OPTIMARK
Rx only Mallinckrodt Inc. August 2013
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: NEPHROGENIC SYSTEMIC FIBROSIS
- OPTIMARK DESCRIPTION
- CLINICAL PHARMACOLOGY
- OPTIMARK INDICATIONS AND USAGE
- OPTIMARK CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- OPTIMARK ADVERSE REACTIONS
- POST-MARKETING EXPERIENCE
- OVERDOSAGE
- OPTIMARK DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 30 mL Syringe
FULL PRESCRIBING INFORMATION
OptiMARK™
(gadoversetamide injection)
For Intravenous Injection Only
Mallinckrodt Inc.
WARNING: NEPHROGENIC SYSTEMIC FIBROSIS
Gadolinium-based contrast agents (GBCAs) increase the risk for NSF among patients with impaired elimination of the drugs. Avoid use of GBCAs in these patients unless the diagnostic information is essential and not available with non-contrasted MRI or other modalities. NSF may result in fatal or debilitating fibrosis affecting the skin, muscle and internal organs.
-
Do not administer OptiMARK™ to patients with:
- chronic, severe kidney disease (GFR <30 mL/min/1.73m2), or
- acute kidney injury (see CONTRAINDICATIONS).
- Screen patients for acute kidney injury and other conditions that may reduce renal function. For patients at risk for chronically reduced renal function (e.g. age >60 years, hypertension or diabetes), estimate the glomerular filtration rate (GFR) through laboratory testing.
- Do not exceed the recommended OptiMARK™ dose and allow a sufficient period of time for elimination of the drug from the body prior to any re-administration (see WARNINGS).
OPTIMARK DESCRIPTION
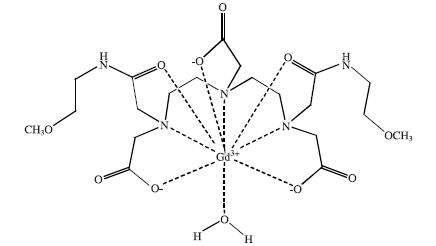
OptiMARK™ (gadoversetamide injection) is a formulation of a nonionic gadolinium chelate of diethylenetriamine pentaacetic acid bismethoxyethylamide (gadoversetamide), for use in magnetic resonance imaging (MRI). OptiMARK™ Injection is to be administered by intravenous injection only.
OptiMARK™ Injection is provided as a sterile, nonpyrogenic, clear, colorless to pale yellow, aqueous solution of gadoversetamide. No preservative is added. Each mL of OptiMARK™ Injection contains 330.9 mg of gadoversetamide (0.5 millimole), 28.4 mg of calcium versetamide sodium (0.05 millimole), 0.7 mg calcium chloride dihydrate (0.005 millimole), and water for injection. Sodium hydroxide and/or hydrochloric acid may have been added for pH adjustment.
OptiMARK™ Injection is designated chemically as [8, 11-bis(carboxymethyl)-14-[2-[(2-methoxyethyl)amino]-2-oxoethyl]-6-oxo-2-oxa-5,8,11,14-tetraazahexadecan-16-oato(3-)] gadolinium with a formula weight of 661.77 g/mol and empirical formula of C20H34N5O10Gd. The structural formula of gadoversetamide in aqueous solution is:
OptiMARK™ Injection has a pH of 5.5 to 7.5 and pertinent physiochemical data are provided below:
| Osmolality (mOsmol/kg water) @ 37°C | 1110 |
| Viscosity (cP) | |
| @ 20°C | 3.1 |
| @ 37°C | 2.0 |
| Density (g/mL) @ 25°C | 1.160 |
OptiMARK™ Injection has an osmolality of approximately 3.9 times that of plasma (285 mOsm/kg water) and is hypertonic under conditions of use.
CLINICAL PHARMACOLOGY
GENERAL
OptiMARK™ Injection contains gadoversetamide, a complex formed between a chelating agent (versetamide) and a paramagnetic ion, gadolinium (III). Gadoversetamide is a paramagnetic agent that develops a magnetic moment when placed in a magnetic field. The relatively large magnetic moment can enhance the relaxation rates of water protons in its vicinity, leading to an increase in signal intensity (brightness) of tissues.
PHARMACOKINETICS
The pharmacokinetics of intravenously administered gadoversetamide in normal subjects conforms to a two-compartment open-model with mean distribution and elimination half-lives (reported as mean ± SD) of about 13.3 ± 6.8 and 103.6 ± 19.5 minutes.
