Mirapex
Boehringer Ingelheim Pharmaceuticals, Inc.
Boehringer Ingelheim Pharmaceuticals, Inc.
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use MIRAPEX ER safely and effectively. See full prescribing information for MIRAPEX ER. MIRAPEX ER® (pramipexole dihydrochloride) extended-release tabletsInitial U.S. Approval: 1997RECENT MAJOR CHANGES Dosage and Administration Dosing for Parkinson’s Disease (2.2) 5/2014 INDICATIONS AND USAGEMIRAPEX ER is a non-ergot dopamine agonist indicated for the treatment of the signs and symptoms of Parkinson’s disease (1) DOSAGE AND ADMINISTRATION MIRAPEX ER tablets are taken once daily, with or without food. (2.1) Tablets must be swallowed whole and must not be chewed, crushed, or divided. (2.1) Starting dose is 0.375 mg given once daily. (2.2) Dose may be increased gradually, not more frequently than every 5 to 7 days, first to 0.75 mg per day and then by 0.75 mg increments up to a maximum recommended dose of 4.5 mg per day. Assess therapeutic response and tolerability at a minimal interval of 5 days or longer after each dose increment. (2.2) Patients may be switched overnight from immediate-release pramipexole tablets to MIRAPEX ER tablets at the same daily dose. Dose adjustment may be needed in some patients. (2.3) MIRAPEX ER tablets should be discontinued gradually. (2.2) DOSAGE FORMS AND STRENGTHSExtended-release tablets: 0.375 mg, 0.75 mg, 1.5 mg, 2.25 mg, 3 mg, 3.75 mg, and 4.5 mg (3) CONTRAINDICATIONSNone (4) WARNINGS AND PRECAUTIONS Falling asleep during activities of daily living: Sudden onset of sleep may occur without warning. Advise patients to report symptoms to the prescriber. (5.1) Symptomatic orthostatic hypotension: Monitor closely especially during dose escalation. (5.2) Impulse control/Compulsive behaviors: Patients may experience compulsive behaviors and other intense urges. (5.3) Hallucinations: May occur. Risk increases with age. (5.4) Dyskinesia: May be caused or exacerbated by MIRAPEX ER. (5.5) Renal impairment: No data available in patients with moderate or severe renal impairment. (5.6) Events reported with dopaminergic therapy: Include withdrawal-emergent hyperpyrexia and confusion, fibrotic complications, and melanoma. (5.9) Side Effects Most common adverse events (incidence ≥5% and greater than placebo) in early Parkinson’s disease without levodopa were somnolence, nausea, constipation, dizziness, fatigue, hallucinations, dry mouth, muscle spasms, and peripheral edema. (6.1) Most common adverse events (incidence ≥5% and greater than placebo) in advanced Parkinson's disease concomitantly treated with levodopa were dyskinesia, nausea, constipation, hallucinations, headache, and anorexia. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Boehringer Ingelheim Pharmaceuticals, Inc. at (800) 542-6257 or (800) 459-9906 TTY or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .DRUG INTERACTIONS Dopamine antagonists: May diminish the effectiveness of pramipexole (7.1) USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, may cause fetal harm (8.1)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 INDICATIONS AND USAGE
- 2 MIRAPEX DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 MIRAPEX CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 MIRAPEX ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 MIRAPEX DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
MIRAPEX ER® tablets are indicated for the treatment of the signs and symptoms of idiopathic Parkinson's disease.
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Considerations
MIRAPEX ER tablets are taken orally once daily, with or without food.
MIRAPEX ER tablets must be swallowed whole and must not be chewed, crushed, or divided.
If a significant interruption in therapy with MIRAPEX ER tablets has occurred, re-titration of therapy may be warranted.
2.2 Dosing for Parkinson's Disease
The starting dose is 0.375 mg given once per day. Based on efficacy and tolerability, dosages may be increased gradually, not more frequently than every 5 to 7 days, first to 0.75 mg per day and then by 0.75 mg increments up to a maximum recommended dose of 4.5 mg per day.
In clinical trials, dosage was initiated at 0.375 mg/day and gradually titrated based on individual therapeutic response and tolerability. Doses greater than 4.5 mg/day have not been studied in clinical trials. Patients should be assessed for therapeutic response and tolerability at a minimal interval of 5 days or longer after each dose increment [ see Clinical Studies (14) ].
Due to the flexible dose design used in clinical trials, specific dose-response information could not be determined [ see Clinical Studies (14) ].
MIRAPEX ER tablets may be tapered off at a rate of 0.75 mg per day until the daily dose has been reduced to 0.75 mg. Thereafter, the dose may be reduced by 0.375 mg per day.
Dosing in Patients with
Renal Impairment
The elimination of
pramipexole is dependent on renal function [
see
Clinical Pharmacology (12.3)
]. Patients with mild renal impairment (a creatinine clearance
above 50 mL/min) require no reduction in daily dose.
In patients with moderate renal impairment (creatinine clearance between 30 and 50 mL/min), MIRAPEX ER tablets should initially be taken every other day. Caution should be exercised and careful assessment of therapeutic response and tolerability should be made before increasing to daily dosing after one week, and before any additional titration in 0.375 mg increments up to 2.25 mg per day. Dose adjustment should occur no more frequently than at weekly intervals.
MIRAPEX ER tablets have not been studied in patients with severe renal impairment (creatinine clearance <30 mL/min) or patients on hemodialysis, and are not recommended in these patients.
2.3 Switching from Immediate-Release Pramipexole Tablets to MIRAPEX ER
Patients may be switched overnight from immediate-release pramipexole tablets to MIRAPEX ER tablets at the same daily dose. When switching between immediate-release pramipexole tablets and MIRAPEX ER tablets, patients should be monitored to determine if dosage adjustment is necessary.
3 DOSAGE FORMS AND STRENGTHS
0.375 mg white
to off-white, round, bevel-edged, extended-release tablets debossed
with "ER" on one side and "0.375" on the other side
0.75
mg white to off-white, round, bevel-edged, extended-release tablets
debossed with "ER" on one side and "0.75" on the other side
1.5 mg white to off-white, oval, extended-release tablets
debossed with "ER" on one side and "1.5" on the other side
2.25 mg white to off-white, oval, extended-release tablets
debossed with "ER" on one side and "2.25" on the other side
3 mg white to off-white, oval, extended-release tablets debossed
with "ER" on one side and "3.0" on the other side
3.75
mg white to off-white, oval, extended-release tablets debossed with
"ER" on one side and "3.75" on the other side
4.5
mg white to off-white, oval, extended-release tablets debossed with
"ER" on one side and "4.5" on the other side
4 CONTRAINDICATIONS
None.
5 WARNINGS AND PRECAUTIONS
5.1 Falling Asleep During Activities of Daily Living
Patients treated with pramipexole have reported falling asleep while engaged in activities of daily living, including the operation of motor vehicles, which sometimes resulted in accidents. Although many of these patients reported somnolence while on pramipexole tablets, some perceived that they had no warning signs such as excessive drowsiness, and believed that they were alert immediately prior to the event. Some of these events had been reported as late as one year after the initiation of treatment. In placebo-controlled clinical trials in Parkinson's disease, the sudden onset of sleep or sleep attacks were reported in 8 of 387 (2%) patients treated with MIRAPEX ER tablets compared to 2 of 281 (1%) patients on placebo.
In early Parkinson’s disease, somnolence was reported in 36% of 223 patients treated with MIRAPEX ER, median dose 3.0 mg/day, compared to 15% of 103 patients on placebo. In advanced Parkinson’s disease, somnolence was reported in 15% of 164 patients treated with MIRAPEX ER tablets, median dose 3 mg/day, compared to 16% of 178 patients on placebo. Many clinical experts believe that falling asleep while engaged in activities of daily living always occurs in a setting of preexisting somnolence, although patients may not give such a history. For this reason, prescribers should continually reassess patients for drowsiness or sleepiness, especially since some of the events occur well after the start of treatment. Prescribers should also be aware that patients may not acknowledge drowsiness or sleepiness until directly questioned about drowsiness or sleepiness during specific activities.
Before initiating treatment with MIRAPEX ER tablets, advise patients of the potential to develop drowsiness, and specifically ask about factors that may increase the risk such as the use of concomitant sedating medications or alcohol, the presence of sleep disorders, and concomitant medications that increase pramipexole plasma levels (e.g., cimetidine) [ see Clinical Pharmacology (12.3) ]. If a patient develops significant daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., conversations, eating, etc.), MIRAPEX ER tablets should ordinarily be discontinued. If a decision is made to continue MIRAPEX ER tablets, advise patients not to drive and to avoid other potentially dangerous activities. While dose reduction reduces the degree of somnolence, there is insufficient information to establish that dose reduction will eliminate episodes of falling asleep while engaged in activities of daily living.
5.2 Symptomatic Orthostatic Hypotension
Dopamine agonists, in clinical studies and clinical experience, appear to impair the systemic regulation of blood pressure, with resulting orthostatic hypotension, especially during dose escalation. Parkinson's disease patients, in addition, appear to have an impaired capacity to respond to an orthostatic challenge. For these reasons, Parkinson's disease patients being treated with dopaminergic agonists, including MIRAPEX ER, ordinarily require careful monitoring for signs and symptoms of orthostatic hypotension, especially during dose escalation, and should be informed of this risk [ see Patient Counseling Information (17.5) ]. In placebo-controlled clinical trials in Parkinson’s disease, symptomatic orthostatic hypotension was reported in 10 of 387 (3%) patients treated with MIRAPEX ER tablets compared to 3 of 281 (1%) patients on placebo. One patient of 387 on MIRAPEX ER tablets discontinued treatment due to hypotension.
5.3 Impulse Control/Compulsive Behaviors
Case reports and the results of cross-sectional studies suggest that patients can experience intense urges to gamble, increased sexual urges, intense urges to spend money, binge eating, and/or other intense urges, and the inability to control these urges while taking one or more of the medications, including MIRAPEX ER, that increase central dopaminergic tone and that are generally used for the treatment of Parkinson’s disease. In some cases, although not all, these urges were reported to have stopped when the dose was reduced or the medication was discontinued. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to specifically ask patients or their caregivers about the development of new or increased gambling urges, sexual urges, uncontrolled spending or other urges while being treated with MIRAPEX ER. Physicians should consider dose reduction or stopping the medication if a patient develops such urges while taking MIRAPEX ER [ see Patient Counseling Information (17.3) ].
