Metronidazole
Pfizer Labs, Division of Pfizer Inc
Claris Lifesciences Limited
Metronidazole Injection, USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- Description
- Clinical Pharmacology
- Metronidazole Indications and Usage
- Contraindications
- Warnings
- Precautions
- Side Effects
- Overdosage
- Dosage and Administration
- How Supplied
- Directions for Use of Plastic Container
- References
- Metronidazole Injection, USP Container Label
- Metronidazole Injection, USP Casepack Label
FULL PRESCRIBING INFORMATION
Rx only
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Metronidazole Injection, USP and other antibacterial drugs, Metronidazole Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
WARNING
Metronidazole has been shown to be carcinogenic in mice and rats (see Precautions). Its use, therefore, should be reserved for the conditions described in the Indications and Usage section below.
Description
Metronidazole Injection, USP,is a parenteral dosage form of the synthetic antibacterial agent 1-(β-hydroxyethyl)-2-methyl-5- nitroimidazole.

Metronidazole Injection, USP, in 100 mL single dose plastic container, is a sterile, nonpyrogenic, iso-osmotic, buffered solution of 500 mg Metronidazole, USP, 790 mg Sodium Chloride, USP, 47.6 mg Anhydrous Disodium Hydrogen Phosphate, USP and 22.9 mg Citric Acid Monohydrate, USP. Metronidazole Injection, USP has an osmolarity of 310 mOsmol/L (calc) and a pH of 5.5 (4.5 to 7.0). Each container contains 14 mEq of sodium.
The plastic container is fabricated from a specially formulated polyvinyl chloride plastic. Water can permeate from inside the container into the overwrap in amounts insufficient to affect the solution significantly. Solutions in contact with the plastic container can leach out certain of its chemical components in very small amounts within the expiration period, e.g., di-2-ethylhexyl phthalate (DEHP), up to 5 parts per million. However, the safety of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers.
Clinical Pharmacology
Metronidazole is a synthetic antibacterial compound. Disposition of metronidazole in the body is similar for both oral and intravenous dosage forms, with an average elimination half-life in healthy humans of eight hours.
The major route of elimination of metronidazole and its metabolites is via the urine (60 - 80% of the dose), with fecal excretion accounting for 6 - 15% of the dose. The metabolites that appear in the urine result primarily from side-chain oxidation (1-[β-hydroxyethyl]-2-hydroxymethyl- 5-nitroimidazole and 2-methyl-5-nitroimidazole-1-yl-acetic acid) and glucuronide conjugation, with unchanged metronidazole accounting for approximately 20% of the total. Renal clearance of metronidazole is approximately 10 mL/min/1.73 m2.
Metronidazole is the major component appearing in the plasma, with lesser quantities of the 2-hydroxymethyl metabolite also being present. Less than 20% of the circulating metronidazole is bound to plasma proteins. Both the parent compound and the metabolite possess in vitro bactericidal activity against most strains of anaerobic bacteria.
Metronidazole appears in cerebrospinal fluid, saliva and breast milk in concentrations similar to those found in plasma. Bactericidal concentrations of metronidazole have also been detected in pus from hepatic abscesses..
Plasma concentrations of metronidazole are proportional to the administered dose. An eight-hour intravenous infusion of 100-4,000 mg of metronidazole in normal subjects showed a linear relationship between dose and peak plasma concentration.
In patients treated with intravenous metronidazole, using a dosage regimen of 15 mg/kg loading dose followed six hours later by 7.5 mg/kg every six hours; peak steady-state plasma concentrations of metronidazole averaged 25 mcg/mL with trough (minimum) concentrations averaging 18 mcg/mL.
Decreased renal function does not alter the single-dose pharmacokinetics of metronidazole. However, plasma clearance of metronidazole is decreased in patients with decreased liver function.
In one study newborn infants appeared to demonstrate diminished capacity to eliminate metronidazole. The elimination half-life, measured during the first three days of life, was inversely related to gestational age. In infants whose gestational ages were between 28 and 40 weeks, the corresponding elimination half-lives ranged from 109 to 22.5 hours.
