Nplate
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use NPLATE safely and effectively. See full prescribing information for NPLATE. Nplate (romiplostim), for subcutaneous injection Initial U.S. Approval: 2008RECENT MAJOR CHANGES Dosage and Administration: Preparation and Administration (2.2) 05/2013 INDICATIONS AND USAGENplate is a thrombopoietin receptor agonist indicated for the treatment of thrombocytopenia in patients with chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.Limitations of Use: Nplate is not indicated for the treatment of thrombocytopenia due to myelodysplastic syndrome (MDS) or any cause of thrombocytopenia other than chronic ITP. Nplate should be used only in patients with ITP whose degree of thrombocytopenia and clinical condition increases the risk for bleeding. Nplate should not be used in an attempt to normalize platelet counts. (1) DOSAGE AND ADMINISTRATION Initial dose of 1 mcg/kg once weekly as a subcutaneous injection. (2.1) Adjust weekly dose by increments of 1 mcg/kg to achieve and maintain a platelet count ≥ 50 x 109/L as necessary to reduce the risk for bleeding. (2.1) Do not exceed the maximum weekly dose of 10 mcg/kg. Do not dose if platelet count is > 400 x 109/L. (2.1) Discontinue Nplate if platelet count does not increase after 4 weeks at the maximum dose. (2.1) Do not shake during reconstitution; protect reconstituted Nplate from light; administer reconstituted Nplate within 24 hours. (2.2) The injection volume may be very small. Use a syringe with graduations to 0.01 mL. (2.2) Discard any unused portion of the single-use vial. (2.2) DOSAGE FORMS AND STRENGTHS 250 mcg or 500 mcg of deliverable romiplostim in single-use vials (3) CONTRAINDICATIONS None (4) WARNINGS AND PRECAUTIONS In patients with MDS, Nplate increases blast cell counts and increases the risk of progression to acute myelogenous leukemia. (5.1) Thrombotic/thromboembolic complications may result from increases in platelet counts with Nplate use. Portal vein thrombosis has been reported in patients with chronic liver disease receiving Nplate. Use with additional caution in ITP patients with chronic liver disease. (5.2) Discontinuation of Nplate may result in worsened thrombocytopenia than was present prior to Nplate therapy. Monitor complete blood counts (CBCs), including platelet counts, for at least 2 weeks following Nplate discontinuation. (5.4) If severe thrombocytopenia develops during Nplate treatment, assess patients for the formation of neutralizing antibodies. (5.5) Side EffectsThe most common adverse reactions (≥ 5% higher patient incidence in Nplate versus placebo) are arthralgia, dizziness, insomnia, myalgia, pain in extremity, abdominal pain, shoulder pain, dyspepsia, and paresthesia. Headache was the most commonly reported adverse reaction that did not occur at ≥ 5% higher patient incidence in Nplate versus placebo. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Amgen Inc. at 1-800-77-AMGEN (1-800-772-6436) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, Nplate may cause fetal harm. (8.1) Nursing Mothers: A decision should be made to discontinue Nplate or nursing, taking into account the importance of Nplate to the mother. (8.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 NPLATE INDICATIONS AND USAGE
- 2 NPLATE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 NPLATE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Risk of Progression of Myelodysplastic Syndromes to Acute Myelogenous Leukemia
- 5.2 Thrombotic/Thromboembolic Complications
- 5.3 Bone Marrow Reticulin Formation and Risk for Bone Marrow Fibrosis
- 5.4 Worsened Thrombocytopenia after Cessation of Nplate
- 5.5 Lack or Loss of Response to Nplate
- 5.6 Laboratory Monitoring
- 6 NPLATE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 NPLATE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- MEDICATION GUIDE
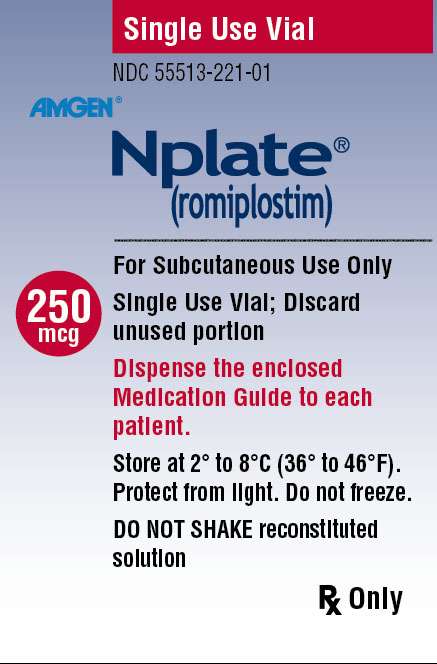
- PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - VIAL, 250 MCG
- PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - VIAL, 500 MCG
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Nplate is indicated for the treatment of thrombocytopenia in patients with chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins or splenectomy.
