Minizide
MINIZIDE CAPSULES(prazosin hydrochloride/polythiazide)
FULL PRESCRIBING INFORMATION: CONTENTS*
- MINIZIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- MINIZIDE INDICATIONS AND USAGE
- MINIZIDE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- MINIZIDE ADVERSE REACTIONS
- OVERDOSAGE
- MINIZIDE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
FULL PRESCRIBING INFORMATION
FOR ORAL ADMINISTRATION
This fixed combination drug is not indicated for initial therapy of hypertension. Hypertension requires therapy titrated to the individual patient. If the fixed combination represents the dose so determined, its use may be more convenient in patient management. The treatment of hypertension is not static, but must be re-evaluated as conditions in each patient warrant.
MINIZIDE DESCRIPTION
MINIZIDE® is a combination of MINIPRESS® (prazosin hydrochloride) plus RENESE® (polythiazide).
MINIPRESS (prazosin hydrochloride), a quinazoline derivative, is the first of that chemical class of antihypertensives. It is the hydrochloride salt of 1-(4-amino-6,7-dimethoxy-2-quinazolinyl)-4-(2-furoyl) piperazine and its structural formula is:
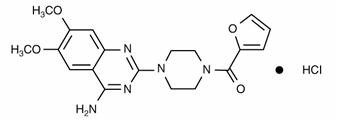
It is a white, crystalline substance, slightly soluble in water and isotonic saline, and has a molecular weight of 419.87. Each 1 mg capsule of MINIPRESS (prazosin hydrochloride) contains drug equivalent to 1 mg free base.
RENESE (polythiazide) is an orally effective, non-mercurial diuretic, saluretic, and antihypertensive agent.
It is designated chemically as 2H-1,2,4-Benzothiadiazine-7-sulfonamide, 6-chloro-3,4-dihydro-2-methyl-3-[[(2,2,2-trifluoroethyl)thio]methyl]-,1,1-dioxide, and has the following structural formula:
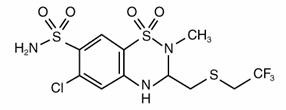
It is a white, crystalline substance insoluble in water, but readily soluble in alkaline solution.
Inert ingredients in the formulations are: hard gelatin capsules (which may contain Blue 1, Green 3, Red 3 and other inert ingredients); magnesium stearate; sodium lauryl sulfate; starch; sucrose.
CLINICAL PHARMACOLOGY
MINIZIDE (prazosin hydrochloride/polythiazide)
MINIZIDE produces a more pronounced antihypertensive response than occurs after either prazosin hydrochloride or polythiazide alone in equivalent doses.
MINIPRESS (prazosin hydrochloride)
The exact mechanism of the hypotensive action of prazosin is unknown. Prazosin causes a decrease in total peripheral resistance and was originally thought to have a direct relaxant action on vascular smooth muscle. Recent animal studies, however, have suggested that the vasodilator effect of prazosin is also related to blockade of postsynaptic alpha-adrenoceptors. The results of dog forelimb experiments demonstrate that the peripheral vasodilator effect of prazosin is confined mainly to the level of the resistance vessels (arterioles). Unlike conventional alpha-blockers, the antihypertensive action of prazosin is usually not accompanied by a reflex tachycardia. Tolerance has not been observed to develop in long term therapy.
Hemodynamic studies have been carried out in man following acute single dose administration and during the course of long term maintenance therapy. The results confirm that the therapeutic effect is a fall in blood pressure unaccompanied by a clinically significant change in cardiac output, heart rate, renal blood flow, and glomerular filtration rate. There is no measurable negative chronotropic effect.
In clinical studies to date, MINIPRESS has not increased plasma renin activity.
In man, blood pressure is lowered in both the supine and standing positions. This effect is most pronounced on the diastolic blood pressure.
Following oral administration, human plasma concentrations reach a peak at about three hours with a plasma half-life of two to three hours. The drug is highly bound to plasma protein. Bioavailability studies have demonstrated that the total absorption relative to the drug in a 20% alcoholic solution is 90%, resulting in peak levels approximately 65% of that of the drug in solution. Animal studies indicate that MINIPRESS is extensively metabolized, primarily by demethylation and conjugation, and excreted mainly via bile and feces. Less extensive human studies suggest similar metabolism and excretion in man.
