OLYSIO
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use OLYSIO™ safely and effectively. See full prescribing information for OLYSIO. OLYSIO (simeprevir) capsules, for oral useInitial U.S. Approval – 2013INDICATIONS AND USAGEOLYSIO is a hepatitis C virus (HCV) NS3/4A protease inhibitor indicated for the treatment of chronic hepatitis C (CHC) infection as a component of a combination antiviral treatment regimen. (1) OLYSIO efficacy has been established in combination with peginterferon alfa and ribavirin in HCV genotype 1 infected subjects with compensated liver disease (including cirrhosis). (1, 14) OLYSIO must not be used as monotherapy. (1) Screening patients with HCV genotype 1a infection for the presence of virus with the NS3 Q80K polymorphism at baseline is strongly recommended. Alternative therapy should be considered for patients infected with HCV genotype 1a containing the Q80K polymorphism. (1, 12, 14 ) DOSAGE AND ADMINISTRATION One 150 mg capsule taken once daily with food. (2.1) OLYSIO should be administered with both peginterferon alfa and ribavirin. The recommended treatment duration of OLYSIO with peginterferon alfa and ribavirin is 12 weeks, followed by either 12 or 36 additional weeks of peginterferon alfa and ribavirin depending on prior response status. (2.1) For specific dosage instructions for peginterferon alfa and ribavirin, see their respective prescribing information. (2.1) A dose recommendation cannot be made for patients of East Asian ancestry. (2.5, 8.6) A dose recommendation cannot be made for patients with moderate to severe hepatic impairment. (2.4, 8.8) DOSAGE FORMS AND STRENGTHSCapsule: 150 mg (3)CONTRAINDICATIONS All contraindications to peginterferon alfa and ribavirin also apply to OLYSIO combination treatment with peginterferon alfa and ribavirin. (4) Because ribavirin may cause birth defects and fetal death, OLYSIO in combination with peginterferon alfa and ribavirin is contraindicated in pregnant women and in men whose female partners are pregnant. (4) WARNINGS AND PRECAUTIONS Embryofetal Toxicity (Use with Ribavirin and Peginterferon Alfa): Ribavirin may cause birth defects and fetal death and animal studies have shown interferons have abortifacient effects; avoid pregnancy in female patients and female partners of male patients. Patients must have a negative pregnancy test prior to initiating therapy, use at least two effective methods of contraception during treatment, and undergo monthly pregnancy tests. (5.1) Photosensitivity: Serious photosensitivity reactions have been observed during combination therapy with OLYSIO, peginterferon alfa and ribavirin. Use sun protection measures and limit sun exposure. Consider discontinuation if a photosensitivity reaction occurs. (5.2) Rash: Rash has been observed during combination therapy with OLYSIO, peginterferon alfa and ribavirin. Discontinue OLYSIO if severe rash occurs. (5.3) Side EffectsThe most common reported adverse reactions (greater than 20% of subjects) in subjects receiving the combination of OLYSIO with peginterferon and ribavirin and occurring with at least 3% higher frequency compared to subjects receiving placebo in combination with peginterferon alfa and ribavirin during the first 12 weeks of treatment were: rash (including photosensitivity), pruritus and nausea. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Janssen Products, LP at 1-800-JANSSEN (1-800-526-7736) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSCo-administration of OLYSIO with drugs that are moderate or strong inducers or inhibitors of CYP3A may significantly affect the plasma concentrations of simeprevir. The potential for drug-drug interactions must be considered prior to and during treatment. (5.6, 7, 12.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 OLYSIO INDICATIONS AND USAGE
- 2 OLYSIO DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 OLYSIO CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 OLYSIO ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 OLYSIO DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PATIENT INFORMATIONOLYSIO™ (oh li' see oh)
- PRINCIPAL DISPLAY PANEL - 150 mg Capsule Bottle Label
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
OLYSIO™ is a hepatitis C virus (HCV) NS3/4A protease inhibitor indicated for the treatment of chronic hepatitis C (CHC) infection as a component of a combination antiviral treatment regimen.
- OLYSIO efficacy has been established in combination with peginterferon alfa and ribavirin, in HCV genotype 1 infected subjects with compensated liver disease (including cirrhosis) [see Clinical Studies (14)].
The following points should be considered when initiating OLYSIO for treatment of chronic hepatitis C infection:
- OLYSIO must not be used as monotherapy [see Warning and Precautions (5.5)].
- OLYSIO efficacy in combination with peginterferon alfa and ribavirin is influenced by baseline host and viral factors [see Clinical Pharmacology (12.5) and Clinical Studies (14)].
- OLYSIO efficacy in combination with peginterferon alfa and ribavirin is substantially reduced in patients infected with HCV genotype 1a with an NS3 Q80K polymorphism at baseline compared to patients infected with hepatitis C virus (HCV) genotype 1a without the Q80K polymorphism [see Microbiology (12.4) and Clinical Studies (14)]. Screening patients with HCV genotype 1a infection for the presence of virus with the NS3 Q80K polymorphism at baseline is strongly recommended. Alternative therapy should be considered for patients infected with HCV genotype 1a containing the Q80K polymorphism.
- OLYSIO efficacy has not been studied in patients who have previously failed therapy with a treatment regimen that includes OLYSIO or other HCV protease inhibitors [see Microbiology (12.4)].
2 DOSAGE AND ADMINISTRATION
2.1 OLYSIO/Peginterferon alfa/Ribavirin Combination Treatment
The recommended dose of OLYSIO is one capsule of 150 mg taken orally once daily with food. The type of food does not affect exposure to simeprevir [see Clinical Pharmacology (12.3)]. The capsule should be swallowed as a whole.
OLYSIO should be used in combination with peginterferon alfa and ribavirin. For peginterferon alfa and ribavirin specific dosage instructions, refer to their respective prescribing information.
Duration of Treatment
The recommended duration of treatment with OLYSIO is 12 weeks in combination with peginterferon alfa and ribavirin.
In all patients, treatment with OLYSIO should be initiated in combination with peginterferon alfa and ribavirin and should be administered for 12 weeks.
All treatment-naïve and prior relapser patients, including those with cirrhosis, should receive an additional 12 weeks of peginterferon alfa and ribavirin after completing 12 weeks of treatment with OLYSIO, peginterferon alfa and ribavirin (total treatment duration of 24 weeks).
All prior non-responder patients (including partial and null-responders), including those with cirrhosis, should receive an additional 36 weeks of peginterferon alfa and ribavirin after completing 12 weeks of treatment with OLYSIO, peginterferon alfa and ribavirin (total treatment duration of 48 weeks).
The recommended duration of treatment with OLYSIO, peginterferon alfa and ribavirin is also presented in Table 1. Refer to Table 2 for treatment stopping rules.
Treatment with OLYSIO, Peginterferon alfa and Ribavirin |
Treatment with Peginterferon alfa and Ribavirin |
Total Treatment Duration |
|
|---|---|---|---|
|
Treatment-naïve and prior relapser patients |
First 12 weeks | Additional 12 weeks | 24 weeks |
|
Prior non-responder patients |
First 12 weeks | Additional 36 weeks | 48 weeks |
HCV RNA levels should be monitored as clinically indicated [see Dosage and Administration (2.2)]. Use of a sensitive assay with a lower limit of quantification of at least 25 IU/mL for monitoring HCV RNA levels during treatment is recommended. Refer to the respective prescribing information for peginterferon alfa and ribavirin for baseline, on-treatment and post-treatment laboratory testing recommendations including hematology, biochemistry (including hepatic enzymes and bilirubin), and pregnancy testing.
2.2 Discontinuation of Dosing
It is unlikely that patients with inadequate on-treatment virologic response will achieve a sustained virologic response (SVR), therefore discontinuation of treatment is recommended in these patients. The HCV RNA thresholds that trigger discontinuation of treatment (i.e., treatment stopping rules) are presented in Table 2.
| HCV RNA | Action |
|---|---|
| Treatment Week 4: greater than or equal to 25 IU/mL | Discontinue OLYSIO, peginterferon alfa and ribavirin |
| Treatment Week 12: greater than or equal to 25 IU/mL | Discontinue peginterferon alfa and ribavirin (treatment with OLYSIO is complete at Week 12) |
| Treatment Week 24: greater than or equal to 25 IU/mL | Discontinue peginterferon alfa and ribavirin |
If peginterferon alfa or ribavirin is discontinued for any reason, OLYSIO must also be discontinued.
2.3 Dosage Adjustment or Interruption
To prevent treatment failure, the dose of OLYSIO must not be reduced or interrupted. If treatment with OLYSIO is discontinued because of adverse reactions or inadequate on-treatment virologic response, OLYSIO treatment must not be reinitiated.
If adverse reactions potentially related to peginterferon alfa and/or ribavirin occur which require dosage adjustment or interruption of either medicine, refer to the instructions outlined in the respective prescribing information for these medicines.
2.4 Hepatic Impairment
No dose recommendation can be given for patients with moderate or severe hepatic impairment (Child-Pugh Class B or C) due to higher simeprevir exposures [see Clinical Pharmacology (12.3)]. In clinical trials, higher simeprevir exposures have been associated with increased frequency of adverse reactions, including rash and photosensitivity [see Adverse Reactions (6.1)].
The safety and efficacy of OLYSIO have not been studied in HCV-infected patients with moderate or severe hepatic impairment (Child-Pugh Class B or C). The combination of peginterferon alfa and ribavirin is contraindicated in patients with decompensated cirrhosis (moderate or severe hepatic impairment). The potential risks and benefits of OLYSIO should be carefully considered prior to use in patients with moderate or severe hepatic impairment.
2.5 Race
Patients of East Asian ancestry exhibit higher simeprevir exposures [see Clinical Pharmacology (12.3)]. In clinical trials, higher simeprevir exposures have been associated with increased frequency of adverse reactions, including rash and photosensitivity [see Adverse Reactions (6.1)]. There are insufficient safety data to recommend an appropriate dose for patients of East Asian ancestry. The potential risks and benefits of OLYSIO should be carefully considered prior to use in patients of East Asian ancestry.
3 DOSAGE FORMS AND STRENGTHS
Each capsule contains 150 mg simeprevir. Capsules are white and marked with "TMC435 150" in black ink.
4 CONTRAINDICATIONS
Contraindications to peginterferon alfa and ribavirin also apply to OLYSIO combination treatment with peginterferon alfa and ribavirin.
OLYSIO in combination with peginterferon alfa and ribavirin is contraindicated in pregnant women and in men whose female partners are pregnant because of the risks for birth defects and fetal death associated with ribavirin [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
Refer to the respective prescribing information for a list of the contraindications for peginterferon alfa and ribavirin.
5 WARNINGS AND PRECAUTIONS
5.1 Embryo-Fetal Toxicity (Use with Ribavirin and Peginterferon alfa)
Ribavirin may cause birth defects and/or death of the exposed fetus and animal studies have shown that interferons have abortifacient effects [see Contraindications (4)]. Therefore, extreme care must be taken to avoid pregnancy in female patients and in female partners of male patients. Ribavirin therapy should not be started unless a report of a negative pregnancy test has been obtained immediately prior to initiation of therapy. Refer also to the prescribing information for ribavirin.
Female patients of childbearing potential and their male partners, as well as male patients and their female partners, must use two effective contraceptive methods during treatment and for 6 months after completion of treatment. Routine monthly pregnancy tests must be performed during this time.
5.2 Photosensitivity
Photosensitivity reactions have been observed with OLYSIO in combination with peginterferon alfa and ribavirin, including serious reactions which resulted in hospitalization [see Adverse Reactions (6.1)]. Photosensitivity reactions occurred most frequently in the first 4 weeks of treatment with OLYSIO in combination with peginterferon alfa and ribavirin, but can occur at any time during treatment. Photosensitivity may present as an exaggerated sunburn reaction, usually affecting areas exposed to light (typically the face, "V" area of the neck, extensor surfaces of the forearms, and dorsa of the hands). Manifestations may include burning, erythema, exudation, blistering, and edema.
Use sun protective measures and limit sun exposure during treatment with OLYSIO in combination with peginterferon alfa and ribavirin. Avoid use of tanning devices during treatment with OLYSIO in combination with peginterferon alfa and ribavirin [see Patient Counseling Information]. Discontinuation of OLYSIO should be considered if a photosensitivity reaction occurs and patients should be monitored until the reaction has resolved. If a decision is made to continue OLYSIO in the setting of a photosensitivity reaction, expert consultation is advised.
