LEXIVA
State of Florida DOH Central Pharmacy
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use LEXIVA safely and effectively. See full prescribing information for LEXIVA.LEXIVA (fosamprenavir calcium) Tablets and Oral SuspensionInitial U.S. Approval: 2003RECENT MAJOR CHANGESDosage and Administration, Patients With Hepatic Impairment (2.3) 4/2009Warnings and Precautions (5.8) 9/2009Warnings and Precautions, Nephrolithiasis (5.11) 9/2009INDICATIONS AND USAGELEXIVA is an HIV protease inhibitor indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection. (1)DOSAGE AND ADMINISTRATION Therapy-Naive Adults: LEXIVA 1,400 mg twice daily; LEXIVA 1,400 mg once daily plus ritonavir 200 mg once daily; LEXIVA 1,400 mg once daily plus ritonavir 100 mg once daily; LEXIVA 700 mg twice daily plus ritonavir 100 mg twice daily. (2.1) Protease Inhibitor-Experienced Adults: LEXIVA 700 mg twice daily plus ritonavir 100 mg twice daily. (2.1) Pediatric Patients (2 to 18 years of age): Dosage should be calculated based on body weight (kg) and should not exceed adult dose. (2.2) Hepatic Impairment: Recommended adjustments for patients with mild, moderate, or severe hepatic impairment. (2.3) Dosing Considerations LEXIVA Tablets may be taken with or without food. (2) LEXIVA Suspension: Adults should take without food; pediatric patients should take with food. (2) DOSAGE FORMS AND STRENGTHS700 mg tablets and 50 mg/mL oral suspension (3)CONTRAINDICATIONS Hypersensitivity to LEXIVA or amprenavir (e.g., Stevens-Johnson syndrome). (4) Drugs highly dependent on CYP3A4 for clearance and for which elevated plasma levels may result in serious and/or life-threatening events. (4) Review ritonavir contraindications when used in combination. (4) WARNINGS AND PRECAUTIONS Certain drugs should not be coadministered with LEXIVA due to risk of serious or life-threatening adverse reactions. (5.1) LEXIVA should be discontinued for severe skin reactions including Stevens-Johnson syndrome. (5.2) LEXIVA should be used with caution in patients with a known sulfonamide allergy. (5.3) Use of higher than approved doses may lead to transaminase elevations. Patients with hepatitis B or C are at increased risk of transaminase elevations. (5.4) Patients receiving LEXIVA may develop new onset or exacerbations of diabetes mellitus, hyperglycemia (5.5), immune reconstitution syndrome (5.6), redistribution/accumulation of body fat (5.7), and elevated triglyceride and cholesterol concentrations (5.8). Monitor cholesterol and triglycerides prior to therapy and periodically thereafter. Acute hemolytic anemia has been reported with amprenavir. (5.9) Hemophilia: Spontaneous bleeding may occur, and additional factor VIII may be required. (5.10) Nephrolithiasis: Cases of nephrolithiasis have been reported with fosamprenavir. (5.11) Side Effects In adults the most common adverse reactions (incidence ≥4%) are diarrhea, rash, nausea, vomiting, headache. (6.1) Vomiting was more frequent in pediatrics than in adults. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONS Coadministration of LEXIVA with drugs that induce CYP3A4 may decrease amprenavir (active metabolite) concentrations leading to potential loss of virologic activity. (7, 12.3) Coadministration with drugs that inhibit CYP3A4 may increase amprenavir concentrations. (7, 12.3) Coadministration of LEXIVA and ritonavir may result in clinically significant interactions with drugs metabolized by CYP2D6. (7)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 LEXIVA INDICATIONS AND USAGE
- 2 LEXIVA DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 LEXIVA CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 LEXIVA ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 LEXIVA DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
LEXIVA® is indicated in combination with other antiretroviral agents for the treatment of human immunodeficiency virus (HIV-1) infection.
The following points should be considered when initiating therapy with LEXIVA plus ritonavir in protease inhibitor-experienced patients:
- The protease inhibitor-experienced patient study was not large enough to reach a definitive conclusion that LEXIVA plus ritonavir and lopinavir plus ritonavir are clinically equivalent [see Clinical Studies (14.2)].
- Once-daily administration of LEXIVA plus ritonavir is not recommended for adult protease inhibitor-experienced patients or any pediatric patients.
2 DOSAGE AND ADMINISTRATION
LEXIVA Tablets may be taken with or without food.
Adults should take LEXIVA Oral Suspension without food. Pediatric patients should take LEXIVA Oral Suspension with food [see Clinical Pharmacology (12.3)]. If emesis occurs within 30 minutes after dosing, re-dosing of LEXIVA Oral Suspension should occur.
Higher-than-approved dose combinations of LEXIVA plus ritonavir are not recommended due to an increased risk of transaminase elevations [see Overdosage (10)].
When LEXIVA is used in combination with ritonavir, prescribers should consult the full prescribing information for ritonavir.
Adults
Therapy-Naive Adults
- LEXIVA 1,400 mg twice daily (without ritonavir).
- LEXIVA 1,400 mg once daily plus ritonavir 200 mg once daily.
- LEXIVA 1,400 mg once daily plus ritonavir 100 mg once daily.
Dosing of LEXIVA 1,400 mg once daily plus ritonavir 100 mg once daily is supported by pharmacokinetic data [see Clinical Pharmacology (12.3)].
- LEXIVA 700 mg twice daily plus ritonavir 100 mg twice daily.
- Dosing of LEXIVA 700 mg twice daily plus 100 mg ritonavir twice daily is supported by pharmacokinetic and safety data [see Clinical Pharmacology (12.3)].
Protease Inhibitor-Experienced Adults
- LEXIVA 700 mg twice daily plus ritonavir 100 mg twice daily
Pediatric Patients (2 to 18 years of age)
The recommended dosage of LEXIVA in patients ≥2 years of age should be calculated based on body weight (kg) and should not exceed the recommended adult dose. The data are insufficient to recommend: (1) once-daily dosing of LEXIVA alone or in combination with ritonavir, and (2) any dosing of LEXIVA in therapy-experienced patients 2 to 5 years of age.
Therapy-Naive 2 to 5 Years of Age
- LEXIVA Oral Suspension 30 mg/kg twice daily, not to exceed the adult dose of LEXIVA 1,400 mg twice daily.
Therapy-Naive ≥6 Years of Age
- Either LEXIVA Oral Suspension 30 mg/kg twice daily not to exceed the adult dose of LEXIVA 1,400 mg twice daily or LEXIVA Oral Suspension 18 mg/kg plus ritonavir 3 mg/kg twice daily not to exceed the adult dose of LEXIVA 700 mg plus ritonavir 100 mg twice daily.
Therapy-Experienced ≥6 Years of Age
- LEXIVA Oral Suspension 18 mg/kg plus ritonavir 3 mg/kg administered twice daily not to exceed the adult dose of LEXIVA 700 mg twice daily plus ritonavir 100 mg twice daily.
Other Dosing Considerations
- When administered without ritonavir, the adult regimen of LEXIVA Tablets 1,400 mg twice daily may be used for pediatric patients weighing at least 47 kg.
- When administered in combination with ritonavir, LEXIVA Tablets may be used for pediatric patients weighing at least 39 kg; ritonavir capsules may be used for pediatric patients weighing at least 33 kg.
2.3 Patients With Hepatic Impairment
See Clinical Pharmacology (12.3).Mild Hepatic Impairment (Child-Pugh score ranging from 5 to 6): LEXIVA should be used with caution at a reduced dosage of 700 mg twice daily without ritonavir (therapy-naive) or 700 mg twice daily plus ritonavir 100 mg once daily (therapy-naive or protease inhibitor-experienced).
Moderate Hepatic Impairment (Child-Pugh score ranging from 7 to 9): LEXIVA should be used with caution at a reduced dosage of 700 mg twice daily without ritonavir (therapy-naive), or 450 mg twice daily plus ritonavir 100 mg once daily (therapy-naive or protease inhibitor-experienced).
Severe Hepatic Impairment (Child-Pugh score ranging from 10 to 15): LEXIVA should be used with caution at a reduced dosage of 350 mg twice daily without ritonavir (therapy-naive) or 300 mg twice daily plus ritonavir 100 mg once daily (therapy-naive or protease inhibitor-experienced).
3 DOSAGE FORMS AND STRENGTHS
LEXIVA Tablets, 700 mg, are pink, film-coated, capsule-shaped, biconvex tablets with “GX LL7” debossed on one face.
LEXIVA Oral Suspension, 50 mg/mL, is a white to off-white suspension that has a characteristic grape-bubblegum-peppermint flavor.
4 CONTRAINDICATIONS
LEXIVA is contraindicated:
- in patients with previously demonstrated clinically significant hypersensitivity (e.g., Stevens-Johnson syndrome) to any of the components of this product or to amprenavir.
- when coadministered with drugs that are highly dependent on CYP3A4 for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events (Table 1).
| Drug Class/Drug Name | Clinical Comment |
|
Antiarrhythmics: Flecainide, propafenone |
POTENTIAL for serious and/or life-threatening reactions such as cardiac arrhythmias secondary to increases in plasma concentrations of antiarrhythmics if LEXIVA is co-prescribed with ritonavir. |
|
Antimycobacterials: Rifampina |
May lead to loss of virologic response and possible resistance to LEXIVA or to the class of protease inhibitors. |
|
Ergot derivatives: Dihydroergotamine, ergonovine, ergotamine, methylergonovine |
POTENTIAL for serious and/or life-threatening reactions such as acute ergot toxicity characterized by peripheral vasospasm and ischemia of the extremities and other tissues. |
|
GI motility agents: Cisapride |
POTENTIAL for serious and/or life-threatening reactions such as cardiac arrhythmias. |
|
Herbal products: St. John’s wort (hypericum perforatum) |
May lead to loss of virologic response and possible resistance to LEXIVA or to the class of protease inhibitors. |
|
HMG co-reductase inhibitors: Lovastatin, simvastatin |
POTENTIAL for serious reactions such as risk of myopathy including rhabdomyolysis. |
|
Neuroleptic: Pimozide |
POTENTIAL for serious and/or life-threatening reactions such as cardiac arrhythmias. |
|
Non-nucleoside reverse transcriptase inhibitor: Delavirdinea |
May lead to loss of virologic response and possible resistance to delavirdine. |
|
Sedative/hypnotics: Midazolam, triazolam |
POTENTIAL for serious and/or life-threatening reactions such as prolonged or increased sedation or respiratory depression. |
a See Clinical Pharmacology (12.3) Tables 10, 11, 12, or 13 for magnitude of interaction.
- when coadministered with ritonavir in patients receiving the antiarrhythmic agents flecainide and propafenone. If LEXIVA is coadministered with ritonavir, reference should be made to the full prescribing information for ritonavir for additional contraindications.
5 WARNINGS AND PRECAUTIONS
Drug Interactions
See Table 1 for listings of drugs that are contraindicated due to potentially life-threatening adverse events, significant drug interactions, or due to loss of virologic activity [see Contraindications (4), Drug Interactions (7.2)].
Skin Reactions
Severe and life-threatening skin reactions, including 1 case of Stevens-Johnson syndrome among 700 patients treated with LEXIVA in clinical studies. Treatment with LEXIVA should be discontinued for severe or life-threatening rashes and for moderate rashes accompanied by systemic symptoms [see Adverse Reactions (6)].
Sulfa Allergy
LEXIVA should be used with caution in patients with a known sulfonamide allergy. Fosamprenavir contains a sulfonamide moiety. The potential for cross-sensitivity between drugs in the sulfonamide class and fosamprenavir is unknown. In a clinical study of LEXIVA used as the sole protease inhibitor, rash occurred in 2 of 10 patients (20%) with a history of sulfonamide allergy compared with 42 of 126 patients (33%) with no history of sulfonamide allergy. In 2 clinical studies of LEXIVA plus low-dose ritonavir, rash occurred in 8 of 50 patients (16%) with a history of sulfonamide allergy compared with 50 of 412 patients (12%) with no history of sulfonamide allergy.