Microbiology: Metronidazole is active in vitro against most obligate anaerobes, but does not appear to possess any clinically relevant activity against facultative anaerobes or obligate aerobes. Against susceptible organisms, metronidazole is generally bactericidal at concentrations equal to or slightly higher than the minimal inhibitory concentrations. Metronidazole has been shown to have in vitro and clinical activity against the following organisms:
Anaerobic gram-negative bacilli, including:
Bacteroides species, including the Bacteroides fragilis group (B.
fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus)
Fusobacterium species
Anaerobic
gram-positive bacilli, including:
Clostridium species and susceptible strains of Eubacterium
Anaerobic gram-positive cocci, including:
Peptococcus species
Peptostreptococcus species
Susceptibility Tests: Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to metronidazole; however, the rapid routine susceptibility testing of individual isolates of anaerobic bacteria is not always practical, and therapy may be started while awaiting these results.
Quantitative methods give the most accurate estimates of susceptibility to antibacterial drugs. A standardized agar dilution method and a broth microdilution method are recommended.1
Control strains are recommended for standardized susceptibility testing. Each time the test is performed, one or more of the following strains should be included: Eubacterium lentum ATCC 43055, Bacteroides fragilis ATCC 25285, and Bacteroides thetaiotaomicron ATCC 29741. The mode metronidazole MICs for those three strains are reported to be 0.125, 0.25, and 0.5 mcg/mL, respectively.
A clinical laboratory test is considered under acceptable control if the results of the control strains are within one doubling dilution of the mode MICs reported for metronidazole.
A bacterial isolate may be considered susceptible if the MIC value for metronidazole is not more than 16 mcg/mL. An organism is considered resistant if the MIC is greater than 16 mcg/mL. A report of “resistant” from the laboratory indicates that the infecting organism is not likely to respond to therapy.
Metronidazole Indications and Usage
Treatment of Anaerobic Infections
Metronidazole Injection, USP is indicated in the treatment of serious infections caused by susceptible anaerobic bacteria. Indicated surgical procedures should be performed in conjunction with Metronidazole Injection, USP therapy. In a mixed aerobic and anaerobic infection, antibiotics appropriate for the treatment of the aerobic infection should be used in addition to Metronidazole Injection, USP.
Metronidazole is effective in Bacteroides fragilis infections resistant to clindamycin, chloramphenicol and penicillin.
Intra-Abdominal Infections, including peritonitis, intra-abdominal abscess and liver abscess, caused by Bacteroides species including the B. fragilis group (B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus), Clostridium species, Eubacterium species, Peptococcus species and Peptostreptococcus species.
Skin and Skin Structure Infections caused by Bacteroides species including the B. fragilis group, Clostridium species, Peptococcus species, Peptostreptococcus species and Fusobacterium species.
Gynecologic Infections, including endometritis, endomyometritis, tubo-ovarian abscess, and post-surgical vaginal cuff infection, caused by Bacteroides species including the B. fragilis group, Clostridium species, Peptostreptococcus species and Fusobacterium species.
Bacterial Septicemia caused by Bacteroides species including the B. fragilis group and Clostridium species.
Bone and Joint Infections, as adjunctive therapy, caused by Bacteroides species including the B. fragilis group.
Central Nervous System (CNS) Infections, including meningitis and brain abscess, caused by Bacteroides species including the B. fragilis group.
Lower Respiratory Tract Infections, including pneumonia, empyema, and lung abscess, caused by Bacteroides species including the B. fragilis group.
Endocarditis caused by Bacteroides species including the B. fragilis group.
Prophylaxis:
The prophylactic administration of Metronidazole Injection, USP preoperatively, intraoperatively and postoperatively may reduce the incidence of postoperative infection in patients undergoing elective colorectal surgery, which is classified as contaminated or potentially contaminated.
Prophylactic use of Metronidazole Injection, USP should be discontinued within 12 hours after surgery. If there are signs of infection, specimens for cultures should be obtained for the identification of the causative organism(s) so that appropriate therapy may be given (see Dosage and Administration).
