Omeprazole
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use omeprazole delayed-release capsules safely and effectively. See full prescribing information for omeprazole delayed-release capsules. Omeprazole Delayed-Release Capsules, USPInitial U.S. Approval: 1989INDICATIONS AND USAGEOmeprazole is a proton pump inhibitor indicated for: Treatment in adults of duodenal ulcer (1.1) and gastric ulcer (1.2) Treatment in adults and children of gastroesophageal reflux disease (GERD) (1.3) and maintenance of healing of erosive esophagitis (1.4) The safety and effectiveness of omeprazole in pediatric patients < 1 year of age have not been established. (8.4)DOSAGE AND ADMINISTRATION Indication Omeprazole Dose Frequency Treatment of Active Duodenal Ulcer (2.1) 20 mg Once daily for 4 weeks. Some patients may require an additional 4 weeks H. pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence (2.2) Triple Therapy: Omeprazole 20 mg Each drug twice Amoxicillin 1000 mg daily for 10 days Clarithromycin 500 mg Dual Therapy: Omeprazole 40 mg Once daily for 14 days Clarithromycin 500 mg Three times daily for 14 days Gastric Ulcer (2.3) 40 mg Once daily for 4 to 8 weeks GERD (2.4) 20 mg Once daily for 4 to 8 weeks Maintenance of Healing of Erosive Esophagitis (2.5) 20 mg Once daily Pathological Hypersecretory Conditions (2.6) 60 mg (varies with individual patient) Once daily Pediatric Patients (2 to 16 years of age) (2.7) GERD And Maintenance of Healing of Erosive Esophagitis Weight 10 < 20 kg≥ 20 kg Dose 10 mg20 mg Once daily DOSAGE FORMS AND STRENGTHS Omeprazole Delayed-Release Capsules, 10 mg, 20 mg and 40 mg (3) CONTRAINDICATIONSKnown hypersensitivity to any component of the formulation or substituted benzimidazoles (angioedema and anaphylaxis have occurred) (4)WARNINGS AND PRECAUTIONS Symptomatic response does not preclude the presence of gastric malignancy (5.1) Atrophic Gastritis: Has been noted with long-term therapy (5.2) Triple therapy for H. pylori - there are risks due to antibiotics, see separate prescribing information for individual antibiotics (5.3, 5.4) Side EffectsAdults: Most common adverse reactions in adults (incidence ≥ 2%) are: Headache, abdominal pain, nausea, diarrhea, vomiting and flatulence (6) Pediatric patients (2 to 16 years of age): Safety profile similar to that in adults, except that respiratory system events and fever were the most frequently reported reactions in pediatric studies (8.4) To report SUSPECTED ADVERSE REACTIONS, contact Mylan Pharmaceuticals Inc. toll free at 1-877-446-3679 (1-877-4-INFO-RX) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONS May interfere with drugs for which gastric pH affects bioavailability (e.g., ketoconazole, iron salts, ampicillin esters, and digoxin) (7.2) Atazanavir and nelfinavir: Omeprazole reduces plasma levels of atazanavir and nelfinavir. Concomitant use is not recommended (7.1) Saquinavir: Omeprazole increases plasma levels of saquinavir. Monitor for toxicity and consider dose reduction of saquinavir (7.1) Cilostazol: Omeprazole increases systemic exposure of cilostazol and one of its active metabolites. Consider dose reduction of cilostazol (7.3) Drugs metabolized by cytochrome P450 (e.g., diazepam, warfarin, phenytoin, cyclosporine, disulfiram, benzodiazepines): Omeprazole can prolong their elimination. Monitor and determine need for dose adjustments (7.3) Patients treated with proton pump inhibitors and warfarin may need to be monitored for increases in INR and prothrombin time (7.3) Tacrolimus: Omeprazole may increase serum levels of tacrolimus (7.4) Combined inhibitor of CYP 2C19 and 3A4 (e.g., voriconazole) may raise omeprazole levels (7.3) USE IN SPECIFIC POPULATIONSPatients with hepatic impairment: Consider dose reduction, particularly for maintenance of healing of erosive esophagitis (12.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 OMEPRAZOLE INDICATIONS AND USAGE
- 2 OMEPRAZOLE DOSAGE AND ADMINISTRATION
- 2.1 Short-Term Treatment of Active Duodenal Ulcer
- 2.2 Eradication for the Reduction of the Risk of Duodenal Ulcer Recurrence
- 2.3 Gastric Ulcer
- 2.4 Gastroesophageal Reflux Disease (GERD)
- 2.5 Maintenance of Healing of Erosive Esophagitis
- 2.6 Pathological Hypersecretory Conditions
- 2.7 Pediatric Patients
- 2.8 Alternative Administration Options
- 3 DOSAGE FORMS AND STRENGTHS
- 4 OMEPRAZOLE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 OMEPRAZOLE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 OMEPRAZOLE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- Principal Display panel
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Duodenal Ulcer (adults)
Omeprazole delayed-release capsules are indicated for short-term treatment of active duodenal ulcer in adults. Most patients heal within 4 weeks. Some patients may require an additional 4 weeks of therapy.
Omeprazole delayed-release capsules, in combination with clarithromycin and amoxicillin, are indicated for treatment of patients with H. pylori infection and duodenal ulcer disease (active or up to one year history) to eradicate H. pylori in adults.
Omeprazole delayed-release capsules, in combination with clarithromycin are indicated for treatment of patients with H. pylori infection and duodenal ulcer disease to eradicate H. pylori in adults.
Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence [see Clinical Studies (14.1) and Dosage and Administration (2)].
Among patients who fail therapy, omeprazole delayed-release capsules with clarithromycin are more likely to be associated with the development of clarithromycin resistance as compared with triple therapy. In patients who fail therapy, susceptibility testing should be done. If resistance to clarithromycin is demonstrated or susceptibility testing is not possible, alternative antimicrobial therapy should be instituted [see Microbiology section (12.4) and the clarithromycin package insert, Microbiology section].
1.2 Gastric Ulcer (adults)
Omeprazole delayed-release capsules are indicated for short-term treatment (4 to 8 weeks) of active benign gastric ulcer in adults [see Clinical Studies (14.2)].
1.3 Treatment of Gastroesophageal Reflux Disease (GERD) (adults and pediatric patients)
Symptomatic GERD
Omeprazole delayed-release capsules are indicated for the treatment of heartburn and other symptoms associated with GERD in pediatric patients and adults.
Erosive Esophagitis
Omeprazole delayed-release capsules are indicated for the short-term treatment (4 to 8 weeks) of erosive esophagitis that has been diagnosed by endoscopy in pediatric patients and adults [see Clinical Studies (14.4)].
The efficacy of omeprazole delayed-release capsules used for longer than 8 weeks in these patients has not been established. If a patient does not respond to 8 weeks of treatment, an additional 4 weeks of treatment may be given. If there is recurrence of erosive esophagitis or GERD symptoms (e.g., heartburn), additional 4 to 8 week courses of omeprazole may be considered.
1.4 Maintenance of Healing of Erosive Esophagitis (adults and pediatric patients)
Omeprazole delayed-release capsules are indicated to maintain healing of erosive esophagitis in pediatric patients and adults.
Controlled studies do not extend beyond 12 months [see Clinical Studies (14.4)].
1.5 Pathological Hypersecretory Conditions (adults)
Omeprazole delayed-release capsules are indicated for the long-term treatment of pathological hypersecretory conditions (e.g., Zollinger-Ellison syndrome, multiple endocrine adenomas and systemic mastocytosis) in adults.
2 DOSAGE AND ADMINISTRATION
Omeprazole delayed-release capsules should be taken before eating. In the clinical trials, antacids were used concomitantly with omeprazole delayed-release capsules.
Patients should be informed that the omeprazole delayed-release capsules should be swallowed whole.
For patients unable to swallow an intact capsule, alternative administration options are available [see Dosage and Administration (2.8)].
2.1 Short-Term Treatment of Active Duodenal Ulcer
The recommended adult oral dose of omeprazole delayed-release capsules is 20 mg once daily. Most patients heal within 4 weeks. Some patients may require an additional 4 weeks of therapy.
2.2 Eradication for the Reduction of the Risk of Duodenal Ulcer Recurrence
Triple Therapy (omeprazole/clarithromycin/amoxicillin) -
The recommended adult oral regimen is omeprazole delayed-release capsules 20 mg plus clarithromycin 500 mg plus amoxicillin 1000 mg each given twice daily for 10 days. In patients with an ulcer present at the time of initiation of therapy, an additional 18 days of omeprazole delayed-release capsules 20 mg once daily is recommended for ulcer healing and symptom relief.
Dual Therapy (omeprazole/clarithromycin) -
The recommended adult oral regimen is omeprazole delayed-release capsules 40 mg once daily plus clarithromycin 500 mg 3 times daily for 14 days. In patients with an ulcer present at the time of initiation of therapy, an additional 14 days of omeprazole delayed-release capsules 20 mg once daily is recommended for ulcer healing and symptom relief.
