Lincocin
Lincocin lincomycin injection, USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING
- LINCOCIN DESCRIPTION
- CLINICAL PHARMACOLOGY
- LINCOCIN INDICATIONS AND USAGE
- LINCOCIN CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- LINCOCIN ADVERSE REACTIONS
- OVERDOSAGE
- LINCOCIN DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- ANIMAL PHARMACOLOGY
- CLINICAL STUDIES
- PHYSICAL COMPATIBILITIES
- PRINCIPAL DISPLAY PANEL - 1-2 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 1-2 mL Vial Carton
FULL PRESCRIBING INFORMATION
To reduce the development of drug-resistant bacteria and maintain the effectiveness of LINCOCIN and other antibacterial drugs, LINCOCIN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
WARNING
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Lincomycin and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
Because lincomycin therapy has been associated with severe colitis which may end fatally, it should be reserved for serious infections where less toxic antimicrobial agents are inappropriate, as described in the INDICATIONS AND USAGE section. It should not be used in patients with nonbacterial infections such as most upper respiratory tract infections.
C.diffficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
LINCOCIN DESCRIPTION
LINCOCIN Sterile Solution contains lincomycin hydrochloride which is the monohydrated salt of lincomycin, a substance produced by the growth of a member of the lincolnensis group of Streptomyces lincolnensis (Fam. Streptomycetaceae). The chemical name for lincomycin hydrochloride is Methyl 6,8-dideoxy-6-(1-methyl-trans-4-propyl-L-2-pyrolidinecarboxamido)-1-thio-D-erythro-α-D-galacto-octopyranoside monohydrochloride monohydrate. The molecular formula of lincomycin hydrochloride is C18H34N2O6S.HCl.H2O and the molecular weight is 461.01.
The structural formula is represented below:
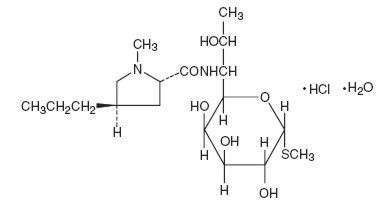
Lincomycin hydrochloride is a white or practically white, crystalline powder and is odorless or has a faint odor. Its solutions are acid and are dextrorotatory. Lincomycin hydrochloride is freely soluble in water; soluble in dimethylformamide and very slightly soluble in acetone.
CLINICAL PHARMACOLOGY
Intramuscular administration of a single dose of 600 mg of lincomycin produces average peak serum levels of 11.6 µg/mL at 60 minutes and maintains therapeutic levels for 17 to 20 hours for most susceptible gram-positive organisms. Urinary excretion after this dose ranges from 1.8 to 24.8 percent (mean: 17.3 percent).
A two hour intravenous infusion of 600 mg of lincomycin achieves average peak serum levels of 15.9 µg/mL and yields therapeutic levels for 14 hours for most susceptible gram-positive organisms. Urinary excretion ranges from 4.9 to 30.3 percent (mean: 13.8 percent).
The biological half-life after intramuscular or intravenous administration is 5.4 ± 1.0 hours. The serum half-life of lincomycin may be prolonged in patients with severe impairment of renal function compared to patients with normal renal function. In patients with abnormal hepatic function, serum half-life may be twofold longer than in patients with normal hepatic function. Hemodialysis and peritoneal dialysis are not effective in removing lincomycin from the serum.
Tissue level studies indicate that bile is an important route of excretion. Significant levels have been demonstrated in the majority of body tissues. Although lincomycin appears to diffuse into cerebrospinal fluid (CSF), levels of lincomycin in the CSF appear inadequate for the treatment of meningitis.
Microbiology
Lincomycin has been shown to be active against most strains of the following organisms both in vitro and in clinical infections: (see
INDICATIONS AND USAGE
).
Staphylococcus aureus (penicillinase- and non-penicillinase producing strains)
Streptococcus pneumoniae
The following in vitro data are available; but their clinical significance is unknown.
Lincomycin has been shown to be active in vitro against the following microorganisms; however, the safety and efficacy of LINCOCIN in treating clinical infections due to these organisms have not been established in adequate and well controlled trials.
Aerobic gram-positive cocci:
Streptococcus pyogenes
Viridans group streptococci
Aerobic gram-positive bacilli:
Corynebacterium diphtheriae
Anaerobic gram-positive non-sporeforming bacilli:
Propionibacterium acnes
Anaerobic gram-positive sporeforming bacilli:
Clostridium tetani
Clostridium perfringens
This drug is not active against most strains of Enterococcus faecalis nor against Neisseria gonorrhoeae, Neisseria meningitidis, Haemophilus influenzae or other gram-negative organisms or yeasts.