Hepatic Toxicity
Use of LEXIVA with ritonavir at higher-than-recommended dosages may result in transaminase elevations and should not be used [see Dosage and Administration (2), Overdosage (10)]. Patients with underlying hepatitis B or C or marked elevations in transaminases prior to treatment may be at increased risk for developing or worsening of transaminase elevations. Appropriate laboratory testing should be conducted prior to initiating therapy with LEXIVA and patients should be monitored closely during treatment.
Diabetes/Hyperglycemia
New onset diabetes mellitus, exacerbation of pre-existing diabetes mellitus, and hyperglycemia have been reported during postmarketing surveillance in HIV-infected patients receiving protease inhibitor therapy. Some patients required either initiation or dose adjustments of insulin or oral hypoglycemic agents for treatment of these events. In some cases, diabetic ketoacidosis has occurred. In those patients who discontinued protease inhibitor therapy, hyperglycemia persisted in some cases. Because these events have been reported voluntarily during clinical practice, estimates of frequency cannot be made and causal relationships between protease inhibitor therapy and these events have not been established.
Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including LEXIVA. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia [PCP], or tuberculosis), which may necessitate further evaluation and treatment.
Fat Redistribution
Redistribution/accumulation of body fat, including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and “cushingoid appearance,” have been observed in patients receiving antiretroviral therapy, including LEXIVA. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
Lipid Elevations
Treatment with LEXIVA plus ritonavir has resulted in increases in the concentration of triglycerides and cholesterol [see Adverse Reactions (6)]. Triglyceride and cholesterol testing should be performed prior to initiating therapy with LEXIVA and at periodic intervals during therapy. Lipid disorders should be managed as clinically appropriate [see Drug Interactions (7)].
Hemolytic Anemia
Acute hemolytic anemia has been reported in a patient treated with amprenavir.
Patients With Hemophilia
There have been reports of spontaneous bleeding in patients with hemophilia A and B treated with protease inhibitors. In some patients, additional factor VIII was required. In many of the reported cases, treatment with protease inhibitors was continued or restarted. A causal relationship between protease inhibitor therapy and these episodes has not been established.
Nephrolithiasis
Cases of nephrolithiasis were reported during postmarketing surveillance in HIV-infected patients receiving LEXIVA.Because these events were reported voluntarily during clinical practice, estimates of frequency cannot be made. If signs or symptoms of nephrolithiasis occur, temporary interruption or discontinuation of therapy may be considered.
Resistance/Cross-Resistance
Because the potential for HIV cross-resistance among protease inhibitors has not been fully explored, it is unknown what effect therapy with LEXIVA will have on the activity of subsequently administered protease inhibitors. LEXIVA has been studied in patients who have experienced treatment failure with protease inhibitors [see Clinical Studies (14.2)].
6 ADVERSE REACTIONS
- Severe or life-threatening skin reactions have been reported with the use of LEXIVA [see Warnings and Precautions (5.2)].
- The most common moderate to severe adverse reactions in clinical studies of LEXIVA were diarrhea, rash, nausea, vomiting, and headache.
- Treatment discontinuation due to adverse events occurred in 6.4% of patients receiving LEXIVA and in 5.9% of patients receiving comparator treatments. The most common adverse reactions leading to discontinuation of LEXIVA (incidence ≤1% of patients) included diarrhea, nausea, vomiting, AST increased, ALT increased, and rash.
6.1 Clinical Trials
Adults
The data for the 3 active-controlled clinical trials described below reflect exposure of 700 HIV-1 infected patients to LEXIVA Tablets, including 599 patients exposed to LEXIVA for >24 weeks, and 409 patients exposed for >48 weeks. The population age ranged from 17 to 72 years. Of these patients, 26% were female, 51% Caucasian, 31% black, 16% American Hispanic, and 70% were antiretroviral-naive. Sixty-one percent received LEXIVA 1,400 mg once daily plus ritonavir 200 mg once daily, 24% received LEXIVA 1,400 mg twice daily, and 15% received LEXIVA 700 mg twice daily plus ritonavir 100 mg twice daily.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Selected adverse reactions reported during the clinical efficacy studies of LEXIVA are shown in Tables 2 and 3. Each table presents adverse reactions of moderate or severe intensity in patients treated with combination therapy for up to 48 weeks.
Table 2. Selected Moderate/Severe Clinical Adverse Reactions Reported in ≥2% of Antiretroviral-Naive Adult Patients
| Adverse Reaction | APV30001a | APV30002a | ||
|
LEXIVA 1,400 mg b.i.d. (n = 166) |
Nelfinavir 1,250 mg b.i.d. (n = 83) |
LEXIVA 1,400 mg q.d./ Ritonavir 200 mg q.d. (n = 322) |
Nelfinavir 1,250 mg b.i.d. (n = 327) |
|
| Gastrointestinal | ||||
| Diarrhea | 5% | 18% | 10% | 18% |
| Nausea | 7% | 4% | 7% | 5% |
| Vomiting | 2% | 4% | 6% | 4% |
| Abdominal pain | 1% | 0% | 2% | 2% |
| Skin | ||||
| Rash | 8% | 2% | 3% | 2% |
| General disorders | ||||
| Fatigue | 2% | 1% | 4% | 2% |
| Nervous system | ||||
| Headache | 2% | 4% | 3% | 3% |
aAll patients also received abacavir and lamivudine twice daily.
Table 3. Selected Moderate/Severe Clinical Adverse Reactions Reported in ≥2% of Protease Inhibitor-Experienced Adult Patients (Study APV30003)
| Adverse Reaction |
LEXIVA 700 mg b.i.d./ Ritonavir 100 mg b.i.d.a (n = 106) |
Lopinavir 400 mg b.i.d./ Ritonavir 100 mg b.i.d.a (n = 103) |
| Gastrointestinal | ||
| Diarrhea | 13% | 11% |
| Nausea | 3% | 9% |
| Vomiting | 3% | 5% |
| Abdominal pain | <1% | 2% |
| Skin | ||
| Rash | 3% | 0% |
| Nervous system | ||
| Headache | 4% | 2% |
aAll patients also received 2 reverse transcriptase inhibitors.
Skin rash (without regard to causality) occurred in approximately 19% of patients treated with LEXIVA in the pivotal efficacy studies. Rashes were usually maculopapular and of mild or moderate intensity, some with pruritus. Rash had a median onset of 11 days after initiation of LEXIVA and had a median duration of 13 days. Skin rash led to discontinuation of LEXIVA in <1% of patients. In some patients with mild or moderate rash, dosing with LEXIVA was often continued without interruption; if interrupted, reintroduction of LEXIVA generally did not result in rash recurrence.
The percentages of patients with Grade 3 or 4 laboratory abnormalities in the clinical efficacy studies of LEXIVA are presented in Tables 4 and 5.
Table 4. Grade 3/4 Laboratory Abnormalities Reported in ≥2% of Antiretroviral-Naive Adult Patients in Studies APV30001 and APV30002
| Laboratory Abnormality | APV30001a | APV30002a | ||
|
LEXIVA 1,400 mg b.i.d. (n = 166) |
Nelfinavir 1,250 mg b.i.d. (n = 83) |
LEXIVA 1,400 mg q.d./ Ritonavir 200 mg q.d. (n = 322) |
Nelfinavir 1,250 mg b.i.d. (n = 327) |
|
| ALT (>5 x ULN) | 6% | 5% | 8% | 8% |
| AST (>5 x ULN) | 6% | 6% | 6% | 7% |
| Serum lipase (>2 x ULN) | 8% | 4% | 6% | 4% |
| Triglyceridesb (>750 mg/dL) | 0% | 1% | 6% | 2% |
| Neutrophil count, absolute (<750 cells/mm3) | 3% | 6% | 3% | 4% |
aAll patients also received abacavir and lamivudine twice daily.
bFasting specimens.
ULN = Upper limit of normal.
The incidence of Grade 3 or 4 hyperglycemia in antiretroviral-naive patients who received LEXIVA in the pivotal studies was <1%.
Table 5. Grade 3/4 Laboratory Abnormalities Reported in ≥2% of Protease Inhibitor-Experienced Adult Patients in Study APV30003
| Laboratory Abnormality |
LEXIVA 700 mg b.i.d./ Ritonavir 100 mg b.i.d.a (n = 104) |
Lopinavir 400 mg b.i.d./ Ritonavir 100 mg b.i.d.a (n = 103) |
| Triglyceridesb (>750 mg/dL) | 11%c | 6%c |
| Serum lipase (>2 x ULN) | 5% | 12% |
| ALT (>5 x ULN) | 4% | 4% |
| AST (>5 x ULN) | 4% | 2% |
| Glucose (>251 mg/dL) | 2%c | 2%c |
aAll patients also received 2 reverse transcriptase inhibitors.
bFasting specimens.
cn = 100 for LEXIVA plus ritonavir, n = 98 for lopinavir plus ritonavir.
ULN = Upper limit of normal.
Pediatric Patients: LEXIVA with and without ritonavir was studied in 144 pediatric patients 2 to 18 years of age in 2 open-label studies. Safety information from 75 pediatric patients receiving LEXIVA twice daily with or without ritonavir follows.
All adverse events regardless of causality, all drug-related adverse events, and all laboratory events occurred with similar frequency in pediatrics compared with adults, with the exception of vomiting. Vomiting, regardless of causality, occurred more frequently among pediatric patients receiving LEXIVA twice daily with ritonavir ([30%] all between 2 and 18 years of age) and without ritonavir ([56%] all between 2 and 5 years of age) compared with adults receiving LEXIVA twice daily with ritonavir (10%) and without ritonavir (16%). The median duration of drug-related vomiting episodes was 1 day (range: 1 to 62 days). Vomiting required temporary dose interruptions in 4 pediatric patients and was treatment-limiting in 1 pediatric patient, all of whom were receiving LEXIVA twice daily with ritonavir.
6.2 Postmarketing Experience
In addition to adverse reactions reported from clinical trials, the following reactions have been identified during post-approval use of LEXIVA. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to LEXIVA.
Cardiac Disorders
Myocardial infarction.
Metabolism and Nutrition Disorders
Hypercholesterolemia.
Nervous System Disorders
Oral paresthesia.
Skin and Subcutaneous Tissue Disorders
Angioedema.
Urogenital
Nephrolithiasis.
7 DRUG INTERACTIONS
See also Contraindications (4), Clinical Pharmacology (12.3).
If LEXIVA is used in combination with ritonavir, see full prescribing information for ritonavir for additional information on drug interactions.
7.1 CYP Inhibitors and Inducers
Amprenavir, the active metabolite of fosamprenavir, is an inhibitor of cytochrome P450 3A4 metabolism and therefore should not be administered concurrently with medications with narrow therapeutic windows that are substrates of CYP3A4. Data also suggest that amprenavir induces CYP3A4.
Amprenavir is metabolized by CYP3A4. Coadministration of LEXIVA and drugs that induce CYP3A4, such as rifampin, may decrease amprenavir concentrations and reduce its therapeutic effect. Coadministration of LEXIVA and drugs that inhibit CYP3A4 may increase amprenavir concentrations and increase the incidence of adverse effects.
The potential for drug interactions with LEXIVA changes when LEXIVA is coadministered with the potent CYP3A4 inhibitor ritonavir. The magnitude of CYP3A4-mediated drug interactions (effect on amprenavir or effect on coadministered drug) may change when LEXIVA is coadministered with ritonavir. Because ritonavir is a CYP2D6 inhibitor, clinically significant interactions with drugs metabolized by CYP2D6 are possible when coadministered with LEXIVA plus ritonavir.
There are other agents that may result in serious and/or life-threatening drug interactions [see Contraindications (4)].
7.2 Drugs That Should Not Be Coadministered With LEXIVA
See Contraindications (4).
7.3 Established and Other Potentially Significant Drug Interactions
Table 6 provides a listing of established or potentially clinically significant drug interactions. Information in the table applies to LEXIVA with or without ritonavir, unless otherwise indicated.
