PENNSAID
HIGHLIGHTS OF PRESCRIBING INFORMATION BOXED WARNING WARNING: CARDIOVASCULAR AND GASTROINTESTINAL RISK See full prescribing information for complete boxed warning. Cardiovascular Risk Nonsteroidal anti-inflammatory drugs (NSAIDs) may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (5.1) PENNSAID is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery. (4) Gastrointestinal Risk NSAIDs, including PENNSAID, cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (5.2) INDICATIONS AND USAGE PENNSAID is a nonsteroidal anti-inflammatory drug (NSAID) indicated for the treatment of the pain of osteoarthritis of the knee(s). (1)DOSAGE AND ADMINISTRATION For the relief of the pain of osteoarthritis of the knee(s): the recommended dose of PENNSAID is 40 mg of diclofenac sodium (2 pump actuations) on each painful knee, 2 times a day. (2) Apply diclofenac sodium topical solution, PENNSAID to clean, dry skin. (2.1) Dispense 40 mg (2 pump actuations) of PENNSAID directly onto the knee or first into the hand and then onto the knee. Spread PENNSAID evenly around front, back and sides of the knee. (2.1) Wash hands completely after administering the product. (2.2) Wait until the area is completely dry before covering with clothing or applying sunscreen, insect repellent, cosmetics, topical medications, or other substances. (2.2) DOSAGE FORMS AND STRENGTHS 2% w/w topical solution (3) CONTRAINDICATIONS Known hypersensitivity to diclofenac sodium. (4) History of asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. (4) Use in the perioperative period of coronary artery bypass graft (CABG) surgery. (4) WARNINGS AND PRECAUTIONS Serious and potentially fatal cardiovascular thrombotic events, myocardial infarction, and stroke can occur with NSAID treatment. Use the lowest effective dose of PENNSAID in patients with known cardiovascular (CV) disease or risk factors for CV disease. (5.1) NSAIDs can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation. Closely monitor patients with a prior history of ulcer disease or gastrointestinal bleeding. (5.2) Elevation of one or more liver tests may occur during therapy with NSAIDs. Discontinue PENNSAID immediately if abnormal liver tests persist or worsen. (5.3) Hypertension can occur with NSAID treatment. Monitor blood pressure closely with PENNSAID treatment. (5.4) Monitor fluid status and cardiac function in patients with fluid retention or heart failure. (5.5) Long-term administration of NSAIDs can result in renal papillary necrosis and other renal injury. Monitor renal function closely in patients at greatest risk of this reaction, including the elderly, those with impaired renal function, heart failure, liver dysfunction, and those taking diuretics and ACE-inhibitors. (5.6) Anaphylactoid reactions may occur in patients with the aspirin triad or in patients without prior exposure to PENNSAID. (5.7) NSAIDs can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. (5.8) Not for use during pregnancy. (5.9) Do not administer to patients with aspirin sensitive asthma and use with caution in patients with preexisting asthma. (5.10) Avoid exposure of treated knee(s) to natural or artificial sunlight. (5.11) Avoid contact of PENNSAID with eyes and mucosa. (5.12) Avoid concurrent use with oral NSAIDs. (5.13) Side EffectsThe most common adverse events with PENNSAID are application site reactions. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Mallinckrodt Brand Pharmaceuticals, Inc. at 1-800-778-7898 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch . DRUG INTERACTIONS Concomitant administration of diclofenac and aspirin is not generally recommended because of the potential of increased adverse effects including increased GI bleeding. (7.1) Concomitant use of anticoagulants and diclofenac have a risk of serious GI bleeding higher than users of either drug alone. (7.2) USE IN SPECIFIC POPULATIONS Pregnancy: Not recommended for use during pregnancy. (8.1) Nursing Mothers: Use with caution, as it is not known if diclofenac is excreted in human milk. (8.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 PENNSAID INDICATIONS AND USAGE
- 2 PENNSAID DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 PENNSAID CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Cardiovascular Thrombotic Events
- 5.2 Gastrointestinal Effects – Risk of GI Ulceration, Bleeding, and Perforation
- 5.3 Hepatic Effects
- 5.4 Hypertension
- 5.5 Congestive Heart Failure and Edema
- 5.6 Renal Effects
- 5.7 Anaphylactoid Reactions
- 5.8 Skin Reactions
- 5.9 Pregnancy
- 5.10 Preexisting Asthma
- 5.11 Sun Exposure
- 5.12 Eye Exposure
- 5.13 Oral Nonsteroidal Anti-Inflammatory Drugs
- 5.14 Corticosteroid Treatment
- 5.15 Inflammation
- 5.16 Hematological Effects
- 5.17 Monitoring
- 6 PENNSAID ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 PENNSAID DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
WARNING: CARDIOVASCULAR AND GASTROINTESTINAL RISK
Cardiovascular Risk
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk [see Warnings and Precautions (5.1)].
- PENNSAID is contraindicated in the perioperative setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4)].
Gastrointestinal Risk
- NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events [see Warnings and Precautions (5.2)].
1 INDICATIONS AND USAGE
PENNSAID is a nonsteroidal anti-inflammatory drug (NSAID) indicated for the treatment of the pain of osteoarthritis of the knee(s).
2 DOSAGE AND ADMINISTRATION
2.1 General Instructions
For relief of the pain of osteoarthritis (OA) of the knee(s), the recommended dose is 40 mg of diclofenac sodium (2 pump actuations) on each painful knee, 2 times a day.
The pump must be primed before first use. Instruct patients to fully depress the pump mechanism (actuation) 4 times while holding the bottle in an upright position. This portion should be discarded to ensure proper priming of the pump. No further priming of the bottle should be required.
After the priming procedure, PENNSAID is properly dispensed by completely depressing the pump 2 times to achieve the prescribed dosage for one knee. Deliver the product directly into the palm of the hand and then apply evenly around front, back, and sides of the knee.
Apply PENNSAID to clean, dry skin.
Application of PENNSAID in an amount exceeding or less than the recommended dose has not been studied and is therefore not recommended.
2.2 Special Precautions
- Avoid showering/bathing for at least 30 minutes after the application of PENNSAID to the treated knee.