Cross resistance has been demonstrated between clindamycin and lincomycin. Some cross resistance with erythromycin including a phenomenon known as dissociated cross resistance or macrolide effect has been reported.
Studies indicate that lincomycin does not share antigenicity with penicillin compounds.
LINCOCIN INDICATIONS AND USAGE
LINCOCIN Sterile Solution is indicated in the treatment of serious infections due to susceptible strains of streptococci, pneumococci, and staphylococci. Its use should be reserved for penicillin-allergic patients or other patients for whom, in the judgment of the physician, a penicillin is inappropriate. Because of the risk of antibiotic-associated pseudomembranous colitis, as described in the WARNING box, before selecting lincomycin the physician should consider the nature of the infection and the suitability of less toxic alternatives (eg, erythromycin).
Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to lincomycin.
Indicated surgical procedures should be performed in conjunction with antibiotic therapy.
Lincomycin has been demonstrated to be effective in the treatment of staphylococcal infections resistant to other antibiotics and susceptible to lincomycin. Staphylococcal strains resistant to LINCOCIN have been recovered; culture and susceptibility studies should be done in conjunction with therapy with LINCOCIN. In the case of macrolides, partial but not complete cross resistance may occur (see Microbiology ). The drug may be administered concomitantly with other antimicrobial agents when indicated.
Lincomycin is not indicated in the treatment of minor bacterial infections or viral infections.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of LINCOCIN and other antibacterial drugs, LINCOCIN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
LINCOCIN CONTRAINDICATIONS
This drug is contraindicated in patients previously found to be hypersensitive to lincomycin or clindamycin.
WARNINGS
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Lincomycin, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Other causes of colitis should also be considered. A careful inquiry should be made concerning previous sensitivities to drugs and other allergens.
LINCOCIN Sterile Solution contains benzyl alcohol as a preservative.
The preservative benzyl alcohol has been associated with serious adverse events, including the "gasping syndrome", and death in pediatric patients. Although normal therapeutic doses of this product ordinarily deliver amounts of benzyl alcohol that are substantially lower than those reported in association with the "gasping syndrome", the minimum amount of benzyl alcohol at which toxicity may occur is not known. The risk of benzyl alcohol toxicity depends on the quantity administered and the hepatic capacity to detoxify the chemical. Premature and low-birth weight infants may be more likely to develop toxicity.
Usage in Meningitis — Although lincomycin appears to diffuse into cerebrospinal fluid, levels of lincomycin in the CSF may be inadequate for the treatment of meningitis.
SERIOUS ANAPHYLACTOID REACTIONS REQUIRE IMMEDIATE EMERGENCY TREATMENT WITH EPINEPHRINE. OXYGEN AND INTRAVENOUS CORTICOSTEROIDS SHOULD ALSO BE ADMINISTERED AS INDICATED. (See ADVERSE REACTIONS .)
PRECAUTIONS
General
Review of experience to date suggests that a subgroup of older patients with associated severe illness may tolerate diarrhea less well. When LINCOCIN is indicated in these patients, they should be carefully monitored for change in bowel frequency.
LINCOCIN should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
LINCOCIN should be used with caution in patients with a history of asthma or significant allergies.
Certain infections may require incision and drainage or other indicated surgical procedures in addition to antibiotic therapy.
The use of LINCOCIN may result in overgrowth of nonsusceptible organisms— particularly yeasts. Should superinfections occur, appropriate measures should be taken as indicated by the clinical situation. When patients with pre-existing monilial infections require therapy with LINCOCIN, concomitant antimonilial treatment should be given.
The serum half-life of lincomycin may be prolonged in patients with severe impairment of renal function compared to patients with normal renal function. In patients with abnormal hepatic function, serum half-life may be twofold longer than in patients with normal hepatic function.
Patients with severe impairment of renal function and/or abnormal hepatic function should be dosed with caution and serum lincomycin levels monitored during high-dose therapy. (See DOSAGE AND ADMINISTRATION Section.)
Lincomycin should not be injected intravenously undiluted as a bolus, but should be infused over at least 60 minutes as directed in the DOSAGE AND ADMINISTRATION Section.
Prescribing LINCOCIN in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs including LINCOCIN should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When LINCOCIN is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by LINCOCIN or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible
Laboratory Tests
During prolonged therapy with LINCOCIN, periodic liver and kidney function tests and blood counts should be performed.