Table 6. Established and Other Potentially Significant Drug Interactions
| Concomitant Drug Class: Drug Name | Effect on Concentration of Amprenavir or Concomitant Drug | Clinical Comment |
| HIV-Antiviral Agents | ||
|
Non-nucleoside reverse transcriptase inhibitor: Efavirenza |
LEXIVA: ↓Amprenavir LEXIVA/ritonavir: ↓Amprenavir |
Appropriate doses of the combinations with respect to safety and efficacy have not been established. An additional 100 mg/day (300 mg total) of ritonavir is recommended when efavirenz is administered with LEXIVA/ritonavir once daily. No change in the ritonavir dose is required when efavirenz is administered with LEXIVA plus ritonavir twice daily. |
|
Non-nucleoside reverse transcriptase inhibitor: Nevirapinea |
LEXIVA: ↓Amprenavir ↑Nevirapine LEXIVA/ritonavir: ↓Amprenavir ↑Nevirapine |
Coadministration of nevirapine and LEXIVA without ritonavir is not recommended. No dosage adjustment required when nevirapine is administered with LEXIVA/ritonavir twice daily. The combination of nevirapine administered with LEXIVA/ritonavir once-daily regimen has not been studied. |
|
HIV protease inhibitor: Atazanavira |
LEXIVA: Interaction has not been evaluated. LEXIVA/ritonavir: ↓Atazanavir ↔Amprenavir |
Appropriate doses of the combinations with respect to safety and efficacy have not been established. |
|
HIV protease inhibitors: Indinavira, nelfinavira |
LEXIVA: ↑Amprenavir Effect on indinavir and nelfinavir is not well established. LEXIVA/ritonavir: Interaction has not been evaluated. |
Appropriate doses of the combinations with respect to safety and efficacy have not been established. |
|
HIV protease inhibitors: Lopinavir/ritonavira |
↓Amprenavir ↓Lopinavir |
An increased rate of adverse events has been observed. Appropriate doses of the combinations with respect to safety and efficacy have not been established. |
|
HIV protease inhibitor: Saquinavira |
LEXIVA: ↓Amprenavir Effect on saquinavir is not well established. LEXIVA/ritonavir: Interaction has not been evaluated. |
Appropriate doses of the combination with respect to safety and efficacy have not been established. |
| Other Agents | ||
|
Antiarrhythmics: Amiodarone, bepridil, lidocaine (systemic), and quinidine |
↑Antiarrhythmics |
Use with caution. Increased exposure may be associated with life-threatening reactions such as cardiac arrhythmias. Therapeutic concentration monitoring, if available, is recommended for antiarrhythmics. |
|
Anticoagulant: Warfarin |
Concentrations of warfarin may be affected. It is recommended that INR (international normalized ratio) be monitored. | |
|
Anticonvulsants: Carbamazepine, phenobarbital, phenytoin Phenytoina |
LEXIVA: ↓Amprenavir LEXIVA/ritonavir: ↑Amprenavir ↓Phenytoin |
Use with caution. LEXIVA may be less effective due to decreased amprenavir plasma concentrations in patients taking these agents concomitantly. Plasma phenytoin concentrations should be monitored and phenytoin dose should be increased as appropriate. No change in LEXIVA/ritonavir dose is recommended. |
|
Antidepressant: Paroxetine, trazodone |
↓Paroxetine ↑Trazodone |
Coadministration of paroxetine with LEXIVA/ritonavir significantly decreased plasma levels of paroxetine. Any paroxetine dose adjustment should be guided by clinical effect (tolerability and efficacy). Concomitant use of trazodone and LEXIVA with or without ritonavir may increase plasma concentrations of trazodone. Adverse events of nausea, dizziness, hypotension, and syncope have been observed following coadministration of trazodone and ritonavir. If trazodone is used with a CYP3A4 inhibitor such as LEXIVA, the combination should be used with caution and a lower dose of trazodone should be considered. |
|
Antifungals: Ketoconazolea, itraconazole |
↑Ketoconazole ↑Itraconazole |
Increase monitoring for adverse events. LEXIVA: Dose reduction of ketoconazole or itraconazole may be needed for patients receiving more than 400 mg ketoconazole or itraconazole per day. LEXIVA/ritonavir: High doses of ketoconazole or itraconazole (>200 mg/day) are not recommended. |
|
Antimycobacterial: Rifabutina |
↑Rifabutin and rifabutin metabolite |
A complete blood count should be performed weekly and as clinically indicated to monitor for neutropenia. LEXIVA: A dosage reduction of rifabutin by at least half the recommended dose is required. LEXIVA/ritonavir: Dosage reduction of rifabutin by at least 75% of the usual dose of 300 mg/day is recommended (a maximum dose of 150 mg every other day or 3 times per week). |
|
Benzodiazepines: Alprazolam, clorazepate, diazepam, flurazepam |
↑Benzodiazepines | Clinical significance is unknown. A decrease in benzodiazepine dose may be needed. |
|
Calcium channel blockers: Diltiazem, felodipine, nifedipine, nicardipine, nimodipine, verapamil, amlodipine, nisoldipine, isradipine |
↑Calcium channel blockers | Use with caution. Clinical monitoring of patients is recommended. |
| Corticosteroid: Dexamethasone | ↓Amprenavir | Use with caution. LEXIVA may be less effective due to decreased amprenavir plasma concentrations. |
|
Histamine H2-receptor antagonists: Cimetidine, famotidine, nizatidine, ranitidinea |
LEXIVA: ↓Amprenavir LEXIVA/ritonavir: Interaction not evaluated |
Use with caution. LEXIVA may be less effective due to decreased amprenavir plasma concentrations. |
|
HMG-CoA reductase inhibitor: Atorvastatina, rosuvastatin |
↑Atorvastatin ↑Rosuvastatin |
Use the lowest possible dose of atorvastatin or rosuvastatin with careful monitoring, or consider other HMG-CoA reductase inhibitors such as fluvastatin or pravastatin. |
|
Immunosuppressants: Cyclosporine, tacrolimus, rapamycin |
↑Immunosuppressants | Therapeutic concentration monitoring is recommended for immunosuppressant agents. |
|
Inhaled/nasal steroid: Fluticasone |
LEXIVA: ↑Fluticasone LEXIVA/ritonavir: ↑Fluticasone |
Use with caution. Consider alternatives to fluticasone, particularly for long-term use. May result in significantly reduced serum cortisol concentrations. Systemic corticosteroid effects including Cushings syndrome and adrenal suppression have been reported during postmarketing use in patients receiving ritonavir and inhaled or intranasally administered fluticasone. Coadministration of fluticasone and LEXIVA/ritonavir is not recommended unless the potential benefit to the patient outweighs the risk of systemic corticosteroid side effects. |
|
Narcotic analgesic: Methadone |
↓Methadone | Data suggest that the interaction is not clinically relevant; however, patients should be monitored for opiate withdrawal symptoms. |
|
Oral contraceptives: Ethinyl estradiol/norethin-dronea |
LEXIVA: ↓Amprenavir ↓Ethinyl estradiol LEXIVA/ritonavir: ↓Ethinyl estradiol |
Alternative methods of non-hormonal contraception are recommended. May lead to loss of virologic response. * Increased risk of transaminase elevations. No data are available on the use of LEXIVA/ritonavir with other hormonal therapies, such as hormone replacement therapy (HRT) for postmenopausal women. |
|
PDE5 inhibitors: Sildenafil, tadalafil, vardenafil |
↑Sildenafil ↑Tadalafil ↑Vardenafil |
May result in an increase in PDE5 inhibitor-associated adverse events, including hypotension, visual changes, and priapism. LEXIVA: Sildenafil: 25 mg every 48 hours. Tadalafil: no more than 10 mg every 72 hours. Vardenafil: no more than 2.5 mg every 24 hours. LEXIVA/ritonavir: Sildenafil: 25 mg every 48 hours. Tadalafil: no more than 10 mg every 72 hours. Vardenafil: no more than 2.5 mg every 72 hours. |
|
Proton pump inhibitors: Esomeprazolea, lansoprazole, omeprazole, pantoprazole, rabeprazole |
LEXIVA: ↔Amprenavir ↑Esomeprazole LEXIVA/ritonavir: ↔Amprenavir ↔Esomeprazole |
Proton pump inhibitors can be administered at the same time as a dose of LEXIVA with no change in plasma amprenavir concentrations. |
|
Tricyclic antidepressants: Amitriptyline, imipramine |
↑Tricyclics | Therapeutic concentration monitoring is recommended for tricyclic antidepressants. |
a See Clinical Pharmacology (12.3) Tables 10, 11, 12, or 13 for magnitude of interaction.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C. Embryo/fetal development studies were conducted in rats (dosed from day 6 to day 17 of gestation) and rabbits (dosed from day 7 to day 20 of gestation). Administration of fosamprenavir to pregnant rats and rabbits produced no major effects on embryo-fetal development; however, the incidence of abortion was increased in rabbits that were administered fosamprenavir. Systemic exposures (AUC0-24 hr) to amprenavir at these dosages were 0.8 (rabbits) to 2 (rats) times the exposures in humans following administration of the maximum recommended human dose (MRHD) of fosamprenavir alone or 0.3 (rabbits) to 0.7 (rats) times the exposures in humans following administration of the MRHD of fosamprenavir in combination with ritonavir. In contrast, administration of amprenavir was associated with abortions and an increased incidence of minor skeletal variations resulting from deficient ossification of the femur, humerus, and trochlea, in pregnant rabbits at the tested dose; approximately one-twentieth the exposure seen at the recommended human dose.
The mating and fertility of the F1 generation born to female rats given fosamprenavir was not different from control animals; however, fosamprenavir did cause a reduction in both pup survival and body weights. Surviving F1 female rats showed an increased time to successful mating, an increased length of gestation, a reduced number of uterine implantation sites per litter, and reduced gestational body weights compared with control animals. Systemic exposure (AUC0-24 hr) to amprenavir in the F0 pregnant rats was approximately 2 times higher than exposures in humans following administration of the MRHD of fosamprenavir alone or approximately the same as those seen in humans following administration of the MRHD of fosamprenavir in combination with ritonavir.
There are no adequate and well-controlled studies in pregnant women. LEXIVA should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Antiretroviral Pregnancy Registry
To monitor maternal-fetal outcomes of pregnant women exposed to LEXIVA, an Antiretroviral Pregnancy Registry has been established. Physicians are encouraged to register patients by calling 1-800-258-4263.
8.3 Nursing Mothers
The Centers for Disease Control and Prevention recommend that HIV-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV. Although it is not known if amprenavir is excreted in human milk, amprenavir is secreted into the milk of lactating rats. Because of both the potential for HIV transmission and the potential for serious adverse reactions in nursing infants, mothers should be instructed not to breastfeed if they are receiving LEXIVA.
8.4 Pediatric Use
The safety, pharmacokinetic profile, and virologic response of LEXIVA Oral Suspension and Tablets were evaluated in pediatric patients 2 to 18 years of age in 2 open-label studies [see Clinical Studies (14.3)]. No data are available for pediatric patients <2 years of age.
The adverse reaction profile seen in pediatrics was similar to that seen in adults. Vomiting, regardless of causality, was more frequent in pediatrics than in adults [see Adverse Reactions (6.1)].
8.5 Geriatric Use
Clinical studies of LEXIVA did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger adults. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
Amprenavir is principally metabolized by the liver; therefore, caution should be exercised when administering LEXIVA to patients with hepatic impairment because amprenavir concentrations may be increased [see Clinical Pharmacology (12.3)]. Patients with impaired hepatic function receiving LEXIVA with or without concurrent ritonavir require dose reduction [see Dosage and Administration (2.3)].
10 OVERDOSAGE
In a healthy volunteer repeat-dose pharmacokinetic study evaluating high-dose combinations of LEXIVA plus ritonavir, an increased frequency of Grade 2/3 ALT elevations (>2.5 x ULN) was observed with LEXIVA 1,400 mg twice daily plus ritonavir 200 mg twice daily (4 of 25 subjects). Concurrent Grade 1/2 elevations in AST (>1.25 x ULN) were noted in 3 of these 4 subjects. These transaminase elevations resolved following discontinuation of dosing.
There is no known antidote for LEXIVA. It is not known whether amprenavir can be removed by peritoneal dialysis or hemodialysis. If overdosage occurs, the patient should be monitored for evidence of toxicity and standard supportive treatment applied as necessary.
