Lisinopril and Hydrochlorothiazide
Lake Erie Medical DBA Quality Care Products LLC
Lisinopril and HCTZ 20 mg / 25 mg
FULL PRESCRIBING INFORMATION
Lisinopril and Hydrochlorothiazide Tablets combine an angiotensin-converting enzyme inhibitor, lisinopril, and a diuretic, hydrochlorothiazide.
Lisinopril, a synthetic peptide derivative, is an oral long-acting angiotensin-converting enzyme inhibitor. It is chemically described as 1-[N 2-[(S)-1-Carboxy-3-phenylpropyl]-L-lysyl]-L-proline dihydrate
As a result of its diuretic effects, hydrochlorothiazide increases plasma renin activity, increases aldosterone secretion, and decreases serum potassium. Administration of lisinopril blocks the renin-angiotensin aldosterone axis and tends to reverse the potassium loss associated with the diuretic.
In clinical studies, the extent of blood pressure reduction seen with the combination of lisinopril and hydrochlorothiazide was approximately additive. The Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg combination worked equally well in black and white patients. The Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg and Lisinopril and Hydrochlorothiazide Tablets 20-25 mg combinations appeared somewhat less effective in black patients, but relatively few black patients were studied. In most patients, the antihypertensive effect of Lisinopril and Hydrochlorothiazide Tablets was sustained for at least 24 hours.
In a randomized, controlled comparison, the mean antihypertensive effects of Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg and Lisinopril and Hydrochlorothiazide Tablets 20-25 mg were similar, suggesting that many patients who respond adequately to the latter combination may be controlled with Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg. (See DOSAGE AND ADMINISTRATION. )
Concomitant administration of lisinopril and hydrochlorothiazide has little or no effect on the bioavailability of either drug. The combination tablet is bioequivalent to concomitant administration of the separate entities.
Lisinopril inhibits angiotensin-converting enzyme (ACE) in human subjects and animals. ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex. Inhibition of ACE results in decreased plasma angiotensin II which leads to decreased vasopressor activity and to decreased aldosterone secretion. The latter decrease may result in a small increase of serum potassium. Removal of angiotensin II negative feedback on renin secretion leads to increased plasma renin activity. In hypertensive patients with normal renal function treated with lisinopril alone for up to 24 weeks, the mean increase in serum potassium was less than 0.1 mEq/L; however, approximately 15 percent of patients had increases greater than 0.5 mEq/L and approximately six percent had a decrease greater than 0.5 mEq/L. In the same study, patients treated with lisinopril plus a thiazide diuretic showed essentially no change in serum potassium (see PRECAUTIONS ).
ACE is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasodepressor peptide, play a role in the therapeutic effects of lisinopril remains to be elucidated.
While the mechanism through which lisinopril lowers blood pressure is believed to be primarily suppression of the renin-angiotensin-aldosterone system, lisinopril is antihypertensive even in patients with low-renin hypertension. Although lisinopril was antihypertensive in all races studied, black hypertensive patients (usually a low-renin hypertensive population) had a smaller average response to lisinopril monotherapy than non-black patients.
Following oral administration of lisinopril, peak serum concentrations occur within about 7 hours. Declining serum concentrations exhibit a prolonged terminal phase which does not contribute to drug accumulation. This terminal phase probably represents saturable binding to ACE and is not proportional to dose. Lisinopril does not appear to be bound to other serum proteins.
Lisinopril does not undergo metabolism and is excreted unchanged entirely in the urine. Based on urinary recovery, the mean extent of absorption of lisinopril is approximately 25%, with large intersubject variability (6% - 60 %) at all doses tested (5-80 mg). Lisinopril absorption is not influenced by the presence of food in the gastrointestinal tract.
Upon multiple dosing, lisinopril exhibits an effective half-life of accumulation of 12 hours.
Impaired renal function decreases elimination of lisinopril, which is excreted principally through the kidneys, but this decrease becomes clinically important only when the glomerular filtration rate is below 30 mL/min. Above this glomerular filtration rate, the elimination half-life is little changed. With greater impairment, however, peak and trough lisinopril levels increase, time to peak concentration increases and time to attain steady state is prolonged. Older patients, on average, have (approximately doubled) higher blood levels and area under the plasma concentration time curve (AUC) than younger patients. (See DOSAGE AND ADMINISTRATION .) In a multiple dose pharmacokinetic study in elderly versus young hypertensive patients using the lisinopril/hydrochlorothiazide combination, the AUC increased approximately 120% for lisinopril and approximately 80% for hydrochlorothiazide in older patients. Lisinopril can be removed by hemodialysis.
Studies in rats indicate that lisinopril crosses the blood-brain barrier poorly. Multiple doses of lisinopril in rats do not result in accumulation in any tissues; however, milk of lactating rats contains radioactivity following administration of 14C lisinopril. By whole body autoradiography, radioactivity was found in the placenta following administration of labeled drug to pregnant rats, but none was found in the fetuses.