Limitations of use:
- Nplate is not indicated for the treatment of thrombocytopenia due to myelodysplastic syndrome (MDS) or any cause of thrombocytopenia other than chronic ITP [see Warnings and Precautions (5.1)].
- Nplate should be used only in patients with ITP whose degree of thrombocytopenia and clinical condition increases the risk for bleeding [see Warnings and Precautions (5.2)].
- Nplate should not be used in an attempt to normalize platelet counts [see Warnings and Precautions (5.2)].
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage Regimen
Use the lowest dose of Nplate to achieve and maintain a platelet count ≥ 50 x 109/L as necessary to reduce the risk for bleeding. Administer Nplate as a weekly subcutaneous injection with dose adjustments based upon the platelet count response.
The prescribed Nplate dose may consist of a very small volume (eg, 0.15 mL). Administer Nplate only with a syringe that contains 0.01 mL graduations.
Initial Dose
The initial dose for Nplate is 1 mcg/kg based on actual body weight.
Dose Adjustments
Use the actual body weight at initiation of therapy, then adjust the weekly dose of Nplate by increments of 1 mcg/kg until the patient achieves a platelet count ≥ 50 x 109/L as necessary to reduce the risk for bleeding; do not exceed a maximum weekly dose of 10 mcg/kg. In clinical studies, most patients who responded to Nplate achieved and maintained platelet counts ≥ 50 x 109/L with a median dose of 2 mcg/kg.
During Nplate therapy, assess CBCs, including platelet counts, weekly until a stable platelet count (≥ 50 x 109/L for at least 4 weeks without dose adjustment) has been achieved. Obtain CBCs, including platelet counts, monthly thereafter.
Adjust the dose as follows:
- If the platelet count is < 50 x 109/L, increase the dose by 1 mcg/kg.
- If platelet count is > 200 x 109/L for 2 consecutive weeks, reduce the dose by 1 mcg/kg.
- If platelet count is > 400 x 109/L, do not dose. Continue to assess the platelet count weekly. After the platelet count has fallen to < 200 x 109/L, resume Nplate at a dose reduced by 1 mcg/kg.
Discontinuation
Discontinue Nplate if the platelet count does not increase to a level sufficient to avoid clinically important bleeding after 4 weeks of Nplate therapy at the maximum weekly dose of 10 mcg/kg [see Warnings and Precautions (5.5)]. Obtain CBCs, including platelet counts, weekly for at least 2 weeks following discontinuation of Nplate [see Warnings and Precautions (5.6)].
2.2 Preparation and Administration
To mitigate against medication errors (both overdose and underdose), ensure that these preparation and administration instructions are followed.
Calculate the dose and reconstitute with the correct volume of sterile water for injection. Withdraw the appropriate volume of the calculated dose from the vial. Only administer subcutaneously [see Overdosage (10)].
Nplate is supplied in single-use vials as a sterile, preservative-free, white lyophilized powder that must be reconstituted as outlined in Table 1 and administered using a syringe with 0.01 mL graduations. Using aseptic technique, reconstitute Nplate with preservative-free Sterile Water for Injection, USP as described in Table 1. Do not use bacteriostatic water for injection.
| Nplate Single-Use Vial |
Total Vial Content of Nplate |
Sterile Water for Injection  |
Deliverable Product and Volume |
Final Concentration |
||
| 250 mcg | 375 mcg | add | 0.72 mL | = | 250 mcg in 0.5 mL | 500 mcg/mL |
| 500 mcg | 625 mcg | add | 1.2 mL | = | 500 mcg in 1 mL | 500 mcg/mL |
Gently swirl and invert the vial to reconstitute. Avoid excess or vigorous agitation: DO NOT SHAKE. Generally, dissolution of Nplate takes less than 2 minutes. The reconstituted Nplate solution should be clear and colorless. Visually inspect the reconstituted solution for particulate matter and/or discoloration. Do not administer Nplate if particulate matter and/or discoloration is observed.
Reconstituted Nplate can be kept at room temperature (25°C/77°F) or refrigerated at 2° to 8°C (36° to 46°F) for up to 24 hours prior to administration. Protect the reconstituted product from light.
To determine the injection volume to be administered, first identify the patient’s total dose in micrograms (mcg) using the dosing information in Section 2.1. For example, a 75 kg patient initiating therapy at 1 mcg/kg will begin with a dose of 75 mcg. Next, calculate the volume of Nplate solution that is given to the patient by dividing the microgram dose by the concentration of the reconstituted Nplate solution (500 mcg/mL). For this patient example, the 75 mcg dose is divided by 500 mcg/mL, resulting in an injection volume of 0.15 mL.