DISTRIBUTION
Gadoversetamide does not undergo protein binding in vitro. In pregnant and lactating rats which received 153Gd-labeled gadoversetamide, radioactivity was detected in the placenta, fetus, and maternal milk (see PRECAUTIONS, PREGNANCY CATEGORY C and NURSING MOTHERS). The volume of distribution at steady state of gadoversetamide in normal subjects is 162 ± 25 mL/kg, roughly equivalent to that of extracellular water (see PRECAUTIONS, PREGNANCY CATEGORY C).
METABOLISM
Biotransformation or decomposition of gadoversetamide was not detected.
ELIMINATION
Gadoversetamide (0.1 mmol/kg) is eliminated primarily in the urine with 95.5 ± 17.4% (mean ± SD) of the administered dose eliminated by 24 hours. Animal data demonstrated that insignificant levels of radioactive [153Gd] MP-1177/10 are eliminated via the feces. In experimentally induced anephria in the rat, hepatobiliary excretion did not significantly compensate for the absence of urinary elimination. The renal and plasma clearance rates of gadoversetamide in normal subjects are essentially identical (69 ± 15.4 and 72 ± 16.3 mL/hr/kg, respectively) indicating that the drug is essentially cleared through the kidneys via glomerular filtration. Within the studied dose range (0.1 to 0.7 mmol/kg), the kinetics of gadoversetamide appear to be linear (see PRECAUTIONS).
SPECIAL POPULATIONS
Renal Insufficiency: A single intravenous dose of 0.1 mmol/kg of OptiMARK™ Injection was administered to 28 (17 men and 11 women) patients with impaired renal function (mean serum creatinine of 2.4 mg/dL). Sixteen patients had concurrent central nervous system or liver pathology. Renal impairment was shown to delay the elimination of gadoversetamide (see Table 2). The mean cumulative urinary excretion of gadoversetamide at 72 hours was approximately 93.5% for renal impaired patients and 95.8% for subjects with normal renal function (see CLINICAL PHARMACOLOGY, ELIMINATION and Hemodialysis ).
Hemodialysis: Gadoversetamide is removed from the body by hemodialysis. Approximately 98% of the administered dose (0.1 mmol/kg) was cleared from the circulation over the three dialysis sessions that occurred 2 hours, 48 hours, and 120 hours after injection. After each of three dialysis sessions, respectively, 70%, 93%, and 98% of the administered dose was cleared from the plasma. The mean dialysis clearance of gadoversetamide was 93.2 ± 17.1 mL/min, or 48% of the creatinine clearance (194 ± 18.6 mL/min), using a high flux PMMA membrane (see CLINICAL PHARMACOLOGY, SPECIAL POPULATIONS and ELIMINATION, PRECAUTIONS).
Hepatic Insufficiency: A single intravenous dose of 0.1 mmol/kg of OptiMARK™ Injection was administered to 4 (2 men and 2 women) patients with impaired hepatic function. Hepatically impaired patients with normal renal function had plasma kinetics similar to normal subjects (see Table 2).
GENDER
Gender differences were not statistically significant within the hepatically impaired or renally impaired subgroups (see Table 2).
| Population | Elimination t 1/2 (hours) | |
| Men (N = 52) | Women (N = 48) | |
| Healthy Volunteers | 1.73 ± 0.31 (N = 8) | 1.73 ± 0.40 (N = 4) |
| Normal Patients | 1.90 ± 0.50 (N = 25) | 1.94 ± 0.57 (N = 31) |
| Renally Impaired | 8.74 ± 5.14 (N = 17) | 6.91 ± 2.46 (N = 11) |
| Hepatically Impaired | 2.09 ± 0.03 (N = 2) | 2.35 ± 1.09 (N = 2) |
AGE
Pharmacokinetic parameters were retrospectively evaluated in 121 patients with a mean age of 46 years (range 18 to 76 years). In these patients, age related effects on pharmacokinetic parameters were not observed.
RACE
Pharmacokinetic differences due to race after intravenous OptiMARK™ Injection were not studied.
DRUG-DRUG INTERACTIONS
Drug interactions have not been studied.
DIETARY EFFECTS
Dietary effects on the pharmacokinetics of OptiMARK™ Injection have not been studied.
PHARMACODYNAMICS
In magnetic resonance imaging (MRI), visualization of normal and pathological brain, spinal and hepatic tissue depends in part on variations in the radiofrequency signal intensity that occurs with: 1) changes in proton density; 2) alterations of the spin-lattice or longitudinal relaxation time (T1); and 3) variation of the spin-spin or transverse relaxation time (T2). When placed in a magnetic field, gadoversetamide decreases T1 and T2 relaxation times in tissues where it accumulates. At the recommended dose, the effect is primarily on T1 relaxation time, and produces an increase in signal intensity (brightness).