5.3 Rash
Rash has been observed in subjects receiving OLYSIO in combination with peginterferon alfa and ribavirin [see Adverse Reactions (6.1)]. Rash occurred most frequently in the first 4 weeks of treatment with OLYSIO in combination with peginterferon alfa and ribavirin, but can occur at any time during treatment. Severe rash and rash requiring discontinuation of OLYSIO have been reported. Most of the rash events in OLYSIO-treated patients were of mild or moderate severity [see Adverse Reactions (6.1)]. Patients with mild to moderate rashes should be followed for possible progression of rash, including the development of mucosal signs (e.g., oral lesions, conjunctivitis) or systemic symptoms. If the rash becomes severe, OLYSIO should be discontinued. Patients should be monitored until the rash has resolved.
5.4 Sulfa Allergy
OLYSIO contains a sulfonamide moiety. In subjects with a history of sulfa allergy (n=16), no increased incidence of rash or photosensitivity reactions has been observed. However, there are insufficient data to exclude an association between sulfa allergy and the frequency or severity of adverse reactions observed with the use of OLYSIO.
5.5 Use with Peginterferon alfa and Ribavirin
OLYSIO must not be used as monotherapy. OLYSIO should be used in combination with both peginterferon alfa and ribavirin. Therefore the prescribing information for peginterferon alfa and ribavirin must be consulted before starting therapy with OLYSIO. Contraindications and Warnings and Precautions related to peginterferon alfa and ribavirin also apply to OLYSIO combination treatment with peginterferon alfa and ribavirin.
5.6 Drug Interactions
Co-administration of OLYSIO with substances that are moderate or strong inducers or inhibitors of cytochrome P450 3A (CYP3A) is not recommended as this may lead to significantly lower or higher exposure of simeprevir, respectively [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
6 ADVERSE REACTIONS
OLYSIO should be administered with peginterferon alfa and ribavirin. Refer to the prescribing information of peginterferon alfa and ribavirin for a description of adverse reactions associated with their use.
The following serious and otherwise important adverse drug reactions (ADRs) are discussed in detail in another section of the labeling:
- Embryo-Fetal Toxicity (Use with Ribavirin and Peginterferon alfa) [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)]
- Photosensitivity [see Warnings and Precautions (5.2)]
- Rash [see Warnings and Precautions (5.3)]
6.1 Clinical Studies Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in clinical practice.
The safety profile of OLYSIO in combination with peginterferon alfa and ribavirin in patients with HCV genotype 1 infection who were treatment-naïve or who had previously relapsed following interferon therapy with or without ribavirin is based on pooled data from three Phase 3 trials. These trials included a total of 1178 subjects who received OLYSIO or placebo in combination with 24 or 48 weeks of peginterferon alfa and ribavirin. Of the 1178 subjects, 781 subjects were randomized to receive OLYSIO 150 mg once daily for 12 weeks and 397 subjects were randomized to receive placebo once daily for 12 weeks.
In the pooled Phase 3 safety data, the majority of the adverse reactions reported during 12 weeks treatment with OLYSIO in combination with peginterferon alfa and ribavirin were Grade 1 to 2 in severity. Grade 3 or 4 adverse reactions were reported in 23% of subjects receiving OLYSIO in combination with peginterferon alfa and ribavirin versus 25% of subjects receiving placebo in combination with peginterferon alfa and ribavirin. Serious adverse reactions were reported in 2% of subjects receiving OLYSIO in combination with peginterferon alfa and ribavirin and in 3% of subjects receiving placebo in combination with peginterferon alfa and ribavirin. Discontinuation of OLYSIO or placebo due to adverse reactions occurred in 2% and 1% of subjects receiving OLYSIO with peginterferon alfa and ribavirin and subjects receiving placebo with peginterferon alfa and ribavirin, respectively.
The following table lists adverse reactions (all Grades) that occurred with at least 3% higher frequency among subjects receiving OLYSIO 150 mg once daily in combination with peginterferon alfa and ribavirin compared to subjects receiving placebo in combination with peginterferon alfa and ribavirin during the first 12 weeks of treatment in the pooled Phase 3 trials in subjects who were treatment-naïve or who had previously relapsed after peginterferon alfa and ribavirin therapy (see Table 3).
| Preferred Term or Grouped Term | OLYSIO + Peginterferon alfa+ Ribavirin First 12 Weeks N=781 % (n) |
Placebo + Peginterferon alfa+ Ribavirin First 12 Weeks N=397 % (n) |
|---|---|---|
| Rash (including photosensitivity) |
28 (218) | 20 (79) |
| Pruritus |
22 (168) | 15 (58) |
| Nausea | 22 (173) | 18 (70) |
| Myalgia | 16 (126) | 13 (53) |
| Dyspnea |
12 (92) | 8 (30) |
Rash and Photosensitivity
In the Phase 3 clinical trials, rash (including photosensitivity reactions) was observed in 28% of OLYSIO-treated subjects compared to 20% of placebo-treated subjects during the 12 weeks of treatment with OLYSIO/placebo in combination with peginterferon alfa and ribavirin. Fifty-six percent (56%) of rash events in the OLYSIO group occurred in the first 4 weeks, with 42% of cases occurring in the first 2 weeks. Most of the rash events in OLYSIO-treated subjects were of mild or moderate severity (Grade 1 or Grade 2). Severe (Grade 3) rash occurred in 1% of OLYSIO-treated subjects and in none of the placebo-treated subjects. There were no reports of life-threatening (Grade 4) rash. Discontinuation of OLYSIO/placebo due to rash occurred in 1% of OLYSIO-treated subjects, compared to less than 1% of placebo-treated subjects. The frequencies of rash and photosensitivity reactions were higher in subjects with higher simeprevir exposures.
All subjects enrolled in the Phase 3 trials were directed to use sun protection measures. In these trials, adverse reactions under the specific category of photosensitivity were reported in 5% of OLYSIO-treated subjects compared to 1% of placebo-treated subjects during the 12 weeks of treatment with OLYSIO/placebo in combination with peginterferon alfa and ribavirin. Most photosensitivity reactions in OLYSIO-treated subjects were of mild or moderate severity (Grade 1 or 2). Two OLYSIO-treated subjects experienced photosensitivity reactions which resulted in hospitalization. No life-threatening photosensitivity reactions were reported.
Dyspnea
During the 12 weeks of treatment with OLYSIO, dyspnea was reported in 12% of OLYSIO-treated subjects compared to 8% of placebo-treated subjects (all grades; pooled Phase 3). All dyspnea events reported in OLYSIO-treated subjects were of mild or moderate severity (Grade 1 or 2). There were no Grade 3 or 4 dyspnea events reported and no subjects discontinued treatment with OLYSIO due to dyspnea. Sixty-one percent (61%) of dyspnea events occurred in the first 4 weeks of treatment with OLYSIO.
Laboratory abnormalities
There were no differences between treatment groups for the following laboratory parameters: hemoglobin, neutrophils, platelets, aspartate aminotransferase, alanine aminotransferase, amylase, or serum creatinine. Treatment-emergent laboratory abnormalities that were observed at a higher incidence in OLYSIO-treated subjects than in placebo-treated subjects are listed in Table 4.
| Laboratory Parameter | WHO Toxicity Range | OLYSIO + Peginterferon alfa + Ribavirin N=781 % |
Placebo+ Peginterferon alfa + Ribavirin N=397 % |
|---|---|---|---|
| Chemistry | |||
|
Alkaline phosphatase |
|||
| Grade 1 | > 1.25 to ≤ 2.50 × ULN |
3 | 1 |
| Grade 2 | > 2.50 to ≤ 5.00 × ULN | < 1 | 0 |
| Hyperbilirubinemia | |||
| Grade 1 | > 1.1 to ≤ 1.5 × ULN | 27 | 15 |
| Grade 2 | > 1.5 to ≤ 2.5 × ULN | 18 | 9 |
| Grade 3 | > 2.5 to ≤ 5.0 × ULN | 4 | 2 |
| Grade 4 | > 5.0 × ULN | < 1 | 0 |
Elevations in bilirubin were predominately mild to moderate (Grade 1 or 2) in severity, and included elevation of both direct and indirect bilirubin. Elevations in bilirubin occurred early after treatment initiation, peaking by study Week 2, and were rapidly reversible upon cessation of OLYSIO. Bilirubin elevations were generally not associated with elevations in liver transaminases.
7 DRUG INTERACTIONS
[See also Warnings and Precautions (5.6) and Clinical Pharmacology (12.3)]
7.1 Potential for OLYSIO to Affect Other Drugs
Simeprevir does not induce CYP1A2 or CYP3A4 in vitro. Simeprevir is not a clinically relevant inhibitor of cathepsin A enzyme activity.
Simeprevir mildly inhibits CYP1A2 activity and intestinal CYP3A4 activity, but does not affect hepatic CYP3A4 activity. Co-administration of OLYSIO with drugs that are primarily metabolized by CYP3A4 may result in increased plasma concentrations of such drugs (see Table 5). Simeprevir does not affect CYP2C9, CYP2C19 or CYP2D6 in vivo.
Simeprevir inhibits OATP1B1/3 and P-glycoprotein (P-gp) transporters. Co-administration of OLYSIO with drugs that are substrates for OATP1B1/3 and P-gp transport may result in increased plasma concentrations of such drugs (see Table 5).
7.2 Potential for Other Drugs to Affect OLYSIO
The primary enzyme involved in the biotransformation of simeprevir is CYP3A [see Clinical Pharmacology (12.3)]. Clinically relevant effects of other drugs on simeprevir pharmacokinetics via CYP3A may occur. Co-administration of OLYSIO with moderate or strong inhibitors of CYP3A may significantly increase the plasma exposure of simeprevir. Co-administration with moderate or strong inducers of CYP3A may significantly reduce the plasma exposure of simeprevir and lead to loss of efficacy (see Table 5). Therefore, co-administration of OLYSIO with substances that are moderate or strong inducers or inhibitors of CYP3A is not recommended [see Warnings and Precautions (5.6)].
7.3 Established and Other Potentially Significant Drug Interactions
Table 5 shows the established and other potentially significant drug interactions based on which alterations in dose or regimen of OLYSIO and/or co-administered drug may be recommended. Drugs that are not recommended for co-administration with OLYSIO are also included in Table 5. For information regarding the magnitude of interaction, see Tables 6 and 7 (see Clinical Pharmacology (12.3) .