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Metronidazole Injection, USP and other antibacterial drugs, Metronidazole Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Contraindications
Metronidazole Injection, USP is contraindicated in patients with a prior history of hypersensitivity to metronidazole or other nitroimidazole derivatives.
Warnings
Central and Peripheral Nervous System Effects:
Convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity, have been reported in patients treated with metronidazole. The appearance of abnormal neurologic signs demands the prompt evaluation of the benefit/risk ratio of the continuation of therapy.
Precautions
General:
Patients with severe hepatic disease metabolize metronidazole slowly, with resultant accumulation of metronidazole and its metabolites in the plasma. Accordingly, for such patients, doses below those usually recommended should be administered cautiously.
Administration of solutions containing sodium ions may result in sodium retention. Care should be taken when administering Metronidazole Injection, USP to patients receiving corticosteroids or to patients predisposed to edema.
Known or previously unrecognized candidiasis may present more prominent symptoms during therapy with Metronidazole Injection, USP and requires treatment with a candidacidal agent.
Prescribing Metronidazole Injection, USP in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Laboratory Tests:
Metronidazole is a nitroimidazole, and should be used with care in patients with evidence of or history of blood dyscrasia. A mild leukopenia has been observed during its administration; however, no persistent hemotologic abnormalities attributable to metronidazole have been observed in clinical studies. Total and differential leukocyte counts are recommended before and after therapy.
Drug Interactions:
Metronidazole has been reported to potentiate the anticoagulant effect of warfarin and other oral coumarin anticoagulants, resulting in a prolongation of prothrombin time. This possible drug interaction should be considered when Metronidazole Injection, USP is prescribed for patients on this type of anticoagulant therapy.
The simultaneous administration of drugs that induce microsomal liver enzyme activity, such as phenytoin or phenobarbital, may accelerate the elimination of metronidazole, resulting in reduced plasma levels; impaired clearance of phenytoin has also been reported.
The simultaneous administration of drugs that decrease microsomal liver enzyme activity, such as cimetidine, may prolong the half-life and decrease plasma clearance of metronidazole.
Alcoholic beverages should not be consumed during metronidazole therapy because abdominal cramps, nausea, vomiting, headaches and flushing may occur.
Psychotic reactions have been reported in alcoholic patients who are using metronidazole and disulfiram concurrently. Metronidazole should not be given to patients who have taken disulfiram within the last two weeks.
Drug/Laboratory Test Interactions:
Metronidazole may interfere with certain types of determinations of serum chemistry values, such as aspartate aminotransferase (AST, SGOT), alanine aminotransferase (ALT, SGPT), lactate dehydrogenase (LDH), triglycerides and hexokinase glucose. Values of zero may be observed. All of the assays in which interference has been reported involve enzymatic coupling of the assay to oxidation-reduction of nicotine adenine dinucleotide (NAD+ ↔ NADH). Interference is due to the similarity in absorbance peaks of NADH (340nm) and metronidazole (322nm) at pH 7.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Tumorigenicity in Rodents - Metronidazole has shown evidence of carcinogenic activity in studies involving chronic, oral administration in mice and rats, but similar studies in the hamster gave negative results. Also, metronidazole has shown mutagenic activity in a number of in vitro assay systems, but studies in mammals (in vivo) failed to demonstrate a potential for genetic damage.
Pregnancy: Teratogenic effects
Pregnancy Category B. Metronidazole crosses the placental barrier and enters the fetal circulation rapidly. Reproduction studies have been performed in rats at doses up to five times the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to metronidazole. Metronidazole administered intraperitoneally to pregnant mice at approximately the human dose caused fetotoxicity; administered orally to pregnant mice, no fetotoxicity was observed. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, and because metronidazole is a carcinogen in rodents, these drugs should be used during pregnancy only if clearly needed.
Nursing Mothers
Because of the potential for tumorigenicity shown for metronidazole in mouse and rat studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Metronidazole is secreted in breast milk in concentrations similar to those found in plasma.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Information for Patients
Patients should be counseled that antibacterial drugs including Metronidazole Injection, USP should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Metronidazole Injection, USP is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Metronidazole Injection, USP or other antibacterial drugs in the future.