- Wash and dry hands after use.
- Do not apply PENNSAID to open wounds.
- Avoid contact of PENNSAID with eyes and mucous membranes.
- Avoid wearing clothing over the PENNSAID-treated knee(s) until the treated knee is dry.
- Protect the treated knee(s) from natural and artificial sunlight.
- PENNSAID was not evaluated under the conditions of heat application, occlusive dressings overlay, or exercise; therefore, concurrent use of PENNSAID under these conditions is not recommended.
- Wait until the treated area is dry before applying sunscreen, insect repellant, lotion, moisturizer, cosmetics, or other topical medication to the same knee you have just treated with PENNSAID.
- Do not use combination therapy with PENNSAID and an oral NSAID unless the benefit outweighs the risk and conduct periodic laboratory evaluations.
3 DOSAGE FORMS AND STRENGTHS
2% w/w topical solution
4 CONTRAINDICATIONS
PENNSAID is contraindicated:
- in patients with a known hypersensitivity to diclofenac sodium or any other component of PENNSAID.
- in patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients [see Warnings and Precautions (5.7, 5.10)].
- in the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)].
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several oral COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction (MI), and stroke, which can be fatal. All NSAIDs, including PENNSAID and COX-2 selective and nonselective orally administered NSAIDs, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Inform patients about the signs and/or symptoms of serious CV events and the steps to take if they occur.
Two large, controlled, clinical trials of an orally administered COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke [see Contraindications (4)].
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and NSAIDs, such as diclofenac, does increase the risk of serious gastrointestinal (GI) events [see Warnings and Precautions (5.2)].
5.2 Gastrointestinal Effects – Risk of GI Ulceration, Bleeding, and Perforation
NSAIDs, including diclofenac, can cause serious GI adverse events including bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3 to 6 months, and in about 2 to 4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
When prescribing PENNSAID, for patients with a prior history of ulcer disease or gastrointestinal bleeding, monitor closely for signs and symptoms of gastrointestinal ulcers and gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients with neither of these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, use special care when treating this population.
To minimize the potential risk for an adverse GI event, use the lowest effective dose for the shortest possible duration. Remain alert for signs and symptoms of GI ulceration and bleeding during diclofenac therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. For high-risk patients, consider alternate therapies that do not involve NSAIDs.
5.3 Hepatic Effects
Borderline elevations (less than 3 times the upper limit of the normal [ULN] range) or greater elevations of transaminases occurred in about 15% of oral diclofenac-treated patients in clinical trials of indications other than acute pain. Of the markers of hepatic function, ALT (SGPT) is recommended for the monitoring of liver injury.
In clinical trials of an oral diclofenac-misoprostol combination product, meaningful elevations (i.e., more than 3 times the ULN) of AST (SGOT) occurred in about 2% of approximately 5,700 patients at some time during diclofenac treatment (ALT was not measured in all studies).
In an open-label, controlled trial of 3,700 patients treated for 2 to 6 months, patients with oral diclofenac were monitored first at 8 weeks and 1,200 patients were monitored again at 24 weeks. Meaningful elevations of ALT and/or AST occurred in about 4% of the 3,700 patients and included marked elevations (>8 times the ULN) in about 1% of the 3,700 patients. In this open-label study, a higher incidence of borderline (less than 3 times the ULN), moderate (3 to 8 times the ULN), and marked (>8 times the ULN) elevations of ALT or AST was observed in patients receiving diclofenac when compared to other NSAIDs. Elevations in transaminases were seen more frequently in patients with osteoarthritis than in those with rheumatoid arthritis. Almost all meaningful elevations in transaminases were detected before patients became symptomatic.
Abnormal tests occurred during the first 2 months of therapy with oral diclofenac in 42 of the 51 patients in all trials who developed marked transaminase elevations. In postmarketing reports, cases of drug-induced hepatotoxicity have been reported in the first month, and in some cases, the first 2 months of NSAID therapy.
Postmarketing surveillance has reported cases of severe hepatic reactions, including liver necrosis, jaundice, fulminant hepatitis with and without jaundice, and liver failure. Some of these reported cases resulted in fatalities or liver transplantation.
In a European retrospective population-based, case-controlled study, 10 cases of oral diclofenac associated drug-induced liver injury with current use compared with non-use of diclofenac were associated with a statistically significant 4-fold adjusted odds ratio of liver injury. In this particular study, based on an overall number of 10 cases of liver injury associated with diclofenac, the adjusted odds ratio increased further with female gender, doses of 150 mg or more, and duration of use for more than 90 days.
Measure transaminases (ALT and AST) periodically in patients receiving long-term therapy with diclofenac, because severe hepatotoxicity may develop without a prodrome of distinguishing symptoms. The optimum times for making the first and subsequent transaminase measurements are not known. Based on clinical trial data and postmarketing experiences, monitor transaminases within 4 to 8 weeks after initiating treatment with diclofenac. However, severe hepatic reactions can occur at any time during treatment with diclofenac. If abnormal liver tests persist or worsen, if clinical signs and/or symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, abdominal pain, diarrhea, dark urine, etc.), discontinue PENNSAID immediately.
To minimize the possibility that hepatic injury will become severe between transaminase measurements, inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms), and the appropriate action to take if these signs and symptoms appear.
To minimize the potential risk for an adverse liver-related event in patients treated with PENNSAID, use the lowest effective dose for the shortest duration possible. When prescribing PENNSAID with concomitant drugs that are known to be potentially hepatotoxic (e.g., acetaminophen, certain antibiotics, antiepileptics), monitor patients for signs of hepatic injury. Instruct patients to avoid taking unprescribed acetaminophen while using PENNSAID.
5.4 Hypertension
NSAIDs, including diclofenac, can lead to new onset or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. When prescribing PENNSAID for patients with hypertension, monitor blood pressure (BP) closely, especially during the initiation of NSAID treatment as well as throughout the course of therapy.
Patients taking ACE-inhibitors, thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs.
5.5 Congestive Heart Failure and Edema
Fluid retention and edema have been observed in some patients treated with NSAIDs, including PENNSAID. When prescribing PENNSAID for patients with fluid retention or heart failure, monitor their fluid status and cardiac function closely.