11 DESCRIPTION
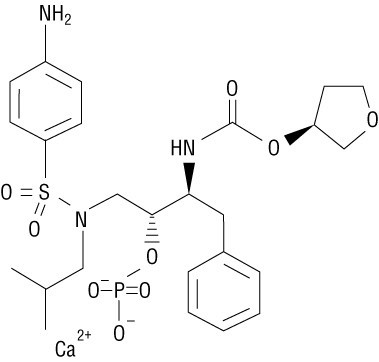
LEXIVA (fosamprenavir calcium) is a prodrug of amprenavir, an inhibitor of HIV protease. The chemical name of fosamprenavir calcium is (3S)-tetrahydrofuran-3-yl (1S,2R)-3-[[(4-aminophenyl) sulfonyl](isobutyl)amino]-1-benzyl-2-(phosphonooxy) propylcarbamate monocalcium salt. Fosamprenavir calcium is a single stereoisomer with the (3S)(1S,2R) configuration. It has a molecular formula of C25H34CaN3O9PS and a molecular weight of 623.7. It has the following structural formula:
Fosamprenavir calcium is a white to cream-colored solid with a solubility of approximately 0.31 mg/mL in water at 25°C.
LEXIVA Tablets are available for oral administration in a strength of 700 mg of fosamprenavir as fosamprenavir calcium (equivalent to approximately 600 mg of amprenavir). Each 700-mg tablet contains the inactive ingredients colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, microcrystalline cellulose, and povidone K30. The tablet film-coating contains the inactive ingredients hypromellose, iron oxide red, titanium dioxide, and triacetin.
LEXIVA Oral Suspension is available in a strength of 50 mg/mL of fosamprenavir as fosamprenavir calcium equivalent to approximately 43 mg of amprenavir. LEXIVA Oral Suspension is a white to off-white suspension with a grape-bubblegum-peppermint flavor. Each one milliliter (1 mL) contains the inactive ingredients artificial grape-bubblegum flavor, calcium chloride dihydrate, hypromellose, methylparaben, natural peppermint flavor, polysorbate 80, propylene glycol, propylparaben, purified water, and sucralose.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fosamprenavir is an antiviral agent [see Clinical Pharmacology (12.4)].
12.3 Pharmacokinetics
The pharmacokinetic properties of amprenavir after administration of LEXIVA, with or without ritonavir, have been evaluated in both healthy adult volunteers and in HIV-infected patients; no substantial differences in steady-state amprenavir concentrations were observed between the 2 populations.
The pharmacokinetic parameters of amprenavir after administration of LEXIVA (with and without concomitant ritonavir) are shown in Table 7.
|
aData shown are median (range). |
||||
|
Regimen |
Cmax (mcg/mL) |
Tmax (hours) a |
AUC24 (mcg•hr/mL) |
Cmin (mcg/mL) |
|
LEXIVA 1,400 mg b.i.d. |
4.82 (4.06-5.72) |
1.3 (0.8-4.0) |
33.0 (27.6-39.2) |
0.35 (0.27-0.46) |
|
LEXIVA 1,400 mg q.d. plus Ritonavir 200 mg q.d. |
7.24 (6.32-8.28) |
2.1 (0.8-5.0) |
69.4 (59.7-80.8) |
1.45 (1.16-1.81) |
|
LEXIVA 1,400 mg q.d. plus Ritonavir 100 mg q.d. |
7.93 (7.25-8.68) |
1.5 (0.75-5.0) |
66.4 (61.1-72.1) |
0.86 (0.74-1.01) |
|
LEXIVA 700 mg b.i.d. plus Ritonavir 100 mg b.i.d. |
6.08 (5.38-6.86) |
1.5 (0.75-5.0) |
79.2 (69.0-90.6) |
2.12 (1.77-2.54) |
The mean plasma amprenavir concentrations of the dosing regimens over the dosing intervals are displayed in Figure 1.

Absorption and Bioavailability
After administration of a single dose of LEXIVA to HIV-1-infected patients, the time to peak amprenavir concentration (Tmax) occurred between 1.5 and 4 hours (median 2.5 hours). The absolute oral bioavailability of amprenavir after administration of LEXIVA in humans has not been established.
After administration of a single 1,400-mg dose in the fasted state, LEXIVA Oral Suspension (50 mg/mL) and LEXIVA Tablets (700 mg) provided similar amprenavir exposures (AUC), however, the Cmax of amprenavir after administration of the suspension formulation was 14.5% higher compared with the tablet.
Effects of Food on Oral Absorption
Administration of a single 1,400-mg dose of LEXIVA Tablets in the fed state (standardized high-fat meal: 967 kcal, 67 grams fat, 33 grams protein, 58 grams carbohydrate) compared with the fasted state was associated with no significant changes in amprenavir Cmax, Tmax, or AUC0-∞ [see Dosage and Administration (2)].
Administration of a single 1,400-mg dose of LEXIVA Oral Suspension in the fed state (standardized high-fat meal: 967 kcal, 67 grams fat, 33 grams protein, 58 grams carbohydrate) compared with the fasted state was associated with a 46% reduction in Cmax, a 0.72-hour delay in Tmax, and a 28% reduction in amprenavir AUC0-∞.
Distribution
In vitro, amprenavir is approximately 90% bound to plasma proteins, primarily to alpha1-acid glycoprotein. In vitro, concentration-dependent binding was observed over the concentration range of 1 to 10 mcg/mL, with decreased binding at higher concentrations. The partitioning of amprenavir into erythrocytes is low, but increases as amprenavir concentrations increase, reflecting the higher amount of unbound drug at higher concentrations.
Metabolism
After oral administration, fosamprenavir is rapidly and almost completely hydrolyzed to amprenavir and inorganic phosphate prior to reaching the systemic circulation. This occurs in the gut epithelium during absorption. Amprenavir is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system. The 2 major metabolites result from oxidation of the tetrahydrofuran and aniline moieties. Glucuronide conjugates of oxidized metabolites have been identified as minor metabolites in urine and feces.
Elimination
Excretion of unchanged amprenavir in urine and feces is minimal. Unchanged amprenavir in urine accounts for approximately 1% of the dose; unchanged amprenavir was not detectable in feces. Approximately 14% and 75% of an administered single dose of 14C-amprenavir can be accounted for as metabolites in urine and feces, respectively. Two metabolites accounted for >90% of the radiocarbon in fecal samples. The plasma elimination half-life of amprenavir is approximately 7.7 hours.
Special Populations
Hepatic Impairment
The pharmacokinetics of amprenavir have been studied after the administration of LEXIVA in combination with ritonavir to adult HIV-1-infected patients with mild, moderate, and severe hepatic impairment. Following 2 weeks of dosing with LEXIVA plus ritonavir, the AUC of amprenavir was increased by approximately 22% in patients with mild hepatic impairment, by approximately 70% in patients with moderate hepatic impairment, and by approximately 80% in patients with severe hepatic impairment compared with HIV-1-infected patients with normal hepatic function. Protein binding of amprenavir was decreased in patients with hepatic impairment. The unbound fraction at 2 hours (approximate Cmax) ranged between a decrease of -7% to an increase of 57% while the unbound fraction at the end of the dosing interval (Cmin) increased from 50% to 102% [see Dosage and Administration (2.3)].
The pharmacokinetics of amprenavir have been studied after administration of amprenavir given as AGENERASE® Capsules to adult patients with hepatic impairment. Following administration of a single 600-mg oral dose the AUC of amprenavir was increased by approximately 2.5-fold in patients with moderate cirrhosis and by approximately 4.5-fold in patients with severe cirrhosis compared with healthy volunteers [see Dosage and Administration (2.3)].
Renal Impairment
The impact of renal impairment on amprenavir elimination in adult patients has not been studied. The renal elimination of unchanged amprenavir represents approximately 1% of the administered dose; therefore, renal impairment is not expected to significantly impact the elimination of amprenavir.
Pediatric Patients
The pharmacokinetics of amprenavir after administration of LEXIVA Oral Suspension and LEXIVA Tablets, with or without ritonavir, have been evaluated in 124 patients 2 to 18 years of age. Pharmacokinetic parameters for LEXIVA administered with food and with or without ritonavir in this patient population are provided in Tables 8 and 9 below.
|
Parameter |
2 to 5 Years |
|
|
n |
LEXIVA 30 mg/kg b.i.d. |
|
|
AUC(24) (mcg•hr/mL) |
8 |
31.4 (13.7, 72.4) |
|
Cmax (mcg/mL) |
8 |
5.00 (1.95, 12.8) |
|
Cmin (mcg/mL) |
17 |
0.454 (0.342, 0.604) |
|
Parameter |
6 to 11 Years |
12 to 18 Years |
||
|
n |
LEXIVA 18 mg/kg plus Ritonavir 3 mg/kg b.i.d. |
n |
LEXIVA 700 mg plus Ritonavir 100 mg b.i.d. |
|
|
AUC(0-24) (mcg•hr/mL) |
9 |
93.4 (67.8, 129) |
8 |
58.8 (38.8, 89.0) |
|
Cmax (mcg/mL) |
9 |
6.07 (4.40, 8.38) |
8 |
4.33 (2.82, 6.65) |
|
Cmin (mcg/mL) |
17 |
2.69 (2.15, 3.36) |
24 |
1.61 (1.21, 2.15) |
Geriatric Patients
The pharmacokinetics of amprenavir after administration of LEXIVA to patients over 65 years of age have not been studied [see Use in Specific Populations (8.5)].
Gender
The pharmacokinetics of amprenavir after administration of LEXIVA do not differ between males and females.
Race
The pharmacokinetics of amprenavir after administration of LEXIVA do not differ between blacks and non-blacks.
Drug Interactions
[See Contraindications (4), Warnings and Precautions (5.1), Drug Interactions (7).]
Amprenavir, the active metabolite of fosamprenavir, is metabolized in the liver by the cytochrome P450 enzyme system. Amprenavir inhibits CYP3A4. Data also suggest that amprenavir induces CYP3A4. Caution should be used when coadministering medications that are substrates, inhibitors, or inducers of CYP3A4, or potentially toxic medications that are metabolized by CYP3A4. Amprenavir does not inhibit CYP2D6, CYP1A2, CYP2C9, CYP2C19, CYP2E1, or uridine glucuronosyltransferase (UDPGT).
Drug interaction studies were performed with LEXIVA and other drugs likely to be coadministered or drugs commonly used as probes for pharmacokinetic interactions. The effects of coadministration on AUC, Cmax, and Cmin values are summarized in Table 10 (effect of other drugs on amprenavir) and Table 12 (effect of LEXIVA on other drugs). In addition, since LEXIVA delivers comparable amprenavir plasma concentrations as AGENERASE, drug interaction data derived from studies with AGENERASE are provided in Tables 11 and 13. For information regarding clinical recommendations, see Drug Interactions (7).