A total of 1056 patients with Parkinson’s disease who participated in two MIRAPEX ER placebo-controlled studies of up to 33 weeks duration were specifically asked at each visit about the occurrence of these symptoms. A total of 14 of 387 (4%) treated with MIRAPEX ER tablets, 12 of 388 (3%) treated with immediate-release pramipexole tablets, and 4 of 281 (1%) treated with placebo reported compulsive behaviors, including pathological gambling, hypersexuality, and/or compulsive buying.
5.4 Hallucinations
In placebo-controlled clinical trials in Parkinson's disease, hallucinations (visual or auditory or mixed) were reported in 25 of 387 (6%) patients treated with MIRAPEX ER tablets compared to 5 of 281 (2%) patients receiving placebo. Hallucinations led to discontinuation of treatment in 5 of 387 (1%) patients on MIRAPEX ER tablets.
Age appears to increase the risk of hallucinations attributable to pramipexole. In placebo-controlled clinical trials in Parkinson’s disease, hallucinations were reported in 15 of 162 (9%) patients ≥65 years of age taking MIRAPEX ER tablets compared to 10 of 225 (4%) patients <65 years of age taking MIRAPEX ER tablets.
5.5 Dyskinesia
MIRAPEX ER tablets may potentiate the dopaminergic side effects of levodopa and may cause or exacerbate preexisting dyskinesia.
5.6 Renal Impairment
The elimination of pramipexole is dependent on renal function [ see Clinical Pharmacology (12.3) ]. Patients with mild renal impairment (a creatinine clearance above 50 mL/min) require no reduction in daily dose. MIRAPEX ER tablets have not been studied in patients with moderate to severe renal impairment (creatinine clearance <50 mL/min) or on hemodialysis [ see Dosage and Administration (2.2), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3) ].
5.7 Rhabdomyolysis
In the clinical development program for immediate-release pramipexole tablets, a single case of rhabdomyolysis occurred in a 49-year-old male with advanced Parkinson's disease. The patient was hospitalized with an elevated CPK (10,631 IU/L). The symptoms resolved with discontinuation of the medication.
Advise patients to contact a physician if they experience any unexplained muscle pain, tenderness, or weakness, as these may be symptoms of rhabdomyolysis.
5.8 Retinal Pathology
A two-year open-label, randomized, parallel-group safety study of retinal deterioration and vision compared immediate-release pramipexole tablets and immediate-release ropinirole. Two hundred thirty four Parkinson’s disease patients (115 on pramipexole, mean dose 3.0 mg/day and 119 on ropinirole, mean dose 9.5 mg/day) were evaluated using a panel of clinical ophthalmological assessments. Of 234 patients who were evaluable, 196 had been treated for two years and 29 were judged to have developed clinical abnormalities that were considered meaningful (19 patients in each treatment arm had received treatment for less than two years). There was no statistical difference in retinal deterioration between the treatment arms; however, the study was only capable of detecting a very large difference between treatments. In addition, because the study did not include an untreated comparison group (placebo treated), it is unknown whether the findings reported in patients treated with either drug are greater than the background rate in an aging population.
Pathologic changes (degeneration and loss of photoreceptor cells) were observed in the retina of albino rats in a 2-year carcinogenicity study. While retinal degeneration was not diagnosed in pigmented rats treated for 2 years, a thinning in the outer nuclear layer of the retina was slightly greater in rats given drug compared with controls. Evaluation of the retinas of albino mice, monkeys, and minipigs did not reveal similar changes. The potential significance of this effect for humans has not been established, but cannot be disregarded because disruption of a mechanism that is universally present in vertebrates (i.e., disk shedding) may be involved [ see Nonclinical Toxicology (13.2) ].
5.9 Events Reported with Dopaminergic Therapy
Although the events enumerated below may not have been reported with the use of pramipexole in its development program, they are associated with the use of other dopaminergic drugs. The expected incidence of these events, however, is so low that even if pramipexole caused these events at rates similar to those attributable to other dopaminergic therapies, it would be unlikely that even a single case would have occurred in a cohort of the size exposed to pramipexole in studies to date.
Although not reported with pramipexole in the clinical development program, a symptom complex resembling the neuroleptic malignant syndrome (characterized by elevated temperature, muscular rigidity, altered consciousness, and autonomic instability), with no other obvious etiology, has been reported in association with rapid dose reduction, withdrawal of, or changes in anti-Parkinsonian therapy.
Cases of retroperitoneal fibrosis, pulmonary infiltrates, pleural effusion, pleural thickening, pericarditis, and cardiac valvulopathy have been reported in patients treated with ergot-derived dopaminergic agents. While these complications may resolve when the drug is discontinued, complete resolution does not always occur.
Although these adverse events are believed to be related to the ergoline structure of these compounds, whether other, non-ergot derived dopamine agonists can cause them is unknown.
Cases of possible fibrotic complications, including peritoneal fibrosis, pleural fibrosis, and pulmonary fibrosis have been reported in the postmarketing experience with immediate-release pramipexole tablets. While the evidence is not sufficient to establish a causal relationship between pramipexole and these fibrotic complications, a contribution of pramipexole cannot be completely ruled out.
Epidemiologic studies have shown that patients with Parkinson’s disease have a higher risk (2- to approximately 6-fold higher) of developing melanoma than the general population. Whether the observed increased risk was due to Parkinson’s disease or other factors, such as drugs used to treat Parkinson’s disease, is unclear.
For the reasons stated above, patients and providers are advised to monitor for melanomas frequently and on a regular basis when using MIRAPEX ER tablets for any indication. Ideally, periodic skin examinations should be performed by appropriately qualified individuals (e.g., dermatologists).
6 ADVERSE REACTIONS
The following are discussed in greater detail in other sections of the labeling:
- Falling Asleep During Activities of Daily Living [ see Warnings and Precautions (5.1) ]
- Symptomatic Orthostatic Hypotension [ see Warnings and Precautions (5.2) ]
- Impulse Control/Compulsive Behaviors [ see Warnings and Precautions (5.3) ]
- Hallucinations [ see Warnings and Precautions (5.4) ]
- Dyskinesia [ see Warnings and Precautions (5.5) ]
- Renal Impairment [ see Warnings and Precautions (5.6) ]
- Rhabdomyolysis [ see Warnings and Precautions (5.7) ]
- Retinal Pathology [ see Warnings and Precautions (5.8) ]
- Events Reported with Dopaminergic Therapy [ see Warnings and Precautions (5.9) ]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse event rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug (or of another development program of a different formulation of the same drug) and may not reflect the rates observed in practice.
During the premarketing development of MIRAPEX ER tablets, patients with early Parkinson's disease were treated with MIRAPEX ER tablets, placebo, or immediate-release pramipexole tablets. In addition, a randomized, double-blind, parallel group trial was conducted in 156 early Parkinson’s disease patients (Hoehn & Yahr Stages I-III) to assess overnight switching of immediate-release pramipexole tablets to MIRAPEX ER tablets. In this latter study, concomitant treatment with stable doses of levodopa, monoamine oxidase B inhibitor (MAOB-I) drugs, anticholinergics, or amantadine, individually or in combination, was allowed. In a third trial, advanced Parkinson’s disease patients received MIRAPEX ER tablets, placebo, or immediate-release pramipexole tablets as adjunctive therapy to levodopa.
Early Parkinson's Disease
The most commonly observed adverse events (≥5%
and more frequent than placebo) after 33 weeks of treatment with MIRAPEX
ER tablets in the trial of early Parkinson’s disease patients were
somnolence, nausea, constipation, dizziness, fatigue, hallucinations,
dry mouth, muscle spasms, and peripheral edema.
Twenty four of 223 (11%) patients treated with MIRAPEX ER tablets for 33 weeks discontinued treatment due to adverse events compared to 4 of 103 (4%) patients who received placebo and approximately 20 of 213 (9%) patients who received immediate-release pramipexole tablets. The adverse event most commonly causing discontinuation of treatment with MIRAPEX ER tablets was nausea (2%).
Table 1 lists adverse events that occurred with a frequency of at least 2% with MIRAPEX ER and were more frequent than with placebo during 33 weeks of treatment in a double-blind, placebo-controlled study in early Parkinson's disease. In this study, patients did not receive concomitant levodopa; however, levodopa was permitted as rescue medication. Adverse events were usually mild (38%) or moderate (41%) in intensity.
| Body System/Adverse Event | Placebo | MIRAPEX ER | Immediate-Release Pramipexole |
| (n=103) | (n=223) | (n=213) | |
| % | % | % | |
| Nervous system disorders | |||
| Somnolence | 15 | 36 | 33 |
| Dizziness | 7 | 12 | 12 |
| Tremor | 1 | 3 | 3 |
| Balance disorder | 1 | 2 | 0 |
| Gastrointestinal disorders | |||
| Nausea | 9 | 22 | 24 |
| Constipation | 2 | 14 | 12 |
| Dry mouth | 1 | 5 | 4 |
| Vomiting | 0 | 4 | 4 |
| Upper abdominal pain | 1 | 3 | 4 |
| Dyspepsia | 2 | 3 | 3 |
| Abdominal discomfort | 0 | 2 | 1 |
| General disorders and administration site conditions | |||
| Fatigue | 4 | 6 | 6 |
| Peripheral edema | 4 | 5 | 8 |
| Asthenia | 2 | 3 | 1 |
| Musculoskeletal and connective tissue disorders | |||
| Muscle spasms | 3 | 5 | 3 |
| Psychiatric disorders | |||
| Hallucinations, including visual, auditory and mixed | 1 | 5 | 6 |
| Insomnia | 3 | 4 | 4 |
| Sleep attacks or sudden onset of sleep | 1 | 3 | 6 |
| Sleep disorder | 1 | 2 | 3 |
| Depression | 0 | 2 | 0 |
| Injury, poisoning and procedural complications | |||
| Fall | 1 | 4 | 4 |
| Vascular disorders | |||
| Orthostatic hypotension | 1 | 3 | 0 |
| Ear and labyrinth disorders | |||
| Vertigo | 1 | 4 | 2 |
| Metabolism and nutrition disorders | |||
| Increased appetite | 1 | 3 | 2 |
| Respiratory, thoracic and mediastinal disorders | |||
| Cough | 1 | 3 | 3 |
Because this study used a flexible dose titration design, it was not possible to assess the effects of dose on the incidence of adverse events.
Adverse events can initially occur in either the titration or maintenance phase. Some adverse events developed in MIRAPEX ER-treated patients during the titration phase and persisted (≥7 days) into the maintenance phase (i.e., MIRAPEX ER % - placebo % = treatment difference ≥2%); persistent adverse events were somnolence, nausea, constipation, fatigue, and dry mouth.
