Ondansetron
The Medicines Company
Fresenius Kabi USA, LLC
Ondansetron Injection USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- ONDANSETRON DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL TRIALS
- ONDANSETRON INDICATIONS AND USAGE
- ONDANSETRON CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- ONDANSETRON ADVERSE REACTIONS
- DRUG ABUSE AND DEPENDENCE
- OVERDOSAGE
- ONDANSETRON DOSAGE AND ADMINISTRATION
- STABILITY
- HOW SUPPLIED
- REFERENCES
FULL PRESCRIBING INFORMATION
Rx only
ONDANSETRON DESCRIPTION
The active ingredient in Ondansetron Injection, USP is ondansetron hydrochloride, the racemic form of ondansetron and a selective blocking agent of the serotonin 5-HT3 receptor type. Chemically it is (±) 1, 2, 3, 9-tetrahydro-9-methyl-3-[(2-methyl-1 H -imidazol-1-yl)methyl]-4 H -carbazol-4-one, monohydrochloride dihydrate. It has the following structural formula:

Ondansetron is a white to off-white powder that is sparingly soluble in water.
Sterile Injection for Intravenous (IV) or Intramuscular (IM) Administration
Each mL of the preservative-free aqueous solution in the 2 mL single-dose vial contains 2 mg of ondansetron as the hydrochloride; 9 mg of sodium chloride, USP; and 0.5 mg of citric acid monohydrate, USP and 0.25 mg of sodium citrate dihydrate, USP as buffers in Water for Injection, USP.
Each mL of the preserved aqueous solution in the 20-mL multidose vial contains 2 mg of ondansetron as the hydrochloride; 8.3 mg of sodium chloride, USP; 0.5 mg of citric acid monohydrate, USP and 0.25 mg of sodium citrate dihydrate, USP as buffers; and 1.2 mg of methylparaben, NF and 0.15 mg of propylparaben, NF as preservatives in Water for Injection, USP.
Ondansetron Injection is a clear, colorless, nonpyrogenic, sterile solution. The pH of the injection solution is 3.3 to 4.0.
CLINICAL PHARMACOLOGY
Pharmacodynamics
Ondansetron is a selective 5-HT3 receptor antagonist. While ondansetron’s mechanism of action has not been fully characterized, it is not a dopamine-receptor antagonist. Serotonin receptors of the 5-HT3 type are present both peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone of the area postrema. It is not certain whether ondansetron’s antiemetic action in chemotherapy-induced nausea and vomiting is mediated centrally, peripherally, or in both sites. However, cytotoxic chemotherapy appears to be associated with release of serotonin from the enterochromaffin cells of the small intestine. In humans, urinary 5-HIAA (5-hydroxyindoleacetic acid) excretion increases after cisplatin administration in parallel with the onset of vomiting. The released serotonin may stimulate the vagal afferents through the 5-HT3 receptors and initiate the vomiting reflex.
In animals, the emetic response to cisplatin can be prevented by pretreatment with an inhibitor of serotonin synthesis, bilateral abdominal vagotomy and greater splanchnic nerve section, or pretreatment with a serotonin 5-HT3 receptor antagonist.
In normal volunteers, single IV doses of 0.15 mg/kg of ondansetron had no effect on esophageal motility, gastric motility, lower esophageal sphincter pressure, or small intestinal transit time. In another study in six normal male volunteers, a 16 mg dose infused over 5 minutes showed no effect of the drug on cardiac output, heart rate, stroke volume, blood pressure, or electrocardiogram (ECG). Multiday administration of ondansetron has been shown to slow colonic transit in normal volunteers. Ondansetron has no effect on plasma prolactin concentrations.
In a gender-balanced pharmacodynamic study (n = 56), ondansetron 4 mg administered intravenously or intramuscularly was dynamically similar in the prevention of nausea and vomiting using the ipecacuanha model of emesis.
Ondansetron does not alter the respiratory depressant effects produced by alfentanil or the degree of neuromuscular blockade produced by atracurium. Interactions with general or local anesthetics have not been studied.
Pharmacokinetics
Ondansetron is extensively metabolized in humans, with approximately 5% of a radiolabeled dose recovered as the parent compound from the urine. The primary metabolic pathway is hydroxylation on the indole ring followed by glucuronide or sulfate conjugation.
Although some nonconjugated metabolites have pharmacologic activity, these are not found in plasma at concentrations likely to significantly contribute to the biological activity of ondansetron.
In vitro metabolism studies have shown that ondansetron is a substrate for human hepatic cytochrome P-450 enzymes, including CYP1A2, CYP2D6, and CYP3A4. In terms of overall ondansetron turnover, CYP3A4 played the predominant role. Because of the multiplicity of metabolic enzymes capable of metabolizing ondansetron, it is likely that inhibition or loss of one enzyme (e.g., CYP2D6 genetic deficiency) will be compensated by others and may result in little change in overall rates of ondansetron elimination. Ondansetron elimination may be affected by cytochrome P-450 inducers. In a pharmacokinetic study of 16 epileptic patients maintained chronically on CYP3A4 inducers, carbamazepine or phenytoin, reduction in AUC, Cmax and T1/2 of ondansetron was observed.1 This resulted in a significant increase in clearance. However, on the basis of available data, no dosage adjustment for ondansetron is recommended (see PRECAUTIONS , Drug Interactions ).
In humans, carmustine, etoposide, and cisplatin do not affect the pharmacokinetics of ondansetron.
In normal adult volunteers, the following mean pharmacokinetic data have been determined following a single 0.15 mg/kg IV dose.
Table 1: Pharmacokinetics in Normal Adult Volunteers
|
Age-group (years) |
n |
Peak Plasma Concentration (ng/mL) |
Mean Elimination Half-Life (h) |
Plasma Clearance (L/h/kg) |
|
19 to 40 |
11 |
102 |
3.5 |
0.381 |
|
61 to 74 |
12 |
106 |
4.7 |
0.319 |
|
≥ 75 |
11 |
170 |
5.5 |
0.262 |
A reduction in clearance and increase in elimination half-life are seen in patients over 75 years of age. In clinical trials with cancer patients, safety and efficacy were similar in patients over 65 years of age and those under 65 years of age; there was an insufficient number of patients over 75 years of age to permit conclusions in that age-group. No dosage adjustment is recommended in the elderly.
In patients with mild-to-moderate hepatic impairment, clearance is reduced 2-fold and mean half-life is increased to 11.6 hours compared to 5.7 hours in normals. In patients with severe hepatic impairment (Child- Pugh2 score of 10 or greater), clearance is reduced 2- fold to 3-fold and apparent volume of distribution is increased with a resultant increase in half-life to 20 hours. In patients with severe hepatic impairment, a total daily dose of 8 mg should not be exceeded.