OptiMARK™ Injection does not cross the intact blood-brain barrier, and, therefore, does not accumulate in the normal brain or in lesions that may have a normal blood-brain barrier (e.g., cysts, mature post-operative scars, etc.). However, disruption of the blood-brain barrier or abnormal vascularity allows accumulation of OptiMARK™ Injection in the extravascular spaces of lesions such as neoplasms, abscesses, and subacute infarcts. The pharmacokinetic parameters of OptiMARK™ Injection in various lesions are not known.
CLINICAL TRIALS
A total of 790 patients were evaluated in 4 controlled clinical trials (two liver and two central nervous system studies) of OptiMARK™ Injection. Of these 790 patients, 461 received OptiMARK™ Injection. Of the 461 OptiMARK™ patients, there were 252 men and 209 women with a mean age of 49 years (range 12 to 82 years). The racial and ethnic representations were 83% Caucasian, 9% Black, 3% Asian, and 5% other racial or ethnic groups. These trials were designed to evaluate the results of combined non-contrast MRI and OptiMARK™ Injection 0.1 mmol/kg contrast MRIs in comparison to non-contrast MRI alone.
In the two controlled central nervous system (CNS) studies, 395 eligible patients were highly suspect for CNS disorders and had an abnormal entry contrast MRI. After enrollment, patients were randomized to receive repeat MRI evaluations with OptiMARK™ Injection 0.1 mmol/kg or with 0.1 mmol/kg of an approved gadolinium contrast agent. Of these 395 patients, 262 received OptiMARK™ Injection and 133 received the approved gadolinium contrast agent. The studies were not prospectively designed to demonstrate superiority or equivalence of either imaging drug. Approximately 40% and 25% of the patients that were enrolled in Study A and B, respectively, had a history of either surgery, biopsy, and/or radiation, and/or chemotherapy.
Pre-contrast and pre-plus-post-contrast images were independently evaluated by three blinded readers (each reader examined approximately 1/3 of the images). The images were evaluated by the blinded readers for the following endpoints using a scale from 1 to 10: the level of conspicuity of all lesions, the ability to delineate lesion borders from parenchyma/structures, the number of lesions, and the confidence in the number of lesions. As shown in Table 3, the first row of each endpoint group represents the difference in the mean score of the combined pre- and post-contrast MRI from the mean score of the pre-contrast MRI alone. Also, the table shows the number of patients whose paired MRI images were better, worse or the same as the pre-contrast MRI. Results from the contrast image alone were not evaluated. In Table 3 for these endpoints, when read in combination with the non-contrast images, OptiMARK™ Injection provided a statistically significant improvement over baseline. In addition to these measures, the images were evaluated for the blinded reader's confidence in the diagnosis. Although improvement over baseline was noted, the diagnosis was not rigorously confirmed.
| Endpoints | Study A | Study B |
| OptiMARK™
N = 132  |
OptiMARK™ N = 129 | |
| Conspicuity: | ||
Difference of Means |
0.39 |
0.66 |
| Worse | 24 (18%) | 24 (19%) |
| Same | 69 (52%) | 52 (40%) |
| Better | 39 (30%) | 53 (41%) |
| Border Delineation: | ||
| Difference of Means | 0.70 |
0.86 |
| Worse | 23 (17%) | 25 (19%) |
| Same | 55 (42%) | 51 (40%) |
| Better | 54 (41%) | 53 (41%) |
| Number of Lesions: | ||
| Difference of Means | ||
| Pre | 1.8 | 3.0 |
| Pair |
2.0 |
3.3 |
| Worse | 9 (7%) | 16 (12%) |
| Same | 101 (77%) | 86 (67%) |
| Better | 22 (16%) | 27 (21%) |
| Confidence in Number of Lesions: | ||
| Difference of Means | 0.11 |
0.56 |
| Worse | 19 (14%) | 18 (14%) |
| Same | 86 (65%) | 60 (47%) |
| Better | 27 (20%) | 51 (40%) |
In the two controlled liver studies of 395 patients, all eligible patients had a contrast CT that was considered highly suspect for a liver abnormality(ies). Of these 395 patients, 199 received OptiMARK™ Injection 0.1 mmol/kg. Patients had both pre-contrast and post-contrast MRI scans covering the entire liver. In each study, the images were read by 3 blinded readers (each reader examined approximately 1/3 of the images). Using a scale of 1 to 10, the images were evaluated by the blinded readers for the level of conspicuity of all lesions, the ability to delineate lesion borders from parenchyma/structures, the number of lesions and confidence in the number of lesions. The results are shown in Table 4.