As the injection volume may be very small, use a syringe with graduations to 0.01 mL. Verify that the syringe contains the correct dosage.
Discard any unused portion. Do not pool unused portions from the vials. Do not administer more than one dose from a vial.
2.3 Use of Nplate With Concomitant Medical ITP Therapies
Nplate may be used with other medical ITP therapies, such as corticosteroids, danazol, azathioprine, intravenous immunoglobulin (IVIG), and anti-D immunoglobulin. If the patient’s platelet count is ≥ 50 x 109/L, medical ITP therapies may be reduced or discontinued [see Clinical Studies (14.1)].
3 DOSAGE FORMS AND STRENGTHS
Single-use vials contain 250 or 500 mcg of deliverable romiplostim as a sterile, lyophilized, solid white powder.
4 CONTRAINDICATIONS
None
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Progression of Myelodysplastic Syndromes to Acute Myelogenous Leukemia
Progression from myelodysplastic syndromes (MDS) to acute myelogenous leukemia (AML) has been observed in clinical trials with Nplate. A randomized, double-blind, placebo-controlled trial enrolling patients with severe thrombocytopenia and International Prognostic Scoring System (IPSS) low or intermediate-1 risk MDS was terminated due to more cases of AML observed in the Nplate treatment arm. At the time of an interim analysis, among 219 MDS patients randomized 2:1 to treatment with Nplate or placebo (147 Nplate: 72 placebo), 11 patients showed progression to AML, including nine on the Nplate arm versus two on the placebo arm. In addition, in peripheral blood counts, the percentage of circulating myeloblasts increased to greater than 10% in 28 patients, 25 of whom were in the romiplostim treatment arm. Of the 28 patients who had an increase in circulating myeloblasts to greater than 10%, eight of these patients were diagnosed to have AML and 20 patients had not progressed to AML. In four patients, increased peripheral blood blast cell counts decreased to baseline after discontinuation of Nplate. In a single-arm trial of Nplate given to 72 patients with thrombocytopenia related to MDS, eight (11%) patients were reported as having possible disease progression, and three patients had confirmation of AML during follow-up. In addition, in three patients, increased peripheral blood blast cell counts decreased to baseline after discontinuation of Nplate.
Nplate is not indicated for the treatment of thrombocytopenia due to MDS or any cause of thrombocytopenia other than chronic ITP.
5.2 Thrombotic/Thromboembolic Complications
Thrombotic/thromboembolic complications may result from increases in platelet counts with Nplate use. Portal vein thrombosis has been reported in patients with chronic liver disease receiving Nplate. Nplate should be used with caution in patients with ITP and chronic liver disease.
To minimize the risk for thrombotic/thromboembolic complications, do not use Nplate in an attempt to normalize platelet counts. Follow the dose adjustment guidelines to achieve and maintain a platelet count of ≥ 50 x 109/L [see Dosage and Administration (2.1)].
5.3 Bone Marrow Reticulin Formation and Risk for Bone Marrow Fibrosis
Nplate administration may increase the risk for development or progression of reticulin fiber formation within the bone marrow. This formation may improve upon discontinuation of Nplate. In a clinical trial, one patient with ITP and hemolytic anemia developed marrow fibrosis with collagen during Nplate therapy. Clinical trials are in progress to assess the risk of bone marrow fibrosis and clinical consequences with cytopenias.
If new or worsening morphological abnormalities or cytopenia(s) occur, consider a bone marrow biopsy to include staining for fibrosis [see Adverse Reactions ( 6.1 )].
5.4 Worsened Thrombocytopenia after Cessation of Nplate
In clinical studies of patients with chronic ITP who had Nplate discontinued, four of 57 patients developed thrombocytopenia of greater severity than was present prior to Nplate therapy. This worsened thrombocytopenia resolved within 14 days. Following discontinuation of Nplate, obtain weekly CBCs, including platelet counts, for at least 2 weeks and consider alternative treatments for worsening thrombocytopenia, according to current treatment guidelines [see Adverse Reactions (6.1)].
5.5 Lack or Loss of Response to Nplate
Hyporesponsiveness or failure to maintain a platelet response with Nplate should prompt a search for causative factors, including neutralizing antibodies to Nplate [see Adverse Reactions (6.3)]. To detect antibody formation, submit blood samples to Amgen (1-800-772-6436). Amgen will assay these samples for antibodies to Nplate and thrombopoietin (TPO). Discontinue Nplate if the platelet count does not increase to a level sufficient to avoid clinically important bleeding after 4 weeks at the highest weekly dose of 10 mcg/kg.