Drug Interactions
Lincomycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used in caution in patients receiving such agents.
Antagonism between lincomycin and erythromycin in vitro has been demonstrated. Because of possible clinical significance, the two drugs should not be administered concurrently.
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of lincomycin has not been evaluated.
Lincomycin was not found to be mutagenic in the Ames Salmonella reversion assay or the V79 Chinese hamster lung cells at the HGPRT locus. It did not induce DNA strand breaks in V79 Chinese hamster lung cells as measured by alkaline elution or chromosomal abnormalities in cultured human lymphocytes. In vivo, lincomycin was negative in both the rat and mouse micronucleus assays and it did not induce sex-linked recessive lethal mutations in the offspring of male Drosophila. However, lincomycin did cause unscheduled DNA syntheses in freshly isolated rat hepatocytes.
Impairment of fertility was not observed in male or female rats given oral 300 mg/kg doses of lincomycin (0.36 times the highest recommended human dose based on mg/m2).
Pregnancy
Pregnancy Category C
LINCOCIN Sterile Solution contains benzyl alcohol as a preservative. Benzyl alcohol can cross the placenta. See WARNINGS .
Teratogenic Effects
There are no studies on the teratogenic potential of lincomycin in animals or adequate and well-controlled studies of pregnant women.
Nonteratogenic Effects
Reproduction studies have been performed in rats using oral doses of lincomycin up to 1000 mg/kg (1.2 times the maximum daily human dose based on mg/m2) and have revealed no adverse effects on survival of offspring from birth to weaning.
Nursing Mothers
Lincomycin has been reported to appear in human milk in concentrations of 0.5 to 2.4 mcg/mL. Because of the potential for serious adverse reactions in nursing infants from LINCOCIN, a decision should be made whether to discontinue nursing, or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
LINCOCIN Sterile Solution contains benzyl alcohol as a preservative. Benzyl alcohol has been associated with a fatal "Gasping Syndrome" in premature infants. See WARNINGS . Safety and effectiveness in pediatric patients below the age of one month have not been established. (See DOSAGE AND ADMINISTRATION Section.)
LINCOCIN ADVERSE REACTIONS
The following reactions have been reported with the use of lincomycin:
Gastrointestinal
Glossitis, stomatitis, nausea, vomiting, antibiotic-associated diarrhea and colitis, and pruritus ani. Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS ).
Hematopoietic
Neutropenia, leukopenia, agranulocytosis and thrombocytopenic purpura have been reported. There have been rare reports of aplastic anemia and pancytopenia in which LINCOCIN could not be ruled out as the causative agent.
Hypersensitivity Reactions
Hypersensitivity reactions such as angioneurotic edema, serum sickness and anaphylaxis have been reported. Rare instances of erythema multiforme, some resembling Stevens-Johnson syndrome, have been associated with LINCOCIN. If an allergic reaction to LINCOCIN occurs, discontinue the drug. Serious acute hypersensitivity reactions may require treatment with epinephrine and other emergency measures, including oxygen, intravenous fluids, intravenous antihistamines, corticosteroids, pressor amines, and airway management, as clinically indicated.
Skin and Mucous Membranes
Skin rashes, urticaria and vaginitis and rare instances of exfoliative and vesiculobullous dermatitis have been reported.
Liver
Although no direct relationship of LINCOCIN to liver dysfunction has been established, jaundice and abnormal liver function tests (particularly elevations of serum transaminase) have been observed.
Renal
Although no direct relationship of lincomycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed in rare instances.
Cardiovascular
After too rapid intravenous administration, rare instances of cardiopulmonary arrest and hypotension have been reported. (See DOSAGE AND ADMINISTRATION .)
Special Senses
Tinnitus and vertigo have been reported occasionally.
Local Reactions
Patients have demonstrated excellent local tolerance to intramuscularly administered LINCOCIN. Reports of pain following injection have been infrequent. Intravenous administration of LINCOCIN in 250 to 500 mL of 5% dextrose injection or 0.9% sodium chloride injection produced no local irritation or phlebitis.
OVERDOSAGE
Serum levels of lincomycin are not appreciably affected by hemodialysis and peritoneal dialysis.
LINCOCIN DOSAGE AND ADMINISTRATION
If significant diarrhea occurs during therapy, this antibiotic should be discontinued. (See WARNING box.)