Due to the very small contribution (5%) of renal clearance to the overall clearance, renal impairment was not expected to significantly influence the total clearance of ondansetron. However, ondansetron mean plasma clearance was reduced by about 41% in patients with severe renal impairment (creatinine clearance <30 mL/min). This reduction in clearance is variable and was not consistent with an increase in half-life. No reduction in dose or dosing frequency in these patients is warranted.
In adult cancer patients, the mean elimination half-life was 4 hours, and there was no difference in the multidose pharmacokinetics over a 4-day period. In a study of 21 pediatric cancer patients (4 to 18 years of age) who received three IV doses of 0.15 mg/kg of ondansetron at 4-hour intervals, patients older than 15 years of age exhibited ondansetron pharmacokinetic parameters similar to those of adults. Patients 4 to 12 years of age generally showed higher clearance and somewhat larger volume of distribution than adults. Most pediatric patients younger than 15 years of age with cancer had a shorter (2.4 hours) ondansetron plasma half-life than patients older than 15 years of age. It is not known whether these differences in ondansetron plasma half-life may result in differences in efficacy between adults and some young pediatric patients (see CLINICAL TRIALS, Pediatric Studies ).
Pharmacokinetic samples were collected from 74 cancer patients 6 to 48 months of age, who received a dose of 0.15 mg/kg of IV ondansetron every 4 hours for 3 doses during a safety and efficacy trial. These data were combined with sequential pharmacokinetics data from 41 surgery patients 1 month to 24 months of age, who received a single dose of 0.1 mg/kg of IV ondansetron prior to surgery with general anesthesia, and a population pharmacokinetic analysis was performed on the combined data set. The results of this analysis are included in Table 2 and are compared to the pharmacokinetic results in cancer patients 4 to 18 years of age.
Table 2: Pharmacokinetics in Pediatric Cancer Patients 1 Month to 18 Years of Age
|
Subjects and Age Group |
N |
CL |
Vdss |
T½ |
|
|
|
Geometric Mean |
Mean |
|
|
Pediatric Cancer Patients |
N = 21 |
0.599 |
1.9 |
2.8 |
|
Population PK Patientsa |
N = 115 |
0.582 |
3.65 |
4.9 |
aPopulation PK (Pharmacokinetic) Patients: 64% cancer patients and 36% surgery patients.
Based on the population pharmacokinetic analysis, cancer patients 6 to 48 months of age who receive a dose of 0.15 mg/kg of IV ondansetron every 4 hours for 3 doses would be expected to achieve a systemic exposure (AUC) consistent with the exposure achieved in previous pediatric studies in cancer patients (4 to 18 years of age) at similar doses.
In a study of 21 pediatric patients (3 to 12 years of age) who were undergoing surgery requiring anesthesia for a duration of 45 minutes to 2 hours, a single IV dose of ondansetron, 2 mg (3 to 7 years) or 4 mg (8 to 12 years), was administered immediately prior to anesthesia induction. Mean weight-normalized clearance and volume of distribution values in these pediatric surgical patients were similar to those previously reported for young adults. Mean terminal half-life was slightly reduced in pediatric patients (range, 2.5 to 3 hours) in comparison with adults (range, 3 to 3.5 hours).
In a study of 51 pediatric patients (1 month to 24 months of age) who were undergoing surgery requiring general anesthesia, a single IV dose of ondansetron, 0.1 or 0.2 mg/kg, was administered prior to surgery. As shown in Table 3, the 41 patients with pharmacokinetic data were divided into 2 groups, patients 1 month to 4 months of age and patients 5 to 24 months of age, and are compared to pediatric patients 3 to 12 years of age.
Table 3: Pharmacokinetics in Pediatric Surgery Patients 1 Month to 12 Years of Age
|
Subjects and Age Group |
N |
CL (L/h/kg) |
Vdss (L/kg) |
T ½ (h) |
|
|
|
Geometric Mean |
Mean |
|
|
Pediatric Surgery Patients 3 to 12 years of Age |
N=21 |
0.439 |
1.65 |
2.9 |
|
Pediatric Surgery Patients 5 to 24 months of Age |
N=22 |
0.581 |
2.3 |
2.9 |
|
Pediatric Surgery Patients 1 month to 4 months of Age |
N=19 |
0.401 |
3.5 |
6.7 |
In general, surgical and cancer pediatric patients younger than 18 years tend to have a higher ondansetron clearance compared to adults leading to a shorter half-life in most pediatric patients. In patients 1 month to 4 months of age, a longer half-life was observed due to the higher volume of distribution in this age group.
In normal volunteers (19 to 39 years old, n = 23), the peak plasma concentration was 264 ng/mL following a single 32 mg dose administered as a 15-minute IV infusion. The mean elimination half-life was 4.1 hours. Systemic exposure to 32 mg of ondansetron was not proportional to dose as measured by comparing dose-normalized AUC values to an 8 mg dose. This is consistent with a small decrease in systemic clearance with increasing plasma concentrations.
A study was performed in normal volunteers (n = 56) to evaluate the pharmacokinetics of a single 4 mg dose administered as a 5-minute infusion compared to a single intramuscular injection. Systemic exposure as measured by mean AUC was equivalent, with values of 156 [95% CI 136, 180] and 161 [95% CI 137, 190] ng•h/mL for IV and IM groups, respectively. Mean peak plasma concentrations were 42.9 [95% CI 33.8, 54.4] ng/mL at 10 minutes after IV infusion and 31.9 [95% CI 26.3, 38.6] ng/mL at 41 minutes after IM injection. The mean elimination half-life was not affected by route of administration.
Plasma protein binding of ondansetron as measured in vitro was 70% to 76%, with binding constant over the pharmacologic concentration range (10 to 500 ng/mL). Circulating drug also distributes into erythrocytes.
A positive lymphoblast transformation test to ondansetron has been reported, which suggests immunologic sensitivity to ondansetron.
CLINICAL TRIALS
Chemotherapy-Induced Nausea and Vomiting
Adult Studies
In a double-blind study of three different dosing regimens of ondansetron injection, 0.015 mg/kg, 0.15 mg/kg, and 0.3 mg/kg, each given three times during the course of cancer chemotherapy, the 0.15 mg/kg dosing regimen was more effective than the 0.015 mg/kg dosing regimen. The 0.3 mg/kg dosing regimen was not shown to be more effective than the 0.15 mg/kg dosing regimen.
Cisplatin-Based Chemotherapy
In a double-blind study in 28 patients, ondansetron injection (three 0.15 mg/kg doses) was significantly more effective than placebo in preventing nausea and vomiting induced by cisplatin-based chemotherapy. Treatment response was as shown in Table 4.