| Concomitant Drug Class Drug Name |
Effect on Concentration of Simeprevir or Concomitant Drug | Clinical Comment |
|---|---|---|
| The direction of the arrow (↑ = increase, ↓ = decrease, ↔ = no change) indicates the direction of the change in PK. | ||
| Antiarrhythmics | ||
| Digoxin |
↑ digoxin | Concomitant use of OLYSIO with digoxin resulted in increased concentrations of digoxin due to inhibition of P-gp by simeprevir. Routine therapeutic drug monitoring of digoxin concentrations is acceptable. |
| Amiodarone Disopyramide Flecainide Mexiletine Propafenone Quinidine |
↑ antiarrhythmics | Concomitant use of OLYSIO with these antiarrhythmics may result in mild increases in concentrations of these antiarrhythmics due to intestinal CYP3A4 inhibition by simeprevir. Caution is warranted and therapeutic drug monitoring for these antiarrhythmics, if available, is recommended when co-administered with OLYSIO. |
| Anticoagulants | ||
Warfarin |
↔ warfarin | No dose adjustment is required when OLYSIO is co-administered with warfarin. Routine monitoring of the international normalized ratio (INR) is acceptable. |
| Anticonvulsants | ||
| Carbamazepine Oxcarbazepine Phenobarbital Phenytoin |
↓ simeprevir | Concomitant use of OLYSIO with carbamazepine, oxcarbazepine, phenobarbital or phenytoin may result in significantly decreased plasma concentrations of simeprevir due to strong CYP3A induction by these anticonvulsants. This may result in loss of therapeutic effect of OLYSIO. It is not recommended to co-administer OLYSIO with these anticonvulsants. |
| Anti-infectives | ||
|
Antibiotics:
Erythromycin  |
↑ simeprevir ↑ erythromycin |
Concomitant use of OLYSIO with erythromycin resulted in significantly increased plasma concentrations of both erythromycin and simeprevir due to inhibition of CYP3A and P-gp by both erythromycin and simeprevir. It is not recommended to co-administer OLYSIO with erythromycin. |
|
Antibiotics:
Clarithromycin Telithromycin |
↑ simeprevir | Concomitant use of OLYSIO with clarithromycin or telithromycin may result in increased plasma concentrations of simeprevir due to CYP3A inhibition by these antibiotics. It is not recommended to co-administer OLYSIO with clarithromycin or telithromycin. |
|
Antifungals (systemic administration):
Itraconazole Ketoconazole Posaconazole |
↑ simeprevir | Concomitant use of OLYSIO with systemic itraconazole, ketoconazole or posaconazole may result in significantly increased plasma concentrations of simeprevir due to strong CYP3A inhibition by these antifungals. It is not recommended to co-administer OLYSIO with systemic itraconazole, ketoconazole or posaconazole. |
|
Antifungals (systemic administration):
Fluconazole Voriconazole |
↑ simeprevir | Concomitant use of OLYSIO with systemic fluconazole or voriconazole may result in increased plasma concentrations of simeprevir due to mild to moderate CYP3A inhibition by these antifungals. It is not recommended to co-administer OLYSIO with systemic fluconazole or voriconazole. |
|
Antimycobacterials:
Rifampin  Rifabutin Rifapentine |
↓ simeprevir ↔ rifampin, rifabutin, rifapentine |
Concomitant use of OLYSIO with rifampin, rifabutin or rifapentine may result in significantly decreased plasma concentrations of simeprevir due to CYP3A4 induction by these antimycobacterials. This may result in loss of therapeutic effect of OLYSIO. It is not recommended to co-administer OLYSIO with rifampin, rifabutin or rifapentine. |
| Calcium Channel Blockers | ||
| Amlodipine Diltiazem Felodipine Nicardipine Nifedipine Nisoldipine Verapamil |
↑ calcium channel blockers | Concomitant use of OLYSIO with calcium channel blockers may result in increased plasma concentrations of calcium channel blockers due to intestinal CYP3A4 and/or P-gp inhibition by simeprevir. Caution is warranted and clinical monitoring of patients is recommended when OLYSIO is co-administered with calcium channel blockers. |
| Corticosteroids | ||
|
Systemic
Dexamethasone |
↓ simeprevir | Concomitant use of OLYSIO with systemic dexamethasone may result in decreased plasma concentrations of simeprevir due to moderate induction of CYP3A4 by dexamethasone. This may result in loss of therapeutic effect of OLYSIO. It is not recommended to co-administer OLYSIO with systemic dexamethasone. |
| Gastrointestinal Products | ||
|
Propulsive:
Cisapride |
↑ cisapride | Cisapride has the potential to cause cardiac arrhythmias. Concomitant use of OLYSIO with cisapride may result in increased plasma concentrations of cisapride due to intestinal CYP3A4 inhibition by simeprevir. It is not recommended to co-administer OLYSIO with cisapride. |
| Herbal Products | ||
| Milk thistle (Silybum marianum) |
↑ simeprevir | Concomitant use of OLYSIO with milk thistle may result in increased plasma concentrations of simeprevir due to CYP3A inhibition by milk thistle. It is not recommended to co-administer OLYSIO with milk thistle. |
| St. John's wort (Hypericum perforatum) | ↓ simeprevir | Concomitant use of OLYSIO with products containing St. John's wort may result in significantly decreased plasma concentrations of simeprevir due to CYP3A induction by St. John's wort. This may result in loss of therapeutic effect of OLYSIO. It is not recommended to co-administer OLYSIO with products containing St. John's wort. |
| HIV Products | ||
| Cobicistat-containing product (elvitegravir/cobicistat/ emtricitabine/tenofovir disoproxil fumarate) |
↑ simeprevir | Concomitant use of OLYSIO and a cobicistat-containing product (elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate) may result in significantly increased plasma concentrations of simeprevir due to strong CYP3A inhibition by cobicistat. It is not recommended to co-administer OLYSIO with a cobicistat-containing product. |
|
Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs):
Efavirenz  |
↓ simeprevir ↔ efavirenz |
Concomitant use of OLYSIO with efavirenz resulted in significantly decreased plasma concentrations of simeprevir due to CYP3A induction by efavirenz. This may result in loss of therapeutic effect of OLYSIO. It is not recommended to co-administer OLYSIO with efavirenz. |
|
Other NNRTIs
(Delavirdine, Etravirine, Nevirapine) |
↑ or ↓ simeprevir | Concomitant use of OLYSIO with delavirdine, etravirine or nevirapine may result in altered plasma concentrations of simeprevir due to CYP3A inhibition (delavirdine) or induction (etravirine and nevirapine) by these drugs. It is not recommended to co-administer OLYSIO with delavirdine, etravirine or nevirapine. |
|
Protease Inhibitors (PIs):
Darunavir/ritonavir  |
↑ simeprevir ↑ darunavir |
Concomitant use of OLYSIO with darunavir/ritonavir resulted in increased plasma concentrations of simeprevir due to CYP3A inhibition by darunavir/ritonavir. It is not recommended to co-administer darunavir/ritonavir and OLYSIO. |
|
Protease Inhibitors (PIs):
Ritonavir  |
↑ simeprevir | Concomitant use of OLYSIO with ritonavir resulted in significantly increased plasma concentrations of simeprevir due to strong CYP3A inhibition by ritonavir. It is not recommended to co-administer OLYSIO with ritonavir. |
| Other ritonavir-boosted or unboosted HIV PIs, e.g., Atazanavir, Fosamprenavir, Lopinavir, Indinavir, Nelfinavir, Saquinavir, Tipranavir | ↑ or ↓ simeprevir | Concomitant use of OLYSIO with ritonavir-boosted or unboosted HIV PIs may result in altered plasma concentrations of simeprevir due to CYP3A inhibition or induction by these HIV PIs. It is not recommended to co-administer OLYSIO with any HIV PI, with or without ritonavir. |
| HMG CO-A Reductase Inhibitors | ||
Rosuvastatin |
↑ rosuvastatin | Concomitant use of OLYSIO with rosuvastatin resulted in increased plasma concentrations of rosuvastatin due to inhibition of OATP1B1 by simeprevir. Initiate rosuvastatin therapy with 5 mg once daily. The rosuvastatin dose should not exceed 10 mg daily when co-administered with OLYSIO. |
Atorvastatin |
↑ atorvastatin | Concomitant use of OLYSIO with atorvastatin resulted in increased plasma concentrations of atorvastatin due to inhibition of OATP1B1 and/or CYP3A4 by simeprevir. Use the lowest necessary dose of atorvastatin, but do not exceed a daily dose of 40 mg when co-administering with OLYSIO. |
Simvastatin |
↑ simvastatin | Concomitant use of OLYSIO with simvastatin resulted in increased plasma concentrations of simvastatin due to inhibition of OATP1B1 and/or CYP3A4 by simeprevir. Titrate the simvastatin dose carefully and use the lowest necessary dose of simvastatin while monitoring for safety when co-administered with OLYSIO. |
| Pitavastatin Pravastatin Lovastatin |
↑ pitavastatin, pravastatin, lovastatin | Concomitant use of OLYSIO with pitavastatin, pravastatin or lovastatin has not been studied. The dose of pitavastatin, pravastatin or lovastatin should be titrated carefully and the lowest necessary dose should be used while monitoring for safety when co-administered with OLYSIO. |
| Immunosuppressants | ||
Cyclosporine |
↑ cyclosporine | No dose adjustment is required when OLYSIO is co-administered with cyclosporine. Routine monitoring of blood concentrations of cyclosporine is acceptable. |
Tacrolimus |
↓ tacrolimus | No dose adjustment is required when OLYSIO is co-administered with tacrolimus. Routine monitoring of blood concentrations of tacrolimus is acceptable. |
| Sirolimus | ↑ or ↓ sirolimus | Concomitant use of OLYSIO and sirolimus may result in mildly increased or decreased plasma concentrations of sirolimus. Routine monitoring of blood concentrations of sirolimus is acceptable. |
| Phosphodiesterase Type 5 (PDE-5) Inhibitors | ||
| Sildenafil Tadalafil Vardenafil |
↑ PDE-5 inhibitors | Concomitant use of OLYSIO with PDE-5 inhibitors may result in mild increases in concentrations of PDE-5 inhibitors due to intestinal CYP3A4 inhibition by simeprevir. No dose adjustment is required when OLYSIO is co-administered with doses of sildenafil, tadalafil or vardenafil indicated for the treatment of erectile dysfunction. Dose adjustment of the PDE-5 inhibitor may be required when OLYSIO is co-administered with sildenafil or tadalafil administered chronically at doses used for the treatment of pulmonary arterial hypertension. Consider starting with the lowest dose of the PDE-5 inhibitor and increase as needed, with clinical monitoring as appropriate. |
| Sedatives/Anxiolytics | ||
Midazolam |
↑ midazolam | Concomitant use of OLYSIO with orally administered midazolam resulted in increased plasma concentrations of midazolam due to mild inhibition of intestinal CYP3A4 by simeprevir. Caution is warranted when this drug, with a narrow therapeutic index, is co-administered with OLYSIO via the oral route. |
| Triazolam (oral administration) | ↑ triazolam | Concomitant use of OLYSIO with orally administered triazolam may result in mild increases in concentrations of triazolam due to intestinal CYP3A4 inhibition by simeprevir. Caution is warranted when this drug, with a narrow therapeutic index, is co-administered with OLYSIO via the oral route. |
In addition to the drugs included in Table 5, the interaction between OLYSIO and the following drugs were evaluated in clinical studies and no dose adjustments are needed for either drug [see Clinical Pharmacology (12.3)]: caffeine, dextromethorphan, escitalopram, ethinyl estradiol/norethindrone, methadone, midazolam (intravenous administration), omeprazole, raltegravir, rilpivirine, and tenofovir disoproxil fumarate.
No clinically relevant drug-drug interaction is expected when OLYSIO is co-administered with antacids, the corticosteroids budesonide, fluticasone, methylprednisolone, and prednisone, fluvastatin, H2-receptor antagonists, the narcotic analgesics buprenorphine and naloxone, NRTIs (such as abacavir, didanosine, emtricitabine, lamivudine, stavudine, zidovudine), maraviroc, methylphenidate, and proton pump inhibitors.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category X: Use with Ribavirin and Peginterferon Alfa
Extreme caution must be taken to avoid pregnancy in female patients and female partners of male patients while taking this combination. Women of childbearing potential and their male partners should not receive ribavirin unless they are using effective contraception (two reliable forms) during treatment with ribavirin and for 6 months after treatment.
A Ribavirin Pregnancy Registry has been established to monitor maternal-fetal outcomes of pregnancies in female patients and female partners of male patients exposed to ribavirin during treatment and for 6 months following cessation of treatment. Healthcare providers and patients are encouraged to report such cases by calling 1-800-593-2214.
Animal Data
Animal studies have shown that ribavirin causes birth defects and/or fetal deaths while peginterferon alfa is abortifacient [see Contraindications (4) and Warnings and Precautions (5.1)]. See the prescribing information for ribavirin. Significant teratogenic and/or embryocidal effects have been demonstrated in all animal species exposed to ribavirin; and therefore ribavirin is contraindicated in women who are pregnant and in the male partners of women who are pregnant [see Contraindications (4) , Warnings and Precautions (5.1) and ribavirin prescribing information]. Interferons have abortifacient effects in animals and should be assumed to have abortifacient potential in humans [see peginterferon alfa prescribing information].
Pregnancy Category C: OLYSIO
There are no adequate and well-controlled studies with OLYSIO alone or in combination with peginterferon alfa and ribavirin in pregnant women.
Animal Data
Simeprevir showed no teratogenicity in rats and mice at exposures 0.5 times (in rats) and 6 times (in mice) the mean AUC in humans at the recommended dose of 150 mg once daily.
In a mouse embryofetal study at doses up to 1000 mg/kg, simeprevir resulted in early and late in utero fetal losses and early maternal deaths at an exposure approximately 6 times higher than the mean AUC in humans at the recommended 150 mg daily dose. Significantly decreased fetal weights and an increase in fetal skeletal variations were seen at exposures approximately 4 times higher than the mean AUC in humans at the recommended daily dose.
In a rat pre- and postnatal study, maternal animals were exposed to simeprevir during gestation and lactation at doses up to 1000 mg/kg/day. In pregnant rats, simeprevir resulted in early deaths at 1000 mg/kg/day corresponding to exposures similar to the mean clinical AUC. Significant reduction in body weight gain was seen from 500 mg/kg/day onwards at an exposure 0.7 times the mean clinical AUC. The developing rat offspring exhibited significant decreased body weight and negative effects on physical growth (delay and small size) and development (decreased motor activity) following simeprevir exposure in utero (via maternal dosing) and during lactation (via maternal milk to nursing pups) at a maternal exposure similar to the mean clinical AUC at the recommended 150 mg once daily dose. Subsequent survival, behavior and reproductive capacity were not affected.
8.3 Nursing Mothers
It is not known whether simeprevir or its metabolites are excreted in human breast milk. When administered to lactating rats, simeprevir was detected in plasma of suckling rats likely due to excretion of simeprevir via milk. Because of the potential for adverse reactions from the drug in nursing infants, a decision must be made whether to discontinue nursing or discontinue treatment with OLYSIO, taking into account the importance of the therapy to the mother.