2.3 Gastric Ulcer
The recommended adult oral dose is 40 mg once daily for 4 to 8 weeks.
2.4 Gastroesophageal Reflux Disease (GERD)
The recommended adult oral dose for the treatment of patients with symptomatic GERD and no esophageal lesions is 20 mg daily for up to 4 weeks. The recommended adult oral dose for the treatment of patients with erosive esophagitis and accompanying symptoms due to GERD is 20 mg daily for 4 to 8 weeks.
2.5 Maintenance of Healing of Erosive Esophagitis
The recommended adult oral dose is 20 mg daily [see Clinical Studies (14.4)].
2.6 Pathological Hypersecretory Conditions
The dosage of omeprazole delayed-release capsules in patients with pathological hypersecretory conditions varies with the individual patient. The recommended adult oral starting dose is 60 mg once daily. Doses should be adjusted to individual patient needs and should continue for as long as clinically indicated. Doses up to 120 mg three times daily have been administered. Daily dosages of greater than 80 mg should be administered in divided doses. Some patients with Zollinger-Ellison syndrome have been treated continuously with omeprazole delayed-release capsules for more than 5 years.
2.7 Pediatric Patients
For the treatment of GERD and maintenance of healing of erosive esophagitis, the recommended daily dose for pediatric patients 2 to 16 years of age is as follows:
| Patient Weight | Omeprazole Daily Dose |
| 10 < 20 kg | 10 mg |
| ≥ 20 kg | 20 mg |
On a per kg basis, the doses of omeprazole delayed-release capsules required to heal erosive esophagitis in pediatric patients are greater than those for adults.
Alternative administrative options can be used for pediatric patients unable to swallow an intact capsule [see Dosage and Administration (2.8)].
2.8 Alternative Administration Options
Omeprazole is available as a delayed-release capsule.
For patients who have difficulty swallowing capsules, the contents of an omeprazole delayed-release capsule can be added to applesauce. One tablespoon of applesauce should be added to an empty bowl and the capsule should be opened. All of the pellets inside the capsule should be carefully emptied on the applesauce. The pellets should be mixed with the applesauce and then swallowed immediately with a glass of cool water to ensure complete swallowing of the pellets. The applesauce used should not be hot and should be soft enough to be swallowed without chewing. The pellets should not be chewed or crushed. The pellets/applesauce mixture should not be stored for future use.
3 DOSAGE FORMS AND STRENGTHS
Omeprazole delayed-release capsules USP, 10 mg, are hard-shell gelatin capsules with a dark green opaque cap and a dark green opaque body axially printed with MYLAN over 5211 in white ink both on the cap and the body. The capsule is filled with white to off-white beads.
Omeprazole delayed-release capsules USP, 20 mg, are hard-shell gelatin capsules with a dark green opaque cap and a blue-green opaque body axially printed with MYLAN over 6150 in white ink both on the cap and the body. The capsule is filled with white to off-white beads.
Omeprazole delayed-release capsules USP, 40 mg, are hard-shell gelatin capsules with a dark green opaque cap and a light-blue opaque body axially printed with MYLAN over 5222 in white ink both on the cap and the body. The capsule is filled with white to off-white beads.
4 CONTRAINDICATIONS
Omeprazole delayed-release capsules are contraindicated in patients with known hypersensitivity to substituted benzimidazoles or to any component of the formulation. Hypersensitivity reactions may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, interstitial nephritis and urticaria [see Adverse Reactions (6)].
5 WARNINGS AND PRECAUTIONS
5.1 Concomitant Gastric Malignancy
Symptomatic response to therapy with omeprazole does not preclude the presence of gastric malignancy.
5.2 Atrophic Gastritis
Atrophic gastritis has been noted occasionally in gastric corpus biopsies from patients treated long-term with omeprazole.
5.3 Combination Use of Omeprazole with Amoxicillin
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients on penicillin therapy. These reactions are more likely to occur in individuals with a history of penicillin hypersensitivity and/or a history of sensitivity to multiple allergens. Before initiating therapy with amoxicillin, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins or other allergens. If an allergic reaction occurs, amoxicillin should be discontinued and appropriate therapy instituted. Serious anaphylactic reactions require immediate emergency treatment with epinephrine. Oxygen, intravenous steroids and airway management, including intubation, should also be administered as indicated.
Pseudomembranous colitis has been reported with nearly all antibacterial agents and may range in severity from mild to life threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents.
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of “antibiotic-associated colitis.”
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of the drug alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation and treatment with an antibacterial drug clinically effective against Clostridium difficile colitis.
5.4 Combination Use of Omeprazole with Clarithromycin
Clarithromycin should not be used in pregnant women except in clinical circumstances where no alternative therapy is appropriate. If pregnancy occurs while taking clarithromycin, the patient should be apprised of the potential hazard to the fetus. (See Warnings in prescribing information for clarithromycin.)
Coadministration of omeprazole and clarithromycin has resulted in increases in plasma levels of omeprazole, clarithromycin and 14-hydroxy-clarithromycin [see Clinical Pharmacology (12)].
Concomitant administration of clarithromycin with cisapride or pimozide, is contraindicated.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience with Omeprazole Monotherapy
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data described below reflects exposure to omeprazole delayed-release capsules in 3,096 patients from worldwide clinical trials (465 patients from U.S. studies and 2,631 patients from international studies). Indications clinically studied in U.S. trials included duodenal ulcer, resistant ulcer and Zollinger-Ellison syndrome. The international clinical trials were double-blind and open-label in design. The most common adverse reactions reported (i.e., with an incidence rate ≥ 2%) from omeprazole-treated patients enrolled in these studies included headache (6.9%), abdominal pain (5.2%), nausea (4%), diarrhea (3.7%), vomiting (3.2%) and flatulence (2.7%).
Additional adverse reactions that were reported with an incidence ≥ 1% included acid regurgitation (1.9%), upper respiratory infection (1.9%), constipation (1.5%), dizziness (1.5%), rash (1.5%), asthenia (1.3%), back pain (1.1%) and cough (1.1%).
The clinical trial safety profile in patients greater than 65 years of age was similar to that in patients 65 years of age or less.
The clinical trial safety profile in pediatric patients who received omeprazole delayed-release capsules was similar to that in adult patients. Unique to the pediatric population, however, adverse reactions of the respiratory system were most frequently reported in the 2 to 16 year age group (18.5%). Similarly, accidental injuries were reported frequently in the 2 to 16 year age group (3.8%) [see Use in Specific Populations (8.4)].
6.2 Clinical Trials Experience with Omeprazole in Combination Therapy for Eradication
In clinical trials using either dual therapy with omeprazole and clarithromycin, or triple therapy with omeprazole, clarithromycin and amoxicillin, no adverse reactions unique to these drug combinations were observed. Adverse reactions observed were limited to those previously reported with omeprazole, clarithromycin or amoxicillin alone.
Dual Therapy (omeprazole/clarithromycin)
Adverse reactions observed in controlled clinical trials using combination therapy with omeprazole and clarithromycin (n = 346) that differed from those previously described for omeprazole alone were taste perversion (15%), tongue discoloration (2%), rhinitis (2%), pharyngitis (1%) and flu-syndrome (1%). (For more information on clarithromycin, refer to the clarithromycin prescribing information, Adverse Reactions section.)
Triple Therapy (omeprazole/clarithromycin/amoxicillin)
The most frequent adverse reactions observed in clinical trials using combination therapy with omeprazole, clarithromycin and amoxicillin (n = 274) were diarrhea (14%), taste perversion (10%) and headache (7%). None of these occurred at a higher frequency than that reported by patients taking antimicrobial agents alone. (For more information on clarithromycin or amoxicillin, refer to the respective prescribing information, Adverse Reactions sections.)
6.3 Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of omeprazole delayed-release capsules. Because these reactions are voluntarily reported from a population of uncertain size, it is not always possible to reliably estimate their actual frequency or establish a causal relationship to drug exposure.
Body as a Whole: Hypersensitivity reactions including anaphylaxis, anaphylactic shock, angioedema, bronchospasm, interstitial nephritis, urticaria, (see also Skin below); fever; pain; fatigue; malaise
Cardiovascular: Chest pain or angina, tachycardia, bradycardia, palpitations, elevated blood pressure, peripheral edema
Endocrine: Gynecomastia
Gastrointestinal: Pancreatitis (some fatal), anorexia, irritable colon, fecal discoloration, esophageal candidiasis, mucosal atrophy of the tongue, stomatitis, abdominal swelling, dry mouth. During treatment with omeprazole, gastric fundic gland polyps have been noted rarely. These polyps are benign and appear to be reversible when treatment is discontinued. Gastroduodenal carcinoids have been reported in patients with ZE syndrome on long-term treatment with omeprazole. This finding is believed to be a manifestation of the underlying condition, which is known to be associated with such tumors.