INTRAMUSCULAR
Adults
Serious infections—600 mg (2 mL) intramuscularly every 24 hours. More severe infections—600 mg (2 mL) intramuscularly every 12 hours or more often.
Pediatric patients over 1 month of age
Serious infections—one intramuscular injection of 10 mg/kg (5 mg/lb) every 24 hours. More severe infections—one intramuscular injection of 10 mg/kg (5 mg/lb) every 12 hours or more often.
INTRAVENOUS
Adults
The intravenous dose will be determined by the severity of the infection. For serious infections doses of 600 mg of lincomycin (2 mL of LINCOCIN) to 1 gram are given every 8 to 12 hours. For more severe infections these doses may have to be increased. In life-threatening situations daily intravenous doses of as much as 8 grams have been given. Intravenous doses are given on the basis of 1 gram of lincomycin diluted in not less than 100 mL of appropriate solution (see PHYSICAL COMPATIBILITIES) and infused over a period of not less than one hour.
| Dose | Vol. Diluent | Time |
|---|---|---|
| 600 mg | 100 mL | 1 hr |
| 1 gram | 100 mL | 1 hr |
| 2 grams | 200 mL | 2 hr |
| 3 grams | 300 mL | 3 hr |
| 4 grams | 400 mL | 4 hr |
These doses may be repeated as often as required to the limit of the maximum recommended daily dose of 8 grams of lincomycin.
Pediatric patients over 1 month of age
10 to 20 mg/kg/day (5 to 10 mg/lb/day) depending on the severity of the infection may be infused in divided doses as described above for adults.
NOTE: Severe cardiopulmonary reactions have occurred when this drug has been given at greater than the recommended concentration and rate.
SUBCONJUNCTIVAL INJECTION
0.25 mL (75 mg) injected subconjunctivally will result in ocular fluid levels of antibiotic (lasting for at least 5 hours) with MICs sufficient for most susceptible pathogens.
Patients with diminished renal function
When therapy with LINCOCIN is required in individuals with severe impairment of renal function, an appropriate dose is 25 to 30% of that recommended for patients with normally functioning kidneys.
HOW SUPPLIED
LINCOCIN Sterile Solution is available in the following strength and package sizes:
300 mg
2 mL Vials — NDC 0009-0555-01
10 mL Vials — NDC 0009-0555-02
Each mL of LINCOCIN Sterile Solution contains lincomycin hydrochloride equivalent to lincomycin 300 mg; also benzyl alcohol, 9.45 mg added as preservative.
Store at controlled room temperature 20° to 25°C (68° to 77°F) [see USP].
ANIMAL PHARMACOLOGY
In vivo experimental animal studies demonstrated the effectiveness of LINCOCIN preparations (lincomycin) in protecting animals infected with Streptococcus viridans,β-hemolytic Streptococcus, Staphylococcus aureus, Diplococcus pneumoniae and Leptospira pomona. It was ineffective in Klebsiella, Pasteurella, Pseudomonas, Salmonella and Shigella infections.
CLINICAL STUDIES
Experience with 345 obstetrical patients receiving this drug revealed no ill effects related to pregnancy.
PHYSICAL COMPATIBILITIES
Physically compatible for 24 hours at room temperature unless otherwise indicated.
Infusion Solutions
5% Dextrose Injection
10% Dextrose Injection
5% Dextrose and 0.9% Sodium Chloride Injection
10% Dextrose and 0.9% Sodium Chloride Injection
Ringer's Injection
1/6 M Sodium Lactate Injection
Travert 10%-Electrolyte No. 1
Dextran in Saline 6% w/v
Vitamins in Infusion Solutions
B-Complex
B-Complex with Ascorbic Acid
Antibiotics in Infusion Solutions
Penicillin G Sodium (Satisfactory for 4 hours)
Cephalothin
Tetracycline HCl
Cephaloridine
Colistimethate (Satisfactory for 4 hours)
Ampicillin
Methicillin
Chloramphenicol
Polymyxin B Sulfate
Physically Incompatible with:
Novobiocin
Kanamycin
IT SHOULD BE EMPHASIZED THAT THE COMPATIBLE AND INCOMPATIBLE DETERMINATIONS ARE PHYSICAL OBSERVATIONS ONLY, NOT CHEMICAL DETERMINATIONS. ADEQUATE CLINICAL EVALUATION OF THE SAFETY AND EFFICACY OF THESE COMBINATIONS HAS NOT BEEN PERFORMED.