5.6 Laboratory Monitoring
Obtain CBCs, including platelet counts, weekly during the dose-adjustment phase of Nplate therapy and then monthly following establishment of a stable Nplate dose. Obtain CBCs, including platelet counts, weekly for at least 2 weeks following discontinuation of Nplate [see Dosage and Administration (2.1) and Warnings and Precautions (5.3, 5.4)].
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Serious adverse reactions associated with Nplate in ITP clinical studies were bone marrow reticulin deposition and worsening thrombocytopenia after Nplate discontinuation [see Warnings and Precautions (5.3, 5.4)].
The data described below reflect Nplate exposure to 271 patients with chronic ITP, aged 18 to 88, of whom 62% were female. Nplate was studied in two randomized, placebo-controlled, double-blind studies that were identical in design, with the exception that Study 1 evaluated nonsplenectomized patients with ITP and Study 2 evaluated splenectomized patients with ITP. Data are also reported from an open-label, single-arm study in which patients received Nplate over an extended period of time. Overall, Nplate was administered to 114 patients for at least 52 weeks and 53 patients for at least 96 weeks.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In the placebo-controlled studies, headache was the most commonly reported adverse drug reaction, occurring in 35% of patients receiving Nplate and 32% of patients receiving placebo. Headaches were usually of mild or moderate severity. Table 2 presents adverse drug reactions from Studies 1 and 2 with a ≥ 5% higher patient incidence in Nplate versus placebo. The majority of these adverse drug reactions were mild to moderate in severity.
| Preferred Term |
Nplate (n = 84) |
Placebo (n = 41) |
| Arthralgia | 26% | 20% |
| Dizziness | 17% | 0% |
| Insomnia | 16% | 7% |
| Myalgia | 14% | 2% |
| Pain in Extremity | 13% | 5% |
| Abdominal Pain | 11% | 0% |
| Shoulder Pain | 8% | 0% |
| Dyspepsia | 7% | 0% |
| Paresthesia | 6% | 0% |
Among 142 patients with chronic ITP who received Nplate in the single-arm extension study, the incidence rates of the adverse reactions occurred in a pattern similar to those reported in the placebo-controlled clinical studies.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of Nplate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Erythromelalgia
- Hypersensitivity
- Angioedema
6.3 Immunogenicity
As with all therapeutic proteins, patients may develop antibodies to the therapeutic protein. Patients were screened for immunogenicity to romiplostim using a BIAcore-based biosensor immunoassay. This assay is capable of detecting both high- and low-affinity binding antibodies that bind to romiplostim and cross-react with TPO. The samples from patients that tested positive for binding antibodies were further evaluated for neutralizing capacity using a cell-based bioassay.
In clinical studies, the incidence of preexisting antibodies to romiplostim was 8% (43/537) and the incidence of binding antibody development during Nplate treatment was 6% (31/537). The incidence of preexisting antibodies to endogenous TPO was 5% (29/537) and the incidence of binding antibody development to endogenous TPO during Nplate treatment was 4% (21/537). Of the patients with positive binding antibodies that developed to romiplostim or to TPO, two (0.4%) patients had neutralizing activity to romiplostim and none had neutralizing activity to TPO. No correlation was observed between antibody activity and clinical effectiveness or safety.
Immunogenicity assay results are highly dependent on the sensitivity and specificity of the assay used in detection and may be influenced by several factors, including sample handling, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to romiplostim with the incidence of antibodies to other products may be misleading.
7 DRUG INTERACTIONS
No formal drug interaction studies of Nplate have been performed.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies of Nplate use in pregnant women. In animal reproduction and developmental toxicity studies, romiplostim crossed the placenta, and adverse fetal effects included thrombocytosis, postimplantation loss, and an increase in pup mortality. Nplate should be used during pregnancy only if the potential benefit to the mother justifies the potential risk to the fetus.
Pregnancy Registry: A pregnancy registry has been established to collect information about the effects of Nplate use during pregnancy. Physicians are encouraged to register pregnant patients, or pregnant women may enroll themselves in the Nplate pregnancy registry by calling 1-800-77-AMGEN (1-800-772-6436).
In rat and rabbit developmental toxicity studies, no evidence of fetal harm was observed at romiplostim doses up to 11 times (rats) and 82 times (rabbits) the maximum human dose (MHD) based on systemic exposure. In mice at doses 5 times the MHD, reductions in maternal body weight and increased postimplantation loss occurred.
In a prenatal and postnatal development study in rats, at doses 11 times the MHD, there was an increase in perinatal pup mortality. Romiplostim crossed the placental barrier in rats and increased fetal platelet counts at clinically equivalent and higher doses.