Side Effects
The most serious adverse reactions reported in patients treated with metronidazole injection have been convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity. Since persistent peripheral neuropathy has been reported in some patients receiving prolonged oral administration of metronidazole, patients should be observed carefully if neurologic symptoms occur and a prompt evaluation made of the benefit/risk ratio of the continuation of therapy.
The following reactions have also been reported during treatment with Metronidazole Injection, USP.
Gastrointestinal: Nausea, vomiting, abdominal discomfort, diarrhea and an unpleasant metallic taste.
Hematopoietic: Reversible neutropenia (leukopenia).
Dermatologic: Erythematous rash and pruritus.
Central Nervous System: Encephalopathy, aseptic meningitis, optic neuropathy, headache, dizziness, syncope, ataxia, confusion and dysarthria.
Local Reactions: Thrombophlebitis after intravenous infusion. This reaction can be minimized or avoided by avoiding prolonged use of indwelling intravenous catheters.
Other: Fever. Instances of darkened urine have also been reported, and this manifestation has been the subject of a special investigation. Although the pigment, which is probably responsible for this phenomenon, has not been positively identified, it is almost certainly a metabolite of metronidazole and seems to have no clinical significance.
The following adverse reactions have been reported during treatment with oral metronidazole:
Gastrointestinal: Nausea, sometimes accompanied by headache, anorexia and occasionally vomiting; diarrhea, epigastric distress, abdominal cramping and constipation.
Mouth: A sharp, unpleasant metallic taste is not unusual. Furry tongue, glossitis and stomatitis have occurred; these may be associated with a sudden overgrowth of Candida , which may occur during effective therapy.
Hematopoietic: Reversible neutropenia (leukopenia); rarely, reversible thrombocytopenia.
Cardiovascular: Flattening of the T-wave may be seen in electrocardiographic tracings.
Central Nervous System: Encephalopathy, aseptic meningitis, convulsive seizures, optic neuropathy, peripheral neuropathy, dizziness, vertigo, incoordination, ataxia, confusion, dysarthria, irritability, depression, weakness and insomnia.
Hypersensitivity: Urticaria, erythematous rash, Stevens-Johnson Syndrome, flushing, nasal congestion, dryness of the mouth (or vagina or vulva) and fever.
Renal: Dysuria, cystitis, polyuria, incontinence, a sense of pelvic pressure and darkened urine.
Other: Proliferation of Candida in the vagina, dyspareunia, decrease of libido, proctitis and fleeting joint pains sometimes resembling “serum sickness.” If patients receiving metronidazole drink alcoholic beverages, they may experience abdominal distress, nausea, vomiting, flushing or headache. A modification of the taste of alcoholic beverages has also been reported. Rare cases of pancreatitis, which abated on withdrawal of the drug, have been reported.
Crohn's disease patients are known to have an increased incidence of gastrointestinal and certain extraintestinal cancers. There have been some reports in the medical literature of breast and colon cancer in Crohn's disease patients who have been treated with metronidazole at high doses for extended periods of time. A cause and effect relationship has not been established. Crohn's disease is not an approved indication for Metronidazole Injection, USP.
Overdosage
Use of dosages of intravenous metronidazole higher than those recommended has been reported. These include the use of 27 mg/kg three times a day for 20 days, and the use of 75 mg/kg as a single loading dose followed by 7.5 mg/kg maintenance doses. No adverse reactions were reported in either of the two cases.
Single oral dose of metronidazole, up to 15 g, have been reported in suicide attempts and accidental overdoses. Symptoms reported included nausea, vomiting and ataxia.
Oral metronidazole has been studied as a radiation sensitizer in the treatment of malignant tumors. Neurotoxic effects, including seizures and peripheral neuropathy, have been reported after 5 to 7 days of doses of 6 to 10.4 g every other day.
Treatment: There is no specific antidote for overdose; therefore, management of the patient should consist of symptomatic and supportive therapy.
Dosage and Administration
In elderly patients the pharmacokinetics of metronidazole may be altered and therefore monitoring of serum levels may be necessary to adjust the metronidazole dosage accordingly.
