Methotrexate
Pfizer Laboratories Div Pfizer Inc.
Onco Therapies Limited
Methotrexate Injection, USP 40 mL
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNINGS
- METHOTREXATE DESCRIPTION
- CLINICAL PHARMACOLOGY
- METHOTREXATE INDICATIONS AND USAGE
- METHOTREXATE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- METHOTREXATE ADVERSE REACTIONS
- Alimentary System
- Blood and Lymphatic System Disorders
- Cardiovascular
- Central Nervous System:
- Hepatobiliary Disorders
- Infection
- Musculoskeletal System
- Ophthalmic
- Pulmonary System
- Skin
- Urogenital System
- Adverse Reactions in Double-Blind Rheumatoid Arthritis Studies
- Adverse Reactions in Psoriasis:
- Adverse Reactions in JRA Studies
- OVERDOSAGE
- METHOTREXATE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- REFERENCES
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
Rx ONLY
WARNINGS
METHOTREXATE SHOULD BE USED ONLY BY PHYSICIANS WHOSE KNOWLEDGE AND EXPERIENCE INCLUDE THE USE OF ANTIMETABOLITE THERAPY. BECAUSE OF THE POSSIBILITY OF SERIOUS TOXIC REACTIONS (WHICH CAN BE FATAL)
METHOTREXATE SHOULD BE USED ONLY IN LIFE THREATENING NEOPLASTIC DISEASES, OR IN PATIENTS WITH PSORIASIS OR RHEUMATOID ARTHRITIS WITH SEVERE, RECALCITRANT, DISABLING DISEASE WHICH IS NOT ADEQUATELY RESPONSIVE TO OTHER FORMS OF THERAPY. DEATHS HAVE BEEN REPORTED WITH THE USE OF METHOTREXATE IN THE TREATMENT OF MALIGNANCY, PSORIASIS, AND RHEUMATOID ARTHRITIS. PATIENTS SHOULD BE CLOSELY MONITORED FOR BONE MARROW, LIVER, LUNG AND KIDNEY TOXICITIES. (See PRECAUTIONS.) PATIENTS SHOULD BE INFORMED BY THEIR PHYSICIAN OF THE RISKS INVOLVED AND BE UNDER A PHYSICIAN’S CARE THROUGHOUT THERAPY. THE USE OF METHOTREXATE HIGH DOSE REGIMENS RECOMMENDED FOR OSTEOSARCOMA REQUIRES METICULOUS CARE. (See DOSAGE AND ADMINISTRATION.) HIGH DOSE REGIMENS FOR OTHER NEOPLASTIC DISEASES ARE INVESTIGATIONAL AND A THERAPEUTIC ADVANTAGE HAS NOT BEEN ESTABLISHED. METHOTREXATE FORMULATIONS AND DILUENTS CONTAINING PRESERVATIVES MUST NOT BE USED FOR INTRATHECAL OR HIGH DOSE METHOTREXATE THERAPY.
- Methotrexate has been reported to cause fetal death and/or congenital anomalies. Therefore, it is not recommended for women of childbearing potential unless there is clear medical evidence that the benefits can be expected to outweigh the considered risks. Pregnant women with psoriasis or rheumatoid arthritis should not receive methotrexate. (See CONTRAINDICATIONS).
- Methotrexate elimination is reduced in patients with impaired renal functions, ascites, or pleural effusions. Such patients require especially careful monitoring for toxicity, and require dose reduction or, in some cases, discontinuation of methotrexate administration.
- Unexpectedly severe (sometimes fatal) bone marrow suppression, aplastic anemia, and gastrointestinal toxicity have been reported with concomitant administration of methotrexate (usually in high dosage) along with some nonsteroidal anti-inflammatory drugs (NSAIDs). (See PRECAUTIONS, Drug Interactions).
- Methotrexate causes hepatotoxicity, fibrosis and cirrhosis, but generally only after prolonged use. Acutely, liver enzyme elevations are frequently seen. These are usually transient and asymptomatic, and also do not appear predictive of subsequent hepatic disease. Liver biopsy after sustained use often shows histologic changes, and fibrosis and cirrhosis have been reported; these latter lesions may not be preceded by symptoms or abnormal liver function tests in the psoriasis population. For this reason, periodic liver biopsies are usually recommended for psoriatic patients who are under long-term treatment. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in the rheumatoid arthritis population. (See PRECAUTIONS, Organ System Toxicity, Hepatic).
- Methotrexate-induced lung disease, including acute or chronic interstitial pneumonitis, is a potentially dangerous lesion, which may occur acutely at any time during therapy and has been reported at low doses. It is not always fully reversible and fatalities have been reported. Pulmonary symptoms (especially a dry, nonproductive cough) may require interruption of treatment and careful investigation.
- Diarrhea and ulcerative stomatitis require interruption of therapy: otherwise, hemorrhagic enteritis and death from intestinal perforation may occur.
- Malignant lymphomas, which may regress following withdrawal of methotrexate, may occur in patients receiving low-dose methotrexate and, thus, may not require cytotoxic treatment. Discontinue methotrexate first and, if the lymphoma does not regress, appropriate treatment should be instituted.
- Like other cytotoxic drugs, methotrexate may induce "tumor lysis syndrome" in patients with rapidly growing tumors. Appropriate supportive and pharmacologic measures may prevent or alleviate this complication.
- Severe, occasionally fatal, skin reactions have been reported following single or multiple doses of methotrexate. Reactions have occurred within days of oral, intramuscular, intravenous, or intrathecal methotrexate administration. Recovery has been reported with discontinuation of therapy. (See PRECAUTIONS, Organ System Toxicity, Skin.)
- Potentially fatal opportunistic infections, especially pneumonia, may occur with methotrexate therapy.
- Methotrexate given concomitantly with radiotherapy may increase the risk of soft tissue necrosis and osteonecrosis.
METHOTREXATE DESCRIPTION
Methotrexate (formerly Amethopterin) is an antimetabolite used in the treatment of certain neoplastic diseases, severe psoriasis, and adult rheumatoid arthritis.
Chemically methotrexate is N-[4-[[(2,4-diamino-6-pteridinyl)methyl]methylamino] benzoyl]-L-glutamic acid.
The structural formula is:
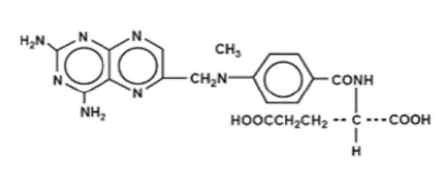
Molecular weight: 454.45 C20H22N8O5
Methotrexate Injection, USP is sterile and non-pyrogenic and may be given by the intramuscular, intravenous, intra-arterial or intrathecal route. Only the preservative free formulation of Methotrexate Injection, USP may be administered by the intrathecal route. (See DOSAGE AND ADMINISTRATION).
Methotrexate Injection, USP, Isotonic Liquid, Preservative Free, for single use only, is available in 2 mL (50 mg), 4 mL (100 mg), 8 mL (200 mg), 10 mL (250 mg) and 40 mL (1 g) vials.
Each 25 mg/mL, 2 mL, 4 mL, 8 mL, 10 mL and 40 mL vial contains methotrexate sodium equivalent to 50 mg, 100 mg, 200 mg, 250 mg and 1 g methotrexate respectively, and the following inactive ingredients: Sodium Chloride 0.490% w/v. Sodium Hydroxide and, if necessary, Hydrochloric Acid are added to adjust the pH to approximately 8.5. The 2 mL, 4 mL, 8 mL, 10 mL and 40 mL solutions contain approximately 0.43 mEq, 0.86 mEq, 1.72 mEq, 2.15 mEq and 8.6 mEq of sodium per vial, respectively, and are isotonic solutions.
CLINICAL PHARMACOLOGY
Methotrexate inhibits dihydrofolic acid reductase. Dihydrofolates must be reduced to tetrahydrofolates by this enzyme before they can be utilized as carriers of one-carbon groups in the synthesis of purine nucleotides and thymidylate. Therefore, methotrexate interferes with DNA synthesis, repair, and cellular replication. Actively proliferating tissues such as malignant cells, bone marrow, fetal cells, buccal and intestinal mucosa, and cells of the urinary bladder are in general more sensitive to this effect of methotrexate. When cellular proliferation in malignant tissues is greater than in most normal tissues, methotrexate may impair malignant growth without irreversible damage to normal tissues.
