, tell your doctor if you:
- have or had liver problems
- have a weakened immune system (immunocompromised)
- have lupus (an autoimmune disease)
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if Lamisil Oral Granules will harm your unborn baby. You should not start taking Lamisil during pregnancy without talking to your doctor.
- are breastfeeding or plan to breastfeed. Lamisil can pass into your breast milk and may harm your baby. Talk to your doctor about the best way to feed your baby if you take Lamisil Oral Granules.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Lamisil Oral Granules may affect the way other medicines work and other medicines may affect how Lamisil Oral Granules works. Especially tell your doctor if you take:
- a medicine for depression
- a medicine for high blood pressure
- a medicine for heart problems
- desipramine (Norpramin)
- caffeine
- cyclosporine (Gengraf, Neoral, Sandimmune)
- fluconazole (Diflucan)
- rifampin (Rifater, Rifamate, Rimactane, Rifadine)
- cimetidine (Tagamet)
If you are not sure if your medicine is one listed above, ask your doctor or pharmacist.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take Lamisil Oral Granules?
- Take Lamisil Oral Granules exactly as your doctor tells you to take it.
- Lamisil comes as oral granules that you sprinkle on food and take by mouth.
- Take Lamisil Oral Granules 1 time each day with pudding or other soft, non-acidic food such as mashed potatoes. Do not use applesauce or a fruit-based food.
- Your doctor will tell you how much Lamisil Oral Granules to take and when to take it.
- If 2 packets are required for each dose:
- sprinkle the content of both packets on 1 spoonful of non-acidic food, or
- sprinkle the contents of each packet on 2 separate spoonfuls of non-acidic food.
Giving Lamisil Oral Granules to children and adults:
- Hold packet with cut line on top.
- Shake packet gently to settle contents.
- Tear packet open along cut line, or use scissors to cut across line.
- Carefully pour entire contents of packet onto a spoonful of a soft food, such as pudding or other soft, non-acidic food such as mashed potatoes.
- Make sure that no granules remain in the packet.
- Swallow combination of food and granules without chewing.
- If you take too much Lamisil Oral Granules call your doctor. You may have the following symptoms:
- nausea
- vomiting
- stomach (abdomen) pain
- dizziness
- rash
- frequent urination
- headache
What should I avoid while taking Lamisil Oral Granules?
- Avoid sunlight. Lamisil Oral Granules can make your skin sensitive to the sun and the light from sunlamps and tanning beds. You can get a severe sunburn. Use sunscreen and wear a hat and clothes that cover your skin if you have to be in sunlight. Talk to your doctor if you get sunburn.
What are the possible side effects of Lamisil Oral Granules?
Lamisil Oral Granules may cause serious side effects, including:
-
liver problems that can lead to the need for liver transplant, or death. Tell your doctor right away if you get any of these symptoms of a liver problem:
- nausea
- upper right stomach-area (abdomen) pain
- poor appetite
- yellowing of your skin or eyes (jaundice)
- tiredness
- dark (tea-colored) urine
- vomiting
- pale or light colored stools
Your doctor should do a blood test to check you for liver problems before you take Lamisil Oral Granules.
-
change in taste or loss of taste may happen with Lamisil Oral Granules and can be severe. This may improve within several weeks after you stop taking Lamisil Oral Granules, but may last for a long time or may become permanent. Tell your doctor if you have:
- change in taste or loss of taste
- poor appetite
- unwanted weight loss
- anxiousness
- change in mood or depressive symptoms
- change in smell or loss of smell may happen with Lamisil Oral Granules. This may improve after you stop taking Lamisil Oral Granules, but may last for a long time or may become permanent.
-
depressive symptoms. Tell your doctor right away if you have any of these signs or symptoms:
- feel sad or worthless
- change in sleep pattern
- loss of energy or interest in daily activities
- restlessness
- mood changes
- low white blood cell count. People taking Lamisil Oral Granules may have a decrease in white blood cells, especially neutrophils. You may have a higher risk of getting an infection when your white blood cell count is low.
-
serious skin or allergic reactions. Tell your doctor right away or get emergency help if you get any of these symptoms:
- skin rash, hives, sores in your mouth, or your skin blisters and peels
- swelling of your face, eyes, lips, tongue or throat
- trouble swallowing or breathing
- drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome – skin rash, fever, swollen lymph glands, involvement of internal organs
-
new or worsening lupus (an autoimmune disease). Stop taking Lamisil Oral Granules and tell your doctor if you get any of the following:
- progressive skin rash that is scaly, red, shows scarring, or loss of pigment
- unusual sensitivity to the sun that can lead to a rash
The most common side effects of Lamisil Oral Granules include:
- Nasal congestion
- vomiting
- headache
- upper respiratory tract infection
- fever
- upper stomach-area (abdomen) pain
- cough
- diarrhea
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of Lamisil Oral Granules. For information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Lamisil Oral Granules?
- Store Lamisil Oral Granules at room temperature between 68°F to 77°F (20°C to 25°C).
Keep Lamisil Oral Granules and all medicines out of the reach of children.
General information about the safe and effective use of Lamisil Oral Granules.
Medicines are sometimes prescribed for purposes other than those listed in Patient Information. Do not use Lamisil Oral Granules for a condition for which it was not prescribed. Do not give Lamisil Oral Granules to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or doctor for information about Lamisil Oral Granules that is written for health professionals.
What are the ingredients in Lamisil Oral Granules?
Active ingredient: terabinafine hydrochloride
Inactive ingredients: basic butylated methacrylate copolymer, colloidal silicon dioxide, dibutyl sebacate, hypromellose, magnesium stearate, microcrystalline cellulose, nitrogen (filling gas), polyethylene glycol, sodium lauryl sulfate, sodium starch glycolate
This Patient Information has been approved by the U.S. Food and Drug Administration.
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
© Novartis
T2013-98
October 2013
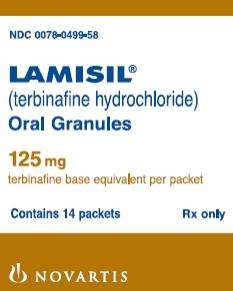
PRINCIPAL DISPLAY PANEL
Package Label – 125 mg
Rx Only NDC 0078-0499-58
Lamisil® (terbinafine hydrochloride)
Oral Granules
125 mg
terbinafine base equivalent per packet
Contains 14 packets
PRINCIPAL DISPLAY PANEL
Package Label – 187.5 mg
Rx Only NDC 0078-0500-58
Lamisil® (terbinafine hydrochloride)
Oral Granules
187.5 mg
terbinafine base equivalent per packet
Contains 14 packets

Lamisilterbinafine hydrochloride GRANULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Lamisilterbinafine hydrochloride GRANULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||