Table 4: Prevention of Chemotherapy-Induced Nausea and Vomiting in Single-Day Cisplatin Therapya in Adults
|
|
Ondansetron Injection |
Placebo |
P Valueb |
|
Number of patients |
14 |
14 |
|
|
Treatment response 0 Emetic episodes 1 to 2 Emetic episodes 3 to 5 Emetic episodes More than 5 emetic episodes/rescued |
2 (14%) 8 (57%) 2 (14%)
2 (14%) |
0 (0%) 0 (0%) 1 (7%)
13 (93%) |
0.001 |
|
Median number of emetic episodes |
1.5 |
Undefinedc |
|
|
Median time to first emetic episode (h) |
11.6 |
2.8 |
0.001 |
|
Median nausea scores (0 to 100) d |
3 |
59 |
0.034 |
|
Global satisfaction with control of nausea and vomiting (0 to 100)e |
96 |
10.5 |
0.009 |
aChemotherapy was high dose (100 and 120 mg/m2; ondansetron injection n = 6, placebo n = 5) or moderate dose (50 and 80 mg/m2; ondansetron injection n = 8, placebo n = 9). Other chemotherapeutic agents included fluorouracil, doxorubicin, and cyclophosphamide. There was no difference between treatments in the types of chemotherapy that would account for differences in response.
b Efficacy based on “all patients treated” analysis.
c Median undefined since at least 50% of the patients were rescued or had more than five emetic episodes.
d Visual analog scale assessment of nausea: 0 = no nausea, 100 = nausea as bad as it can be.
e Visual analog scale assessment of satisfaction: 0 = not at all satisfied, 100 = totally satisfied.
Ondansetron was compared with metoclopramide in a single-blind trial in 307 patients receiving cisplatin ≥ 100 mg/m2 with or without other chemotherapeutic agents. Patients received the first dose of ondansetron or metoclopramide 30 minutes before cisplatin. Two additional ondansetron doses were administered 4 and 8 hours later, or five additional metoclopramide doses were administered 2, 4, 7, 10, and 13 hours later. Cisplatin was administered over a period of 3 hours or less. Episodes of vomiting and retching were tabulated over the period of 24 hours after cisplatin. The results of this study are summarized in Table 5.
Table 5: Prevention of Vomiting Induced by Cisplatin (≥ 100 mg/m 2 ) Single-Day Therapya in Adults
|
|
Ondansetron Injection |
Metoclopramide |
P Value |
|
Dose |
0.15 mg/kg x 3 |
2 mg/kg x 6 |
|
|
Number of patients in efficacy population |
136 |
138 |
|
|
Treatment response 0 Emetic episodes 1 to 2 Emetic episodes 3 to 5 Emetic episodes More than 5 emetic episodes/rescued |
54 (40%) 34 (25%) 19 (14%)
29 (21%) |
41 (30%) 30 (22%) 18 (13%)
49 (36%) |
|
|
Comparison of treatments with respect to 0 Emetic episodes More than 5 emetic episodes/rescued |
54/136
29/136 |
41/138
49/138 |
0.083
0.009 |
|
Median number of emetic episodes |
1 |
2 |
0.005 |
|
Median time to first emetic episode (h) |
20.5 |
4.3 |
<0.001 |
|
Global satisfaction with control of nausea and vomiting (0 to 100) b |
85 |
63 |
0.001 |
|
Acute dystonic reactions |
0 |
8 |
0.005 |
|
Akathisia |
0 |
10 |
0.002 |
aIn addition to cisplatin, 68% of patients received other chemotherapeutic agents, including cyclophosphamide, etoposide, and fluorouracil. There was no difference between treatments in the types of chemotherapy that would account for differences in response.
b Visual analog scale assessment: 0 = not at all satisfied, 100 = totally satisfied.
In a stratified, randomized, double-blind, parallel-group, multicenter study, a single 32 mg dose of ondansetron was compared with three 0.15 mg/kg doses in patients receiving cisplatin doses of either 50 to 70 mg/m2 or ≥100 mg/m2. Patients received the first ondansetron dose 30 minutes before cisplatin. Two additional ondansetron doses were administered 4 and 8 hours later to the group receiving three 0.15 mg/kg doses. In both strata, significantly fewer patients on the single 32 mg dose than those receiving the three-dose regimen failed.
Table 6: Prevention of Chemotherapy-Induced Nausea and Vomiting in Single-Dose Therapy in Adults
|
|
0.15 mg/kg x 3 |
Ondansetron Dose 32 mg x 1 |
P Value |
|
High-dose cisplatin ( ≥100 mg/m2) |
|
|
|
|
Number of patients |
100 |
102 |
|
|
Treatment response 0 Emetic episodes 1 to 2 Emetic episodes 3 to 5 Emetic episodes More than 5 emetic episodes/rescued |
41 (41%) 19 (19%) 4 (4%)
36 (36%) |
49 (48%) 25 (25%) 8 (8%)
20 (20%) |
0.315
0.009 |
|
Median time to first emetic episode (h) |
21.7 |
23 |
0.173 |
|
Median nausea scores (0 to 100) a |
28 |
13 |
0.004 |
|
Median-dose cisplatin (50 to 70 mg/m2) |
|
|
|
|
Number of patients |
101 |
93 |
|
|
Treatment response 0 Emetic episodes 1 to 2 Emetic episodes 3 to 5 Emetic episodes More than 5 emetic episodes/rescued |
62 (61%) 11 (11%) 6 (6%) 22 (22%) |
68 (73%) 14 (15%) 3 (3%) 8 (9%) |
0.083
0.011 |
|
Median time to first emetic episode (h) |
Undefinedb |
Undefined |
|
|
Median nausea scores (0 to 100)a |
9 |
3 |
0.131 |
a Visual analog scale assessment: 0 = no nausea, 100 = nausea as bad as it can be.
b Median undefined since at least 50% of patients did not have any emetic episodes.
Cyclophosphamide-Based Chemotherapy
In a double-blind, placebo-controlled study of ondansetron injection (three 0.15 mg/kg doses) in 20 patients receiving cyclophosphamide (500 to 600 mg/m2) chemotherapy, ondansetron injection was significantly more effective than placebo in preventing nausea and vomiting. The results are summarized in Table 7.