Administration of lisinopril to patients with hypertension results in a reduction of supine and standing blood pressure to about the same extent with no compensatory tachycardia. Symptomatic postural hypotension is usually not observed although it can occur and should be anticipated in volume and/or salt-depleted patients. (See WARNINGS .)
In most patients studied, onset of antihypertensive activity was seen at one hour after oral administration of an individual dose of lisinopril, with peak reduction of blood pressure achieved by six hours.
In some patients achievement of optimal blood pressure reduction may require two to four weeks of therapy.
At recommended single daily doses, antihypertensive effects have been maintained for at least 24 hours, after dosing, although the effect at 24 hours was substantially smaller than the effect six hours after dosing.
The antihypertensive effects of lisinopril have continued during long-term therapy. Abrupt withdrawal of lisinopril has not been associated with a rapid increase in blood pressure; nor with a significant overshoot of pretreatment blood pressure.
In hemodynamic studies in patients with essential hypertension, blood pressure reduction was accompanied by a reduction in peripheral arterial resistance with little or no change in cardiac output and in heart rate. In a study in nine hypertensive patients, following administration of lisinopril, there was an increase in mean renal blood flow that was not significant. Data from several small studies are inconsistent with respect to the effect of lisinopril on glomerular filtration rate in hypertensive patients with normal renal function, but suggest that changes, if any, are not large.
In patients with renovascular hypertension lisinopril has been shown to be well tolerated and effective in controlling blood pressure(see PRECAUTIONS ).
The mechanism of the antihypertensive effect of thiazides is unknown. Thiazides do not usually affect normal blood pressure.
Hydrochlorothiazide is a diuretic and antihypertensive. It affects the distal renal tubular mechanism of electrolyte reabsorption. Hydrochlorothiazide increases excretion of sodium and chloride in approximately equivalent amounts. Natriuresis may be accompanied by some loss of potassium and bicarbonate.
After oral use diuresis begins within two hours, peaks in about four hours and lasts about 6 to 12 hours.
Hydrochlorothiazide is not metabolized but is eliminated rapidly by the kidney. When plasma levels have been followed for at least 24 hours, the plasma half-life has been observed to vary between 5.6 and 14.8 hours. At least 61 percent of the oral dose is eliminated unchanged within 24 hours. Hydrochlorothiazide crosses the placental but not the blood-brain barrier.
Uses
Lisinopril and Hydrochlorothiazide Tablets are indicated for the treatment of hypertension.
These fixed-dose combinations are not indicated for initial therapy (see DOSAGE AND ADMINISTRATION ).
In using Lisinopril and Hydrochlorothiazide Tablets, consideration should be given to the fact that an angiotensin-converting enzyme inhibitor, captopril, has caused agranulocytosis, particularly in patients with renal impairment or collagen vascular disease, and that available data are insufficient to show that lisinopril does not have a similar risk. (See WARNINGS .)
In considering the use of Lisinopril and Hydrochlorothiazide Tablets, it should be noted that ACE inhibitors have been associated with a higher rate of angioedema in black than in non-black patients.(See WARNINGS, Angioedema. )
Lisinopril and Hydrochlorothiazide Tablets are contraindicated in patients who are hypersensitive to this product and in patients with a history of angioedema related to previous treatment with an angiotensin-converting enzyme inhibitor and in patients with hereditary or idiopathic angioedema. Because of the hydrochlorothiazide component, this product is contraindicated in patients with anuria or hypersensitivity to other sulfonamide-derived drugs.
Presumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors (including Lisinopril and Hydrochlorothiazide Tablets) may be subject to a variety of adverse reactions, some of them serious.
Angioedema of the face, extremities, lips, tongue, glottis and/or larynx has been reported in patients treated with angiotensin-converting enzyme inhibitors, including lisinopril. This may occur at any time during treatment. ACE inhibitors have been associated with a higher rate of angioedema in black than in non-black patients. Lisinopril and Hydrochlorothiazide Tablets should be promptly discontinued and the appropriate therapy and monitoring should be provided until complete and sustained resolution of signs and symptoms has occurred. Even in those instances where swelling of only the tongue is involved, without respiratory distress, patients may require prolonged observation since treatment with antihistamines and corticosteroids may not be sufficient. Very rarely, fatalities have been reported due to angioedema associated with laryngeal edema or tongue edema. Patients with involvement of the tongue, glottis or larynx are likely to experience airway obstruction, especially those with history of airway surgery. Where there is involvement of the tongue, glottis or larynx, likely to cause airway obstruction, subcutaneous epinephrine solution 1:1000 (0.3 mL to 0.5 mL) and/or measures necessary to ensure a patent airway should be promptly provided. (See ADVERSE REACTIONS.)
Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor. Intestinal angioedema should be included in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
Patients with a history of angioedema unrelated to ACE inhibitor therapy may be at increased risk of angioedema while receiving an ACE inhibitor (see also INDICATIONS AND USAGE and CONTRAINDICATIONS ).
Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Thiazide-containing combination products are not recommended in patients with severe renal dysfunction. Sudden and potentially life-threatening anaphylactoid reactions have been reported in some patients dialyzed with high-flux membranes (e.g., AN69®*) and treated concomitantly with an ACE inhibitor. In such patients, dialysis must be stopped immediately, and aggressive therapy for anaphylactoid reactions must be initiated. Symptoms have not been relieved by antihistamines in these situations. In these patients, consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive agent. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
Excessive hypotension was rarely seen in uncomplicated hypertensive patients but is a possible consequence of lisinopril use in salt/volume-depleted persons such as those treated vigorously with diuretics or patients on dialysis. (See PRECAUTIONS, Drug Interactions and ADVERSE REACTIONS .)
Syncope has been reported in 0.8 percent of patients receiving Lisinopril and Hydrochlorothiazide Tablets. In patients with hypertension receiving lisinopril alone, the incidence of syncope was 0.1 percent. The overall incidence of syncope may be reduced by proper titration of the individual components. (See PRECAUTIONS, Drug Interactions , ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION .)
In patients with severe congestive heart failure, with or without associated renal insufficiency, excessive hypotension has been observed and may be associated with oliguria and/or progressive azotemia, and rarely with acute renal failure and/or death. Because of the potential fall in blood pressure in these patients, therapy should be started under very close medical supervision. Such patients should be followed closely for the first two weeks of treatment and whenever the dose of lisinopril and/or diuretic is increased. Similar considerations apply to patients with ischemic heart or cerebrovascular disease in whom an excessive fall in blood pressure could result in a myocardial infarction or cerebrovascular accident.
If hypotension occurs, the patient should be placed in supine position and, if necessary, receive an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further doses which usually can be given without difficulty once the blood pressure has increased after volume expansion.
Another angiotensin-converting enzyme inhibitor, captopril, has been shown to cause agranulocytosis and bone marrow depression, rarely in uncomplicated patients but more frequently in patients with renal impairment, especially if they also have a collagen vascular disease. Available data from clinical trials of lisinopril are insufficient to show that lisinopril does not cause agranulocytosis at similar rates. Marketing experience has revealed rare cases of leukopenia/neutropenia and bone marrow depression in which a causal relationship to lisinopril cannot be excluded. Periodic monitoring of white blood cell counts in patients with collagen vascular disease and renal disease should be considered.
Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice or hepatitis and progresses to fulminant hepatic necrosis and (sometimes) death. The mechanism of this syndrome is not understood. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up.
Teratogenicity studies were conducted in mice and rats with up to 90 mg/kg/day of lisinopril (56 times the maximum recommended human dose) in combination with 10 mg/kg/day of hydrochlorothiazide (2.5 times the maximum recommended human dose). Maternal or fetotoxic effects were not seen in mice with the combination. In rats decreased maternal weight gain and decreased fetal weight occurred down to 3/10 mg/kg/day (the lowest dose tested). Associated with the decreased fetal weight was a delay in fetal ossification. The decreased fetal weight and delay in fetal ossification were not seen in saline-supplemented animals given 90/10 mg/kg/day.
When used in pregnancy during the second and third trimesters, ACE inhibitors can cause injury and even death to the developing fetus. When pregnancy is detected, Lisinopril and Hydrochlorothiazide Tablets should be discontinued as soon as possible. (See Lisinopril, Fetal/Neonatal Morbidity and Mortality, below.)
ACE inhibitors can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature. When pregnancy is detected, ACE inhibitor therapy should be discontinued as soon as possible.
In a published retrospective epidemiological study, infants whose mothers had taken an ACE inhibitor drug during the first trimester of pregnancy appeared to have an increased risk of major congenital malformations compared with infants whose mothers had not undergone first trimester exposure to ACE inhibitor drugs. The number of cases of birth defects is small and the findings of this study have not yet been repeated.
These adverse effects do not appear to have resulted from intrauterine ACE-inhibitor exposure that has been limited to the first trimester. Mothers whose embryos and fetuses are exposed to ACE inhibitors only during the first trimester should be so informed. Nonetheless, when patients become pregnant, physicians should make every effort to discontinue the use of Lisinopril and Hydrochlorothiazide Tablets as soon as possible.
Rarely (probably less often than once in every thousand pregnancies), no alternative to ACE inhibitors will be found. In these rare cases, the mothers should be apprised of the potential hazards to their fetuses, and serial ultrasound examinations should be performed to assess the intraamniotic environment.
