Levlite
LEVLITE 28 Tablets(levonorgestrel and ethinyl estradiol tablets, USP)
FULL PRESCRIBING INFORMATION: CONTENTS*
- LEVLITE DESCRIPTION
- CLINICAL PHARMACOLOGY
- PHARMACOKINETICS
- LEVLITE INDICATIONS AND USAGE
- LEVLITE CONTRAINDICATIONS
- WARNINGS
- THROMBOEMBOLIC DISORDERS AND OTHER VASCULAR PROBLEMS
- ESTIMATES OF MORTALITY FROM CONTRACEPTIVE USE
- CARCINOMA OF THE REPRODUCTIVE ORGANS
- HEPATIC NEOPLASIA
- OCULAR LESIONS
- ORAL CONTRACEPTIVE USE BEFORE OR DURING EARLY PREGNANCY
- GALLBLADDER DISEASE
- CARBOHYDRATE AND LIPID METABOLIC EFFECTS
- ELEVATED BLOOD PRESSURE
- HEADACHE
- BLEEDING IRREGULARITIES
- PRECAUTIONS
- LEVLITE ADVERSE REACTIONS
- OVERDOSAGE
- NON-CONTRACEPTIVE HEALTH BENEFITS
- LEVLITE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- BRIEF SUMMARY PATIENT PACKAGE INSERT
FULL PRESCRIBING INFORMATION
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Rx only
LEVLITE DESCRIPTION
Each cycle of LEVLITE® 28 (levonorgestrel and ethinyl estradiol tablets, USP) consists of 21 pink active tablets each containing 0.100 mg levonorgestrel and 0.020 mg ethinyl estradiol; and seven white tablets—inert. The inactive ingredients are Calcium Carbonate USP, Corn Starch NF, Ferric Oxide/red/E 172 NF, Ferric Oxide/yellow/E 172 NF, Glycerin 85% Ph. Eur./DAB, Lactose Monohydrate NF, Magnesium Stearate NF, Montanglycol Wax (Wax E) DAB, Polyethylene glycol 6,000 NF, Povidone 25,000 USP, Povidone 700,000 USP, Pregelatinized Starch NF (Modified Starch), Sucrose NF, Talc USP and Titanium Dioxide, E 171 USP.
Levonorgestrel has a molecular weight of 312.4 and a molecular formula of C21H28O2. Ethinyl estradiol has a molecular weight of 296.4 and a molecular formula of C20H24O2. The structural formulas are as follows:

CLINICAL PHARMACOLOGY
Combination oral contraceptives act by suppression of gonadotropins. Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus (which increase the difficulty of sperm entry into the uterus) and the endometrium (which reduce the likelihood of implantation).
PHARMACOKINETICS
Absorption
No specific investigation of the absolute bioavailability of levonorgestrel and ethinyl estradiol of LEVLITE in humans has been conducted. However, literature indicates that levonorgestrel is rapidly and completely absorbed after oral administration and is not subject to first-pass metabolism. Ethinyl estradiol is rapidly and almost completely absorbed from the gastrointestinal tract but, due to first-pass metabolism in gut mucosa and liver, the absolute bioavailability of ethinyl estradiol is about 40%.
After a single dose of three LEVLITE Tablets to 17 women under fasting conditions, the extents of absorption of levonorgestrel and ethinyl estradiol were 98.6% and 99.0%, respectively, relative to the same dose of the 2 drugs when given as a microcrystalline suspension in water. The effect of food on the bioavailability of LEVLITE Tablets following oral administration has not been evaluated.
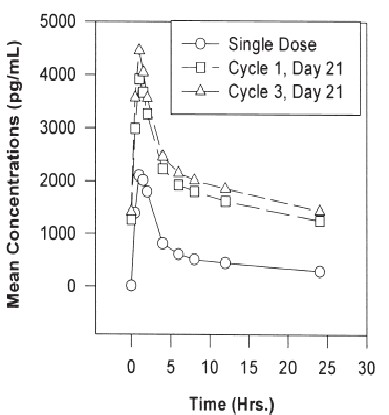
The pharmacokinetics of levonorgestrel and ethinyl estradiol following daily administration of LEVLITE Tablets for 21 days per cycle for three cycles, were determined in 18 women. Estimates of the pharmacokinetic parameters of levonorgestrel and ethinyl estradiol following single and multiple dose administration of LEVLITE Tablets are summarized in Table I. Mean levonorgestrel and ethinyl estradiol levels after a single dose and on day 21 at steady state are shown in Figure I.