Rx only
LAB-0138-5.0
December 2013
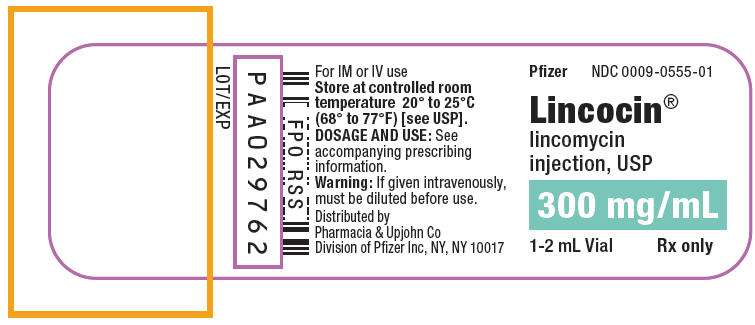
PRINCIPAL DISPLAY PANEL - 1-2 mL Vial Label
Pfizer
NDC 0009-0555-01
Lincocin
®
lincomycin
injection, USP
300 mg/mL
1-2 mL Vial
Rx only
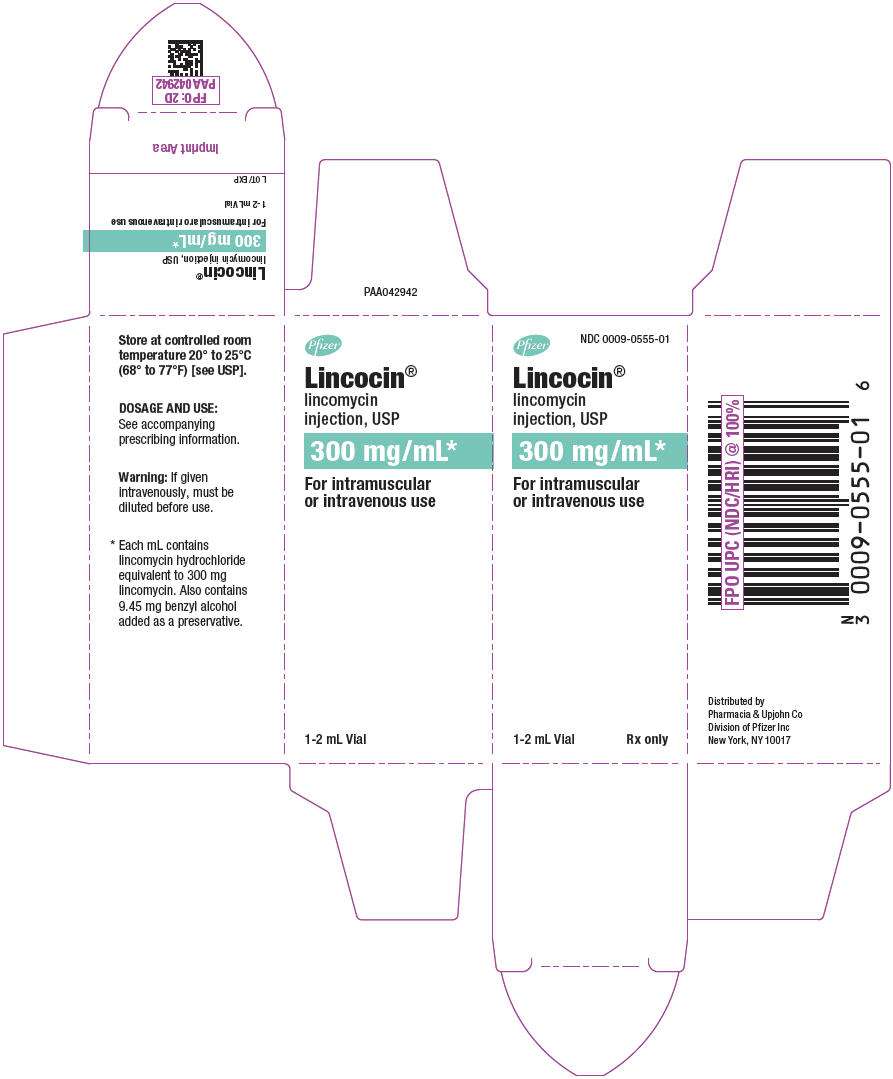
PRINCIPAL DISPLAY PANEL - 1-2 mL Vial Carton
Pfizer
NDC 0009-0555-01
Lincocin
®
lincomycin
injection, USP
300 mg/mL*
For intramuscular
or intravenous use
1-2 mL Vial
Rx only
Lincocinlincomycin hydrochloride INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||