If oligohydramnios is observed, Lisinopril and Hydrochlorothiazide Tablets should be discontinued unless it is considered lifesaving for the mother. Contraction stress testing (CST), a non-stress test (NST), or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Infants with histories of in utero exposure to ACE inhibitors should be closely observed for hypotension, oliguria, and hyperkalemia. If oliguria occurs, attention should be directed toward support of blood pressure and renal perfusion. Exchange transfusion or dialysis may be required as means of reversing hypotension and/or substituting for disordered renal function. Lisinopril, which crosses the placenta, has been removed from neonatal circulation by peritoneal dialysis with some clinical benefit, and theoretically may be removed by exchange transfusion, although there is no experience with the latter procedure.
No teratogenic effects of lisinopril were seen in studies of pregnant rats, mice, rabbits. On a mg/kg basis, the doses used were up to 625 times (in mice), 188 times (in rats), and 0.6 times (in rabbits) the maximum recommended human dose.
Reproduction studies in the rabbit, the mouse and the rat at doses up to 100 mg/kg/day (50 times the human dose) showed no evidence of external abnormalities of the fetus due to hydrochlorothiazide. Hydrochlorothiazide given in a two-litter study in rats at doses of 4 - 5.6 mg/kg/day (approximately 1-2 times the usual daily human dose) did not impair fertility or produce birth abnormalities in the offspring. Thiazides cross the placental barrier and appear in cord blood.
These may include fetal or neonatal jaundice, thrombocytopenia, and possibly other adverse reactions have occurred in the adult.
Thiazides should be used with caution in severe renal disease. In patients with renal disease, thiazides may precipitate azotemia. Cumulative effects of the drug may develop in patients with impaired renal function.
Thiazides should be used with caution in patients with impaired hepatic function or progressive liver disease, since minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
Sensitivity reactions may occur in patients with or without a history of allergy or bronchial asthma.
The possibility of exacerbation or activation of systemic lupus erythematosus has been reported.
Lithium generally should not be given with thiazides (see PRECAUTIONS, Drug Interactions, Lisinopril and Hydrochlorothiazide ).
PRECAUTIONS
As with all vasodilators, lisinopril should be given with caution to patients with obstruction in the outflow tract of the left ventricle.
As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function may be anticipated in susceptible individuals. In patients with severe congestive heart failure whose renal function may depend on the activity of the renin-angiotensin-aldosterone system, treatment with angiotensin-converting enzyme inhibitors, including lisinopril, may be associated with oliguria and/or progressive azotemia and rarely with acute renal failure and/or death.
In hypertensive patients with unilateral or bilateral renal artery stenosis, increases in blood urea nitrogen and serum creatinine may occur. Experience with another angiotensin-converting enzyme inhibitor suggests that these increases are usually reversible upon discontinuation of lisinopril and/or diuretic therapy. In such patients renal function should be monitored during the first few weeks of therapy.
Some hypertensive patients with no apparent pre-existing renal vascular disease have developed increases in blood urea and serum creatinine, usually minor and transient, especially when lisinopril has been given concomitantly with a diuretic. This is more likely to occur in patients with pre-existing renal impairment. Dosage reduction of lisinopril and/or discontinuation of the diuretic may be required.
Evaluation of the hypertensive patient should always include assessment of renal function. (See DOSAGE AND ADMINISTRATION.)
In clinical trials hyperkalemia (serum potassium greater than 5.7 mEq/L) occurred in approximately 1.4 percent of hypertensive patients treated with lisinopril plus hydrochlorothiazide. In most cases these were isolated values which resolved despite continued therapy. Hyperkalemia was not a cause of discontinuation of therapy. Risk factors for the development of hyperkalemia include renal insufficiency, diabetes mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements and/or potassium-containing salt substitutes. Hyperkalemia can cause serious, sometimes fatal, arrhythmias. Lisinopril and Hydrochlorothiazide Tablets should be used cautiously, if at all, with these agents and with frequent monitoring of serum potassium (See Drug Interactions.)
Presumably due to the inhibition of the degradation of endogenous bradykinin, persistent nonproductive cough has been reported with all ACE inhibitors, almost always resolving after discontinuation of therapy. ACE inhibitor-induced cough should be considered in the differential diagnosis of cough.
In patients undergoing major surgery or during anesthesia with agents that produce hypotension, lisinopril may block angiotensin II formation secondary to compensatory renin release. If hypotension occurs and is considered to be due to this mechanism, it can be corrected by volume expansion.
Periodic determination of serum electrolytes to detect possible electrolyte imbalance should be performed at appropriate intervals.
All patients receiving thiazide therapy should be observed for clinical signs of fluid or electrolyte imbalance: namely, hyponatremia, hypochloremic alkalosis, and hypokalemia. Serum and urine electrolyte determinations are particularly important when the patient is vomiting excessively or receiving parenteral fluids. Warning signs or symptoms of fluid and electrolyte imbalance, irrespective of cause, include dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, confusion, seizures, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, and gastrointestinal disturbances such as nausea and vomiting.