5.6 Renal Effects
Patients with considerable dehydration are at greater risk for renal injury when exposed to NSAIDs. Monitor renal function closely and consider correcting fluid status prior to initiating treatment with PENNSAID.
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE-inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of PENNSAID in patients with advanced renal disease. Therefore, treatment with PENNSAID is not recommended in patients with advanced renal disease. If PENNSAID therapy is initiated, closely monitor the patient's renal function.
5.7 Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur in patients without prior exposure to PENNSAID. Do not prescribe PENNSAID to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs [see Contraindications (4) and Warnings and Precautions (5.10)]. Seek emergency help in cases where an anaphylactoid reaction occurs.
5.8 Skin Reactions
Do not apply PENNSAID to open skin wounds, infections, inflammations, or exfoliative dermatitis, as it may affect absorption and tolerability of the drug.
NSAIDs, including PENNSAID, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin manifestations, and discontinue use of the drug at the first appearance of skin rash or any other signs of hypersensitivity.
5.9 Pregnancy
PENNSAID should not be used by pregnant or nursing women or those intending to become pregnant.
5.10 Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm, which can be fatal. Since cross-reactivity, including bronchospasm, between aspirin and other nonsteroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, do not administer PENNSAID to patients with this form of aspirin sensitivity and with use in patients with preexisting asthma, monitor closely for signs of worsening symptoms.
5.11 Sun Exposure
Instruct patients to avoid exposure to natural or artificial sunlight on treated knee(s) because studies in animals indicated topical diclofenac treatment resulted in an earlier onset of ultraviolet light-induced skin tumors. The potential effects of PENNSAID on skin response to ultraviolet damage in humans are not known.
5.12 Eye Exposure
Avoid contact of PENNSAID with eyes and mucosa. Advise patients that if eye contact occurs, immediately wash out the eye with water or saline and consult a physician if irritation persists for more than an hour.
5.13 Oral Nonsteroidal Anti-Inflammatory Drugs
Concomitant use of oral NSAIDs with PENNSAID 1.5% resulted in a higher rate of rectal hemorrhage, more frequent abnormal creatinine, urea and hemoglobin. Therefore, do not use combination therapy with PENNSAID and an oral NSAID unless the benefit outweighs the risk and conduct periodic laboratory evaluations.
5.14 Corticosteroid Treatment
PENNSAID cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to exacerbation of corticosteroid-response illness. For patients on prolonged corticosteroid therapy, taper slowly if a decision is made to discontinue corticosteroids.
5.15 Inflammation
The pharmacological activity of PENNSAID in reducing inflammation, and possibly fever, may diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
5.16 Hematological Effects
Anemia is sometimes seen in patients receiving NSAIDs. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Check hemoglobin or hematocrit of patients on PENNSAID if they exhibit any signs or symptoms of anemia or blood loss.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration and reversible. Carefully monitor patients receiving PENNSAID who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants.
The effects of PENNSAID 1.5% on platelet function were studied in 10 healthy subjects administered 80 drops four times a day for 7 days. There was no significant change in platelet aggregation following one week of treatment.
5.17 Monitoring
Because serious GI tract ulcerations and bleeding can occur without warning symptoms in patients taking NSAIDs, monitor patients for signs or symptoms of GI bleeding. Check CBC and a chemistry profile periodically in patients on long-term treatment with NSAIDs. Discontinue PENNSAID if abnormal liver tests or renal tests persist or worsen.
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
PENNSAID
The data described below reflect exposure to PENNSAID of 130 patients treated for 4 weeks (mean duration of 28 days) in one Phase 2 controlled trial. This population’s mean age was approximately 60 years, 85% of patients were Caucasian, 65% were females, and all patients had primary osteoarthritis. The most common adverse events with PENNSAID were application site skin reactions. These events were the most common reason for withdrawing from the study.
Application site reactions:
In this controlled trial, application site reactions were characterized by one or more of the following: dryness (22%), exfoliation (7%), erythema (4%), pruritus (2%), pain (2%), induration (2%), rash (2%), and scabbing (<1%).
Other Common Adverse Reactions:
Table 1 lists all adverse reactions occurring in >1% of patients receiving PENNSAID, where the rate in the PENNSAID group exceeded vehicle, from a controlled study conducted in patients with osteoarthritis.
Table 1: Incidence of Adverse Reactions Occurring in >1% of Subjects with Osteoarthritis Using PENNSAID and More Often than in Subjects with OA Using Vehicle Control (Pooled)
|
Adverse Reaction |
PENNSAID N=130 n (%) |
Vehicle Control N=129 n (%) |
|
Urinary tract infection |
4 (3%) |
1 (<1%) |
|
Application site induration |
2 (2%) |
1 (<1%) |
|
Contusion |
2 (2%) |
1 (<1%) |
|
Sinus congestion |
2 (2%) |
1 (<1%) |
|
Nausea |
2 (2%) |
0 |
PENNSAID 1.5%
The safety of PENNSAID 2% is based in part, on prior experience with PENNSAID 1.5%. The data described below reflect exposure to PENNSAID 1.5% of 911 patients treated between 4 and 12 weeks (mean duration of 49 days) in seven Phase 3 controlled trials, as well as exposure of 793 patients treated in an open-label study, including 463 patients treated for at least 6 months, and 144 patients treated for at least 12 months. The population mean age was approximately 60 years, 89% of patients were Caucasian, 64% were females, and all patients had primary osteoarthritis. The most common adverse events with PENNSAID 1.5% were application site skin reactions. These events were the most common reason for withdrawing from the studies.
Application site reactions:
In controlled trials, application site reactions were characterized by one or more of the following: dryness, erythema, induration, vesicles, paresthesia, pruritus, vasodilation, acne, and urticaria. The most frequent of these reactions were dry skin (32%), contact dermatitis characterized by skin erythema and induration (9%), contact dermatitis with vesicles (2%) and pruritus (4%). In one controlled trial, a higher rate of contact dermatitis with vesicles (4%) was observed after treatment of 152 subjects with the combination of PENNSAID 1.5% and oral diclofenac. In the open label uncontrolled long-term safety study, contact dermatitis occurred in 13% and contact dermatitis with vesicles in 10% of patients, generally within the first 6 months of exposure, leading to a withdrawal rate for an application site event of 14%.