Hepatic: Liver disease including hepatic failure (some fatal), liver necrosis (some fatal), hepatic encephalopathy hepatocellular disease, cholestatic disease, mixed hepatitis, jaundice and elevations of liver function tests [ALT, AST, GGT, alkaline phosphatase and bilirubin]
Metabolic/Nutritional: Hypoglycemia, hyponatremia, weight gain
Musculoskeletal: Muscle weakness, myalgia, muscle cramps, joint pain, leg pain
Nervous System/Psychiatric: Psychiatric and sleep disturbances including depression, agitation, aggression, hallucinations, confusion, insomnia, nervousness, apathy, somnolence, anxiety and dream abnormalities; tremors, paresthesia; vertigo
Respiratory: Epistaxis, pharyngeal pain
Skin: Severe generalized skin reactions including toxic epidermal necrolysis (some fatal), Stevens-Johnson Syndrome and erythema multiforme; photosensitivity; urticaria; rash; skin inflammation; pruritus; petechiae; purpura; alopecia; dry skin; hyperhidrosis
Special Senses: Tinnitus, taste perversion
Ocular: Optic atrophy, anterior ischemic optic neuropathy, optic neuritis, dry eye syndrome, ocular irritation, blurred vision, double vision
Urogenital: Interstitial nephritis, hematuria, proteinuria, elevated serum creatinine, microscopic pyuria, urinary tract infection, glycosuria, urinary frequency, testicular pain
Hematologic: Agranulocytosis (some fatal), hemolytic anemia, pancytopenia, neutropenia, anemia, thrombocytopenia, leukopenia, leucocytosis
7 DRUG INTERACTIONS
7.1 Interference with Antiretroviral Therapy
Concomitant use of atazanavir and nelfinavir with proton pump inhibitors is not recommended. Coadministration of atazanavir with proton pump inhibitors is expected to substantially decrease atazanavir plasma concentrations and may result in a loss of therapeutic effect and the development of drug resistance. Coadministration of saquinavir with proton pump inhibitors is expected to increase saquinavir concentrations, which may increase toxicity and require dose reduction.
Omeprazole has been reported to interact with some antiretroviral drugs. The clinical importance and the mechanisms behind these interactions are not always known. Increased gastric pH during omeprazole treatment may change the absorption of the antiretroviral drug. Other possible interaction mechanisms are via CYP 2C19.
Reduced concentrations of atazanavir and nelfinavir
For some antiretroviral drugs, such as atazanavir and nelfinavir, decreased serum levels have been reported when given together with omeprazole. Following multiple doses of nelfinavir (1250 mg, twice daily) and omeprazole (40 mg daily), AUC was decreased by 36% and 92%, Cmax by 37% and 89% and Cmin by 39% and 75% respectively for nelfinavir and M8. Following multiple doses of atazanavir (400 mg, daily) and omeprazole (40 mg, daily, 2 hours before atazanavir), AUC was decreased by 94%, Cmax by 96%, and Cmin by 95%. Concomitant administration with omeprazole and drugs such as atazanavir and nelfinavir is therefore not recommended.
Increased concentrations of saquinavir
For other antiretroviral drugs, such as saquinavir, elevated serum levels have been reported, with an increase in AUC by 82%, in Cmax by 75%, and in Cmin by 106%, following multiple dosing of saquinavir/ritonavir (1000 mg/100 mg) twice daily for 15 days with omeprazole 40 mg daily coadministered days 11 to 15. Therefore, clinical and laboratory monitoring for saquinavir toxicity is recommended during concurrent use with omeprazole. Dose reduction of saquinavir should be considered from the safety perspective for individual patients.
There are also some antiretroviral drugs of which unchanged serum levels have been reported when given with omeprazole.
7.2 Drugs for which Gastric pH can Affect Bioavailability
Because of its profound and long lasting inhibition of gastric acid secretion, it is theoretically possible that omeprazole may interfere with absorption of drugs where gastric pH is an important determinant of their bioavailability (e.g., ketoconazole, ampicillin esters, and iron salts). In the clinical trials, antacids were used concomitantly with the administration of omeprazole.
7.3 Effects on Hepatic Metabolism/Cytochrome P450 Pathways
Omeprazole can prolong the elimination of diazepam, warfarin and phenytoin, drugs that are metabolized by oxidation in the liver. There have been reports of increased INR and prothrombin time in patients receiving proton pump inhibitors, including omeprazole, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin may need to be monitored for increases in INR and prothrombin time.
Although in normal subjects no interaction with theophylline or propranolol was found, there have been clinical reports of interaction with other drugs metabolized via the cytochrome P450 system (e.g., cyclosporine, disulfiram, benzodiazepines). Patients should be monitored to determine if it is necessary to adjust the dosage of these drugs when taken concomitantly with omeprazole.
Concomitant administration of omeprazole and voriconazole (a combined inhibitor of CYP2C19 and CYP3A4) resulted in more than doubling of the omeprazole exposure. Dose adjustment of omeprazole is not normally required. However, in patients with Zollinger-Ellison syndrome, who may require higher doses up to 240 mg/day, dose adjustment may be considered. When voriconazole (400 mg Q12h x 1 day, then 200 mg x 6 days) was given with omeprazole (40 mg once daily x 7 days) to healthy subjects, it significantly increased the steady-state Cmax and AUC0 to 24 of omeprazole, an average of 2 times (90% CI: 1.8, 2.6) and 4 times (90% CI: 3.3, 4.4) respectively as compared to when omeprazole was given without voriconazole.
Omeprazole acts as an inhibitor of CYP 2C19. Omeprazole, given in doses of 40 mg daily for one week to 20 healthy subjects in crossover study, increased Cmax and AUC of cilostazol by 18% and 26% respectively. Cmax and AUC of one of its active metabolites, 3,4dihydro-cilostazol, which has 4 to 7 times the activity of cilostazol, were increased by 29% and 69% respectively. Coadministration of cilostazol with omeprazole is expected to increase concentrations of cilostazol and its above mentioned active metabolite. Therefore a dose reduction of cilostazol from 100 mg b.i.d. to 50 mg b.i.d. should be considered.
7.4 Tacrolimus
Concomitant administration of omeprazole and tacrolimus may increase the serum levels of tacrolimus.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Reproductive studies in rats and rabbits with omeprazole and multiple cohort studies in pregnant women with omeprazole use during the first trimester do not show an increased risk of congenital anomalies or adverse pregnancy outcomes. There are no adequate and well controlled studies on the use of omeprazole in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. The vast majority of reported experience with omeprazole during human pregnancy is first trimester exposure and the duration of use is rarely specified, e.g., intermittent vs. chronic. An expert review of published data on experiences with omeprazole use during pregnancy by TERIS - the Teratogen Information System - concluded that therapeutic doses during pregnancy are unlikely to pose a substantial teratogenic risk (the quantity and quality of data were assessed as fair).
Three epidemiological studies compared the frequency of congenital abnormalities among infants born to women who used omeprazole during pregnancy with the frequency of abnormalities among infants of women exposed to H2-receptor antagonists or other controls. A population-based prospective cohort epidemiological study from the Swedish Medical Birth Registry, covering approximately 99% of pregnancies, reported on 955 infants (824 exposed during the first trimester with 39 of these exposed beyond first trimester, and 131 exposed after the first trimester) whose mothers used omeprazole during pregnancy. In utero exposure to omeprazole was not associated with increased risk of any malformation (odds ratio 0.82, 95% CI 0.50 to 1.34), low birth weight or low Apgar score. The number of infants born with ventricular septal defects and the number of stillborn infants was slightly higher in the omeprazole-exposed infants than the expected number in the normal population. The author concluded that both effects may be random.
A retrospective cohort study reported on 689 pregnant women exposed to either H2-blockers or omeprazole in the first trimester (134 exposed to omeprazole). The overall malformation rate was 4.4% (95% CI 3.6 to 5.3) and the malformation rate for first trimester exposure to omeprazole was 3.6% (95% CI 1.5 to 8.1). The relative risk of malformations associated with first trimester exposure to omeprazole compared with non-exposed women was 0.9 (95% CI 0.3 to 2.2). The study could effectively rule out a relative risk greater than 2.5 for all malformations. Rates of preterm delivery or growth retardation did not differ between the groups.
A controlled prospective observational study followed 113 women exposed to omeprazole during pregnancy (89% first trimester exposures). The reported rates of major congenital malformations was 4% for the omeprazole group, 2% for controls exposed to non-teratogens and 2.8% in disease-paired controls (background incidence of major malformations 1% to 5%). Rates of spontaneous and elective abortions, preterm deliveries, gestational age at delivery and mean birth weight did not differ between the groups. The sample size in this study has 80% power to detect a 5-fold increase in the rate of major malformation.