The mechanism of action in rheumatoid arthritis is unknown; it may affect immune function. Two reports describe in vitro methotrexate inhibition of DNA precursor uptake by stimulated mononuclear cells, and another describes in animal polyarthritis partial correction by methotrexate of spleen cell hyporesponsiveness and suppressed IL 2 production. Other laboratories, however, have been unable to demonstrate similar effects.
Clarification of methotrexate’s effect on immune activity and its relation to rheumatoid immunopathogenesis await further studies.
In patients with rheumatoid arthritis, effects of methotrexate on articular swelling and tenderness can be seen as early as 3 to 6 weeks. Although methotrexate clearly ameliorates symptoms of inflammation (pain, swelling, stiffness), there is no evidence that it induces remission of rheumatoid arthritis nor has a beneficial effect been demonstrated on bone erosions and other radiologic changes which result in impaired joint use, functional disability, and deformity.
Most studies of methotrexate in patients with rheumatoid arthritis are relatively short term (3 to 6 months). Limited data from long-term studies indicate that an initial clinical improvement is maintained for at least two years with continued therapy.
In psoriasis, the rate of production of epithelial cells in the skin is greatly increased over normal skin. This differential in proliferation rates is the basis for the use of methotrexate to control the psoriatic process.
Methotrexate in high doses, followed by leucovorin rescue, is used as a part of the treatment of patients with non-metastatic osteosarcoma. The original rationale for high dose methotrexate therapy was based on the concept of selective rescue of normal tissues by leucovorin. More recent evidence suggests that high dose methotrexate may also overcome methotrexate resistance caused by impaired active transport, decreased affinity of dihydrofolic acid reductase for methotrexate, increased levels of dihydrofolic acid reductase resulting from gene amplification, or decreased polyglutamation of methotrexate. The actual mechanism of action is unknown.
In a 6-month double-blind, placebo-controlled trial of 127 pediatric patients with juvenile rheumatoid arthritis (JRA) (mean age, 10.1 years; age range, 2.5 to 18 years; mean duration of disease, 5.1 years) on background nonsteroidal anti-inflammatory drugs (NSAIDs) and/or prednisone, methotrexate given weekly at an oral dose of 10 mg/m2 provided significant clinical improvement compared to placebo as measured by either the physician’s global assessment, or by a patient composite (25% reduction in the articular-severity score plus improvement in parent and physician global assessments of disease activity). Over two-thirds of the patients in this trial had polyarticular-course JRA, and the numerically greatest response was seen in this subgroup treated with 10 mg/m2/wk methotrexate. The overwhelming majority of the remaining patients had systemic-course JRA. All patients were unresponsive to NSAIDs; approximately one-third were using low dose corticosteroids. Weekly methotrexate at a dose of 5 mg/m2 was not significantly more effective than placebo in this trial.
Two Pediatric Oncology Group studies (one randomized and one non-randomized) demonstrated a significant improvement in relapse-free survival in patients with nonmetastatic osteosarcoma, when high dose methotrexate with leucovorin rescue was used in combination with other chemotherapeutic agents following surgical resection of the primary tumor. These studies were not designed to demonstrate the specific contribution of high dose methotrexate/leucovorin rescue therapy to the efficacy of the combination. However, a contribution can be inferred from the reports of objective responses to this therapy in patients with metastatic osteosarcoma, and from reports of extensive tumor necrosis following preoperative administration of this therapy to patients with non-metastatic osteosarcoma.
Pharmacokinetics
Absorption
In adults, oral absorption appears to be dose dependent. Peak serum levels are reached within one to two hours. At doses of 30 mg/m2 or less, methotrexate is generally well absorbed with a mean bioavailability of about 60%. The absorption of doses greater than 80 mg/m2 is significantly less, possibly due to a saturation effect.
In leukemic pediatric patients, oral absorption of methotrexate also appears to be dose dependent and has been reported to vary widely (23% to 95%). A twenty fold difference between highest and lowest peak levels Cmax: 0.11 to 2.3 micromolar after a 20 mg/m2 dose) has been reported. Significant interindividual variability has also been noted in time to peak concentration (Tmax: 0.67 to 4 hrs after a 15 mg/m2 dose) and fraction of dose absorbed. The absorption of doses greater than 40 mg/m2 has been reported to be significantly less than that of lower doses. Food has been shown to delay absorption and reduce peak concentration. Methotrexate is generally completely absorbed from parenteral routes of injection. After intramuscular injection, peak serum concentrations occur in 30 to 60 minutes. As in leukemic pediatric patients, a wide interindividual variability in the plasma concentrations of methotrexate has been reported in pediatric patients with JRA. Following oral administration of methotrexate in doses of 6.4 to 11.2 mg/m2/week in pediatric patients with JRA, mean serum concentrations were 0.59 micromolar (range, 0.03 to 1.40) at 1 hour, 0.44 micromolar (range, 0.01 to 1.00) at 2 hours, and 0.29 micromolar (range, 0.06 to 0.58) at 3 hours. In pediatric patients receiving methotrexate for acute lymphocytic leukemia (6.3 to 30 mg/m2), or for JRA (3.75 to 26.2 mg/m2), the terminal half-life has been reported to range from 0.7 to 5.8 hours or 0.9 to 2.3 hours, respectively.
Distribution
After intravenous administration, the initial volume of distribution is approximately 0.18 L/kg (18% of body weight) and steady-state volume of distribution is approximately 0.4 to 0.8 L/kg (40 to 80% of body weight). Methotrexate competes with reduced folates for active transport across cell membranes by means of a single carrier-mediated active transport process. At serum concentrations greater than 100 micromolar, passive diffusion becomes a major pathway by which effective intracellular concentrations can be achieved. Methotrexate in serum is approximately 50% protein bound. Laboratory studies demonstrate that it may be displaced from plasma albumin by various compounds including sulfonamides, salicylates, tetracyclines, chloramphenicol, and phenytoin.
Methotrexate does not penetrate the blood-cerebrospinal fluid barrier in therapeutic amounts when given orally or parenterally. High CSF concentrations of the drug may be attained by intrathecal administration.
In dogs, synovial fluid concentrations after oral dosing were higher in inflamed than uninflamed joints. Although salicylates did not interfere with this penetration, prior prednisone treatment reduced penetration into inflamed joints to the level of normal joints.
Metabolism
After absorption, methotrexate undergoes hepatic and intracellular metabolism to polyglutamated forms which can be converted back to methotrexate by hydrolase enzymes. These polyglutamates act as inhibitors of dihydrofolate reductase and thymidylate synthetase. Small amounts of methotrexate polyglutamates may remain in tissues for extended periods. The retention and prolonged drug action of these active metabolites vary among different cells, tissues and tumors. A small amount of metabolism to 7-hydroxymethotrexate may occur at doses commonly prescribed. Accumulation of this metabolite may become significant at the high doses used in osteogenic sarcoma. The aqueous solubility of 7-hydroxymethotrexate is 3 to 5 fold lower than the parent compound. Methotrexate is partially metabolized by intestinal flora after oral administration.
Half-Life
The terminal half-life reported for methotrexate is approximately three to ten hours for patients receiving treatment for psoriasis, or rheumatoid arthritis or low dose antineoplastic therapy (less than 30 mg/m2). For patients receiving high doses of methotrexate, the terminal half-life is eight to 15 hours.
Excretion
Renal excretion is the primary route of elimination and is dependent upon dosage and route of administration. With IV administration, 80% to 90% of the administered dose is excreted unchanged in the urine within 24 hours. There is limited biliary excretion amounting to 10% or less of the administered dose. Enterohepatic recirculation of methotrexate has been proposed.
Renal excretion occurs by glomerular filtration and active tubular secretion. Nonlinear elimination due to saturation of renal tubular reabsorption has been observed in psoriatic patients at doses between 7.5 and 30 mg. Impaired renal function, as well as concurrent use of drugs such as weak organic acids that also undergo tubular secretion, can markedly increase methotrexate serum levels. Excellent correlation has been reported between methotrexate clearance and endogenous creatinine clearance.