Other Common Adverse Reactions:
In controlled trials, subjects treated with PENNSAID 1.5% experienced some adverse events associated with the NSAID class more frequently than subjects using placebo (constipation, diarrhea, dyspepsia, nausea, flatulence, abdominal pain, edema; see Table 2). The combination of PENNSAID 1.5% and oral diclofenac, compared to oral diclofenac alone, resulted in a higher rate of rectal hemorrhage (3% vs. less than 1%), and more frequent abnormal creatinine (12% vs. 7%), urea (20% vs. 12%), and hemoglobin (13% vs. 9%), but no difference in elevation of liver transaminases.
Table 2 lists all adverse reactions occurring in ≥1% of patients receiving PENNSAID 1.5%, where the rate in the PENNSAID 1.5% group exceeded placebo, from seven controlled studies conducted in patients with osteoarthritis. Since these trials were of different durations, these percentages do not capture cumulative rates of occurrence.
Table 2: Adverse Reactions Occurring in ≥1% of Patients Treated with PENNSAID 1.5% Topical Solution in Placebo and Oral Diclofenac-Controlled Trials
|
Treatment Group: |
PENNSAID 1.5% N=911 |
Topical Placebo N=332 |
|
Adverse Reaction |
N (%) |
N (%) |
|
Dry Skin (Application Site) |
292 (32) |
17 (5) |
|
Contact Dermatitis (Application Site) |
83 (9) |
6 (2) |
|
Dyspepsia |
72 (8) |
13 (4) |
|
Abdominal Pain |
54 (6) |
10 (3) |
|
Flatulence |
35 (4) |
1 (<1) |
|
Pruritus (Application Site) |
34 (4) |
7 (2) |
|
Diarrhea |
33 (4) |
7 (2) |
|
Nausea |
33 (4) |
3 (1) |
|
Pharyngitis |
40 (4) |
13 (4) |
|
Constipation |
29 (3) |
1 (<1) |
|
Edema |
26 (3) |
0 |
|
Rash (Non-Application Site) |
25 (3) |
5 (2) |
|
Infection |
25 (3) |
8 (2) |
|
Ecchymosis |
19 (2) |
1 (<1) |
|
Dry Skin (Non-Application Site) |
19 (2) |
1 (<1) |
|
Contact Dermatitis, vesicles (Application Site) |
18 (2) |
0 |
|
Paresthesia (Non-Application Site) |
14 (2) |
3 (<1) |
|
Accidental Injury |
22 (2) |
7 (2) |
|
Pruritus (Non-Application Site) |
15 (2) |
2 (<1) |
|
Sinusitis |
10 (1) |
2 (<1) |
|
Halitosis |
11 (1) |
1 (<1) |
|
Application Site Reaction (not otherwise specified) |
11 (1) |
3 (<1) |
6.2 Postmarketing Experience
In postmarketing surveillance, the following adverse reactions have been reported during post-approval use of PENNSAID 1.5%. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole: abdominal pain, accidental injury, allergic reactions, asthenia, back pain, body odor, chest pain, edema, face edema, halitosis, headache, neck rigidity, pain
Cardiovascular: palpitation, cardiovascular disorder
Gastrointestinal: diarrhea, dry mouth, dyspepsia, gastroenteritis, decreased appetite, lip swelling, mouth ulceration, nausea, rectal hemorrhage, ulcerative stomatitis, swollen tongue
Metabolic and Nutritional: creatinine increased
Musculoskeletal: leg cramps, myalgia
Nervous: depression, dizziness, drowsiness, lethargy, paresthesia at application site
Respiratory: asthma, dyspnea, laryngismus, laryngitis, pharyngitis, throat swelling
Skin and Appendages: At the Application Site: rash, skin burning sensation; Other Skin and Appendages Adverse Reactions: eczema, skin discoloration, urticaria
Special Senses: abnormal vision, blurred vision, cataract, ear pain, eye disorder, eye pain, taste perversion
Vascular: blood pressure increased, hypertension
7 DRUG INTERACTIONS
Drug interactions with the use of PENNSAID have not been studied. The following drug interactions [Sections 7.1 to 7.7] are noted for oral diclofenac sodium.
7.1 Aspirin
When diclofenac is administered with aspirin, the binding of diclofenac to protein is reduced, although the clearance of free diclofenac is not altered. The clinical significance of this interaction is not known; however, concomitant administration of diclofenac and aspirin is not generally recommended because of the potential of increased adverse effects.
7.2 Anticoagulants
The effects of anticoagulants such as warfarin and NSAIDs on GI bleeding are synergistic, such that users of both drugs together have a risk of serious GI bleeding higher than users of either drug alone.
7.3 ACE-Inhibitors
NSAIDs may diminish the antihypertensive effect of angiotensin converting enzyme (ACE) inhibitors. Consider this interaction in patients taking NSAIDs concomitantly with ACE-inhibitors.
7.4 Diuretics
Clinical studies, as well as postmarketing observations, have shown that NSAIDs can reduce the natriuretic effect of furosemide and thiazides in some patients. The response has been attributed to inhibition of renal prostaglandin synthesis. During concomitant therapy with NSAIDs, observe the patient closely for signs of renal failure [see Warnings and Precautions (5.6)], as well as to assure diuretic efficacy.
7.5 Lithium
NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15% and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by the NSAID. Thus, when NSAIDs, including diclofenac, and lithium are administered concurrently, observe patients carefully for signs of lithium toxicity.
7.6 Methotrexate
NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Monitor renal function when prescribing PENNSAID concomitantly with methotrexate.
7.7 Cyclosporine
Diclofenac, like other NSAIDs, may affect renal prostaglandins and increase the toxicity of certain drugs. Therefore, concomitant therapy with diclofenac may increase cyclosporine’s nephrotoxicity. Monitor renal function when prescribing PENNSAID concomitantly with cyclosporine.