Table 7: Prevention of Chemotherapy-Induced Nausea and Vomiting in Single-Day Cyclophosphamide Therapya in Adults
|
|
Ondansetron Injection |
Placebo |
P Valueb |
|
Number of patients |
10 |
10 |
|
|
Treatment response 0 Emetic episodes 1 to 2 Emetic episodes 3 to 5 Emetic episodes More than 5 emetic episodes/rescued |
7 (70%) 0 (0%) 2 (20%)
1 (10%) |
0 (0%) 2 (20%) 4 (40%)
4 (40%) |
0.001
0.131 |
|
Median number of emetic episodes |
0 |
4 |
0.008 |
|
Median time to first emetic episode (h) |
Undefinedc |
8.79 |
|
|
Median nausea scores (0 to 100)d |
0 |
60 |
0.001 |
|
Global satisfaction with control of nausea and vomiting (0 to 100)e |
100 |
52 |
0.008 |
a Chemotherapy consisted of cyclophosphamide in all patients, plus other agents, including fluorouracil, doxorubicin, methotrexate, and vincristine. There was no difference between treatments in the type of chemotherapy that would account for differences in response.
b Efficacy based on “all patients treated” analysis.
c Median undefined since at least 50% of patients did not have any emetic episodes.
d Visual analog scale assessment of nausea: 0 = no nausea, 100 = nausea as bad as it can be.
e Visual analog scale assessment of satisfaction: 0 = not at all satisfied, 100 = totally satisfied.
Re-treatment
In uncontrolled trials, 127 patients receiving cisplatin (median dose, 100 mg/m2) and ondansetron who had two or fewer emetic episodes were re-treated with ondansetron and chemotherapy, mainly cisplatin, for a total of 269 re-treatment courses (median, 2; range, 1 to 10). No emetic episodes occurred in 160 (59%), and two or fewer emetic episodes occurred in 217 (81%) re-treatment courses.
Pediatric Studies
Four open-label, noncomparative (one US, three foreign) trials have been performed with 209 pediatric cancer patients 4 to 18 years of age given a variety of cisplatin or noncisplatin regimens. In the three foreign trials, the initial ondansetron injection dose ranged from 0.04 to 0.87 mg/kg for a total dose of 2.16 to 12 mg. This was followed by the oral administration of ondansetron ranging from 4 to 24 mg daily for 3 days. In the US trial, ondansetron injection was administered intravenously (only) in three doses of 0.15 mg/kg each for a total daily dose of 7.2 to 39 mg. In these studies, 58% of the 196 evaluable patients had a complete response (no emetic episodes) on day 1. Thus, prevention of vomiting in these pediatric patients was essentially the same as for patients older than 18 years of age.
An open-label, multicenter, noncomparative trial has been performed in 75 pediatric cancer patients 6 to 48 months of age receiving at least one moderately or highly emetogenic chemotherapeutic agent. Fifty-seven percent (57%) were females; 67% were white, 18% were American Hispanic, and 15% were black patients. Ondansetron was administered intravenously over 15 minutes in three doses of 0.15 mg/kg. The first dose was administered 30 minutes before the start of chemotherapy, the second and third doses were administered 4 and 8 hours after the first dose, respectively. Eighteen patients (25%) received routine prophylactic dexamethasone (i.e., not given as rescue). Of the 75 evaluable patients, 56% had a complete response (no emetic episodes) on day 1. Thus, prevention of vomiting in these pediatric patients was comparable to the prevention of vomiting in patients 4 years of age and older.
Postoperative Nausea and Vomiting
Prevention of Postoperative Nausea and Vomiting
Adult Studies
Adult surgical patients who received ondansetron immediately before the induction of general balanced anesthesia (barbiturate: thiopental, methohexital, or thiamylal; opioid: alfentanil or fentanyl; nitrous oxide; neuromuscular blockade: succinylcholine/curare and/or vecuronium or atracurium; and supplemental isoflurane) were evaluated in two double-blind US studies involving 554 patients. Ondansetron injection (4 mg) IV given over 2 to 5 minutes was significantly more effective than placebo. The results of these studies are summarized in Table 8.
Table 8: Prevention of Postoperative Nausea and Vomiting in Adult Patients
|
|
Ondansetron 4 mg IV |
Placebo |
P Value |
|
Study 1 |
|
|
|
|
Emetic episodes: Number of patients Treatment response over 24-h post- operative period 0 Emetic episodes 1 Emetic episode More than 1 emetic episode/rescued |
136
103 (76%) 13 (10%)
20 (15%) |
139
64 (46%) 17 (12%)
58 (42%) |
< 0.001 |
|
Nausea assessments: Number of patients No nausea over 24-h postoperative period
|
134
56 (42%) |
136
39 (29%) |
|
|
Study 2 |
|
|
|
|
Emetic episodes: Number of patients Treatment response over 24-h post- operative period 0 Emetic episodes 1 Emetic episode More than 1 emetic episode/rescued
|
136
85 (63%) 16 (12%)
35 (26%) |
143
63 (44%) 29 (20%)
51 (36%) |
0.002 |
|
Nausea assessments: Number of patients No nausea over 24-h postoperative period |
125
48 (38%) |
133
42 (32%) |
|
The study populations in Table 8 consisted mainly of females undergoing laparoscopic procedures.
In a placebo-controlled study conducted in 468 males undergoing outpatient procedures, a single 4 mg IV ondansetron dose prevented postoperative vomiting over a 24-hour study period in 79% of males receiving drug compared to 63% of males receiving placebo ( P <0.001 ).
Two other placebo-controlled studies were conducted in 2,792 patients undergoing major abdominal or gynecological surgeries to evaluate a single 4 mg or 8 mg IV ondansetron dose for prevention of postoperative nausea and vomiting over a 24-hour study period. At the 4 mg dosage, 59% of patients receiving ondansetron versus 45% receiving placebo in the first study ( P <0.001) and 41% of patients receiving ondansetron versus 30% receiving placebo in the second study ( P =0.001) experienced no emetic episodes. No additional benefit was observed in patients who received IV ondansetron 8 mg compared to patients who received IV ondansetron 4 mg.
Pediatric Studies
Three double-blind, placebo-controlled studies have been performed (one US, two foreign) in 1,049 male and female patients (2 to 12 years of age) undergoing general anesthesia with nitrous oxide. The surgical procedures included tonsillectomy with or without adenoidectomy, strabismus surgery, herniorrhaphy, and orchidopexy. Patients were randomized to either single IV doses of ondansetron (0.1 mg/kg for pediatric patients weighing 40 kg or less, 4 mg for pediatric patients weighing more than 40 kg) or placebo. Study drug was administered over at least 30 seconds, immediately prior to or following anesthesia induction. Ondansetron was significantly more effective than placebo in preventing nausea and vomiting.
The results of these studies are summarized in Table 9.
Table 9: Prevention of Postoperative Nausea and Vomiting in Pediatric Patients 2 to 12 Years of Age
|
Treatment Response Over 24 Hours |
Ondansetron n(%) |
Placebo n(%) |
P Value |
|
Study 1 |
|
|
|
|
Number of patients 0 Emetic episodes Failurea |
205 140 (68%) 65 (32%) |
210 82 (39%) 128 (61%) |
≤ 0.001 |
|
Study 2 |
|
|
|
|
Number of patients 0 Emetic episodes Failurea |
112 68 (61%) 44 (39%) |
110 38 (35%) 72 (65%) |
≤ 0.001 |
|
Study 3 |
|
|
|
|
Number of patients 0 Emetic episodes Failurea Nausea assessmentsb: Number of patients None |
206 123 (60%) 83 (40%)
185 119 (64%)
|
206 96 (47%) 110 (53%)
191 99 (52%)
|
≤ 0.01
≤ 0.01 |
a Failure was one or more emetic episodes, rescued, or withdrawn.
b Nausea measured as none, mild, or severe.
