Nucynta
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use NUCYNTA safely and effectively. See full prescribing information for NUCYNTA. NUCYNTA (tapentadol) oral solution C-IIInitial U.S. Approval: 2008INDICATIONS AND USAGENUCYNTA® is an opioid analgesic indicated for the management of moderate to severe acute pain in adults.DOSAGE AND ADMINISTRATION Individualize dosing according to the severity of pain being treated, the previous experience with similar drugs and the ability to monitor the patient. (2.1) Initiate NUCYNTA® with or without food at a dose of 2.5 mL (50 mg), 3.75 mL (75 mg), or 5 mL (100 mg) every 4 to 6 hours depending upon pain intensity. On the first day of dosing, the second dose may be administered as soon as one hour after the first dose, if adequate pain relief is not attained with the first dose. Subsequent dosing is 2.5 mL (50 mg), 3.75 mL (75 mg), or 5 mL (100 mg) every 4 to 6 hours and should be adjusted to maintain adequate analgesia with acceptable tolerability. Daily doses greater than 700 mg on the first day of therapy and 600 mg on subsequent days have not been studied and are, therefore, not recommended. (2.2) Instructions for Use (2.7) DOSAGE FORMS AND STRENGTHSOral Solution: 20 mg/mLCONTRAINDICATIONS Significant respiratory depression (4) Acute or severe bronchial asthma, hypercarbia (4) Known or suspected paralytic ileus (4) Hypersensitivity to tapentadol or to any other ingredients of the product (4) Concurrent use of monoamine oxidase (MAO) inhibitors or use within the last 14 days. (4) WARNINGS AND PRECAUTIONS Misuse, Abuse and Diversion: NUCYNTA® is a Schedule II controlled substance with abuse liability similar to other opioids: monitor patients closely for signs of misuse, abuse and addiction. (5.1) Elderly, cachectic, and debilitated patients and patients with chronic pulmonary disease: Monitor closely because of increased risk of respiratory depression. (5.5) Interaction with CNS depressants including other opioids, sedatives, alcohol, and illicit drugs: Consider dose reduction of one or both drugs because of additive effects. (5.7) Hypotensive effect: Monitor for signs of hypotension. (5.8) Patients with head injury or increased intracranial pressure: Monitor for sedation and respiratory depression. Avoid use of NUCYNTA® in patients with impaired consciousness or coma susceptible to intracranial effects of CO2 retention. (5.9) Impaired mental/physical abilities: Caution must be used with potentially hazardous activities. (5.14) Seizures: Use with caution in patients with a history of seizures. (5.10) Serotonin Syndrome: Potentially life-threatening condition could result from concomitant serotonergic administration. (5.11) Withdrawal: Withdrawal symptoms may occur if NUCYNTA® is discontinued abruptly. (5.13) Side EffectsThe most common (≥10%) adverse reactions were nausea, dizziness, vomiting and somnolence. To report SUSPECTED ADVERSE REACTIONS, contact Janssen Pharmaceuticals, Inc. at 1-800-526-7736 (1-800-JANSSEN) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONS CNS depressants: Increased risk of respiratory depression, hypotension, profound sedation, coma or death. When combined therapy with CNS depressant is contemplated, the dose of one or both agents should be reduced. (7.3) Mixed agonist/antagonist opioids (i.e., pentazocine, nalbuphine, and butorphanol): May reduce analgesic effect and/or precipitate withdrawal symptoms. (7.5) Monitor for signs of serotonin syndrome when NUCYNTA® is used concurrently with SSRIs, SNRIs, tricyclic antidepressants, or triptans. (7.4) USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, may cause fetal harm. (8.1) Nursing mothers: Closely monitor infants of nursing women receiving. NUCYNTA®. (8.3) Renal or hepatic impairment: not recommended in patients with severe renal or hepatic impairment. Reduce dose in patients with moderate hepatic impairment. (8.7, 8.8)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 NUCYNTA INDICATIONS AND USAGE
- 2 NUCYNTA DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 NUCYNTA CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Abuse Potential
- 5.2 Life Threatening Respiratory Depression
- 5.3 Accidental Exposure
- 5.4 Interactions with Alcohol, Other Opioids, and Drugs of Abuse
- 5.5 Elderly, Cachectic, and Debilitated Patients
- 5.6 Use in Patients with Chronic Pulmonary Disease
- 5.7 Interactions with CNS Depressants and Illicit Drugs
- 5.8 Hypotensive Effect
- 5.9 Use in Patients with Head Injury or Increased Intracranial Pressure
- 5.10 Seizures
- 5.11 Serotonin Syndrome Risk
- 5.12 Use in Patients with Gastrointestinal Conditions
- 5.13 Withdrawal
- 5.14 Driving and Operating Heavy Machinery
- 5.15 Hepatic Impairment
- 5.16 Renal Impairment
- 6 NUCYNTA ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 NUCYNTA DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NON-CLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PRINCIPAL DISPLAY PANEL - 100 mL Bottle Label
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
NUCYNTA® (tapentadol) is indicated for the management of moderate to severe acute pain in adults.
2 DOSAGE AND ADMINISTRATION
NUCYNTA® oral solution is available in one concentration: 20 mg/mL.
Take care when prescribing and administering NUCYNTA® oral solution to avoid dosing errors, which could result in accidental overdose and death. Take care to ensure the proper dose is communicated and dispensed. Include the dose in milliliters (mL) and milligrams (mg) when writing prescriptions. Always use the enclosed calibrated oral syringe when administering NUCYNTA® oral solution to ensure the dose is measured and administered accurately.
2.1 Individualization of Dosage
As with any opioid drug product, adjust the dosing regimen for each patient individually, taking into account the patient's prior analgesic treatment experience. In the selection of the initial dose of tapentadol, give attention to the following:
- the total daily dose, potency and specific characteristics of the opioid the patient has been taking previously;
- the reliability of the relative potency estimate used to calculate the equivalent morphine sulfate dose needed;
- the patient's degree of opioid tolerance;
- the general condition and medical status of the patient;
- concurrent medications;
- the type and severity of the patient's pain;
- risk factors for abuse, addiction or diversion, including a prior history of abuse, addiction or diversion.
The following dosing recommendations, therefore, can only be considered suggested approaches to what is actually a series of clinical decisions over time in the management of the pain of each individual patient. Continual re-evaluation of the patient receiving tapentadol is important, with special attention to the maintenance of pain control and the relative incidence of side effects associated with therapy. During chronic therapy, especially for non-cancer-related pain, periodically re-assess the continued need for the use of opioid analgesics.
During periods of changing analgesic requirements, including initial titration, frequent contact is recommended between physician, other members of the healthcare team, the patient, and the caregiver/family.
2.2 Initiation of Therapy
The dose is 2.5 mL (equivalent to 50 mg), 3.75 mL (equivalent to 75 mg), or 5 mL (equivalent to 100 mg) every 4 to 6 hours depending upon pain intensity.
On the first day of dosing, the second dose may be administered as soon as one hour after the first dose, if adequate pain relief is not attained with the first dose. Subsequent dosing is 2.5 mL (equivalent to 50 mg), 3.75 mL (equivalent to 75 mg), or 5 mL (equivalent to 100 mg) every 4 to 6 hours and should be adjusted to maintain adequate analgesia with acceptable tolerability.
Daily doses greater than 700 mg on the first day of therapy and 600 mg on subsequent days have not been studied and are not recommended.
NUCYNTA® may be given with or without food [see Clinical Pharmacology (12.3)].