7.8 Oral Nonsteroidal Anti-Inflammatory Drugs
Concomitant use of oral NSAIDs with PENNSAID 1.5% has been evaluated in one Phase 3 controlled trial and in combination with oral diclofenac, compared to oral diclofenac alone, resulted in a higher rate of rectal hemorrhage (3% vs. less than 1%), and more frequent abnormal creatinine (12% vs. 7%), urea (20% vs. 12%) and hemoglobin (13% vs. 9%). Therefore, do not use combination therapy with PENNSAID and an oral NSAID unless the benefit outweighs the risk and conduct periodic laboratory evaluations.
7.9 Topical Treatments
Instruct patients that before applying sunscreen, insect repellant, lotion, moisturizer, cosmetics, or other topical medication to the same skin surface of the knee treated with PENNSAID they must wait until the treated area is completely dry.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C prior to 30 weeks gestation; Category D starting 30 weeks gestation.
Teratogenic Effects:
There are no adequate and well-controlled studies of PENNSAID in pregnant women. PENNSAID should not be used by pregnant women as its safe use has not been adequately determined and starting at 30 weeks gestation, diclofenac and other NSAIDs should be avoided by pregnant women as premature closure of the ductus arteriosus in the fetus may occur. Developmental studies in animals demonstrated that diclofenac sodium administration did not produce teratogenicity despite the induction of maternal toxicity and fetal toxicity in mice at doses up to 20 mg/kg/day (0.6-fold the maximum recommended human dose [MRHD] of 162 mg/day based on body surface area comparison), and in rats and rabbits at doses up to 10 mg/kg/day (approximately 0.6-fold and 1.3-fold the MRHD, respectively). Published reproductive and developmental studies of dimethyl sulfoxide (DMSO, the solvent used in PENNSAID) are equivocal as to potential teratogenicity.
Nonteratogenic Effects:
In rats, maternally toxic doses of diclofenac were associated with dystocia, prolonged gestation, reduced fetal weights and growth, and reduced fetal survival.
8.2 Labor and Delivery
The effects of PENNSAID on labor and delivery in pregnant women are unknown. In rat studies maternal exposure to diclofenac, as with other NSAID drugs, known to inhibit prostaglandin synthesis, increased the incidence of dystocia, delayed parturition, and decreased offspring survival.
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk; however, there is a case report in the literature indicating that diclofenac can be detected at low levels in breast milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from PENNSAID, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Of the 911 patients treated with PENNSAID 1.5% in seven controlled, Phase 3 clinical trials, 444 subjects were 65 years of age and over. There was no age-related difference in the incidence of adverse events. Of the 793 patients treated with PENNSAID 1.5% in one open-labeled safety trial, 334 subjects were 65 years of age and over including 107 subjects 75 and over. There was no difference in the incidence of adverse events with long-term exposure to PENNSAID 1.5% for this elderly population.
When prescribing PENNSAID to elderly patients (65 years and older), monitor renal function since they are more likely to have decreased baseline renal function.
10 OVERDOSAGE
There have been no known experiences of overdose with PENNSAID.
Symptoms following acute NSAID overdose are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Hypertension, acute renal failure, respiratory depression and coma may occur, but are rare. Anaphylactoid reactions have been reported with therapeutic ingestion of NSAIDs, and may occur following an overdose.
Manage patients using symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. Emesis is not recommended due to a possibility of aspiration and subsequent respiratory irritation by DMSO contained in PENNSAID. Activated charcoal (60 to 100 g in adults, 1 to 2 g/kg in children) and/or osmotic cathartic may be indicated in patients seen within 4 hours of ingestion with symptoms or following a large overdose (5 to 10 times the usual dose). Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
For additional information about overdose treatment, call a poison control center (1-800-222-1222).
11 DESCRIPTION
PENNSAID is a clear, colorless to faintly pink or orange solution for topical application.
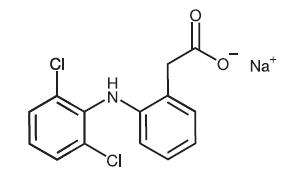
PENNSAID contains 2% w/w diclofenac sodium, a benzeneacetic acid derivative that is a nonsteroidal anti-inflammatory drug, designated chemically as 2-[(2,6-dichlorophenyl)amino]-benzeneacetic acid, monosodium salt. The molecular weight is 318.14. Its molecular formula is C14H10Cl2NNaO2 and it has the following structural formula:
Each 1 gram of solution contains 20 mg of diclofenac sodium. In addition, PENNSAID contains the following inactive ingredients: dimethyl sulfoxide USP (DMSO, 45.5% w/w), ethanol, purified water, propylene glycol, and hydroxypropyl cellulose.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of diclofenac is similar to that of other nonsteroidal anti-inflammatory drugs. Diclofenac inhibits the enzyme, cyclooxygenase (COX), an early component of the arachidonic acid cascade, resulting in the reduced formation of prostaglandins, thromboxanes and prostacylin. It is not completely understood how reduced synthesis of these compounds results in therapeutic efficacy.
12.2 Pharmacodynamics
Diclofenac, the active component of PENNSAID has anti-inflammatory, anti-nociception, and antipyretic effects.
12.3 Pharmacokinetics:
Absorption :
After administration of PENNSAID topical solution (40 mg/knee every 12 h; total daily diclofenac exposure: 80 mg/knee) for 7.5 days, the mean (SD) AUC0-12 and mean (SD) Cmax were 77.27 (49.89) ng•h/mL and 12.16 (7.66) ng/mL, respectively, on Day 1; and 204.58 (111.02) ng•h/mL and 25.24 (12.95) ng/mL, respectively, at steady state on Day 8. After administration of PENNSAID 1.5% topical solution (19.3 mg/knee every 6 h; total daily diclofenac exposure 77.2 mg/knee), the mean (SD) AUC0-12 and mean (SD) Cmax were 27.46 (23.97) ng•h/mL and 2.30 (2.02) ng/mL, respectively, on Day 1; and 141.49 (92.47) ng•h/mL and 17.04 (11.28) ng/mL, respectively, at steady state on Day 8.