A double-blind, randomized, parallel group trial evaluated the tolerability of an overnight switch from immediate-release pramipexole tablets to MIRAPEX ER tablets at the same daily dose in 156 early Parkinson’s disease patients with or without levodopa. One of 104 patients switched from immediate-release pramipexole tablets to MIRAPEX ER tablets discontinued due to adverse events (vertigo and nausea).
Advanced Parkinson's Disease
The most commonly observed adverse events (≥5%
and greater frequency than in placebo) during 18 weeks of treatment
with MIRAPEX ER tablets in the trial of advanced Parkinson’s disease
patients with concomitant levodopa were dyskinesia, nausea, constipation,
hallucinations, headache, and anorexia.
Eight of 164 (5%) patients treated with MIRAPEX ER tablets for 18 weeks discontinued treatment due to adverse events compared to 7 of 178 (4%) patients who received placebo and 8 of 175 (5%) patients who received immediate-release pramipexole tablets. The most common adverse events leading to discontinuation of treatment with MIRAPEX ER tablets were nausea (1%) and hallucination (1%).
Table 2 lists adverse events that occurred with a frequency of at least 2% with MIRAPEX ER and were more frequent than with placebo during 18 weeks of treatment in patients with advanced Parkinson’s disease treated with MIRAPEX ER tablets. In this study, MIRAPEX ER tablets, immediate-release pramipexole tablets, or placebo was administered to patients who were also receiving concomitant levodopa. Adverse events were usually mild (32%) or moderate (17%) in intensity.
| *18-week final analysis | |||
| Body System/Adverse Event | Placebo | MIRAPEX ER | Immediate-Release Pramipexole |
| n=178 | n=164 | n=175 | |
| % | % | % | |
| Nervous system disorders | |||
| Dyskinesia | 8 | 17 | 18 |
| Headache | 3 | 7 | 4 |
| Dizziness (postural) | 1 | 2 | 3 |
| Gastrointestinal disorders | |||
| Nausea | 10 | 11 | 11 |
| Constipation | 5 | 7 | 6 |
| Salivary hypersecretion | 0 | 2 | 0 |
| Diarrhea | 1 | 2 | 1 |
| Psychiatric disorders | |||
| Hallucinations, including visual, auditory and mixed | 2 | 9 | 7 |
| Insomnia | 2 | 4 | 4 |
| Metabolism and nutrition disorders | |||
| Anorexia | 2 | 5 | 1 |
| Musculoskeletal and connective tissue disorders | |||
| Back pain | 1 | 2 | 3 |
Because this flexible dose study used a titration design, it was not possible to assess the effects of dose on the incidence of adverse events.
Adverse events can initially occur in either the titration or maintenance phase. Some adverse events developed in MIRAPEX ER-treated patients during the titration phase and persisted (≥7 days) into the maintenance phase (i.e., MIRAPEX ER % - placebo % = treatment difference ≥2%); persistent adverse events were dyskinesia and insomnia.
Laboratory Testing
During the development of MIRAPEX ER tablets,
no systematic abnormalities on routine laboratory testing were noted.
Therefore, no specific guidance is offered regarding routine monitoring;
the practitioner retains responsibility for determining how best to
monitor the patient in his or her care.
Other adverse events observed during
clinical trials of immediate-release pramipexole tablets
Adverse events not listed above but reported
on at least two occasions (one occasion if the event was serious)
in clinical studies involving 2509 individuals who received pramipexole
immediate-release tablets are listed below. The reported events are
included without regard to determination of a causal relationship
to pramipexole immediate-release tablets.
Blood and lymphatic system disorders: anemia, iron deficiency anemia, leukocytosis, leukopenia, lymphadenitis, lymphadenopathy, thrombocythaemia, thrombocytopenia
Cardiac disorders: angina pectoris, arrhythmia supraventricular, atrial fibrillation, atrioventricular block first degree, atrioventricular block second degree, bradycardia, bundle branch block, cardiac arrest, cardiac failure, cardiac failure congestive, cardiomegaly, coronary artery occlusion, cyanosis, extrasystoles, left ventricular failure, myocardial infarction, nodal arrhythmia, sinus arrhythmia, sinus bradycardia, sinus tachycardia, supraventricular extrasystoles, supraventricular tachycardia, tachycardia, ventricular fibrillation, ventricular extrasystoles, ventricular hypertrophy
Congenital, familial, and genetic disorders: atrial septal defect, congenital foot malformation, spine malformation
Ear and labyrinth disorders: deafness, ear pain, hearing impaired, hypoacusis, motion sickness, vestibular ataxia
Endocrine disorders: goiter, hyperthyroidism, hypothyroidism
Eye disorders: accommodation abnormalities, amaurosis fugax, blepharitis, blepharospasm, cataract, dacryostenosis acquired, diplopia, dry eye, eye hemorrhage, eye irritation, eye pain, eyelid edema, eyelid ptosis, glaucoma, keratitis, macular degeneration, myopia, photophobia, retinal detachment, retinal vascular disorder, scotoma, vision abnormalities, vision blurred, visual acuity reduced, vitreous floaters
Gastrointestinal disorders: abdominal distension, aphthous stomatitis, ascites, cheilitis, colitis, colitis ulcerative, dyspepsia, dysphagia, duodenal ulcer, duodenal ulcer hemorrhage, enteritis, eructation, fecal incontinence, gastric ulcer, gastric ulcer hemorrhage, gastritis, gastrointestinal hemorrhage, gastroesophageal reflux disease, gingivitis, haematemesis, haematochezia, hemorrhoids, hiatus hernia, hyperchlorhydria, ileus, inguinal hernia, intestinal obstruction, irritable bowel syndrome, esophageal spasm, esophageal stenosis, esophagitis, pancreatitis, periodontitis, rectal hemorrhage, reflux esophagitis, tongue edema, tongue ulceration, toothache, umbilical hernia
General disorders: chest discomfort, chills, death, drug withdrawal syndrome, face edema, feeling cold, feeling hot, feeling jittery, fever, gait disturbance, impaired healing, influenza-like illness, irritability, localized edema, edema, malaise, pitting edema, thirst
Hepatobiliary disorders: biliary colic, cholecystitis, cholecystitis chronic, cholelithiasis
Immune system disorders: drug hypersensitivity
Infections and infestations: abscess, acute tonsillitis, appendicitis, bronchiolitis, bronchitis, bronchopneumonia, cellulitis, cystitis, dental caries, diverticulitis, ear infection, eye infection, folliculitis, fungal infection, furuncle, gangrene, gastroenteritis, gingival infection, herpes simplex, herpes zoster, hordeolum, influenza, intervertebral discitis, laryngitis, lobar pneumonia, nail infection, onychomycosis, oral candidiasis, orchitis, osteomyelitis, otitis externa, otitis media, paronychia, pyelonephritis, pyoderma, sepsis, skin infection, tonsillitis, tooth abscess, tooth infection, upper respiratory tract infection, urethritis, vaginal candidiasis, vaginal infection, viral infection, wound infection
Injury, poisoning, and procedural complications: accidental falls, drug toxicity epicondylitis, road traffic accident, sunburn, tendon rupture
Metabolism and nutrition disorders: cachexia, decreased appetite, decreased weight, dehydration, diabetes mellitus, fluid retention, gout, hypercholesterolemia, hyperglycemia, hyperlipidemia, hyperuricemia, hypocalcemia, hypoglycemia, hypokalemia, hyponatremia, hypovitaminosis, increased creatine PK, metabolic alkalosis
Musculoskeletal and connective tissue disorders: bone pain, bursitis, fasciitis, flank pain, intervertebral disc disorder, intervertebral disc protrusion, joint effusion, joint stiffness, joint swelling, monarthritis, muscle rigidity, musculoskeletal stiffness, myasthenia, myopathy, myositis, nuchal rigidity, osteoarthritis, osteonecrosis, osteoporosis, pain in extremity, polymyalgia, rheumatoid arthritis, shoulder pain, spinal osteoarthritis, tendonitis, tenosynovitis, twitching
Neoplasms benign, malignant, and unspecified: abdominal neoplasm, adenocarcinoma, adenoma benign, basal cell carcinoma, bladder cancer, breast cancer, breast neoplasm, chronic lymphocytic leukemia, colon cancer, colorectal cancer, endometrial cancer, gallbladder cancer, gastric cancer, gastrointestinal neoplasm, hemangioma, hepatic neoplasm, hepatic neoplasm malignant, lip and/or oral cavity cancer, lung neoplasm malignant, lung cancer metastatic, lymphoma, malignant melanoma, melanocytic naevus, metastases to lung, multiple myeloma, oral neoplasm benign, neoplasm, neoplasm malignant, neoplasm prostate, neoplasm skin, neuroma, ovarian cancer, prostate cancer, prostatic adenoma, pseudo lymphoma, renal neoplasm, skin cancer, skin papilloma, squamous cell carcinoma, thyroid neoplasm, uterine leiomyoma
Nervous system disorders: ageusia, akinesia, amnesia, akathisia, anticholinergic syndrome, aphasia, brain edema, carotid artery occlusion, carpal tunnel syndrome, cerebral artery embolism, cerebral hemorrhage, cerebral infarction, cerebral ischemia, chorea, cognitive disorder, coma, convulsion, coordination abnormal, dementia, depressed level of consciousness, disturbance in attention, dizziness postural, dysarthria, dysgraphia, dystonia, extrapyramidal syndrome, facial palsy, grand mal convulsion, hemiplegia, hyperaesthesia, hyperkinesia, hyperreflexia, hyporeflexia, hypertonia, hypesthesia, hypotonia, lethargy, loss of consciousness, memory impairment, migraine, muscle contractions involuntary, myoclonus, narcolepsy, neuralgia, neuropathy, nystagmus, parosmia, psychomotor hyperactivity, sciatica, sedation, sensory disturbance, sleep phase rhythm disturbance, sleep talking, stupor, syncope vasovagal, tension headache, thinking abnormalities
Psychiatric disorders: affect lability, aggression, agitation, bradyphrenia, bruxism, suicide, delirium, delusions, delusional disorder persecutory type, disorientation, dissociation, emotional distress, euphoric mood, initial insomnia, libido increased, mania, middle insomnia, mood altered, nightmare, obsessive thoughts, obsessive-compulsive disorder, panic reaction, paranoid reaction, parasomnia, personality disorder, psychotic disorder, restlessness, sleep walking, suicidal ideation
Renal and urinary disorders: chromaturia, dysuria, glycosuria, hematuria, urgency, nephrolithiasis, neurogenic bladder, nocturia, oliguria, pollakiuria, proteinuria, renal artery stenosis, renal colic, renal cyst, renal failure, renal impairment, urinary frequency, urinary incontinence, urinary retention, urinary tract infection
Reproductive system and breast disorders: amenorrhea, breast pain, dysmenorrhea, epididymitis, gynaecomastia, impotence, menopausal symptoms, menorrhagia, metrorrhagia, ovarian cyst, priapism, prostatitis, sexual dysfunction, uterine hemorrhage, vaginal discharge, vaginal hemorrhage
Respiratory, thoracic, and mediastinal disorders: apnea, aspiration, asthma, choking, chronic obstructive pulmonary disease, dry throat, dysphonia, dyspnea exertional, epistaxis, haemoptysis, hiccups, hyperventilation, increased bronchial secretion, laryngospasm, nasal congestion, nasal dryness, nasal polyps, obstructive airways disorder, pharyngolaryngeal pain, pleurisy, pneumonia, pneumonia aspiration, pneumothorax, postnasal drip, productive cough, pulmonary embolism, pulmonary edema, respiratory alkalosis, respiratory distress, respiratory failure, respiratory tract congestion, rhinitis allergic, rhinorrhea, sinus congestion, sleep apnoea syndrome, sneezing, snoring, tachypnea, wheezing
Skin and subcutaneous tissue disorders: acne, alopecia, cold sweat, dermal cyst, dermatitis, dermatitis bullous, dermatitis contact, dry skin, ecchymosis, eczema, erythema, hyperkeratosis, livedo reticularis, night sweats, periorbital edema, petechiae, photosensitivity allergic reaction, psoriasis, purpura, rash erythematous, rash maculo-papular, rash papular, rosacea, seborrhea, seborrheic dermatitis, skin burning sensation, skin discoloration, skin disorders, skin exfoliation, skin hyperpigmentation, skin hypertrophy, skin irritation, skin nodule, skin odor abnormal, skin ulcer, urticaria
Vascular disorders: aneurysm, angiopathy, arteriosclerosis, circulatory collapse, deep vein thrombosis, embolism, hematoma, hot flush, hypertensive crisis, lymphoedema, pallor, phlebitis, Raynaud’s phenomenon, shock, thrombophlebitis, thrombosis, varicose vein
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of immediate-release pramipexole tablets, primarily in Parkinson’s disease patients. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) strength of causal connection to pramipexole tablets. Similar types of events were grouped into a smaller number of standardized categories using the MedDRA terminology: abnormal behavior, abnormal dreams, accidents (including fall), blackouts, compulsive shopping, fatigue, hallucinations (all kinds), headache, hypotension (including postural hypotension), inappropriate antidiuretic hormone secretion (SIADH), increased eating (including binge eating, compulsive eating, and hyperphagia), libido disorders (including increased and decreased libido, and hypersexuality), pathological gambling, pruritus, syncope, vomiting, and weight increase.