|
Coadministered Drug(s) and Dose(s) |
Dose of LEXIVA a |
n | % Change in Amprenavir Pharmacokinetic Parameters (90% CI) | ||
| Cmax | AUC | Cmin | |||
|
Antacid (MAALOX TC®) 30 mL single dose |
1,400 mg single dose |
30 |
↓35 (↓24 to ↓42) |
↓18 (↓9 to ↓26) |
↑14 (↓7 to ↑39) |
|
Atazanavir 300 mg q.d. for 10 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 10 days |
22 | ↔ | ↔ | ↔ |
|
Atorvastatin 10 mg q.d. for 4 days |
1,400 mg b.i.d. for 2 weeks |
16 |
↓18 (↓34 to ↑1) |
↓27 (↓41 to ↓12) |
↓12 (↓27 to ↓6) |
|
Atorvastatin 10 mg q.d. for 4 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
16 | ↔ | ↔ | ↔ |
|
Efavirenz 600 mg q.d. for 2 weeks |
1,400 mg q.d. plus ritonavir 200 mg q.d. for 2 weeks |
16 | ↔ |
↓13 (↓30 to ↑7) |
↓36 (↓8 to ↓56) |
|
Efavirenz 600 mg q.d. plus additional ritonavir 100 mg q.d. for 2 weeks |
1,400 mg q.d. plus ritonavir 200 mg q.d. for 2 weeks |
16 |
↑18 (↑1 to ↑38) |
↑11 (0 to ↑24) |
↔ |
|
Efavirenz 600 mg q.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
16 | ↔ | ↔ |
↓17 (↓4 to ↓29) |
|
Esomeprazole 20 mg q.d. for 2 weeks |
1,400 mg b.i.d. for 2 weeks | 25 | ↔ | ↔ | ↔ |
|
Esomeprazole 20 mg q.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
23 | ↔ | ↔ | ↔ |
|
Ethinyl estradiol/norethin-drone 0.035 mg/0.5 mg q.d. for 21 days |
700 mg b.i.d. plus ritonavirb 100 mg b.i.d. for 21 days |
25 |
↔c |
↔c |
↔c |
|
Ketoconazoled 200 mg q.d. for 4 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 4 days |
15 | ↔ | ↔ | ↔ |
|
Lopinavir/ritonavir 533 mg/133 mg b.i.d. |
1,400 mg b.i.d. for 2 weeks |
18 | ↓13e | ↓26e | ↓42e |
|
Lopinavir/ritonavir 400 mg/100 mg b.i.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
18 |
↓58 (↓42 to ↓70) |
↓63 (↓51 to ↓72) |
↓65 (↓54 to ↓73) |
|
Methadone 70 to 120 mg q.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
19 | ↔c | ↔c | ↔c |
|
Nevirapine 200 mg b.i.d. for 2 weeksf |
1,400 mg b.i.d. for 2 weeks | 17 |
↓25 (↓37 to ↓10) |
↓33 (↓45 to ↓20) |
↓35 (↓50 to ↓15) |
|
Nevirapine 200 mg b.i.d. for 2 weeksf |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
17 | ↔ |
↓11 (↓23 to ↑3) |
↓19 (↓32 to ↓4) |
|
Phenytoin 300 mg q.d. for 10 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 10 days |
13 | ↔ |
↑20 (↑8 to ↑34) |
↑19 (↑6 to ↑33) |
|
Ranitidine 300 mg single dose (administered 1 hour before fosamprenavir) |
1,400 mg single dose |
30 |
↓51 (↓43 to ↓58) |
↓30 (↓22 to ↓37) |
↔ (↓19 to ↑21) |
|
Rifabutin 150 mg q.o.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
15 |
↑36c (↑18 to ↑55) |
↑35c (↑17 to ↑56) |
↑17c (↓1 to ↑39) |
|
Tenofovir 300 mg q.d. for 4 to 48 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 4 to 48 weeks |
45 | NA | NA | ↔g |
|
Tenofovir 300 mg q.d. for 4 to 48 weeks |
1,400 mg q.d. plus ritonavir 200 mg q.d. for 4 to 48 weeks |
60 | NA | NA | ↔g |
a Concomitant medication is also shown in this column where appropriate.
b Ritonavir Cmax, AUC, and Cmin increased by 63%, 45%, and 13%, respectively, compared with historical control.
c Compared with historical control.
d Patients were receiving LEXIVA/ritonavir for 10 days prior to the 4-day treatment period with both ketoconazole and LEXIVA/ritonavir.
e Compared with LEXIVA 700 mg/ritonavir 100 mg b.i.d. for 2 weeks.
f Patients were receiving nevirapine for at least 12 weeks prior to study.
g Compared with parallel control group.
↑= Increase; ↓= Decrease; ↔ = No change (↑or ↓≤10%), NA = Not applicable.
|
Coadministered Drug(s) and Dose(s) |
Dose of AGENERASE a |
n |
% Change in Amprenavir Pharmacokinetic Parameters (90% CI) |
||
| Cmax | AUC | Cmin | |||
|
Abacavir 300 mg b.i.d. for 2 to 3 weeks |
900 mg b.i.d. for 2 to 3 weeks |
4 | ↔a | ↔a | ↔a |
|
Clarithromycin 500 mg b.i.d. for 4 days |
1,200 mg b.i.d. for 4 days |
12 |
↑15 (↑1 to ↑31) |
↑18 (↑8 to ↑29) |
↑39 (↑31 to ↑47) |
|
Delavirdine 600 mg b.i.d. for 10 days |
600 mg b.i.d. for 10 days |
9 | ↑40b | ↑130b | ↑125b |
|
Ethinyl estradiol/norethindrone 0.035 mg/1 mg for 1 cycle |
1,200 mg b.i.d. for 28 days |
10 |
↔ |
↓22 (↓35 to ↓8) |
↓20 (↓41 to ↑8) |
|
Indinavir 800 mg t.i.d. for 2 weeks (fasted) |
750 or 800 mg t.i.d. for 2 weeks (fasted) | 9 |
↑18 (↑13 to ↑58) |
↑33 (↑2 to ↑73) |
↑25 (↓27 to ↑116) |
|
Ketoconazole 400 mg single dose |
1,200 mg single dose |
12 |
↓16 (↓25 to ↓6) |
↑31 (↑20 to ↑42) |
NA |
|
Lamivudine 150 mg single dose |
600 mg single dose |
11 | ↔ | ↔ | NA |
|
Methadone 44 to 100 mg q.d. for >30 days |
1,200 mg b.i.d. for 10 days |
16 | ↓27c | ↓30c | ↓25c |
|
Nelfinavir 750 mg t.i.d. for 2 weeks (fed) |
750 or 800 mg t.i.d. for 2 weeks (fed) | 6 |
↓14 (↓38 to ↑20) |
↔ |
↑189 (↑52 to ↑448) |
|
Rifabutin 300 mg q.d. for 10 days |
1,200 mg b.i.d. for 10 days |
5 |
↔ |
↓15 (↓28 to 0) |
↓15 (↓38 to ↑17) |
|
Rifampin 300 mg q.d. for 4 days |
1,200 mg b.i.d. for 4 days |
11 |
↓70 (↓76 to ↓62) |
↓82 (↓84 to ↓78) |
↓92 (↓95 to ↓89) |
|
Saquinavir 800 mg t.i.d. for 2 weeks (fed) |
750 or 800 mg t.i.d. for 2 weeks (fed) | 7 |
↓37 (↓54 to ↓14) |
↓32 (↓49 to ↓9) |
↓14 (↓52 to ↑54) |
|
Zidovudine 300 mg single dose |
600 mg single dose |
12 | ↔ |
↑13 (↓2 to ↑31) |
NA |
a Compared with parallel control group.
b Median percent change; confidence interval not reported.
c Compared with historical data.
↑ = Increase; ↓ = Decrease; ↔= No change (↑or ↓<10%); NA = Cmin not calculated for single-dose study.
|
Coadministered Drug(s) and Dose(s) |
Dose of LEXIVA a |
n |
% Change in Pharmacokinetic Parameters of Coadministered Drug (90% CI) | ||
| Cmax | AUC | Cmin | |||
|
Atazanavir 300 mg q.d. for 10 daysb |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 10 days |
21 |
↓24 (↓39 to ↓6) |
↓22 (↓34 to ↓9) |
↔ |
|
Atorvastatin 10 mg q.d. for 4 days |
1,400 mg b.i.d. for 2 weeks |
16 |
↑304 (↑205 to ↑437) |
↑130 (↑100 to ↑164) |
↓10 (↓27 to ↑12) |
|
Atorvastatin 10 mg q.d. for 4 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
16 |
↑184 (↑126 to ↑257) |
↑153 (↑115 to ↑199) |
↑73 (↑45 to ↑108) |
|
Esomeprazole 20 mg q.d. for 2 weeks |
1,400 mg b.i.d. for 2 weeks | 25 | ↔ |
↑55 (↑39 to ↑73) |
ND |
|
Esomeprazole 20 mg q.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for2 weeks |
23 | ↔ | ↔ | ND |
|
Ethinyl estradiolc 0.035 mg q.d. for 21 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 21 days |
25 |
↓28 (↓21 to ↓35) |
↓37 (↓30 to ↓42) |
ND |
|
Ketoconazoled 200 mg q.d. for 4 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 4 days |
15 |
↑25 (↑0 to ↑56) |
↑169 (↑108 to ↑248) |
ND |
|
Lopinavir/ritonavire 533 mg/133 mg b.i.d. for 2 weeks |
1,400 mg b.i.d. for 2 weeks |
18 | ↔f | ↔f | ↔f |
|
Lopinavir/ritonavire 400 mg/100 mg b.i.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
18 |
↑30 (↓15 to ↑47) |
↑37 (↓20 to ↑55) |
↑52 (↓28 to ↑82) |
|
Methadone 70 to 120 mg q.d. for 2 weeks |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
19 | R-Methadone (active) | ||
|
↓21g (↓30 to ↓12) |
↓18g (↓27 to ↓8) |
↓11g (↓21 to ↑1) |
|||
| S-Methadone (inactive) | |||||
|
↓43g (↓49 to ↓37) |
↓43g (↓50 to ↓36) |
↓41g (↓49 to ↓31) |
|||
|
Nevirapine 200 mg b.i.d. for 2 weeksh |
1,400 mg b.i.d. for 2 weeks |
17 |
↑25 (↑14 to ↑37) |
↑29 (↑19 to ↑40) |
↑34 (↑20 to ↑49) |
|
Nevirapine 200 mg b.i.d. for 2 weeks h |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks | 17 |
↑13 (↑3 to ↑24) |
↑14 (↑5 to ↑24) |
↑22 (↑9 to ↑35) |
|
Norethindronec 0.5 mg q.d. for 21 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 21 days |
25 |
↓38 (↓32 to ↓44) |
↓34 (↓30 to ↓37) |
↓26 (↓20 to ↓32) |
|
Phenytoin 300 mg q.d. for 10 days |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 10 days |
14 |
↓20 (↓12 to ↓27) |
↓22 (↓17 to ↓27) |
↓29 (↓23 to ↓34) |
|
Rifabutin 150 mg every other day for 2 weeks c (25-O-desacetylrifabutin metabolite) Rifabutin + 25-O- desacetylrifabutin metabolite |
700 mg b.i.d. plus ritonavir 100 mg b.i.d. for 2 weeks |
15 |
↓14 (↓28 to ↑4) ↑579 (↑479 to ↑698) NA |
↔ ↑1,120 (↑965 to ↑1,300) ↑64 (↑46 to ↑84) |
↑28 (↑12 to ↑46) ↑2,510 (↑1,910 to ↑3,300) NA |
a Concomitant medication is also shown in this column where appropriate.
b Comparison arm of atazanavir 300 mg q.d. plus ritonavir 100 mg q.d. for 10 days.
c Administered as a combination oral contraceptive tablet: ethinyl estradiol 0.035 mg/norethindrone 0.5 mg.
d Patients were receiving LEXIVA/ritonavir for 10 days prior to the 4-day treatment period with both ketoconazole and LEXIVA/ritonavir.
e Data represent lopinavir concentrations.
f Compared with lopinavir 400 mg/ritonavir 100 mg b.i.d. for 2 weeks.
g Dose normalized to methadone 100 mg. The unbound concentration of the active moiety, R-methadone, was unchanged.
h Patients were receiving nevirapine for at least 12 weeks prior to study.††Comparison arm of rifabutin 300 mg q.d. for 2 weeks. AUC is AUC(0-48 hr).