The pharmacokinetics of total levonorgestrel are non-linear due to an increase in binding to SHBG, which is attributed to increased SHBG levels that are induced by the daily administration of ethinyl estradiol. Increased binding of levonorgestrel to SHBG leads to decreased clearance of levonorgestrel. Observed maximum levonorgestrel concentrations increased from day 1 to day 21 of the 1st and 3rd cycles by 66% and 83%, respectively.
In calculating the mean concentration for ethinyl estradiol, any individual subject value below the quantifiable limit (i.e., 20 pg/mL) was converted to 0; and the 0 values were included for calculation of the mean concentration. Table I provides a summary of levonorgestrel and ethinyl estradiol pharmacokinetic parameters.
| Levonorgestrel | ||||||
Day (cycle) | Cmax | tmax | AUC | CL/F | Vz | SHBG nmol/L |
| 1 | 2.36 (0.79) | 1.3 (0.4) | 29.2 (10.0) | 1.0 (0.3) | 129 (46) | 64.5 (22.0) |
AUC (0-24h) ng•h/mL | ||||||
| 21 (1) | 4.04 (2.08) | 1.0 (0.3) | 43.8 (22.4) | 0.73 (0.34) | 106 (42) | 94.7 (37.4) |
| 21 (3) | 4.53 (1.94) | 1.0 (0.3) | 49.5 (24.5) | 0.65 (0.33) | 96 (35) | 107.4 (45.8) |
| Ethinyl Estradiol | |||
Day (cycle) | Cmax | tmax | AUC(0-24) |
| 1 | 49.5 (13.4) | 1.5 (0.4) | 298 (215) |
| 21 (1) | 66.2 (29.5) | 1.4 (0.4) | 596 (494) |
| 21 (3) | 58.1 (19.3) | 1.4 (0.3) | 417 (289) |
Distribution
Levonorgestrel in serum is primarily bound to SHBG. Protein binding values for levonorgestrel are provided in Table II. Ethinyl estradiol is about 97% bound to plasma albumin. Ethinyl estradiol does not bind to SHBG, but induces SHBG synthesis.
| Parameter | Single Dose | Cycle 2 | Cycle 4 |
| % free | 1.11 (0.27) | 0.79 (0.22) | 0.80 (0.23) |
| % SHBG-bound | 64.5 (8.54) | 75.6 (6.59) | 74.7 (7.89) |
| % albumin-bound | 34.4 (8.28) | 23.6 (6.41) | 24.5 (7.67) |
Metabolism
Levonorgestrel
The most important metabolic pathway occurs in the reduction of the Δ4-3-oxo group and hydroxylation at positions 2α, 1β, and 16β, followed by conjugation. Most of the metabolites that circulate in the blood are sulfates of 3α, 5β-tetrahydro-levonorgestrel, while excretion occurs predominantly in the form of glucuronides. Some of the parent levonorgestrel also circulates as 17β-sulfate. Metabolic clearance rates may differ among individuals by several-fold, and this may account in part for the wide variation in levonorgestrel concentrations among users.
Ethinyl estradiol
Cytochrome P450 enzymes (CYP3A4) in the liver are responsible for the 2-hydroxylation that is the major oxidative reaction. The 2-hydroxy metabolite is further transformed by methylation and glucuronidation prior to urinary and fecal excretion. Levels of Cytochrome P450 (CYP3A) vary widely among individuals and can explain the variation in the rates of ethinyl estradiol 2-hydroxylation. Ethinyl estradiol is excreted in the urine and feces as glucuronide and sulfate conjugates and undergoes enterohepatic circulation.
Excretion
The elimination half-life for levonorgestrel after a single dose of LEVLITE® is 25.4 ± 9.7 hours. Levonorgestrel and its metabolites are primarily excreted in the urine. The elimination half-life of ethinyl estradiol has been reported to be between 15 and 25 hours.
SPECIAL POPULATIONS
Hepatic Insufficiency
No formal studies have evaluated the effect of hepatic disease on the disposition of LEVLITE. However, steroid hormones may be poorly metabolized in patients with impaired liver function.
Renal Insufficiency
No formal studies have evaluated the effect of renal disease on the disposition of LEVLITE.
Drug-Drug Interactions
Interactions between ethinyl estradiol and other drugs have been reported in the literature.