2.3 Renal Impairment
No dosage adjustment is recommended in patients with mild or moderate renal impairment.
NUCYNTA® use in patients with severe renal impairment is not recommended [see Warnings and Precautions (5.16) and Clinical Pharmacology (12.3).
2.4 Hepatic Impairment
No dosage adjustment is recommended in patients with mild hepatic impairment [see Clinical Pharmacology (12.3)].
NUCYNTA® should be used with caution in patients with moderate hepatic impairment. Treatment in these patients should be initiated at 50 mg administered no more frequently than once every 8 hours (maximum of three doses in 24 hours). Further treatment should reflect maintenance of analgesia with acceptable tolerability, to be achieved by either shortening or lengthening the dosing interval [see Clinical Pharmacology (12.3)].
The safety and efficacy of NUCYNTA® has not been studied in patients with severe hepatic impairment and use in this population is not recommended [see Warnings and Precautions (5.15)].
2.5 Elderly Patients
In general, recommended dosing for elderly patients with normal renal and hepatic function is the same as for younger adult patients with normal renal and hepatic function. Because elderly patients are more likely to have decreased renal and hepatic function, consideration should be given to starting elderly patients with the lower range of recommended doses.
2.6 Cessation of Therapy
When the patient no longer requires therapy with tapentadol, gradually taper the dose to prevent signs and symptoms of withdrawal in the physically dependent patient [see Warnings and Precautions (5.13)].
2.7 Instructions for Use
Concentration and Dispensing: The oral solution contains 20 mg tapentadol per milliliter (mL) and prescriptions should be written in milliliters (mL) and milligrams (mg). An oral syringe is supplied with dose marks corresponding directly to 2.5 mL (equals 50 mg) oral solution, 3.75 mL (equals 75 mg) oral solution, and 5 mL (equals 100 mg) oral solution.
Inform patients of the availability of FDA-approved patient labeling, Instructions for Use, for step-by-step instructions for patients on how to use the medicine bottle and the oral syringe.
3 DOSAGE FORMS AND STRENGTHS
NUCYNTA® oral solution: 20 mg/mL oral solution in 100 mL and 200 mL fill bottles with child-resistant closure [see Description (11) and How Supplied/Storage and Handling (16)].
4 CONTRAINDICATIONS
NUCYNTA® is contraindicated in:
- Patients with significant respiratory depression
- Patients with acute or severe bronchial asthma or hypercarbia in an unmonitored setting or in the absence of resuscitative equipment
- Patients with known or suspected paralytic ileus
- Patients with hypersensitivity (e.g. anaphylaxis, angioedema) to tapentadol or to any other ingredients of the product [see Adverse Reactions (6.2)].
- Patients who are receiving monoamine oxidase (MAO) inhibitors or who have taken them within the last 14 days due to potential additive effects on norepinephrine levels which may result in adverse cardiovascular events [see Drug Interactions (7.2)].
5 WARNINGS AND PRECAUTIONS
5.1 Abuse Potential
NUCYNTA® contains tapentadol, an opioid agonist and a Schedule II controlled substance. Tapentadol can be abused in a manner similar to other opioid agonists legal or illicit. Opioid agonists are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing NUCYNTA® in situations where there is concern about increased risks of misuse, abuse, or diversion. Concerns about abuse, addiction, and diversion should not, however, prevent the proper management of pain.
Assess each patient's risk for opioid abuse or addiction prior to prescribing NUCYNTA®. The risk for opioid abuse is increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). Patients at increased risk may still be appropriately treated with modified-release opioid formulations; however these patients will require intensive monitoring for signs of misuse, abuse, or addiction. Routinely monitor all patients receiving opioids for signs of misuse, abuse, and addiction because these drugs carry a risk for addiction even under appropriate medical use.
Misuse or abuse of NUCYNTA® by injecting the oral solution will pose a significant risk that could result in overdose and death [see Overdosage (10)].
Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product [see Drug Abuse and Dependence (9)].
5.2 Life Threatening Respiratory Depression
Respiratory depression is the chief hazard of opioid agonists, including NUCYNTA®. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Respiratory depression from opioids is manifested by a reduced urge to breathe and a decreased rate of respiration, often associated with a "sighing" pattern of breathing (deep breaths separated by abnormally long pauses). Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient's clinical status [see Overdosage (10)].
Instruct patients against use by individuals other than the patient for whom NUCYNTA® was prescribed and to keep NUCYNTA® out of the reach of children, as such inappropriate use may result in fatal respiratory depression.
Patients with conditions accompanied by hypoxia, hypercarbia or decreased respiratory reserve such as: asthma, chronic obstructive pulmonary disease or cor pulmonale, central nervous system (CNS) depression, or coma may be at increased risk for increased airway resistance and decreased respiratory drive to the point of apnea even with usual therapeutic doses of NUCYNTA®. Consider the use of alternative non-mu-opioid agonist analgesics and use NUCYNTA® only under careful medical supervision at the lowest effective dose in such patients. If respiratory depression occurs, treat the patient for mu-opioid agonist-induced respiratory depression [see Overdosage (10)]. To reduce the risk of respiratory depression, proper dosing of NUCYNTA® is essential [see Dosage and Administration (2)].
5.3 Accidental Exposure
Accidental ingestion of NUCYNTA®, especially in children, can result in a fatal overdose of tapentadol.
5.4 Interactions with Alcohol, Other Opioids, and Drugs of Abuse
Due to its mu-opioid agonist activity, NUCYNTA® may be expected to have additive effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression, respiratory depression, hypotension, and profound sedation, coma or death [see Drug Interactions (7.3)]. Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products containing alcohol, other opioids, or drugs of abuse while on NUCYNTA® therapy [see Drug Interactions (7.1)].
5.5 Elderly, Cachectic, and Debilitated Patients
Respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients. Therefore, closely monitor such patients, particularly when NUCYNTA® is given concomitantly with other drugs that depress respiration [see Warnings and Precautions (5.2)].
5.6 Use in Patients with Chronic Pulmonary Disease
Monitor for respiratory depression those patients with significant chronic obstructive pulmonary disease or cor pulmonale, and patients having a substantially decreased respiratory reserve, hypoxia, hypercarbia, or pre-existing respiratory depression, as in these patients, even usual therapeutic doses of NUCYNTA® may decrease respiratory drive to the point of apnea [see Warnings and Precautions (5.2)]. Consider the use of alternative non-opioid analgesics in these patients if possible.
5.7 Interactions with CNS Depressants and Illicit Drugs
Hypotension, and profound sedation, coma or respiratory depression may result if NUCYNTA® is used concomitantly with other CNS depressants (e.g., sedatives, anxiolytics, hypnotics, neuroleptics, muscle relaxants, other opioids and illicit drugs). When considering the use of NUCYNTA® in a patient taking a CNS depressant, assess the duration of use of the CNS depressant and the patient's response, including the degree of tolerance that has developed to CNS depression. Additionally, consider the patient's use, if any, of alcohol and/or illicit drugs that can cause CNS depression. If NUCYNTA® therapy is to be initiated in a patient taking a CNS depressant, start with a lower NUCYNTA® dose than usual and monitor patients for signs of sedation and respiratory depression and consider using a lower dose of the concomitant CNS depressant [see Drug Interactions (7.3) ].
5.8 Hypotensive Effect
NUCYNTA® may cause severe hypotension. There is an increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions (7.3)]. Monitor these patients for signs of hypotension after the dose of NUCYNTA®. In patients with circulatory shock, NUCYNTA® may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of NUCYNTA® in patients with circulatory shock.