The first row of each endpoint group represents the difference in the mean score of the combined pre- and post-contrast MRI from the mean score of the pre-contrast MRI alone. Also, the table shows the number of patients whose paired MRI images were better, worse or the same as the pre-contrast MRI. Results from the contrast image alone were not evaluated. As shown in Table 4 for these endpoints, when read in combination with the non-contrast image, OptiMARK™ Injection provided a statistically significant improvement over non-contrast images. In addition to these measures, the images were evaluated for the blinded reader's confidence in the diagnosis. Although improvement over baseline was noted, the trial was not designed to rigorously confirm the diagnosis.
| Endpoints | Study C | Study D |
| OptiMARK™
N = 99 |
OptiMARK™
N = 100 |
|
| Conspicuity: Difference of Means  |
0.77 |
0.75 |
| Worse | 21 (21%) | 14 (14%) |
| Same | 37 (37%) | 50 (50%) |
| Better | 41 (41%) | 36 (36%) |
| Border Delineation: Difference of Means |
0.77 |
0.69 |
| Worse | 21 (21%) | 15 (15%) |
| Same | 38 (38%) | 45 (45%) |
| Better | 40 (40%) | 40 (40%) |
| Number of Lesions: |
||
| Difference of Means |
||
| Pre |
2.4 | 3.5 |
| Pair |
3.0 |
3.8 |
| Worse | 13 (13%) | 16 (16%) |
| Same | 50 (51%) | 58 (58%) |
| Better | 36 (36%) | 26 (26%) |
| Confidence in Number of Lesions: | ||
| Difference of Means | 1.6 |
1.0 |
| Worse | 39 (39%) | 38 (38%) |
| Same | 2 (2%) | 8 (8%) |
| Better | 58 (59%) | 54 (54%) |
A subsequent study of 140 normal volunteers evaluated the safety of OptiMARK™ Injection 0.1 mmol/kg delivered by power injector. Imaging results were not studied. The normal volunteers were randomized to receive OptiMARK™ injected manually, or OptiMARK™ or saline injected at 3 different power injector rates. At 2 mL/sec, the adverse event rates were comparable in the OptiMARK™ and saline controls when delivered manually and by power injector. In these small sample sizes, there was a trend towards increasing adverse events with increasing rates of power injection. Patients with abnormal vascularity were not evaluated. The safety and efficacy of power injector rates higher than 2 mL/sec has not been established.
OPTIMARK INDICATIONS AND USAGE
CNS (CENTRAL NERVOUS SYSTEM)
OptiMARK™ Injection is indicated for use with magnetic resonance imaging (MRI) in patients with abnormal blood-brain barrier or abnormal vascularity of the brain, spine and associated tissues.
LIVER
OptiMARK™ Injection is indicated for use with MRI to provide contrast enhancement and facilitate visualization of lesions with abnormal vascularity in the liver in patients who are highly suspect for liver structural abnormalities on computed tomography.
OPTIMARK CONTRAINDICATIONS
OptiMARK™ is contraindicated in patients with:
- chronic, severe kidney disease (glomerular filtration rate, GFR <30 mL/min/1.73m2), or
- acute kidney injury, or
- known allergic or hypersensitivity reactions to gadolinium, versetamide or any of the inert ingredients.
WARNINGS
NEPHROGENIC SYSTEMIC FIBROSIS (NSF)
Gadolinium-based contrast agents (GBCAs) increase the risk for nephrogenic systemic fibrosis (NSF) among patients with impaired elimination of the drugs. Avoid use of GBCAs among these patients unless the diagnostic information is essential and not available with non-contrast enhanced MRI or other modalities. The GBCA-associated NSF risk appears highest for patients with chronic, severe kidney disease (GFR <30 mL/min/1.73m2) as well as patients with acute kidney injury. Do not administer OptiMARK™ to these patients. The risk appears lower for patients with chronic, moderate kidney disease (GFR 30 - 59 mL/min/1.73m2) and little, if any, for patients with chronic, mild kidney disease (GFR 60 - 89 mL/min/1.73m2). NSF may result in fatal or debilitating fibrosis affecting the skin, muscle and internal organs. Report any diagnosis of NSF following OptiMARK™ administration to Mallinckrodt Inc. (1-800-778-7898) or FDA (1-800-FDA-1088 or www.fda.gov/medwatch).
Screen patients for acute kidney injury and other conditions that may reduce renal function. Features of acute kidney injury consist of rapid (over hours to days) and usually reversible decrease in kidney function, commonly in the setting of surgery, severe infection, injury or drug-induced kidney toxicity. Serum creatinine levels and estimated GFR may not reliably assess renal function in the setting of acute kidney injury. For patients at risk for chronic kidney disease (e.g., age >60 years, diabetes mellitus or chronic hypertension), estimate the GFR through laboratory testing.