Interactions with Absorption. Diarrhea may increase gastrointestinal motility and reduce hormone absorption. Similarly, any drug which reduces gut transit time may reduce hormone concentrations in the blood.
Interactions with Metabolism
Gastrointestinal Wall
Sulfation of ethinyl estradiol has been shown to occur in the gastrointestinal wall. Therefore, drugs which act as competitive inhibitors for sulfation in the gastrointestinal wall may increase ethinyl estradiol bioavailability.
Hepatic metabolism
Interactions can occur with drugs that induce microsomal enzymes which can decrease ethinyl estradiol concentrations (e.g., rifampin, barbiturates, phenylbutazone, phenytoin, griseofulvin).
Interference with Enterohepatic Circulation
Some clinical reports suggest that enteroheptic circulation of estrogens may decrease when certain antibiotic agents are given, which may reduce ethinyl estradiol concentrations (e.g., ampicillin, tetracycline).
Interference in the Metabolism of Other Drugs
Ethinyl estradiol may interfere with the metabolism of other drugs by inhibiting hepatic microsomal enzymes or by inducing hepatic drug conjugation, particularly glucuronidation. Accordingly, plasma and tissue concentrations may either be increased or decreased, respectively (e.g., cyclosporin, theophylline).
LEVLITE INDICATIONS AND USAGE
Oral contraceptives are indicated for the prevention of pregnancy in women who elect to use this product as a method of contraception.
Oral contraceptives are highly effective. Table III lists the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
| Source: Trussell J, Contraceptive efficacy. In Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Kowal D, Guest F, Contraceptive Technology: Seventeenth Revised Edition. New York NY: Irvington Publishers, 1998. | |||
% of Women Experiencing an Accidental Pregnancy within the First Year of Use | % of Women Continuing Use at One Year | ||
Method (1) | Typical Use | Perfect Use | (4) |
Chance  | 85 | 85 | |
Spermicides | 26 | 6 | 40 |
| Periodic abstinence | 25 | 63 | |
| Calendar | 9 | ||
| Ovulation method | 3 | ||
Sympto-thermal | 2 | ||
| Post Ovulation | 1 | ||
| Withdrawal | 19 | 4 | |
Cap | |||
| Parous women | 40 | 26 | 42 |
| Nulliparous women | 20 | 9 | 56 |
Sponge | |||
| Parous women | 40 | 20 | 42 |
| Nulliparous women | 20 | 9 | 56 |
Diaphragm | 20 | 6 | 56 |
Condom | |||
| Female (Reality) | 21 | 5 | 56 |
| Male | 14 | 3 | 61 |
| Pill | 5 | 71 | |
| progestin only | 0.5 | ||
| combined | 0.1 | ||
IUD | |||
| Progesterone T | 2 | 1.5 | 81 |
| Copper T 380A | 0.8 | 0.6 | 78 |
| Lng 20 | 0.1 | 0.1 | 81 |
| Depo Provera | 0.3 | 0.3 | 70 |
| Norplant and Norplant-2 | 0.05 | 0.05 | 88 |
| Female sterilization | 0.5 | 0.5 | 100 |
| Male sterilization | 0.15 | 0.10 | 100 |
LEVLITE CONTRAINDICATIONS
Oral contraceptives should not be used in women who currently have the following conditions:
- Thrombophlebitis or thromboembolic disorders
- A past history of deep-vein thrombophlebitis or thromboembolic disorders
- Cerebral-vascular or coronary-artery disease
- Known or suspected carcinoma of the breast
- Carcinoma of the endometrium or other known or suspected estrogen-dependent neoplasia
- Undiagnosed abnormal genital bleeding
- Cholestatic jaundice of pregnancy or jaundice with prior pill use
- Hepatic adenomas or carcinomas
- Known or suspected pregnancy
WARNINGS
Cigarette smoking increases the risk of serious cardiovascular side effects from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should be strongly advised not to smoke.
THROMBOEMBOLIC DISORDERS AND OTHER VASCULAR PROBLEMS
Myocardial infarction
An increased risk of myocardial infarction has been attributed to oral contraceptive use. This risk is primarily in smokers or women with other underlying risk factors for coronary-artery disease such as hypertension, hypercholesterolemia, morbid obesity, and diabetes. The relative risk of heart attack for current oral contraceptive users has been estimated to be two to six. The risk is very low under the age of 30.