Several studies have reported no apparent adverse short-term effects on the infant when single dose oral or intravenous omeprazole was administered to over 200 pregnant women as premedication for cesarean section under general anesthesia.
Reproductive studies conducted with omeprazole on rats at oral doses up to 56 times the human dose and in rabbits at doses up to 56 times the human dose did not show any evidence of teratogenicity. In pregnant rabbits, omeprazole at doses about 5.5 to 56 times the human dose produced dose related increases in embryo-lethality, fetal resorptions and pregnancy loss. In rats treated with omeprazole at doses about 5.6 to 56 times the human dose, dose related embryo/fetal toxicity and postnatal developmental toxicity occurred in offspring [see Animal Toxicology and/or Pharmacology (13.2)].
8.3 Nursing Mothers
Omeprazole concentrations have been measured in breast milk of a woman following oral administration of 20 mg. The peak concentration of omeprazole in breast milk was less than 7% of the peak serum concentration. This concentration would correspond to 0.004 mg of omeprazole in 200 mL of milk. Because omeprazole is excreted in human milk, because of the potential for serious adverse reactions in nursing infants from omeprazole, and because of the potential for tumorigenicity shown for omeprazole in rat carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Use of omeprazole in pediatric and adolescent patients 2 to 16 years of age for the treatment of GERD is supported by a) extrapolation of results, already included in the currently approved labeling, from adequate and well controlled studies that supported the approval of omeprazole for adults, and b) safety and pharmacokinetic studies performed in pediatric and adolescent patients [see Clinical Pharmacology, Pharmacokinetics, Pediatric for pharmacokinetic information (12.3) and Dosage and Administration (2), Adverse Reactions (6.1) and Clinical Studies, (14.6)]. The safety and effectiveness of omeprazole for the treatment of GERD in patients < 1 year of age have not been established. The safety and effectiveness of omeprazole for other pediatric uses have not been established.
8.5 Geriatric Use
Omeprazole was administered to over 2,000 elderly individuals (≥ 65 years of age) in clinical trials in the U.S. and Europe. There were no differences in safety and effectiveness between the elderly and younger subjects. Other reported clinical experience has not identified differences in response between the elderly and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
Pharmacokinetic studies have shown the elimination rate was somewhat decreased in the elderly and bioavailability was increased. The plasma clearance of omeprazole was 250 mL/min (about half that of young volunteers) and its plasma half-life averaged one hour, about twice that of young healthy volunteers. However, no dosage adjustment is necessary in the elderly [see Clinical Pharmacology (12.3)].
8.6 Hepatic Impairment
Consider dose reduction, particularly for maintenance of healing of erosive esophagitis [see Clinical Pharmacology (12.3)].
8.7 Renal Impairment
No dosage reduction is necessary [see Clinical Pharmacology (12.3)].
8.8 Asian Population
Consider dose reduction, particularly for maintenance of healing of erosive esophagitis [see Clinical Pharmacology (12.3)].
10 OVERDOSAGE
Reports have been received of overdosage with omeprazole in humans. Doses ranged up to 2400 mg (120 times the usual recommended clinical dose). Manifestations were variable, but included confusion, drowsiness, blurred vision, tachycardia, nausea, vomiting, diaphoresis, flushing, headache, dry mouth and other adverse reactions similar to those seen in normal clinical experience [see Adverse Reactions (6)]. Symptoms were transient, and no serious clinical outcome has been reported when omeprazole was taken alone. No specific antidote for omeprazole overdosage is known. Omeprazole is extensively protein bound and is, therefore, not readily dialyzable. In the event of overdosage, treatment should be symptomatic and supportive.
As with the management of any overdose, the possibility of multiple drug ingestion should be considered. For current information on treatment of any drug overdose, contact a Poison Control Center at 1-800-222-1222.
Single oral doses of omeprazole at 1350, 1339 and 1200 mg/kg were lethal to mice, rats and dogs, respectively. Animals given these doses showed sedation, ptosis, tremors, convulsions and decreased activity, body temperature and respiratory rate and increased depth of respiration.
11 DESCRIPTION
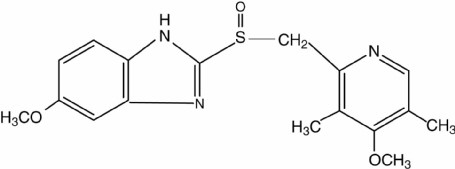
The active ingredient in omeprazole delayed-release capsules is a substituted benzimidazole, 5-methoxy-2-[[(4-methoxy-3, 5-dimethyl-2-pyridinyl) methyl] sulfinyl]1H-benzimidazole, a compound that inhibits gastric acid secretion. Its molecular formula is C17H19N3O3S, with a molecular weight of 345.42. The structural formula is:
Omeprazole, USP is a white to off-white crystalline powder which melts with decomposition at about 155°C. It is a weak base, freely soluble in ethanol and methanol, and slightly soluble in acetone and isopropanol and very slightly soluble in water. The stability of omeprazole is a function of pH; it is rapidly degraded in acid media, but has acceptable stability under alkaline conditions.
Omeprazole is supplied as delayed-release capsules for oral administration. Each delayed-release capsule contains either 10 mg, 20 mg or 40 mg of omeprazole, USP in the form of enteric-coated granules with the following inactive ingredients: ammonium hydroxide, dibutyl sebacate, ethylcellulose, fumed silica, hypromellose, methacrylic acid, oleic acid, sugar spheres, talc, titanium dioxide and triethyl citrate. The empty gelatin capsule shells contain D&C Yellow No. 10, FD&C Green No. 3, gelatin, silicon dioxide, sodium lauryl sulfate and titanium dioxide. The 40 mg empty gelatin capsule shell also contains FD&C Blue No. 1. In addition, the white imprinting ink contains ammonium hydroxide, pharmaceutical glaze, simethicone and titanium dioxide.
Omeprazole Delayed-Release Capsules USP, 10 mg, 20 mg and 40 mg meet USP Drug Release Test 2.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Omeprazole belongs to a class of antisecretory compounds, the substituted benzimidazoles, that suppress gastric acid secretion by specific inhibition of the H+/K+ ATPase enzyme system at the secretory surface of the gastric parietal cell. Because this enzyme system is regarded as the acid (proton) pump within the gastric mucosa, omeprazole has been characterized as a gastric acid-pump inhibitor, in that it blocks the final step of acid production. This effect is dose related and leads to inhibition of both basal and stimulated acid secretion irrespective of the stimulus. Animal studies indicate that after rapid disappearance from plasma, omeprazole can be found within the gastric mucosa for a day or more.
12.2 Pharmacodynamics
Antisecretory Activity
After oral administration, the onset of the antisecretory effect of omeprazole occurs within one hour, with the maximum effect occurring within 2 hours. Inhibition of secretion is about 50% of maximum at 24 hours and the duration of inhibition lasts up to 72 hours. The antisecretory effect thus lasts far longer than would be expected from the very short (less than one hour) plasma half-life, apparently due to prolonged binding to the parietal H+/K+ATPase enzyme. When the drug is discontinued, secretory activity returns gradually, over 3 to 5 days. The inhibitory effect of omeprazole on acid secretion increases with repeated once-daily dosing, reaching a plateau after 4 days.
Results from numerous studies of the antisecretory effect of multiple doses of 20 mg and 40 mg of omeprazole in normal volunteers and patients are shown below. The “max” value represents determinations at a time of maximum effect (2 to 6 hours after dosing), while “min” values are those 24 hours after the last dose of omeprazole.
| Omeprazole | Omeprazole | |||
| Parameter | 20 mg | 40 mg | ||
| % Decrease in Basal Acid | Max | Min | Max | Min |
| Output | 78 |
58 to 80 | 94 |
80 to 93 |
| % Decrease in Peak Acid | ||||
| Output | 79 |
50 to 59 | 88 |
62 to 68 |
| % Decrease in 24-hr | ||||
| Intragastric Acidity | 80 to 97 | 92 to 94 | ||
Single daily oral doses of omeprazole ranging from a dose of 10 mg to 40 mg have produced 100% inhibition of 24 hour intragastric acidity in some patients.
Serum Gastric Effects
In studies involving more than 200 patients, serum gastrin levels increased during the first 1 to 2 weeks of once-daily administration of therapeutic doses of omeprazole in parallel with inhibition of acid secretion. No further increase in serum gastrin occurred with continued treatment. In comparison with histamine H2-receptor antagonists, the median increases produced by 20 mg doses of omeprazole were higher (1.3- to 3.6-fold vs. 1.1- to 1.8-fold increase). Gastrin values returned to pretreatment levels, usually within 1 to 2 weeks after discontinuation of therapy.