A double-blind, multicenter, placebo-controlled study was conducted in 670 pediatric patients 1 month to 24 months of age who were undergoing routine surgery under general anesthesia. Seventy-five percent (75%) were males; 64% were white, 15% were black, 13% were American Hispanic, 2% were Asian, and 6% were “other race” patients. A single 0.1 mg/kg IV dose of ondansetron administered within 5 minutes following induction of anesthesia was statistically significantly more effective than placebo in preventing vomiting. In the placebo group, 28% of patients experienced vomiting compared to 11% of subjects who received ondansetron ( P ≤ 0.01). Overall, 32 (10%) of placebo patients and 18 (5%) of patients who received ondansetron received antiemetic rescue medication(s) or prematurely withdrew from the study.
Prevention of Further Postoperative Nausea and Vomiting
Adult Studies
Adult surgical patients receiving general balanced anesthesia (barbiturate: thiopental, methohexital, or thiamylal; opioid: alfentanil or fentanyl; nitrous oxide; neuromuscular blockade: succinylcholine/curare and/or vecuronium or atracurium; and supplemental isoflurane) who received no prophylactic antiemetics and who experienced nausea and/or vomiting within 2 hours postoperatively were evaluated in two double-blind US studies involving 441 patients. Patients who experienced an episode of postoperative nausea and/or vomiting were given ondansetron injection (4 mg) IV over 2 to 5 minutes, and this was significantly more effective than placebo.
The results of these studies are summarized in Table 10.
Table 10: Prevention of Further Postoperative Nausea and Vomiting in Adult Patients
|
|
Ondansetron 4 mg IV |
Placebo |
P Value |
|
Study 1 |
|
|
|
|
Emetic episodes: Number of patients Treatment response 24-h after study drug 0 Emetic episodes 1 Emetic episode More than 1 emetic episode/rescued Median time to first emetic episode (min)a |
104
49 (47%) 12 (12%)
43 (41%)
55 |
117
19 (16%) 9 (8%)
89 (76%)
43 |
< 0.001 |
|
Nausea assessments: Number of patients Mean nausea score over 24-h postoperative periodb |
98
1.7 |
102
3.1 |
|
|
Study 2 |
|
|
|
|
Emetic episodes: Number of patients Treatment response 24-h after study drug 0 Emetic episodes 1 Emetic episode More than 1 emetic episode/rescued Median time to first emetic episode (min)a |
112
49 (44%) 14 (13%)
49 (44%)
60.5 |
108
28 (26%) 3 (3%)
77 (71%)
34 |
0.006 |
|
Nausea assessments: Number of patients Mean nausea score over 24-h post- operative periodb
|
105
1.9 |
85
2.9 |
|
aAfter administration of study drug.
b Nausea measured on a scale of 0 to 10 with 0 = no nausea, 10 = nausea as bad as it can be.
The study populations in Table 10 consisted mainly of women undergoing laparoscopic procedures.
Repeat Dosing in Adults
In patients who do not achieve adequate control of postoperative nausea and vomiting following a single, prophylactic, preinduction, IV dose of ondansetron 4 mg, administration of a second IV dose of ondansetron 4 mg postoperatively does not provide additional control of nausea and vomiting.
Pediatric Study
One double-blind, placebo-controlled, US study was performed in 351 male and female outpatients (2 to 12 years of age) who received general anesthesia with nitrous oxide and no prophylactic antiemetics. Surgical procedures were unrestricted. Patients who experienced two or more emetic episodes within 2 hours following discontinuation of nitrous oxide were randomized to either single IV doses of ondansetron (0.1 mg/kg for pediatric patients weighing 40 kg or less, 4 mg for pediatric patients weighing more than 40 kg) or placebo administered over at least 30 seconds. Ondansetron was significantly more effective than placebo in preventing further episodes of nausea and vomiting. The results of the study are summarized in Table 11.
Table 11: Prevention of Further Postoperative Nausea and Vomiting in Pediatric Patients 2 to 12 Years of Age
|
Treatment Response Over 24 Hours |
Ondansetron n (%) |
Placebo n (%) |
P Value |
|
Number patients 0 Emetic episodes Failurea |
180 96 (53%) 84 (47%) |
171 29 (17%) 142 (83%) |
≤ 0.001 |
aFailure was one or more emetic episodes, rescued, or withdrawn.
ONDANSETRON INDICATIONS AND USAGE
1. Prevention of nausea and vomiting associated with initial and repeat courses of emetogenic cancer chemotherapy, including high-dose cisplatin. Efficacy of the 32 mg single dose beyond 24 hours in these patients has not been established.
2. Prevention of postoperative nausea and/or vomiting. As with other antiemetics, routine prophylaxis is not recommended for patients in whom there is little expectation that nausea and/or vomiting will occur postoperatively. In patients where nausea and/or vomiting must be avoided postoperatively, ondansetron injection is recommended even where the incidence of postoperative nausea and/or vomiting is low. For patients who do not receive prophylactic ondansetron injection and experience nausea and/or vomiting postoperatively, ondansetron injection may be given to prevent further episodes (see CLINICAL TRIALS ).
ONDANSETRON CONTRAINDICATIONS
The concomitant use of apomorphine with ondansetron is contraindicated based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron.
Ondansetron injection is contraindicated for patients known to have hypersensitivity to the drug.
WARNINGS
Hypersensitivity reactions have been reported in patients who have exhibited hypersensitivity to other selective 5-HT3 receptor antagonists.
PRECAUTIONS
General
Ondansetron is not a drug that stimulates gastric or intestinal peristalsis. It should not be used instead of nasogastric suction. The use of ondansetron in patients following abdominal surgery or in patients with chemotherapy-induced nausea and vomiting may mask a progressive ileus and/or gastric distention.
Rarely and predominantly with intravenous ondansetron, transient ECG changes including QT interval prolongation have been reported.
Drug Interactions
Ondansetron does not itself appear to induce or inhibit the cytochrome P-450 drug-metabolizing enzyme system of the liver (see CLINICAL PHARMACOLOGY: Pharmacokinetics ). Because ondansetron is metabolized by hepatic cytochrome P-450 drug-metabolizing enzymes (CYP3A4, CYP2D6, CYP1A2), inducers or inhibitors of these enzymes may change the clearance and, hence, the half-life of ondansetron. On the basis of limited available data, no dosage adjustment is recommended for patients on these drugs.