Smoking in combination with oral contraceptive use has been shown to contribute substantially to the incidence of myocardial infarctions in women in their mid-thirties or older with smoking accounting for the majority of excess cases. Mortality rates associated with circulatory disease have been shown to increase substantially in smokers over the age of 35 and nonsmokers over the age of 40 (Table IV) among women who use oral contraceptives.
| Adapted from P.M. Layde and V. Beral | ||||
| AGE | EVER- USERS NON- SMOKERS | EVER- USERS SMOKERS | CONTROLS NON- SMOKERS | CONTROL SMOKERS |
| 15–24 | 0.0 | 10.5 | 0.0 | 0.0 |
| 25–34 | 4.4 | 14.2 | 2.7 | 4.2 |
| 35–44 | 21.5 | 63.4 | 6.4 | 15.2 |
| 45+ | 52.4 | 206.7 | 11.4 | 27.9 |
Oral contraceptives may compound the effects of well-known risk factors, such as hypertension, diabetes, hyperlipidemias, age and obesity. ln particular, some progestogens are known to decrease HDL cholesterol and cause glucose intolerance, while estrogens may create a state of hyperinsulinism. Oral contraceptives have been shown to increase blood pressure among users (see section 9 in "WARNINGS"). Similar effects on risk factors have been associated with an increased risk of heart disease. Oral contraceptives must be used with caution in women with cardiovascular disease risk factors.
Thromboembolism
An increased risk of thromboembolic and thrombotic disease associated with the use of oral contraceptives is well established. Case control studies have found the relative risk of users compared to nonusers to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease. Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases and about 4.5 for new cases requiring hospitalization. The risk of thromboembolic disease due to oral contraceptives is not related to length of use and disappears after pill use is stopped.
A two- to four-fold increase in the relative risk of post-operative thromboembolic complications has been reported with the use of oral contraceptives. The relative risk of venous thrombosis in women who have predisposing conditions is twice that of women without such medical conditions. If feasible, oral contraceptives should be discontinued from at least four weeks prior to and for two weeks after elective surgery of a type associated with an increase in risk of thromboembolism and during and following prolonged immobilization. Since the immediate postpartum period is also associated with an increased risk of thromboembolism, oral contraceptives should be started no earlier than four to six weeks after delivery in women who elect not to breast-feed.
Cerebrovascular diseases
Oral contraceptives have been shown to increase both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes), although, in general, the risk is greatest among older (>35 years), hypertensive women who also smoke. Hypertension was found to be a risk factor, for both users and nonusers, for both types of strokes, while smoking interacted to increase the risk for hemorrhagic strokes.
ln a large study, the relative risk of thrombotic strokes has been shown to range from 3 for normotensive users to 14 for users with severe hypertension. The relative risk of hemorrhagic stroke is reported to be 1.2 for nonsmokers who used oral contraceptives, 2.6 for smokers who did not use oral contraceptives, 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users and 25.7 for users with severe hypertension. The attributable risk is also greater in older women.
Dose-related risk of vascular disease from oral contraceptives
A positive association has been observed between the amount of estrogen and progestogen in oral contraceptives and the risk of vascular disease. A decline in serum high-density lipoproteins (HDL) has been reported with many progestational agents. A decline in serum high-density lipoproteins has been associated with an increased incidence of ischemic heart disease. Because estrogens increase HDL cholesterol, the net effect of an oral contraceptive depends on a balance achieved between doses of estrogen and progestogen and the nature and absolute amount of progestogen used in the contraceptive. The amount of both hormones should be considered in the choice of an oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular estrogen/progestogen combination, the dosage regimen prescribed should be one which contains the least amount of estrogen and progestogen that is compatible with a low failure rate and the needs of the individual patient. New acceptors of oral contraceptive agents should be started on preparations containing the lowest estrogen content which provides satisfactory results in the individual.
Persistence of risk of vascular disease
There are two studies which have shown persistence of risk of vascular disease for ever-users of oral contraceptives. ln a study in the United States, the risk of developing myocardial infarction after discontinuing oral contraceptives persists for at least 9 years for women aged 40 to 49 years who had used oral contraceptives for five or more years, but this increased risk was not demonstrated in other age groups. ln another study in Great Britain, the risk of developing cerebrovascular disease persisted for at least 6 years after discontinuation of oral contraceptives, although excess risk was very small. However, both studies were performed with oral contraceptive formulations containing 50 micrograms or higher of estrogens.