8.4 Pediatric Use
The safety and efficacy of OLYSIO in children and adolescents less than 18 years of age have not been established.
8.5 Geriatric Use
Clinical studies of OLYSIO did not include sufficient numbers of patients older than 65 years to determine whether they respond differently from younger patients. No dose adjustment of OLYSIO is required in geriatric patients [see Clinical Pharmacology (12.3)].
8.6 Race
Patients of East Asian ancestry exhibit higher simeprevir exposures [see Clinical Pharmacology (12.3)]. In clinical trials, higher simeprevir exposures have been associated with increased frequency of adverse reactions, including rash and photosensitivity [see Adverse Reactions (6.1)]. There are insufficient safety data to recommend an appropriate dose for patients of East Asian ancestry. The potential risks and benefits of OLYSIO should be carefully considered prior to use in patients of East Asian ancestry.
8.7 Renal Impairment
No dose adjustment of OLYSIO is required in patients with mild, moderate or severe renal impairment [see Clinical Pharmacology (12.3)]. The safety and efficacy of OLYSIO have not been studied in HCV-infected patients with severe renal impairment (creatinine clearance below 30 mL/min) or end-stage renal disease, including patients requiring dialysis. Simeprevir is highly protein-bound; therefore, dialysis is unlikely to result in significant removal of simeprevir [see Clinical Pharmacology (12.3)].
Refer to the respective prescribing information for peginterferon alfa and ribavirin regarding use in patients with renal impairment.
8.8 Hepatic Impairment
No dose adjustment of OLYSIO is required in patients with mild hepatic impairment (Child-Pugh Class A); no dose recommendation can be given for patients with moderate or severe hepatic impairment (Child-Pugh Class B or C) due to higher simeprevir exposures [see Clinical Pharmacology (12.3)]. In clinical trials, higher simeprevir exposures have been associated with increased frequency of adverse reactions, including rash and photosensitivity [see Adverse Reactions (6.1)].
The safety and efficacy of OLYSIO have not been studied in HCV-infected patients with moderate or severe hepatic impairment (Child-Pugh Class B or C). The combination of peginterferon alfa and ribavirin is contraindicated in patients with decompensated cirrhosis (moderate or severe hepatic impairment). The potential risks and benefits of OLYSIO should be carefully considered prior to use in patients with moderate or severe hepatic impairment.
8.9 Other HCV Genotypes
The safety and efficacy of OLYSIO in combination with peginterferon alfa and ribavirin has not been established in patients with other HCV genotypes.
8.10 Liver Transplantation
The safety and efficacy of OLYSIO alone or in combination with peginterferon alfa and ribavirin have not been studied in liver transplant patients.
10 OVERDOSAGE
Human experience of overdose with OLYSIO is limited. There is no specific antidote for overdose with OLYSIO. In the event of an overdose, patient's clinical status should be observed and the usual supportive measures employed.
Simeprevir is highly protein-bound; therefore, dialysis is unlikely to result in significant removal of simeprevir [see Clinical Pharmacology (12.3)].
11 DESCRIPTION
OLYSIO (simeprevir) is an inhibitor of the HCV NS3/4A protease.
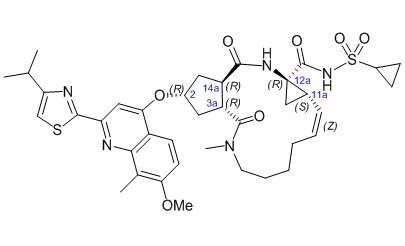
The chemical name for simeprevir is (2R,3aR,10Z,11aS,12aR,14aR)-N-(cyclopropylsulfonyl)-2-[[2-(4-isopropyl-1,3-thiazol-2-yl)-7-methoxy-8-methyl-4-quinolinyl]oxy]-5-methyl-4,14-dioxo-2,3,3a,4,5,6,7,8,9,11a,12,13,14,14a-tetradecahydrocyclopenta[c]cyclopropa[g][1,6]diazacyclotetradecine-12a(1H)-carboxamide. Its molecular formula is C38H47N5O7S2 and its molecular weight is 749.94. Simeprevir has the following structural formula:
Simeprevir drug substance is a white to almost white powder. Simeprevir is practically insoluble in water over a wide pH range. It is practically insoluble in propylene glycol, very slightly soluble in ethanol, and slightly soluble in acetone. It is soluble in dichloromethane and freely soluble in some organic solvents (e.g., tetrahydrofuran and N,N-dimethylformamide).
OLYSIO (simeprevir) for oral administration is available as 150 mg strength hard gelatin capsules. Each capsule contains 154.4 mg of simeprevir sodium salt, which is equivalent to 150 mg of simeprevir. OLYSIO (simeprevir) capsules contain the following inactive ingredients: colloidal anhydrous silica, croscarmellose sodium, lactose monohydrate, magnesium stearate and sodium lauryl sulphate. The white capsule contains gelatin and titanium dioxide (E171) and is printed with ink containing iron oxide black (E172) and shellac (E904).
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Simeprevir is a direct-acting antiviral (DAA) agent against the hepatitis C virus [see Microbiology (12.4)].
12.2 Pharmacodynamics
Evaluation of Effects on Electrocardiogram
The effect of simeprevir 150 mg once daily and 350 mg once daily for 7 days on the QT interval was evaluated in a randomized, double-blind, placebo- and positive-controlled (moxifloxacin 400 mg once daily), 4-way cross-over study in 60 healthy subjects. No meaningful changes in QTc interval were observed with either the recommended dose of 150 mg once daily or the supratherapeutic dose of 350 mg once daily.
12.3 Pharmacokinetics
The pharmacokinetic properties of simeprevir have been evaluated in healthy adult subjects and in adult HCV-infected subjects. Plasma Cmax and the area under the plasma concentration time curve (AUC) increased more than dose-proportionally after multiple doses between 75 mg and 200 mg once daily, with accumulation occurring following repeated dosing. Steady-state was reached after 7 days of once daily dosing. Plasma exposure (AUC) of simeprevir in HCV-infected subjects was about 2- to 3-fold higher compared to that observed in HCV-uninfected subjects. Plasma Cmax and AUC of simeprevir were similar during co-administration of simeprevir with peginterferon alfa and ribavirin compared with administration of simeprevir alone. In HCV-infected subjects, the mean steady-state predose plasma concentration was 1936 ng/mL (standard deviation: 2640) and the mean steady-state AUC24 was 57469 ng.h/mL (standard deviation: 63571).
Absorption
Simeprevir is orally bioavailable. Maximum plasma concentrations (Cmax) are typically achieved between 4 to 6 hours post dose.
In vitro studies with human Caco-2 cells indicated that simeprevir is a substrate of P-gp.
Effects of Food on Oral Absorption
Administration of simeprevir with food to healthy subjects increased the relative bioavailability (AUC) by 61% and 69% after a high-fat, high-caloric (928 kcal) and normal-caloric (533 kcal) breakfast, respectively, and delayed the absorption by 1 hour and 1.5 hours, respectively.
Distribution
Simeprevir is extensively bound to plasma proteins (greater than 99.9%), primarily to albumin and, to a lesser extent, alfa 1-acid glycoprotein. Plasma protein binding is not meaningfully altered in patients with renal or hepatic impairment.
In animals, simeprevir is extensively distributed to gut and liver (liver:blood ratio of 29:1 in rat) tissues. In vitro data and physiologically-based pharmacokinetic modeling and simulations indicate that hepatic uptake in humans is mediated by OATP1B1/3.
Metabolism
Simeprevir is metabolized in the liver. In vitro experiments with human liver microsomes indicated that simeprevir primarily undergoes oxidative metabolism by the hepatic CYP3A system. Involvement of CYP2C8 and CYP2C19 cannot be excluded. Co-administration of OLYSIO with moderate or strong inhibitors of CYP3A may significantly increase the plasma exposure of simeprevir, and co-administration with moderate or strong inducers of CYP3A may significantly reduce the plasma exposure of simeprevir [see Drug Interactions (7)].
Following a single oral administration of 200 mg 14C-simeprevir to healthy subjects, the majority of the radioactivity in plasma (mean: 83%) was accounted for by unchanged drug and a small part of the radioactivity in plasma was related to metabolites (none being major metabolites). Metabolites identified in feces were formed via oxidation at the macrocyclic moiety or aromatic moiety or both and by O-demethylation followed by oxidation.
Elimination
Elimination of simeprevir occurs via biliary excretion. Renal clearance plays an insignificant role in its elimination. Following a single oral administration of 200 mg 14C-simeprevir to healthy subjects, on average 91% of the total radioactivity was recovered in feces. Less than 1% of the administered dose was recovered in urine. Unchanged simeprevir in feces accounted for on average 31% of the administered dose.
The terminal elimination half-life of simeprevir was 10 to 13 hours in HCV-uninfected subjects and 41 hours in HCV-infected subjects receiving 200 mg simeprevir.
Specific Populations
Geriatric Use
There is limited data on the use of OLYSIO in patients aged 65 years and older. Age (18–73 years) had no clinically meaningful effect on the pharmacokinetics of simeprevir based on a population pharmacokinetic analysis of HCV-infected subjects treated with OLYSIO. No dose adjustment of OLYSIO is required in geriatric patients [see Use in Specific Populations (8.5)].
Renal Impairment
Renal elimination of simeprevir is negligible. Compared to HCV-uninfected subjects with normal renal function (classified using the Modification of Diet in Renal Disease [MDRD] eGFR formula; eGFR greater than or equal to 80 mL/min) the mean steady-state AUC of simeprevir was 62% higher in HCV-uninfected subjects with severe renal impairment (eGFR below 30 mL/min). Based on the observed and expected changes in simeprevir exposure, no dose adjustment of OLYSIO is needed in patients with mild, moderate or severe renal impairment. The safety and efficacy of OLYSIO have not been studied in HCV-infected patients with severe renal impairment or end-stage renal disease, including patients requiring dialysis [see Use in Specific Populations (8.7)].
In a population pharmacokinetic analysis of mild or moderate renally impaired HCV-infected subjects treated with OLYSIO 150 mg once daily, creatinine clearance was not found to influence the pharmacokinetic parameters of simeprevir. It is therefore not expected that renal impairment will have a clinically relevant effect on the exposure to simeprevir.
As simeprevir is highly bound to plasma proteins, it is unlikely that it will be significantly removed by dialysis.
Refer to the respective prescribing information for peginterferon alfa and ribavirin regarding use in patients with renal impairment.
Hepatic Impairment
Simeprevir is primarily metabolized by the liver. Compared to HCV-uninfected subjects with normal hepatic function, the mean steady-state AUC of simeprevir was 2.4-fold higher in HCV-uninfected subjects with moderate hepatic impairment (Child-Pugh Class B) and 5.2-fold higher in HCV-uninfected subjects with severe hepatic impairment (Child-Pugh Class C). No dose adjustment of OLYSIO is necessary in patients with mild hepatic impairment (Child-Pugh Class A). The safety and efficacy of OLYSIO have not been studied in HCV-infected patients with moderate or severe hepatic impairment (Child-Pugh Class B or C). In clinical trials, higher simeprevir exposures have been associated with increased frequency of adverse reactions, including rash and photosensitivity. No dose recommendation can be given for patients with moderate or severe hepatic impairment (Child-Pugh Class B or C). The potential risks and benefits of OLYSIO should be carefully considered prior to use in patients with moderate or severe hepatic impairment [see Dosage and Administration (2.4) and Use in Specific Populations (8.8)].
Based on a population pharmacokinetic analysis of HCV-infected subjects treated with OLYSIO, liver fibrosis stage did not have a clinically relevant effect on the pharmacokinetics of simeprevir.
Refer to the respective prescribing information for peginterferon alfa and ribavirin regarding use in patients with hepatic impairment.
Gender, Body Weight, Body Mass Index
No dose adjustment is necessary based on gender, body weight or body mass index. These characteristics have no clinically meaningful relevant effect on the pharmacokinetics of simeprevir based on a population pharmacokinetic analysis of HCV-infected subjects treated with OLYSIO.
Race
Based on results from studies in HCV-uninfected subjects and HCV-infected subjects, simeprevir exposures are higher in Asians compared to Caucasians. In the Phase 3 trials, the mean simeprevir plasma exposure in Asian subjects (n=14) was 3.4-fold higher than in the pooled Phase 3 population. In clinical trials, higher simeprevir exposures have been associated with increased frequency of adverse reactions, including rash and photosensitivity. There are insufficient safety data to recommend an appropriate dose for patients of East Asian ancestry. The potential risks and benefits of OLYSIO should be carefully considered prior to use in patients of East Asian ancestry [see Dosage and Administration (2.5) and Use in Specific Populations (8.6)].
Population pharmacokinetic estimates of exposure of simeprevir were comparable between Caucasian and Black/African American HCV-infected subjects.