MINIPRESS has been administered without any adverse drug interaction in limited clinical experience to date with the following: (1) cardiac glycosides—digitalis and digoxin; (2) hypoglycemics—insulin, chlorpropamide, phenformin, tolazamide, and tolbutamide; (3) tranquilizers and sedatives—chlordiazepoxide, diazepam, and phenobarbital; (4) antigout—allopurinol, colchicine, and probenecid; (5) antiarrhythmics—procainamide, propranolol (see WARNINGS however), and quinidine; and (6) analgesics, antipyretics and anti-inflammatories—propoxyphene, aspirin, indomethacin, and phenylbutazone.
RENESE (polythiazide)
RENESE is a member of the benzothiadiazine (thiazide) family of diuretic/antihypertensive agents. Its mechanism of action results in an interference with the renal tubular mechanism of electrolyte reabsorption. At maximal therapeutic dosage all thiazides are approximately equal in their diuretic potency. The mechanism whereby thiazides function in the control of hypertension is unknown. Renese is well absorbed, giving peak human plasma concentrations about 5 hours after oral administration. Drug is removed slowly thereafter with a plasma elimination half-life of approximately 27 hours. One fifth of the drug is recovered unchanged in human urine; the remainder is cleared via feces and as metabolites. Animal studies indicate metabolism occurs by rupture of the thiadiazine ring and loss of the side chain.
MINIZIDE INDICATIONS AND USAGE
MINIZIDE is indicated in the treatment of hypertension. (See box warning.)
MINIZIDE CONTRAINDICATIONS
RENESE (polythiazide) is contraindicated in patients with anuria, and in patients known to be sensitive to thiazides or to other sulfonamide derivatives.
WARNINGS
MINIPRESS (prazosin hydrochloride)
MINIPRESS may cause syncope with sudden loss of consciousness. In most cases this is believed to be due to an excessive postural hypotensive effect, although occasionally the syncopal episode has been preceded by a bout of severe tachycardia with heart rates of 120–160 beats per minute. Syncopal episodes have usually occurred within 30 to 90 minutes of the initial dose of the drug; occasionally they have been reported in association with rapid dosage increases or the introduction of another antihypertensive drug into the regimen of a patient taking high doses of MINIPRESS. The incidence of syncopal episodes is approximately 1% in patients given an initial dose of 2 mg or greater. Clinical trials conducted during the investigational phase of this drug suggest that syncopal episodes can be minimized by limiting the initial dose of the drug to 1 mg, by subsequently increasing the dosage slowly, and by introducing any additional antihypertensive drugs into the patient's regimen with caution (see DOSAGE AND ADMINISTRATION). Hypotension may develop in patients given MINIPRESS who are also receiving a beta-blocker such as propranolol.
If syncope occurs, the patient should be placed in the recumbent position and treated supportively as necessary. This adverse effect is self-limiting and in most cases does not recur after the initial period of therapy or during subsequent dose titration.
Patients should always be started on the 1 mg capsules of MINIPRESS (prazosin hydrochloride). The 2 and 5 mg capsules are not indicated for initial therapy.
More common than loss of consciousness are the symptoms often associated with lowering of the blood pressure, namely, dizziness and lightheadedness. The patient should be cautioned about these possible adverse effects and advised what measures to take should they develop. The patient should also be cautioned to avoid situations where injury could result should syncope occur during the initiation of MINIPRESS therapy.
RENESE (polythiazide)
RENESE should be used with caution in severe renal disease. In patients with renal disease, thiazides may precipitate azotemia. Cumulative effects of the drug may develop in patients with impaired renal function.
Thiazides should be used with caution in patients with impaired hepatic function or progressive liver disease, since minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
Sensitivity reactions may occur in patients with a history of allergy or bronchial asthma.
The possibility of exacerbation or activation of systemic lupus erythematosus has been reported.
Thiazides may be additive or potentiative of the action of other antihypertensive drugs.
Potentiation occurs with ganglionic or peripheral adrenergic blocking drugs.
Periodic determinations of serum electrolytes to detect possible electrolyte imbalance should be performed at appropriate intervals.
All patients receiving thiazide therapy should be observed for clinical signs of fluid or electrolyte imbalance, namely, hyponatremia, hypochloremic alkalosis, and hypokalemia. Serum and urine electrolyte determinations are particularly important when the patient is vomiting excessively or receiving parenteral fluids. Medications such as digitalis may also influence serum electrolytes. Warning signs, irrespective of cause, are: dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, and gastrointestinal disturbances such as nausea and vomiting.
Hypokalemia may develop with thiazides as with any potent diuretic, especially with brisk diuresis, when severe cirrhosis is present, or during concomitant use of corticosteroids or ACTH.
Interference with adequate oral electrolyte intake will also contribute to hypokalemia. Digitalis therapy may exaggerate the metabolic effects of hypokalemia, especially with reference to myocardial activity.