5.9 Use in Patients with Head Injury or Increased Intracranial Pressure
Monitor patients taking NUCYNTA® who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors) for signs of sedation and respiratory depression. NUCYNTA® may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Opioids may also obscure the clinical course in a patient with a head injury.
Avoid the use of NUCYNTA® in patients with impaired consciousness or coma.
5.10 Seizures
NUCYNTA® has not been evaluated in patients with a predisposition to a seizure disorder, and such patients were excluded from clinical studies. The active ingredient tapentadol in NUCYNTA® may aggravate convulsions in patients with convulsive disorders, and may induce or aggravate seizures in some clinical settings. Monitor patients with a history of seizure disorders for worsened seizure control during NUCYNTA® therapy.
5.11 Serotonin Syndrome Risk
Cases of life-threatening serotonin syndrome have been reported with the concurrent use of tapentadol and serotonergic drugs. Serotonergic drugs comprise Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, drugs that affect the serotonergic neurotransmitter system (e.g. mirtazapine, trazodone, and tramadol), and drugs that impair metabolism of serotonin (including MAOIs). This may occur within the recommended dose. Serotonin syndrome may include mental-status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination) and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea) and can be fatal [see Serotonergic Drugs (7.4)].
5.12 Use in Patients with Gastrointestinal Conditions
NUCYNTA® is contraindicated in patients with GI obstruction, including paralytic ileus. The tapentadol in NUCYNTA® may cause spasm of the sphincter of Oddi. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
5.13 Withdrawal
Withdrawal symptoms may occur if NUCYNTA® is discontinued abruptly. These symptoms may include: anxiety, sweating, insomnia, rigors, pain, nausea, tremors, diarrhea, upper respiratory symptoms, piloerection, and rarely, hallucinations. Withdrawal symptoms may be reduced by tapering NUCYNTA® [see Dependence (9.3)].
5.14 Driving and Operating Heavy Machinery
NUCYNTA® may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of NUCYNTA® and know how they will react to the medication.
5.15 Hepatic Impairment
A study with NUCYNTA® in subjects with hepatic impairment showed higher serum concentrations of tapentadol than in those with normal hepatic function. Avoid use of NUCYNTA® in patients with severe hepatic impairment. Reduce the dose of NUCYNTA® in patients with moderate hepatic impairment [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)]. Closely monitor patients with moderate hepatic impairment for respiratory and central nervous system depression when receiving NUCYNTA®.
5.16 Renal Impairment
Use of NUCYNTA® in patients with severe renal impairment is not recommended due to accumulation of a metabolite formed by glucuronidation of tapentadol. The clinical relevance of the elevated metabolite is not known [see Clinical Pharmacology (12.3)].
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling:
- Respiratory Depression [see Warnings and Precautions (5.2)]
- Interaction with Alcohol [see Warnings and Precautions (5.4)]
- Chronic Pulmonary Disease [see Warnings and Precautions (5.6)]
- Hypotensive Effects [see Warnings and Precautions (5.8)]
- Interactions with Other CNS Depressants [see Warnings and Precautions (5.7)]
- Drug abuse, addiction, and dependence [see Abuse and Dependence (9.2, 9.3)]
- Gastrointestinal Effects [see Warnings and Precautions (5.12)]
- Seizures [see Warnings and Precautions (5.10)]
- Serotonin Syndrome [see Warnings and Precautions (5.11)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. Based on data from nine Phase 2/3 studies that administered multiple doses (seven placebo- and/or active-controlled, one noncontrolled and one Phase 3 active-controlled safety study) the most common adverse reactions (reported by ≥10% in any NUCYNTA® dose group) were: nausea, dizziness, vomiting and somnolence.
The most common reasons for discontinuation due to adverse reactions in the studies described above (reported by ≥1% in any NUCYNTA® dose group) were dizziness (2.6% vs. 0.5%), nausea (2.3% vs. 0.6%), vomiting (1.4% vs. 0.2%), somnolence (1.3% vs. 0.2%) and headache (0.9% vs. 0.2%) for NUCYNTA®- and placebo-treated patients, respectively.
Seventy-six percent of NUCYNTA®-treated patients from the nine studies experienced adverse events.
NUCYNTA® was studied in multiple-dose, active- or placebo-controlled studies, or noncontrolled studies (n = 2178), in single-dose studies (n = 870), in open-label study extension (n = 483) and in Phase 1 studies (n = 597). Of these, 2034 patients were treated with doses of 50 mg to 100 mg of NUCYNTA® dosed every 4 to 6 hours.
The data described below reflect exposure to NUCYNTA® in 3161 patients, including 449 exposed for 45 days. NUCYNTA® was studied primarily in placebo- and active-controlled studies (n = 2266, and n = 2944, respectively). The population was 18 to 85 years old (mean age 46 years), 68% were female, 75% white and 67% were postoperative. Most patients received NUCYNTA® doses of 50 mg, 75 mg, or 100 mg every 4 to 6 hours.
| System/Organ Class MedDRA Preferred Term |
NUCYNTA®
21 mg – 120 mg (n = 2178) % |
Placebo (n = 619) % |
|---|---|---|
| Gastrointestinal disorders | ||
| Nausea | 30 | 13 |
| Vomiting | 18 | 4 |
| Constipation | 8 | 3 |
| Dry mouth | 4 | <1 |
| Dyspepsia | 2 | <1 |
| General disorders and administration site conditions | ||
| Fatigue | 3 | <1 |
| Feeling hot | 1 | <1 |
| Infections and infestations | ||
| Nasopharyngitis | 1 | <1 |
| Upper respiratory tract infection | 1 | <1 |
| Urinary tract infection | 1 | <1 |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 2 | 0 |
| Nervous system disorders | ||
| Dizziness | 24 | 8 |
| Somnolence | 15 | 3 |
| Tremor | 1 | <1 |
| Lethargy | 1 | <1 |
| Psychiatric disorders | ||
| Insomnia | 2 | <1 |
| Confusional state | 1 | 0 |
| Abnormal dreams | 1 | <1 |
| Anxiety | 1 | <1 |
| Skin and subcutaneous tissue disorders | ||
| Pruritus | 5 | 1 |
| Hyperhidrosis | 3 | <1 |
| Pruritus generalized | 3 | <1 |
| Rash | 1 | <1 |
| Vascular disorders | ||
| Hot flush | 1 | <1 |
The following adverse drug reactions occurred in less than 1% of NUCYNTA®-treated patients in the pooled safety data from nine Phase 2/3 clinical studies:
Cardiac disorders: heart rate increased, heart rate decreased
Eye disorders: visual disturbance
Gastrointestinal disorders: abdominal discomfort, impaired gastric emptying
General disorders and administration site conditions: irritability, edema, drug withdrawal syndrome, feeling drunk
Immune system disorders: hypersensitivity
Investigations: gamma-glutamyltransferase increased, alanine aminotransferase increased, aspartate aminotransferase increased
Musculoskeletal and connective tissue disorders: involuntary muscle contractions, sensation of heaviness
Nervous system disorders: hypoesthesia, paresthesia, disturbance in attention, sedation, dysarthria, depressed level of consciousness, memory impairment, ataxia, presyncope, syncope, coordination abnormal, seizure
Psychiatric disorders: euphoric mood, disorientation, restlessness, agitation, nervousness, thinking abnormal
Renal and urinary disorders: urinary hesitation, pollakiuria
Respiratory, thoracic and mediastinal disorders: oxygen saturation decreased, cough, dyspnea, respiratory depression
Skin and subcutaneous tissue disorders: urticaria
Vascular disorders: blood pressure decreased
In the pooled safety data, the overall incidence of adverse reactions increased with increased dose of NUCYNTA®, as did the percentage of patients with adverse reactions of nausea, dizziness, vomiting, somnolence, and pruritus.