Enterochromaffin-Like (ECL) Cell Effects
Human gastric biopsy specimens have been obtained from more than 3,000 patients treated with omeprazole in long-term clinical trials. The incidence of ECL cell hyperplasia in these studies increased with time; however, no case of ECL cell carcinoids, dysplasia or neoplasia has been found in these patients [see Clinical Pharmacology (12)]. However, these studies are of insufficient duration and size to rule out the possible influence of long-term administration of omeprazole on the development of any premalignant or malignant conditions.
Other Effects
Systemic effects of omeprazole in the CNS, cardiovascular and respiratory systems have not been found to date. Omeprazole, given in oral doses of 30 mg or 40 mg for 2 to 4 weeks, had no effect on thyroid function, carbohydrate metabolism or circulating levels of parathyroid hormone, cortisol, estradiol, testosterone, prolactin, cholecystokinin or secretin.
No effect on gastric emptying of the solid and liquid components of a test meal was demonstrated after a single dose of omeprazole 90 mg. In healthy subjects, a single I.V. dose of omeprazole (0.35 mg/kg) had no effect on intrinsic factor secretion. No systematic dose dependent effect has been observed on basal or stimulated pepsin output in humans.
However, when intragastric pH is maintained at 4.0 or above, basal pepsin output is low, and pepsin activity is decreased.
As do other agents that elevate intragastric pH, omeprazole administered for 14 days in healthy subjects produced a significant increase in the intragastric concentrations of viable bacteria. The pattern of the bacterial species was unchanged from that commonly found in saliva. All changes resolved within 3 days of stopping treatment.
The course of Barrett’s esophagus in 106 patients was evaluated in a U.S. double-blind controlled study of omeprazole 40 mg twice daily for 12 months followed by 20 mg twice daily for 12 months or ranitidine 300 mg twice daily for 24 months. No clinically significant impact on Barrett’s mucosa by antisecretory therapy was observed. Although neosquamous epithelium developed during antisecretory therapy, complete elimination of Barrett’s mucosa was not achieved. No significant difference was observed between treatment groups in development of dysplasia in Barrett’s mucosa and no patient developed esophageal carcinoma during treatment. No significant differences between treatment groups were observed in development of ECL cell hyperplasia, corpus atrophic gastritis, corpus intestinal metaplasia or colon polyps exceeding 3 mm in diameter [see Clinical Pharmacology (12)].
12.3 Pharmacokinetics
Absorption
Omeprazole delayed-release capsules contain an enteric-coated granule formulation of omeprazole (because omeprazole is acid-labile), so that absorption of omeprazole begins only after the granules leave the stomach. Absorption is rapid, with peak plasma levels of omeprazole occurring within 0.5 to 3.5 hours. Peak plasma concentrations of omeprazole and AUC are approximately proportional to doses up to 40 mg, but because of a saturable first-pass effect, a greater than linear response in peak plasma concentration and AUC occurs with doses greater than 40 mg. Absolute bioavailability (compared with intravenous administration) is about 30% to 40% at doses of 20 mg to 40 mg, due in large part to presystemic metabolism. In healthy subjects the plasma half-life is 0.5 to 1 hour, and the total body clearance is 500 to 600 mL/min.
The bioavailability of omeprazole increases slightly upon repeated administration of omeprazole delayed-release capsules.
Omeprazole delayed-release capsule 40 mg was bioequivalent when administered with and without applesauce. However, omeprazole delayed-release capsule 20 mg was not bioequivalent when administered with and without applesauce. When administered with applesauce, a mean 25% reduction in Cmax was observed without a significant change in AUC for omeprazole delayed-release capsule 20 mg. The clinical relevance of this finding is unknown.
Distribution
Protein binding is approximately 95%.
Metabolism
Omeprazole is extensively metabolized by the cytochrome P450 (CYP) enzyme system.
Excretion
Following single dose oral administration of a buffered solution of omeprazole, little if any unchanged drug was excreted in urine. The majority of the dose (about 77%) was eliminated in urine as at least six metabolites. Two were identified as hydroxyomeprazole and the corresponding carboxylic acid. The remainder of the dose was recoverable in feces. This implies a significant biliary excretion of the metabolites of omeprazole. Three metabolites have been identified in plasma — the sulfide and sulfone derivatives of omeprazole and hydroxyomeprazole. These metabolites have very little or no antisecretory activity.
Combination Therapy with Antimicrobials
Omeprazole 40 mg daily was given in combination with clarithromycin 500 mg every 8 hours to healthy adult male subjects. The steady state plasma concentrations of omeprazole were increased (Cmax, AUC0 to 24, and T1/2 increases of 30%, 89% and 34% respectively) by the concomitant administration of clarithromycin. The observed increases in omeprazole plasma concentration were associated with the following pharmacological effects. The mean 24 hour gastric pH value was 5.2 when omeprazole was administered alone and 5.7 when coadministered with clarithromycin.
The plasma levels of clarithromycin and 14-hydroxy-clarithromycin were increased by the concomitant administration of omeprazole. For clarithromycin, the mean Cmax was 10% greater, the mean Cmin was 27% greater, and the mean AUC0 to 8 was 15% greater when clarithromycin was administered with omeprazole than when clarithromycin was administered alone. Similar results were seen for 14- hydroxy-clarithromycin, the mean Cmax was 45% greater, the mean Cmin was 57% greater, and the mean AUC0 to 8 was 45% greater. Clarithromycin concentrations in the gastric tissue and mucus were also increased by concomitant administration of omeprazole.
| Tissue | Clarithromycin | Clarithromycin + Omeprazole |
| Antrum | 10.48 ± 2.01 (n = 5) | 19.96 ± 4.71 (n = 5) |
| Fundus | 20.81 ± 7.64 (n = 5) | 24.25 ± 6.37 (n = 5) |
| Mucus | 4.15 ± 7.74 (n = 4) | 39.29 ± 32.79 (n = 4) |
Special Populations
Geriatric Population
The elimination rate of omeprazole was somewhat decreased in the elderly and bioavailability was increased. Omeprazole was 76% bioavailable when a single 40 mg oral dose of omeprazole (buffered solution) was administered to healthy elderly volunteers, vs. 58% in young volunteers given the same dose. Nearly 70% of the dose was recovered in urine as metabolites of omeprazole and no unchanged drug was detected. The plasma clearance of omeprazole was 250 mL/min (about half that of young volunteers) and its plasma half-life averaged one hour, about twice that of young healthy volunteers.
Pediatric Use
The pharmacokinetics of omeprazole have been investigated in pediatric patients 2 to 16 years of age:
| Single or | Children |
Children |
Adults |
| Repeated | ≤ 20 kg | > 20 kg | (mean 76 kg) |
| Oral Dosing | 2 to 5 years | 6 to 16 years | 23 to 29 years |
| /Parameter | 10 mg | 20 mg | (n = 12) |
| Single Dosing | |||
Cmax
 (ng/mL) |
288 (n = 10) |
495 (n = 49) |
668 |
AUC (ng h/mL) |
511 (n = 7) |
1,140 (n = 32) |
1,220 |
| Repeated Dosing | |||
Cmax
 (ng/mL) |
539 (n = 4) |
851 (n = 32) |
1,458 |
AUC (ng h/mL) |
1,179 (n = 2) |
2.276 (n = 23) |
3,352 |
| Doses of 10 mg, 20 mg and 40 mg omeprazole as enteric-coated granules | |||
Following comparable mg/kg doses of omeprazole, younger children (2 to 5 years of age) have lower AUCs than children 6 to 16 years of age or adults; AUCs of the latter two groups did not differ [see Dosage and Administration (2)].
Hepatic Impairment
In patients with chronic hepatic disease, the bioavailability increased to approximately 100% compared with an I.V. dose, reflecting decreased first-pass effect, and the plasma half-life of the drug increased to nearly 3 hours compared with the half-life in normals of 0.5 to 1 hour. Plasma clearance averaged 70 mL/min, compared with a value of 500 to 600 mL/min in normal subjects. Dose reduction, particularly where maintenance of healing of erosive esophagitis is indicated, for the hepatically impaired should be considered.
Renal Impairment
In patients with chronic renal impairment, whose creatinine clearance ranged between 10 and 62 mL/min/1.73 m2, the disposition of omeprazole was very similar to that in healthy volunteers, although there was a slight increase in bioavailability. Because urinary excretion is a primary route of excretion of omeprazole metabolites, their elimination slowed in proportion to the decreased creatinine clearance. No dose reduction is necessary in patients with renal impairment.
Asian Population
In pharmacokinetic studies of single 20 mg omeprazole doses, an increase in AUC of approximately 4-fold was noted in Asian subjects compared with Caucasians. Dose reduction, particularly where maintenance of healing of erosive esophagitis is indicated, for Asian subjects should be considered.
12.4 Microbiology
Omeprazole and clarithromycin dual therapy and omeprazole, clarithromycin and amoxicillin triple therapy have been shown to be active against most strains of Helicobacter pylori in vitro and in clinical infections as described in the Indications and Usage section (1.1).