Any chloride deficit is generally mild and usually does not require specific treatment except under extraordinary circumstances (as in hepatic or renal disease). Dilutional hyponatremia may occur in edematous patients in hot weather; appropriate therapy is water restriction rather than administration of salt, except in rare instances when the hyponatremia is life-threatening. In actual salt depletion, appropriate replacement is the therapy of choice.
Hyperuricemia may occur or frank gout may be precipitated in certain patients receiving thiazide therapy.
Insulin requirements in diabetic patients may be either increased, decreased, or unchanged. Latent diabetes mellitus may become manifest during thiazide administration.
Thiazide drugs may increase responsiveness to tubocurarine.
The antihypertensive effects of the drug may be enhanced in the post-sympathectomy patient.
Thiazides may decrease arterial responsiveness to norepinephrine. This diminution is not sufficient to preclude effectiveness of the pressor agent for therapeutic use.
If progressive renal impairment becomes evident, as indicated by a rising nonprotein nitrogen or blood urea nitrogen, a careful reappraisal of therapy is necessary with consideration given to withholding or discontinuing diuretic therapy.
Thiazides may decrease serum protein-bound iodine levels without signs of thyroid disturbance.
PRECAUTIONS
Drug/Laboratory Test Interactions
In a study on five patients given from 12 to 24 mg of prazosin per day for 10 to 14 days, there was an average increase of 42% in the urinary metabolite of norepinephrine and an average increase in urinary VMA of 17%. Therefore, false positive results may occur in screening tests for pheochromocytoma in patients who are being treated with prazosin. If an elevated VMA is found, prazosin should be discontinued and the patient retested after a month.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenic or mutagenic studies have been conducted with MINIZIDE. However, no carcinogenic potential was demonstrated in 18 month studies in rats with either MINIPRESS or RENESE at dose levels more than 100 times the usual maximum human doses. MINIPRESS was not mutagenic in in vivo genetic toxicology studies.
MINIZIDE produced no impairment of fertility in male or female rats at 50 and 25 mg/kg/day of MINIPRESS and RENESE respectively. In chronic studies (one year or more) of MINIPRESS in rats and dogs, testicular changes consisting of atrophy and necrosis occurred at 25 mg/kg/day (60 times the usual maximum recommended human dose). No testicular changes were seen in rats or dogs at 10 mg/kg/day (24 times the usual maximum recommended human dose). In view of the testicular changes observed in animals, 105 patients on long term MINIPRESS therapy were monitored for 17-ketosteroid excretion and no changes indicating a drug effect were observed. In addition, 27 males on MINIPRESS alone for up to 51 months did not have changes in sperm morphology suggestive of drug effect.
Use in Pregnancy
Pregnancy Category C. MINIZIDE was not teratogenic in either rats or rabbits when administered in oral doses more than 100 times the usual maximum human dose. Studies in rats indicated that the combination of RENESE (40 times the usual maximum recommended human dose) and MINIPRESS (8 times the usual maximum recommended human dose) caused a greater number of stillbirths, a more prolonged gestation, and a decreased survival of pups to weaning than that caused by MINIPRESS alone. There are no adequate and well controlled studies in pregnant women. Therefore, MINIZIDE should be used in pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is not known whether MINIPRESS or RENESE is excreted in human milk. Thiazides appear in breast milk. Thus, if use of the drug is deemed essential the patient should stop nursing.
Pediatric Use
Safety and effectiveness in children has not been established.
MINIZIDE ADVERSE REACTIONS
MINIPRESS (prazosin hydrochloride)
The most common reactions associated with MINIPRESS therapy are: dizziness 10.3%, headache 7.8%, drowsiness 7.6%, lack of energy 6.9%, weakness 6.5%, palpitations 5.3%, and nausea 4.9%. In most instances side effects have disappeared with continued therapy or have been tolerated with no decrease in dose of drug.
The following reactions have been associated with MINIPRESS, some of them rarely. (In some instances exact causal relationships have not been established.)
Gastrointestinal: vomiting, diarrhea, constipation, abdominal discomfort and/or pain, liver function abnormalities, pancreatitis.
Cardiovascular: edema, dyspnea, syncope, tachycardia.
Central Nervous System: nervousness, vertigo, depression, paresthesia, hallucinations.
Dermatologic: rash, pruritus, alopecia, lichen planus.
Genitourinary: urinary frequency, incontinence, impotence, priapism.
EENT: blurred vision, reddened sclera, epistaxis, tinnitus, dry mouth, nasal congestion.