6.2 Post-marketing Experience
The following additional adverse reactions have been identified during post-approval use of NUCYNTA®. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency reliably.
Gastrointestinal disorders: diarrhea
Nervous system disorders: headache
Psychiatric disorders: hallucination, suicidal ideation, panic attack
Cardiac disorders: palpitations
Anaphylaxis, angioedema, and anaphylactic shock have been reported very rarely with ingredients contained in NUCYNTA®. Advise patients how to recognize such reactions and when to seek medical attention.
7 DRUG INTERACTIONS
NUCYNTA® is mainly metabolized by glucuronidation. The following substances have been included in a set of interaction studies without any clinically significant finding: acetaminophen, acetylsalicylic acid, naproxen and probenecid [see Clinical Pharmacology (12.3)].
The pharmacokinetics of tapentadol were not affected when gastric pH or gastrointestinal motility were increased by omeprazole and metoclopramide, respectively [see Clinical Pharmacology (12.3)].
7.1 Alcohol, Other Opioids, and Drugs of Abuse
Due to its mu-opioid agonist activity, NUCYNTA® may be expected to have additive effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression, respiratory depression, hypotension, and profound sedation, coma or death. Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products containing alcohol, other opioids, or drugs of abuse while on NUCYNTA® therapy [see Warnings and Precautions (5.4)].
7.2 Monoamine Oxidase Inhibitors
NUCYNTA® is contraindicated in patients who are receiving monoamine oxidase (MAO) inhibitors or who have taken them within the last 14 days due to potential additive effects on norepinephrine levels which may result in adverse cardiovascular events [see Contraindications (4)].
7.3 CNS Depressants
Concurrent use of NUCYNTA® and other central nervous system (CNS) depressants including sedatives or hypnotics, general anesthetics, phenothiazines, tranquilizers, and alcohol can increase the risk of respiratory depression, hypotension, profound sedation or coma. Monitor patients receiving CNS depressants and NUCYNTA® for signs of respiratory depression and hypotension. When such combined therapy is contemplated, start NUCYNTA® at 1/3 to 1/2 of the usual dosage and consider using a lower dose of the concomitant CNS depressant [see Warnings and Precautions (5.7)].
7.4 Serotonergic Drugs
There have been post-marketing reports of serotonin syndrome with the concomitant use of tapentadol and serotonergic drugs (e.g., SSRIs and SNRIs). Caution is advised when NUCYNTA® is co-administered with other drugs that may affect serotonergic neurotransmitter systems such as SSRIs, SNRIs, MAOIs, and triptans. If concomitant treatment of NUCYNTA® with a drug affecting the serotonergic neurotransmitter system is clinically warranted, careful observation of the patient is advised [see Warning and Precautions (5.11)].
7.5 Mixed Agonist/Antagonist Opioid Analgesics
The concomitant use of NUCYNTA® with mixed agonist/antagonists (e.g., butorphanol, nalbuphine, and pentazocine) and partial agonists (e.g., buprenorphine) may precipitate withdrawal symptoms. Avoid the use of agonist/antagonists and partial agonists with NUCYNTA®.
7.6 Anticholinergics
The use of NUCYNTA® with anticholinergic products may increase the risk of urinary retention and/or severe constipation, which may lead to paralytic ileus.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C: There are no adequate and well-controlled studies of NUCYNTA® in pregnant women. NUCYNTA® should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Tapentadol HCl was evaluated for teratogenic effects in pregnant rats and rabbits following intravenous and subcutaneous exposure during the period of embryofetal organogenesis. When tapentadol was administered twice daily by the subcutaneous route in rats at dose levels of 10, 20, or 40 mg/kg/day [producing up to 1 times the plasma exposure at the maximum recommended human dose (MRHD) of 700 mg/day based on an area under the time-curve (AUC) comparison], no teratogenic effects were observed. Evidence of embryofetal toxicity included transient delays in skeletal maturation (i.e. reduced ossification) at the 40 mg/kg/day dose which was associated with significant maternal toxicity. Administration of tapentadol HCl in rabbits at doses of 4, 10, or 24 mg/kg/day by subcutaneous injection [producing 0.2, 0.6, and 1.85 times the plasma exposure at the MRHD based on an AUC comparison] revealed embryofetal toxicity at doses ≥10 mg/kg/day. Findings included reduced fetal viability, skeletal delays and other variations. In addition, there were multiple malformations including gastroschisis/thoracogastroschisis, amelia/phocomelia, and cleft palate at doses ≥10 mg/kg/day and above, and ablepharia, encephalopathy, and spina bifida at the high dose of 24 mg/kg/day. Embryofetal toxicity, including malformations, may be secondary to the significant maternal toxicity observed in the study.
In a study of pre- and postnatal development in rats, oral administration of tapentadol at doses of 20, 50, 150, or 300 mg/kg/day to pregnant and lactating rats during the late gestation and early postnatal period [resulting in up to 1.7 times the plasma exposure at the MRHD on an AUC basis] did not influence physical or reflex development, the outcome of neurobehavioral tests or reproductive parameters. Treatment-related developmental delay was observed, including incomplete ossification, and significant reductions in pup body weights and body weight gains at doses associated with maternal toxicity (150 mg/kg/day and above). At maternal tapentadol doses ≥150 mg/kg/day, a dose-related increase in pup mortality was observed through postnatal Day 4.
8.2 Labor and Delivery
NUCYNTA® is not for use in women during and immediately prior to labor. Occasionally, opioid analgesics may prolong labor by temporarily reducing the strength, duration, and frequency of uterine contractions. However, these effects are not consistent and may be offset by an increased rate of cervical dilatation which tends to shorten labor.
Opioids cross the placenta and may produce respiratory depression and psychophysiologic effects in neonates. Closely observe neonates whose mothers received opioid analgesics during labor for signs of respiratory depression. An opioid antagonist, such as naloxone, should be available for reversal of opioid-induced respiratory depression in the neonate in such situations
8.3 Nursing Mothers
There is insufficient/limited information on the excretion of tapentadol in human or animal breast milk. Physicochemical and available pharmacodynamic/toxicological data on tapentadol point to excretion in breast milk and risk to the breastfeeding child cannot be excluded.
Because of the potential for adverse reactions in nursing infants from NUCYNTA®, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Withdrawal symptoms can occur in breast-feeding infants when maternal administration of NUCYNTA® is stopped.
8.4 Pediatric Use
The safety and effectiveness of NUCYNTA® in pediatric patients less than 18 years of age have not been established.
8.5 Geriatric Use
Of the total number of patients in Phase 2/3 double-blind, multiple-dose clinical studies of NUCYNTA®, 19% were 65 and over, while 5% were 75 and over. No overall differences in effectiveness were observed between these patients and younger patients. The rate of constipation was higher in subjects greater than or equal to 65 years than those less than 65 years (12% vs. 7%).
In general, recommended dosing for elderly patients with normal renal and hepatic function is the same as for younger adult patients with normal renal and hepatic function. Because elderly patients are more likely to have decreased renal and hepatic function, consideration should be given to starting elderly patients with the lower range of recommended doses [see Clinical Pharmacology (12.3)].