8.3 Nursing Mothers
It is not known whether Nplate is excreted in human milk; however, human IgG is excreted in human milk. Published data suggest that breast milk antibodies do not enter the neonatal and infant circulation in substantial amounts. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Nplate, a decision should be made whether to discontinue nursing or to discontinue Nplate, taking into account the importance of Nplate to the mother and the known benefits of nursing.
8.4 Pediatric Use
The safety and effectiveness in pediatric patients (<18 years) have not been established.
8.5 Geriatric Use
Of the 271 patients who received Nplate in ITP clinical studies, 55 (20%) were age 65 and over, and 27 (10%) were 75 and over. No overall differences in safety or efficacy have been observed between older and younger patients in the placebo-controlled studies, but greater sensitivity of some older individuals cannot be ruled out. In general, dose adjustment for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
No clinical studies were conducted in patients with renal impairment. Use Nplate with caution in this population.
8.7 Hepatic Impairment
No clinical studies were conducted in patients with hepatic impairment. Use Nplate with caution in this population.
10 OVERDOSAGE
Overdoses due to medication errors have been reported in patients receiving Nplate. In the event of overdose, platelet counts may increase excessively and result in thrombotic/thromboembolic complications. In this case, discontinue Nplate and monitor platelet counts. Reinitiate treatment with Nplate in accordance with dosing and administration recommendations [see Dosage and Administration (2.1, 2.2)].
11 DESCRIPTION
Romiplostim, a member of the TPO mimetic class, is an Fc-peptide fusion protein (peptibody) that activates intracellular transcriptional pathways leading to increased platelet production via the TPO receptor (also known as cMpl). The peptibody molecule contains two identical single-chain subunits, each consisting of human immunoglobulin IgG1 Fc domain, covalently linked at the C-terminus to a peptide containing two thrombopoietin receptor-binding domains. Romiplostim has no amino acid sequence homology to endogenous TPO. Romiplostim is produced by recombinant DNA technology in Escherichia coli (E coli).
Nplate is supplied as a sterile, preservative-free, lyophilized, solid white powder for subcutaneous injection. Two vial presentations are available, which contain a sufficient amount of active ingredient to provide either 250 mcg or 500 mcg of deliverable romiplostim, respectively. Each single-use 250 mcg vial of Nplate contains the following: 375 mcg romiplostim, 30 mg mannitol, 15 mg sucrose, 1.2 mg L-histidine, 0.03 mg polysorbate 20, and sufficient HCl to adjust the pH to a target of 5.0. Each single-use 500 mcg vial of Nplate contains the following: 625 mcg romiplostim, 50 mg mannitol, 25 mg sucrose, 1.9 mg L-histidine, 0.05 mg polysorbate 20, and sufficient HCl to adjust the pH to a target of 5.0 [see Dosage and Administration (2.2)].
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Nplate increases platelet production through binding and activation of the TPO receptor, a mechanism analogous to endogenous TPO.
12.2 Pharmacodynamics
In clinical studies, treatment with Nplate resulted in dose-dependent increases in platelet counts. After a single subcutaneous dose of 1 to 10 mcg/kg Nplate in patients with chronic ITP, the peak platelet count was 1.3 to 14.9 times greater than the baseline platelet count over a 2- to 3-week period. The platelet counts were above 50 x 109/L for seven out of eight patients with chronic ITP who received six weekly doses of Nplate at 1 mcg/kg.
12.3 Pharmacokinetics
In the long-term extension study in patients with ITP receiving weekly treatment of Nplate subcutaneously, the pharmacokinetics of romiplostim over the dose range of 3 to 15 mcg/kg indicated that peak serum concentrations of romiplostim were observed about 7 to 50 hours post dose (median: 14 hours) with half-life values ranging from 1 to 34 days (median: 3.5 days). The serum concentrations varied among patients and did not correlate with the dose administered. The elimination of serum romiplostim is in part dependent on the TPO receptor on platelets. As a result, for a given dose, patients with high platelet counts are associated with low serum concentrations and vice versa. In another ITP clinical study, no accumulation in serum concentrations was observed (n = 4) after six weekly doses of Nplate (3 mcg/kg). The accumulation at higher doses of romiplostim is unknown.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of romiplostim has not been evaluated. The mutagenic potential of romiplostim has not been evaluated. Romiplostim had no effect on the fertility of rats at doses up to 37 times the MHD based on systemic exposure.
13.2 Animal Toxicology and/or Pharmacology
In a 4-week repeat-dose toxicity study in which rats were dosed subcutaneously three times per week, romiplostim caused extramedullary hematopoiesis, bone hyperostosis, and marrow fibrosis at clinically equivalent and higher doses. In this study, these findings were not observed in animals after a 4-week post treatment recovery period. Studies of long-term treatment with romiplostim in rats have not been conducted; therefore, it is not known if the fibrosis of the bone marrow is reversible in rats after long-term treatment.
