Loperamide Hydrochloride
Lake Erie Medical DBA Quality Care Products LLC
Loperamide Hydrochloride 2 mg
FULL PRESCRIBING INFORMATION
DESCRIPTION
293322
Loperamide hydrochloride is available in 2 mg capsules.
Each capsule, for oral administration, contains 2 mg loperamide hydrochloride. Loperamide hydrochloride capsules USP also contain the inactive ingredients: pregelatinized corn starch, gelatin capsules, iron oxides, lactose monohydrate, magnesium stearate, and titanium dioxide.
CLINICAL PHARMACOLOGY
In vitro and animal studies show that loperamide hydrochloride acts by slowing intestinal motility and by affecting water and electrolyte movement through the bowel. Loperamide binds to the opiate receptor in the gut wall. Consequently, it inhibits the release of acetylcholine and prostaglandins, thereby reducing peristalsis, and increasing intestinal transit time. Loperamide increases the tone of the anal sphincter, thereby reducing incontinence and urgency.
in vitroUses
Loperamide hydrochloride capsules are indicated for the control and symptomatic relief of acute nonspecific diarrhea and of chronic diarrhea associated with inflammatory bowel disease. Loperamide hydrochloride capsules are also indicated for reducing the volume of discharge from ileostomies.
Loperamide hydrochloride capsules are contraindicated in patients with known hypersensitivity to loperamide hydrochloride or to any of the excipients.
Loperamide hydrochloride is contraindicated in patients with abdominal pain in the absence of diarrhea.
Loperamide hydrochloride is not recommended in infants below 24 months of age.
Loperamide hydrochloride should not be used as the primary therapy:
- in patients with acute dysentery, which is characterized by blood in stools and high fever,
- in patients with acute ulcerative colitis,
- in patients with bacterial enterocolitis caused by invasive organisms including Salmonella, Shigella, and Campylobacter,
- in patients with pseudomembranous colitis associated with the use of broad-spectrum antibiotics.
Fluid and electrolyte depletion often occur in patients who have diarrhea. In such cases, administration of appropriate fluid and electrolytes is very important. The use of loperamide hydrochloride does not preclude the need for appropriate fluid and electrolyte therapy.
In general, loperamide hydrochloride should not be used when inhibition of peristalsis is to be avoided due to the possible risk of significant sequelae including ileus, megacolon and toxic megacolon. Loperamide hydrochloride must be discontinued promptly when constipation, abdominal distention or ileus develop.
Treatment of diarrhea with loperamide hydrochloride is only symptomatic. Whenever an underlying etiology can be determined, specific treatment should be given when appropriate (or when indicated).
Patients with AIDS treated with loperamide hydrochloride for diarrhea should have therapy stopped at the earliest signs of abdominal distention. There have been isolated reports of toxic megacolon in AIDS patients with infectious colitis from both viral and bacterial pathogens treated with loperamide hydrochloride. {ref EDMS-PSDB-2564186, p. 12}
Loperamide hydrochloride should be used with special caution in young children because of the greater variability of response in this age group. Dehydration, particularly in younger children, may further influence the variability of response to loperamide hydrochloride.
PRECAUTIONS
Nonclinical data have shown that loperamide is a P-glycoprotein substrate. Concomitant administration of loperamide (16 mg single dose) with a 600 mg single dose of either quinidine or ritonavir, both of which are P-glycoprotein inhibitors, resulted in a 2 to 3 fold increase in loperamide plasma levels. Due to the potential for enhanced central effects when loperamide is coadministered with quinidine and with ritonavir, caution should be exercised when loperamide is administered at the recommended dosages (2 mg, up to 16 mg maximum daily dose) with P-glycoprotein inhibitors.
When a single 16 mg dose of loperamide is coadministered with a 600 mg single dose of saquinavir, loperamide decreased saquinavir exposure by 54%, which may be of clinical relevance due to reduction of therapeutic efficacy of saquinavir. The effect of saquinavir on loperamide is of less clinical significance. Therefore, when loperamide is given with saquinavir, the therapeutic efficacy of saquinavir should be closely monitored.
In an 18 month rat study with oral doses up to 40 mg/kg/day (21 times the maximum human dose of 16 mg/day, based on a body surface area comparison), there was no evidence of carcinogenesis.
Loperamide was not genotoxic in the Ames test, the SOS chromotest in E. coli, the dominant lethal test in female mice, or the mouse embryo cell transformation assay.