Other: diaphoresis, fever.
Single reports of pigmentary mottling and serous retinopathy, and a few reports of cataract development or disappearance have been reported. In these instances, the exact causal relationship has not been established because the baseline observations were frequently inadequate.
In more specific slit-lamp and funduscopic studies, which included adequate baseline examinations, no drug-related abnormal ophthalmological findings have been reported.
Literature reports exist associating MINIPRESS therapy with a worsening of pre-existing narcolepsy. A causal relationship is uncertain in these cases.
RENESE (polythiazide)
Gastrointestinal: anorexia, gastric irritation, nausea, vomiting, cramping, diarrhea, constipation, jaundice (intrahepatic cholestatic jaundice), pancreatitis.
Central Nervous System: dizziness, vertigo, paresthesia, headache, xanthopsia.
Hematologic: leukopenia, agranulocytosis, thrombocytopenia, aplastic anemia.
Dermatologic: purpura, photosensitivity, rash, urticaria, necrotizing angiitis, (vasculitis) (cutaneous vasculitis).
Cardiovascular: Orthostatic hypotension may occur and be aggravated by alcohol, barbiturates, or narcotics.
Other: hyperglycemia, glycosuria, hyperuricemia, muscle spasm, weakness, restlessness.
OVERDOSAGE
MINIPRESS (prazosin hydrochloride)
Accidental ingestion of at least 50 mg of MINIPRESS in a two year old child resulted in profound drowsiness and depressed reflexes. No decrease in blood pressure was noted. Recovery was uneventful.
Should overdosage lead to hypotension, support of the cardiovascular system is of first importance. Restoration of blood pressure and normalization of heart rate may be accomplished by keeping the patient in the supine position. If this measure is inadequate, shock should first be treated with volume expanders. If necessary, vasopressors should then be used. Renal function should be monitored and supported as needed. Laboratory data indicate that MINIPRESS is not dialyzable because it is protein bound.
RENESE (polythiazide)
Should overdosage with RENESE occur, electrolyte balance and adequate hydration should be maintained. Gastric lavage is recommended, followed by supportive treatment. Where necessary, this may include intravenous dextrose and saline with potassium and other electrolyte therapy, administered with caution as indicated by laboratory testing at appropriate intervals.
MINIZIDE DOSAGE AND ADMINISTRATION
MINIZIDE (prazosin hydrochloride/polythiazide)
Dosage: as determined by individual titration of MINIPRESS (prazosin hydrochloride) and RENESE (polythiazide). (See box warning.)
Usual MINIZIDE dosage is one capsule two or three times daily, the strength depending upon individual requirement following titration.
The following is a general guide to the administration of the individual components of MINIZIDE:
MINIPRESS (prazosin hydrochloride)
Initial Dose
1 mg two or three times a day. (See WARNINGS.)
Maintenance Dose
Dosage may be slowly increased to a total daily dose of 20 mg given in divided doses. The therapeutic dosages most commonly employed have ranged from 6 mg to 15 mg daily given in divided doses. Doses higher than 20 mg usually do not increase efficacy, however a few patients may benefit from further increases up to a daily dose of 40 mg given in divided doses. After initial titration some patients can be maintained adequately on a twice daily dosage regimen.
Use With Other Drugs
When adding a diuretic or other antihypertensive agent, the dose of MINIPRESS should be reduced to 1 mg or 2 mg three times a day and retitration then carried out.
RENESE (polythiazide)
The usual dose of RENESE for antihypertensive therapy is 2 to 4 mg daily.
HOW SUPPLIED
| STRENGTH | COMPONENTS | COLOR | CAPSULE CODE | PKG. SIZE |
|---|---|---|---|---|
MINIZIDE 1 | 1 mg prazosin + 0.5 mg polythiazide (NDC 0663-4300-66) (NDC 0069-4300-66) | Blue- Green | 430 | 100's |
MINIZIDE 2 | 2 mg prazosin + 0.5 mg polythiazide (NDC 0663-4320-66) (NDC 0069-4320-66) | Blue- Green/ Pink | 432 | 100's |
MINIZIDE 5 | 5 mg prazosin + 0.5 mg polythiazide (NDC 0663-4360-66) (NDC 0069-4360-66) | Blue- Green/ Blue | 436 | 100's |
Rx Only

LAB-0213-2.0
Revised August 2006
Minizideprazosin hydrochloride and polythiazide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Minizideprazosin hydrochloride and polythiazide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Minizideprazosin hydrochloride and polythiazide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||