7 DRUG INTERACTIONS
No drug interaction studies were conducted with MIRAPEX ER tablets since the potential for drug interactions mainly depends on the active drug substance pramipexole and not the formulation. Data are available for the immediate-release pramipexole tablet formulation [ see Clinical Pharmacology (12.3) ].
7.1 Dopamine Antagonists
Since pramipexole is a dopamine agonist, it is possible that dopamine antagonists, such as the neuroleptics (phenothiazines, butyrophenones, thioxanthenes) or metoclopramide, may diminish the effectiveness of MIRAPEX ER tablets.
7.2 Drug/Laboratory Test Interactions
There are no known interactions between pramipexole and laboratory tests.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There
are no adequate and well-controlled studies in pregnant women. MIRAPEX
ER should be used during pregnancy only if the potential benefit justifies
the potential risk to the fetus.
When pramipexole was given to female rats throughout pregnancy, implantation was inhibited at a dose of 2.5 mg/kg/day [5 times the maximum recommended human dose (MRHD) on a mg/m2 basis]. Administration of 1.5 mg/kg/day of pramipexole to pregnant rats during the period of organogenesis (gestation days 7 through 16) resulted in a high incidence of total resorption of embryos. The plasma AUC in rats at this dose was 4 times the AUC in humans at the MRHD. These findings are thought to be due to the prolactin-lowering effect of pramipexole, since prolactin is necessary for implantation and maintenance of early pregnancy in rats (but not rabbits or humans). Because of pregnancy disruption and early embryonic loss in these studies, the teratogenic potential of pramipexole could not be adequately evaluated. There was no evidence of adverse effects on embryo-fetal development following administration of up to 10 mg/kg/day to pregnant rabbits during organogenesis (plasma AUC was 70 times that in humans at the MRHD). Postnatal growth was inhibited in the offspring of rats treated with 0.5 mg/kg/day (approximately equivalent to the MRHD on a mg/m2 basis) or greater during the latter part of pregnancy and throughout lactation.
8.3 Nursing Mothers
A single-dose, radio-labeled study showed that drug-related material was present in rat milk at concentrations three to six times higher than in plasma at equivalent time points.
Studies have shown that pramipexole treatment resulted in an inhibition of prolactin secretion in humans and rats.
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from pramipexole, a decision should be made as to whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The pharmacokinetics, safety, and efficacy of MIRAPEX ER tablets in pediatric patients have not been evaluated.
8.5 Geriatric Use
Pramipexole total oral clearance is approximately 30% lower in subjects older than 65 years compared with younger subjects, because of a decline in pramipexole renal clearance due to an age-related reduction in renal function. This resulted in an increase in elimination half-life from approximately 8.5 hours to 12 hours. In a placebo-controlled clinical trial of MIRAPEX ER tablets in early Parkinson’s disease, 47% of the 259 patients were ≥65 years of age. Among patients receiving MIRAPEX ER tablets, hallucinations were more common in the elderly, occurring in 13% of the patients ≥65 years of age compared to 2% of the patients <65 years of age.
8.6 Patients with Renal Impairment
The elimination of pramipexole is dependent upon renal function. Pramipexole clearance is extremely low in dialysis patients, as a negligible amount of pramipexole is removed by dialysis [ see Dosage and Administration (2.2), Warnings and Precautions (5.6), and Clinical Pharmacology (12.3) ].
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Pramipexole is not a controlled substance.
9.2 Abuse and Dependence
Pramipexole has not been systematically studied in animals or humans for its potential for abuse, tolerance, or physical dependence. However, in a rat model of cocaine self-administration, pramipexole had little or no effect.
10 OVERDOSAGE
There is no clinical experience with significant overdosage. One patient took 11 mg/day of pramipexole for 2 days in a clinical trial for an investigational use. Blood pressure remained stable, although pulse rate increased to between 100 and 120 beats/minute. No other adverse events were reported related to the increased dose.
There is no known antidote for overdosage of a dopamine agonist. If signs of central nervous system stimulation are present, a phenothiazine or other butyrophenone neuroleptic agent may be indicated; the efficacy of such drugs in reversing the effects of overdosage has not been assessed. Management of overdose may require general supportive measures along with gastric lavage, intravenous fluids, and electrocardiogram monitoring.
11 DESCRIPTION
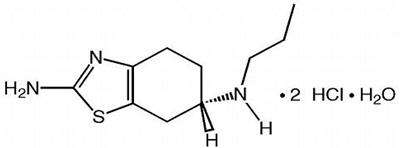
MIRAPEX ER tablets contain pramipexole, a non-ergot dopamine agonist. The chemical name of pramipexole dihydrochloride is ( S )-2-amino-4,5,6,7-tetrahydro-6-(propylamino)benzothiazole dihydrochloride monohydrate. Its empirical formula is C10 H17 N3 S • 2HCl • H2O, and its molecular weight is 302.26.
The structural formula is:
Pramipexole dihydrochloride is a white to off-white powder substance. Melting occurs in the range of 296°C to 301°C, with decomposition. Pramipexole dihydrochloride is more than 20% soluble in water, about 8% in methanol, about 0.5% in ethanol, and practically insoluble in dichloromethane.
MIRAPEX ER tablets, for oral administration, contain 0.375 mg, 0.75 mg, 1.5 mg, 2.25 mg, 3 mg, 3.75 mg, or 4.5 mg of pramipexole dihydrochloride monohydrate. Inactive ingredients are hypromellose, corn starch, carbomer homopolymer, colloidal silicon dioxide, and magnesium stearate.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pramipexole is a non-ergot dopamine agonist with high relative in vitro specificity and full intrinsic activity at the D2 subfamily of dopamine receptors, binding with higher affinity to D3 than to D2 or D4 receptor subtypes.
The precise mechanism of action of pramipexole as a treatment for Parkinson's disease is unknown, although it is believed to be related to its ability to stimulate dopamine receptors in the striatum. This conclusion is supported by electrophysiologic studies in animals that have demonstrated that pramipexole influences striatal neuronal firing rates via activation of dopamine receptors in the striatum and the substantia nigra, the site of neurons that send projections to the striatum. The relevance of D3 receptor binding in Parkinson’s disease is unknown.
12.2 Pharmacodynamics
The effect of pramipexole on the QT interval of the ECG was investigated in a clinical study in 60 healthy male and female volunteers. All subjects initiated treatment with 0.375 mg MIRAPEX ER tablets administered once daily, and were up-titrated every 3 days to 2.25 mg and 4.5 mg daily, a faster rate of titration than recommended in the label. No dose- or exposure-related effect on mean QT intervals was observed; however the study did not have a valid assessment of assay sensitivity. The effect of pramipexole on QTc intervals at higher exposures achieved either due to drug interactions (e.g., with cimetidine), renal impairment, or at higher doses has not been systematically evaluated.
Although mean values remained within normal reference ranges throughout the study, supine systolic blood pressure (SBP), diastolic blood pressure (DBP), and pulse rate for subjects treated with pramipexole generally increased during the rapid up-titration phase, by 10 mmHg, 7 mmHg, and 10 bpm higher than placebo, respectively. Higher SBP, DBP, and pulse rates compared to placebo were maintained until the pramipexole doses were tapered; values on the last day of tapering were generally similar to baseline values. Such effects have not been observed in clinical studies with Parkinson’s disease patients, who were titrated according to labeled recommendations.
12.3 Pharmacokinetics
MIRAPEX ER tablets, like immediate-release pramipexole tablets, display linear pharmacokinetics over the entire clinical dosage range. Slow release of pramipexole from MIRAPEX ER tablets with once-daily administration results in the same daily maximum and minimum pramipexole plasma concentrations (Cmax, Cmin) as three times daily administration of immediate-release pramipexole tablets.