ESTIMATES OF MORTALITY FROM CONTRACEPTIVE USE
One study gathered data from a variety of sources which have estimated the mortality rate associated with different methods of contraception at different ages (Table V). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that with the exception of oral contraceptive users 35 and older who smoke and 40 and older who do not smoke, mortality associated with all methods of birth control is less than that associated with childbirth.
The observation of a possible increase in risk of mortality with age for oral contraceptive users is based on data gathered in the 1970's—but not reported until 1983. However, current clinical practice involves the use of lower estrogen dose formulations combined with careful restriction of oral contraceptive use to women who do not have the various risk factors listed in this labeling.
Because of these changes in practice and, also, because of some limited new data which suggest that the risk of cardiovascular disease with the use of oral contraceptives may now be less than previously observed, the Fertility and Maternal Health Drugs Advisory Committee was asked to review the topic in 1989. The Committee concluded that although cardiovascular disease risks may be increased with oral contraceptive use after age 40 in healthy nonsmoking women (even with the newer low-dose formulations), there are greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures which may be necessary if such women do not have access to effective and acceptable means of contraception.
Therefore, the Committee recommended that the benefits of oral contraceptive use by healthy nonsmoking women over 40 may outweigh the possible risks. Of course, older women, as all women who take oral contraceptives, should take the lowest possible dose formulation that is effective.
| Adapted from H.W. Ory, Family Planning Perspectives, 15:57-63, 1983. | ||||||
| Method of Control and Outcome | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 |
No fertility control methods | 7.0 | 7.4 | 9.1 | 14.8 | 25.7 | 28.2 |
Oral contraceptives nonsmoker | 0.3 | 0.5 | 0.9 | 1.9 | 13.8 | 31.6 |
Oral contraceptives smoker | 2.2 | 3.4 | 6.6 | 13.5 | 51.1 | 117.2 |
lUD | 0.8 | 0.8 | 1.0 | 1.0 | 1.4 | 1.4 |
Condom | 1.1 | 1.6 | 0.7 | 0.2 | 0.3 | 0.4 |
Diaphragm/spermicide | 1.9 | 1.2 | 1.2 | 1.3 | 2.2 | 2.8 |
Periodic abstinence | 2.5 | 1.6 | 1.6 | 1.7 | 2.9 | 3.6 |
CARCINOMA OF THE REPRODUCTIVE ORGANS
Numerous epidemiological studies have been performed on the incidence of breast, endometrial, ovarian and cervical cancer in women using oral contraceptives. The overwhelming evidence in the literature suggests that use of oral contraceptives is not associated with an increase in the risk of developing breast cancer, regardless of the age and parity of first use or with most of the marketed brands and doses. The Cancer and Steroid Hormone (CASH) study also showed no latent effect on the risk of breast cancer for at least a decade following long-term use. A few studies have shown a slightly increased relative risk of developing breast cancer, although the methodology of these studies, which included differences in examination of users and nonusers and differences in age at start of use, has been questioned.
Some studies suggest that oral contraceptive use has been associated with an increase in the risk of cervical intraepithelial neoplasia in some populations of women. However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
ln spite of many studies of the relationship between oral contraceptive use and breast and cervical cancers, a cause-and-effect relationship has not been established.
HEPATIC NEOPLASIA
Benign hepatic adenomas are associated with oral contraceptive use, although the incidence of benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases/100,000 for users, a risk that increases after four or more years of use. Rupture of rare, benign, hepatic adenomas may cause death through intra-abdominal hemorrhage.
Studies from Britain have shown an increased risk of developing hepatocellular carcinoma in long-term (>8 years) oral contraceptive users. However, these cancers are extremely rare in the U.S. and the attributable risk (the excess incidence) of liver cancers in oral contraceptive users approaches less than one per million users.
OCULAR LESIONS
There have been clinical case reports of retinal thrombosis associated with the use of oral contraceptives. Oral contraceptives should be discontinued if there is unexplained partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
ORAL CONTRACEPTIVE USE BEFORE OR DURING EARLY PREGNANCY
Extensive epidemiological studies have revealed no increased risk of birth defects in women who have used oral contraceptives prior to pregnancy. Studies also do not suggest a teratogenic effect, particularly insofar as cardiac anomalies and limb-reduction defects are concerned, when taken inadvertently during early pregnancy.