Methotrexate clearance rates vary widely and are generally at higher doses. Delayed drug clearance has been identified as one of the major factors responsible for methotrexate toxicity. It has been postulated that the toxicity of methotrexate for normal tissues is more dependent upon the duration of exposure to the drug rather than the peak level achieved. When a patient has delayed drug elimination due to compromised renal function, a third space effusion, or other causes, methotrexate serum concentrations may remain elevated for prolonged periods.
The potential for toxicity from high dose regimens or delayed excretion is reduced by the administration of leucovorin calcium during the final phase of methotrexate plasma elimination.
Pharmacokinetic monitoring of methotrexate serum concentrations may help identify those patients at high risk for methotrexate toxicity and aid in proper adjustments of leucovorin dosing.
Guidelines for monitoring serum methotrexate levels, and for adjustment of leucovorin dosing to reduce the risk of methotrexate toxicity, are provided below in DOSAGE AND ADMINISTRATION.
Methotrexate has been detected in human breast milk. The highest breast milk to plasma concentration ratio reached was 0.08:1.
METHOTREXATE INDICATIONS AND USAGE
Neoplastic Diseases
Methotrexate is indicated in the treatment of gestational choriocarcinoma, chorioadenoma destruens and hydatidiform mole.
In acute lymphocytic leukemia, methotrexate is indicated in the prophylaxis of meningeal leukemia and is used in maintenance therapy in combination with other chemotherapeutic agents. Methotrexate is also indicated in the treatment of meningeal leukemia.
Methotrexate is used alone or in combination with other anticancer agents in the treatment of breast cancer, epidermoid cancers of the head and neck, advanced mycosis fungoides (cutaneous T cell lymphoma), and lung cancer, particularly squamous cell and small cell types. Methotrexate is also used in combination with other chemotherapeutic agents in the treatment of advanced stage non-Hodgkin’s lymphomas.
Methotrexate in high doses followed by leucovorin rescue in combination with other chemotherapeutic agents is effective in prolonging relapse-free survival in patients with non-metastatic osteosarcoma who have undergone surgical resection or amputation for the primary tumor.
Psoriasis
Methotrexate is indicated in the symptomatic control of severe, recalcitrant, disabling psoriasis that is not adequately responsive to other forms of therapy, but only when the diagnosis has been established, as by biopsy and/or after dermatologic consultation. It is important to ensure that a psoriasis "flare" is not due to an undiagnosed concomitant disease affecting immune responses.
Rheumatoid Arthritis including Polyarticular-Course Juvenile Rheumatoid
Arthritis
Methotrexate is indicated in the management of selected adults with severe, active rheumatoid arthritis (ACR criteria), or children with active polyarticular-course juvenile rheumatoid arthritis, who have had an insufficient therapeutic response to, or are intolerant of, an adequate trial of first-line therapy including full dose non-steroidal anti-inflammatory agents (NSAIDs).
Aspirin, (NSAIDs), and/or low dose steroids may be continued, although the possibility of increased toxicity with concomitant use of NSAIDs including salicylates has not been fully explored. (See PRECAUTIONS, Drug Interactions.) Steroids may be reduced gradually in patients who respond to methotrexate. Combined use of methotrexate with gold, penicillamine, hydroxychloroquine, sulfasalazine, or cytotoxic agents, has not been studied and may increase the incidence of adverse effects. Rest and physiotherapy as indicated should be continued.
METHOTREXATE CONTRAINDICATIONS
Methotrexate can cause fetal death or teratogenic effects when administered to a pregnant woman. Methotrexate is contraindicated in pregnant women with psoriasis or rheumatoid arthritis and should be used in the treatment of neoplastic diseases only when the potential benefit outweighs the risk to the fetus. Women of childbearing potential should not be started on methotrexate until pregnancy is excluded and should be fully counseled on the serious risk to the fetus (see PRECAUTIONS) should they become pregnant while undergoing treatment. Pregnancy should be avoided if either partner is receiving methotrexate; during and for a minimum of three months after therapy for male patients, and during and for at least one ovulatory cycle after therapy for female patients. (See Boxed WARNINGS).
Because of the potential for serious adverse reactions from methotrexate in breast fed infants, it is contraindicated in nursing mothers.
Patients with psoriasis or rheumatoid arthritis with alcoholism, alcoholic liver disease or other chronic liver disease should not receive methotrexate.
Patients with psoriasis or rheumatoid arthritis who have overt or laboratory evidence of immunodeficiency syndromes should not receive methotrexate.
Patients with psoriasis or rheumatoid arthritis who have preexisting blood dyscrasias, such as bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anemia, should not receive methotrexate.
Patients with a known hypersensitivity to methotrexate should not receive the drug.
WARNINGS
(SEE BOXED WARNINGS)
Methotrexate formulations and diluents containing preservatives must not be used for intrathecal or high dose methotrexate therapy.
PRECAUTIONS
General
Methotrexate has the potential for serious toxicity (See Boxed WARNINGS). Toxic effects may be related in frequency and severity to dose or frequency of administration but have been seen at all doses. Because they can occur at any time during therapy, it is necessary to follow patients on methotrexate closely. Most adverse reactions are reversible if detected early. When such reactions do occur, the drug should be reduced in dosage or discontinued and appropriate corrective measures should be taken. If necessary, this could include the use of leucovorin calcium and/or acute, intermittent hemodialysis with a high-flux dialyzer. (See OVERDOSAGE). If methotrexate therapy is reinstituted, it should be carried out with caution, with adequate consideration of further need for the drug and increased alertness as to possible recurrence of toxicity.
The clinical pharmacology of methotrexate has not been well studied in older individuals. Due to diminished hepatic and renal function as well as decreased folate stores in this population, relatively low doses should be considered, and these patients should be closely monitored for early signs of toxicity.
Some of the effects mentioned under ADVERSE REACTIONS, such as dizziness and fatigue, may affect the ability to drive or operate machinery.
Information for Patients
Patients should be informed of the early signs and symptoms of toxicity, of the need to see their physician promptly if they occur, and the need for close follow-up, including periodic laboratory tests to monitor toxicity.
Both the physician and pharmacist should emphasize to the patient that the recommended dose is taken weekly in rheumatoid arthritis and psoriasis, and that mistaken daily use of the recommended dose has led to fatal toxicity. Prescriptions should not be written or refilled on a PRN basis.
Patients should be informed of the potential benefit and risk in the use of methotrexate. The risk of effects on reproduction should be discussed with both male and female patients taking methotrexate.
Laboratory Tests
Patients undergoing methotrexate therapy should be closely monitored so that toxic effects are detected promptly. Baseline assessment should include a complete blood count with differential and platelet counts, hepatic enzymes, renal function tests and a chest X-ray. During therapy of rheumatoid arthritis and psoriasis, monitoring of these parameters is recommended: hematology at least monthly, renal function and liver function every 1 to 2 months. More frequent monitoring is usually indicated during antineoplastic therapy.
During initial or changing doses, or during periods of increased risk of elevated methotrexate blood levels (e.g., dehydration), more frequent monitoring may also be indicated.
Transient liver function test abnormalities are observed frequently after methotrexate administration and are usually not cause for modification of methotrexate therapy. Persistent liver function test abnormalities, and/or depression of serum albumin may be indicators of serious liver toxicity and require evaluation. (See PRECAUTIONS, Organ System Toxicity, Hepatic).
A relationship between abnormal liver function tests and fibrosis or cirrhosis of the liver has not been established for patients with psoriasis. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in the rheumatoid arthritis population. Pulmonary function tests may be useful if methotrexate-induced lung disease is suspected, especially if baseline measurements are available.
Drug Interactions
Nonsteroidal anti-inflammatory drugs should not be administered prior to or concomitantly with the high doses of methotrexate, such as used in the treatment of osteosarcoma. Concomitant administration of some NSAIDs with high dose methotrexate therapy has been reported to elevate and prolong serum methotrexate levels, resulting in deaths from severe hematologic and gastrointestinal toxicity.
Caution should be used when NSAIDs and salicylates are administered concomitantly with lower doses of methotrexate. These drugs have been reported to reduce the tubular secretion of methotrexate in an animal model and may enhance its toxicity.
Despite the potential interactions, studies of methotrexate in patients with rheumatoid arthritis have usually included concurrent use of constant dosage regimens of NSAIDs, without apparent problems. It should be appreciated, however, that the doses used in rheumatoid arthritis (7.5 to 15 mg/week) are somewhat lower than those used in psoriasis and that larger doses could lead to unexpected toxicity.