Drug Interactions
[See also Warnings and Precautions (5.6) and Drug Interactions (7).]
In vitro studies indicated that simeprevir is a substrate and mild inhibitor of CYP3A and a substrate and inhibitor of P-gp and OATP1B1/3. Simeprevir does not affect CYP2C9, CYP2C19 or CYP2D6 in vivo. Simeprevir does not induce CYP1A2 or CYP3A4 in vitro. In vivo, simeprevir mildly inhibits the CYP1A2 activity and intestinal CYP3A4 activity, while it does not affect hepatic CYP3A4 activity.
Simeprevir is transported into the liver by OATP1B1/3 where it undergoes metabolism by CYP3A. Based on results from in vivo studies, co-administration of OLYSIO with moderate or strong inhibitors of CYP3A may significantly increase the plasma exposure of simeprevir and co-administration with moderate or strong inducers of CYP3A may significantly reduce the plasma exposure of simeprevir, which may lead to loss of efficacy.
Drug interaction studies were performed in healthy adults with simeprevir (at the recommended dose of 150 mg once daily unless otherwise noted) and drugs likely to be co-administered or drugs commonly used as probes for pharmacokinetic interactions. The effects of co-administration of other drugs on the Cmax, AUC, and Cmin values of simeprevir are summarized in Table 6 (effect of other drugs on OLYSIO). The effect of co-administration of OLYSIO on the Cmax, AUC, and Cmin values of other drugs are summarized in Table 7 (effect of OLYSIO on other drugs). For information regarding clinical recommendations, see Drug Interactions (7) .
| Drug | Dose and Schedule | N | Effect on PK |
LS Mean Ratio (90% CI) of Simeprevir PK Parameters with/without Drug | |||
|---|---|---|---|---|---|---|---|
| Drug | Simeprevir | Cmax | AUC | Cmin | |||
| CI = Confidence Interval; N = number of subjects with data; NA = not available; PK = pharmacokinetics; LS = least square; q.d. = once daily; b.i.d. = twice daily; t.i.d. = three times a day | |||||||
| Erythromycin | 500 mg t.i.d. for 7 days | 150 mg q.d. for 7 days | 24 | ↑ | 4.53 (3.91–5.25) |
7.47 (6.41–8.70) |
12.74 (10.19–15.93) |
| Escitalopram | 10 mg q.d. for 7 days | 150 mg q.d. for 7 days | 18 | ↓ | 0.80 (0.71–0.89) |
0.75 (0.68–0.83) |
0.68 (0.59–0.79) |
| Rifampin | 600 mg q.d. for 7 days | 200 mg q.d. for 7 days | 18 | ↓ | 1.31 (1.03–1.66) |
0.52 (0.41–0.67) |
0.08 (0.06–0.11) |
| Anti-HIV Drugs | |||||||
| Darunavir/Ritonavir |
800/100 mg q.d. for 7 days | 50 mg and 150 mg q.d. for 7 days | 25 | ↑ | 1.79 (1.55–2.06) |
2.59 (2.15–3.11) |
4.58 (3.54–5.92) |
| Efavirenz | 600 mg q.d. for 14 days | 150 mg q.d. for 14 days | 23 | ↓ | 0.49 (0.44–0.54) |
0.29 (0.26–0.33) |
0.09 (0.08–0.12) |
| Raltegravir | 400 mg b.i.d. for 7 days | 150 mg q.d. for 7 days | 24 | ↔ | 0.93 (0.85–1.02) |
0.89 (0.81–0.98) |
0.86 (0.75–0.98) |
| Rilpivirine | 25 mg q.d. for 11 days | 150 mg q.d. for 11 days | 21 | ↔ | 1.10 (0.97–1.26) |
1.06 (0.94–1.19) |
0.96 (0.83–1.11) |
| Ritonavir | 100 mg b.i.d. for 15 days | 200 mg q.d. for 7 days | 12 | ↑ | 4.70 (3.84–5.76) |
7.18 (5.63–9.15) |
14.35 (10.29–20.01) |
| Tenofovir disoproxil fumarate | 300 mg q.d. for 7 days | 150 mg q.d. for 7 days | 24 | ↓ | 0.85 (0.73–0.99) |
0.86 (0.76–0.98) |
0.93 (0.78–1.11) |
| Drug | Dose and Schedule | N | Effect on PK |
LS Mean Ratio (90% CI) of Co-Administered Drug PK Parameters with/without OLYSIO | |||
|---|---|---|---|---|---|---|---|
| Drug | Simeprevir | Cmax | AUC | Cmin | |||
| CI = Confidence Interval; i.v.= intravenous; N = number of subjects with data; NA = not available; PK = pharmacokinetics; LS = least square; q.d. = once daily; b.i.d. = twice daily; t.i.d. = three times a day | |||||||
| Atorvastatin | 40 mg single dose | 150 mg q.d. for 10 days | 18 | ↑ | 1.70 (1.42–2.04) |
2.12 (1.72–2.62) |
NA |
| 2-hydroxy-atorvastatin | ↑ | 1.98 (1.70–2.31) |
2.29 (2.08–2.52) |
NA | |||
| Caffeine |
150 mg | 150 mg q.d. for 11 days | 16 | ↑ | 1.12 (1.06–1.19) |
1.26 (1.21–1.32) |
NA |
| Cyclosporine | 100 mg single dose | 150 mg q.d. for 7 days | 14 | ↑ | 1.16 (1.07–1.26) |
1.19 (1.13–1.26) |
NA |
| Dextromethorphan | 30 mg | 150 mg q.d. for 11 days | 16 | ↑ | 1.21 (0.93–1.57) |
1.08 (0.87–1.35) |
NA |
| Dextrorphan | ↔ | 1.03 (0.93–1.15) |
1.09 (1.03–1.15) |
NA | |||
| Digoxin | 0.25 mg single dose | 150 mg q.d. for 7 days | 16 | ↑ | 1.31 (1.14–1.51) |
1.39 (1.16–1.67) |
NA |
| Erythromycin | 500 mg t.i.d. for 7 days | 150 mg q.d. for 7 days | 24 | ↑ | 1.59 (1.23–2.05) |
1.90 (1.53–2.36) |
3.08 (2.54–3.73) |
| Escitalopram | 10 mg q.d. for 7 days | 150 mg q.d. for 7 days | 17 | ↔ | 1.03 (0.99–1.07) |
1.00 (0.97–1.03) |
1.00 (0.95–1.05) |
| Ethinyl estradiol (EE), co-administered with norethindrone (NE) | 0.035 mg q.d. EE + 1 mg q.d. NE for 21 days | 150 mg q.d. for 10 days | 18 | ↔ | 1.18 (1.09–1.27) |
1.12 (1.05–1.20) |
1.00 (0.89–1.13) |
| Midazolam (oral) | 0.075 mg/kg | 150 mg q.d. for 10 days | 16 | ↑ | 1.31 (1.19–1.45) |
1.45 (1.35–1.57) |
NA |
| Midazolam (i.v.) | 0.025 mg/kg | 150 mg q.d. for 11 days | 16 | ↑ | 0.78 (0.52–1.17) |
1.10 (0.95–1.26) |
NA |
| R(-) methadone |
30–150 mg q.d., individualised dose | 150 mg q.d. for 7 days | 12 | ↔ | 1.03 (0.97–1.09) |
0.99 (0.91–1.09) |
1.02 (0.93–1.12) |
| Norethindrone (NE), co-administered with EE | 0.035 mg q.d. EE + 1 mg q.d. NE for 21 days | 150 mg q.d. for 10 days | 18 | ↔ | 1.06 (0.99–1.14) |
1.15 (1.08–1.22) |
1.24 (1.13–1.35) |
| Omeprazole | 40 mg single dose | 150 mg q.d. for 11 days | 16 | ↑ | 1.14 (0.93–1.39) |
1.21 (1.00–1.46) |
NA |
| Rifampin | 600 mg q.d. for 7 days | 200 mg q.d. for 7 days | 18 | ↔ | 0.92 (0.80–1.07) |
1.00 (0.93–1.08) |
NA |
| 25-desacetyl-rifampin | 17 | ↑ | 1.08 (0.98–1.19) |
1.24 (1.13–1.36) |
NA | ||
| Rosuvastatin | 10 mg single dose | 150 mg q.d. for 7 days | 16 | ↑ | 3.17 (2.57–3.91) |
2.81 (2.34–3.37) |
NA |
| Simvastatin | 40 mg single dose | 150 mg q.d. for 10 days | 18 | ↑ | 1.46 (1.17–1.82) |
1.51 (1.32–1.73) |
NA |
| Simvastatin acid | ↑ | 3.03 (2.49–3.69) |
1.88 (1.63–2.17) |
NA | |||
| Tacrolimus | 2 mg single dose | 150 mg q.d. for 7 days | 14 | ↓ | 0.76 (0.65–0.90) |
0.83 (0.59–1.16) |
NA |
| S-Warfarin | 10 mg single dose | 150 mg q.d. for 11 days | 16 | ↔ | 1.00 (0.94–1.06) |
1.04 (1.00–1.07) |
NA |
| Anti-HIV Drugs | |||||||
Darunavir |
800mg q.d. for 7 days | 50 mg q.d. for 7 days | 25 | ↑ | 1.04 (0.99–1.10) |
1.18 (1.11–1.25) |
1.31 (1.13–1.52) |
Ritonavir |
100 mg q.d. for 7 days | ↑ | 1.23 (1.44–1.32) |
1.32 (1.25–1.40) |
1.44 (1.30–1.61) |
||
| Efavirenz | 600 mg q.d. for 14 days | 150 mg q.d. for 14 days | 23 | ↔ | 0.97 (0.89–1.06) |
0.90 (0.85–0.95) |
0.87 (0.81–0.93) |
| Raltegravir | 400 mg b.i.d. for 7 days | 150 mg q.d. for 7 days | 24 | ↑ | 1.03 (0.78–1.36) |
1.08 (0.85–1.38) |
1.14 (0.97–1.36) |
| Rilpivirine | 25 mg q.d. for 11 days | 150 mg q.d. for 11 days | 23 | ↔ | 1.04 (0.95–1.13) |
1.12 (1.05–1.19) |
1.25 (1.16–1.35) |
| Tenofovir disoproxil fumarate | 300 mg q.d. for 7 days | 150 mg q.d. for 7 days | 24 | ↔ | 1.19 (1.10–1.30) |
1.18 (1.13–1.24) |
1.24 (1.15–1.33) |
12.4 Microbiology
Mechanism of Action
Simeprevir is an inhibitor of the HCV NS3/4A protease which is essential for viral replication. In a biochemical assay simeprevir inhibited the proteolytic activity of recombinant genotype 1a and 1b HCV NS3/4A proteases, with median Ki values of 0.5 nM and 1.4 nM, respectively.
Antiviral Activity
The median simeprevir EC50 and EC90 values against a HCV genotype 1b replicon were 9.4 nM (7.05 ng/mL) and 19 nM (14.25 ng/mL), respectively. Activity of simeprevir against a selection of genotype 1a (N=78) and genotype 1b (N=59) chimeric replicons carrying NS3 sequences derived from HCV NS3/4A protease-inhibitor-naïve subjects resulted in median fold change (FC) in EC50 values of 1.4 (interquartile range, IQR: 0.8 to 11) and 0.4 (IQR: 0.3 to 0.7) compared to reference genotype 1b replicon, respectively. Genotype 1a (N=33) and 1b (N=2) isolates with a baseline Q80K polymorphism resulted in median FC in simeprevir EC50 value of 11 (IQR: 7.4 to 13) and 8.4, respectively. The presence of 50% human serum reduced simeprevir replicon activity by 2.4-fold. Combination of simeprevir with interferon, ribavirin, NS5A inhibitors, NS5B nucleoside analog polymerase inhibitors or NS5B non-nucleoside analog polymerase inhibitors, including NS5B thumb 1-, thumb 2-, and palm-domain targeting drugs, was not antagonistic.
Resistance in Cell Culture
Resistance to simeprevir was characterized in HCV genotype 1a and 1b replicon-containing cells. Ninety-six percent (96%) of simeprevir-selected genotype 1 replicons carried one or multiple amino acid substitutions at NS3 protease positions F43, Q80, R155, A156, and/or D168, with substitutions at NS3 position D168 being most frequently observed (78%). Additionally, resistance to simeprevir was evaluated in HCV genotype 1a and 1b replicon assays using site-directed mutants and chimeric replicons carrying NS3 sequences derived from clinical isolates. Amino acid substitutions at NS3 positions F43, Q80, S122, R155, A156, and D168 reduced susceptibility to simeprevir. Replicons with D168V or A, and R155K substitutions displayed large reductions in susceptibility to simeprevir (FC in EC50 value greater than 50), whereas other substitutions such as Q80K or R, S122R, and D168E displayed lower reductions in susceptibility (FC in EC50 value between 2 and 50). Other substitutions such as Q80G or L, S122G, N or T did not reduce susceptibility to simeprevir in the replicon assay (FC in EC50 value lower than 2). Amino acid substitutions at NS3 positions Q80, S122, R155, and/or D168 that were associated with lower reductions in susceptibility to simeprevir when occurring alone, reduced susceptibility to simeprevir by more than 50-fold when present in combination.