↑= Increase; ↓= Decrease; ↔ = No change (↑or ↓<10%); ND = Interaction cannot be determined as Cmin was below the lower limit of quantitation.
|
Coadministered Drug(s) and Dose(s) |
Dose of AGENERASE | n | % Change in Pharmacokinetic Parameters of Coadministered Drug (90% CI) | ||
| Cmax | AUC | Cmin | |||
|
Abacavir 300 mg b.i.d. for 2 to 3 weeks |
900 mg b.i.d for 2 to 3 weeks |
4 | ↔a | ↔a | ↔a |
|
Clarithromycin 500 mg b.i.d. for 4 days |
1,200 mg b.i.d. for 4 days |
12 |
↓10 (↓24 to ↑7) |
↔ |
↔ |
|
Delavirdine 600 mg b.i.d. for 10 days |
600 mg b.i.d. for 10 days |
9 | ↓47b | ↓61b | ↓88b |
|
Ethinyl estradiol 0.035 mg for 1 cycle |
1,200 mg b.i.d. for 28 days |
10 | ↔ | ↔ |
↑32 (↓3 to ↑79) |
|
Indinavir 800 mg t.i.d. for 2 weeks (fasted) |
750 mg or 800 mg t.i.d. for 2 weeks (fasted) | 9 | ↓22a | ↓38a | ↓27a |
|
Ketoconazole 400 mg single dose |
1,200 mg single dose |
12 |
↑19 (↑8 to ↑33) |
↑44 (↑31 to ↑59) |
NA |
|
Lamivudine 150 mg single dose |
600 mg single dose |
11 | ↔ | ↔ | NA |
|
Methadone 44 to 100 mg q.d. for >30 days |
1,200 mg b.i.d. for 10 days |
16 | R-Methadone (active) | ||
|
↓25 (↓32 to ↓18) |
↓13 (↓21 to ↓5) |
↓21 (↓32 to ↓9) |
|||
| S-Methadone (inactive) | |||||
|
↓48 (↓55 to ↓40) |
↓40 (↓46 to ↓32) |
↓53 (↓60 to ↓43) |
|||
|
Nelfinavir 750 mg t.i.d. for 2 weeks (fed) |
750 mg or 800 mg t.i.d. for 2 weeks (fed) | 6 | ↑12a | ↑15a | ↑14a |
|
Norethindrone 1 mg for 1 cycle |
1,200 mg b.i.d. for 28 days |
10 | ↔ |
↑18 (↑1 to ↑38) |
↑45 (↑13 to ↑88) |
|
Rifabutin 300 mg q.d. for 10 days |
1,200 mg b.i.d. for 10 days |
5 |
↑119 (↑82 to ↑164) |
↑193 (↑156 to ↑235) |
↑271 (↑171 to ↑409) |
|
Rifampin 300 mg q.d. for 4 days |
1,200 mg b.i.d. for 4 days |
11 | ↔ | ↔ | ND |
|
Saquinavir 800 mg t.i.d. for 2 weeks (fed) |
750 mg or 800 mg t.i.d. for 2 weeks (fed) | 7 | ↑21a | ↓19a | ↓48a |
|
Zidovudine 300 mg single dose |
600 mg single dose |
12 |
↑40 (↑14 to ↑71) |
↑31 (↑19 to ↑45) |
NA |
a Compared with historical data.
b Median percent change; confidence interval not reported.
↑ = Increase; ↓ = Decrease; ↔= No change (↑or ↓<10%); NA = Cmin not calculated for single-dose study; ND = Interaction cannot be determined as Cmin was below the lower limit of quantitation.
Microbiology
Mechanism of Action
Fosamprenavir is a prodrug that is rapidly hydrolyzed to amprenavir by cellular phosphatases in the gut epithelium as it is absorbed. Amprenavir is an inhibitor of HIV-1 protease. Amprenavir binds to the active site of HIV-1 protease and thereby prevents the processing of viral Gag and Gag-Pol polyprotein precursors, resulting in the formation of immature non-infectious viral particles.
Antiviral Activity
Fosamprenavir has little or no antiviral activity in vitro. The in vitro antiviral activity of amprenavir was evaluated against HIV-1 IIIB in both acutely and chronically infected lymphoblastic cell lines (MT-4, CEM-CCRF, H9) and in peripheral blood lymphocytes. The 50% effective concentration (EC50) of amprenavir ranged from 0.012 to 0.08 μM in acutely infected cells and was 0.41 μM in chronically infected cells (1 μM = 0.50 mcg/mL). The median EC50 value of amprenavir against HIV-1 isolates from clades A to G was 0.00095 µM in peripheral blood mononuclear cells (PBMCs). Similarly, the EC50 values for amprenavir against monocytes/macrophage tropic HIV-1 isolates (clade B) ranged from 0.003 to 0.075 µM in monocyte/macrophage cultures. The EC50 values of amprenavir against HIV-2 isolates grown in PBMCs were higher than those for HIV-1 isolates, and ranged from 0.003 to 0.11 µM. Amprenavir exhibited synergistic anti–HIV-1 activity in combination with the nucleoside reverse transcriptase inhibitors (NRTIs) abacavir, didanosine, lamivudine, stavudine, tenofovir, and zidovudine; the non-nucleoside reverse transcriptase inhibitors (NNRTIs) delavirdine and efavirenz; and the protease inhibitors atazanavir and saquinavir. Amprenavir exhibited additive anti–HIV-1 activity in combination with the NNRTI nevirapine, the protease inhibitors indinavir, lopinavir, nelfinavir, and ritonavir; and the fusion inhibitor enfuvirtide. These drug combinations have not been adequately studied in humans.
Resistance
HIV-1 isolates with decreased susceptibility to amprenavir have been selected in vitro and obtained from patients treated with fosamprenavir. Genotypic analysis of isolates from treatment-naive patients failing amprenavir-containing regimens showed mutations in the HIV-1 protease gene resulting in amino acid substitutions primarily at positions V32I, M46I/L, I47V, I50V, I54L/M, and I84V, as well as mutations in the p7/p1 and p1/p6 Gag and Gag-Pol polyprotein precursor cleavage sites. Some of these amprenavir resistance-associated mutations have also been detected in HIV-1 isolates from antiretroviral-naive patients treated with LEXIVA. Of the 488 antiretroviral-naive patients treated with LEXIVA 1,400 mg twice daily or LEXIVA 1,400 mg plus ritonavir 200 mg once daily in studies APV30001 and APV30002, respectively, 61 patients (29 receiving LEXIVA and 32 receiving LEXIVA/ritonavir) with virologic failure (plasma HIV-1 RNA >1,000 copies/mL on 2 occasions on or after Week 12) were genotyped. Five of the 29 antiretroviral-naive patients (17%) receiving LEXIVA without ritonavir in study APV30001 had evidence of genotypic resistance to amprenavir: I54L/M (n = 2), I54L + L33F (n = 1), V32I + I47V (n = 1), and M46I + I47V (n = 1). No amprenavir resistance-associated mutations were detected in antiretroviral-naive patients treated with LEXIVA/ritonavir for 48 weeks in study APV30002. However, the M46I and I50V mutations were detected in isolates from 1 virologic failure patient receiving LEXIVA/ritonavir once daily at Week 160 (HIV-1 RNA >500 copies/mL). Upon retrospective analysis of stored samples using an ultrasensitive assay, these resistant mutants were traced back to Week 84 (76 weeks prior to clinical virologic failure).
Cross-Resistance
Varying degrees of cross-resistance among HIV-1 protease inhibitors have been observed. An association between virologic response at 48 weeks (HIV-1 RNA level <400 copies/mL) and protease inhibitor-resistance mutations detected in baseline HIV-1 isolates from protease inhibitor-experienced patients receiving LEXIVA/ritonavir twice daily (n = 88), or lopinavir/ritonavir twice daily (n = 85) in study APV30003 is shown in Table 14. The majority of subjects had previously received either one (47%) or 2 protease inhibitors (36%), most commonly nelfinavir (57%) and indinavir (53%). Out of 102 subjects with baseline phenotypes receiving twice-daily LEXIVA/ritonavir, 54% (n = 55) had resistance to at least one protease inhibitor, with 98% (n = 54) of those having resistance to nelfinavir. Out of 97 subjects with baseline phenotypes in the lopinavir/ritonavir arm, 60% (n = 58) had resistance to at least one protease inhibitor, with 97% (n = 56) of those having resistance to nelfinavir.
|
aResults should be interpreted with caution because the subgroups were small. |
||||
|
bMost patients had >1 protease inhibitor resistance-associated mutation at baseline. |
||||
|
PI-mutationsb |
LEXIVA/Ritonavir b.i.d. (n = 88) |
Lopinavir/Ritonavir b.i.d. (n = 85) |
||
|
D30N |
21/22 |
95% |
17/19 |
89% |
|
N88D/S |
20/22 |
91% |
12/12 |
100% |
|
L90M |
16/31 |
52% |
17/29 |
59% |
|
M46I/L |
11/22 |
50% |
12/24 |
50% |
|
V82A/F/T/S |
2/9 |
22% |
6/17 |
35% |
|
I54V |
2/11 |
18% |
6/11 |
55% |
|
I84V |
1/6 |
17% |
2/5 |
40% |
The virologic response based upon baseline phenotype was assessed. Baseline isolates from protease inhibitor-experienced patients responding to LEXIVA/ritonavir twice daily had a median shift in susceptibility to amprenavir relative to a standard wild-type reference strain of 0.7 (range: 0.1 to 5.4, n = 62), and baseline isolates from individuals failing therapy had a median shift in susceptibility of 1.9 (range: 0.2 to 14, n = 29). Because this was a select patient population, these data do not constitute definitive clinical susceptibility break points. Additional data are needed to determine clinically relevant break points for LEXIVA.
Isolates from 15 of the 20 patients receiving twice-daily LEXIVA/ritonavir up to Week 48 and experiencing virologic failure/ongoing replication were subjected to genotypic analysis. The following amprenavir resistance-associated mutations were found either alone or in combination: V32I, M46I/L, I47V, I50V, I54L/M, and I84V. Isolates from 4 of the 16 patients continuing to receive twice-daily LEXIVA/ritonavir up to Week 96 who experienced virologic failure underwent genotypic analysis. Isolates from 2 patients contained amprenavir resistance-associated mutations: V32I, M46I, and I47V in 1 isolate and I84V in the other.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In long-term carcinogenicity studies, fosamprenavir was administered orally for up to 104 weeks at doses of 250, 400, or 600 mg/kg/day in mice and at doses of 300, 825, or 2,250 mg/kg/day in rats. Exposures at these doses were 0.3- to 0.7-fold (mice) and 0.7- to 1.4-fold (rats) those in humans given 1,400 mg twice daily of fosamprenavir alone, and 0.2- to 0.3-fold (mice) and 0.3- to 0.7-fold (rats) those in humans given 1,400 mg once daily of fosamprenavir plus 200 mg ritonavir once daily. Exposures in the carcinogenicity studies were 0.1- to 0.3-fold (mice) and 0.3- to 0.6-fold (rats) those in humans given 700 mg of fosamprenavir plus 100 mg ritonavir twice daily. There was an increase in hepatocellular adenomas and hepatocellular carcinomas at all doses in male mice and at 600 mg/kg/day in female mice, and in hepatocellular adenomas and thyroid follicular cell adenomas at all doses in male rats, and at 835 mg/kg/day and 2,250 mg/kg/day in female rats. The relevance of the hepatocellular findings in the rodents for humans is uncertain. Repeat dose studies with fosamprenavir in rats produced effects consistent with enzyme induction, which predisposes rats, but not humans, to thyroid neoplasms. In addition, in rats only there was an increase in interstitial cell hyperplasia at 825 mg/kg/day and 2,250 mg/kg/day, and an increase in uterine endometrial adenocarcinoma at 2,250 mg/kg/day. The incidence of endometrial findings was slightly increased over concurrent controls, but was within background range for female rats. The relevance of the uterine endometrial adenocarcinoma findings in rats for humans is uncertain.
Fosamprenavir was not mutagenic or genotoxic in a battery of in vitro and in vivo assays. These assays included bacterial reverse mutation (Ames), mouse lymphoma, rat micronucleus, and chromosome aberrations in human lymphocytes.
The effects of fosamprenavir on fertility and general reproductive performance were investigated in male (treated for 4 weeks before mating) and female rats (treated for 2 weeks before mating through postpartum day 6). Systemic exposures (AUC0-24 hr) to amprenavir in these studies were 3 (males) to 4 (females) times higher than exposures in humans following administration of the MRHD of fosamprenavir alone or similar to those seen in humans following administration of fosamprenavir in combination with ritonavir. Fosamprenavir did not impair mating or fertility of male or female rats and did not affect the development and maturation of sperm from treated rats.
14 CLINICAL STUDIES
Therapy-Naive Adult Patients
Study APV30001
APV30001 was a randomized, open-label study, comparing treatment with LEXIVA Tablets (1,400 mg twice daily) versus nelfinavir (1,250 mg twice daily) in 249 antiretroviral treatment-naive patients. Both groups of patients also received abacavir (300 mg twice daily) and lamivudine (150 mg twice daily).