Methotrexate is partially bound to serum albumin, and toxicity may be increased because of displacement by certain drugs, such as salicylates, phenylbutazone, phenytoin, and sulfonamides. Renal tubular transport is also diminished by probenecid; use of methotrexate with this drug should be carefully monitored.
In the treatment of patients with osteosarcoma, caution must be exercised if high-dose methotrexate is administered in combination with a potentially nephrotoxic chemotherapeutic agent (e.g., cisplatin).
Methotrexate increases the plasma levels of mercaptopurine. The combination of methotrexate and mercaptopurine may therefore require dose adjustment.
Oral antibiotics such as tetracycline, chloramphenicol, and nonabsorbable broad spectrum antibiotics, may decrease intestinal absorption of methotrexate or interfere with the enterohepatic circulation by inhibiting bowel flora and suppressing metabolism of the drug by bacteria.
Penicillins may reduce the renal clearance of methotrexate; increased serum concentrations of methotrexate with concomitant hematologic and gastrointestinal toxicity have been observed with high and low dose methotrexate. Use of methotrexate with penicillins should be carefully monitored.
The potential for increased hepatotoxicity when methotrexate is administered with other hepatotoxic agents has not been evaluated. However, hepatotoxicity has been reported in such cases. Therefore, patients receiving concomitant therapy with methotrexate and other potential hepatotoxins (e.g., azathioprine, retinoids, sulfasalazine) should be closely monitored for possible increased risk of hepatotoxicity.
Methotrexate may decrease the clearance of theophylline; theophylline levels should be monitored when used concurrently with methotrexate.
Vitamin preparations containing folic acid or its derivatives may decrease responses to systemically administered methotrexate. Preliminary animal and human studies have shown that small quantities of intravenously administered leucovorin enter the CSF primarily as 5-methyltetrahydrofolate and, in humans, remain 1 to 3 orders of magnitude lower than the usual methotrexate concentrations following intrathecal administration. However, high doses of leucovorin may reduce the efficacy of intrathecally administered
methotrexate.
Folate deficiency states may increase methotrexate toxicity. Trimethoprim/ sulfamethoxazole has been reported rarely to increase bone marrow suppression in patients receiving methotrexate, probably by decreased tubular secretion and/or an additive antifolate effect.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No controlled human data exist regarding the risk of neoplasia with methotrexate. Methotrexate has been evaluated in a number of animal studies for carcinogenic potential with inconclusive results. Although there is evidence that methotrexate causes chromosomal damage to animal somatic cells and human bone marrow cells, the clinical significance remains uncertain. Non-Hodgkin’s lymphoma and other tumors have been reported in patients receiving low-dose oral methotrexate. However, there have been instances of malignant lymphoma arising during treatment with low-dose oral methotrexate, which have regressed completely following withdrawal of methotrexate, without requiring active anti-lymphoma treatment. Benefits should be weighed against the potential risk before using methotrexate alone or in combination with other drugs, especially in pediatric patients or young adults. Methotrexate causes embryotoxicity, abortion, and fetal defects in humans. It has also been reported to cause impairment of fertility, oligospermia and menstrual dysfunction in humans, during and for a short period after cessation of therapy.
Pregnancy
Psoriasis and rheumatoid arthritis: Methotrexate is in Pregnancy Category X. See CONTRAINDICATIONS.
Nursing Mothers
See CONTRAINDICATIONS.
Pediatric Use
Safety and effectiveness in pediatric patients have been established only in cancer chemotherapy and in polyarticular-course juvenile rheumatoid arthritis.
Published clinical studies evaluating the use of methotrexate in children and adolescents (i.e., patients 2 to 16 years of age) with JRA demonstrated safety comparable to that observed in adults with rheumatoid arthritis (see CLINICAL PHARMACOLOGY, ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION.)
Methotrexate injectable formulations containing the preservative benzyl alcohol are not recommended for use in neonates. There have been reports of fatal "gasping syndrome" in neonates (children less than one month of age) following the administration of intravenous solutions containing the preservative benzyl alcohol. Symptoms include a striking onset of gasping respiration, hypotension, bradycardia, and cardiovascular collapse.
Serious neurotoxicity, frequently manifested as generalized or focal seizures, has been reported with unexpectedly increased frequency among pediatric patients with acute lymphoblastic leukemia who were treated with intermediate-dose intravenous methotrexate (1 gm/m2). (See PRECAUTIONS, Organ System Toxicity, Neurologic.)
Geriatric Use
Clinical studies of methotrexate did not include sufficient numbers of subjects age 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious reflecting the greater frequency of decreased hepatic and renal function, decreased folate stores, concomitant disease or other drug therapy (i.e., that interfere with renal function, methotrexate or folate metabolism) in this population (See PRECAUTIONS, Drug Interactions). Since decline in renal function may be associated with increases in adverse events and serum creatinine measurements may over estimate renal function in the elderly, more accurate methods (i.e., creatinine clearance) should be considered. Serum methotrexate levels may also be helpful. Elderly patients should be closely monitored for early signs of hepatic, bone marrow and renal toxicity. In chronic use situations, certain toxicities may be reduced by folate supplementation. Post-marketing experience suggests that the occurrence of bone marrow suppression, thrombocytopenia, and pneumonitis may increase with age. See Boxed WARNINGS and ADVERSE REACTIONS.
Organ System Toxicity
Gastrointestinal
If vomiting, diarrhea, or stomatitis occur, which may result in dehydration, methotrexate should be discontinued until recovery occurs. Methotrexate should be used with extreme caution in the presence of peptic ulcer disease or ulcerative colitis.
Hematologic
Methotrexate can suppress hematopoiesis and cause anemia, aplastic anemia, pancytopenia, leukopenia, neutropenia, and/or thrombocytopenia. In patients with malignancy and preexisting hematopoietic impairment, the drug should be used with caution, if at all. In controlled clinical trials in rheumatoid arthritis (n=128), leukopenia (WBC <3000/mm3) was seen in 2 patients, thrombocytopenia (platelets <100,000/mm3) in 6 patients, and pancytopenia in 2 patients.
In psoriasis and rheumatoid arthritis, methotrexate should be stopped immediately if there is a significant drop in blood counts. In the treatment of neoplastic diseases, methotrexate should be continued only if the potential benefit warrants the risk of severe myelosuppression. Patients with profound granulocytopenia and fever should be evaluated immediately and usually require parenteral broad-spectrum antibiotic therapy.
Hepatic
Methotrexate has the potential for acute (elevated transaminases) and chronic (fibrosis and cirrhosis) hepatotoxicity. Chronic toxicity is potentially fatal; it generally has occurred after prolonged use (generally two years or more) and after a total dose of at least 1.5 grams. In studies in psoriatic patients, hepatotoxicity appeared to be a function of total cumulative dose and appeared to be enhanced by alcoholism, obesity, diabetes and advanced age. An accurate incidence rate has not been determined; the rate of progression and reversibility of lesions is not known. Special caution is indicated in the presence of preexisting liver damage or impaired hepatic function.
In psoriasis, liver function tests, including serum albumin, should be performed periodically prior to dosing but are often normal in the face of developing fibrosis or cirrhosis. These lesions may be detectable only by biopsy. The usual recommendation is to obtain a liver biopsy at 1) pretherapy or shortly after initiation of therapy (2 to 4 months), 2) a total cumulative dose of 1.5 grams, and 3) after each additional 1.0 to 1.5 grams. Moderate fibrosis or any cirrhosis normally leads to discontinuation of the drug; mild fibrosis normally suggests a repeat biopsy in 6 months. Milder histologic findings such as fatty change and low grade portal inflammation, are relatively common pretherapy. Although these mild changes are usually not a reason to avoid or discontinue
methotrexate therapy, the drug should be used with caution.
In rheumatoid arthritis, age at first use of methotrexate and duration of therapy have been reported as risk factors for hepatotoxicity; other risk factors, similar to those observed in psoriasis, may be present in rheumatoid arthritis but have not been confirmed to date. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in this population. There is a combined reported experience in 217 rheumatoid arthritis patients with liver biopsies both before and during treatment (after a cumulative dose of at lease 1.5 g) and in 714 patients with a biopsy only during treatment. There are
64 (7%) cases of fibrosis and 1 (0.1%) case of cirrhosis. Of the 64 cases of fibrosis, 60 were deemed mild. The reticulin stain is more sensitive for early fibrosis and its use may increase these figures. It is unknown whether even longer use will increase these risks.