8.6 Neonatal Withdrawal Syndrome
Chronic maternal use of NUCYNTA® during pregnancy can affect the neonate with subsequent withdrawal signs. Neonatal withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. The onset, duration and severity of neonatal withdrawal syndrome vary based on the drug used, duration of use, the dose of last maternal use, and rate of elimination drug by the newborn. Neonatal opioid withdrawal syndrome may be life-threatening and should be treated according to protocols developed by neonatology experts.
8.7 Renal Impairment
The safety and effectiveness of NUCYNTA® has not been established in patients with severe renal impairment (CLCR <30 mL/min). Use of NUCYNTA® in patients with severe renal impairment is not recommended due to accumulation of a metabolite formed by glucuronidation of tapentadol. The clinical relevance of the elevated metabolite is not known [see Clinical Pharmacology (12.3)].
8.8 Hepatic Impairment
Administration of tapentadol resulted in higher exposures and serum levels of tapentadol in subjects with impaired hepatic function compared to subjects with normal hepatic function [see Clinical Pharmacology (12.3)]. The dose of NUCYNTA® should be reduced in patients with moderate hepatic impairment (Child-Pugh Score 7 to 9) [see Dosage and Administration (2.4)].
Use of NUCYNTA® is not recommended in patients with severe hepatic impairment (Child-Pugh Score 10 to 15) [see Warnings and Precautions (5.15)].
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
NUCYNTA® contains tapentadol, a Schedule II controlled substance with a high potential for abuse similar to fentanyl, methadone, morphine, oxycodone, and oxymorphone. NUCYNTA® is subject to misuse, abuse, addiction, and criminal diversion [see Warnings and Precautions (5.1)].
9.2 Abuse
All patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Drug abuse is the intentional non-therapeutic use of an over-the-counter or prescription drug, even once, for its rewarding psychological or physiological effects. Drug abuse includes, but is not limited to the following examples: the use of a prescription or over-the-counter drug to get "high", or the use of steroids for performance enhancement and muscle build up.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and include: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal.
"Drug seeking" behavior is very common in addicts, and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated claims of loss of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). "Healthcare professional shopping" (visiting multiple prescribers) to obtain additional prescriptions is common among drug abusers, people suffering from untreated addiction and criminals seeking drugs to sell.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances.
NUCYNTA® can be diverted for non-medical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
9.3 Dependence
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dose reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity, e.g., naloxone, nalmefene, or mixed agonist/antagonist analgesics (pentazocine, butorphanol, buprenorphine, nalbuphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, piloerection, myalgia, mydriasis, irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, increased blood pressure, respiratory rate, or heart rate. Withdrawal symptoms may be reduced by tapering NUCYNTA®.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms [see Use in Specific Populations (8.1, 8.2)].
10 OVERDOSAGE
10.1 Clinical Presentation
Acute overdosage with opioids can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and sometimes pulmonary edema, bradycardia, hypotension and death. Marked mydriasis rather than miosis may be seen due to severe hypoxia in overdose situations.
In case of overdose, priorities are the re-establishment of a patent and protected airway and institution of assisted or controlled ventilation if needed. Employ other supportive measures (including oxygen, vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life support techniques.
The opioid antagonists, naloxone or nalmefene, are specific antidotes to respiratory depression resulting from opioid overdose. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to tapentadol overdose. Such agents should be administered cautiously to patients who are known, or suspected to be, physically dependent on NUCYNTA®. In such cases, an abrupt or complete reversal of opioid effects may precipitate an acute withdrawal syndrome.
Because the duration of reversal would be expected to be less than the duration of action of tapentadol in NUCYNTA®, carefully monitor the patient until spontaneous respiration is reliably re-established. If the response to opioid antagonists is suboptimal or not sustained, additional antagonist should be given as directed in the product's prescribing information.
In an individual physically dependent on opioids, administration of an opioid receptor antagonist may precipitate an acute withdrawal. The severity of the withdrawal produced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be begun with care and by titration with smaller than usual doses of the antagonist.
11 DESCRIPTION
NUCYNTA® (tapentadol) is a mu-opioid receptor agonist, supplied in a liquid solution for oral administration. The chemical name is 3-[(1R,2R)-3-(dimethylamino)-1-ethyl-2-methylpropyl]phenol monohydrochloride. The structural formula is:
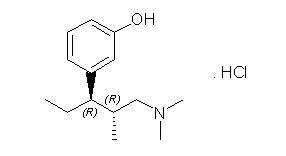
The molecular weight of tapentadol HCl is 257.80, and the molecular formula is C14H23NO•HCl. The n-octanol:water partition coefficient log P value is 2.87. The pKa values are 9.34 and 10.45.
NUCYNTA® (tapentadol) oral solution is supplied as a clear, colorless solution and contains 20 mg/mL of tapentadol (corresponding to 23 mg/mL of tapentadol hydrochloride) and the following inactive ingredients: citric acid monohydrate, purified water, raspberry flavor, sodium hydroxide, and sucralose.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tapentadol is a centrally-acting synthetic analgesic. The exact mechanism of action is unknown. Although the clinical relevance is unclear, preclinical studies have shown that tapentadol is a mu-opioid receptor (MOR) agonist and a norepinephrine reuptake inhibitor (NRI). Analgesia in animal models is derived from both of these properties.
12.2 Pharmacodynamics
Tapentadol is 18 times less potent than morphine in binding to the human mu-opioid receptor and is 2–3 times less potent in producing analgesia in animal models. Tapentadol has been shown to inhibit norepinephrine reuptake in the brains of rats resulting in increased norepinephrine concentrations. In preclinical models, the analgesic activity due to the mu-opioid receptor agonist activity of tapentadol can be antagonized by selective mu-opioid antagonists (e.g., naloxone), whereas the norepinephrine reuptake inhibition is sensitive to norepinephrine modulators. Tapentadol exerts its analgesic effects without a pharmacologically active metabolite.
Effects on the cardiovascular system: There was no effect of therapeutic and supratherapeutic doses of tapentadol on the QT interval. In a randomized, double-blind, placebo- and positive-controlled crossover study, healthy subjects were administered five consecutive doses of NUCYNTA® 100 mg every 6 hours, NUCYNTA® 150 mg every 6 hours, placebo and a single oral dose of moxifloxacin. Similarly, NUCYNTA® had no relevant effect on other ECG parameters (heart rate, PR interval, QRS duration, T-wave or U-wave morphology).
Concentration-Efficacy Relationships
The minimum effective plasma concentration of tapentadol for analgesia varies widely among patients, especially among patients who have been previously treated with agonist opioids.
Concentration-Adverse Experience Relationships
There is a general relationship between increasing opioid plasma concentration and increasing frequency of adverse experiences such as nausea, vomiting, CNS effects, and respiratory depression.
Effects on the Central Nervous System (CNS)
The principal therapeutic action of tapentadol is analgesia. Tapentadol causes respiratory depression, in part by a direct effect on the brainstem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation. Tapentadol depresses the cough reflex by direct effect on the cough center in the medulla.
Tapentadol causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings). Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Overdosage (10)].
Effects on the Gastrointestinal Tract and on Other Smooth Muscle
Gastric, biliary and pancreatic secretions are decreased by tapentadol. Tapentadol causes a reduction in motility and is associated with an increase in tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm. The end result is constipation. Tapentadol can cause a marked increase in biliary tract pressure as a result of spasm of the sphincter of Oddi, and transient elevations in serum amylase. Tapentadol may also cause spasm of the sphincter of the urinary bladder.