Among the factors that may increase the risk for NSF are repeated or higher than recommended doses of a GBCA and the degree of renal impairment at the time of exposure. Record the specific GBCA and the dose administered to a patient. When administering Optimark, do not exceed the recommended dose and allow a sufficient period of time for elimination of the drug prior to any re-administration (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
ACUTE KIDNEY INJURY (AKI)
In patients with chronically reduced renal function, acute kidney injury requiring dialysis has occurred with the use of GBCAs. The risk of acute kidney injury may increase with increasing dose of the contrast agent; administer the lowest dose necessary for adequate imaging.
HYPERSENSITIVITY REACTIONS
Severe hypersensitivity reactions including anaphylaxis have been observed with administration of gadolinium products including OptiMARK™. Patients with a history of allergy, drug reactions or other hypersensitivity-like disorders may be at greater risk and should be closely observed during the procedure and for several hours after drug administration. If a reaction occurs, stop OptiMARK™ and immediately begin appropriate therapy including resuscitation. Patients with a history of allergy, drug reactions or other hypersensitivity-like disorders should be closely observed during the procedure and for several hours after drug administration (see PRECAUTIONS, GENERAL ).
Deoxygenated sickle erythrocytes have been shown in vitro studies to align perpendicular to a magnetic field; this may result in vaso-occlusive complications in vivo. The enhancement of magnetic moment by gadoversetamide may potentiate sickle erythrocyte alignment. OptiMARK™ Injection in patients with sickle cell anemia and other hemoglobinopathies has not been studied.
The potential risk of hemolysis after injection of OptiMARK™ Injection in patients with other hemolytic anemias has not been studied. Patients with history of allergy, renal insufficiency or drug reaction should be observed for several hours after drug administration (see PRECAUTIONS).
PRECAUTIONS
GENERAL
Diagnostic procedures that involve the use of contrast agents should be carried out under direction of a physician with the prerequisite training and a thorough knowledge of the procedure to be performed.
Personnel trained in resuscitation techniques and resuscitation equipment should be available.
The possibility of a reaction, including serious, life threatening, fatal, anaphylactoid or cardiovascular reactions or other idiosyncratic reactions should always be considered especially in those patients with a known clinical hypersensitivity, a history of asthma, or other respiratory disorders (see ADVERSE REACTIONS).
Some paramagnetic contrast agents may impair the visualization of existing lesions, which are seen on the unenhanced, non-contrast MRI. This may be due to effects of the paramagnetic contrast agent, imaging parameters, misregistration, etc. CAUTION SHOULD BE EXERCISED WHEN A CONTRAST ENHANCED INTERPRETATION IS MADE IN THE ABSENCE OF A COMPANION UNENHANCED MRI.
Since gadoversetamide is cleared from the body by glomerular filtration, caution should be exercised in patients with impaired renal function (GFR ≥30 and <90 mL/min/1.73m2). Dose adjustments in renal impairment have not been studied. OptiMARK™ Injection has been shown to be removed from the body by hemodialysis (see CLINICAL PHARMACOLOGY, ELIMINATION and SPECIAL POPULATIONS, Renal Insufficiency).
INFORMATION FOR PATIENTS
Patients receiving OptiMARK™ Injection should be instructed before injection to:
- Inform their physician or health care provider if they are pregnant or breast feeding (see PRECAUTIONS, PREGNANCY CATEGORY C and NURSING MOTHERS).
- Inform their physician or health care provider if they have a history of renal and/or liver disease, anemia, hemoglobinopathies, or diseases that affect red blood cells.
- Inform their physician or health care provider if they have a history of asthma or allergic respiratory disorders, seizures, or heart disease.
- Inform their physician or health care provider of all medications they may be taking.
- Inform their physician if they have recently received a GBCA.
GBCAs increase the risk for NSF among patients with impaired elimination of the drugs. To counsel patients at risk for NSF:
- Describe the clinical manifestations of NSF
- Describe procedures to screen for the detection of renal impairment
Instruct the patients to contact their physician if they develop signs or symptoms of NSF following OptiMARK™ administration, such as burning, itching, swelling, scaling, hardening and tightening of the skin; red or dark patches on the skin; stiffness in joints with trouble moving, bending or straightening the arms, hands, legs or feet; pain in the hip bones or ribs; or muscle weakness.
DRUG INTERACTIONS
Drug interactions with other contrast agents and other drugs have not been studied.