The pharmacokinetics and effect of PENNSAID were not evaluated under the conditions of heat application, occlusive dressings overlay, or exercise following product application. Therefore, concurrent use of PENNSAID under these conditions is not recommended.
Distribution:
Diclofenac is more than 99% bound to human serum proteins, primarily to albumin.
Diclofenac diffuses into and out of the synovial fluid. Diffusion into the joint occurs when plasma levels are higher than those in the synovial fluid, after which the process reverses and synovial fluid levels are higher than plasma levels. It is not known whether diffusion into the joint plays a role in the effectiveness of diclofenac.
Metabolism:
Five diclofenac metabolites have been identified in human plasma and urine. The metabolites include 4'‑hydroxy-, 5-hydroxy-, 3'-hydroxy-, 4', 5-dihydroxy- and 3'-hydroxy-4'-methoxy diclofenac. The major diclofenac metabolite, 4'-hydroxy-diclofenac, has very weak pharmacologic activity. The formation of 4'‑hydroxy diclofenac is primarily mediated by CYP2C9. Both diclofenac and its oxidative metabolites undergo glucuronidation or sulfation followed by biliary excretion. Acylglucuronidation mediated by UGT2B7 and oxidation mediated by CYP2C8 may also play a role in diclofenac metabolism. CYP3A4 is responsible for the formation of minor metabolites, 5-hydroxy and 3'-hydroxy-diclofenac.
Excretion:
Diclofenac is eliminated through metabolism and subsequent urinary and biliary excretion of the glucuronide and the sulfate conjugates of the metabolites.
Little or no free unchanged diclofenac is excreted in the urine.
Special Populations:
Pediatric: The pharmacokinetics of PENNSAID has not been investigated in pediatric patients.
Race: Pharmacokinetic differences due to race have not been studied.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies in mice and rats administered diclofenac sodium as a dietary constituent for 2 years resulted in no significant increases in tumor incidence at doses up to 2 mg/kg/day corresponding to approximately 0.85- and 1.7-fold (mouse and rat, respectively) of the maximum recommended human topical dose of PENNSAID (based on apparent bioavailability and body surface area comparison).
In a dermal carcinogenicity study conducted in albino mice, daily topical applications of diclofenac sodium for two years at concentrations up to 0.035% diclofenac sodium (a 57-fold lower diclofenac sodium concentration than present in PENNSAID) did not increase neoplasm incidence.
In a photococarcinogenicity study conducted in hairless mice, topical application of diclofenac sodium at doses up to 0.035% diclofenac sodium (a 57-fold lower diclofenac sodium concentration than present in PENNSAID) resulted in an earlier median time of onset of tumors.
Mutagenesis: Diclofenac was not mutagenic or clastogenic in a battery of genotoxicity tests that included the bacterial reverse mutation assay, in vitro mouse lymphoma point mutation assay, chromosomal aberration studies in Chinese hamster ovarian cells in vitro, and in vivo rat chromosomal aberration assay of bone marrow cells.
Impairment of Fertility: Fertility studies have not been conducted with PENNSAID. Diclofenac sodium administered to male and female rats at doses up to 4 mg/kg/day (3.4-fold of the MRHD of PENNSAID based on apparent bioavailability and body surface area comparison) did not affect fertility. Studies conducted in rats found no effect of dermally applied DMSO on fertility, reproductive performance, or offspring performance.
13.2 Animal Toxicology and/or Pharmacology
Ocular Effects:
No adverse effects were observed using indirect ophthalmoscopy after multiple-daily dermal application to rats for 26 weeks and minipigs for 52 weeks of DMSO at twice the concentration found in PENNSAID. Published studies of dermal or oral administration of DMSO to rabbits, dogs and pigs described refractive changes of lens curvature and cortical fibers indicative of myopic changes and/or incidences of lens opacity or discoloration when evaluated using slit-lamp biomicroscopy examination, although no ocular abnormalities were observed in rhesus monkeys during daily oral or dermal treatment with DMSO for 9 to 18 months.
14 CLINICAL STUDIES
14.1 Study in Osteoarthritis of the Knee
PENNSAID
The use of PENNSAID for the treatment of pain of osteoarthritis of the knee was evaluated in a single double-blind controlled trial conducted in the US, involving patients treated with PENNSAID at a dose of 2 pumps twice a day for 4 weeks. PENNSAID was compared to topical vehicle, applied directly to the study knee. In this trial, patients treated with PENNSAID experienced a greater reduction in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale compared to patients treated with vehicle. Numerical results of the WOMAC pain subscale are summarized in Table 4.
Table 4: Change in Treatment Outcomes after 4 Weeks of Treatment with PENNSAID
|
Efficacy Variable |
Treatment |
|
|
|
PENNSAID |
Vehicle Control |
|
WOMAC Pain Subscale* Baseline Mean Change from Baseline |
12.4 -4.5 |
12.6 -3.6 |
* WOMAC pain subscale is based on the sum of pain scores for five items using a 5-point Likert scale.
16 HOW SUPPLIED/STORAGE AND HANDLING
PENNSAID is supplied as a clear, colorless to faintly pink or orange solution containing 20 mg of diclofenac sodium per gram of solution, in a white polypropylene -dose pump bottle with a clear cap. Each pump actuation delivers 20 mg of diclofenac sodium in 1 gram of solution.
NDC Number & Size
112 g bottle………………………………………….NDC # 23635-510-12
Storage
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide and Instructions for Use)
17.1 Patient/Caregiver Instructions
Inform patients of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. Encourage patients to read the NSAID Medication Guide that accompanies each prescription dispensed prior to using PENNSAID [see Medication Guide]. Also instruct patient/caregiver to read the Patient Instructions for Use.
17.2 Cardiovascular Effects
PENNSAID, like other NSAIDs, may cause serious CV side effects, such as MI or stroke, which may result in hospitalization and even death. Although serious CV events can occur without warning symptoms, instruct patients to be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and to ask for medical advice when observing any indicative sign or symptoms. Inform patients of the importance of this follow-up [see Warnings and Precautions (5.1)].