Liver function tests should be performed at baseline at 4 to 8 week intervals in patients receiving methotrexate for rheumatoid arthritis. Pretreatment liver biopsy should be performed for patients with a history of excessive alcohol consumption, persistently abnormal baseline liver function test values or chronic hepatitis B or C infection. During therapy, liver biopsy should be performed if there are persistent liver function test abnormalities or there is a decrease in serum albumin below the normal range (in the setting of well controlled rheumatoid arthritis).
If the results of a liver biopsy show mild changes (Roenigk, grades I, II, IIIa), methotrexate may be continued and the patient monitored as per recommendations listed above. Methotrexate should be discontinued in any patient who displays persistently abnormal liver function tests and refuses liver biopsy or in any patient whose liver biopsy shows moderate to severe changes (Roenigk grade IIIb or IV).
Infection or Immunologic States
Methotrexate should be used with extreme caution in the presence of active infection, and is usually contraindicated in patients with overt or laboratory evidence of immunodeficiency syndromes. Immunization may be ineffective when given during methotrexate therapy. Immunization with live virus vaccines is generally not recommended. There have been reports of disseminated vaccinia infections after smallpox immunizations in patients receiving methotrexate therapy. Hypogammaglobulinemia has been reported rarely.
Potentially fatal opportunistic infections, especially Pneumocystis carinii pneumonia, may occur with methotrexate therapy. When a patient presents with pulmonary symptoms, the possibility of Pneumocystis carinii pneumonia should be considered.
Neurologic
There have been reports of leukoencephalopathy following intravenous administration of methotrexate to patients who have had craniospinal irradiation. Serious neurotoxicity, frequently manifested as generalized or focal seizures, has been reported with unexpectedly increased frequency among pediatric patients with acute lymphoblastic leukemia who were treated with intermediate-dose intravenous methotrexate (1 gm/m2). Symptomatic patients were commonly noted to have leukoencephalopathy and/or microangiopathic calcifications on diagnostic imaging studies. Chronic leukoencephalopathy has also been reported in patients who received repeated doses of high-dose methotrexate with leucovorin rescue even without cranial irradiation. Discontinuation of methotrexate does not always result in complete recovery.
A transient acute neurologic syndrome has been observed in patients treated with high dose regimens. Manifestations of this stroke-like encephalopathy may include confusion, hemiparesis, transient blindness, seizures and coma. The exact cause is unknown. After the intrathecal use of methotrexate, the central nervous system toxicity which may occur can be classified as follows: acute chemical arachnoiditis manifested by such symptoms as headache, back pain, nuchal rigidity, and fever; sub-acute myelopathy characterized by paraparesis/paraplegia associated with involvement with one or more spinal nerve roots; chronic leukoencephalopathy manifested by confusion, irritability, somnolence, ataxia, dementia, seizures and coma. This condition can be progressive and even fatal.
Pulmonary
Pulmonary symptoms (especially a dry nonproductive cough) or a non-specific pneumonitis occurring during methotrexate therapy may be indicative of a potentially dangerous lesion and require interruption of treatment and careful investigation. Although clinically variable, the typical patient with methotrexate induced lung disease presents with fever, cough, dyspnea, hypoxemia, and an infiltrate on chest X-ray; infection (including pneumonia) needs to be excluded. This lesion can occur at all dosages.
Renal
Methotrexate may cause renal damage that may lead to acute renal failure. High doses of methotrexate used in the treatment of osteosarcoma may cause renal damage leading to acute renal failure. Nephrotoxicity is due primarily to the precipitation of methotrexate and 7-hydroxymethotrexate in the renal tubules. Close attention to renal function including adequate hydration, urine alkalinization and measurement of serum methotrexate and creatinine levels are essential for safe administration.
Skin
Severe, occasionally fatal, dermatologic reactions, including toxic epidermal necrolysis, Stevens-Johnson syndrome, exfoliative dermatitis, skin necrosis, and erythema multiforme, have been reported in children and adults, within days of oral, intramuscular, intravenous, or intrathecal methotrexate administration. Reactions were noted after single or multiple low, intermediate, or high doses of methotrexate in patients with neoplastic and non-neoplastic diseases.
Other precautions
Methotrexate should be used with extreme caution in the presence of debility.
Methotrexate exits slowly from third space compartments (e.g., pleural effusions or ascites). This results in a prolonged terminal plasma half-life and unexpected toxicity. In patients with significant third space accumulations, it is advisable to evacuate the fluid before treatment and to monitor plasma methotrexate levels.
Lesions of psoriasis may be aggravated by concomitant exposure to ultraviolet radiation. Radiation dermatitis and sunburn may be "recalled" by the use of methotrexate.
METHOTREXATE ADVERSE REACTIONS
IN GENERAL, THE INCIDENCE AND SEVERITY OF ACUTE SIDE EFFECTS ARE RELATED TO DOSE AND FREQUENCY OF ADMINISTRATION. THE MOST SERIOUS REACTIONS ARE DISCUSSED ABOVE UNDER ORGAN SYSTEM TOXICITY IN THE PRECAUTION SECTION. THAT SECTION SHOULD ALSO BE CONSULTED WHEN LOOKING FOR INFORMATION ABOUT ADVERSE REACTIONS WITH METHOTREXATE.
The most frequently reported adverse reactions include ulcerative stomatitis, leukopenia, nausea, and abdominal distress. Other frequently reported adverse effects are malaise, undue fatigue, chills and fever, dizziness and decreased resistance to infection.
Other adverse reactions that have been reported with methotrexate are listed below by organ system. In the oncology setting, concomitant treatment and the underlying disease make specific attribution of a reaction to methotrexate difficult.
Alimentary System
Gingivitis, pharyngitis, stomatitis, anorexia, nausea, vomiting, diarrhea, hematemesis, melena, gastrointestinal ulceration and bleeding, enteritis, pancreatitis.
Blood and Lymphatic System Disorders
Suppressed hematopoiesis, anemia, aplastic anemia, pancytopenia, leukopenia, neutropenia, thrombocytopenia, agranulocytosis, eosinophilia, lymphadenopathy and lymphoproliferative disorders (including reversible). Hypogammaglobulinemia has been reported rarely.
Cardiovascular
Pericarditis, pericardial effusion, hypotension, and thromboembolic events (including arterial thrombosis, cerebral thrombosis, deep vein thrombosis, retinal vein thrombosis, thrombophlebitis, and pulmonary embolus).
Central Nervous System:
Headaches, drowsiness, blurred vision, transient blindness, speech impairment including dysarthria and aphasia, hemiparesis, paresis and convulsions have also occurred following administration of methotrexate. Following low doses, there have been occasional reports of transient subtle cognitive dysfunction, mood alteration or unusual cranial sensations, leukoencephalopathy, or encephalopathy.
Hepatobiliary Disorders
Hepatotoxicity, acute hepatitis, chronic fibrosis and cirrhosis, hepatic failure, decrease in serum albumin, liver enzyme elevations.
Infection
There have been case reports of sometimes fatal opportunistic infections in patients receiving methotrexate therapy for neoplastic and non-neoplastic diseases. Pneumocystis carinii Pneumonia was the most common opportunistic infection. There have also been reports of infections, pneumonia, Cytomegalovirus infection, including cytomegaloviral pneumonia, sepsis, fatal sepsis, nocardiosis; histoplasmosis, cryptococcosis, Herpes zoster, H. simplex hepatitis, and disseminated H. simplex.
Musculoskeletal System
Stress fracture.
Ophthalmic
Conjunctivitis, serious visual changes of unknown etiology.
Pulmonary System
Respiratory fibrosis, respiratory failure, alveolitis, interstitial pneumonitis deaths have been reported, and chronic interstitial obstructive pulmonary disease has occasionally occurred.
Skin
Erythematous rashes, pruritus, urticaria, photosensitivity, pigmentary changes, alopecia, ecchymosis, telangiectasia, acne, furunculosis, erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome, skin necrosis, skin ulceration and exfoliative dermatitis.
Urogenital System
Severe nephropathy or renal failure, azotemia, cystitis, hematuria, proteinuria; defective oogenesis or spermatogenesis, transient oligospermia, menstrual dysfunction, vaginal discharge, and gynecomastia; infertility, abortion, fetal death, fetal defects.