Absorption
The absolute bioavailability of pramipexole
is greater than 90%, indicating that it is well absorbed and undergoes
little presystemic metabolism.
Increase in systemic exposure of pramipexole following oral administration of 0.375 mg to 4.5 mg of MIRAPEX ER tablets was dose-proportional. For MIRAPEX ER tablets, steady state of exposure is reached within 5 days of continuous dosing.
Relative bioavailability of MIRAPEX ER tablets compared with immediate-release tablets was approximately 100%. In a repeat-dose study in healthy, normal volunteers, MIRAPEX ER tablets 4.5 mg administered once daily was bioequivalent with regard to Cmax and AUC over 24 hours to immediate-release pramipexole tablets 1.5 mg administered three times daily. The average time-to-peak concentration for MIRAPEX ER tablets is 6 hours. Administration of MIRAPEX ER tablets with food (i.e., high-fat meal) did not affect AUC but increased Cmax by approximately 20% and delayed Tmax by approximately 2 hours compared with dosing under fasted conditions; these differences are not considered to be clinically relevant [ see Dosage and Administration (2.1) ].
Distribution
Pramipexole
is extensively distributed, having a volume of distribution of about
500 L (coefficient of variation [CV] = 20%). It is about 15% bound
to plasma proteins. Pramipexole distributes into red blood cells as
indicated by an erythrocyte-to-plasma ratio of approximately 2.
Metabolism
Pramipexole is metabolized only to a negligible
extent (<10%). No specific active metabolite has been identified
in human plasma or urine.
Elimination
Urinary excretion
is the major route of pramipexole elimination, with 90% of a pramipexole
dose recovered in urine, almost all as unchanged drug. The renal clearance
of pramipexole is approximately 400 mL/min (CV=25%), approximately
three times higher than the glomerular filtration rate. Thus, pramipexole
is secreted by the renal tubules, probably by the organic cation transport
system.
Pharmacokinetics
in Specific Populations
Because therapy
with MIRAPEX ER tablets is initiated at a low dose and gradually titrated
upward according to clinical tolerability to obtain the optimum therapeutic
effect, adjustment of the initial dose based on gender, weight, race,
or age is not necessary. However, renal insufficiency causes a large
decrease in the ability to eliminate pramipexole. This will necessitate
dosage adjustment in patients with moderate to severe renal impairment
[
see Dosage and Administration (2.2)
].
Gender
Pramipexole clearance is about 30% lower in women than in men, but
this difference can be accounted for by differences in body weight.
There is no difference in plasma half-life between males and females.
Age
Pramipexole clearance is reduced by approximately 30%
in the elderly (aged 65 years or older) compared with young, healthy
volunteers (aged less than 40 years). This difference is most likely
due to the reduction in renal function with age, since pramipexole
clearance is correlated with renal function, as measured by creatinine
clearance.
Race
No racial differences in metabolism
and elimination have been identified.
Hepatic Impairment
The influence of hepatic insufficiency on pramipexole
pharmacokinetics has not been evaluated. Because approximately 90%
of the recovered dose is excreted in the urine as unchanged drug,
hepatic impairment would not be expected to have a significant effect
on pramipexole elimination.
Renal Impairment
Clearance
of immediate-release pramipexole was about 75% lower in patients with
severe renal impairment (creatinine clearance approximately 20 mL/min)
and about 60% lower in patients with moderate impairment (creatinine
clearance approximately 40 mL/min) compared with healthy volunteers
[
see Dosage and Administration (2.2) and Warnings and Precautions (5.6)
]. In patients
with varying degrees of renal impairment, pramipexole clearance correlates
well with creatinine clearance. Therefore, creatinine clearance can
be used as a predictor of the extent of decrease in pramipexole clearance.
Drug Interactions
No specific pharmacokinetic drug interaction
trials were conducted with MIRAPEX ER tablets since the potential
for drug interactions mainly depends on the active drug substance
pramipexole and not the formulation. The following interaction data
were obtained using immediate-release pramipexole tablets.
Carbidopa/levodopa: Carbidopa/levodopa did not influence the pharmacokinetics of pramipexole in healthy volunteers (N=10). Pramipexole did not alter the extent of absorption (AUC) or the elimination of carbidopa/levodopa, although it caused an increase in levodopa Cmax by about 40% and a decrease in Tmax from 2.5 to 0.5 hours.
Selegiline: In healthy volunteers (N=11), selegiline did not influence the pharmacokinetics of pramipexole.
Amantadine: Population pharmacokinetic analyses suggest that amantadine may slightly decrease the oral clearance of pramipexole.
Cimetidine: Cimetidine, a known inhibitor of renal tubular secretion of organic bases via the cationic transport system, caused a 50% increase in pramipexole AUC and a 40% increase in half-life (N=12).
Probenecid: Probenecid, a known inhibitor of renal tubular secretion of organic acids via the anionic transporter, did not noticeably influence pramipexole pharmacokinetics (N=12).
Other drugs eliminated via renal secretion: Population pharmacokinetic analysis suggests that co-administration of drugs that are secreted by the cationic transport system (e.g., cimetidine, ranitidine, diltiazem, triamterene, verapamil, quinidine, and quinine) decreases the oral clearance of pramipexole by about 20%, while those secreted by the anionic transport system (e.g., cephalosporins, penicillins, indomethacin, hydrochlorothiazide, and chlorpropamide) are likely to have little effect on the oral clearance of pramipexole. Other known organic cation transport substrates and/or inhibitors (e.g., cisplatin and procainamide) may also decrease the clearance of pramipexole.
CYP interactions: Inhibitors of cytochrome P450 enzymes would not be expected to affect pramipexole elimination because pramipexole is not appreciably metabolized by these enzymes in vivo or in vitro . Pramipexole does not inhibit CYP enzymes CYP1A2, CYP2C9, CYP2C19, CYP2E1, and CYP3A4. Inhibition of CYP2D6 was observed with an apparent Ki of 30 μM, indicating that pramipexole will not inhibit CYP enzymes at plasma concentrations observed following the clinical dose of 4.5 mg/day.
Drugs affecting gastrointestinal
motility or gastric pH:
Population
pharmacokinetic analysis suggests that co-administration of antacids
(N=6) decreased the oral clearance of pramipexole by about 25%, while
H2-blockers (N=5), anticholinergics (N=27), propulsive (N=7), and
proton pump inhibitors (N=16) are likely to have little effect on
the oral clearance of pramipexole.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year carcinogenicity studies with pramipexole have been conducted in mice and rats. Pramipexole was administered in the diet to mice at doses up to 10 mg/kg/day [or approximately 10 times the maximum recommended human dose (MRHD) of 1.5 mg TID on a mg/m2 basis]. Pramipexole was administered in the diet to rats at doses up to 8 mg/kg/day. These doses were associated with plasma AUCs up to approximately 12 times that in humans at the MRHD. No significant increases in tumors occurred in either species.
Pramipexole was not mutagenic or clastogenic in a battery of in vitro (bacterial reverse mutation, V79/HGPRT gene mutation, chromosomal aberration in CHO cells) and in vivo (mouse micronucleus) assays.
In rat fertility studies, pramipexole at a dose of 2.5 mg/kg/day (5 times the MRHD on a mg/m2 basis) prolonged estrus cycles and inhibited implantation. These effects were associated with reductions in serum levels of prolactin, a hormone necessary for implantation and maintenance of early pregnancy in rats.
13.2 Animal Toxicology and/or Pharmacology
Retinal Pathology in Albino Rats
Pathologic changes (degeneration and loss of photoreceptor
cells) were observed in the retina of albino rats in the 2-year carcinogenicity
study with pramipexole. These findings were first observed during
week 76 and were dose-dependent in animals receiving 2 or 8 mg/kg/day
(plasma AUCs equal to 2.5 and 12.5 times that in humans at the MRHD
of 1.5 mg TID). In a similar study of pigmented rats with 2-years
exposure to pramipexole at 2 or 8 mg/kg/day, retinal degeneration
was not observed. Animals given drug had thinning in the outer nuclear
layer of the retina that was only slightly greater than that seen
in control rats.
Investigative studies demonstrated that pramipexole reduced the rate of disk shedding from the photoreceptor rod cells of the retina in albino rats, which was associated with enhanced sensitivity to the damaging effects of light. In a comparative study, degeneration and loss of photoreceptor cells occurred in albino rats after 13 weeks of treatment with 25 mg/kg/day of pramipexole (54 times the highest clinical dose on a mg/m2 basis) and constant light (100 lux), but not in pigmented rats exposed to the same dose and higher light intensities (500 lux). Thus, the retina of albino rats is considered to be uniquely sensitive to the damaging effects of pramipexole and light. Similar changes in the retina did not occur in a 2-year carcinogenicity study in albino mice treated with 0.3, 2, or 10 mg/kg/day (0.3, 2.2, and 11 times the highest clinical dose on a mg/m2 basis). Evaluation of the retinas of monkeys given 0.1, 0.5, or 2.0 mg/kg/day of pramipexole (0.4, 2.2, and 8.6 times the highest clinical dose on a mg/m2 basis) for 12 months and minipigs given 0.3, 1, or 5 mg/kg/day of pramipexole for 13 weeks also detected no changes.
The potential significance of this effect in humans has not been established, but cannot be disregarded because disruption of a mechanism that is universally present in vertebrates (i.e., disk shedding) may be involved.
Fibro-osseous Proliferative Lesions in Mice
An increased incidence of fibro-osseous proliferative lesions occurred
in the femurs of female mice treated for 2 years with 0.3, 2.0, or
10 mg/kg/day (0.3, 2.2, and 11 times the highest clinical dose on
a mg/m2 basis). Lesions occurred at a lower
rate in control animals. Similar lesions were not observed in male
mice or rats and monkeys of either sex that were treated chronically
with pramipexole. The significance of this lesion to humans is not
known.
14 CLINICAL STUDIES
The effectiveness of MIRAPEX ER tablets in the treatment of Parkinson’s disease was supported by clinical pharmacokinetic data [ see Clinical Pharmacology (12.3) ] and two randomized, double-blind, placebo-controlled, multicenter clinical trials in early and advanced Parkinson's disease. In both randomized studies, the Unified Parkinson’s Disease Rating Scale (UPDRS) served as a primary outcome assessment measure. The UPDRS is a four-part multi-item rating scale intended to evaluate mentation (Part I), activities of daily living (Part II), motor performance (Part III), and complications of therapy (Part IV).