LABORATORY TEST INTERACTIONS
Interference by OptiMARK™ Injection in the measurement of serum iron, copper and zinc has been observed. OptiMARK™ Injection causes interference in the measurement of serum calcium using the ortho-cresophthalin complexone (OCP) colorimetric method. In the presence of OptiMARK™ Injection, OCP produces an erroneous, low value for serum calcium. The magnitude of this artifact is proportional to the concentration of OptiMARK™ Injection in the blood, and accurate values can be obtained approximately 90 minutes following injection. In patients with renal insufficiency, clearance of OptiMARK™ Injection is slowed and the interference with calcium determination by OCP is prolonged. Neither the arsenazo III dye system nor the inductively coupled plasma mass spectroscopy methods for calcium assay are affected by OptiMARK™ Injection.
CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
Long-term animal studies have not been performed to evaluate the carcinogenic potential of gadoversetamide. The results of the following genotoxicity assays were negative: Salmonella/E. Coli reverse mutation (Ames) assay, mouse lymphoma mutagenesis assay, and the in vivo mammalian micronucleus assay. The in vitro CHO chromosome aberration assay without metabolic activation was positive.
OptiMARK™ Injection administered to rats in a fertility study was shown to have irreversible reduction and degeneration of spermatocytes in testes and epididymides, and impaired male fertility, following intravenous doses of 2.0 mmol/kg/day (4 times the human dose based on body surface area) for 7 weeks. These effects were not observed at 0.5 mmol/kg/day (1 times the human dose based on a body surface area).
In a separate 28-day repeat dose study in rats, OptiMARK™ Injection was shown to have irreversible reduction of male reproductive organ weights, degeneration of the germinal epithelium of the testes, presence of germ cells in the epididymides, and reduced sperm count following daily intravenous doses of 3.0 mmol/kg/day (6 times the human dose based on body surface area). These effects were not observed at 0.6 mmol/kg/day (1 times the human dose based on surface area). These effects were not observed in similar studies conducted in dogs.
In a single dose study in rats, OptiMARK™ Injection did not produce adverse effects on the male reproductive system 24 hours and 14 days after intravenous administration of 0.5 to 15 mmol/kg (1 to 25 times the human dose based on body surface area).
PREGNANCY CATEGORY C
OptiMARK™ Injection reduced neonatal weights from birth through weaning at maternal doses of 0.5 mmol/kg/day (1 times the human dose based on body surface area) for 5 weeks (including gestation) and paternal doses of 0.5 mmol/kg/day for 12 weeks. This effect was not observed at 0.1 mmol/kg (0.2 times the human dose based on a body surface area). Maternal toxicity was not observed at any dose.
OptiMARK™ Injection caused a reduced mean fetal weight, abnormal liver lobation, delayed ossification of sternebrae, and delayed behavioral development (startle reflex and air rights reflex) in fetuses from female rats dosed with 4.9 mmol/kg/day (10 times the human dose based on body surface area) on days 7 through 17 of gestation. These effects were not observed at 0.7 mmol/kg/day (1 times the human dose based on body surface area). Maternal toxicity was observed at 4.9 mmol/kg/day.
OptiMARK™ Injection caused forelimb flexures and cardiovascular changes in fetuses from female rabbits dosed with 0.4 and 1.6 mmol/kg/day (respectively, 1 and 4 times the human dose based on body surface area) on gestation days 6 through 18. The cardiovascular changes were malformed thoracic arteries, a septal defect, and abnormal ventricle. These effects were not observed at 0.1 mmol/kg/day (0.3 times the human dose based on body surface area). Maternal toxicity was not observed at any dose.
Adequate and well-controlled studies were not conducted in pregnant women. OptiMARK™ Injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
NURSING MOTHERS
153Gd-labeled OptiMARK™ Injection was excreted in the milk of lactating rats receiving a single intravenous dose of 0.1 mmol/kg. Women should discontinue nursing and discard breast milk up to 72 hours after OptiMARK™ Injection administration (see CLINICAL PHARMACOLOGY, DISTRIBUTION).
PEDIATRIC USE
The safety and effectiveness of OptiMARK™ Injection in pediatric patients has not been established. Pediatric patients may be particularly vulnerable to adverse GBCA reactions due to renal immaturity and/or unrecognized renal insufficiency.
OPTIMARK ADVERSE REACTIONS
A total of 1309 subjects (24 healthy volunteers and 1285 patients) received OptiMARK™ Injection and 46 subjects received placebo (saline). Of the 1309 subjects who received OptiMARK™ Injection, 680 (52%) were men and 629 (48%) were women with a mean age of 50 years (range 12 to 85 years). In this population there were 1102 (84%) white, 116 (9%) black, 33 (3%) Asian, and 58 (4%) subjects and patients of other racial groups.
In the clinical trials there were 8 serious adverse events and 1 death. The one death occurred in a patient with advanced multisystem disease and appeared to be related to the underlying disease. Six of the eight serious events appeared to be related to underlying disease. Two patients had either persistent paresthesia or numbness of unknown etiology that required hospitalization for diagnostic evaluations or treatment.