Resistance in Clinical Studies
In a pooled analysis of subjects treated with 150 mg OLYSIO in combination with peginterferon alfa and ribavirin who did not achieve SVR in the controlled Phase 2b and Phase 3 clinical trials, emerging amino acid substitutions at NS3 positions Q80, S122, R155 and/or D168 were observed in 180 out of 197 (91%) subjects. Substitutions D168V and R155K alone or in combination with other substitutions at these positions emerged most frequently (Table 8). Most of these emerging substitutions have been shown to reduce susceptibility to simeprevir in cell culture replicon assays.
HCV genotype 1 subtype-specific patterns of simeprevir treatment-emergent amino acid substitutions were observed in subjects not achieving SVR. Subjects with HCV genotype 1a predominately had emerging R155K alone or in combination with amino acid substitutions at NS3 positions Q80, S122 and/or D168, while subjects with HCV genotype 1b had most often an emerging D168V substitution (Table 8). In subjects with HCV genotype 1a with a baseline Q80K amino acid substitution an emerging R155K substitution was observed most frequently at failure.
| Emerging Amino Acid Substitutions in NS3 | Genotype 1a N=116 % (n) |
Genotype 1b N=81 % (n) |
|---|---|---|
| Note: substitutions at NS3 position F43 and A156 were selected in cell culture and associated with reduced simeprevir activity in the replicon assay but were not observed at time of failure. | ||
| Any substitution at NS3 position F43, Q80, S122, R155, A156, or D168 |
95 (110) | 86 (70) |
| D168E | 15 (17) | 17 (14) |
| D168V | 10 (12) | 61 (49) |
Q80R |
4 (5) | 12 (10) |
| R155K | 77 (89) | 0 (0) |
Q80X+D168X |
4 (5) | 14 (11) |
R155X+D168X |
13 (15) | 4 (3) |
Q80K   |
Less than 10% | Less than 10% |
Persistence of Resistance–Associated Substitutions
The persistence of simeprevir-resistant NS3 amino acid substitutions was assessed following treatment failure in the pooled analysis of subjects receiving 150 mg OLYSIO in combination with peginterferon alfa and ribavirin in the Phase 2b and Phase 3 trials. The proportion of subjects with detectable levels of treatment-emergent, resistance-associated variants was followed post treatment for a median time of 28 weeks (range 0 to 70 weeks). Resistant variants remained at detectable levels in 32 out of 66 subjects (48%) with single emerging R155K and in 16 out of 48 subjects (33%) with single emerging D168V.
The lack of detection of virus containing a resistance-associated substitution does not necessarily indicate that the resistant virus is no longer present at clinically significant levels. The long-term clinical impact of the emergence or persistence of virus containing OLYSIO-resistance-associated substitutions is unknown.
Effect of Baseline HCV Polymorphisms on Treatment Response
Analyses were conducted to explore the association between naturally-occurring baseline NS3/4A amino acid substitutions (polymorphisms) and treatment outcome. In the pooled analysis of the Phase 3 trials QUEST 1 and QUEST 2, and in the PROMISE trial, the efficacy of OLYSIO in combination with peginterferon alfa and ribavirin was substantially reduced in subjects infected with HCV genotype 1a virus with the NS3 Q80K polymorphism at baseline [see Clinical Pharmacology (12.5) and Clinical Studies (14)].
The observed prevalence of NS3 Q80K polymorphic variants at baseline in the overall population of the Phase 2b and Phase 3 trials was 14%; while the observed prevalence of the Q80K polymorphism was 30% in subjects infected with HCV genotype 1a and 0.5% in subjects infected with HCV genotype 1b. The observed prevalence of Q80K polymorphic variants at baseline in the U.S. population of the Phase 2b and Phase 3 trials was 35% overall, 48% in subjects infected with HCV genotype 1a and 0% in subjects infected with HCV genotype 1b. With the exception of the NS3 Q80K substitution, baseline polymorphic variants at NS3 positions F43, Q80, S122, R155, A156, and/or D168, which were associated with reduced simeprevir activity in replicon assays, were generally uncommon (1.3%) in subjects with HCV genotype 1 infection in the Phase 2b and Phase 3 trials (n=2007).
Cross-Resistance
Cross-resistance is expected among NS3/4A protease inhibitors. Some of the treatment-emergent NS3 amino acid substitutions detected in OLYSIO-treated subjects who did not achieve SVR in clinical trials, including R155K, which emerged frequently, and I170T, which emerged infrequently, have been shown to reduce the anti-HCV activity of the NS3/4A protease inhibitors, boceprevir and/or telaprevir.
The most frequently occurring boceprevir or telaprevir treatment-emergent NS3 amino acid substitutions that are expected to impact subsequent treatment with OLYSIO include R155K and A156T or V. The NS3 amino substitutions V36A or G and I170A or T, which displayed slight shifts in susceptibility to simeprevir in replicon cultures, may emerge in patients who do not achieve SVR with boceprevir or telaprevir, and may therefore also impact subsequent treatment with OLYSIO.
12.5 Pharmacogenomics
A genetic variant near the gene encoding interferon-lambda-3 (IL28B rs12979860, a C to T change) is a strong predictor of response to peginterferon alfa and ribavirin (PR). In the Phase 3 trials, IL28B genotype was a stratification factor.
Overall, SVR rates were lower in subjects with the CT and TT genotypes compared to those with the CC genotype. Among both treatment-naïve subjects and those who experienced previous treatment failures, subjects of all IL28B genotypes had the highest SVR rates with OLYSIO-containing regimens (Table 9).
| Trial (Population) | IL28B rs12979860 Genotype | OLYSIO + PR % (n/N) |
Placebo + PR % (n/N) |
|---|---|---|---|
| SVR12: sustained virologic response 12 weeks after planned end of treatment (EOT). | |||
|
QUEST 1 and QUEST 2 (treatment-naïve) |
C/C | 95 (144/152) | 80 (63/79) |
| C/T | 78 (228/292) | 41 (61/147) | |
| T/T | 61 (47/77) | 21 (8/38) | |
|
PROMISE (prior relapser) |
C/C | 89 (55/62) | 53 (18/34) |
| C/T | 78 (131/167) | 34 (28/83) | |
| T/T | 65 (20/31) | 19 (3/16) | |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Use with Ribavirin and Peginterferon alfa: Ribavirin is genotoxic in in vitro and in vivo assays. Ribavirin was not oncogenic in a 6-month p53+/- transgenic mouse study or a 2-year carcinogenicity study in rats. See the prescribing information for ribavirin.
Simeprevir was not genotoxic in a series of in vitro and in vivo tests including the Ames test, the mammalian forward mutation assay in mouse lymphoma cells or the in vivo mammalian micronucleus test. Carcinogenicity studies with simeprevir have not been conducted.
Fertility
Use with Ribavirin and Peginterferon alfa: Animal studies have shown that ribavirin induced reversible toxicity in males while peginterferon alfa may impair female fertility. See the prescribing information for ribavirin and peginterferon alfa.
In a rat fertility study at doses up to 500 mg/kg/day, 3 male rats treated with simeprevir (2/24 at 50 mg/kg/day and 1/24 rats at 500 mg/kg/day) showed no motile sperm, small testes and epididymides that resulted in infertility in 2 out of 3 of the male rats at approximately 0.2 times the mean AUC in humans.
13.2 Animal Toxicology and/or Pharmacology
Cardiovascular toxicity consisting of acute endocardial and myocardial necrosis restricted to the left ventricular subendocardial area was seen in 2 out of 6 animals in a 2-week oral dog toxicity study at an exposure approximately 28 times the mean AUC in humans at the recommended daily dose of 150 mg. No cardiac findings were observed in a 6-month and a 9-month oral toxicity study at exposures, respectively, of 11 and 4 times the mean AUC in humans at the recommended daily dose of 150 mg.
14 CLINICAL STUDIES
The efficacy of OLYSIO in patients with HCV genotype 1 infection was evaluated in two Phase 3 trials in treatment-naïve subjects (trials QUEST 1 and QUEST 2), one Phase 3 trial in subjects who relapsed after prior interferon-based therapy (PROMISE) and one Phase 2b trial in subjects who failed prior therapy with peginterferon (Peg-IFN) and ribavirin (RBV) (including prior relapsers, partial and null responders) (ASPIRE). Prior relapsers were subjects who had undetectable HCV RNA at the end of prior IFN-based therapy and detectable HCV RNA during follow-up; prior partial responders were subjects with prior on-treatment greater than or equal to 2 log10 reduction in HCV RNA from baseline at Week 12 and detectable HCV RNA at the end of prior therapy with Peg-IFN and RBV; and null responders were subjects with prior on-treatment less than 2 log10 reduction in HCV RNA from baseline at Week 12 during prior therapy with Peg-IFN and RBV. Subjects in these trials had compensated liver disease (including cirrhosis), HCV RNA of at least 10000 IU/mL, and liver histopathology consistent with CHC.
In subjects who were treatment-naïve and prior relapsers, the overall duration of treatment with Peg-IFN-alfa and RBV in the Phase 3 trials was response-guided. In these subjects, the planned total duration of HCV treatment was 24 weeks if the following on-treatment protocol-defined response-guided therapy (RGT) criteria were met: HCV RNA lower than 25 IU/mL (detectable or undetectable) at Week 4 AND undetectable HCV RNA at Week 12. Plasma HCV RNA levels were measured using the Roche COBAS® TaqMan® HCV test (version 2.0), for use with the High Pure System (25 IU/mL LLOQ and 15 IU/mL limit of detection). Treatment stopping rules for HCV therapy were used to ensure that subjects with inadequate on-treatment virologic response discontinued treatment in a timely manner.
SVR (virologic cure) was defined as undetectable HCV RNA 24 weeks after planned end of treatment (SVR24) in the Phase 2b trial and was defined as HCV RNA lower than 25 IU/mL detectable or undetectable 12 weeks after the planned end of treatment (SVR12) in the Phase 3 trials.
14.1 Treatment-Naïve Adult Subjects with HCV Genotype 1 Infection
The efficacy of OLYSIO in treatment-naïve patients with HCV genotype 1 infection was demonstrated in two randomized, double-blind, placebo-controlled, 2-arm, multicenter, Phase 3 trials (QUEST 1 and QUEST 2). The design of both trials was similar. All subjects received 12 weeks of once daily treatment with 150 mg OLYSIO or placebo, plus Peg-IFN-alfa-2a (QUEST 1 and QUEST 2) or Peg-IFN-alfa-2b (QUEST 2) and RBV, followed by 12 or 36 weeks of therapy with Peg-IFN-alfa and RBV in accordance with the on-treatment protocol-defined RGT criteria. Subjects in the control groups received 48 weeks of Peg-IFN-alfa-2a or -2b and RBV.
In the pooled analysis for QUEST 1 and QUEST 2, demographics and baseline characteristics were balanced between both trials and between the OLYSIO and placebo treatment groups. In the pooled analysis of trials (QUEST 1 and QUEST 2), the 785 enrolled subjects had a median age of 47 years (range: 18 to 73 years); 56% were male; 91% were White, 7% Black or African American, 1% Asian, and 17% Hispanic; 23% had a body mass index (BMI) greater than or equal to 30 kg/m2; 78% had HCV RNA levels greater than 800000 IU/mL; 74% had METAVIR fibrosis score F0, F1 or F2, 16% METAVIR fibrosis score F3, and 10% METAVIR fibrosis score F4 (cirrhosis); 48% had HCV genotype 1a, and 51% HCV genotype 1b; 29% had IL28B CC genotype, 56% IL28B CT genotype, and 15% IL28B TT genotype; 17% of the overall population and 34% of the subjects with genotype 1a virus had the NS3 Q80K polymorphism at baseline. In QUEST 1, all subjects received Peg-IFN-alfa-2a; in QUEST 2, 69% of the subjects received Peg-IFN-alfa-2a and 31% received Peg-IFN-alfa-2b.