Part II of the UPDRS contains 13 questions related to activities of daily living, which are scored from 0 (normal) to 4 (maximal severity) for a maximum (worst) score of 52. Part III of the UPDRS contains 14 items designed to assess the severity of the cardinal motor findings in patients with Parkinson’s disease (e.g., tremor, rigidity, bradykinesia, postural instability, etc.), scored for different body regions and has a maximum (worst) score of 108.
Early Parkinson's Disease
The effectiveness of MIRAPEX ER tablets in early
Parkinson's disease patients (Hoehn & Yahr Stages I-III) who were
not on levodopa therapy was established in a randomized, double-blind,
placebo-controlled, 3-parallel-group clinical study. Patients were
treated with MIRAPEX ER tablets, immediate-release pramipexole tablets,
or placebo; those treated with MIRAPEX ER tablets or immediate-release
pramipexole tablets had a starting dose of 0.375 mg/day followed by
a flexible up-titration, based on efficacy and tolerability, up to
4.5 mg/day. Levodopa was permitted during the study as rescue medication.
Stable doses of concomitant MAO-B inhibitors, anticholinergics, or
amantadine, individually or in combination, were allowed. The primary
efficacy endpoint was the mean change from baseline in the UPDRS Parts
II+III score for MIRAPEX ER tablets versus placebo following 18 weeks
of treatment.
At 18 weeks of treatment, the mean change from baseline UPDRS Parts II+III score was –8.1 points in patients receiving MIRAPEX ER tablets (n=102) and –5.1 points in patients receiving placebo (n=50), a difference that was statistically significant (p<0.03). Seven patients treated with placebo (14%) and 3 patients treated with MIRAPEX ER tablets (3%) received levodopa rescue medication. At 18 weeks, the mean dose of MIRAPEX ER was 3 mg/day.
At 33-weeks, the adjusted mean improvement from baseline UPDRS Parts II+III score was –8.6 points in patients receiving MIRAPEX ER tablets (n=213), compared to –3.8 points in patients receiving placebo (n=103).
At 18 and 33 weeks, the mean dose of MIRAPEX ER tablets was approximately 3 mg/day. Twenty-two patients treated with placebo (21%) and 15 patients treated with MIRAPEX ER tablets (7%) received levodopa rescue medication before the final assessment.
No differences in effectiveness based on age or gender were detected. Patients receiving MAOB-I, anticholinergics, or amantadine had responses similar to patients not receiving these drugs.
Advanced
Parkinson's Disease
The effectiveness
of MIRAPEX ER tablets in advanced Parkinson's disease patients (Hoehn
& Yahr Stages II-IV at "on" time) who were on concomitant levodopa
therapy (at an optimized dose) and who had motor fluctuations (at
least 2 cumulative hours of "off" time per day) was established in
a randomized, double-blind, placebo-controlled, 3-parallel-group clinical
study. Patients were treated with MIRAPEX ER tablets, immediate-release
pramipexole tablets, or placebo; those treated with MIRAPEX ER tablets
or immediate-release pramipexole tablets had a starting dose of 0.375
mg/day followed by a flexible up-titration over 7 weeks, based on
efficacy and tolerability, up to 4.5 mg/day, followed by a 26 week
maintenance period. Levodopa dosage reduction was permitted only in
the case of dopaminergic adverse events. The primary efficacy endpoint
was the adjusted mean change from baseline in the UPDRS Parts II+III
score for MIRAPEX ER tablets versus placebo following 18 weeks of
treatment.
At 18 weeks of treatment, the adjusted mean improvement from baseline UPDRS Parts II+III score was –11.0 points in patients receiving MIRAPEX ER tablets (n=161) and –6.1 points in patients receiving placebo (n=174), (p=0.0001). At week 18, the adjusted mean improvement from baseline in "off" time was –2.1 hours for MIRAPEX ER and –1.4 hours for placebo (p=0.0199).
At 33-weeks the adjusted mean improvement from baseline UPDRS Parts II+III score was –11.1 points in patients receiving MIRAPEX ER tablets (n=117) and –6.8 points in patients receiving placebo (n=136) (p=0.0135).
At both 18 and 33 weeks the mean daily dose of MIRAPEX ER was 2.6 mg/day. At week 18, 4 patients (3%) in the placebo group and 14 patients (11%) in the MIRAPEX ER group had decreased their levodopa daily dose compared to baseline due to dopaminergic adverse events. No clinically relevant difference in effectiveness was observed in the sub-group analyses based on gender, age, race (White vs Asian), or concomitant use of antiparkinsonian treatment (MAOB-I, amantadine or anticholinergics).
16 HOW SUPPLIED/STORAGE AND HANDLING
MIRAPEX ER tablets are available as follows:
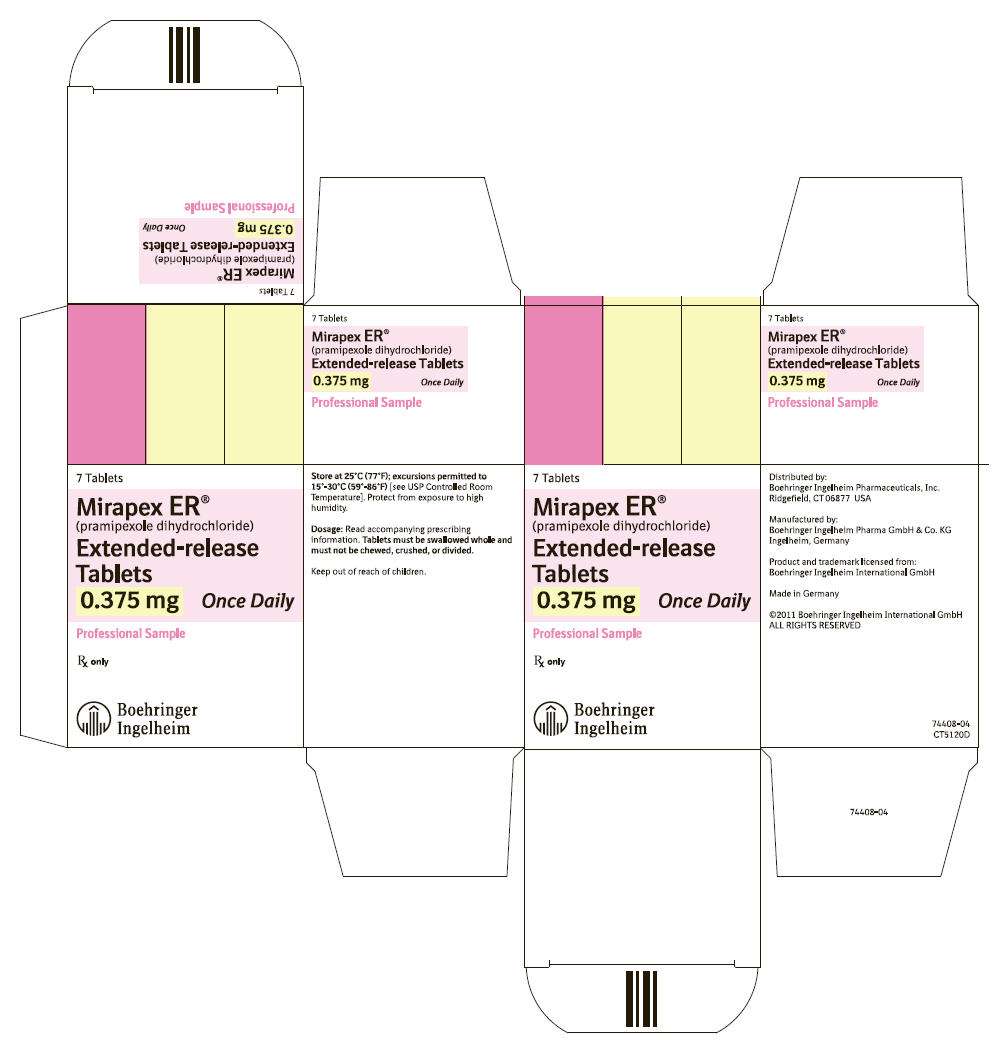
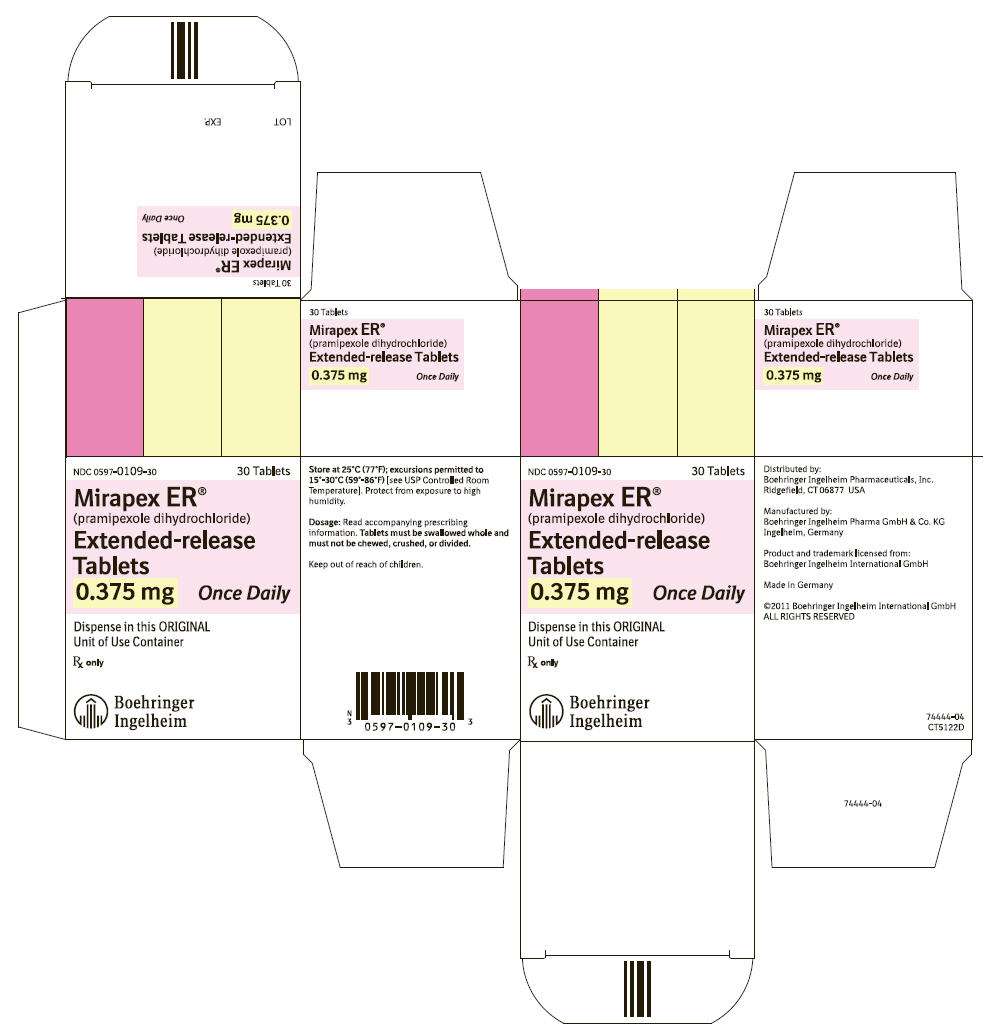
0. 375 mg:
white
to off-white, round, bevel-edged, extended-release tablets debossed
with "ER" on one side and "0.375" on the other side.