Of the 1309 subjects, 460 (35%) reported at least one adverse event out of a total of 997 adverse events; and 22 (47.8%) of the 46 subjects who received placebo reported at least one adverse event out of a total of 81 adverse events.
The most commonly noted adverse events were headache (9.4%), vasodilatation (6.4%), taste perversion (6.2%), dizziness (3.7%), nausea (3.2%), and paresthesia (2.2%). All adverse events reported in 1% or greater of all patients are listed in Table 5. Of the subjects and patients who experienced adverse events, 95.8% of the adverse events were of mild or moderate intensity after dosing with OptiMARK™ Injection.
| Body System or Event Type | OptiMARK ™ (N = 1309) |
| Number of patients with one or more adverse events |
460 (35.1%) |
| Total Number of Adverse Events | 997 |
| Patients with any injection associated discomfort |
345 (26.4%) |
| Body as a Whole | 193 (14.7%) |
| Headache | 123 (9.4%) |
| Pain Abdomen | 24 (1.8%) |
| Asthenia | 20 (1.5%) |
| Pain Back | 16 (1.2%) |
| Pain | 13 (1.0%) |
| Cardiovascular | 103 (7.9%) |
| Vasodilatation | 84 (6.4%) |
| Digestive | 99 (7.6%) |
| Nausea | 42 (3.2%) |
| Diarrhea | 25 (1.9%) |
| Dyspepsia | 16 (1.2%) |
| Injection Site | 35 (2.7%) |
| Injection Site Reaction | 20 (1.5%) |
| Musculoskeletal | 18 (1.4%) |
| Nervous System | 109 (8.3%) |
| Dizziness | 49 (3.7%) |
| Paresthesia | 29 (2.2%) |
| Respiratory | 46 (3.5%) |
| Rhinitis | 20 (1.5%) |
| Skin and Appendages | 37 (2.8%) |
| Special Senses | 96 (7.3%) |
| Taste Perversion | 81 (6.2%) |
The following adverse reactions occurred in less than 1% of the patients:
Body as a Whole: allergic reaction, edema face, fever, flu-like syndrome, malaise, mucous membrane discharge, neck rigidity, neck pain, pelvic pain, increased sweating
Cardiovascular: arrhythmia, chest pain, hypertension, hypotension, pallor, palpitation, syncope, tachycardia, vasospasm
Digestive: anorexia, increased appetite, constipation, dry mouth, dysphagia, eructation, flatulence, increased salivation, thirst, vomiting
Hemic and Lymphatic: thrombocytopenia
Metabolic and Nutritional: increased creatinine, edema, hypercalcemia, hyperglycemia, hypoglycemia, hyponatremia
Musculoskeletal: arthralgia, leg cramps, myalgia, myasthenia, spasm
Nervous System: agitation, anxiety, confusion, depersonalization, diplopia, dystonia, hallucinations, hypertonia, hypesthesia, nervousness, somnolence, tremor, vertigo
Respiratory System: asthma, cough, dyspnea, epistaxis, hemoptysis, laryngismus, pharyngitis, sinusitis, voice alteration
Skin and Appendages: application site reaction, edema injection site, erythema multiforme, pruritus, rash macular-papular and vesicullous bullous, skin dry, thrombophlebitis, inflammation injection site, urticaria
Special Senses: amblyopia, conjunctivitis, hyperacusis, parosmia, tinnitus
Urogenital: dysuria, oliguria, urine frequency
POST-MARKETING EXPERIENCE
The following adverse reactions have been identified during post-approval use of OptiMARK™. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to OptiMARK™.
Nephrogenic Systemic Fibrosis (NSF) (see WARNINGS ); hypersensitivity reactions including bronchospasm and laryngeal/pharyngeal edema; and seizure.
OVERDOSAGE
Clinical consequences of overdosage with OptiMARK™ Injection have not been reported. Treatment of an overdose is directed toward the support of all vital functions and prompt institution of symptomatic therapy. OptiMARK™ Injection has been shown to be dialyzable (see CLINICAL PHARMACOLOGY).