Other rarer reactions related to or attributed to the use of methotrexate such as nodulosis, vasculitis, arthralgia/myalgia, loss of libido/impotence, diabetes, osteoporosis, sudden death, lymphoma, including reversible lymphomas, tumor lysis syndrome, soft tissue necrosis and osteonecrosis. Anaphylactoid reactions have been reported.
Side Effects in Double-Blind Rheumatoid Arthritis Studies
The approximate incidences of methotrexate-attributed (i.e. placebo rate subtracted) adverse reactions in 12 to 18 week double-blind studies of patients (n=128) with rheumatoid arthritis treated with low-dose oral (7.5 to 15 mg/week) pulse methotrexate, are listed below. Virtually all of these patients were on concomitant nonsteroidal anti-inflammatory drugs and some were also taking low dosages of corticosteroids. Hepatic histology was not examined in these short-term studies. (See PRECAUTIONS).
Incidence greater than 10%: Elevated liver function tests 15%, nausea/vomiting 10%.
Incidence 3% to 10%: Stomatitis, thrombocytopenia (platelet count less than 100,000/mm3).
Incidence 1% to 3%: Rash/pruritis/dermatitis, diarrhea, alopecia, leukopenia (WBC less than 3000/mm3), pancytopenia, dizziness.
Two other controlled trials of patients (n=680) with Rheumatoid Arthritis on 7.5 mg to 15 mg/wk oral doses showed an incidence of interstitial pneumonitis of 1%. (See PRECAUTIONS.)
Other less common reactions included decreased hematocrit, headache, upper respiratory infection, anorexia, arthralgias, chest pain, coughing, dysuria, eye discomfort, epistatix, fever, infection, sweating, tinnitus, and vaginal discharge.
Side Effects in Psoriasis:
There are no recent placebo-controlled trials in patients with psoriasis. There are two literature reports (Roenigk, 1969, and Nyfors, 1978) describing large series (n=204, 248) of psoriasis patients treated with methotrexate. Dosages ranged up to 25 mg per week and treatment was administered for up to four years. With the exception of alopecia, photosensitivity, and "burning of skin lesions" (each 3% to 10%), the adverse reaction rates in these reports were very similar to those in the rheumatoid arthritis studies. Rarely, painful plaque erosions may appear (Pearce, HP and Wilson, BB: Am Acad Dermatol 35: 835-838, 1996).
Side Effects in JRA Studies
The approximate incidences of adverse reactions reported in pediatric patients with JRA treated with oral, weekly doses of methotrexate (5 to 20 mg/m2/wk or 0.1 to 0.65 mg/kg/wk) were as follows (virtually all patients were receiving concomitant nosteroidal anti-inflammatory drugs, and some also were taking low doses of corticosteroids): elevated liver function tests, 14%; gastrointestinal reactions (e.g., nausea, vomiting, diarrhea), 11%; stomatitis, 2%; leukopenia, 2%; headache, 1.2%; alopecia, 0.5%; dizziness, 0.2%; and rash, 0.2%. Although there is experience with dosing up to 30 mg/m2/wk in JRA, the published data for doses above 20 mg/m2/wk are too limited to provide reliable estimates of adverse reaction rates.
OVERDOSAGE
Leucovorin is indicated to diminish the toxicity and counteract the effect of inadvertently administered overdosages of methotrexate. Leucovorin administration should begin as promptly as possible. As the time interval between methotrexate administration and leucovorin initiation increases, the effectiveness of leucovorin in counteracting toxicity decreases. Monitoring of the serum methotrexate concentration is essential in determining the optimal dose and duration of treatment with leucovorin.
In cases of massive overdosage, hydration and urinary alkalinization may be necessary to prevent the precipitation of methotrexate and/or its metabolites in the renal tubules. Generally speaking, neither hemodialysis nor peritoneal dialysis has been shown to improve methotrexate elimination. However, effective clearance of methotrexate has been reported with acute, intermittent hemodialysis using a high-flux dialyzer (Wall, SM et al: Am J Kidney Dis 28 (6): 846-854, 1996).
Accidental intrathecal overdosage may require intensive systemic support, high-dose systemic leucovorin, alkaline diuresis and rapid CSF drainage and ventriculolumbar perfusion.
In postmarketing experience, overdose with methotrexate has generally occurred with oral and intrathecal administration, although intravenous and intramuscular overdose have also been reported.
Reports of oral overdose often indicate accidental daily administration instead of weekly (single or divided doses). Symptoms commonly reported following oral overdose include those symptoms and signs reported at pharmacologic doses, particularly hematologic and gastrointestinal reaction. For example, leukopenia, thrombocytopenia, anemia, pancytopenia, bone marrow suppression, mucositis, stomatitis, oral ulceration, nausea, vomiting, gastrointestinal ulceration, gastrointestinal bleeding. In some cases, no symptoms were reported. There have been reports of death following overdose. In these cases, events such as sepsis or septic shock, renal failure, and aplastic anemia were also reported.
Symptoms of intrathecal overdose are generally central nervous system (CNS) symptoms, including headache, nausea and vomiting, seizure or convulsion, and acute toxic encephalopathy. In some cases, no symptoms were reported. There have been reports of death following intrathecal overdose. In these cases, cerebellar herniation associated with increased intracranial pressure, and acute toxic encephalopathy have also been reported.
There are published case reports of intravenous and intrathecal carboxypeptidase G2 treatment to hasten clearance of methotrexate in cases of overdose.
METHOTREXATE DOSAGE AND ADMINISTRATION
Neoplastic Diseases
Oral administration in tablet form is often preferred when low doses are being administered since absorption is rapid and effective serum levels are obtained. Methotrexate injection may be given by the intramuscular, intravenous, intra-arterial or intrathecal (Only preservative free) route. However, the preserved formulation contains Benzyl Alcohol and must not be used for intrathecal or high dose therapy. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Choriocarcinoma and similar trophoblastic diseases
Methotrexate is administered orally or intramuscularly in doses of 15 to 30 mg daily for a five-day course. Such courses are usually repeated for 3 to 5 times as required, with rest periods of one or more weeks interposed between courses, until any manifesting toxic symptoms subside. The effectiveness of therapy is ordinarily evaluated by 24 hour quantitative analysis of urinary chorionic gonadotropin (hCG), which should return to normal or less than 50 IU/24 hr usually after the third or fourth course and usually be followed by a complete resolution of measurable lesions in 4 to 6 weeks. One to two courses of methotrexate after normalization of hCG is usually recommended. Before each course of the drug careful clinical assessment is essential. Cyclic combination therapy of methotrexate with other antitumor drugs has been reported as being useful.
Since hydatidiform mole may precede choriocarcinoma, prophylactic chemotherapy with methotrexate has been recommended.
Chorioadenoma destruens is considered to be an invasive form of hydatidiform mole.
Methotrexate is administered in these disease states in doses similar to those recommended for choriocarcinoma.
Leukemia
Acute lymphoblastic leukemia in pediatric patients and young adolescents is the most responsive to present day chemotherapy. In young adults and older patients, clinical remission is more difficult to obtain and early relapse is more common.
Methotrexate alone or in combination with steroids was used initially for induction of remission in acute lymphoblastic leukemias. More recently corticosteroid therapy, in combination with other antileukemic drugs or in cyclic combinations with methotrexate included, has appeared to produce rapid and effective remissions.
When used for induction, methotrexate in doses of 3.3 mg/m2 in combination with 60 mg/m2 of prednisone, given daily, produced remissions in 50% of patients treated, usually within a period of 4 to 6 weeks. Methotrexate in combination with other agents appears to be the drug of choice for securing maintenance of drug-induced remissions. When remission is achieved and supportive care has produced general clinical improvement, maintenance therapy is initiated, as follows: Methotrexate is administered 2 times weekly either by mouth or intramuscularly in total weekly doses of 30 mg/m2. It has also been given in doses of 2.5 mg/kg intravenously every 14 days. If and when
relapse does occur, reinduction of remission can again usually be obtained by repeating the initial induction regimen.
A variety of combination chemotherapy regimens have been used for both induction and maintenance therapy in acute lymphoblastic leukemia. The physician should be familiar with the new advances in antileukemic therapy.