Treatment of Anaerobic Infections
The recommended dosage schedule for adults is:
|
Loading Dose: |
15 mg/kg infused over one hour (approximately 1 g for a 70-kg adult). |
|
Maintenance Dose: |
7.5 mg/kg infused over one hour every six hours (approximately 500 mg for a 70-kg adult). The first maintenance dose should be instituted six hours following the initiation of the loading dose. |
Parenteral therapy may be changed to oral metronidazole when conditions warrant, based upon the severity of the disease and the response of the patient to Metronidazole Injection, USP treatment. The usual adult oral dosage is 7.5 mg/kg every six hours.
A maximum of 4 g should not be exceeded during a 24-hour period.
Patients with severe hepatic disease metabolize metronidazole slowly, with resultant accumulation of metronidazole and its metabolites in the plasma. Accordingly, for such patients, doses below those usually recommended should be administered cautiously. Close monitoring of plasma metronidazole levels2 and toxicity is recommended.
In patients receiving Metronidazole Injection, USP in whom gastric secretions are continuously removed by nasogastric aspiration, sufficient metronidazole may be removed in the aspirate to cause a reduction in serum levels.
The dose of Metronidazole Injection, USP should not be specifically reduced in anuric patients since accumulated metabolites may be rapidly removed by dialysis.
The usual duration of therapy is 7 to 10 days; however, infections of the bone and joint, lower respiratory tract and endocardium may require longer treatment.
Prophylaxis:
For surgical prophylactic use, to prevent postoperative infection in contaminated or potentially contaminated colorectal surgery, the recommended dosage schedule for adults is:
- 15 mg/kg infused over 30 to 60 minutes and completed approximately one hour before surgery; followed by
- 7.5 mg/kg infused over 30 to 60 minutes at 6 and 12 hours after the initial dose.
It is important that (1) administration of the initial preoperative dose be completed approximately one hour before surgery so that adequate drug levels are present in the serum and tissues at the time of initial incision, and (2) Metronidazole Injection, USP be administered, if necessary, at 6-hour intervals to maintain effective drug levels. Prophylactic use of Metronidazole Injection, USP should be limited to the day of surgery only, following the above guidelines.
Caution: Metronidazole Injection, USP is to be administered by slow intravenous drip infusion only, either as a continuous or intermittent infusion. Additives should not be introduced into Metronidazole Injection, USP. If used with a primary intravenous fluid system, the primary solution should be discontinued during metronidazole infusion. DO NOT USE EQUIPMENT CONTAINING ALUMINUM (e.g., NEEDLES, CANNULAE) THAT WOULD COME IN CONTACT WITH THE DRUG SOLUTION.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
How Supplied
Metronidazole Injection, USP is sterile and is supplied in 100 mL single dose plastic containers, each containing an iso-osmotic, buffered solution of 500 mg metronidazole as follows:
NDC 0069-2390-01 500 mg/100 mL
Four groups of 6 bags each are placed in a carton, separated by a divider. Two cartons are then packed into a shipper. Store at 20° - 25°C (68° - 77°F) (see USP controlled room temperature). Protect from light during storage. Avoid excessive heat. Protect from freezing. Do not remove unit from overwrap until ready for use. The overwrap is a moisture barrier. The inner bag maintains the sterility of the product. After removing overwrap, check for minute leaks by squeezing the inner bag firmly. If leaks are found, discard solution, as sterility may be impaired.
Directions for Use of Plastic Container
Metronidazole Injection, USP is a ready-to-use iso-osmotic solution.No dilution or buffering is required. Do not refrigerate. Each container of Metronidazole Injection, USP contains 14 mEq of sodium.
Warning: Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is completed.
To open
Tear overwrap at the top and remove solution container. Some opacity of the plastic due to moisture absorption during the sterilization process may be observed. This is normal and does not affect the solution quality or safety. The opacity will diminish gradually. Check for leaks. Do not add supplementary medication.
Preparation for Administration
- Suspend container from eyelet support.
- Remove plastic protector from outlet port at bottom of container.
- Attach administration set. Refer to complete directions accompanying set.