Hypokalemia may develop, especially with brisk diuresis, when severe cirrhosis is present, or after prolonged therapy.
Interference with adequate oral electrolyte intake will also contribute to hypokalemia. Hypokalemia may cause cardiac arrhythmia and may also sensitize or exaggerate the response of the heart to the toxic effects of digitalis (e.g., increased ventricular irritability). Because lisinopril reduces the production of aldosterone, concomitant therapy with lisinopril attenuates the diuretic-induced potassium loss (see Drug Interactions, Agents Increasing Serum Potassium ).
Although any chloride deficit is generally mild and usually does not require specific treatment, except under extraordinary circumstances (as in liver disease or renal disease), chloride replacement may be required in the treatment of metabolic alkalosis.
Dilutional hyponatremia may occur in edematous patients in hot weather; appropriate therapy is water restriction, rather than administration of salt except in rare instances when the hyponatremia is life-threatening. In actual salt depletion, appropriate replacement is the therapy of choice.
Hyperuricemia may occur or frank gout may be precipitated in certain patients receiving thiazide therapy.
In diabetic patients dosage adjustments of insulin or oral hypoglycemic agents may be required. Hyperglycemia may occur with thiazide diuretics. Thus latent diabetes mellitus may become manifest during thiazide therapy.
The antihypertensive effects of the drug may be enhanced in the postsympathectomy patient.
If progressive renal impairment becomes evident consider withholding or discontinuing diuretic therapy.
Thiazides have been shown to increase the urinary excretion of magnesium; this may result in hypomagnesemia.
Thiazides may decrease urinary calcium excretion. Thiazides may cause intermittent and slight elevation of serum calcium in the absence of known disorders of calcium metabolism. Marked hypercalcemia may be evidence of hidden hyperparathyroidism. Thiazides should be discontinued before carrying out tests for parathyroid function.
Increases in cholesterol and triglyceride levels may be associated with thiazide diuretic therapy.
Angioedema, including laryngeal edema, may occur at any time during treatment with angiotensin-converting enzyme inhibitors, including Lisinopril and Hydrochlorothiazide Tablets. Patients should be so advised and told to report immediately any signs or symptoms suggesting angioedema (swelling of face, extremities, eyes, lips, tongue, difficulty in swallowing or breathing) and to take no more drug until they have consulted with the prescribing physician.
Patients should be cautioned to report lightheadedness especially during the first few days of therapy. If actual syncope occurs, the patients should be told to discontinue the drug until they have consulted with the prescribing physician.
All patients should be cautioned that excessive perspiration and dehydration may lead to an excessive fall in blood pressure because of reduction in fluid volume. Other causes of volume depletion such as vomiting or diarrhea may also lead to a fall in blood pressure; patients should be advised to consult with their physician.
Patients should be told not to use salt substitutes containing potassium without consulting their physician.
Patients should be told to report promptly any indication of infection (e.g., sore throat, fever) which may be a sign of leukopenia/neutropenia.
Female patients of childbearing age should be told about the consequences of exposure to ACE inhibitors during pregnancy. These patients should be asked to report pregnancies to their physicians as soon as possible.
NOTE: As with many other drugs, certain advice to patients being treated with Lisinopril and Hydrochlorothiazide Tablets is warranted. This information is intended to aid in the safe and effective use of this medication. It is not a disclosure of all possible adverse or intended effects.
ADVERSE REACTIONS
Lisinopril and Hydrochlorothiazide Tablets have been evaluated for safety in 930 patients including 100 patients treated for 50 weeks or more.
In clinical trials with Lisinopril and Hydrochlorothiazide Tablets no adverse experiences peculiar to this combination drug have been observed. Adverse experiences that have occurred have been limited to those that have been previously reported with lisinopril or hydrochlorothiazide.
WARNINGSAdverse experiences occurring in greater than one percent of patients treated with lisinopril plus hydrochlorothiazide in controlled clinical trials are shown below.