Helicobacter
Helicobacter pylori-Pretreatment Resistance
Clarithromycin pretreatment resistance rates were 3.5% (4/113) in the omeprazole/clarithromycin dual therapy studies (4 and 5) and 9.3% (41/439) in omeprazole/clarithromycin/amoxicillin triple therapy studies (1, 2 and 3).
Amoxicillin pretreatment susceptible isolates (≤ 0.25 mcg/mL) were found in 99.3% (436/439) of the patients in the omeprazole/clarithromycin/amoxicillin triple therapy studies (1, 2 and 3). Amoxicillin pretreatment minimum inhibitory concentrations (MICs) > 0.25 mcg /mL occurred in 0.7% (3/439) of the patients, all of whom were in the clarithromycin and amoxicillin study arm. One patient had an unconfirmed pretreatment amoxicillin minimum inhibitory concentration (MIC) of > 256 mcg /mL by Etest®.
| Clarithromycin Susceptibility Test Results and Clinical/Bacteriological Outcomes | ||||||
| Clarithromycin Pretreatment Results |
Clarithromycin Post-treatment Results | |||||
|
H. pylori negative -eradicated |
H. pylori positive-not eradicated | |||||
| Post-treatment susceptibility results | ||||||
S |
I |
R  |
No MIC | |||
| Dual Therapy - (omeprazole 40 mg once daily/clarithromycin 500 mg three times daily for 14 days followed by omeprazole 20 mg once daily for another 14 days) (Studies 4, 5) | ||||||
Susceptible |
108 | 72 | 1 | 26 | 9 | |
Intermediate |
1 | 1 | ||||
Resistant  |
4 | 4 | ||||
| Triple Therapy - (omeprazole 20 mg twice daily/clarithromycin 500 mg twice daily/amoxicillin 1 g twice daily for 10 days - Studies 1, 2, 3; followed by omeprazole 20 mg once daily for another 18 days - Studies 1, 2) | ||||||
Susceptible  |
171 | 153 | 7 | 3 | 8 | |
Intermediate  |
||||||
Resistant  |
14 | 4 | 1 | 6 | 3 | |
Patients not eradicated of H. pylori following omeprazole/clarithromycin/amoxicillin triple therapy or omeprazole/clarithromycin dual therapy will likely have clarithromycin resistant H. pylori isolates. Therefore, clarithromycin susceptibility testing should be done, if possible. Patients with clarithromycin resistant H. pylori should not be treated with any of the following: omeprazole/clarithromycin dual therapy, omeprazole/clarithromycin/amoxicillin triple therapy, or other regimens which include clarithromycin as the sole antimicrobial agent.
Amoxicillin Susceptibility Test Results and Clinical/Bacteriological Outcomes
In the triple therapy clinical trials, 84.9% (157/185) of the patients in the omeprazole/clarithromycin/amoxicillin treatment group who had pretreatment amoxicillin susceptible MICs (≤ 0.25 mcg/mL) were eradicated of H. pylori and 15.1% (28/185) failed therapy. Of the 28 patients who failed triple therapy, 11 had no post-treatment susceptibility test results and 17 had post-treatment H. pylori isolates with amoxicillin susceptible MICs. Eleven of the patients who failed triple therapy also had post-treatment H. pylori isolates with clarithromycin resistant MICs.
Susceptibility Test for
The reference methodology for susceptibility testing of H. pylori is agar dilution MICs1. One to three microliters of an inoculum equivalent to a No. 2 McFarland standard (1 x 107 to 1 x 108 CFU/mL for H. pylori) are inoculated directly onto freshly prepared antimicrobial containing Mueller-Hinton agar plates with 5% aged defibrinated sheep blood (≥ 2 weeks old). The agar dilution plates are incubated at 35°C in a microaerobic environment produced by a gas generating system suitable for campylobacters. After 3 days of incubation, the MICs are recorded as the lowest concentration of antimicrobial agent required to inhibit growth of the organism. The clarithromycin and amoxicillin MIC values should be interpreted according to the following criteria:
Clarithromycin MIC (mcg/mL) |
Interpretation |
| ≤0.25 | Susceptible (S) |
| 0.5 | Intermediate (I) |
| >1 | Resistant (R) |
Amoxicillin MIC (mcg/mL) |
Interpretation |
| ≤0.25 | Susceptible (S) |
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard clarithromycin and amoxicillin powders should provide the following MIC values:
| Microorganism | Antimicrobial Agent | MIC (mcg/mL) |
| H. pylori ATCC 43504 | Clarithromycin | 0.016 to 0.12 (mcg/mL) |
| H. pylori ATCC 43504 | Amoxicillin | 0.016 to 0.12 (mcg/mL) |
Effects on Gastrointestinal Microbial Ecology
Decreased gastric acidity due to any means including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and possibly Clostridium difficile in hospitalized patients.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In two 24-month carcinogenicity studies in rats, omeprazole at daily doses of 1.7, 3.4, 13.8, 44 and 140.8 mg/kg/day (about 0.7 to 57 times a human dose of 20 mg/day, as expressed on a body surface area basis) produced gastric ECL cell carcinoids in a dose related manner in both male and female rats; the incidence of this effect was markedly higher in female rats, which had higher blood levels of omeprazole. Gastric carcinoids seldom occur in the untreated rat. In addition, ECL cell hyperplasia was present in all treated groups of both sexes. In one of these studies, female rats were treated with 13.8 mg omeprazole/kg/day (about 6 times a human dose of 20 mg/day, based on body surface area) for one year and then followed for an additional year without the drug. No carcinoids were seen in these rats. An increased incidence of treatment-related ECL cell hyperplasia was observed at the end of one year (94% treated vs. 10% controls). By the second year the difference between treated and control rats was much smaller (46% vs. 26%) but still showed more hyperplasia in the treated group. Gastric adenocarcinoma was seen in one rat (2%). No similar tumor was seen in male or female rats treated for 2 years. For this strain of rat no similar tumor has been noted historically, but a finding involving only one tumor is difficult to interpret. In a 52-week toxicity study in Sprague-Dawley rats, brain astrocytomas were found in a small number of males that received omeprazole at dose levels of 0.4, 2 and 16 mg/kg/day (about 0.2 to 6.5 times the human dose on a body surface area basis). No astrocytomas were observed in female rats in this study. In a 2-year carcinogenicity study in Sprague-Dawley rats, no astrocytomas were found in males or females at the high dose of 140.8 mg/kg/day (about 57 times the human dose on a body surface area basis). A 78-week mouse carcinogenicity study of omeprazole did not show increased tumor occurrence, but the study was not conclusive. A 26-week p53 (+/-) transgenic mouse carcinogenicity study was not positive.
Omeprazole was positive for clastogenic effects in an in vitro human lymphocyte chromosomal aberration assay, in one of two in vivo mouse micronucleus tests, and in an in vivo bone marrow cell chromosomal aberration assay. Omeprazole was negative in the in vitro Ames test, an in vitro mouse lymphoma cell forward mutation assay, and an in vivo rat liver DNA damage assay.
Omeprazole at oral doses up to 138 mg/kg/day in rats (about 56 times the human dose on a body surface area basis) was found to have no effect on fertility and reproductive performance.
In 24-month carcinogenicity studies in rats, a dose related significant increase in gastric carcinoid tumors and ECL cell hyperplasia was observed in both male and female animals [see Warnings and Precautions (5)]. Carcinoid tumors have also been observed in rats subjected to fundectomy or long-term treatment with other proton pump inhibitors or high doses of H2-receptor antagonists.
13.2 Animal Toxicology and/or Pharmacology
Reproductive Toxicology Studies
Reproductive studies conducted with omeprazole in rats at oral doses up to 138 mg/kg/day (about 56 times the human dose on a body surface area basis) and in rabbits at doses up to 69 mg/kg/day (about 56 times the human dose on a body surface area basis) did not disclose any evidence for a teratogenic potential of omeprazole. In rabbits, omeprazole in a dose range of 6.9 to 69.1 mg/kg/day (about 5.5 to 56 times the human dose on a body surface area basis) produced dose related increases in embryo-lethality, fetal resorptions and pregnancy disruptions. In rats, dose related embryo/fetal toxicity and postnatal developmental toxicity were observed in offspring resulting from parents treated with omeprazole at 13.8 to 138 mg/kg/day (about 5.6 to 56 times the human doses on a body surface area basis).
14 CLINICAL STUDIES
14.1 Duodenal Ulcer Disease
Active Duodenal Ulcer
In a multicenter, double-blind, placebo-controlled study of 147 patients with endoscopically documented duodenal ulcer, the percentage of patients healed (per protocol) at 2 and 4 weeks was significantly higher with omeprazole 20 mg once daily than with placebo (p ≤ 0.01).
| Omeprazole | Placebo | |
| 20 mg a.m. | a.m. | |
| (n = 99) | (n = 48) | |
| Week 2 |
 |
13 |
| Week 4 |
 |
27 |
Complete daytime and nighttime pain relief occurred significantly faster (p ≤ 0.01) in patients treated with omeprazole 20 mg than in patients treated with placebo. At the end of the study, significantly more patients who had received omeprazole had complete relief of daytime pain (p ≤ 0.05) and nighttime pain (p ≤ 0.01).