Meningeal Leukemia
In the treatment of prophylaxis of meningeal leukemia, methotrexate must be administered intrathecally. Preservative free methotrexate is diluted to a concentration of 1 mg/mL in an appropriate sterile, preservative free medium such as 0.9% Sodium Chloride Injection, USP.
The cerebrospinal fluid volume is dependent on age and not on body surface area. The CSF is at 40% of the adult volume at birth and reaches the adult volume in several years.
Intrathecal methotrexate administration at a dose of 12 mg/m2 (maximum 15 mg) has been reported to result in low CSF methotrexate concentrations and reduced efficacy in pediatric patients and high concentrations and neurotoxicity in adults. The following dosage regimen is based on age instead of body surface area:
|
AGE
(
years
)
|
DOSE
(
mg
)
|
| <1 |
6 |
| 1 |
8 |
| 2 |
10 |
| 3 or older |
12 |
In one study in patients under the age of 40, this dosage regimen appeared to result in more consistent CSF methotrexate concentrations and less neurotoxicity. Another study in pediatric patients with acute lymphocytic leukemia compared this regimen to a dose of 12 mg/m2 (maximum 15 mg), a significant reduction in the rate of CNS relapse was observed in the group whose dose was based on age.
Because the CSF volume and turnover may decrease with age, a dose reduction may be indicated in elderly patients.
For treatment of meningeal leukemia, intrathecal methotrexate may be given at intervals of 2 to 5 days. However, administration at intervals of less than 1 week may result in increased subacute toxicity. Methotrexate is administered until the cell count of the cerebrospinal fluid returns to normal. At this point one additional dose is advisable. For prophylaxis against meningeal leukemia, the dosage is the same as for treatment except for the intervals of administration. On this subject, it is advisable for the physician to consult the medical literature.
Untoward side effects may occur with any given intrathecal injection and are commonly neurological in character. Large doses may cause convulsions. Methotrexate given by the intrathecal route appears significantly in the systemic circulation and may cause systemic methotrexate toxicity. Therefore, systemic antileukemic therapy with the drug should be appropriately adjusted, reduced or discontinued. Focal leukemic involvement of the central nervous system may not respond to intrathecal chemotherapy and is best treated with radiotherapy.
Lymphomas
In Burkitt’s tumor, Stages I-II, methotrexate has produced prolonged remissions in some cases. Recommended dosage is 10 to 25 mg/day orally for 4 to 8 days. In Stage III, methotrexate is commonly given concomitantly with other antitumor agents. Treatment in all stages usually consists of several courses of the drug interposed with 7 to 10 day rest periods. Lymphosarcomas in Stage III may respond to combined drug therapy with methotrexate given in doses of 0.625 to 2.5 mg/kg daily.
Mycosis fungoides (cutaneous T cell lymphoma)
Therapy with methotrexate as a single agent appears to produce clinical responses in up to 50% of patients treated. Dosage in early stages is usually 5 to 50 mg once weekly. Dose reduction or cessation is guided by patient response and hematologic monitoring. Methotrexate has also been administered twice weekly in doses ranging from 15 to 37.5 mg in patients who have responded poorly to weekly therapy. Combination chemotherapy regimens that include intravenous methotrexate administered at higher doses with leucovorin rescue have been utilized in advanced stages of the disease.
Osteosarcoma
An effective adjuvant chemotherapy regimen requires the administration of several cytotoxic chemotherapeutic agents. In addition to high-dose methotrexate with leucovorin rescue, these agents may include doxorubicin, cisplatin, and the combination of bleomycin, cyclophosphamide and dactinomycin (BCD) in the doses and schedule shown in the table below. The starting dose for high-dose methotrexate treatment is 12 grams/m2. If this dose is not sufficient to produce a peak serum methotrexate concentration of 1,000 micromolar (10-3 mol/L) at the end of the methotrexate infusion, the dose may be escalated to 15 grams/m2 in subsequent treatments. If the patient is vomiting or is unable to tolerate oral medication, leucovorin is given IV or IM at the same dose and schedule.
|
*Link MP, Goorin AM, Miser AW, et al: The effect of adjuvant chemotherapy on relapse-free survival in patients with osteosarcoma of the extremity. N
Engl
J
of
Med 1986; 314 (No.25): 1600-1606. |
||
|
†See each respective package insert for full prescribing information. Dosage modifications may be necessary because of drug-induced toxicity. |
||
|
When these higher doses of methotrexate are to be administered, the following safety guidelines should be |
||
|
closely observed. |
||
|
Drug
*
|
Dose
*
|
Treatment
Week
After Surgery |
| Methotrexate
|
12 g/m2 IV as 4 hour infusion (starting dose) |
4,5,6,7,11,12,15,16,29,30,44,45 |
|
|
15 mg orally every six hours for |
|
| Leucovorin |
10 doses starting at 24 hours after |
- - - |
|
|
start of methotrexate infusion |
|
| Doxorubicin† as a single drug
|
30 mg/m2 day IV x 3 days
|
8,17 |
| Doxorubicin†
|
50 mg/m2 IV
|
20,23,33,36 |
| Cisplatin†
|
100 mg/m2 IV
|
20,23,33,36 |
| Bleomycin†
|
15 units/m2 IV x 2 days
|
2,13,26,39,42 |
| Cyclophosphamide†
|
600 mg/m2 IV x 2 days
|
2,13,26,39,42 |
| Dactinomycin†
|
0.6 mg/m2 IV x 2 days
|
2,13,26,39,42 |
GUIDELINES FOR METHOTREXATE THERAPY WITH
LEUCOVORIN RESCUE
- Administration of methotrexate should be delayed until recovery if:
- the WBC count is less than 1500/microliter
- the neutrophil count is less than 200/microliter
- the platelet count is less than 75,000/microliter
- the serum bilirubin level is greater than 1.2 mg/dL
- the SGPT level is greater than 450 U
- mucositis is present, until there is evidence of healing
- persistent pleural effusion is present; this should be drained dry prior to infusion.
- Adequate renal function must be documented.
- Serum creatinine must be normal, and creatinine clearance must be greater than 60 mL/min, before initiation of therapy.
- Serum creatinine must be measured prior to each subsequent course of therapy. If serum creatinine has increased by 50% or more compared to a prior value, the creatinine clearance must be measured and documented to be greater than 60 mL/min (even if the serum creatinine is still within the normal range).
- Patients must be well hydrated, and must be treated with sodium bicarbonate for urinary alkalinization.
- Administer 1,000 mL/m2 of intravenous fluid over 6 hours prior to initiation of the methotrexate infusion. Continue hydration at 125 mL/m2/hr (3 liters/m2/day) during the methotrexate infusion, and for 2 days after the infusion has been completed.
- Alkalinize urine to maintain pH above 7.0 during methotrexate infusion and leucovorin calcium therapy. This can be accomplished by the administration of sodium bicarbonate orally or by incorporation into a separate intravenous solution.
- Repeat serum creatinine and serum methotrexate 24 hours after starting methotrexate and at least once daily until the methotrexate level is below 5 x 10-8 mol/L (0.05 micromolar).
- The table below provides guidelines for leucovorin calcium dosage based upon serum methotrexate levels. (See table below.‡) Patients who experience delayed early methotrexate elimination are likely to develop nonreversible oliguric renal failure. In addition to appropriate leucovorin therapy, these patients require continuing hydration and urinary alkalinization, and close monitoring of fluid and electrolyte status, until the serum methotrexate level has fallen to below 0.05 micromolar and the renal failure has resolved. If necessary, acute, intermittent hemodialysis with a high-flux dialyzer may also be beneficial in these patients.
- Some patients will have abnormalities in methotrexate elimination, or abnormalities in renal function following methotrexate administration, which are significant but less severe than the abnormalities described in the table below. These abnormalities may or may not be associated with significant clinical toxicity. If significant toxicity is observed, leucovorin rescue should be extended for an additional 24 hours (total 14 doses over 84 hours) in subsequent courses of therapy. The possibility that the patient is taking other medications which interact with methotrexate (e.g., medications which may interfere with methotrexate binding to serum albumin, or elimination) should always be reconsidered when laboratory abnormalities or clinical toxicities are observed.
CAUTION: DO NOT ADMINISTER LEUCOVORIN INTRATHECALLY.