References
- M11-A5-Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; approved Standard-Fifth Edition, National Committee for Clinical Laboratory Standards; and Sutter, et al.: Collaborative Evaluation of a Proposed Reference Dilution Method of Susceptibility Testing of Anaerobic Bacteria, Antimicrob. Agents Chemother. 16:495-502 (Oct.) 1979; and Tally, et al.: In Vitro Activity of Thienamycin, Antimicrob. Agents Chemother. 14:436-438 (Sept.) 1978.
- Ralph, E.D. and Kirby, W.M.M.: Bioassay of Metronidazole with Either Anaerobic and Aerobic Incubation, J. Infect. Dis. 132:587-591 (Nov.) 1975; or Gulaid, et al.: Determination of Metronidazole and its Major Metabolites in Biological Fluids by High Pressure Liquid Chromatography. BR. J. Clin. Pharmacol. 6:430-432, 1978.
Pfizer Injectables
Distributed by
Pfizer Labs
Division of Pfizer Inc,
NY, NY 10017
1400002852
Made in India
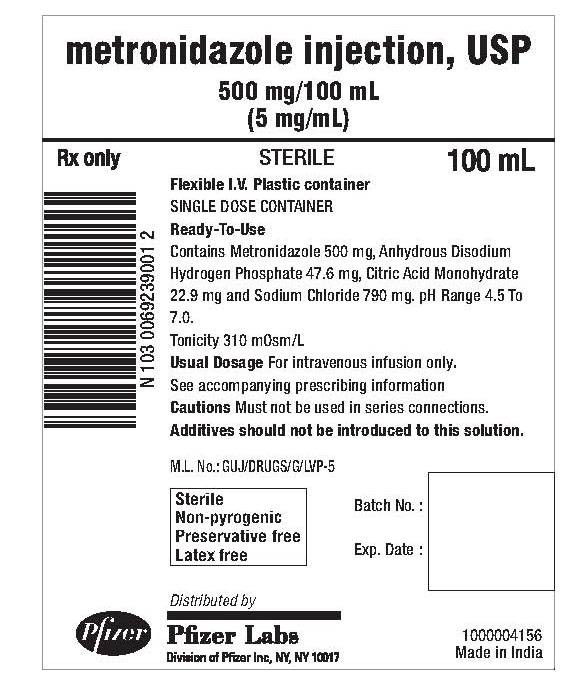
Metronidazole Injection, USP Container Label
metronidazole Injection, USP
500 mg/100 mL
(5 mg/mL)
Rx Only Sterile 100 mL
Flexible I.V. Plastic container
SINGLE DOSE CONTAINER
Ready-To-Use
Contains Metronidazole 500 mg, Anhydrous Disodiurn Hydrogen Phosphate 47.6 mg, Citric Acid Monohydrate 22.9 mg and Sodium Chloride 790 mg. pH Range 4.5 To 7.0.
Tonicity 310 mOsm/L
Usual Dosage For intravenous infusion only.
See accompanying prescribing information
Cautions Must not be used in series connections.
Additives should not be introduced to this solution.
M.L. No.: GUJ/DRUGS/G/LVP-5
Sterile
Non-pyrogenic
Preservative free
Latex free
Distributed by:
Pfizer Labs
Division of Pfizer Inc,
NY, NY 10017
Batch No.:
Exp. Date:
1000004156
Made in India
Metronidazole Injection, USP Casepack Label
NDC 0069-2390-01
2427
24 x 100 mL Bags
metronidazole Injection, USP
500 mg/100 mL
(5 mg/mL)
Rx Only
STORE AT 20° - 25°c (68° - 77°F) [SEE USP CONTROLLED ROOM TEMPERATURE]. PROTECT FROM LIGHT DURING STORAGE. AVOID EXCESSIVE HEAT. PROTECT FROM FREEZING.
Distributed by:
Pfizer Labs
Division of Pfizer Inc,
NY, NY 10017
Batch No.:
Exp. Date:
M.L. No.: GUJ/DRUGS/G/LVP-5
1000004157
Made in India

MetronidazoleMetronidazole INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||