14 CLINICAL STUDIES
14.1 Chronic ITP
The safety and efficacy of Nplate were assessed in two double-blind, placebo-controlled clinical studies and in an open-label extension study.
Studies 1 and 2
In Studies 1 and 2, patients with chronic ITP who had completed at least one prior treatment and had a platelet count of ≤ 30 x 109/L prior to study entry were randomized (2:1) to 24 weeks of Nplate (1 mcg/kg subcutaneous [SC]) or placebo. Prior ITP treatments in both study groups included corticosteroids, immunoglobulins, rituximab, cytotoxic therapies, danazol, and azathioprine. Patients already receiving ITP medical therapies at a constant dosing schedule were allowed to continue receiving these medical treatments throughout the studies. Rescue therapies (ie, corticosteroids, IVIG, platelet transfusions, and anti-D immunoglobulin) were permitted for bleeding, wet purpura, or if the patient was at immediate risk for hemorrhage. Patients received single weekly SC injections of Nplate, with individual dose adjustments to maintain platelet counts (50 x 109/L to 200 x 109/L).
Study 1 evaluated patients who had not undergone a splenectomy. The patients had been diagnosed with ITP for approximately 2 years and had received a median of three prior ITP treatments. Overall, the median platelet count was 19 x 109/L at study entry. During the study, the median weekly Nplate dose was 2 mcg/kg (25th–75th percentile: 1–3 mcg/kg).
Study 2 evaluated patients who had undergone a splenectomy. The patients had been diagnosed with ITP for approximately 8 years and had received a median of six prior ITP treatments. Overall, the median platelet count was 14 x 109/L at study entry. During the study, the median weekly Nplate dose was 3 mcg/kg (25th–75th percentile: 2–7 mcg/kg).
Study 1 and 2 outcomes are shown in Table 3. A durable platelet response was the achievement of a weekly platelet count ≥ 50 x 109/L for any 6 of the last 8 weeks of the 24-week treatment period in the absence of rescue medication at any time. A transient platelet response was the achievement of any weekly platelet counts ≥ 50 x 109/L for any 4 weeks during the treatment period without a durable platelet response. An overall platelet response was the achievement of either a durable or a transient platelet response. Platelet responses were excluded for 8 weeks after receiving rescue medications.
| Outcomes |
Study 1 |
Study 2 |
||
| Nplate (n = 41) |
Placebo (n = 21) |
Nplate (n = 42) |
Placebo (n = 21) |
|
| Platelet Responses and Rescue Therapy | ||||
| Durable Platelet Response, n (%) | 25 (61%) | 1 (5%) | 16 (38%) | 0 (0%) |
| Overall Platelet Response, n (%) | 36 (88%) | 3 (14%) | 33 (79%) | 0 (0%) |
| Number of Weeks With Platelet Counts ≥ 50 x 109/L, average | 15 | 1 | 12 | 0 |
| Requiring Rescue Therapy, n (%) | 8 (20%) | 13 (62%) | 11 (26%) | 12 (57%) |
| Reduction/Discontinuation of Baseline Concurrent ITP Medical Therapy | ||||
| Receiving Therapy at Baseline | (n = 11) | (n = 10) | (n = 12) | (n = 6) |
| Patients Who Had > 25% Dose Reduction in Concurrent Therapy, n (%) | 4/11 (36%) | 2/10 (20%) | 4/12 (33%) | 1/6 (17%) |
Patients Who Discontinued Baseline Therapy, n (%)
 |
4/11 (36%) | 3/10 (30%) | 8/12 (67%) | 0/6 (0%) |
In Studies 1 and 2, nine patients reported a serious bleeding event [five (6%) Nplate, four (10%) placebo]. Bleeding events that were grade 2 severity or higher occurred in 15% of patients treated with Nplate and 34% of patients treated with placebo.
Extension Study
Patients who had participated in either Study 1 or Study 2 were withdrawn from study medications. If platelet counts subsequently decreased to ≤ 50 x 109/L, the patients were allowed to receive Nplate in an open-label extension study with weekly dosing based on platelet counts. Following Nplate discontinuation in Studies 1 and 2, seven patients maintained platelet counts of ≥ 50 x 109/L. Among 100 patients who subsequently entered the extension study, platelet counts were increased and sustained regardless of whether they had received Nplate or placebo in the prior placebo-controlled studies. The majority of patients reached a median platelet count of 50 x 109/L after receiving one to three doses of Nplate, and these platelet counts were maintained throughout the remainder of the study with a median duration of Nplate treatment of 60 weeks and a maximum duration of 96 weeks.
16 HOW SUPPLIED/STORAGE AND HANDLING
Nplate is supplied in single-use vials containing 250 mcg (NDC 55513-221-01) and 500 mcg (NDC 55513-222-01) deliverable romiplostim.