The mean age of the patients in this study was 37 years (range: 17 to 70 years), 69% of the patients were males, 20% were CDC Class C (AIDS), 24% were Caucasian, 32% were black, and 44% were Hispanic. At baseline, the median CD4+ cell count was 212 cells/mm3 (range: 2 to 1,136 cells/mm3; 18% of patients had a CD4+ cell count of <50 cells/mm3 and 30% were in the range of 50 to <200 cells/mm3). Baseline median HIV-1 RNA was 4.83 log10 copies/mL (range: 1.69 to 7.41 log10 copies/mL; 45% of patients had >100,000 copies/mL).
The outcomes of randomized treatment are provided in Table 15.
|
a Patients achieved and maintained confirmed HIV-1 RNA <400 copies/mL (<50 copies/mL) through Week 48 (Roche AMPLICOR HIV-1 MONITOR Assay Version 1.5). |
||
|
b Includes consent withdrawn, lost to follow up, protocol violations, those with missing data, and other reasons. |
||
|
Outcome (Rebound or discontinuation = failure) |
LEXIVA 1,400 mg b.i.d. (n = 166) |
Nelfinavir 1,250 mg b.i.d. (n = 83) |
|
Respondera |
66% (57%) |
52% (42%) |
|
Virologic failure |
19% |
32% |
|
Rebound |
16% |
19% |
|
Never suppressed through Week 48 |
3% |
13% |
|
Clinical progression |
1% |
1% |
|
Death |
0% |
1% |
|
Discontinued due to adverse reactions |
4% |
2% |
|
Discontinued due to other reasonsb |
10% |
10% |
Treatment response by viral load strata is shown in Table 16.
|
Screening Viral Load HIV-1 RNA (copies/mL) |
LEXIVA 1,400 mg b.i.d. |
Nelfinavir 1,250 mg b.i.d. |
||
|
<400 copies/mL |
n |
<400 copies/mL |
n |
|
|
≤100,000 |
65% |
93 |
65% |
46 |
|
>100,000 |
67% |
73 |
36% |
37 |
Through 48 weeks of therapy, the median increases from baseline in CD4+ cell counts were 201 cells/mm3 in the group receiving LEXIVA and 216 cells/mm3 in the nelfinavir group.
Study APV30002
APV30002 was a randomized, open-label study, comparing treatment with LEXIVA Tablets (1,400 mg once daily) plus ritonavir (200 mg once daily) versus nelfinavir (1,250 mg twice daily) in 649 treatment-naive patients. Both treatment groups also received abacavir (300 mg twice daily) and lamivudine (150 mg twice daily).
The mean age of the patients in this study was 37 years (range: 18 to 69 years), 73% of the patients were males, 22% were CDC Class C, 53% were Caucasian, 36% were black, and 8% were Hispanic. At baseline, the median CD4+ cell count was 170 cells/mm3 (range: 1 to 1,055 cells/mm3; 20% of patients had a CD4+ cell count of <50 cells/mm3 and 35% were in the range of 50 to <200 cells/mm3). Baseline median HIV-1 RNA was 4.81 log10 copies/mL (range: 2.65 to 7.29 log10 copies/mL; 43% of patients had >100,000 copies/mL).
The outcomes of randomized treatment are provided in Table 17.
|
a Patients achieved and maintained confirmed HIV-1 RNA <400 copies/mL (<50 copies/mL) through Week 48 (Roche AMPLICOR HIV-1 MONITOR Assay Version 1.5). |
||
|
b Includes consent withdrawn, lost to follow up, protocol violations, those with missing data, and other reasons. |
||
|
Outcome (Rebound or discontinuation = failure) |
LEXIVA 1,400 mg q.d./ Ritonavir 200 mg q.d. (n = 322) |
Nelfinavir 1,250 mg b.i.d. (n = 327) |
|
Respondera |
69% (58%) |
68% (55%) |
|
Virologic failure |
6% |
16% |
|
Rebound |
5% |
8% |
|
Never suppressed through Week 48 |
1% |
8% |
|
Death |
1% |
0% |
|
Discontinued due to adverse reactions |
9% |
6% |
|
Discontinued due to other reasonsb |
15% |
10% |
Treatment response by viral load strata is shown in Table 18.
|
Screening Viral Load HIV-1 RNA |
LEXIVA 1,400 mg q.d./Ritonavir 200 mg q.d. |
Nelfinavir 1,250 mg b.i.d. |
|||
|
(copies/mL) |
<400 copies/mL |
n |
<400 copies/mL |
n |
|
|
≤100,000 |
72% |
197 |
73% |
194 |
|
|
>100,000 |
66% |
125 |
64% |
133 |
|
Through 48 weeks of therapy, the median increases from baseline in CD4+ cell counts were 203 cells/mm3 in the group receiving LEXIVA and 207 cells/mm3 in the nelfinavir group.
Protease Inhibitor-Experienced Adult Patients
Study APV30003
APV30003 was a randomized, open-label, multicenter study comparing 2 different regimens of LEXIVA plus ritonavir (LEXIVA Tablets 700 mg twice daily plus ritonavir 100 mg twice daily or LEXIVA Tablets 1,400 mg once daily plus ritonavir 200 mg once daily) versus lopinavir/ritonavir (400 mg/100 mg twice daily) in 315 patients who had experienced virologic failure to 1 or 2 prior protease inhibitor-containing regimens.
The mean age of the patients in this study was 42 years (range: 24 to 72 years), 85% were male, 33% were CDC Class C, 67% were Caucasian, 24% were black, and 9% were Hispanic. The median CD4+ cell count at baseline was 263 cells/mm3 (range: 2 to 1,171 cells/mm3). Baseline median plasma HIV-1 RNA level was 4.14 log10 copies/mL (range: 1.69 to 6.41 log10 copies/mL).
The median durations of prior exposure to NRTIs were 257 weeks for patients receiving LEXIVA/ritonavir twice daily (79% had ≥3 prior NRTIs) and 210 weeks for patients receiving lopinavir/ritonavir (64% had ≥3 prior NRTIs). The median durations of prior exposure to protease inhibitors were 149 weeks for patients receiving LEXIVA/ritonavir twice daily (49% received ≥2 prior protease inhibitors) and 130 weeks for patients receiving lopinavir/ritonavir (40% received ≥2 prior protease inhibitors).
The time-averaged changes in plasma HIV-1 RNA from baseline (AAUCMB) at 48 weeks (the endpoint on which the study was powered) were -1.4 log10 copies/mL for twice-daily LEXIVA/ritonavir and -1.67 log10 copies/mL for the lopinavir/ritonavir group.
The proportions of patients who achieved and maintained confirmed HIV-1 RNA <400 copies/mL (secondary efficacy endpoint) were 58% with twice-daily LEXIVA/ritonavir and 61% with lopinavir/ritonavir (95% CI for the difference: -16.6, 10.1). The proportions of patients with HIV-1 RNA <50 copies/mL with twice-daily LEXIVA/ritonavir and with lopinavir/ritonavir were 46% and 50%, respectively (95% CI for the difference: -18.3, 8.9). The proportions of patients who were virologic failures were 29% with twice-daily LEXIVA/ritonavir and 27% with lopinavir/ritonavir.
The frequency of discontinuations due to adverse events and other reasons, and deaths were similar between treatment arms.
Through 48 weeks of therapy, the median increases from baseline in CD4+ cell counts were 81 cells/mm3 with twice-daily LEXIVA/ritonavir and 91 cells/mm3 with lopinavir/ritonavir.
This study was not large enough to reach a definitive conclusion that LEXIVA/ritonavir and lopinavir/ritonavir are clinically equivalent.
Once-daily administration of LEXIVA plus ritonavir is not recommended for protease inhibitor-experienced patients. Through Week 48, 50% and 37% of patients receiving LEXIVA 1,400 mg plus ritonavir 200 mg once daily had plasma HIV-1 RNA <400 copies/mL and <50 copies/mL, respectively.
Pediatric Patients
Two open-label studies in pediatric patients 2 to 18 years of age were conducted. In one study, twice-daily dosing regimens (LEXIVA with or without ritonavir) were evaluated in combination with other antiretroviral agents. A second study evaluated once-daily dosing of LEXIVA with ritonavir; the data from this study were insufficient to support a once-daily dosing regimen in any pediatric patient population.
LEXIVA: Eighteen (16 therapy-naive and 2 therapy-experienced) pediatric patients received LEXIVA Oral Suspension without ritonavir twice daily. At Week 24, 67% (12/18) achieved HIV-1 RNA <400 copies/mL, and the median increase from baseline in CD4+ cell count was 353 cells/mm3.
LEXIVA plus ritonavir: Twenty-seven protease inhibitor-naive and 30 protease inhibitor-experienced pediatric patients received LEXIVA Oral Suspension or Tablets with ritonavir twice daily. At Week 24, 70% of protease inhibitor-naive (19/27) and 57% of protease inhibitor-experienced (17/30) patients achieved HIV-1 RNA <400 copies/mL; median increases from baseline in CD4+ cell counts were 131 cells/mm3 and 149 cells/mm3 in protease inhibitor-naive and experienced patients, respectively.
16 HOW SUPPLIED/STORAGE AND HANDLING
LEXIVA Tablets, 700 mg, are pink, film-coated, capsule-shaped, biconvex tablets, with “GX LL7” debossed on one face.
Store at controlled room temperature of 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) (see USP Controlled Room Temperature). Keep container tightly closed.
LEXIVA Oral Suspension, a white to off-white grape-bubblegum-peppermint-flavored suspension, contains 50 mg of fosamprenavir as fosamprenavir calcium equivalent to approximately 43 mg of amprenavir in each 1 mL.
This product does not require reconstitution.
Store at 5° to 30°C (41° to 86°F). Shake vigorously before using. Do not freeze.
This product is supplied by State of Florida DOH Central Pharmacy as follows:
| NDC | Strength | Quantity/Form | Color | Source Prod. Code |
| 53808-0281-1 | 700 mg | 30 Tablets in a Blister Pack | PINK | 0173-0721 |
17 PATIENT COUNSELING INFORMATION
See FDA-approved Patient Labeling
Drug Interactions
A statement to patients and healthcare providers is included on the product's bottle label: ALERT: Find out about medicines that should NOT be taken with LEXIVA.
LEXIVA may interact with many drugs; therefore, patients should be advised to report to their healthcare provider the use of any other prescription or nonprescription medication or herbal products, particularly St. John's wort.
Patients receiving PDE5 inhibitors should be advised that they may be at an increased risk of PDE5 inhibitor-associated adverse events, including hypotension, visual changes, and priapism, and should promptly report any symptoms to their healthcare provider.
Patients receiving hormonal contraceptives should be instructed to use alternate contraceptive measures during therapy with LEXIVA because hormonal levels may be altered, and if used in combination with LEXIVA and ritonavir, liver enzyme elevations may occur.
Sulfa Allergy
Patients should inform their healthcare provider if they have a sulfa allergy. The potential for cross-sensitivity between drugs in the sulfonamide class and fosamprenavir is unknown.
Redistribution/Accumulation of Body Fat
Patients should be informed that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy, including LEXIVA, and that the cause and long-term health effects of these conditions are not known at this time.
Information About Therapy With LEXIVA
Patients should be informed that LEXIVA is not a cure for HIV infection and that they may continue to develop opportunistic infections and other complications associated with HIV disease. The long-term effects of LEXIVA are unknown at this time. Patients should be told that there are currently no data demonstrating that therapy with LEXIVA can reduce the risk of transmitting HIV to others.
Patients should be told that sustained decreases in plasma HIV-1 RNA have been associated with a reduced risk of progression to AIDS and death. Patients should remain under the care of a physician while using LEXIVA. Patients should be advised to take LEXIVA every day as prescribed. LEXIVA must always be used in combination with other antiretroviral drugs. Patients should not alter the dose or discontinue therapy without consulting their physician. If a dose is missed, patients should take the dose as soon as possible and then return to their normal schedule. However, if a dose is skipped, the patient should not double the next dose.
Oral Suspension
Patients should be instructed to shake the bottle vigorously before each use and that refrigeration of the oral suspension may improve the taste for some patients.