Table 10 shows the response rates in treatment-naïve adult subjects with HCV genotype 1 infection. In the OLYSIO treatment group, SVR12 rates were lower in subjects with genotype 1a virus with the NS3 Q80K polymorphism at baseline compared to subjects infected with genotype 1a virus without the Q80K polymorphism.
| Treatment Outcome | OLYSIO + PR N=521 % (n/N) |
Placebo + PR N=264 % (n/N) |
|---|---|---|
| OLYSIO: 150 mg OLYSIO for 12 weeks with Peg-IFN-alfa-2a or -2b and RBV for 24 or 48 weeks; Placebo: placebo for 12 weeks with Peg-IFN-alfa-2a or -2b and RBV for 48 weeks. SVR12: sustained virologic response 12 weeks after planned EOT. | ||
| Overall SVR12 (genotype 1a and 1b) | 80 (419/521) | 50 (132/264) |
| Genotype 1a | 75 (191/254) | 47 (62/131) |
| Without Q80K | 84 (138/165) | 43 (36/83) |
| With Q80K | 58 (49/84) | 52 (23/44) |
| Genotype 1b | 85 (228/267) | 53 (70/133) |
| Outcome for all subjects without SVR12 | ||
| On-treatment failure |
8 (42/521) | 33 (87/264) |
| Viral relapse |
11 (51/470) | 23 (39/172) |
In the pooled analysis of QUEST 1 and QUEST 2, 88% (459/521) of OLYSIO-treated subjects were eligible for a total treatment duration of 24 weeks. In these subjects, the SVR12 rate was 88% (405/459).
Seventy-eight percent (78%; 404/521) of OLYSIO-treated subjects had undetectable HCV RNA at Week 4 (RVR); in these subjects the SVR12 rate was 90% (362/404), while 8% (32/392) with undetectable HCV RNA at end of treatment had viral relapse.
SVR12 rates were higher for the OLYSIO treatment group compared to the placebo treatment group by sex, age, race, BMI, HCV genotype/subtype, baseline HCV RNA load (less than or equal to 800000 IU/mL, greater than 800000 IU/mL), METAVIR fibrosis score, and IL28B genotype. Table 11 shows the SVR rates by METAVIR fibrosis score.
| Subgroup | OLYSIO + PR % (n/N) |
Placebo + PR % (n/N) |
|---|---|---|
| OLYSIO: 150 mg OLYSIO for 12 weeks with Peg-IFN-alfa-2a or -2b and RBV for 24 or 48 weeks; Placebo: placebo for 12 weeks with Peg-IFN-alfa-2a or -2b and RBV for 48 weeks. SVR12: sustained virologic response 12 weeks after planned EOT. | ||
| F0-2 | 84 (317/378) | 55 (106/192) |
| F3-4 | 68 (89/130) | 36 (26/72) |
SVR12 rates were higher for subjects receiving OLYSIO with Peg-IFN-alfa-2a or Peg-IFN-alfa-2b and RBV (88% and 78%, respectively) compared to subjects receiving placebo with Peg-IFN-alfa-2a or Peg-IFN-alfa-2b and RBV (62% and 42%, respectively) (QUEST 2).
14.2 Adult Subjects with HCV Genotype 1 Infection who Failed Prior Therapy
The PROMISE trial was a randomized, double-blind, placebo-controlled, 2-arm, multicenter, Phase 3 trial in subjects with HCV genotype 1 infection who relapsed after prior IFN-based therapy. All subjects received 12 weeks of once daily treatment with 150 mg OLYSIO or placebo, plus Peg-IFN-alfa-2a and RBV, followed by 12 or 36 weeks of therapy with Peg-IFN-alfa-2a and RBV in accordance with the protocol-defined RGT criteria. Subjects in the control group received 48 weeks of Peg-IFN-alfa-2a and RBV.
Demographics and baseline characteristics were balanced between the OLYSIO and placebo treatment groups. The 393 subjects enrolled in the PROMISE trial had a median age of 52 years (range: 20 to 71 years); 66% were male; 94% were White, 3% Black or African American, 2% Asian, and 7% Hispanic; 26% had a BMI greater than or equal to 30 kg/m2; 84% had HCV RNA levels greater than 800000 IU/mL; 69% had METAVIR fibrosis score F0, F1 or F2, 15% METAVIR fibrosis score F3, and 15% METAVIR fibrosis score F4 (cirrhosis); 42% had HCV genotype 1a, and 58% HCV genotype 1b; 24% had IL28B CC genotype, 64% IL28B CT genotype, and 12% IL28B TT genotype; 13% of the overall population and 31% of the subjects with genotype 1a virus had the NS3 Q80K polymorphism at baseline. The prior IFN-based HCV therapy was Peg-IFN-alfa-2a /RBV (68%) or Peg-IFN-alfa-2b/RBV (27%).
Table 12 shows the response rates for the OLYSIO and placebo treatment groups in adult subjects with HCV genotype 1 infection who relapsed after prior interferon-based therapy. In the OLYSIO treatment group, SVR12 rates were lower in subjects infected with genotype 1a virus with the NS3 Q80K polymorphism at baseline compared to subjects infected with genotype 1a virus without the Q80K polymorphism.
| Treatment Outcome | OLYSIO + PR N=260 % (n/N) |
Placebo + PR N=133 % (n/N) |
|---|---|---|
| OLYSIO: 150 mg OLYSIO for 12 weeks with Peg-IFN-alfa-2a and RBV for 24 or 48 weeks; Placebo: placebo for 12 weeks with Peg-IFN-alfa-2a and RBV for 48 weeks. SVR12: sustained virologic response 12 weeks after planned EOT. | ||
| Overall SVR12 (genotype 1a and 1b) | 79 (206/260) | 37 (49/133) |
| Genotype 1a | 70 (78/111) | 28 (15/54) |
| Without Q80K | 78 (62/79) | 26 (9/34) |
| With Q80K | 47 (14/30) | 30 (6/20) |
| Genotype 1b | 86 (128/149) | 43 (34/79) |
| Outcome for all subjects without SVR12 | ||
| On-treatment failure |
3 (8/260) | 27 (36/133) |
| Viral relapse |
18 (46/249) | 48 (45/93) |
In PROMISE, 93% (241/260) of OLYSIO-treated subjects were eligible for a total treatment duration of 24 weeks. In these subjects, the SVR12 rate was 83% (200/241).
Seventy-seven percent (77%; 200/260) of OLYSIO-treated subjects had undetectable HCV RNA at Week 4 (RVR); in these subjects the SVR12 rate was 87% (173/200), while 13% (25/196) with undetectable HCV RNA at end of treatment had viral relapse.
SVR12 rates were higher for the OLYSIO treatment group compared to the placebo treatment group by sex, age, race, BMI, HCV genotype/subtype, baseline HCV RNA load (less than or equal to 800000 IU/mL, greater than 800000 IU/mL), prior HCV therapy, METAVIR fibrosis score, and IL28B genotype. Table 13 shows the SVR rates by METAVIR fibrosis score.
| Subgroup | OLYSIO + PR % (n/N) |
Placebo + PR % (n/N) |
|---|---|---|
| OLYSIO: 150 mg OLYSIO for 12 weeks with Peg-IFN-alfa-2a and RBV for 24 or 48 weeks; Placebo: placebo for 12 weeks with Peg-IFN-alfa-2a and RBV for 48 weeks. SVR12: sustained virologic response 12 weeks after planned EOT. | ||
| F0-2 | 82 (137/167) | 41 (40/98) |
| F3-4 | 73 (61/83) | 24 (8/34) |
The ASPIRE trial was a randomized, double-blind, placebo-controlled, 7-arm, Phase 2b trial in subjects with HCV genotype 1 infection, who failed prior therapy with Peg-IFN-alfa and RBV (including prior relapsers, partial responders or null responders). Subjects received 12, 24 or 48 weeks of 100 mg or 150 mg OLYSIO in combination with 48 weeks of Peg-IFN-alfa-2a and RBV, or 48 weeks of placebo in combination with 48 weeks of Peg-IFN-alfa-2a and RBV.
Demographics and baseline characteristics were balanced between the OLYSIO and placebo treatment groups. The 462 subjects enrolled in the ASPIRE trial had a median age of 50 years (range: 20 to 69 years); 67% were male; 93% were White, 5% Black or African American, and 2% Asian; 25% had a BMI greater than or equal to 30 kg/m2; 86% had HCV RNA levels greater than 800000 IU/mL; 63% had METAVIR fibrosis score F0, F1, or F2, 19% METAVIR fibrosis score F3, and 18% METAVIR fibrosis score F4 (cirrhosis); 41% had HCV genotype 1a, and 58% HCV genotype 1b; 18% had IL28B CC genotype, 65% IL28B CT genotype, and 18% IL28B TT genotype (information available for 328 subjects); 12% of the overall population and 27% of the subjects with genotype 1a virus had the NS3 Q80K polymorphism at baseline. Forty percent (40%) of subjects were prior relapsers, 35% prior partial responders, and 25% prior null responders following prior therapy with Peg-INF-alfa and RBV. One hundred ninety-nine subjects received OLYSIO 150 mg once daily (pooled analysis) of which 66 subjects received OLYSIO for 12 weeks and 66 subjects received placebo in combination with Peg-IFN-alfa and RBV.
Table 14 shows the response rates for the OLYSIO and placebo treatment groups in prior relapsers, prior partial responders and prior null responders.
| Treatment Outcome | 150 mg OLYSIO 12 Weeks + PR N=66 % (n/N) |
Pooled 100 mg and 150 mg OLYSIO 12 Weeks + PR N=132 % (n/N) |
Placebo + PR N=66 % (n/N) |
|---|---|---|---|
| 150 mg OLYSIO: 150 mg OLYSIO for 12 weeks with Peg-IFN-alfa-2a and RBV for 48 weeks; Placebo: placebo with Peg-IFN-alfa-2a and RBV for 48 weeks. SVR24: sustained virologic response 24 weeks after planned EOT. | |||
| SVR24 | |||
| Prior relapser | 77 (20/26) | 83 (44/53) | 37 (10/27) |
| Prior partial responders | 65 (15/23) | 67 (31/46) | 9 (2/23) |
| Prior null responders | 53 (9/17) | 45 (15/33) | 19 (3/16) |
| Outcome for all subjects without SVR24 | |||
| On-treatment virologic failure |
|||
| Prior relapser | 8 (2/26) | 6 (3/53) | 22 (6/27) |
| Prior partial responders | 22 (5/23) | 20 (9/46) | 78 (18/23) |
| Prior null responders | 35 (6/17) | 36 (12/33) | 75 (12/16) |
| Viral Relapse |
|||
| Prior relapser | 13 (3/23) | 8 (4/49) | 47 (9/19) |
| Prior partial responders | 6 (1/17) | 8 (3/36) | 50 (2/4) |
| Prior null responders | 18 (2/11) | 20 (4/20) | 25 (1/4) |
In prior partial responders, SVR24 rates in subjects receiving OLYSIO with Peg-IFN-alfa and RBV were 47% and 77% in subjects with HCV genotype 1a and 1b, respectively, compared to 13% and 7%, respectively, in subjects receiving placebo with Peg-IFN-alfa and RBV. In prior null responders, SVR24 rates in subjects receiving OLYSIO with Peg-IFN-alfa and RBV were 41% and 47% in subjects with HCV genotype 1a and 1b, respectively, compared to 0% and 33%, respectively, in subjects receiving placebo with Peg-IFN-alfa and RBV.
SVR24 rates were higher in the OLYSIO-treated subjects compared to subjects receiving placebo in combination with Peg-IFN-alfa and RBV, regardless of HCV geno/subtype, METAVIR fibrosis score, and IL28B genotype.
16 HOW SUPPLIED/STORAGE AND HANDLING
OLYSIO (simeprevir) 150 mg capsules are white, marked with "TMC435 150" in black ink. The capsules are packaged into a bottle containing 28 capsules (NDC 59676-225-28) or a bottle of 7 capsules (emergency supply; NDC 59676-225-07).
Store OLYSIO capsules in the original bottle in order to protect from light. Store OLYSIO capsules at room temperature below 30°C (86°F).
17 PATIENT COUNSELING INFORMATION
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
OLYSIO should be used in combination with peginterferon alfa and ribavirin, and thus contraindications and warnings for peginterferon alfa and ribavirin also apply to OLYSIO combination treatment.
Pregnancy
Ribavirin must not be used by female patients who are pregnant or by men whose female partners are pregnant. Ribavirin therapy should not be initiated until a report of a negative pregnancy test has been obtained immediately before starting therapy. OLYSIO in combination treatment with peginterferon alfa and ribavirin is contraindicated in women who are pregnant and in men whose female partners are pregnant (see also the prescribing information for ribavirin).