17.3 Gastrointestinal Effects
PENNSAID, like other NSAIDs, may cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, inform patients to be alert for the signs and symptoms of ulceration and bleeding, and to ask for medical advice when observing any indicative sign or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Instruct patients of the importance of this follow-up [see Warnings and Precautions (5.2)].
17.4 Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, instruct patients to stop therapy with PENNSAID and seek immediate medical therapy [see Warnings and Precautions (5.3)].
17.5 Adverse Skin Reactions
PENNSAID, like other NSAIDs, can cause serious systemic skin side effects such as exfoliative dermatitis, SJS, and TEN, which may result in hospitalizations and even death. Although serious systemic skin reactions may occur without warning, instruct patients to be alert for the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and to ask for medical advice when observing any indicative signs or symptoms [see Warnings and Precautions (5.8)].
Advise patients to stop PENNSAID immediately if they develop any type of generalized rash and contact their physicians as soon as possible.
PENNSAID can cause a localized skin reaction at the application site. Advise patients to contact their physicians as soon as possible if they develop any type of localized application site rash.
Instruct patients not to apply PENNSAID to open skin wounds, infections, inflammations, or exfoliative dermatitis, as it may affect absorption and reduce tolerability of the drug.
Instruct patients to wait until the area treated with PENNSAID is completely dry before applying sunscreen, insect repellant, lotion, moisturizer, cosmetics, or other topical medication.
Instruct patients to minimize or avoid exposure of treated knee(s) to natural or artificial sunlight.
17.6 Weight Gain and Edema
Instruct patients to promptly report to their physician signs or symptoms of unexplained weight gain or edema following treatment with PENNSAID [see Warnings and Precautions (5.5)].
17.7 Anaphylactoid Reactions
Inform patients of the signs of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). If these occur, instruct patients to seek immediate emergency help [see Warnings and Precautions (5.7)].
17.8 Effects During Pregnancy
Instruct patients who are pregnant or intending to become pregnant not to use PENNSAID [see Use in Specific Populations (8.1) and Impairment of Fertility (13.1)].
17.9 Eye Exposure
Instruct patients to avoid contact of PENNSAID with the eyes and mucosa. Advise patients that if eye contact occurs, immediately wash out the eye with water or saline and consult a physician if irritation persists for more than an hour.
Medication Guide For Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
(See the end of this Medication Guide for a list of prescription NSAID medicines.)
What is the most important information I should know about medicines called Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAID medicines may increase the chance of a heart attack or stroke that can lead to dea th.
This chance increases:
- with longer use of NSAID medicines
- in people who have heart disease
NSAID medicines should never be used right before or after a heart surgery called a “coronary artery bypass graft (CABG).”
NSAID medicines can cause ulcers and bleeding in the stomach and intestines at any time during treatment. Ulcers and bleeding:
- can happen without warning symptoms
- may cause death
The chance of a person getting an ulcer or bleeding increases with:
- taking medicines called "corticosteroids" and "anticoagulants"
- longer use
- smoking
- drinking alcohol
- older age
- having poor health
NSAID medicines should only be used:
- exactly as prescribed
- at the lowest dose possible for your treatment
- for the shortest time needed
What are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAID medicines are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as:
- different types of arthritis
- menstrual cramps and other types of short-term pain
Who should not take a Non-Steroidal Anti-Inflammatory Drug (NSAID)?
Do not take an NSAID medicine:
- if you had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAID medicine
- for pain right before or after heart bypass surgery
Tell your healthcare provider:
- about all of your medical conditions.
- about all of the medicines you take. NSAIDs and some other medicines can interact with each other and cause serious side effects. Keep a list of your medicines to show to your healthcare provider and pharmacist.
- if you are pregnant. NSAID medicines should not be used past 30 weeks of pregnancy.
- if you are breastfeeding. Talk to your healthcare provider.
What are the possible side effects of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
|
Serious side effects include:
|
Other side effects include:
|
Get emergency help right away if you have any of the following symptoms:
- shortness of breath or trouble breathing
- chest pain
- slurred speech
- weakness in one part or side of your body
- swelling of the face or throat
Stop your NSAID medicine and call your healthcare provider right away if you have any of the following symptoms:
- nausea
- more tired or weaker than usual
- itching
- your skin or eyes look yellow
- stomach pain
- flu-like symptoms
- vomit blood
- there is blood in your bowel movement or it is black and sticky like tar
- unusual weight gain
- skin rash or blisters with fever
- swelling of the arms and legs, hands and feet
These are not all the side effects with NSAID medicines. Talk to your healthcare provider or pharmacist for more information about NSAID medicines.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Other information about Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
- Aspirin is an NSAID medicine but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some of these NSAID medicines are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
NSAID medicines that need a prescription
|
Generic Name |
Tradename |
|
Celecoxib |
Celebrex® |
|
Diclofenac |
Zorvolex, Zipsor, Flector, Cataflam®, Voltaren®, Voltaren gel, Arthrotec™ (combined with misoprostol), PENNSAID® 1.5%, PENNSAID |
|
Diflunisal |
Dolobid® |
|
Etodolac |
Lodine®, Lodine® XL |
|
Fenoprofen |
Nalfon®, Nalfon® 200 |
|
Flurbirofen |
Ansaid® |
|
Ibuprofen |
Motrin®, Tab-Profen®, Vicoprofen®* (combined with hydrocodone), Combunox™ (combined with oxycodone), Duexis (combined with famotidine) |
|
Indomethacin |
Indocin®, Indocin® SR, Indo-Lemmon™, Indomethagan™ |
|
Ketoprofen |
Oruvail, Nexcede® |
|
Ketorolac |
Toradol, Sprix® |
|
Mefenamic Acid |
Ponstel® |
|
Meloxicam |
Mobic® |
|
Nabumetone |
Relafen® |
|
Naproxen |
Naprosyn®, Anaprox®, Anaprox® DS, EC-Naproxyn®, Naprelan®, Naprapac® (copackaged with lansoprazole), Treximet (combined with sumatriptan succinate) and Vimovo (combined with esomeprazole magnesium) |
|
Oxaprozin |
Daypro® |
|
Piroxicam |
Feldene® |
|
Sulindac |
Clinoril® |
|
Tolmetin |
Tolectin®, Tolectin DS®, Tolectin® 600 |
* Vicoprofen contains the same dose of ibuprofen as over-the-counter (OTC) NSAID, and is usually used for less than 10 days to treat pain. The OTC NSAID label warns that long term continuous use may increase the risk of heart attack or stroke.