Effects on the Cardiovascular System
Tapentadol produces peripheral vasodilation which may result in orthostatic hypotension.
Effects on the Endocrine System
Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown.
CNS Depressant/Alcohol Interaction
Additive pharmacodynamic effects may be expected when NUCYNTA® is used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression.
12.3 Pharmacokinetics
Absorption
The mean absolute bioavailability after single-dose administration (fasting) of NUCYNTA® is approximately 32% due to extensive first-pass metabolism. Maximum serum concentrations of tapentadol are typically observed at around 1.25 hours after dosing.
Dose-proportional increases in the Cmax and AUC values of tapentadol have been observed over the 50 to 150 mg dose range.
A multiple (every 6 hour) dose study with doses ranging from 75 to 175 mg tapentadol showed a mean accumulation factor of 1.6 for the parent drug and 1.8 for the major metabolite tapentadol-O-glucuronide, which are primarily determined by the dosing interval and apparent half-life of tapentadol and its metabolite.
Food Effect
The AUC and Cmax increased by 25% and 16%, respectively, when NUCYNTA® was administered after a high-fat, high-calorie breakfast. NUCYNTA® may be given with or without food.
Distribution
Tapentadol is widely distributed throughout the body. Following intravenous administration, the volume of distribution (Vz) for tapentadol is 540 +/- 98 L. The plasma protein binding is low and amounts to approximately 20%.
Metabolism and Elimination
In humans, about 97% of the parent compound is metabolized. Tapentadol is mainly metabolized via Phase 2 pathways, and only a small amount is metabolized by Phase 1 oxidative pathways. The major pathway of tapentadol metabolism is conjugation with glucuronic acid to produce glucuronides. After oral administration approximately 70% (55% O-glucuronide and 15% sulfate of tapentadol) of the dose is excreted in urine in the conjugated form. A total of 3% of drug was excreted in urine as unchanged drug. Tapentadol is additionally metabolized to N-desmethyl tapentadol (13%) by CYP2C9 and CYP2C19 and to hydroxy tapentadol (2%) by CYP2D6, which are further metabolized by conjugation. Therefore, drug metabolism mediated by cytochrome P450 system is of less importance than phase 2 conjugation.
None of the metabolites contribute to the analgesic activity.
Tapentadol and its metabolites are excreted almost exclusively (99%) via the kidneys. The terminal half-life is on average 4 hours after oral administration. The total clearance is 1530 +/- 177 mL/min.
Special Populations
Geriatric Patients
The mean exposure (AUC) to tapentadol was similar in elderly subjects compared to young adults, with a 16% lower mean Cmax observed in the elderly subject group compared to young adult subjects.
Renal Impairment
AUC and Cmax of tapentadol were comparable in subjects with varying degrees of renal function (from normal to severely impaired). In contrast, increasing exposure (AUC) to tapentadol-O-glucuronide was observed with increasing degree of renal impairment. In subjects with mild (CLCR = 50 to <80 mL/min), moderate (CLCR = 30 to <50 mL/min), and severe (CLCR = <30 mL/min) renal impairment, the AUC of tapentadol-O-glucuronide was 1.5-, 2.5-, and 5.5-fold higher compared with normal renal function, respectively.
Hepatic Impairment
Administration of NUCYNTA® resulted in higher exposures and serum levels to tapentadol in subjects with impaired hepatic function compared to subjects with normal hepatic function. The ratio of tapentadol pharmacokinetic parameters for the mild hepatic impairment group (Child-Pugh Score 5 to 6) and moderate hepatic impairment group (Child-Pugh Score 7 to 9) in comparison to the normal hepatic function group were 1.7 and 4.2, respectively, for AUC; 1.4 and 2.5, respectively, for Cmax; and 1.2 and 1.4, respectively, for t1/2. The rate of formation of tapentadol-O-glucuronide was lower in subjects with increased liver impairment.
Pharmacokinetic Drug Interactions
Tapentadol is mainly metabolized by Phase 2 glucuronidation, a high capacity/low affinity system; therefore, clinically relevant interactions caused by Phase 2 metabolism are unlikely to occur. Naproxen and probenecid increased the AUC of tapentadol by 17% and 57%, respectively. No changes in the pharmacokinetic parameters of tapentadol were observed when acetaminophen and acetylsalicylic acid were given concomitantly. These changes are not considered clinically relevant and no change in dose is required.
In vitro studies did not reveal any potential of tapentadol to either inhibit or induce cytochrome P450 enzymes. Furthermore, a minor amount of NUCYNTA® is metabolized via the oxidative pathway. Thus, clinically relevant interactions mediated by the cytochrome P450 system are unlikely to occur.
The pharmacokinetics of tapentadol were not affected when gastric pH or gastrointestinal motility were increased by omeprazole and metoclopramide, respectively.
Plasma protein binding of tapentadol is low (approximately 20%). Therefore, the likelihood of pharmacokinetic drug-drug interactions by displacement from the protein binding site is low.
13 NON-CLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Tapentadol was administered to rats (diet) and mice (oral gavage) for two years.
In mice, tapentadol HCl was administered by oral gavage at dosages of 50, 100 and 200 mg/kg/day for 2 years (up to 0.2 times the plasma exposure at the maximum recommended human dose [MRHD] on an area under the time-curve [AUC] basis). No increase in tumor incidence was observed at any dose level.
In rats, tapentadol HCl was administered in diet at dosages of 10, 50, 125 and 250 mg/kg/day for two years (up to 0.2 times in the male rats and 0.6 times in the female rats the MRHD on an AUC basis). No increase in tumor incidence was observed at any dose level.
Mutagenesis
Tapentadol did not induce gene mutations in bacteria, but was clastogenic with metabolic activation in a chromosomal aberration test in V79 cells. The test was repeated and was negative in the presence and absence of metabolic activation. The one positive result for tapentadol was not confirmed in vivo in rats, using the two endpoints of chromosomal aberration and unscheduled DNA synthesis, when tested up to the maximum tolerated dose.
Impairment of Fertility
Tapentadol HCl was administered intravenously to male or female rats at dosages of 3, 6, or 12 mg/kg/day (representing exposures of up to approximately 0.4 times the exposure at the MRHD on an AUC basis, based on extrapolation from toxicokinetic analyses in a separate 4-week intravenous study in rats). Tapentadol did not alter fertility at any dose level. Maternal toxicity and adverse effects on embryonic development, including decreased number of implantations, decreased numbers of live conceptuses, and increased pre- and post-implantation losses occurred at dosages ≥6 mg/kg/day.
13.2 Animal Toxicology and/or Pharmacology
In toxicological studies with tapentadol, the most common systemic effects of tapentadol were related to the mu-opioid receptor agonist and norepinephrine reuptake inhibition pharmacodynamic properties of the compound. Transient, dose-dependent and predominantly CNS-related findings were observed, including impaired respiratory function and convulsions, the latter occurring in the dog at plasma levels (Cmax) which are in the range associated with the maximum recommended human dose (MRHD).
14 CLINICAL STUDIES
The efficacy and safety of NUCYNTA® in the treatment of moderate to severe acute pain has been established in two randomized, double-blind, placebo- and active-controlled studies of moderate to severe pain from first metatarsal bunionectomy and end-stage degenerative joint disease.