Apomorphine
Based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron, concomitant use of apomorphine with ondansetron is contraindicated (see CONTRAINDICATIONS ).
Phenytoin, Carbamazepine, and Rifampin
In patients treated with potent inducers of CYP3A4 (i.e., phenytoin, carbamazepine, and rifampin), the clearance of ondansetron was significantly increased and ondansetron blood concentrations were decreased. However, on the basis of available data, no dosage adjustment for ondansetron is recommended for patients on these drugs.1,3
Tramadol
Although no pharmacokinetic drug interaction between ondansetron and tramadol has been observed, data from 2 small studies indicate that ondansetron may be associated with an increase in patient controlled administration of tramadol.4,5
Chemotherapy
Tumor response to chemotherapy in the P 388 mouse leukemia model is not affected by ondansetron. In humans, carmustine, etoposide, and cisplatin do not affect the pharmacokinetics of ondansetron.
In a crossover study in 76 pediatric patients, IV ondansetron did not increase blood levels of high-dose methotrexate.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenic effects were not seen in 2-year studies in rats and mice with oral ondansetron doses up to 10 and 30 mg/kg per day, respectively. Ondansetron was not mutagenic in standard tests for mutagenicity. Oral administration of ondansetron up to 15 mg/kg per day did not affect fertility or general reproductive performance of male and female rats.
Pregnancy
Teratogenic Effects: Pregnancy Category B.
Reproduction studies have been performed in pregnant rats and rabbits at IV doses up to 4 mg/kg per day and have revealed no evidence of impaired fertility or harm to the fetus due to ondansetron. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Ondansetron is excreted in the breast milk of rats. It is not known whether ondansetron is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ondansetron is administered to a nursing woman.
Pediatric Use
Little information is available about the use of ondansetron in pediatric surgical patients younger than 1 month of age (see CLINICAL TRIALS section for studies of ondansetron in prevention of postoperative nausea and vomiting in patients 1 month of age and older). Little information is available about the use of ondansetron in pediatric cancer patients younger than 6 months of age (see CLINICAL TRIALS section for studies of ondansetron in chemotherapy-induced nausea and vomiting in pediatric patients 6 months of age and older) (see DOSAGE AND ADMINISTRATION ).
The clearance of ondansetron in pediatric patients 1 month to 4 months of age is slower and the half-life is ~ 2.5 fold longer than patients who are >4 to 24 months of age. As a precaution, it is recommended that patients less than 4 months of age receiving this drug be closely monitored (see CLINICAL PHARMACOLOGY : Pharmacokinetics ) .
The frequency and type of adverse events reported in pediatric patients receiving ondansetron were similar to those in patients receiving placebo (see ADVERSE EVENTS ).
Geriatric Use
Of the total number of subjects enrolled in cancer chemotherapy-induced and postoperative nausea and vomiting in US- and foreign-controlled clinical trials, 862 were 65 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Dosage adjustment is not needed in patients over the age of 65 (see CLINICAL PHARMACOLOGY ).
ONDANSETRON ADVERSE REACTIONS
Chemotherapy-Induced Nausea and Vomiting
The adverse events in Table 12 have been reported in adults receiving ondansetron at a dosage of three 0.15 mg/kg doses or as a single 32 mg dose in clinical trials. These patients were receiving concomitant chemotherapy, primarily cisplatin, and IV fluids. Most were receiving a diuretic.
Table 12: Principal Adverse Events in Comparative Trials in Adults
|
|
Number of Adult Patients with Event |
|||
|
|
Ondansetron Injection 0.15 mg/kg x 3 n = 419 |
Ondansetron Injection 32 mg x 1 n = 220 |
Metoclopramide n = 156 |
Placebo n = 34 |
|
Diarrhea |
16% |
8% |
44% |
18% |
|
Headache |
17% |
25% |
7% |
15% |
|
Fever |
8% |
7% |
5% |
3% |
|
Akathisia |
0% |
0% |
6% |
0% |
|
Acute dystonic reactionsa |
0% |
0% |
5% |
0% |
a See Neurological.
The following have been reported during controlled clinical trials:
Cardiovascular: Rare cases of angina (chest pain), electrocardiographic alterations, hypotension, and tachycardia have been reported. In many cases, the relationship to ondansetron injection was unclear.
Gastrointestinal: Constipation has been reported in 11% of chemotherapy patients receiving multiday ondansetron.
Hepatic: In comparative trials in cisplatin chemotherapy patients with normal baseline values of aspartate transaminase (AST) and alanine transaminase (ALT), these enzymes have been reported to exceed twice the upper limit of normal in approximately 5% of patients. The increases were transient and did not appear to be related to dose or duration of therapy. On repeat exposure, similar transient elevations in transaminase values occurred in some courses, but symptomatic hepatic disease did not occur.
Integumentary: Rash has occurred in approximately 1% of patients receiving ondansetron.
Neurological: There have been rare reports consistent with, but not diagnostic of, extrapyramidal reactions in patients receiving ondansetron injection, and rare cases of grand mal seizure. The relationship to ondansetron injection was unclear.
Other: Rare cases of hypokalemia have been reported. The relationship to ondansetron injection was unclear.
Postoperative Nausea and Vomiting
The adverse events in Table 13 have been reported in ≥ 2% of adults receiving ondansetron at a dosage of 4 mg IV over 2 to 5 minutes in clinical trials. Rates of these events were not significantly different in the ondansetron and placebo groups. These patients were receiving multiple concomitant perioperative and postoperative medications.
Table 13: Adverse Events in ≥ 2% of Adults Receiving Ondansetron at a Dosage of 4 mg IV over 2 to 5 Minutes in Clinical Trials
|
|
Ondansetron Injection 4 mg IV n = 547 patients |
Placebo n = 547 patients |
|
Headache |
92 (17%) |
77 (14%) |
|
Dizziness |
67 (12%) |
88 (16%) |
|
Musculoskeletal pain |
57 (10%) |
59 (11%) |
|
Drowsiness/sedation |
44 (8%) |
37 (7%) |
|
Shivers |
38 (7%) |
39 (7%) |
|
Malaise/fatigue |
25 (5%) |
30 (5%) |
|
Injection site reaction |
21 (4%) |
18 (3%) |
|
Urinary retention |
17 (3%) |
15 (3%) |
|
Postoperative CO2 –related paina |
12 (2%) |
16 (3%) |
|
Chest pain (unspecified) |
12 (2%) |
15 (3%) |
|
Anxiety/agitation |
11 (2%) |
16 (3%) |
|
Dysuria |
11 (2%) |
9 (2%) |
|
Hypotension |
10 (2%) |
12 (2%) |
|
Fever |
10 (2%) |
6 (1%) |
|
Cold sensation |
9 (2%) |
8 (1%) |
|
Pruritus |
9 (2%) |
3 (< 1%) |
|
Paresthesia |
9 (2%) |
2 (< 1%) |
a Sites of pain included abdomen, stomach, joints, rib cage, shoulder.