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion. It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period. Oral contraceptive use should be discontinued if pregnancy is confirmed.
GALLBLADDER DISEASE
Earlier studies have reported an increased lifetime relative risk of gallbladder surgery in users of oral contraceptives and estrogens. More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral contraceptive users may be minimal. The recent findings of minimal risk may be related to the use of oral contraceptive formulations containing lower hormonal doses of estrogens and progestogens.
CARBOHYDRATE AND LIPID METABOLIC EFFECTS
Oral contraceptives have been shown to cause glucose intolerance in a significant percentage of users. Oral contraceptives containing greater than 75 micrograms of estrogens cause hyperinsulinism, while lower doses of estrogen cause less glucose intolerance. Progestogens increase insulin secretion and create insulin resistance, this effect varying with different progestational agents. However, in the nondiabetic woman, oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, prediabetic and diabetic women should be carefully observed while taking oral contraceptives.
A small proportion of women will have persistent hypertriglyceridemia while on the pill. As discussed earlier (see "WARNINGS" 1a. and 1d.), changes in serum triglycerides and lipoprotein levels have been reported in oral contraceptive users.
ELEVATED BLOOD PRESSURE
An increase in blood pressure has been reported in women taking oral contraceptives and this increase is more likely in older oral contraceptive users and with continued use. Data from the Royal College of General Practitioners and subsequent randomized trials have shown that the incidence of hypertension increases with increasing quantities of progestogens.
Women with a history of hypertension or hypertension-related diseases, or renal disease should be encouraged to use another method of contraception. If women with hypertension elect to use oral contraceptives, they should be monitored closely, and if significant elevation of blood pressure occurs, oral contraceptives should be discontinued. For most women, elevated blood pressure will return to normal after stopping oral contraceptives, and there is no difference in the occurrence of hypertension among ever- and never-users.
HEADACHE
The onset or exacerbation of migraine or development of headache with a new pattern which is recurrent, persistent or severe requires discontinuation of oral contraceptives and evaluation of the cause.
BLEEDING IRREGULARITIES
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. Nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If pathology has been excluded, time or a change to another formulation may solve the problem. ln the event of amenorrhea, pregnancy should be ruled out.
Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.
PRECAUTIONS
GENERAL
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
PHYSICAL EXAMINATION AND FOLLOW-UP
It is good medical practice for all women to have annual history and physical examinations, including women using oral contraceptives. The physical examination, however, may be deferred until after initiation of oral contraceptives if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology and relevant laboratory tests. ln case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
LIPID DISORDERS
Women who are being treated for hyperlipidemias should be followed closely if they elect to use oral contraceptives. Some progestogens may elevate LDL levels and may render the control of hyperlipidemias more difficult.
LIVER FUNCTION
If jaundice develops in any woman receiving such drugs, the medication should be discontinued. Steroid hormones may be poorly metabolized in patients with impaired liver function.
FLUID RETENTION
Oral contraceptives may cause some degree of fluid retention. They should be prescribed with caution, and only with careful monitoring, in patients with conditions which might be aggravated by fluid retention.
EMOTIONAL DISORDERS
Women with a history of depression should be carefully observed and the drug discontinued if depression recurs to a serious degree.
CONTACT LENSES
Contact-lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
DRUG INTERACTIONS
Reduced efficacy and increased incidence of breakthrough bleeding and menstrual irregularities have been associated with concomitant use of rifampin. A similar association, though less marked, has been suggested with barbiturates, phenylbutazone, phenytoin sodium, and possibly with griseofulvin, ampicillin and tetracyclines.
INTERACTIONS WITH LABORATORY TESTS
Certain endocrine- and liver-function tests and blood components may be affected by oral contraceptives:
a. Increased prothrombin and factors VII, VIII, IX and X; decreased antithrombin 3; increased norepinephrine-induced platelet aggregability.
b. Increased thyroid-binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 by column or by radioimmunoassay. Free T3 resin uptake is decreased, reflecting the elevated TBG, free T4 concentration is unaltered.
c. Other binding proteins may be elevated in serum.
d. Sex-binding globulins are increased and result in elevated levels of total circulating sex steroids and corticoids; however, free or biologically active levels remain unchanged.
e. Triglycerides may be increased.
f. Glucose tolerance may be decreased.
g. Serum folate levels may be depressed by oral contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing oral contraceptives.
CARCINOGENESIS
See "WARNINGS" section.
PREGNANCY
Pregnancy Category X.