In a multicenter, double-blind study of 293 patients with endoscopically documented duodenal ulcer, the percentage of patients healed (per protocol) at 4 weeks was significantly higher with omeprazole 20 mg once daily than with ranitidine 150 mg b.i.d. (p < 0.01).
| Omeprazole | Ranitidine | |
| 20 mg a.m. (n = 145) |
150 mg twice daily (n = 148) |
|
| Week 2 | 42 | 34 |
| Week 4 | 82 | 63 |
Healing occurred significantly faster in patients treated with omeprazole than in those treated with ranitidine 150 mg b.i.d. (p < 0.01).
In a foreign multinational randomized, double-blind study of 105 patients with endoscopically documented duodenal ulcer, 20 mg and 40 mg of omeprazole were compared with 150 mg b.i.d. of ranitidine at 2, 4 and 8 weeks. At 2 and 4 weeks both doses of omeprazole were statistically superior (per protocol) to ranitidine, but 40 mg was not superior to 20 mg of omeprazole, and at 8 weeks there was no significant difference between any of the active drugs.
| Omeprazole | Ranitidine | ||
| 20 mg | 40 mg | 150 mg twice daily | |
| (n = 34) | (n = 36) | (n = 35) | |
| Week 2 |
 |
 |
53 |
| Week 4 |
 |
 |
82 |
| Week 8 | 100 | 100 | 94 |
Eradication in Patients with Duodenal Ulcer Disease
Triple Therapy (omeprazole/clarithromycin/amoxicillin)
Three U.S., randomized, double-blind clinical studies in patients with H. pylori infection and duodenal ulcer disease (n = 558) compared omeprazole plus clarithromycin plus amoxicillin with clarithromycin plus amoxicillin. Two studies (1 and 2) were conducted in patients with an active duodenal ulcer, and the other study (3) was conducted in patients with a history of a duodenal ulcer in the past 5 years but without an ulcer present at the time of enrollment. The dose regimen in the studies was omeprazole 20 mg twice daily plus clarithromycin 500 mg twice daily plus amoxicillin 1 g twice daily for 10 days; or clarithromycin 500 mg twice daily plus amoxicillin 1 g twice daily for 10 days. In studies 1 and 2, patients who took the omeprazole regimen also received an additional 18 days of omeprazole 20 mg once daily. Endpoints studied were eradication of H. pylori and duodenal ulcer healing (studies 1 and 2 only). H. pylori status was determined by CLOtest®, histology and culture in all three studies. For a given patient, H. pylori was considered eradicated if at least two of these tests were negative, and none was positive.
The combination of omeprazole plus clarithromycin plus amoxicillin was effective in eradicating H. pylori.
| omeprazole + clarithromycin | clarithromycin + amoxicillin | |||
| + amoxicillin | ||||
Per-Protocol |
Intent-to-Treat |
Per-Protocol |
Intent-to-Treat |
|
| Study 1 |
 |
 |
43 [31, 56] | 37 [27, 48] |
| (n = 64) | (n = 80) | (n = 67) | (n = 84) | |
| Study 2 |
 |
 |
41 [29, 54] | 36 [26, 47] |
| (n = 65) | (n = 77) | (n = 68) | (n = 83) | |
| Study 3 |  |
 |
33 [24, 44] | 32 [23, 42] |
| (n = 69) | (n = 84) | (n = 93) | (n = 99) | |
Dual Therapy (omeprazole/clarithromycin)
Four randomized, double-blind, multi-center studies (4, 5, 6 and 7) evaluated omeprazole 40 mg once daily plus clarithromycin 500 mg three times daily for 14 days, followed by omeprazole 20 mg once daily, (Studies 4, 5 and 7) or by omeprazole 40 mg once daily (Study 6) for an additional 14 days in patients with active duodenal ulcer associated with H. pylori. Studies 4 and 5 were conducted in the U.S. and Canada and enrolled 242 and 256 patients, respectively. H. pylori infection and duodenal ulcer were confirmed in 219 patients in Study 4 and 228 patients in Study 5. These studies compared the combination regimen to omeprazole and clarithromycin monotherapies. Studies 6 and 7 were conducted in Europe and enrolled 154 and 215 patients, respectively. H. pylori infection and duodenal ulcer were confirmed in 148 patients in study 6 and 208 patients in Study 7. These studies compared the combination regimen with omeprazole monotherapy. The results for the efficacy analyses for these studies are described below. H. pylori eradication was defined as no positive test (culture or histology) at 4 weeks following the end of treatment, and two negative tests were required to be considered eradicated of H. pylori. In the per-protocol analysis, the following patients were excluded: dropouts, patients with missing H. pylori tests post-treatment, and patients that were not assessed for H. pylori eradication because they were found to have an ulcer at the end of treatment.
The combination of omeprazole and clarithromycin was effective in eradicating H. pylori.
| omeprazole + | |||
| clarithromycin | omeprazole | clarithromycin | |
| U.S. Studies | |||
| Study 4 | 74 [60, 85]  |
0 [0, 7] | 31 [18, 47] |
| (n = 53) | (n = 54) | (n = 42) | |
| Study 5 | 64 [51, 76]  |
0 [0, 6] | 39 [24, 55] |
| (n = 61) | (n = 59) | (n = 44) | |
| Non U.S. Studies | |||
| Study 6 | 83 [71, 92] |
1 [0, 7] | N/A |
| (n = 60) | (n = 74) | ||
| Study 7 | 74 [64, 83] |
1 [0, 6] | N/A |
| (n = 86) | (n = 90) |
Ulcer healing was not significantly different when clarithromycin was added to omeprazole therapy compared with omeprazole therapy alone.
The combination of omeprazole and clarithromycin was effective in eradicating H. pylori and reduced duodenal ulcer recurrence.
|
Duodenal Ulcer Recurrence Rates by |
||
|
H. pylori eradicated |
H. pylori not eradicated |
|
| U.S. Studies | ||
| 6 months post-treatment | ||
| Study 4 |
|
60 (n = 88) |
| Study 5 |
|
60 (n = 106) |
| Non U.S. Studies | ||
| 6 months post-treatment | ||
| Study 6 |
|
46 (n = 78) |
| Study 7 |
|
43 (n = 107) |
| 12 months post-treatment | ||
| Study 6 |
|
68 (n = 71) |
14.2 Gastric Ulcer
In a U.S. multicenter, double-blind, study of omeprazole 40 mg once daily, 20 mg once daily and placebo in 520 patients with endoscopically diagnosed gastric ulcer, the following results were obtained.
| Omeprazole | Omeprazole | ||
| 20 mg once daily | 40 mg once daily | Placebo | |
| (n = 202) | (n = 214) | (n = 104) | |
| Week 4 | 47.5 |
55.6 |
30.8 |
| Week 8 | 74.8 |
82.7  |
48.1 |
For the stratified groups of patients with ulcer size less than or equal to 1 cm, no difference in healing rates between 40 mg and 20 mg was detected at either 4 or 8 weeks. For patients with ulcer size greater than 1 cm, 40 mg was significantly more effective than 20 mg at 8 weeks.
In a foreign, multinational, double-blind study of 602 patients with endoscopically diagnosed gastric ulcer, omeprazole 40 mg once daily, 20 mg once daily and ranitidine 150 mg twice a day were evaluated.
| Omeprazole | Omeprazole | Ranitidine | |
| 20 mg once daily | 40 mg once daily | 150 mg twice daily | |
| (n = 200) | (n = 187) | (n = 199) | |
| Week 4 | 63.5 | 78.1  |
56.3 |
| Week 8 | 81.5 | 91.4  |
78.4 |
14.3 Gastroesophageal Reflux Disease (GERD)
Symptomatic GERD
A placebo-controlled study was conducted in Scandinavia to compare the efficacy of omeprazole 20 mg or 10 mg once daily for up to 4 weeks in the treatment of heartburn and other symptoms in GERD patients without erosive esophagitis. Results are shown below.
| Omeprazole | Omeprazole | Placebo | |
| 20 mg a.m. | 10 mg a.m. | a.m. | |
| All patients | 46  |
31 |
13 |
| (n = 205) | (n = 199) | (n = 105) | |
| Patients with | 56  |
36 |
14 |
| confirmed GERD | (n = 115) | (n = 109) | (n = 59) |
14.4 Erosive Esophagitis
In a U.S. multicenter double-blind placebo controlled study of 20 mg or 40 mg of omeprazole delayed-release capsules in patients with symptoms of GERD and endoscopically diagnosed erosive esophagitis of grade 2 or above, the percentage healing rates (per protocol) were as follows:
| 20 mg Omeprazole | 40 mg Omeprazole | Placebo | |
| Week | (n = 83) | (n = 87) | (n = 43) |
| 4 | 39 |
45  |
7 |
| 8 | 74 |
75  |
14 |
In this study, the 40 mg dose was not superior to the 20 mg dose of omeprazole in the percentage healing rate. Other controlled clinical trials have also shown that omeprazole is effective in severe GERD. In comparisons with histamine H2-receptor antagonists in patients with erosive esophagitis, grade 2 or above, omeprazole in a dose of 20 mg was significantly more effective than the active controls. Complete daytime and nighttime heartburn relief occurred significantly faster (p < 0.01) in patients treated with omeprazole than in those taking placebo or histamine H2- receptor antagonists.