Unit of Use Bottles of 7 NDC 0597-0109-17
Unit of Use Bottles of 30
NDC 0597-0109-30
0.75 mg:
white to off-white, round, bevel-edged,
extended-release tablets debossed with "ER" on one side and "0.75"
on the other side.
Unit of Use Bottles
of 7 NDC 0597-0285-17
Unit of Use Bottles of 30 NDC 0597-0285-30
1.5 mg:
white to off-white, oval, extended-release tablets debossed with
"ER" on one side and "1.5" on the other side.
Unit of Use Bottles of 7 NDC 0597-0113-17
Unit of Use Bottles of 30
NDC 0597-0113-30
2.25 mg:
white to off-white, oval, extended-release
tablets debossed with "ER" on one side and "2.25" on the other side.
Unit of Use Bottles of 30
NDC 0597-0286-30
3 mg:
white to off-white, oval, extended-release
tablets debossed with "ER" on one side and "3.0" on the other side.
Unit of Use Bottles of 30
NDC 0597-0115-30
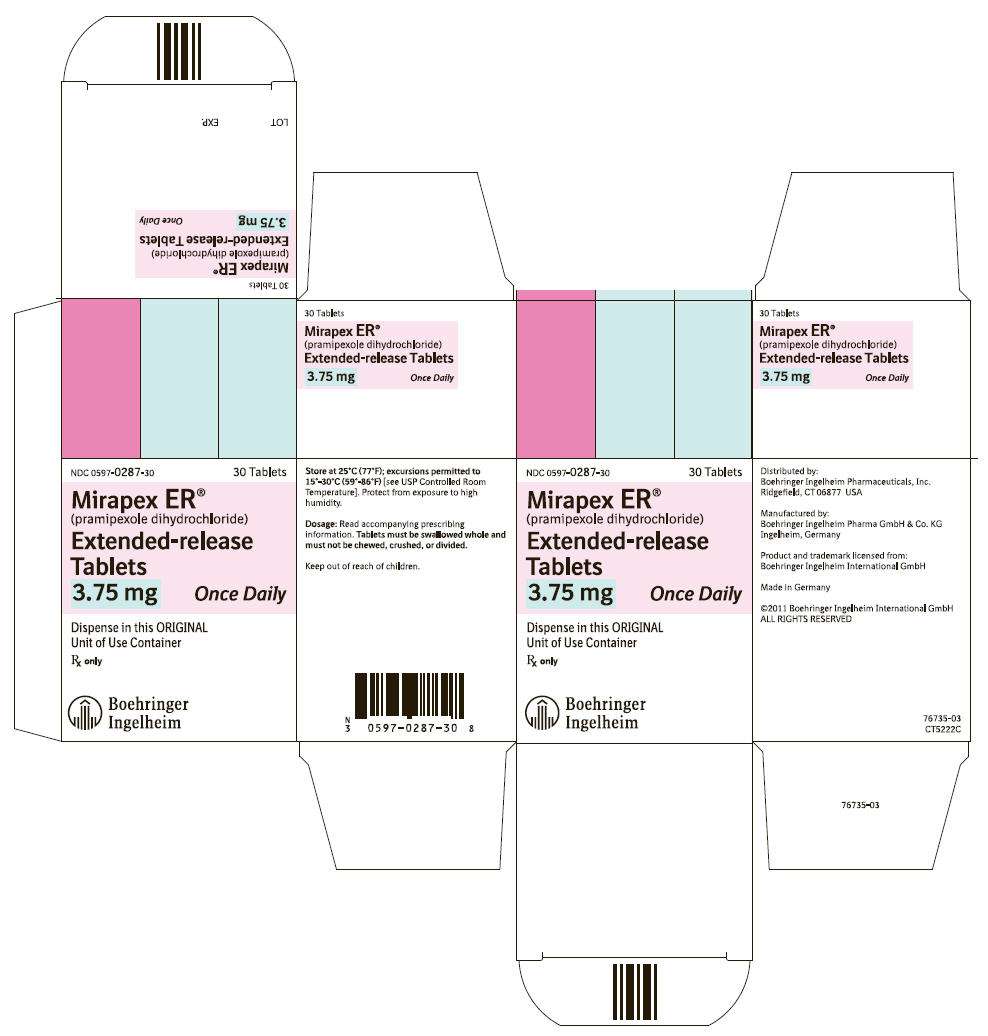
3.75 mg:
white to off-white, oval, extended-release
tablets debossed with "ER" on one side and "3.75" on the other side.
Unit of Use Bottles of 30
NDC 0597-0287-30
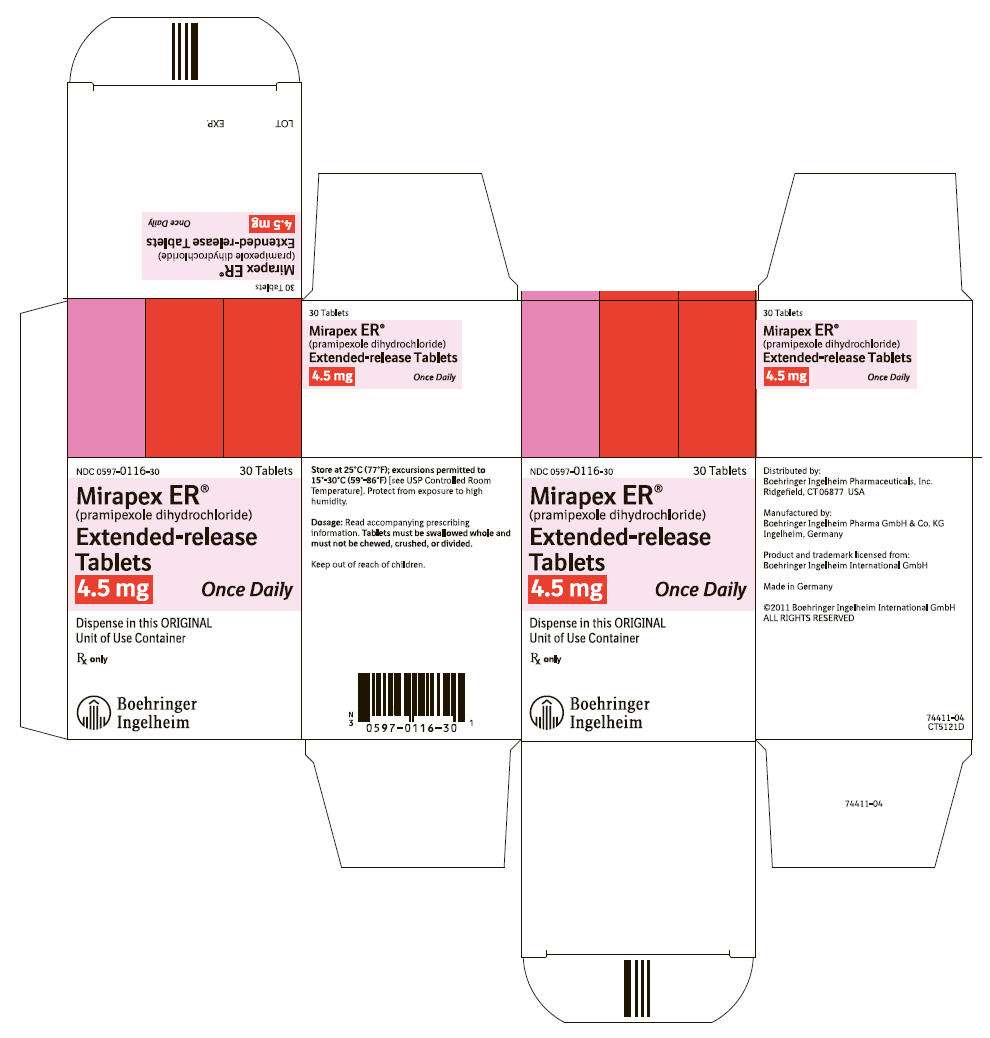
4.5 mg:
white to off-white, oval, extended-release
tablets debossed with "ER" on one side and "4.5" on the other side.
Unit of Use Bottles of 30
NDC 0597-0116-30
Storage
Store at 25°C
(77°F); excursions permitted to 15°-30°C (59°-86°F)
[see USP Controlled Room Temperature]. Protect from exposure to
high humidity. Store in a safe place out of the reach of children.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling
17.1 Dosing Instructions
Instruct patients to take MIRAPEX ER tablets only as prescribed. If a dose is missed, MIRAPEX ER tablets should be taken as soon as possible, but no later than 12 hours after the regularly scheduled time. After 12 hours, the missed dose should be skipped and the next dose should be taken on the following day at the regularly scheduled time.
MIRAPEX ER tablets can be taken with or without food. If patients develop nausea, advise that taking MIRAPEX ER tablets with food may reduce the occurrence of nausea.
MIRAPEX ER tablets should be swallowed whole. They should not be chewed, crushed, or divided [ see Dosage and Administration (2.1) ].
Pramipexole is the active ingredient that is in both MIRAPEX ER tablets and immediate-release pramipexole tablets. Ensure that patients do not take both immediate-release pramipexole and MIRAPEX ER.
17.2 Sedating Effects
Alert patients to the potential sedating effects of MIRAPEX ER tablets, including somnolence and the possibility of falling asleep while engaged in activities of daily living. Since somnolence is a frequent adverse event with potentially serious consequences, patients should neither drive a car nor engage in other potentially dangerous activities until they have gained sufficient experience with MIRAPEX ER tablets to gauge whether or not it affects their mental and/or motor performance adversely. Advise patients that if increased somnolence or new episodes of falling asleep during activities of daily living (e.g., conversations or eating) are experienced at any time during treatment, they should not drive or participate in potentially dangerous activities until they have contacted their physician. Because of possible additive effects, caution should be advised when patients are taking other sedating medications or alcohol in combination with MIRAPEX ER and when taking concomitant medications that increase plasma levels of pramipexole (e.g., cimetidine) [ see Warnings and Precautions (5.1) ].