See "CONTRAINDICATIONS" and "WARNINGS" sections.
NURSING MOTHERS
Small amounts of oral contraceptive steroids have been identified in the milk of nursing mothers, and a few adverse effects on the child have been reported, including jaundice and breast enlargement. ln addition, oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk. If possible, the nursing mother should be advised not to use oral contraceptives but to use other forms of contraception until she has completely weaned her child.
PEDIATRIC USE
Safety and efficacy of LEVLITE have been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 and for users 16 years and older. Use of this product before menarche is not indicated.
Information for the patient
See "BRIEF SUMMARY PATIENT PACKAGE INSERT" printed below.
LEVLITE ADVERSE REACTIONS
An increased risk of the following serious adverse reactions has been associated with the use of oral contraceptives (see "WARNINGS" section).
- Thrombophlebitis
- Arterial thromboembolism
- Pulmonary embolism
- Myocardial infarction
- Cerebral hemorrhage
- Cerebral thrombosis
- Hypertension
- Gallbladder disease
- Hepatic adenomas or benign liver tumors
There is evidence of an association between the following conditions and the use of oral contraceptives, although additional confirmatory studies are needed:
- Mesenteric thrombosis
- Retinal thrombosis
The following adverse reactions have been reported in patients receiving oral contraceptives and are believed to be drug related:
- Nausea
- Vomiting
- Gastrointestinal symptoms, (such as abdominal cramps and bloating)
- Breakthrough bleeding
- Spotting
- Change in menstrual flow
- Amenorrhea
- Temporary infertility after discontinuation of treatment
- Edema
- Melasma which may persist
- Breast changes: tenderness, enlargement, secretion
- Change in weight (increase or decrease)
- Change in cervical erosion and secretion
- Diminution in lactation when given immediately postpartum
- Cholestatic jaundice
- Migraine
- Rash (allergic)
- Mental depression
- Reduced tolerance to carbohydrates
- Vaginal candidiasis
- Change in corneal curvature (steepening)
- Intolerance to contact lenses
The following adverse reactions have been reported in users of oral contraceptives and the association has been neither confirmed nor refuted:
- Pre-menstrual syndrome
- Cataracts
- Optic neuritis
- Changes in appetite
- Cystitis-like syndrome
- Headache
- Nervousness
- Dizziness
- Hirsutism
- Loss of scalp hair
- Erythema multiforme
- Erythema nodosum
- Hemorrhagic eruption
- Vaginitis
- Porphyria
- lmpaired renal function
- Hemolytic uremic syndrome
- Budd-Chiari syndrome
- Acne
- Changes in libido
- Colitis
OVERDOSAGE
Serious ill effects have not been reported following acute ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea, and withdrawal bleeding may occur in females.
NON-CONTRACEPTIVE HEALTH BENEFITS
The following non-contraceptive health benefits related to the use of oral contraceptives are supported by epidemiological studies which largely utilized oral contraceptive formulations containing doses exceeding 0.035 mg of ethinyl estradiol or 0.05 mg mestranol.
Effects on menses
- increased menstrual cycle regularity
- decreased blood loss and decreased incidence of iron-deficiency anemia
- decreased incidence of dysmenorrhea
Effects related to inhibition of ovulation:
- decreased incidence of functional ovarian cysts
- decreased incidence of ectopic pregnancies
Effects from long-term use:
- decreased incidence of fibroadenomas and fibrocystic disease of the breast
- decreased incidence of acute pelvic inflammatory disease
- decreased incidence of endometrial cancer
- decreased incidence of ovarian cancer
LEVLITE DOSAGE AND ADMINISTRATION
LEVLITE 28 Tablets To achieve maximum contraceptive effectiveness, LEVLITE 28 Tablets (levonorgestrel and ethinyl estradiol tablets, USP) must be taken exactly as directed at intervals not exceeding 24-hours.
LEVLITE 28 Tablets are a monophasic preparation plus 7 inert tablets. The dosage of LEVLITE 28 Tablets is one tablet daily for 21 consecutive days per menstrual cycle plus 7 white inert tablets according to the prescribed schedule. It is recommended that LEVLITE 28 Tablets be taken at the same time each day, preferably after the evening meal or at bedtime. During the first cycle of medication, the patient should be instructed to take one pink LEVLITE 28 Tablet daily and then 7 white inert tablets for twenty-eight (28) consecutive days, beginning on day one (1) of her menstrual cycle. (The first day of menstruation is day one.) Withdrawal bleeding usually occurs within 3 days following the last pink tablet. (If LEVLITE 28 Tablets are first taken later than the first day of the first menstrual cycle of medication or postpartum, contraceptive reliance should not be placed on LEVLITE 28 Tablets until after the first 7 consecutive days of administration. The possibility of ovulation and conception prior to initiation of medication should be considered.)