14.1 Orthopedic Surgery – Bunionectomy
A randomized, double-blind, parallel-group, active- and placebo-controlled, multiple-dose study demonstrated the efficacy of 50 mg, 75 mg, and 100 mg NUCYNTA® given every 4 to 6 hours for 72 hours in patients aged 18 to 80 years experiencing moderate to severe pain following unilateral, first metatarsal bunionectomy surgery. Patients who qualified for the study with a baseline pain score of ≥4 on an 11-point rating scale ranging from 0 to 10 were randomized to 1 of 5 treatments. Patients were allowed to take a second dose of study medication as soon as 1 hour after the first dose on study Day 1, with subsequent dosing every 4 to 6 hours. If rescue analgesics were required, the patients were discontinued for lack of efficacy. Efficacy was evaluated by comparing the sum of pain intensity difference over the first 48 hours (SPID48) versus placebo. NUCYNTA® at each dose provided a greater reduction in pain compared to placebo based on SPID48 values.
For various degrees of improvement from baseline to the 48-hour endpoint, Figure 1 shows the fraction of patients achieving that level of improvement. The figures are cumulative, such that every patient that achieves a 50% reduction in pain from baseline is included in every level of improvement below 50%. Patients who did not complete the 48-hour observation period in the study were assigned 0% improvement.
| Figure 1: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by Pain Severity at 48 Hours Compared to Baseline- Post Operative Bunionectomy |
|
|
The proportions of patients who showed reduction in pain intensity at 48 hours of 30% or greater, or 50% or greater were significantly higher in patients treated with NUCYNTA® at each dose versus placebo.
14.2 End-Stage Degenerative Joint Disease
A randomized, double-blind, parallel-group, active- and placebo-controlled, multiple-dose study evaluated the efficacy and safety of 50 mg and 75 mg NUCYNTA® given every 4 to 6 hours during waking hours for 10 days in patients aged 18 to 80 years, experiencing moderate to severe pain from end stage degenerative joint disease of the hip or knee, defined as a 3-day mean pain score of ≥5 on an 11-point pain intensity scale, ranging from 0 to 10. Pain scores were assessed twice daily and assessed the pain the patient had experienced over the previous 12 hours. Patients were allowed to continue non-opioid analgesic therapy for which they had been on a stable regimen before screening throughout the study. Eighty-three percent (83%) of patients in the tapentadol treatment groups and the placebo group took such analgesia during the study. The 75 mg treatment group was dosed at 50 mg for the first day of the study, followed by 75 mg for the remaining nine days. Patients requiring rescue analgesics other than study medication were discontinued for lack of efficacy. Efficacy was evaluated by comparing the sum of pain intensity difference (SPID) versus placebo over the first five days of treatment. NUCYNTA® 50 mg and 75 mg provided improvement in pain compared with placebo based on the 5-Day SPID.
For various degrees of improvement from baseline to the Day 5 endpoint, Figure 2 shows the fraction of patients achieving that level of improvement. The figures are cumulative, such that every patient that achieves a 50% reduction in pain from baseline is included in every level of improvement below 50%. Patients who did not complete the 5-day observation period in the study were assigned 0% improvement.
| Figure 2: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by Average Pain Severity for the Previous 12 hours, Measured on Study Day 5 Compared to Baseline -- End Stage Degenerative Joint Disease |
|
|
The proportions of patients who showed reduction in pain intensity at 5 days of 30% or greater, or 50% or greater were significantly higher in patients treated with NUCYNTA® at each dose versus placebo.
16 HOW SUPPLIED/STORAGE AND HANDLING
NUCYNTA® oral solution, 20 mg/mL, is available as a clear, colorless solution.
Supplied with calibrated syringe:
Bottles of 100 mL (NDC 50458-817-01)
Bottles of 200 mL (NDC 50458-817-02)
Storage and Handling
Store up to 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Store the oral solution bottle upright after opening.
Keep NUCYNTA® in a secure place out of reach of children.
NUCYNTA® oral solution that is no longer needed should be destroyed by flushing down the toilet.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide and Instructions for Use).
Inform patients of the availability of a Medication Guide and Instructions for Use, and instruct them to read the Medication Guide and Instructions for Use prior to taking NUCYNTA® oral solution.
Instruct patients to take NUCYNTA® oral solution only as prescribed.
Abuse Potential
Inform patients that NUCYNTA® contains tapentadol, a Schedule II controlled substance that is subject to abuse. Instruct patients not to share NUCYNTA® with others and to take steps to protect NUCYNTA® from theft or misuse.
Life-threatening Respiratory Depression
Discuss the risk of respiratory depression with patients, explaining that the risk is greatest when starting NUCYNTA® or when the dose is increased. Advise patients how to recognize respiratory depression and to seek medical attention if they are experiencing breathing difficulties.
Accidental Exposure
Instruct patients to take steps to store NUCYNTA® securely. Accidental exposure, especially in children, may results in serious harm or death. Advise patients to dispose of unused NUCYNTA® by flushing the oral solution down the toilet.
Important Administration Instructions
Instruct patients how to properly take NUCYNTA® oral solution, including the following:
- Advise patients to always use the enclosed calibrated oral syringe when administering NUCYNTA® oral solution to ensure the dose is measured and administered accurately.
- Using NUCYNTA® oral solution exactly as prescribed to reduce the risk of life-threatening adverse reactions (e.g., respiratory depression).
- Not discontinuing NUCYNTA® without first discussing the need for a tapering regimen with the prescriber.
Risks from Concomitant Use of Alcohol and other CNS Depressants
Inform patients that the concomitant use of alcohol with NUCYNTA® can increase the risk of life-threatening respiratory depression. Instruct patients not to consume alcoholic beverages, as well as prescription and over-the-counter drug products that contain alcohol, during treatment with NUCYNTA®.
Inform patients that potentially serious additive effects may occur if NUCYNTA® is used with other CNS depressants, and not to use such drugs unless supervised by a health care provider.
Concurrent use of MAOI
Inform patients not to take NUCYNTA® while using any drugs that inhibit monoamine oxidase. Patients should not start any new medications while taking NUCYNTA®.
Seizures
Inform patients that NUCYNTA® could cause seizures if they are at risk for seizures or have epilepsy. Patients should be advised to stop taking NUCYNTA® if they have a seizure while taking NUCYNTA® and call their healthcare provider right away.
Serotonin Syndrome
Inform patients that NUCYNTA® could cause a rare but potentially life-threatening condition resulting from concomitant administration of serotonergic drugs (including Serotonin Reuptake Inhibitors, Serotonin and Norepinephrine Reuptake Inhibitors and tricyclic antidepressants. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop.
Instruct patients to inform their physicians if they are taking, or plan to take additional medications including CNS Depressants, MAO inhibitors, mixed agonists/antagonist opioid analgesics, anticholinergics, SSRIs, SNRIs, or tricyclic antidepressants.
Hypotension
Inform patients that NUCYNTA® may cause orthostatic hypotension and syncope. Instruct patients how to recognize symptoms of low blood pressure and how to reduce the risk of serious consequences should hypotension occur (e.g., sit or lie down, carefully rise from a sitting or lying position).
Driving or Operating Heavy Machinery
Inform patients that NUCYNTA® may impair the ability to perform potentially hazardous activities such as driving a car or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication.
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention.
Anaphylaxis
Inform patients that anaphylaxis has been reported with ingredients contained in NUCYNTA®. Advise patients how to recognize such a reaction and when to seek medical attention.
Pregnancy
Advise female patients that NUCYNTA® can cause fetal harm and to inform the prescriber if they are pregnant or plan to become pregnant.
Manufactured by:
Patheon Pharmaceuticals, Inc.
Cincinnati, OH 45237
Manufactured for:
Janssen Pharmaceuticals, Inc.