|
Lisinopril and Hydrochlorothiazide |
||
| (n=930) | Placebo | |
| Incidence | (n=207) | |
| (discontinuation) | Incidence | |
| Dizziness | 7.5 (0.8) | 1.9 |
| Headache | 5.2 (0.3) | 1.9 |
| Cough | 3.9 (0.6) | 1.0 |
| Fatigue | 3.7 (0.4) | 1.0 |
| Orthostatic Effects | 3.2 (0.1) | 1.0 |
| Diarrhea | 2.5 (0.2) | 2.4 |
| Nausea | 2.2 (0.1) | 2.4 |
| Upper Respiratory Infection | 2.2 (0.0) | 0.0 |
| Muscle Cramps | 2.0 (0.4) | 05 |
| Asthenia | 1.8 (0.2) | 1.0 |
| Paresthesia | 1.5 (0.1) | 0.0 |
| Hypotension | 1.4 (0.3) | 0.5 |
| Vomiting | 1.4 (01) | 0.5 |
| Dyspepsia | 1.3 (0.0) | 0.0 |
| Rash | 1.2 (0.1) | 0.5 |
| Impotence | 1.2 (0.3) | 0.0 |
Clinical adverse experiences occurring in 0.3 % to 1.0 % of patients in controlled trials and rarer, serious, possibly drug-related events reported in marketing experience are listed below:
Body as a Whole: Chest pain, abdominal pain, syncope, chest discomfort, fever, trauma, virus infection. Cardiovascular: Palpitation, orthostatic hypotension. Digestive: Gastrointestinal cramps, dry mouth, constipation, heartburn. Musculoskeletal: Back pain, shoulder pain, knee pain, back strain, myalgia, foot pain. Nervous/Psychiatric: Decreased libido,vertigo, depression, somnolence. Respiratory: Common cold, nasal congestion, influenza, bronchitis, pharyngeal pain,dyspnea, pulmonary congestion, chronic sinusitis, allergic rhinitis, pharyngeal discomfort. Skin: Flushing, pruritus, skininflammation, diaphoresis, cutaneous pseudolymphoma. Special Senses: Blurred vision, tinnitus, otalgia. Urogenital: Urinarytract infection.
Angioedema: Angioedema of the face, extremities, lips, tongue, glottis and/or larynx has been reported (See WARNINGS ).
In rare cases, intestinal angioedema has been reported in post marketing experience.
Hypotension: In clinical trials, adverse effects relating to hypotension occurred as follows: hypotension (1.4%), orthostatic hypotension (0.5%), other orthostatic effects (3.2%). In addition syncope occurred in 0.8% of patients (See WARNINGS ).
Cough: See PRECAUTIONS, Cough .
Clinical Laboratory Test FindingsSerum Electrolytes: See PRECAUTIONS .
Creatinine, Blood Urea Nitrogen: Minor reversible increases in blood urea nitrogen and serum creatinine were observed in patients with essential hypertension treated with Lisinopril and Hydrochlorothiazide Tablets. More marked increases have also been reported and were more likely to occur in patients with renal artery stenosis. (See PRECAUTIONS .)
Serum Uric Acid, Glucose, Magnesium, Cholesterol, Triglycerides and Calcium: See PRECAUTIONS .
Hemoglobin and Hematocrit: Small decreases in hemoglobin and hematocrit (mean decreases of approximately 0.5 g % and 1.5 vol %, respectively) occurred frequently in hypertensive patients treated with Lisinopril and Hydrochlorothiazide Tablets but were rarely of clinical importance unless another cause of anemia coexisted. In clinical trials, 0.4% of patients discontinued therapy due to anemia.
Liver Function Tests: Rarely, elevations of liver enzymes and/or serum bilirubin have occurred (See WARNINGS, Hepatic Failure ).
Other adverse reactions that have been reported with the individual components are listed below:
In clinical trials adverse reactions which occurred with lisinopril were also seen with Lisinopril and Hydrochlorothiazide Tablets. In addition, and since lisinopril has been marketed, the following adverse reactions have been reported with lisinopril and should be considered potential adverse reactions for Lisinopril and Hydrochlorothiazide Tablets: Body as a Whole: Anaphylactoid reactions (see WARNINGS , Anaphylactoid Reactions During Membrane Exposure ), malaise, edema, facial edema, pain, pelvic pain, flank pain, chills; Cardiovascular: Cardiac arrest, myocardial infarction or cerebrovascular accident, possibly secondary to excessive hypotension in high risk patients (see WARNINGS, Hypotension ), pulmonary embolism and infarction, worsening of heart failure, arrhythmias (including tachycardia, ventricular tachycardia, atrial tachycardia, atrial fibrillation, bradycardia, and premature ventricular contractions), angina pectoris, transient ischemic attacks, paroxysmal nocturnal dyspnea, decreased blood pressure, peripheral edema, vasculitis; Digestive: Pancreatitis, hepatitis (hepatocellular or cholestatic jaundice), (see WARNINGS, Hepatic Failure ), gastritis, anorexia, flatulence, increased salivation; Endocrine: Diabetes mellitus; inappropriate antidiuretic hormone secretion; Hematologic: Rare cases of bone marrow depression, hemolytic anemia, leukopenia/neutropenia, and thrombocytopenia have been reported in which a causal relationship to lisinoprol can not be excluded; Metabolic: Gout, weight loss, dehydration, fluid overload, weight gain; Musculoskeletal: Arthritis, arthralgia, neck pain, hip pain, joint pain, leg pain, arm pain, lumbago; Nervous System/Psychiatric: Ataxia, memory impairment, tremor, insomnia, stroke, nervousness, confusion, peripheral neuropathy(e.g., paresthesia, dysesthesia), spasm, hypersomnia, irritability; mood alterations (including depressive symptoms); Respiratory: Malignant lung neoplasms, hemoptysis, pulmonary edema, pulmonary infiltrates, bronchospasm, asthma,pleural effusion, pneumonia, eosinophilic pneumonitis, wheezing, orthopnea, painful respiration, epistaxis, laryngitis,sinusitis, pharyngitis, rhinitis, rhinorrhea, chest sound abnormalities; Skin: Urticaria, alopecia, herpes zoster,photosensitivity, skin lesions, skin infections, pemphigus, erythema, rare cases of other severe skin reactions, including toxic epidermal necrolysis and Stevens-Johnson Syndrome (causal relationship has not been established); Special Senses: Visual loss, diplopia, photophobia, taste alteration, olfactory disturbance; Urogenital: Acute renal failure, oliguria, anuria, uremia, progressive azotemia, renal dysfunction (see PRECAUTIONS and DOSAGE AND ADMINISTRATION ), pyelonephritis, dysuria, breast pain.