OPTIMARK DOSAGE AND ADMINISTRATION
OptiMARK™ Injection should be administered as a bolus peripheral intravenous injection at a dose of 0.2 mL/kg (0.1 mmol/kg) and at a rate of 1 to 2 mL/sec delivered by manual or by power injection.
| Body Weight | 0.1 mmol/kg | |
| Kilograms (kg) | Pounds (lb) | Volume (mL) |
| 40 | 88 | 8.0 |
| 50 | 110 | 10.0 |
| 60 | 132 | 12.0 |
| 70 | 154 | 14.0 |
| 80 | 176 | 16.0 |
| 90 | 198 | 18.0 |
| 100 | 220 | 20.0 |
| 110 | 242 | 22.0 |
| 120 | 264 | 24.0 |
| 130 | 286 | 26.0 |
| 140 | 308 | 28.0 |
| 150 | 330 | 30.0 |
IMAGING
The imaging procedure should be completed within 1 hour of the injection of OptiMARK™ Injection. The safety of repeat doses has not been studied. OptiMARK™ MRI images should be interpreted in comparison to unenhanced MRI (see CLINICAL PHARMACOLOGY, PHARMACODYNAMICS and CLINICAL TRIALS).
DRUG HANDLING
Parenteral products should be inspected visually for particulate matter and discoloration prior to administration. Do not use the solution if it is discolored or particulate matter is present.
Concurrent medications or Parenteral Nutrition should not be physically mixed with contrast agents and should not be administered in the same intravenous line because of the potential for chemical incompatibility.
When OptiMARK ™ Injection is to be injected using plastic disposable syringes, the contrast should be drawn into the syringe and used immediately.
This product has not been evaluated for use in magnetic resonance angiography.
OptiMARK™ Injection should be drawn into the syringe and administered using sterile technique. If nondisposable equipment is used, scrupulous care should be taken to prevent residual contamination with traces of cleansing agents. To ensure complete injection of the contrast medium the injection should be followed by a 5 mL normal saline flush. Unused portions of the drug must be discarded.
HOW SUPPLIED
OptiMARK™ Injection is a clear, colorless to slightly yellow solution containing 330.9 mg/mL, 0.5 mmol/mL of gadoversetamide. OptiMARK™ Injection is supplied in 10 mL vials containing 5 mL or 10 mL of solution and is also provided in 20 mL vials containing 15 mL or 20 mL of solution. Each single dose vial is rubber stoppered with an aluminum seal and the contents are sterile. OptiMARK™ Injection is supplied in 10 mL, 15 mL, 20 mL or 30 mL syringes containing 10 mL, 15 mL, 20 mL or 30 mL of solution respectively. Each syringe is sealed with rubber closures and the contents are sterile. Vials and syringes are contained in shipping cartons with the following configurations:
5 mL in glass vials in cartons of 10 vials (NDC Code 0019-1177-02)
10 mL in glass vials in cartons of 10 vials (NDC Code 0019-1177-04)
15 mL in glass vials in cartons of 10 vials (NDC Code 0019-1177-06)
20 mL in glass vials in cartons of 10 vials (NDC Code 0019-1177-08)
10 mL in plastic syringes in cartons of 10 syringes (NDC Code 0019-1177-11)
15 mL in plastic syringes in cartons of 10 syringes (NDC Code 0019-1177-16)
20 mL in plastic syringes in cartons of 10 syringes (NDC Code 0019-1177-21)
30 mL in plastic syringes in cartons of 10 syringes (NDC Code 0019-1177-31)
STORAGE
OptiMARK™ Injection should be stored at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature] and protected from light and freezing. OptiMARK™ Injection may be stored at 37°C for up to one month in a contrast media warmer utilizing circulating warm air. For periods longer than one month, store at 20°C to 25°C (68°F to 77°F).
This product is covered by U.S. Patent No. 5130120, 5137711, 5508388. The use of this product is covered by U.S. Patent No. 5130120 and 5137711.
OptiMARK is a trademark of Mallinckrodt Inc.
Copyright 1998, Mallinckrodt Inc.
All rights reserved
Manufactured and Distributed by:
Mallinckrodt Inc.
St. Louis, MO 63042 U.S.A.
Printed in U.S.A.
tyco
Healthcare
Mallinckrodt
Mallinckrodt Inc.
St. Louis, MO 63042 U.S.A.
www.Mallinckrodt.com
MKR 1177Cb0813
Revised 08/13
Printed in U.S.A.
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 30 mL Syringe
Sterile Solution
30 mL
NDC 0019-1177-31
OptiMARK™ 0.5mmol/mL
(gadoversetamide injection)
For Intravenous Injection Only
Dosage: See Package Insert.
Rx Only
MEDICATION AND FLUID PATHWAY ARE STERILE
OUTSIDE OF SYRINGE IS NOT STERILE
SINGLE DOSE UNIT, DISCARD UNUSED PORTION
PROTECT FROM LIGHT - PROTECT FROM FREEZING
Store at Controlled Room Temperature
20 - 25°C (68 - 77°F) [See USP]
Mallinckrodt Inc.
St. Louis, MO 63042 USA
www.Mallinckrodt.com
tyco
/ Healthcare
MALLINCKRODT
11630414

OPTIMARKgadoversetamide INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||