When switching from another oral contraceptive, LEVLITE 28 Tablets should be started on the first day of bleeding following the last active tablet taken of the previous oral contraceptive.
The patient begins her next and all subsequent 28-day courses of LEVLITE 28 Tablets on the same day of the week that she began her first course, following the same schedule. She begins taking her pink tablets on the next day after ingestion of the last white tablet, regardless of whether or not a menstrual period has occurred or is still in progress. Anytime a subsequent cycle of LEVLITE 28 Tablets is started later than the next day, the patient should be protected by another means of contraception until she has taken a tablet daily for seven consecutive days.
If spotting or breakthrough bleeding occurs, the patient is instructed to continue on the same regimen. This type of bleeding is usually transient and without significance, however, if the bleeding is persistent or prolonged, the patient is advised to consult her physician. Although the occurrence of pregnancy is highly unlikely if LEVLITE 28 Tablets are taken according to directions, if withdrawal bleeding does not occur, the possibility of pregnancy must be considered. If the patient has not adhered to the prescribed schedule (missed one or more active tablets or started taking them on a day later than she should have), the probability of pregnancy should be considered at the time of the first missed period and appropriate diagnostic measures taken before the medication is resumed. If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out before continuing the contraceptive regimen.
The risk of pregnancy increases with each active (pink) tablet missed. For additional patient instructions regarding missed pills, see the "WHAT TO DO IF YOU MISS PILLS" section in the DETAILED PATIENT LABELING below. If breakthrough bleeding occurs following missed tablets, it will usually be transient and of no consequence. If the patient misses one or more white tablets, she is still protected against pregnancy provided she begins taking pink tablets again on the proper day.
In the nonlactating mother, LEVLITE 28 Tablets may be initiated postpartum, for contraception. When the tablets are administered in the postpartum period, the increased risk of thromboembolic disease associated with the postpartum period must be considered. (See "CONTRAINDICATIONS," "WARNINGS," and "PRECAUTIONS" concerning thromboembolic disease.) It is to be noted that early resumption of ovulation may occur if bromocriptine mesylate has been used for the prevention of lactation.
HOW SUPPLIED
LEVLITE 28 Tablets (levonorgestrel and ethinyl estradiol tablets, USP), are available in packages of 3 SLIDECASE® dispensers. Each cycle contains 28 round, unscored coated tablets as follows:
NDC 50419-022, 21 pink tablets marked "B'' on one side and "22'' on the other side, each containing 0.100 mg levonorgestrel and 0.020 mg ethinyl estradiol;
NDC 50419-029, seven white inert tablets marked "B'' on one side and "29'' on the other side.
In packages of: 3 SLIDECASE® dispensers .......................................NDC 50419-408-03
Keep at room temperature, approximately 25°C (77°F).
REFERENCES FURNISHED UPON REQUEST
BRIEF SUMMARY PATIENT PACKAGE INSERT
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Oral contraceptives, also known as "birth-control pills" or "the pill", are taken to prevent pregnancy, and when taken correctly, have a failure rate of less than 1% per year when used without missing any pills. The typical failure rate of large numbers of pill users is less than 3% per year when women who miss pills are included. For most women oral contraceptives are also free of serious or unpleasant side effects. However, forgetting to take pills considerably increases the chances of pregnancy.
For the majority of women, oral contraceptives can be taken safely. But there are some women who are at high risk of developing certain serious diseases that can be life-threatening or may cause temporary or permanent disability or death. The risks associated with taking oral contraceptives increase significantly if you:
- smoke
- have high blood pressure, diabetes, high cholesterol
- have or have had clotting disorders, heart attack, stroke, angina pectoris, cancer of the breast or sex organs, jaundice, or malignant or benign liver tumors.
You should not take the pill if you suspect you are pregnant or have unexplained vaginal bleeding.
Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should not smoke.
Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should not smoke.
Levlitelevonorgestrel and ethinyl estradiol KIT
| ||||||||||||||||||||||||||||||||