Store Nplate vials in their carton to protect from light until time of use. Keep Nplate vials refrigerated at 2° to 8°C (36° to 46°F). Do not freeze.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Medication Guide.
17.1 Information for Patients
Prior to treatment, patients should fully understand the risks and benefits of Nplate. Inform patients that the risks associated with long-term administration of Nplate are unknown.
Inform patients of the following risks and considerations for Nplate:
- Nplate therapy is administered to achieve and maintain a platelet count ≥ 50 x 109/L as necessary to reduce the risk for bleeding; Nplate is not used to normalize platelet counts.
- Following discontinuation of Nplate, thrombocytopenia and risk of bleeding may develop that is worse than that experienced prior to the Nplate therapy.
- Nplate therapy may increase the risk of reticulin fiber formation within the bone marrow. This formation may improve upon discontinuation. Detection of peripheral blood cell abnormalities may necessitate a bone marrow examination.
- Too much Nplate may result in excessive platelet counts and a risk for thrombotic/thromboembolic complications.
- Nplate stimulates certain bone marrow cells to make platelets and increases the risk of progression to acute myelogenous leukemia in patients with myelodysplastic syndromes.
- Platelet counts and CBCs must be performed weekly until a stable Nplate dose has been achieved; thereafter, platelet counts and CBCs, must be performed monthly while taking Nplate.
- Patients must be closely monitored with weekly platelet counts and CBCs for at least 2 weeks following Nplate discontinuation.
- Even with Nplate therapy, patients should continue to avoid situations or medications that may increase the risk for bleeding.
[Amgen logo]
Nplate® (romiplostim)
Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, California 91320-1799
This product, its production, and/or its use may be covered by one or more U.S. Patents, including U.S. Patent Nos. 6,835,809, 7,189,827, 7,994,117, and 8,044,174, as well as other patents or patents pending.
© 2008-2013 Amgen Inc. All rights reserved.
www.nplate.com
1xxxxx
v8
PMV 8
MEDICATION GUIDE
Nplate®
(N-plāt)
(romiplostim)
Read this Medication Guide before you start Nplate and before each Nplate injection. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about Nplate?
Nplate can cause serious side effects:
- Worsening of a precancerous blood condition to a blood cancer (leukemia). Nplate is not for use in people with a precancerous condition called myelodysplastic syndromes (MDS) or for any condition other than chronic (lasting a long time) immune thrombocytopenia (ITP). If you have MDS and receive Nplate, your MDS condition may worsen and become an acute leukemia. If MDS worsens to become acute leukemia you may die sooner from the acute leukemia.
-
Higher risk for blood clots.
- You may have a higher risk of getting a blood clot if your platelet count becomes high during treatment with Nplate. You may have severe complications or die from some forms of blood clots, such as clots that spread to the lungs or that cause heart attacks or strokes. Your healthcare provider will check your blood platelet counts and change your dose or stop Nplate if your platelet counts get high.
- If you have a chronic liver disease, you may get blood clots in the veins of your liver. This may affect your liver function.
- Bone marrow changes (increased reticulin and possible bone marrow fibrosis). Nplate may cause changes in your bone marrow, but these changes may improve if you stop taking Nplate. These changes may lead to abnormal blood cells or your body making less blood cells. The mild form of these bone marrow changes is called “increased reticulin.” It is not known if this may progress to a more severe form called “fibrosis.” The mild form may cause no problems while the severe form may cause life-threatening blood problems. Signs of bone marrow changes may show up as abnormalities in your blood tests. Your healthcare provider will decide if abnormal blood tests mean that you should have bone marrow tests or if you should stop taking Nplate.
- Worsening low blood platelet count (thrombocytopenia) and risk of bleeding shortly after stopping Nplate. When you stop receiving Nplate, your low blood platelet count (thrombocytopenia) may become worse than before you started receiving Nplate. These effects are most likely to happen shortly after stopping Nplate and may last about 2 weeks. The lower platelet counts during this time period may increase your risk of bleeding, especially if you are taking a blood thinner or other medicine that affects platelets. Your healthcare provider will check your blood platelet counts for at least two weeks after you stop taking Nplate. Call your healthcare provider right away to report any bruising or bleeding.
When you are being treated with Nplate, your healthcare provider will closely monitor your Nplate dose and blood tests, including platelet counts.
- Injection of too much Nplate may cause a dangerous increase in your blood platelet count and serious side effects.
- During Nplate therapy, your healthcare provider may change your Nplate dose, depending upon the change in your blood platelet count. You must have blood platelet counts done before you start Nplate, during Nplate therapy, and after Nplate therapy is stopped.