This Medication Guide has been approved by the U.S. Food and Drug Administration .
Instructions for Use
PENNSAID® ( pen-sed )
(diclofenac sodium topical solution) 2%
Read the Medication Guide that comes with PENNSAID first. Be sure that you read, understand and follow these Instructions for Use before you use PENNSAID for the first time.
Important: For use on the skin only (topical). Do not get PENNSAID in your eyes, nose or mouth.
Before you use PENNSAID:
- Apply PENNSAID exactly as your healthcare provider tells you. Talk with your healthcare provider or pharmacist if you are not sure.
- Only use PENNSAID to treat pain from osteoarthritis in your knee or knees.
- Apply PENNSAID on clean, dry skin that does not have any cuts, infections or rashes.
- Use PENNSAID two times a day on your knee or knees as prescribed.
- If you get PENNSAID in your eyes, rinse your eyes right away with water or saline. Call your healthcare provider if your eyes are irritated for more than one hour.
Before you use PENNSAID for the first time, you will need to prime the pump. To prime the pump, remove the cap (See Figure A) and fully press the top of the pump all the way down 4 times while holding the bottle in an upright position (See Figure B). Dispense this portion of the medicine into a tissue or paper towel and throw it away in a trash can. The pump is now ready to use. You should not need to prime the pump again.
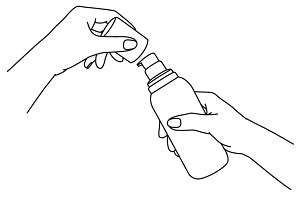
Figure A.
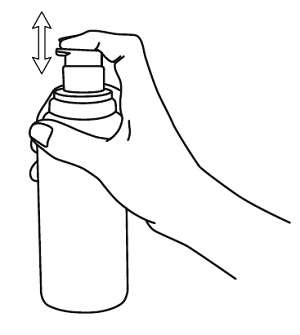
Figure B.
Steps for using PENNSAID:
Step 1. Wash your hands with soap and water before applying PENNSAID.
Step 2. Remove the bottle cap and press the pump head down firmly and fully to dispense PENNSAID into the palm of your hand. Release the pump head and then press the pump head down firmly and fully a second time. When you use your PENNSAID, you can hold the bottle at an angle. Put 2 pumps of PENNSAID on your hand (See Figure C).
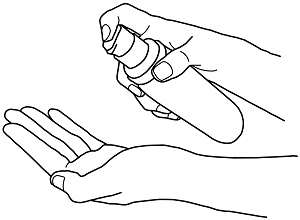
Figure C.
Step 3. Apply PENNSAID evenly around the front, back, and sides of your knee. PENNSAID should be applied without massaging the knee (See Figures D and E).
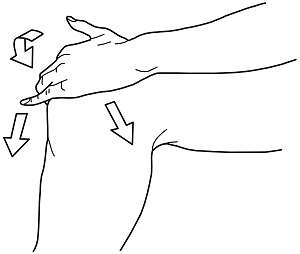
Figure D.
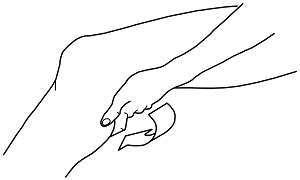
Figure E.
Step 4: Repeat Steps 2 and 3 for your other knee if your healthcare provider has prescribed PENNSAID for both knees.
Step 5: Wash your hands with soap and water right away after applying PENNSAID.
Step 6: Replace the cap on the bottle and store in an upright position.
After you use PENNSAID:
Do not:
- cover your knee with clothing until your knee is completely dry.
- put sunscreen, insect repellant, lotion, moisturizer, cosmetics, or other topical medicines on your knee until it is completely dry.
- take a shower or a bath for at least 30 minutes after you put PENNSAID on your knee(s).
- use heating pads or cover the treated area with bandages where you have applied PENNSAID.
- exercise following application of PENNSAID.
- use sunlamp and tanning beds. Protect your treated knee from sunlight. Wear clothes that cover your skin if you have to be in the sunlight.
How should I store PENNSAID?
- Store PENNSAID at room temperature between 68°F to 77°F (20°C to 25°C).
Keep PENNSAID and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
PENNSAID is a registered trademark of Nuvo Research Inc. Other brands are trademarks of their respective owners.
Distributed by:
Mallinckrodt Brand Pharmaceuticals, Inc.
Hazelwood, MO 63042 USA
Manufactured by:
Nuvo Manufacturing
Varennes, Quebec, J3X 1P7 Canada
E0169-00
Issued 01/2014
Mallinckrodt™ Pharmaceuticals
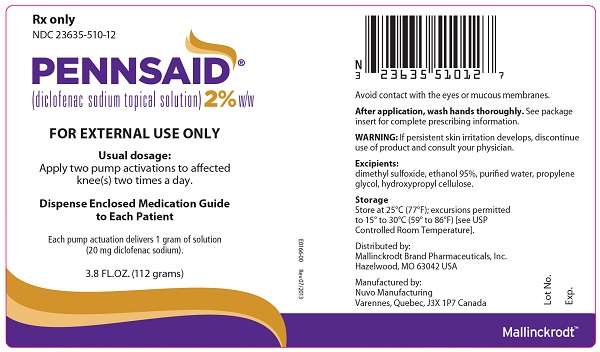
PRINCIPAL DISPLAY PANEL
Rx only
NDC 23635-510-12
PENNSAID®
(diclofenac sodium topical solution)2% w/w
FOR EXTERNAL USE ONLY
Usual dosage:
Apply two pump activations to affected knee(s) two times a day.
Dispense Enclosed Medication Guide To Each Patient
Each pump actuation delivers 1 gram of solution (20 mg diclofenac sodium).
3.8 Fl. OZ. (112 grams)
E0166-00 Rev 07/2013
PENNSAIDdiclofenac sodium topical solution SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||