Fertility and reproductive performance was evaluated in rats using oral doses of 2.5, 10, and 40 mg/kg/day in one study, and 1, 5, 10, 20, and 40 mg/kg/day (females only) in a second study. Oral administration of 20 mg/kg/day (approximately 11 times the human dose based on a body surface area comparison) and higher produced strong impairment of female fertility. Treatment of female rats with up to 10 mg/kg/day p.o. (approximately 5 times the human dose based on a body surface area comparison) had no effect on fertility. Treatment of male rats with 40 mg/kg/day p.o. (approximately 21 times the human dose based on a body surface area comparison) produced impairment of male fertility, whereas administration of up to 10 mg/kg/day (approximately 5 times the human dose based on a body surface area comparison) had no effect.
In a peri- and post-natal reproduction study in rats, oral administration of 40 mg/kg/day produced impairment of growth and survival of offspring.
Small amounts of loperamide may appear in human breast milk. Therefore, loperamide hydrochloride is not recommended during breast-feeding.
See the WARNINGS section for information on the greater variability of response in this age group.
In case of accidental overdosage of loperamide hydrochloride by pediatric patients, see OVERDOSAGE section for suggested treatment.
The adverse effects reported during clinical investigations of loperamide hydrochloride are difficult to distinguish from symptoms associated with the diarrheal syndrome. Adverse experiences recorded during clinical studies with loperamide hydrochloride were generally of a minor and self-limiting nature. They were more commonly observed during the treatment of chronic diarrhea.
The adverse events reported are summarized irrespective of the causality assessment of the investigators.
1) Adverse events from 4 placebo-controlled studies in patients with acute diarrhea
The adverse events with an incidence of 1.0% or greater, which were reported at least as often in patients on loperamide hydrochloride as on placebo, are presented in the table below.
|
|
Acute Diarrhea | |
|
|
Loperamide Hydrochloride | Placebo |
| No. of treated patients | 231 | 236 |
| Gastrointestinal AE% |
|
|
| Constipation | 2.6% | 0.8% |
The adverse events with an incidence of 1.0% or greater, which were more frequently reported in patients on placebo than on loperamide hydrochloride were: nausea, vomiting, headache, meteorism, abdominal pain, abdominal cramp and colic.
3) Adverse events from seventy-six controlled and uncontrolled studies in patients with acute or chronic diarrhea
The adverse events with an incidence of 1.0% or greater in patients from all studies are given in the table below.
|
|
Chronic Diarrhea | |
| Loperamide Hydrochloride | Placebo | |
| No. of treated patients | 285 | 277 |
| Gastrointestinal AE% | ||
| Constipation | 5.3% | 0% |
| Central and peripheral nervous system AE% |
|
|
| Dizziness | 1.4% | 0.7% |
The adverse events with an incidence of 1.0% or greater, which were more frequently reported in patients on placebo than on loperamide hydrochloride were: nausea, vomiting, headache, meteorism, abdominal pain, abdominal cramp and colic.
3) Adverse events from seventy-six controlled and uncontrolled studies in patients with acute or chronic diarrhea
The adverse events with an incidence of 1.0% or greater in patients from all studies are given in the table below.
|
|
Acute Diarrhea | Chronic Diarrhea | All Studies a |
| No. of treated patients | 1913 | 1371 | 3740 |
| Gastrointestinal AE% | |||
| Nausea | 0.7% | 3.2% | 1.8% |
| Constipation | 1.6% | 1.9% | 1.7% |
| Abdominal cramps | 0.5% | 3.0% | 1.4% |
a All patients in all studies, including those in which it was not specified if the adverse events occurred in patients with acute or chronic diarrhea.
Postmarketing Experience
The following adverse events have been reported:
Rash, pruritus, urticaria, angioedema, and extremely rare cases of bullous eruption including erythema multiforme, Stevens-Johnson syndrome and Toxic Epidermal Necrolysis have been reported with use of loperamide hydrochloride.
Isolated occurrences of allergic reactions and in some cases severe hypersensitivity reactions including anaphylactic shock and anaphylactoid reactions have been reported with the use of loperamide hydrochloride.
Dry mouth, abdominal pain, distention or discomfort, nausea, vomiting, flatulence, dyspepsia, constipation, paralytic ileus, megacolon, including toxic megacolon (see CONTRAINDICATIONS and WARNINGS).
Urinary retention.
Drowsiness, dizziness.
Tiredness.
A number of the adverse events reported during the clinical investigations and postmarketing experience with loperamide are frequent symptoms of the underlying diarrheal syndrome (abdominal pain/discomfort, nausea, vomiting, dry mouth, tiredness, drowsiness, dizziness, constipation, and flatulence). These symptoms are often difficult to distinguish from undesireable drug effects.