Pediatric Use
The adverse events in Table 14 were the most commonly reported adverse events in pediatric patients receiving ondansetron (a single 0.1 mg/kg dose for pediatric patients weighing 40 kg or less, or 4 mg for pediatric patients weighing more than 40 kg) administered intravenously over at least 30 seconds. Rates of these events were not significantly different in the ondansetron and placebo groups. These patients were receiving multiple concomitant perioperative and postoperative medications.
Table 14: Frequency of Adverse Events from Controlled Studies in Pediatric Patients 2 to 12 Years of Age
|
Adverse Event |
Ondansetron n = 755 Patients |
Placebo n = 731 Patients |
|
Wound problem |
80 (11%) |
86 (12%) |
|
Anxiety/agitation |
49 (6%) |
47 (6%) |
|
Headache |
44 (6%) |
43 (6%) |
|
Drowsiness/ sedation |
41 (5%) |
56 (8%) |
|
Pyrexia |
32 (4%) |
41 (6%) |
The adverse events in Table 15 were the most commonly reported adverse events in pediatric patients, 1 month to 24 months of age, receiving a single 0.1 mg/kg IV dose of ondansetron. The incidence and type of adverse events were similar in both the ondansetron and placebo groups. These patients were receiving multiple concomitant perioperative and postoperative medications.
Table 15: Frequency of Adverse Events (Greater Than or Equal to 2% in Either Treatment Group) in Pediatric Patients 1 Month to 24 Months of Age
|
Adverse Event |
Ondansetron n = 336 Patients |
Placebo n = 334 Patients |
|
Pyrexia |
14 (4%) |
14 (4%) |
|
Bronchospasm |
2 (< 1%) |
6 (2%) |
|
Post-procedural pain |
4 (1%) |
6 (2%) |
|
Diarrhea |
6 (2%) |
3 (< 1%) |
Observed During Clinical Practice
In addition to adverse events reported from clinical trials, the following events have been identified during post-approval use of intravenous formulations of ondansetron injection. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. The events have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to ondansetron injection.
Cardiovascular: Arrhythmias (including ventricular and supraventricular tachycardia, premature ventricular contractions, and atrial fibrillation), bradycardia, electrocardiographic alterations (including second-degree heart block, QT interval prolongation, and ST segment depression), palpitations, and syncope.
General: Flushing. Rare cases of hypersensitivity reactions, sometimes severe (e.g., anaphylaxis/anaphylactoid reactions, angioedema, bronchospasm, cardiopulmonary arrest, hypotension, laryngeal edema, laryngospasm, shock, shortness of breath, stridor) have also been reported.
Hepatobiliary: Liver enzyme abnormalities have been reported. Liver failure and death have been reported in patients with cancer receiving concurrent medications including potentially hepatotoxic cytotoxic chemotherapy and antibiotics. The etiology of the liver failure is unclear.
Local Reactions: Pain, redness, and burning at site of injection.
Lower Respiratory: Hiccups
Neurological: Oculogyric crisis, appearing alone, as well as with other dystonic reactions.
Skin: Urticaria
Special Senses: Transient dizziness during or shortly after IV infusion.
Eye Disorders: Transient blurred vision, in some cases associated with abnormalities of accommodation. Cases of transient blindness, predominantly during intravenous administration, have been reported. These cases of transient blindness were reported to resolve within a few minutes up to 48 hours.
DRUG ABUSE AND DEPENDENCE
Animal studies have shown that ondansetron is not discriminated as a benzodiazepine nor does it substitute for benzodiazepines in direct addiction studies.
OVERDOSAGE
There is no specific antidote for ondansetron overdose. Patients should be managed with appropriate supportive therapy. Individual doses as large as 150 mg and total daily dosages (three doses) as large as 252 mg have been administered intravenously without significant adverse events. These doses are more than 10 times the recommended daily dose.
In addition to the adverse events listed above, the following events have been described in the setting of ondansetron overdose: “Sudden blindness” (amaurosis) of 2 to 3 minutes’ duration plus severe constipation occurred in one patient that was administered 72 mg of ondansetron intravenously as a single dose. Hypotension (and faintness) occurred in another patient that took 48 mg of oral ondansetron. Following infusion of 32 mg over only a 4-minute period, a vasovagal episode with transient second-degree heart block was observed. In all instances, the events resolved completely.
ONDANSETRON DOSAGE AND ADMINISTRATION
Prevention of Chemotherapy-Induced Nausea and Vomiting
Adult Dosing:
The recommended IV dosage of Ondansetron Injection for adults is a single 32 mg dose or three 0.15 mg/kg doses. A single 32 mg dose is infused over 15 minutes beginning 30 minutes before the start of emetogenic chemotherapy. The recommended infusion rate should not be exceeded (see OVERDOSAGE ). With the three-dose (0.15 mg/kg) regimen, the first dose is infused over 15 minutes beginning 30 minutes before the start of emetogenic chemotherapy. Subsequent doses (0.15 mg/kg) are administered 4 and 8 hours after the first dose of Ondansetron Injection.
Ondansetron Injection should not be mixed with solutions for which physical and chemical compatibility have not been established. In particular, this applies to alkaline solutions as a precipitate may form.
DILUTE BEFORE USE FOR PREVENTION OF CHEMOTHERAPY–INDUCED NAUSEA AND VOMITING. Ondansetron Injection should be diluted in 50 mL of 5% Dextrose Injection or 0.9% Sodium Chloride Injection before administration.
Pediatric Dosing:
On the basis of the available information (see CLINICAL TRIALS : Pediatric Studies and CLINICAL PHARMACOLOGY: Pharmacokinetics ), the dosage in pediatric cancer patients 6 months to 18 years of age should be three 0.15 mg/kg doses. The first dose is to be administered 30 minutes before the start of moderately to highly emetogenic chemotherapy, subsequent doses (0.15 mg/kg are administered 4 and 8 hours after the first dose of ondansetron injection. The drug should be infused intravenously over 15 minutes. Little information is available about dosage in pediatric cancer patients younger than 6 months of age.
DILUTE BEFORE USE FOR PREVENTION OF CHEMOTHERAPY - INDUCED NAUSEA AND VOMITING. Ondansetron Injection should be diluted in 50 mL of 5% Dextrose Injection or 0.9% Sodium Chloride Injection before administration.
Geriatric Dosing:
The dosage recommendation is the same as for the general population.