17.3 Impulse Control Symptoms Including Compulsive Behaviors
Patients and their caregivers should be alerted to the possibility that they may experience intense urges to spend money, intense urges to gamble, increased sexual urges, binge eating and/or other intense urges and the inability to control these urges while taking MIRAPEX ER [ see Warnings and Precautions (5.3) ].
17.4 Hallucinations
Inform patients that hallucinations can occur and that the elderly are at a higher risk than younger patients with Parkinson's disease [ see Warnings and Precautions (5.4) ].
17.5 Postural (Orthostatic) Hypotension
Advise patients that they may develop postural (orthostatic) hypotension, with or without symptoms such as dizziness, nausea, fainting, or blackouts, and sometimes, sweating. Hypotension may occur more frequently during initial therapy. Accordingly, caution patients against rising rapidly after sitting or lying down, especially if they have been doing so for prolonged periods and especially at the initiation of treatment with MIRAPEX ER [ see Warnings and Precautions (5.2) ].
17.6 Pregnancy
Because the teratogenic potential of pramipexole has not been completely established in laboratory animals, and because experience in humans is limited, advise women to notify their physicians if they become pregnant or intend to become pregnant during therapy [ see Use in Specific Populations (8.1) ].
17.7 Nursing Mothers
Because of the possibility that pramipexole may be excreted in breast milk, advise women to notify their physicians if they intend to breast-feed or are breast-feeding an infant [ see Use in Specific Populations (8.3) ].
Distributed by:
Boehringer
Ingelheim Pharmaceuticals, Inc.
Ridgefield, CT 06877 USA
Licensed from:
Boehringer Ingelheim
International GmbH
Address medical inquiries to: (800) 542-6257 or (800) 459-9906 TTY.
Trademark under license from:
Boehringer
Ingelheim International GmbH
Copyright ©2014 Boehringer Ingelheim International GmbH
ALL RIGHTS RESERVED
OT220011YE142014
74988-11
Patient Information
Mirapex ER®
[mîr′-ah-pěx]
(pramipexole dihydrochloride)
extended-release tablets
Read this Patient Information before you start taking MIRAPEX ER and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment.
What is MIRAPEX ER?
MIRAPEX ER is a prescription medicine used to treat the signs and symptoms of Parkinson's disease.
It is not known if MIRAPEX ER is safe and effective in children.
What should I tell my doctor before taking MIRAPEX ER?
Before taking MIRAPEX ER, tell your doctor if you:
- feel sleepy during the day
- have low blood pressure, or if you feel dizzy or faint, especially when getting up from sitting or lying down.
- have trouble controlling your muscles (dyskinesia)
- have kidney problems
- drink alcohol. Alcohol can increase the chance that MIRAPEX ER will make you feel sleepy or fall asleep when you should be awake.
- are pregnant or plan to become pregnant. It is not known if MIRAPEX ER will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if MIRAPEX ER passes into your breast milk. You and your doctor should decide if you will take MIRAPEX ER or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
MIRAPEX ER and other medicines may affect each other causing side effects. MIRAPEX ER may affect the way other medicines work, and other medicines may affect how MIRPAEX ER works.
Especially tell your doctor if you take:
- medicines called neuroleptics (phenothiazines, butyrophenones, thioxanthenes) or metoclopramide. MIRAPEX ER may not work as well if you take these medicines.
- pramipexole (MIRAPEX). Pramipexole is the active ingredient in both MIRAPEX ER and MIRAPEX. If you are taking MIRAPEX, you should not take MIRAPEX ER.
- any other medicines that make you sleepy or may increase the effects of MIRAPEX ER, such as cimetidine (Tagamet).
Ask your doctor for a list of these medicines if you are not sure.
Know the medicines you take. Keep a list of them and show it to your doctor and pharmacist when you get a new medicine.
How should I take MIRAPEX ER?
- MIRAPEX ER is taken once daily.
- Your doctor will tell you how much MIRAPEX ER to take and when to take it. Do not take more or less MIRAPEX ER than your doctor tells you to.
- Swallow MIRAPEX ER whole. Do not chew, crush, or cut MIRAPEX ER.
- MIRAPEX ER can be taken with or without food. Taking MIRAPEX ER with food may lower your chances of getting nausea.
- If you miss a dose of MIRAPEX ER it should be taken as soon as possible, but no later than 12 hours after your regularly scheduled time. If it is later than 12 hours, the missed dose should be skipped and the next dose should be taken on the following day at your regularly scheduled time. Do not double your next MIRAPEX ER dose.
-
Do not stop taking MIRAPEX ER without talking
to your doctor first. If your doctor tells you to stop taking MIRAPEX
ER, you should ask your doctor for specific instructions on how to
slowly and safely discontinue taking MIRAPEX ER. If you stop taking
MIRAPEX ER too quickly you may have withdrawal symptoms such as:
- fever
- confusion
- severe muscle stiffness
What should I avoid while taking MIRAPEX ER?
- Do not drink alcohol while taking MIRAPEX ER. It can increase your chance of having serious side effects. See “What are the possible side effects of MIRAPEX ER?”
- Do not drive a car, operate a machine, or do other dangerous activities until you know how MIRAPEX ER affects you. Sleepiness caused by MIRAPEX ER can happen as late as 1 year after you start your treatment.
What are the possible side effects of MIRAPEX ER?
MIRAPEX ER may cause serious side effects, including:
-
falling asleep during normal daily activities. MIRAPEX ER may cause you to fall asleep while you are doing daily
activities such as driving, talking with other people, or eating.
- Some people taking the medicine in MIRAPEX ER have had car accidents because they fell asleep while driving.
- Some people did not feel sleepy before they fell asleep while driving. You could fall asleep without any warning.
Tell your doctor right away if you fall asleep while you are doing activities such as talking, eating, driving, or if you feel sleepier than normal for you. -
low blood pressure when you sit or stand up quickly. After you have been sitting or lying down, stand up slowly until
you know how MIRAPEX ER affects you. This may help reduce the following
symptoms while you are taking MIRAPEX ER:
- dizziness
- nausea
- fainting
- sweating
-
unusual urges. Some people who take certain
medicines to treat Parkinson’s disease, including MIRAPEX ER, have
reported problems, such as gambling, compulsive eating, compulsive
buying, and increased sex drive.
If you or your family members notice that you are developing unusual urges or behaviors, talk to your doctor. - seeing visions, hearing sounds or feeling sensations that are not real (hallucinations). Your chance of having hallucinations is higher if you are age 65 or older.
- uncontrolled sudden movements (dyskinesia). If you have new dyskinesia, or your existing dyskinesia gets worse, tell your doctor.
- skin cancer (melanoma). Some people with Parkinson’s disease may have a higher chance of having melanoma than people who do not have Parkinson’s disease. It is not known if the chance of having melanoma is higher because of the medicines to treat Parkinson’s disease, like MIRAPEX ER, or from the Parkinson’s disease. People who take MIRAPEX ER should have regular skin examinations to check for melanoma.
The most common side effects in people taking MIRAPEX ER for early Parkinson’s disease are:
-
- nausea and vomiting
- constipation
- dizziness
- fatigue
- dry mouth
- swelling of the feet and ankles
The most common side effects in people taking MIRAPEX ER who have later stage Parkinson’s disease are nausea, constipation, headache and weight loss (anorexia).
These are not all the possible side effects of MIRAPEX ER. Tell your doctor if you have any side effect that bothers you.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store MIRAPEX ER?
-
- Store MIRAPEX ER at room temperature between 68ºF to 77ºF (20ºC to 25ºC).
- Keep MIRAPEX ER away from high humidity or moisture.
- Keep MIRAPEX ER and all medicines out of the reach of children.
General Information about the safe and effective use of MIRAPEX ER.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use MIRAPEX ER for a condition for which it was not prescribed. Do not give MIRAPEX ER to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about MIRAPEX ER. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for more information about MIRAPEX ER tablets that is written for healthcare professionals.
For more information, go to www.mirapexer.com (or scan the code below to go to www.mirapexer.com) or call Boehringer Ingelheim Pharmaceuticals, Inc. at 1-800-542-6257 or (TTY) 1-800-459-9906.

What are the ingredients in MIRAPEX ER?
Active Ingredient: pramipexole dihydrochloride monohydrate.
Inactive Ingredients: hypromellose, corn starch, carbomer homopolymer, colloidal silicon dioxide, and magnesium stearate.
What does MIRAPEX ER look like?
These pictures show what MIRAPEX ER tablets look like. Notice that each strength tablet looks different. Immediately call your pharmacist if you receive a MIRAPEX ER tablet that does not look like one of the tablets shown below, as you may have received the wrong medication.
| Tablets not actual size. | ||
| Strength | Front | Back |
| 0.375 mg |

|

|
| 0.75 mg |

|

|
| 1.5 mg |

|

|
| 2.25 mg |

|

|
| 3 mg |

|

|
| 3.75 mg |

|

|
| 4.5 mg |

|
|
This Patient Information has been approved by the U.S. Food and Drug Administration.
Distributed by:
Boehringer Ingelheim
Pharmaceuticals, Inc.
Ridgefield, CT 06877 USA
Licensed from:
Boehringer Ingelheim
International GmbH
Trademark
under license from:
Boehringer Ingelheim International
GmbH
Copyright ©2014 Boehringer
Ingelheim International GmbH
ALL RIGHTS RESERVED
Revised: May 2014
OT220011YE142014
74988-11
Mirapex ER Sample
0.375 mg Tablets
NDC 0597-0109-07
Mirapex ER
0.375 mg Tablets
NDC 0597-0109-30
Mirapex ER
0.75 mg Tablets
NDC 0597-0285-30
Mirapex ER
1.5 mg Tablets
NDC 0597-0113-30
Mirapex ER
2.25 mg Tablets
NDC 0597-0286-30
Mirapex ER
3.0 mg Tablets
NDC 0597-0115-30
Mirapex ER
3.75 mg Tablets
NDC 0597-0287-30
Mirapex ER
4.5 mg Tablets
NDC 0597-0116-30
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mirapexpramipexole dihydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||