Miscellaneous: A symptom complex has been reported which may include a positive ANA, an elevated erythrocyte sedimentation rate, arthralgia/arthritis, myalgia, fever, vasculitis, eosinophilia and leukocytosis. Rash, photosensitivity or other dermatological manifestations may occur alone or in combination with these symptoms.
Fetal/Neonatal Morbidity and Mortality: See WARNINGS, Pregnancy, Lisinopril, Fetal/Neonatal Morbidity and Mortality.
Body as a Whole: Weakness; Digestive: Anorexia, gastric irritation, cramping, jaundice (intrahepatic cholestatic jaundice - See WARNINGS, Hepatic Failure), pancreatitis, sialoadenitis, constipation; Hematologic: Leukopenia, agranulocytosis, thrombocytopenia, aplastic anemia, hemolytic anemia; Musculoskeletal: Muscle spasm; Nervous System/Psychiatric: Restlessness; Renal: Renal failure, renal dysfunction, interstitial nephritis (see WARNINGS ); Skin: Erythema multiforme including Stevens-Johnson Syndrome, exfoliative dermatitis including toxic epidermal necrolysis, alopecia; Special Senses: Xanthopsia; Hypersensitivity: Purpura, photosensitivity, urticaria, necrotizing angiitis (vasculitis and cutaneous vasculitis), respiratory distress including pneumonitis and pulmonary edema, anaphylactic reactions.
To report SUSPECTED ADVERSE REACTIONS, contact West-ward Pharmaceutical Corp. at 1-877-233-2001, or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
No specific information is available on the treatment of overdosage with Lisinopril and Hydrochlorothiazide Tablets. Treatment is symptomatic and supportive. Therapy with Lisinopril and Hydrochlorothiazide Tablets should be discontinued and the patient observed closely. Suggested measures include induction of emesis and/or gastric lavage, and correction of dehydration, electrolyte imbalance and hypotension by established procedures.
Following a single oral dose of 20 g/kg, no lethality occurred in rats and death occurred in one of 20 mice receiving the same dose. The most likely manifestation of overdosage would be hypotension, for which the usual treatment would be intravenous infusion of normal saline solution.
Lisinopril can be removed by hemodialysis. (See WARNINGS,Anaphylactoid reactions during membrane exposure.)
Oral administration of a single oral dose of 10 g/kg to mice and rats was not lethal. The most common signs and symptoms observed are those caused by electrolyte depletion (hypokalemia, hypochloremia, hyponatremia) and dehydration resulting from excessive diuresis. If digitalis has also been administered, hypokalemia may accentuate cardiac arrhythmias.
DOSAGE AND ADMINISTRATION
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 - 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS ) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose- independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
A patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension. (See WARNINGS ). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour (see WARNINGS and PRECAUTIONS, Drug Interactions ).
Concomitant administration of Lisinopril and Hydrochlorothiazide Tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS ).
The combination may be substituted for the titrated individual components.
Regimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended(see WARNINGS, Anaphylactoid reactions during membrane exposure ).
Lisinopril and Hydrochlorothiazide Tablets, 10-12.5 mg are Blue with White Mottling, Round, Unscored Tablet, Debossed “WW 62” and are available in:
- Bottles of 30 tablets.
- Bottles of 100 tablets.
- Bottles of 500 tablets.
- Bottles of 1000 tablets.
Lisinopril and Hydrochlorothiazide Tablets, 20-12.5 mg are Yellow with White Mottling, Round, Unscored Tablet, Debossed 'WW 63' and are available in:
- Bottles of 30 tablets.
- Bottles of 100 tablets.
- Bottles of 500 tablets.