Prevention of Postoperative Nausea and Vomiting
Adult Dosing:
The recommended IV dosage of Ondansetron Injection for adults is 4 mg undiluted administered intravenously in not less than 30 seconds, preferably over 2 to 5 minutes, immediately before induction of anesthesia, or postoperatively if the patient experiences nausea and/or vomiting occurring shortly after surgery. Alternatively, 4 mg undiluted may be administered intramuscularly as a single injection for adults. While recommended as a fixed dose for patients weighing more than 40 kg, few patients above 80 kg have been studied. In patients who do not achieve adequate control of postoperative nausea and vomiting following a single, prophylactic, preinduction, IV dose of ondansetron 4 mg, administration of a second IV dose of 4 mg ondansetron postoperatively does not provide additional control of nausea and vomiting.
REQUIRES NO DILUTION FOR ADMINISTRATION FOR POSTOPERATIVE NAUSEA AND VOMITING.
Pediatric Dosing:
The recommended IV dosage of Ondansetron Injection for pediatric surgical patients (1 month to 12 years of age) is a single 0.1 mg/kg dose for patients weighing 40 kg or less, or a single 4 mg dose for patients weighing more than 40 kg. The rate of administration should not be less than 30 seconds, preferably over 2 to 5 minutes immediately prior to or following anesthesia induction, or postoperatively if the patient experiences nausea and/or vomiting occurring shortly after surgery. Prevention of further nausea and vomiting was only studied in patients who had not received prophylactic ondansetron injection.
REQUIRES NO DILUTION FOR ADMINISTRATION FOR POSTOPERATIVE NAUSEA AND VOMITING.
Geriatric Dosing:
The dosage recommendation is the same as for the general population.
Dosage Adjustments for Patients With Impaired Renal Function
The dosage recommendation is the same as for the general population. There is no experience beyond first-day administration of ondansetron.
Dosage Adjustment for Patients With Impaired Hepatic Function
In patients with severe hepatic impairment (Child- Pugh2 score of 10 or greater), a single maximal daily dose of 8 mg to be infused over 15 minutes beginning 30 minutes before the start of the emetogenic chemotherapy is recommended. There is no experience beyond first-day administration of ondansetron.
STABILITY
Ondansetron Injection is stable at room temperature under normal lighting conditions for 48 hours after dilution with the following IV fluids: 0.9% Sodium Chloride Injection, 5% Dextrose Injection, 5% Dextrose and 0.9% Sodium Chloride Injection, 5% Dextrose and 0.45% Sodium Chloride Injection, and 3% Sodium Chloride Injection.
Although Ondansetron Injection is chemically and physically stable when diluted as recommended, sterile precautions should be observed because diluents generally do not contain preservative. After dilution, do not use beyond 24 hours.
Note: Parenteral drug products should be inspected visually for particulate matter and discoloration before administration whenever solution and container permit.
Precaution: Occasionally, ondansetron precipitates at the stopper/vial interface in vials stored upright. Potency and safety are not affected. If a precipitate is observed, resolubilize by shaking the vial vigorously.
HOW SUPPLIED
Ondansetron Injection, USP, available as a single dose ( preservative free ) vial, is supplied as follows:
|
Product No. |
NDC No. |
Strength |
Vial Size |
|
MC370302 |
65293-373-25 |
2 mg/mL |
2 mL |
Packaged in twenty-fives.
Ondansetron Injection, USP, available as a multiple dose ( preserved ) vial, is supplied as follows:
|
Product No. |
NDC No. |
Strength |
Vial Size |
|
MC370420 |
65293-374-01 |
2 mg/mL |
20 mL |
Packaged individually.
Store between 2° to 25°C (36° to 77°F). Protect from light.
Vial stoppers do not contain natural rubber latex.
REFERENCES
1. Britto MR, Hussey EK, Mydlow P, et al. Effect of enzyme inducers on ondansetron (OND) metabolism in humans. Clin Pharmacol Ther. 1997; 61:228.
2. Pugh RNH, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Brit J Surg . 1973;60:646-649.
3. Villikka K, Kivisto KT, Neuvonen PJ. The effect of rifampin on the pharmacokinetics of oral and intravenous ondansetron. Clin Pharmacol Ther. 1999; 65:377-381.
4. De Witte JL, Schoenmaekers B, Sessler DI, et al. Anesth Analg. 2001; 92:1319-1321.
5. Arcioni R, della Rocca M, Romanò R, et al. Anesth Analg. 2002; 94:1553-1557.
451294
Issued: July 2012
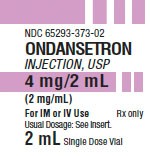
PACKAGE LABEL - PRINCIPAL DISPLAY - Ondansetron 2 mL Single Dose Vial Label
NDC 65293-373-02
ONDANSETRON INJECTION, USP
4 mg/2 mL (2 mg/mL)
For IM or IV Use
Rx only
Usual Dosage: See insert.
2 mL Single Dose Vial
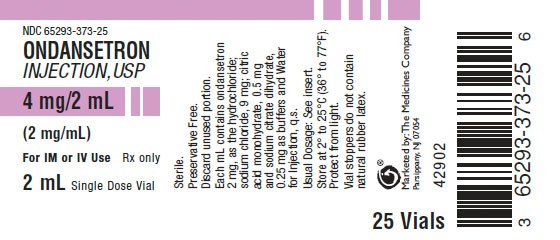
PACKAGE LABEL - PRINCIPAL DISPLAY - Ondansetron 2 mL Single Dose Vial Tray Panel
NDC 65293-373-25
ONDANSETRON INJECTION, USP
4 mg/2 mL (2 mg/mL)
For IM or IV Use
Rx only
2 mL Single Dose Vial
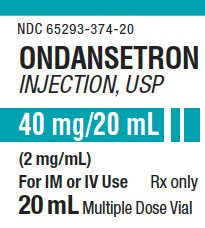
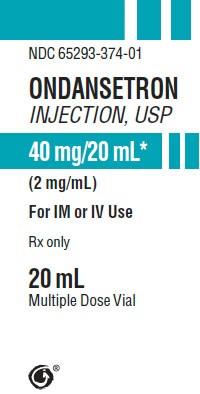
PACKAGE LABEL - PRINCIPAL DISPLAY - Ondansetron 20 mL Multiple Dose Vial Label
NDC 65293-374-20
ONDANSETRON INJECTION, USP
40 mg/20 mL (2 mg/mL)
For IM or IV Use
Rx only
20 mL Multiple Dose Vial
NDC 65293-374-01
ONDANSETRON INJECTION, USP
40 mg/20 mL* (2 mg/mL)
For IM or IV Use
Rx only
20 mL Multiple Dose Vial
OndansetronONDANSETRON HYDROCHLORIDE INJECTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
OndansetronONDANSETRON HYDROCHLORIDE INJECTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||