See “What are the possible side effects of Nplate?” for other side effects of Nplate.
What is Nplate?
Nplate is a man-made protein medicine used to treat low blood platelet counts in adults with chronic immune thrombocytopenia (ITP), when certain other medicines, or surgery to remove your spleen, have not worked well enough.
Nplate is not for use in people with a precancerous condition called myelodysplastic syndrome (MDS) or low platelet count caused by any condition other than chronic (lasting a long time) immune thrombocytopenia (ITP).
Nplate is only used if your low platelet count and medical condition increase your risk of bleeding.
Nplate is used to try to keep your platelet count about 50,000 per microliter in order to lower the risk for bleeding. Nplate is not used to make your platelet count normal.
It is not known if Nplate works or if it is safe in people under the age of 18.
What should I tell my healthcare provider before taking Nplate?
Tell your healthcare provider about all your medical conditions, including if you:
- Have had surgery to remove your spleen (splenectomy).
- Have a bone marrow problem, including a blood cancer or MDS.
- Have or had a blood clot.
- Have chronic liver disease.
- Have bleeding problems.
- Have any other medical condition.
- Are pregnant, or plan to become pregnant. It is not known if Nplate will harm your unborn baby.
Pregnancy Registry: There is a registry for women who become pregnant during treatment with Nplate. If you become pregnant, consider this registry. The purpose of the registry is to collect safety information about the health of you and your baby. Contact the registry as soon as you become aware of the pregnancy, or ask your healthcare provider to contact the registry for you. You or your healthcare provider can get information and enroll in the registry by calling 1-800-77-AMGEN (1-800-772-6436).
- Are breast-feeding or plan to breast-feed. It is not known if Nplate passes into your breast milk. You and your healthcare provider should decide whether you will take Nplate or breast-feed. You should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal products. Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take Nplate?
Before you receive Nplate you should first talk with your healthcare provider and understand the benefits and risks of Nplate.
- Nplate is given as a subcutaneous (SC) injection under the skin one time each week. You may not give Nplate injections to yourself.
Your healthcare provider will check your platelet count every week and change your dose of Nplate as needed. This will continue until your healthcare provider decides that your dose of Nplate can stay the same. After that, you will need to have blood tests every month. When you stop receiving Nplate, you will need blood tests for at least 2 weeks to check if your platelet count drops too low.
Tell your healthcare provider about any bruising or bleeding that occurs while you are receiving Nplate.
If you miss a scheduled dose of Nplate, call your healthcare provider to arrange for your next dose as soon as possible.
What should I avoid while receiving Nplate?
Avoid situations that may increase your risk of bleeding, such as missing a scheduled dose of Nplate. You should arrange for your next dose as soon as possible and call your healthcare provider.
What are the possible side effects of Nplate?
Nplate may cause serious side effects. See “What is the most important information I should know about Nplate?”
The most common side effects of Nplate are:
|
|
These are not all the possible side effects of Nplate. Tell your healthcare provider if you have any side effect that bothers you or that does not go away. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
You may also report side effects to Amgen at 1-800-77-AMGEN (1-800-772-6436).
General information about the safe and effective use of Nplate.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. This Medication Guide summarizes the most important information about Nplate. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about Nplate that is written for health professionals.
What are the ingredients in Nplate?
Active ingredient: romiplostim
Inactive ingredients: L-histidine, sucrose, mannitol, polysorbate 20, and hydrochloric acid
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Nplate® (romiplostim)
Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, California 91320-1799
Revised: 12/2011
This product, its production, and/or its use may be covered by one or more U.S. Patents, including U.S. Patent Nos. 6,835,809, 7,189,827, 7,994,117 and 8,044,174, as well as other patents or patents pending.
© 2008-2011 Amgen Inc. All rights reserved.
www.nplate.com
1xxxxxx
v3
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - VIAL, 250 MCG
Single Use Vial
NDC 55513-221-01
Amgen®
Nplate®
(romiplostim)
250 mcg
For Subcutaneous Use Only
Single Use Vial; Discard unused portion
Dispense the enclosed Medication Guide to each patient.
Store at 2° to 8°C (36° to 46°F).
Protect from light. Do not freeze.
DO NOT SHAKE reconstituted solution
Rx Only
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - VIAL, 500 MCG
Single Use Vial
NDC 55513-222-01
Amgen®
Nplate®
(romiplostim)
500 mcg
For Subcutaneous Use Only
Single Use Vial; Discard unused portion
Dispense the enclosed Medication Guide to each patient.
Store at 2° to 8°C (36° to 46°F).
Protect from light. Do not freeze.
DO NOT SHAKE reconstituted solution
Rx Only

Nplateromiplostim INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Nplateromiplostim INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||