Titusville, NJ 08560
Revised: September 2013
© Janssen Pharmaceuticals, Inc. 2009
Medication Guide
NUCYNTA® (new-SINN-tah)
(tapentadol) oral solution, CII
What is the most important information I should know about NUCYNTA® oral solution?
- Get emergency help right away if you take too much NUCYNTA® oral solution (overdose). NUCYNTA® oral solution can cause life threatening breathing problems that can lead to death.
- Never give anyone else your NUCYNTA® oral solution. They could die from taking it. Store NUCYNTA® oral solution away from children and in a safe place to prevent stealing or abuse. Selling or giving away NUCYNTA® oral solution is against the law.
- Do not change your dose. Take NUCYNTA® oral solution exactly as prescribed by your healthcare provider.
- Always use the oral syringe provided with NUCYNTA® oral solution, 20 mg/mL to help make sure you measure the right amount.
What is NUCYNTA® oral solution?
NUCYNTA® oral solution is a strong prescription pain medicine that contains an opioid (narcotic) that is used to treat moderate to severe pain that is expected to last a short time.
Who should not take NUCYNTA® oral solution?
Do not take NUCYNTA® oral solution if you:
- have severe asthma, trouble breathing, or other lung problems
- have a bowel blockage or narrowing of the stomach or intestines
- take a monoamine oxidase inhibitor (MAOI) medicine or have taken an MAOI medicine within the last 14 days
- are allergic to tapentadol or any of its ingredients.
What should I tell my healthcare provider before taking NUCYNTA® oral solution?
Before taking NUCYNTA® oral solution, tell your healthcare provider if you have a history of:
|
|
|
|
Tell your healthcare provider if you are:
- pregnant or planning to become pregnant. NUCYNTA® oral solution may harm your unborn baby.
- breastfeeding. NUCYNTA® oral solution may pass into your breast milk and harm your baby.
- planning to have surgery
- taking prescription or over-the-counter medicines, vitamins, or herbal supplements.
How should I take NUCYNTA® oral solution?
- Do not change your dose. Take NUCYNTA® oral solution exactly as prescribed by your healthcare provider.
- If you miss a dose of NUCYNTA® oral solution you can take the dose when you remember if you have pain, or you can wait for the next dose.
- You can take NUCYNTA® oral solution with or without food.
- Make sure you understand exactly how to measure your dose. Always use the oral syringe provided with your NUCYNTA® oral solution to help make sure you measure the right amount. Call your pharmacist if you have difficulties with measuring your medicine.
- Call your healthcare provider if the dose you are taking does not control your pain.
- Do not stop taking NUCYNTA® oral solution without talking to your healthcare provider.
- After you stop taking NUCYNTA® oral solution, flush any unused oral solution down the toilet.
What should I avoid while taking NUCYNTA® oral solution?
While taking NUCYNTA® oral solution do not:
- Drive or operate heavy machinery, until you know how NUCYNTA® oral solution affects you. NUCYNTA® oral solution can make you sleepy, dizzy, or lightheaded.
- Drink alcohol or use prescription or over-the-counter medicines that contain alcohol.
What are the possible side effects of NUCYNTA® oral solution?
The possible side effects of NUCYNTA ® oral solution are:
- constipation, nausea, dizziness, vomiting, and sleepiness. Call your healthcare provider if you have any of these symptoms and they are severe.
Get emergency medical help if you:
- have trouble breathing, shortness of breath, fast heartbeat, chest pain, swelling of your face, tongue or throat, extreme drowsiness, a seizure, or you are feeling faint.
- are feeling agitated or restless, have hallucinations, pass out (become unconscious), feel overheated, have heavy sweating that is not due to activity, or loss of coordination.
These are not all the possible side effects of NUCYNTA® oral solution.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
For more information, go to dailymed.nlm.nih.gov
Manufactured by:Patheon Pharmaceuticals, Inc., Cincinnati, OH 45237
Manufactured for:Janssen Pharmaceuticals, Inc.,Titusville, NJ 08560
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Issue: October 2012
Instructions for Use
NUCYNTA® (tapentadol), CII
oral solution
20 mg/mL
Read the Instructions for Use before you start taking NUCYNTA® oral solution and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Important information about measuring NUCYNTA® oral solution
- Always use the oral syringe provided with your NUCYNTA® oral solution to make sure you measure the right amount.
- You will be provided (See Figure A.):
- 1 bottle of NUCYNTA® oral solution
- 1 oral syringe
- 1 adapter
If you do not receive an oral syringe with your NUCYNTA ® oral solution, ask your pharmacist to give you one.
Before you use NUCYNTA ® oral solution for the first time:
| 1. | Remove the child-resistant cap and completely remove the foil seal (See Figure B). |
|
| 2. | Push the ribbed end of the adapter into the neck of the bottle until it is firmly in place. The bottom edge of the adapter should fully contact the top rim of the bottle (See Figure C). Do not remove the adapter from the bottle after it is inserted. |
|
| To prepare a dose of NUCYNTA ® oral solution: | ||
| 3. | Hold the oral syringe in one hand. With your other hand, fully push down (depress) the plunger (See Figure D). |
|
| 4. | Insert the tip of the oral syringe into the adapter (See Figure E). |
|
| 5. | Turn the bottle upside down. Pull back slowly on the oral syringe plunger to withdraw the dose prescribed by your healthcare provider (2.5 mL, 3.75 mL, or 5 mL). If you see air bubbles in the oral syringe, fully push in the plunger so that the oral solution flows back into the bottle. Then, withdraw your prescribed dose of oral solution (See Figure F). |
|
| 6. | Leave the oral syringe in the bottle adapter and turn the bottle right-side up. Place the bottle onto a flat surface. Remove the oral syringe from the bottle (See Figure G). |
|
| 7. | Place the tip of the oral syringe in your mouth. Squirt the oral solution into your mouth by pushing on the plunger until the oral syringe is empty (See Figure H). |
|
| 8. | Leave the adapter in the bottle. Put the child-resistant cap back on the bottle (See Figure I). |
|
| 9. | Remove the plunger from the oral syringe barrel. Rinse the oral syringe with water after each use and let it air dry. When the oral syringe is dry, put the plunger back into the oral syringe barrel for the next use. Do not throw away the oral syringe. |
|
|
||
What are the ingredients in NUCYNTA® oral solution?
Active ingredient: tapentadol
Inactive ingredients: citric acid monohydrate, sucralose, raspberry flavor, sodium hydroxide, and purified water.
How should I store NUCYNTA® oral solution?
- Store NUCYNTA® oral solution at room temperature between 68°F to 77°F (20°C to 25°C).
- Store the NUCYNTA® oral solution bottle upright after opening. Keep the oral syringe with your medicine.
- After you stop taking NUCYNTA® oral solution, flush the unused oral solution down the toilet.
Keep NUCYNTA® oral solution out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Patheon Pharmaceuticals, Inc.
Cincinnati, OH 45237
Manufactured for:
Janssen Pharmaceuticals, Inc.
Titusville, NJ 08560
Revised: October 2012
© Janssen Pharmaceuticals, Inc. 2009
PRINCIPAL DISPLAY PANEL - 100 mL Bottle Label
NDC 50458-817-01
100mL
Nucynta
®
(tapentadol)
Oral Solution
20mg/mL
CII
Each 1mL contains 20mg of
tapentadol in solution
ATTENTION PHARMACIST: Dispense
the accompanying Medication
Guide to each patient

Nucyntatapentadol hydrochloride SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||