In cases of overdosage, (including relative overdose due to hepatic dysfunction), urinary retention, paralytic ileus and CNS depression may occur. Children may be more sensitive to CNS effects than adults. Clinical trials have demonstrated that a slurry of activated charcoal administered promptly after ingestion of loperamide hydrochloride can reduce the amount of drug which is absorbed into the systemic circulation by as much as ninefold. If vomiting occurs spontaneously upon ingestion, a slurry of 100 grams of activated charcoal should be administered orally as soon as fluids can be retained.
If vomiting has not occurred, gastric lavage should be performed followed by administration of 100 grams of the activated charcoal slurry through the gastric tube. In the event of overdosage, patients should be monitored for signs of CNS depression for at least 24 hours.
If symptoms of overdose occur, naloxone can be given as an antidote. If responsive to naloxone, vital signs must be monitored carefully for recurrence of symptoms of drug overdose for at least 24 hours after the last dose of naloxone.
In view of the prolonged action of loperamide and the short duration (one to three hours) of naloxone, the patient must be monitored closely and treated repeatedly with naloxone as indicated. Since relatively little drug is excreted in the urine, forced diuresis is not expected to be effective for loperamide hydrochloride overdosage.
In clinical trials an adult who took three 20 mg doses within a 24 hour period was nauseated after the second dose and vomited after the third dose. In studies designed to examine the potential for side effects, intentional ingestion of up to 60 mg of loperamide hydrochloride in a single dose to healthy subjects resulted in no significant adverse effects.
(1 capsule = 2 mg)
Patients should receive appropriate fluid and electrolyte replacement as needed.
The recommended initial dose is 4 mg (two capsules) followed by 2 mg (one capsule) after each unformed stool. Daily dosage should not exceed 16 mg (eight capsules). Clinical improvement is usually observed within 48 hours.
In children 2 to 5 years of age (20 kg or less), the non-prescription liquid formulation (loperamide hydrochloride for oral solution, 1 mg/5 mL) should be used; for ages 6 to 12, either loperamide hydrochloride capsules or loperamide hydrochloride for oral solution may be used. For children 2 to 12 years of age, the following schedule for capsules or liquid will usually fulfill initial dosage requirements:
Recommended First Day Dosage Schedule
Two to five years: 1 mg t.i.d. (3 mg daily dose) (13 to 20 kg)
Six to eight years: 2 mg b.i.d. (4 mg daily dose) (20 to 30 kg)
Eight to twelve years: 2 mg t.i.d. (6 mg daily dose) (greater than 30 kg)
Recommended Subsequent Daily Dosage
Following the first treatment day, it is recommended that subsequent loperamide hydrochloride doses (1 mg/10 kg body weight) be administered only after a loose stool. Total daily dosage should not exceed recommended dosages for the first day.
Although loperamide hydrochloride has been studied in a limited number of children with chronic diarrhea; the therapeutic dose for the treatment of chronic diarrhea in a pediatric population has not been established.
The recommended initial dose is 4 mg (two capsules) followed by 2 mg (one capsule) after each unformed stool until diarrhea is controlled, after which the dosage of loperamide hydrochloride capsules should be reduced to meet individual requirements. When the optimal daily dosage has been established, this amount may then be administered as a single dose or in divided doses.
The average daily maintenance dosage in clinical trials was 4 to 8 mg (two to four capsules). A dosage of 16 mg (eight capsules) was rarely exceeded. If clinical improvement is not observed after treatment with 16 mg per day for at least 10 days, symptoms are unlikely to be controlled by further administration. Loperamide hydrochloride capsules administration may be continued if diarrhea cannot be adequately controlled with diet or specific treatment.
The use of loperamide hydrochloride in children under 2 years is not recommended. There have been rare reports of paralytic ileus associated with abdominal distention. Most of these reports occurred in the setting of acute dysentery, overdose, and with very young children less than two years of age.
No formal pharmacokinetic studies were conducted in elderly subjects. However, there were no major differences in the drug disposition in elderly patients with diarrhea relative to young patients. No dosage adjustment is required for the elderly.
No pharmacokinetic data are available in patients with renal impairment. Since the metabolites and the unchanged drug are mainly excreted in the feces, no dosage adjustment is required for patients with renal impairment (see PRECAUTIONS).
Although no pharmacokinetic data are available in patients with hepatic impairment, loperamide hydrochloride should be used with caution in such patients because of reduced first pass metabolism (see PRECAUTIONS).