In this and five other controlled GERD studies, significantly more patients taking 20 mg omeprazole (84%) reported complete relief of GERD symptoms than patients receiving placebo (12%).
Long-Term Maintenance of Healing of Erosive Esophagitis
In a U.S. double-blind, randomized, multicenter, placebo controlled study, two dose regimens of omeprazole were studied in patients with endoscopically confirmed healed esophagitis. Results to determine maintenance of healing of erosive esophagitis are shown below.
| Omeprazole | Omeprazole | ||
| 20 mg once daily | 20 mg 3 days per week | Placebo | |
| (n = 138) | (n = 137) | (n = 131) | |
| Percent in endoscopic | |||
| remission at 6 months | 70 | 34 | 11 |
In an international multicenter double-blind study, omeprazole 20 mg daily and 10 mg daily were compared with ranitidine 150 mg twice daily in patients with endoscopically confirmed healed esophagitis. The table below provides the results of this study for maintenance of healing of erosive esophagitis.
| Omeprazole | Omeprazole | Ranitidine | |
| 20 mg once daily | 10 mg once daily | 150 mg twice daily | |
| (n = 131) | (n = 133) | (n = 128) | |
| Percent in endoscopic | |||
| remission at 12 months | 77 | 58 | 46 |
In patients who initially had grades 3 or 4 erosive esophagitis, for maintenance after healing 20 mg daily of omeprazole was effective, while 10 mg did not demonstrate effectiveness.
14.5 Pathological Hypersecretory Conditions
In open studies of 136 patients with pathological hypersecretory conditions, such as Zollinger-Ellison (ZE) syndrome with or without multiple endocrine adenomas, omeprazole delayed-release capsules significantly inhibited gastric acid secretion and controlled associated symptoms of diarrhea, anorexia and pain. Doses ranging from 20 mg every other day to 360 mg per day maintained basal acid secretion below 10 mEq/hr in patients without prior gastric surgery, and below 5 mEq/hr in patients with prior gastric surgery.
Initial doses were titrated to the individual patient need, and adjustments were necessary with time in some patients [see Dosage and Administration (2)]. Omeprazole was well tolerated at these high dose levels for prolonged periods (> 5 years in some patients). In most ZE patients, serum gastrin levels were not modified by omeprazole. However, in some patients serum gastrin increased to levels greater than those present prior to initiation of omeprazole therapy. At least 11 patients with ZE syndrome on long-term treatment with omeprazole developed gastric carcinoids. These findings are believed to be a manifestation of the underlying condition, which is known to be associated with such tumors, rather than the result of the administration of omeprazole [see Adverse Reactions (6)].
14.6 Pediatric GERD
Symptomatic GERD
The effectiveness of omeprazole for the treatment of nonerosive GERD in pediatric patients 2 to 16 years of age is based in part on data obtained from pediatric patients in an uncontrolled Phase III study [see Use in Specific Populations (8.4)].
The study enrolled 113 pediatric patients 2 to 16 years of age with a history of symptoms suggestive of nonerosive GERD. Patients were administered a single dose of omeprazole (10 mg or 20 mg, based on body weight) for 4 weeks either as an intact capsule or as an open capsule in applesauce. Successful response was defined as no moderate or severe episodes of either pain-related symptoms or vomiting/regurgitation during the last 4 days of treatment. Results showed success rates of 60% (9/15; 10 mg omeprazole) and 59% (58/98; 20 mg omeprazole), respectively.
Healing of Erosive Esophagitis
In an uncontrolled, open-label dose-titration study, healing of erosive esophagitis in pediatric patients 1 to 16 years of age required doses that ranged from 0.7 to 3.5 mg/kg/day (80 mg/day). Doses were initiated at 0.7 mg/kg/day. Doses were increased in increments of 0.7 mg/kg/day (if intraesophageal pH showed a pH of < 4 for less than 6% of a 24-hour study). After titration, patients remained on treatment for 3 months. Forty-four percent of the patients were healed on a dose of 0.7 mg/kg body weight; most of the remaining patients were healed with 1.4 mg/kg after an additional 3 months’ treatment. Erosive esophagitis was healed in 51 of 57 (90%) children who completed the first course of treatment in the healing phase of the study. In addition, after 3 months of treatment, 33% of the children had no overall symptoms, 57% had mild reflux symptoms and 40% had less frequent regurgitation/vomiting.
Maintenance of Healing of Erosive Esophagitis
In an uncontrolled, open-label study of maintenance of healing of erosive esophagitis in 46 pediatric patients, 54% of patients required half the healing dose. The remaining patients increased the healing dose (0.7 to a maximum of 2.8 mg/kg/day) either for the entire maintenance period or returned to half the dose before completion. Of the 46 patients who entered the maintenance phase, 19 (41%) had no relapse. In addition, maintenance therapy in erosive esophagitis patients resulted in 63% of patients having no overall symptoms.
15 REFERENCES
1. National Committee for Clinical Laboratory Standards. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically—Fifth Edition. Approved Standard NCCLS Document M7-A5, Vol, 20, No. 2, NCCLS, Wayne, PA, January 2000.
16 HOW SUPPLIED/STORAGE AND HANDLING
Omeprazole Delayed-Release Capsules, USP are available in the following strength: 20 mg.
The 20 mg capsule is a hard-shell gelatin capsule with a dark green opaque cap and a blue-green opaque body axially printed with MYLAN over 6150 in white ink both on the cap and the body. The capsule is filled with white to off-white beads. They are available as follows:
NDC 51079-007-20 - Unit dose blister packages of 100 (10 cards of 10 capsules each).
NDC 51079-007-19 - Robot Ready blister packages of 25 (25 cards of 1 capsule each).
NDC 51079-007-56 - Unit dose punch cards of 300 (10 punch cards of 30 capsules each).
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Protect from light and moisture.
17 PATIENT COUNSELING INFORMATION
Omeprazole delayed-release capsules should be taken before eating. Patients should be informed that the omeprazole delayed-release capsules should be swallowed whole.
For patients who have difficulty swallowing capsules, the contents of an omeprazole delayed-release capsule can be added to applesauce. One tablespoon of applesauce should be added to an empty bowl and the capsule should be opened. All of the pellets inside the capsule should be carefully emptied on the applesauce. The pellets should be mixed with the applesauce and then swallowed immediately with a glass of cool water to ensure complete swallowing of the pellets. The applesauce used should not be hot and should be soft enough to be swallowed without chewing. The pellets should not be chewed or crushed. The pellets/applesauce mixture should not be stored for future use.
Jointly manufactured by:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.
and
Laboratorios Dr. Esteve, S.A.
08107 Martorelles (Barcelona), Spain
Distributed by:
UDL Laboratories, Inc.
Rockford, IL 61103
Repacked by:
H. J. Harkins Company, Inc.
Nipomo, CA 93444
S-8162 R11
9/10
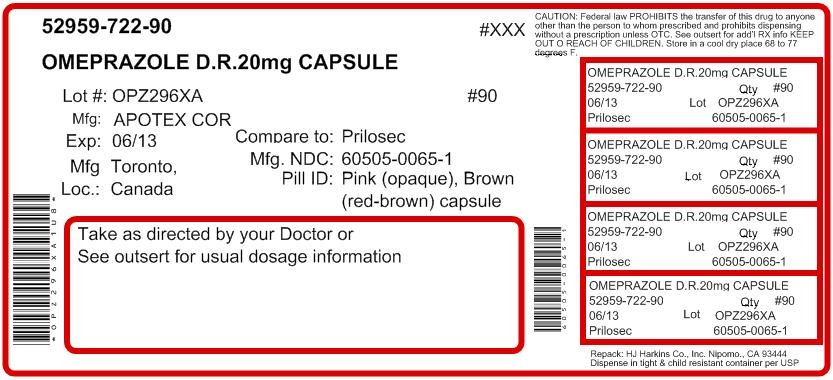
Principal Display panel
Omeprazole Delayed-Release Capsules, USP
20 mg
10 Capsules
OmeprazoleOmeprazole CAPSULE, DELAYED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||