Female patients of childbearing potential and male patients with female partners of childbearing potential must be advised of the teratogenic/embryocidal risks of ribavirin and should be advised that extreme care must be taken to avoid pregnancy in female patients and in female partners of male patients - both during treatment and for 6 months after the completion of all treatment. Women of childbearing potential and men must use at least two forms of effective contraception during treatment and for 6 months post-treatment. Women of childbearing potential and men must be counseled about use of effective contraception (two methods) prior to initiating treatment.
Patients (both male and female) should be advised to notify their healthcare provider immediately in the event of a pregnancy [see Contraindications (4), Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
Photosensitivity
Patients should be advised of the risk of photosensitivity reactions related to the use of OLYSIO in combination with peginterferon and ribavirin and that these reactions may be severe. Patients should be advised to contact their healthcare provider immediately if they develop a photosensitivity reaction. Patients should not stop OLYSIO due to photosensitivity reactions unless instructed by their healthcare provider [see Warning and Precautions (5.2)].
Patients should be advised to use sun protection measures (such as a hat, sunglasses, protective clothing, sunscreen) during treatment with OLYSIO. Patients should limit exposure to natural sunlight and avoid artificial sunlight (tanning beds or phototherapy) during treatment with OLYSIO.
Rash
Patients should be advised of the risk of rash related to the use of OLYSIO in combination with peginterferon and ribavirin and that rash may become severe. Patients should be advised to contact their healthcare provider immediately if they develop a rash. Patients should not stop OLYSIO due to rash unless instructed by their healthcare provider [see Warning and Precautions (5.3)].
Administration
Patients should be advised that OLYSIO should be administered in combination with both peginterferon alfa and ribavirin. If peginterferon alfa and/or ribavirin is discontinued for any reason, OLYSIO must also be discontinued.
Patients should be advised that the dose of OLYSIO must not be reduced or interrupted, as it may increase the possibility of treatment failure.
If the patient misses a dose of OLYSIO and remembers within 12 hours of the usual dosing time, the patient should take the missed dose of OLYSIO with food as soon as possible and then take the next dose of OLYSIO at the regularly scheduled time. If a patient misses a dose of OLYSIO by more than 12 hours after the usual dosing time, the patient should not take the missed dose of OLYSIO, but resume the usual dosing of OLYSIO with food at the regularly scheduled time. Inform the patient that he or she should not take more or less than the prescribed dose of OLYSIO at any one time.
Hepatitis C Virus Transmission
Patients should be informed that the effect of treatment of hepatitis C infection on transmission is not known, and that appropriate precautions to prevent transmission of the hepatitis C virus should be taken.
Product of Belgium
Manufactured by:
Janssen-Cilag SpA, Latina, Italy
Manufactured for:
Janssen Therapeutics, Division of Janssen Products, LP
Titusville NJ 08560
Licensed from Medivir AB
OLYSIO™ is a trademark of Johnson & Johnson
© Janssen Products, LP 2013
PATIENT INFORMATIONOLYSIO™ (oh li' see oh)
(simeprevir)
Capsules
Read this Patient Information before you start taking OLYSIO and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
OLYSIO is used in combination with other antiviral medicines. When taking OLYSIO in combination with peginterferon alfa and ribavirin you should also read those Medication Guides.
The information in this Patient Information leaflet talks about OLYSIO when it is used in combination with peginterferon alfa and ribavirin.
What is the most important information I should know about OLYSIO?
OLYSIO, in combination with peginterferon alfa and ribavarin may cause birth defects or death of your unborn baby. If you are pregnant or your sexual partner is pregnant, or plans to become pregnant, do not take these medicines. You or your sexual partner should not become pregnant while taking OLYSIO with peginterferon alfa and ribavirin and for 6 months after treatment is over.
- Females and males must use two effective forms of birth control during treatment and for 6 months after treatment with OLYSIO, peginterferon alfa, and ribavirin combination therapy. Talk to your healthcare provider about forms of birth control that may be used during this time.
- Females must have a pregnancy test before starting treatment with OLYSIO, peginterferon alfa, and ribavarin combination therapy, every month while being treated, and every month for 6 months after your treatment with OLYSIO, peginterferon alfa, and ribavirin combination therapy is over.
- If you or your female sexual partner becomes pregnant while taking OLYSIO, peginterferon alfa, and ribavirin combination therapy or within 6 months after you stop taking these medicines, tell your healthcare provider right away. You or your healthcare provider should contact the Ribavirin Pregnancy Registry by calling 1-800-593-2214. The Ribavirin Pregnancy Registry collects information about what happens to mothers and their babies if the mother takes ribavirin while she is pregnant.
OLYSIO in combination with peginterferon alfa and ribavirin may cause rashes and skin reactions to sunlight. These rashes and skin reactions to sunlight can be severe and you may need to be treated in a hospital. Rashes and skin reactions to sunlight are most common during the first 4 weeks of treatment, but can happen at any time during treatment with OLYSIO, peginterferon alfa, and ribavirin combination therapy.
- Use sunscreen, and wear a hat, sunglasses, and protective clothing when you will be exposed to sunlight during treatment with OLYSIO.
- Limit sunlight exposure during treatment with OLYSIO.
- Avoid use of tanning beds, sunlamps, or other types of light therapy during treatment with OLYSIO.
- Call your healthcare provider right away if you get any of the following symptoms:
- burning, redness, swelling or blisters on your skin
- mouth sores or ulcers
- red or inflamed eyes, like "pink eye" (conjunctivitis)
Do not take OLYSIO alone. OLYSIO should be used together with peginterferon alfa and ribavirin to treat chronic hepatitis C infection.
What is OLYSIO?
- OLYSIO is a prescription medicine used with other antiviral medicines to treat chronic (lasting a long time) hepatitis C in adults.
- OLYSIO must not be taken alone.
It is not known if OLYSIO is safe and effective in children under 18 years of age.
Who should not take OLYSIO?
See "What is the most important information I should know about OLYSIO?"
What should I tell my healthcare provider before taking OLYSIO?
Before taking OLYSIO, tell your healthcare provider if you:
- have liver problems other than hepatitis C virus infection
- have taken the medicines telaprevir (Incivek®) or boceprevir (Victrelis®)
- had a liver transplant
- are receiving phototherapy
- have any other medical condition
- are of East Asian descent
- are breastfeeding. It is not known if OLYSIO passes into your breast milk. You and your healthcare provider should decide if you will take OLYSIO or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
OLYSIO and other medicines may affect each other. This can cause you to have too much or not enough OLYSIO or other medicines in your body, which may affect the way OLYSIO or your other medicines work, or may cause side effects. Do not start taking a new medicine without telling your healthcare provider or pharmacist.
Especially tell your healthcare provider if you take any of the following medicines:
- amiodarone (Cordarone®, Pacerone®)
- amlodipine (Norvasc®)
- atazanavir (Reyataz®)
- atorvastatin (Lipitor®, Caduet®)
- carbamazepine (Carbatrol®, Epitol®, Equetro®, Tegretol®)
- cisapride (Propulsid®, Propulsid Quicksolv®)
- clarithromycin (Biaxin®, Prevpac®)
- cobicistat-containing medicine (Stribild®)
- cyclosporine (Gengraf®, Neoral®, Sandimmune®)
- darunavir (Prezista®)
- delavirdine mesylate (Rescriptor®)
- dexamethasone (when administered by injection or when taken by mouth)
- digoxin (Lanoxin®)
- diltiazem (Cardizem®, Dilacor XR®, Tiazac®)
- disopyramide (Norpace®)
- efavirenz (Sustiva®, Atripla®)
- erythromycin (E.E.S.®, Eryc®, Ery-Tab®, Erythrocin®, Erythrocin Stearate®)
- etravirine (Intelence®)
- felodipine (Plendil®)
- flecainide (Tambocor®)
- fluconazole (when taken by mouth or when administered by injection) (Diflucan®)
- fosamprenavir (Lexiva®)
- indinavir (Crixivan®)
- itraconazole (when taken by mouth) (Sporanox®, Onmel®)
- ketoconazole (when taken by mouth) (Nizoral®)
- lopinavir (Kaletra®)
- lovastatin (Advicor®, Altoprev®, Mevacor®)
- mexiletine (Mexitil®)
- midazolam (when taken by mouth)
- milk thistle (Silybum marianum) or products containing milk thistle
- nelfinavir (Viracept®)
- nevirapine (Viramune®, Viramune XR®)
- nicardipine (Cardene®)
- nifedipine (Adalat CC®, Afeditab CR®, Procardia®)
- nisoldipine (Sular®)
- oxcarbazepine (Trileptal®)
- phenobarbital (Luminal®)
- phenytoin (Dilantin®, Phenytek®)
- pitavastatin (Livalo®)
- posaconazole (when taken by mouth) (Noxafil®)
- pravastatin (Pravachol®)
- propafenone (Rythmol SR®)
- quinidine (Nuedexta®, Duraquin®, Quinaglute®)
- rifabutin (Mycobutin®)
- rifampin (Rifadin®, Rifamate®, Rifater®)
- rifapentine (Priftin®)
- ritonavir (Norvir®)
- rosuvastatin (Crestor®)
- saquinavir mesylate (Invirase®)
- sildenafil (Revatio®, Viagra®)
- simvastatin (Zocor®, Vytorin®, Simcor®)
- sirolimus (Rapamune®)
- St. John's wort (Hypericum perforatum) or products containing St. John's wort
- tacrolimus (Prograf®)
- tadalafil (Adcirca®, Cialis®)
- telithromycin (Ketek®)
- tipranavir (Aptivus®)
- triazolam (when taken by mouth) (Halcion®)
- verapamil (Calan®, Covera-HS®, Isoptin®, Tarka®)
- voriconazole (when taken by mouth or when administered by injection) (Vfend®)
- warfarin (Coumadin®)
This is not a complete list of medicines that could interact with OLYSIO. Ask your healthcare provider or pharmacist if you are not sure if your medicine is one that is listed above.
Know the medicines you take. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take OLYSIO?
- Take OLYSIO exactly as your healthcare provider tells you to take it. Do not change your dose unless your healthcare provider tells you to.
- Do not stop taking OLYSIO unless your healthcare provider tells you to. If you think there is a reason to stop taking OLYSIO, talk to your healthcare provider before doing so.
- Take one OLYSIO capsule each day with food.
- Swallow OLYSIO capsules whole.
- If you miss a dose of OLYSIO and it is more than 12 hours until your next dose, take the missed dose as soon as possible with food. Take the next dose of OLYSIO at your regular time.
- If you miss a dose of OLYSIO and it is less than 12 hours until your next dose, skip the missed dose. Take the next dose of OLYSIO at your regular time.
- Do not take two doses of OLYSIO at the same time to make up for a missed dose.
- If you take too much OLYSIO, call your healthcare provider right away or go to the nearest hospital emergency room.
What are the possible side effects of OLYSIO?
The most common side effects of OLYSIO when used in combination with peginterferon alfa and ribavirin include:
- skin rash. See "What is the most important information I should know about OLYSIO?" section of this leaflet.
- itching
- nausea
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of OLYSIO. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store OLYSIO?
- Store OLYSIO at room temperature below 86°F (30°C).
- Store OLYSIO in the original bottle to protect it from light.
Keep OLYSIO and all medicines out of the reach of children.
General Information about the safe and effective use of OLYSIO
It is not known if treatment with OLYSIO will prevent you from infecting another person with the hepatitis C virus during your treatment. Talk with your healthcare provider about ways to prevent spreading the hepatitis C virus.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use OLYSIO for a condition for which it was not prescribed. Do not give your OLYSIO to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about OLYSIO, talk with your pharmacist or healthcare provider. You can ask your pharmacist or healthcare provider for information about OLYSIO that is written for health professionals.
For more information about OLYSIO, go to www.OLYSIO.com or call 1-800-526-7736.
What are the ingredients in OLYSIO?
Active ingredient: simeprevir
Inactive ingredients: colloidal anhydrous silica, croscarmellose sodium, lactose monohydrate, magnesium stearate, sodium lauryl sulphate. The white capsule contains gelatin and titanium dioxide (E171) and is printed with ink containing iron oxide black (E172) and shellac (E904).
This Patient Information has been approved by the U.S. Food and Drug Administration.
Product of Belgium
Manufactured by:
Janssen-Cilag SpA, Latina, Italy
Manufactured for:
Janssen Therapeutics, Division of Janssen Products, LP, Titusville NJ 08560
Licensed from Medivir AB
Issued: November 2013
OLYSIO™ is a trademark of Johnson & Johnson
© Janssen Products, LP 2013
PRINCIPAL DISPLAY PANEL - 150 mg Capsule Bottle Label
NDC 59676-225-28
28 Capsules
Olysio™
(simeprevir) Capsules
150 mg
Each capsule contains simeprevir sodium
equivalent to 150 mg simeprevir
Rx only
janssen

OLYSIOsimeprevir CAPSULE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||