Loperamide hydrochloride capsules USP, 2 mg are available as:
A light brown opaque body and dark brown opaque capsule, imprinted "93"-"311" and packaged in bottles of 100 and 500.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a well-closed container, as defined in the USP, with a child-resistant closure (as required).
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
Manufactured By:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. J 12/2005
Patients should be advised to check with their physician if their diarrhea does not improve in 48 hours or if they note blood in their stools, develop a fever or develop abdominal distention.
Tiredness, dizziness, or drowsiness may occur in the setting of diarrheal syndromes treated with loperamide hydrochloride. Therefore, it is advisable to use caution when driving a car or operating machinery. (See ADVERSE REACTIONS).
Image of label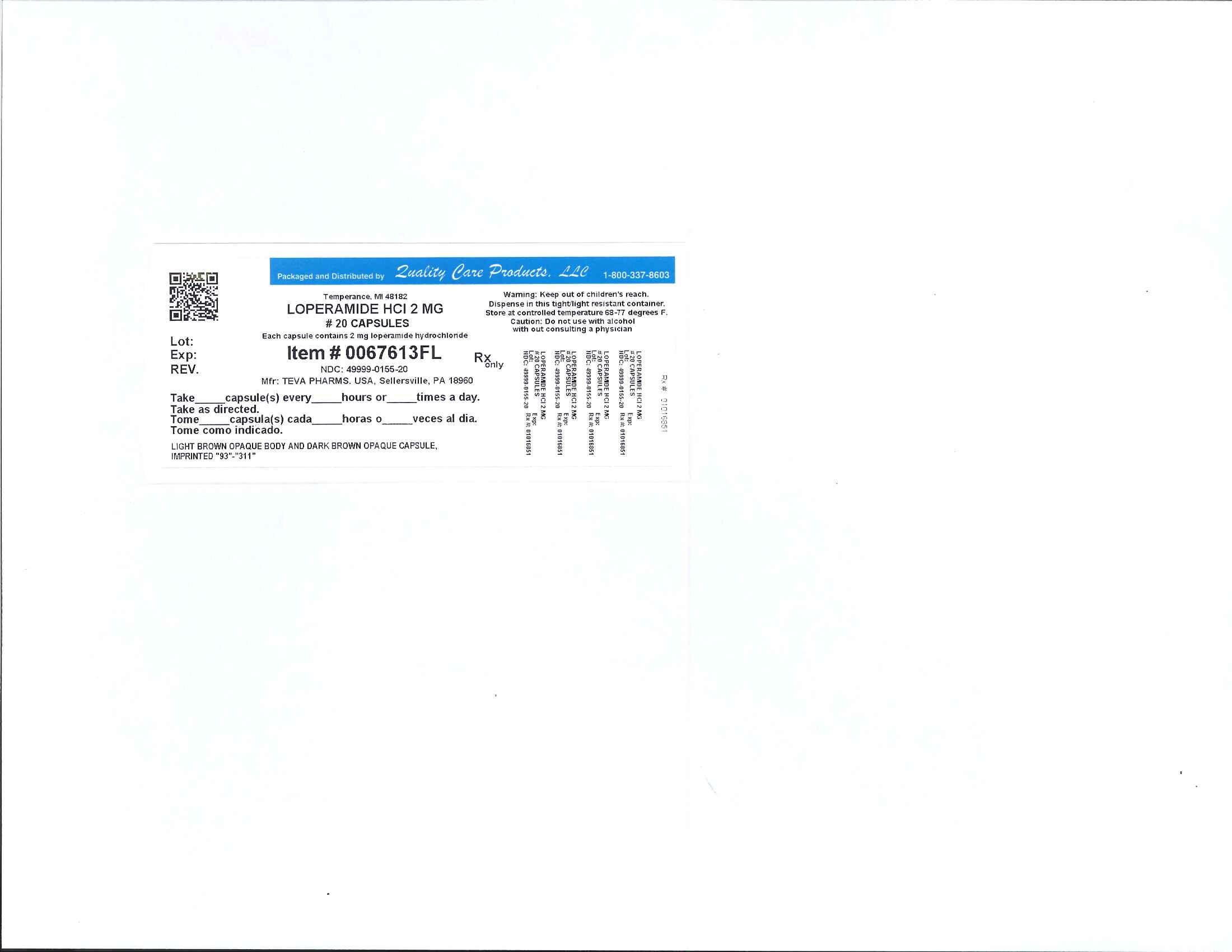
Loperamide HydrochlorideLoperamide Hydrochloride CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||