- Bottles of 1000 tablets.
Lisinopril and Hydrochlorothiazide Tablets, 20-25 mg are Peach-Red with White Mottling, Round, Unscored Tablet, Debossed 'WW 64' and are available in:
- Bottles of 30 tablets.
- Bottles of 100 tablets.
- Bottles of 500 tablets.
- Bottles of 1000 tablets.
Store at 20-25°C (68-77°F) [See USP Controlled Room Temperature]. Protect from excessive light and humidity.
Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Manufactured By:
West-ward Pharmaceutical
Corp.
Eatontown, NJ 07724
Revised April 2010
When used in pregnancy, during the second and third trimesters, ACE inhibitors can cause injury and even death to the developing fetus. When pregnancy is detected, Lisinopril and Hydrochlorothiazide Tablets should be discontinued as soon as possible. See WARNINGS, Pregnancy Lisinopril, Fetal/Neonatal Morbidity and Mortality.
Image of label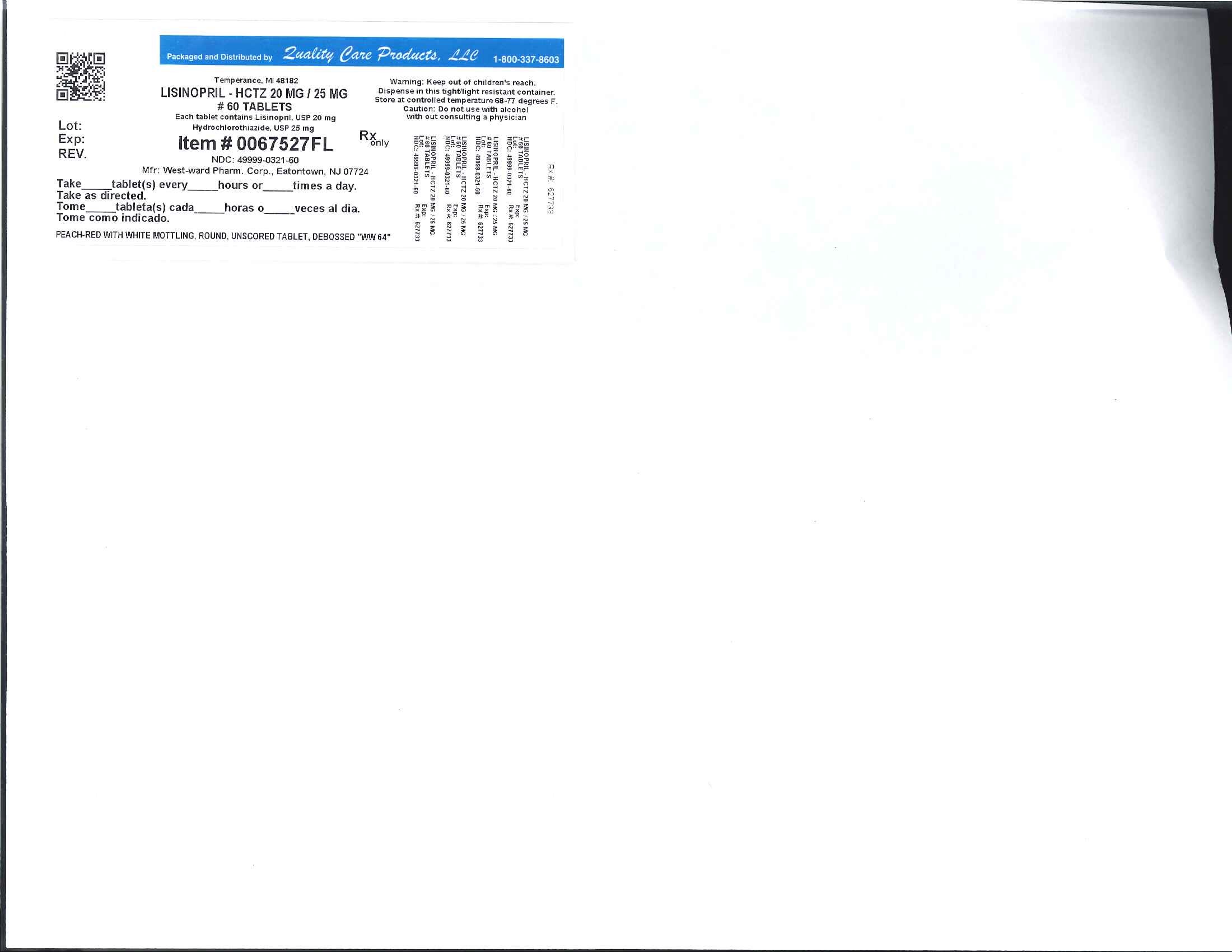
Lisinopril and HydrochlorothiazideLisinopril and Hydrochlorothiazide TABLET
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||