LEXIVA and AGENERASE are registered trademarks of GlaxoSmithKline.
GlaxoSmithKline Vertex Pharmaceuticals Incorporated
Research Triangle Park, NC 27709 Cambridge, MA 02139
©2009, GlaxoSmithKline. All rights reserved.
PHARMACIST-DETACH HERE AND GIVE INSTRUCTIONS TO PATIENT
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ __ _ _ _ _ _ _ _ _
PATIENT INFORMATION
LEXIVA®
(lex-EE-vah)
(fosamprenavir calcium)
Tablets and Oral Suspension
Read the Patient Information that comes with LEXIVA before you start taking it and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment. It is important to remain under a healthcare provider's care while taking LEXIVA. Do not change or stop treatment without first talking with your healthcare provider. Talk to your healthcare provider or pharmacist if you have any questions about LEXIVA.
What is the most important information I should know about LEXIVA?
LEXIVA can cause dangerous and life-threatening interactions if taken with certain other medicines. Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements.
- Some medicines cannot be taken at all with LEXIVA.
- Some medicines will require dose changes if taken with LEXIVA.
- Some medicines will require close monitoring if you take them with LEXIVA.
Know all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Keep a list of the medicines you take. Show this list to all your healthcare providers and pharmacists anytime you get a new medicine or refill. Your healthcare providers and pharmacists must know all the medicines you take. They will tell you if you can take other medicines with LEXIVA. Do not start any new medicines while you are taking LEXIVA without talking with your healthcare provider or pharmacist. You can ask your healthcare provider or pharmacist for a list of medicines that can interact with LEXIVA.
What is LEXIVA?
LEXIVA is a medicine you take by mouth to treat HIV infection. HIV is the virus that causes AIDS (acquired immune deficiency syndrome). LEXIVA belongs to a class of anti-HIV medicines called protease inhibitors. LEXIVA is always used with other anti-HIV medicines. When used in combination therapy, LEXIVA may help lower the amount of HIV found in your blood, raise CD4+ (T) cell counts, and keep your immune system as healthy as possible, so it can help fight infection. However, LEXIVA does not work in all patients with HIV.
LEXIVA does not:
- cure HIV infection or AIDS. We do not know if LEXIVA will help you live longer or have fewer of the medical problems (opportunistic infections) that people get with HIV or AIDS. Opportunistic infections are infections that develop because the immune system is weak. Some of these conditions are pneumonia, herpes virus infections, and Mycobacterium avium complex (MAC) infections. It is very important that you see your healthcare provider regularly while you are taking LEXIVA. The long-term effects of LEXIVA are not known.
- lower the risk of passing HIV to other people through sexual contact, sharing needles, or being exposed to your blood. For your health and the health of others, it is important to always practice safer sex by using a latex or polyurethane condom to lower the chance of sexual contact with semen, vaginal secretions, or blood. Never use or share dirty needles.
LEXIVA has not been fully studied in children under the age of 2 or in adults over the age of 65.
Who should not take LEXIVA?
Do not take LEXIVA if you:
- are taking certain other medicines. Read the section“What is the most important information I should know about LEXIVA?” Do not take the following medicines* with LEXIVA. You could develop serious or life-threatening problems.
- HALCION® (triazolam; used for insomnia)
- Ergot medicines: dihydroergotamine, ergonovine, ergotamine, and methylergonovine such as CAFERGOT®, MIGRANAL®, D.H.E. 45®, ergotrate maleate, METHERGINE®, and others (used for migraine headaches)
- PROPULSID® (cisapride), used for certain stomach problems
- VERSED® (midazolam), used for sedation
- ORAP® (pimozide), used for Tourette’s disorder
- are allergic to LEXIVA or any of its ingredients. The active ingredient is fosamprenavir calcium. See the end of this leaflet for a list of all the ingredients in LEXIVA.
- are allergic to AGENERASE (amprenavir).
You should not take AGENERASE (amprenavir) and LEXIVA at the same time.
There are other medicines you should not take if you are taking LEXIVA and NORVIR® (ritonavir) together. You could develop serious or life-threatening problems. Tell your healthcare provider about all medicines you are taking before you begin taking LEXIVA and NORVIR (ritonavir) together.
What should I tell my healthcare provider before taking LEXIVA?
Before taking LEXIVA, tell your healthcare provider about all of your medical conditions including if you:
- are pregnant or planning to become pregnant. It is not known if LEXIVA can harm your unborn baby. You and your healthcare provider will need to decide if LEXIVA is right for you. If you use LEXIVA while you are pregnant, talk to your healthcare provider about how you can be on the Antiretroviral Pregnancy Registry.
- are breastfeeding. You should not breastfeed if you are HIV-positive because of the chance of passing the HIV virus to your baby through your milk. Also, it is not known if LEXIVA can pass into your breast milk and if it can harm your baby. If you are a woman who has or will have a baby, talk with your healthcare provider about the best way to feed your baby.
- have liver problems. You may be given a lower dose of LEXIVA or LEXIVA may not be right for you.
- have kidney problems
- have diabetes. You may need dose changes in your insulin or other diabetes medicines.
- have hemophilia
- are allergic to sulfa medicines
Before taking LEXIVA, tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. LEXIVA can cause dangerous and life-threatening interactions if taken with certain other medicines. You may need dose changes in some of your medicines or closer monitoring with some medicines if you also take LEXIVA (see “What is the most important information I should know about LEXIVA.”). Know all the medicines that you take and keep a list of them with you to show healthcare providers and pharmacists.
Women who use birth control pills should choose a different kind of contraception. The use of LEXIVA with NORVIR (ritonavir) in combination with birth control pills may be harmful to your liver. The use of LEXIVA with or without NORVIR may decrease the effectiveness of birth control pills. Talk to your healthcare provider about choosing an effective contraceptive.
How should I take LEXIVA?
- Take LEXIVA exactly as your healthcare provider prescribed.
- Do not take more or less than your prescribed dose of LEXIVA at any one time. Do not change your dose or stop taking LEXIVA without talking with your healthcare provider.
- You can take LEXIVA Tablets with or without food.
- Adults should take LEXIVA Oral Suspension without food.
- Pediatric patients should take LEXIVA Oral Suspension with food. If vomiting occurs within 30 minutes after dosing, the dose should be repeated.
- Shake LEXIVA Oral Suspension vigorously before each use.
- When your supply of LEXIVA or other anti-HIV medicine starts to run low, get more from your healthcare provider or pharmacy. The amount of HIV virus in your blood may increase if one or more of the medicines are stopped, even for a short time.
- Stay under the care of a healthcare provider while using LEXIVA.
- It is important that you do not miss any doses. If you miss a dose of LEXIVA by more than 4 hours, wait and take the next dose at the regular time. However, if you miss a dose by fewer than 4 hours, take your missed dose right away. Then take your next dose at the regular time.
- If you take too much LEXIVA, call your healthcare provider or poison control center right away.
What should I avoid while taking LEXIVA?
- Do not use certain medicines while you are taking LEXIVA. See “What is the most important information I should know about LEXIVA" and "Who should not take LEXIVA?”
- Do not breastfeed. See “Before taking LEXIVA, tell your healthcare provider”. Talk with your healthcare provider about the best way to feed your baby.
- Avoid doing things that can spread HIV infection since LEXIVA doesn't stop you from passing the HIV infection to others.
- Do not share needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes or razor blades.
- Do not have any kind of sex without protection. Always practice safer sex by using a latex or polyurethane condom to lower the chance of sexual contact with semen, vaginal secretions, or blood.
What are the possible side effects of LEXIVA?
LEXIVA may cause the following side effects:
- skin rash. Skin rashes, some with itching, have happened in patients taking LEXIVA. Swelling of the face, lips, and tongue (angioedema) has also been reported. Tell your healthcare provider if you get a rash or develop facial swelling after starting LEXIVA.
- diabetes and high blood sugar (hyperglycemia). Some patients had diabetes before taking LEXIVA while others did not. Some patients may need changes in their diabetes medicine. Others may need a new diabetes medicine.
- increased bleeding problems in some patients with hemophilia.
- worse liver disease. Patients with liver problems, including hepatitis B or C, are more likely to get worse liver disease when they take anti-HIV medicines like LEXIVA.
- changes in blood tests. Some people have changes in blood tests while taking LEXIVA. These include increases seen in liver function tests and blood fat levels, and decreases in white blood cells. Your healthcare provider may do regular blood tests to see if LEXIVA is affecting your body.
- changes in body fat. These changes have happened in patients taking antiretroviral medicines like LEXIVA. The changes may include an increased amount of fat in the upper back and neck ("buffalo hump"), breast, and around the trunk. Loss of fat from the legs, arms, and face may also happen. The cause and long-term health effects of these conditions are not known at this time.
- kidney stones have been reported in some patients taking LEXIVA. If you develop signs or symptoms of kidney stones (pain in your side, blood in your urine, pain when you urinate) tell your healthcare provider right away.
Common side effects of LEXIVA are nausea, vomiting, and diarrhea. Tell your healthcare provider about any side effects that bother you or that won't go away.
This list of side effects of LEXIVA is not complete. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store LEXIVA?
- LEXIVA Tablets should be stored at room temperature between 59° and 86°F (15° to 30°C). Keep the container of LEXIVA Tablets tightly closed.
- LEXIVA Oral Suspension may be stored at room temperature or refrigerated. Refrigeration of LEXIVA Oral Suspension may improve taste for some patients. Do not freeze.
- Keep LEXIVA and all medicines out of the reach of children.
- Do not keep medicine that is out of date or that you no longer need. Be sure that if you throw any medicine away, it is out of the reach of children.
General information about LEXIVA
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use LEXIVA for a condition for which it was not prescribed. Do not give LEXIVA to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about LEXIVA. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about LEXIVA that is written for health professionals. For more information you can call toll-free 888-825-5249 or visit www.LEXIVA.com.
What are the ingredients in LEXIVA?
Tablets:
Active Ingredient: fosamprenavir calcium.
Inactive Ingredients: colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, microcrystalline cellulose, and povidone K30. The tablet film-coating contains the inactive ingredients hypromellose, iron oxide red, titanium dioxide, and triacetin.
LEXIVA Tablets, 700 mg, are pink in color and are capsule-shaped, with the letters “GX LL7” printed on one side of the tablet.

Oral Suspension:
Active Ingredient: fosamprenavir calcium
Inactive ingredients: artificial grape-bubblegum flavor, calcium chloride dihydrate, hypromellose, methylparaben, natural peppermint flavor, polysorbate 80, propylene glycol, propylparaben, purified water, and sucralose.
LEXIVA and AGENERASE are registered trademarks of GlaxoSmithKline.
* The brands listed are trademarks of their respective owners and are not trademarks of GlaxoSmithKline. The makers of these brands are not affiliated with and do not endorse GlaxoSmithKline or its products.
GlaxoSmithKline Vertex Pharmaceuticals Incorporated
Research Triangle Park, NC 27709 Cambridge, MA 02139
©2009, GlaxoSmithKline. All rights reserved.
This Product was Repackaged By:
State of Florida DOH Central Pharmacy
104-2 Hamilton Park Drive
Tallahassee, FL 32304
United States
Principal Display Panel
NDC 53808-0281-1
30 Tablets
LEXIVA® (fosamprenavir calcium) TABLETS
700 mg
ALERT: Find out about medicines that should NOT be taken with LEXIVA.
Rx only
Note to Pharmacist: Do not cover ALERT box with pharmacy label.
For use in combination regimens with or without ritonavir.
Each tablet contains 700 mg of fosamprenavir as fosamprenavir calcium.
Store at controlled room temperature of 25˚C (77˚F); excursions permitted to 15˚ to 30˚C (59˚ to 86˚F) (see USP Controlled Room Temperature).
See package insert for Dosage and Administration.
LEXIVA is a trademark of GlaxoSmithKline.
Licensed from
VERTEX
Vertex Pharmaceuticals Incorporated
Cambridge, MA 02139
GlaxoSmithKline GlaxoSmithKline
Research Triangle Park, NC 27709
Made in England
_009575f9.jpg)
LEXIVAfosamprenavir calcium TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||