Psoriasis, Rheumatoid Arthritis, and Juvenile Rheumatoid Arthritis
Adult Rheumatoid Arthritis: Recommended Starting Dosage Schedules
- Single oral doses of 7.5 mg once weekly. †
- Divided oral dosages of 2.5 mg at 12 hour intervals for 3 doses given as a course once weekly.†
† Methotrexate Sodium Tablets for oral administration are available.
Polyarticular-Course Juvenile Rheumatoid Arthritis: The recommended starting dose is 10 mg/m2 given once weekly.
For either adult RA or polyarticular-course JRA, dosages may be adjusted gradually to achieve an optimal response. Limited experience shows a significant increase in the incidence and severity of serious toxic reactions, especially bone marrow suppression, at doses greater than 20 mg/wk in adults. Although there is experience with doses up to 30 mg/m2/wk in children, there are too few published data to assess how doses over 20 mg/m2/wk might affect the risk of serious toxicity in children. Experience does suggest, however, that children receiving 20 to 30 mg/m2/wk (0.65 to 1.0 mg/kg/wk) may have better absorption and fewer gastrointestinal side effects if methotrexate is administered either intramuscularly or subcutaneously.
Therapeutic response usually begins within 3 to 6 weeks and the patient may continue to improve for another 12 weeks or more.
The optimal duration of therapy is unknown. Limited data available from long-term studies in adults indicate that the initial clinical improvement is maintained for at least two years with continued therapy. When methotrexate is discontinued, the arthritis usually worsens within 3 to 6 weeks.
The patient should be fully informed of the risks involved and should be under constant supervision of the physician. (See Information for Patients under PRECAUTIONS). Assessment of hematologic, hepatic, renal, and pulmonary function should be made by history, physical examination, and laboratory tests before beginning, periodically during, and before reinstituting methotrexate therapy. (See PRECAUTIONS). Appropriate steps should be taken to avoid conception during methotrexate therapy. (See PRECAUTIONS and CONTRAINDICATIONS).
All schedules should be continually tailored to the individual patient. An initial test dose may be given prior to the regular dosing schedule to detect any extreme sensitivity to adverse effects (See ADVERSE REACTIONS). Maximal myelosuppression usually occurs in seven to ten days.
Psoriasis: Recommended Starting Dose Schedule:
- Weekly single oral, IM or IV dosage schedule: 10 to 25 mg per week until adequate response is achieved. †
- Divided oral dose schedule 2.5 mg at 12 hour intervals for three doses. †
†Methotrexate Sodium Tablets for oral administration are available.
Dosages in each schedule may be gradually adjusted to achieve optimal clinical response; 30 mg/week should not ordinarily be exceeded.
Once optimal clinical response has been achieved, each dosage schedule should be reduced to the lowest possible amount of drug and to the longest possible rest period. The use of methotrexate may permit the return to conventional topical therapy, which should be encouraged.
HANDLING AND DISPOSAL
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1-7 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
DILUTION INSTRUCTIONS FOR LIQUID METHOTREXATE INJECTION PRODUCT
If desired, the solution may be further diluted immediately prior to use with an appropriate sterile, preservative free medium such as 5% Dextrose Solution, USP or Sodium Chloride Injection, USP.
HOW SUPPLIED
Parenteral
Methotrexate Injection, USP is a preservative free solution supplied in single dose vials.
Each 25 mg/mL, 2 mL, 4 mL, 8 mL, 10 mL and 40 mL vial packed individually contains methotrexate sodium equivalent to 50 mg, 100 mg, 200 mg, 250 mg and 1 g methotrexate respectively.
NDC 0069-0146-01 50 mg in 2 mL (Individually boxed)
NDC 0069-0147-01 100 mg in 4 mL (Individually boxed)
NDC 0069-0181-01 200 mg in 8 mL (Individually boxed)
NDC 0069-0148-01 250 mg in 10 mL (Individually boxed)
NDC 0069-0146-02 50 mg in 2 mL (5 individually boxed vials in a carton)
NDC 0069-0147-02 100 mg in 4 mL (10 individually boxed vials in a carton)
NDC 0069-0181-02 200 mg in 8 mL (10 individually boxed vials in a carton)
NDC 0069-0149-01 1 g in 40 mL Vial (Individually boxed)
Store at 20° to 25° C (68° to77° F) [see USP controlled room temperature]
PROTECT FROM LIGHT
Distributed by
Pfizer labs
Division of Pfizer Inc.
New York, NY 10017
Revision: March 2012
|
Clinical
Situation
|
Laboratory
Findings
|
Leucovorin
Dosage
and
Duration
|
| Normal Methotrexate Elimination
|
Serum methotrexate level approximately 10 micromolar at 24 hours after administration, 1 micromolar at 48 hours, and less than 0.2 micromolar at 72 hours. |
15 mg PO, IM, or IV q 6 hours
for 60 hours (10 doses starting at 24 hours after start of methotrexate infusion). |
| Delayed Late Methotrexate Elimination |
Serum methotrexate level
remaining above 0.2 micromolar at 72 hours, and more than 0.05 micromolar at 96 hours after administration. |
Continue 15 mg PO, IM, or IV q six hours, until methotrexate level is less than 0.05 micromolar.
|
| Delayed Early Methotrexate Elimination and/or Evidence of Acute Renal Injury |
Serum methotrexate level of 50 micromolar or more at 24 hours, or 5micromolar or more at 48hours after administration, or; a100% or greater increase in serum creatinine level at 24 hours after methotrexate administration, (e.g., an increase from 0.5 mg/dL to a level of 1 mg/dL or more). |
150 mg IV q three hours, until
methotrexate level is less than 1 micromolar; then 15 mg IV q three hours until methotrexate level is less than 0.05 micromolar. |
REFERENCES
- Controlling Occupation Exposure to Hazardous Drugs (OSHA Work-Practice Guidelines). Am J Health Syst Pharma 1996: 53:1669-1685.
- Recommendations for the Safe Handling of Parenteral Antineoplastic Drugs. NIH Publication No. 83-2621. For sale by the Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402.
- AMA Council Report. Guidelines for Handling Parenteral Antineoplastics. JAMA,1985; 253(11):1590-1592.
- National Study Commission on Cytotoxic Exposure-Recommendations for Handling Cytotoxic Agents. Available from Louis P. Jeffrey, ScD, Chairman, National Study Commission on Cytotoxic Exposure, Massachusetts College of Pharmacy and Allied Health Sciences, 179 Longwood Avenue, Boston, Massachusetts 02115.
- Clinical Oncological Society of Australia: Guidelines and Recommendations for Safe Handling of Antineoplastic Agents. Med J Australia 1983; 1:426-428.
- Jones RB, et al. Safe Handling of Chemotherapeutic Agents: A Report from the Mount Sinai Medical Center. Ca- A Cancer Journal for Clinicians Sept/Oct 1983; 258-263.
- American Society of Hospital Pharmacists Technical Assistance Bulletin on Handling Cytotoxic and Hazardous Drugs. Am J Hosp Pharm 1990; 47:1033-1049.
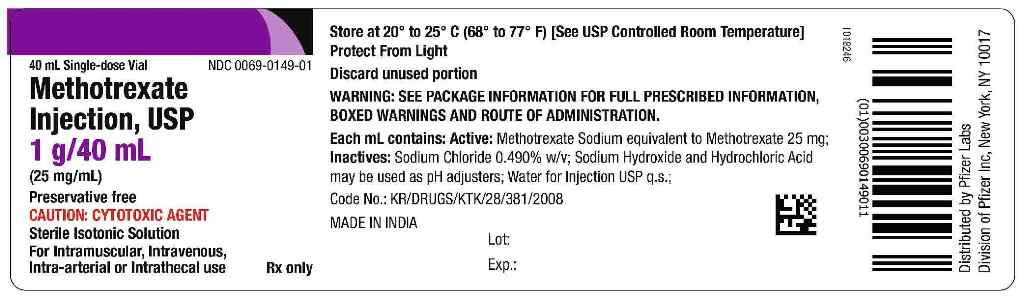
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Methotrexate Injection, USP 1 g/40 mL
Rx Only
40 mL Single Dose Vial
Preservative free
Sterile Isotonic Solution
For Intramuscular, Intravenous, Intra-arterial or Intrathecal use
Cytotoxic Agent
MethotrexateMethotrexate INJECTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||