Phytonadione
Amphastar Pharmaceuticals, Inc.
PHYTONADIONE INJECTABLE EMULSION, USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- PHYTONADIONE DESCRIPTION
- CLINICAL PHARMACOLOGY
- PHYTONADIONE INDICATIONS AND USAGE
- CONTRAINDICATION
- WARNINGS
- PRECAUTIONS
- PHYTONADIONE ADVERSE REACTIONS
- OVERDOSAGE
- PHYTONADIONE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PRINCIPAL DISPLAY PANEL - MIN-I-JET vial injector Carton
FULL PRESCRIBING INFORMATION
Aqueous Colloidal Solution of Vitamin K1
Rx Only
Severe reactions, including fatalities, have occurred during and immediately after the parenteral administration of Phytonadione. Typically these severe reactions have resembled hypersensitivity or anaphylaxis, including shock and cardiac and/or respiratory arrest. Some patients have exhibited these severe reactions on receiving Phytonadione for the first time. The majority of these reported events occurred following intravenous administration, even when precautions have been taken to dilute the Phytonadione and to avoid rapid infusion. Therefore, the INTRAVENOUS route should be restricted to those situations where another route is not feasible and the increased risk involved is considered justified.
PHYTONADIONE DESCRIPTION
Phytonadione is a vitamin, which is a clear, yellow to amber, viscous, odorless or nearly odorless liquid. It is insoluble in water, soluble in chloroform and slightly soluble in ethanol. It has a molecular weight of 450.71.
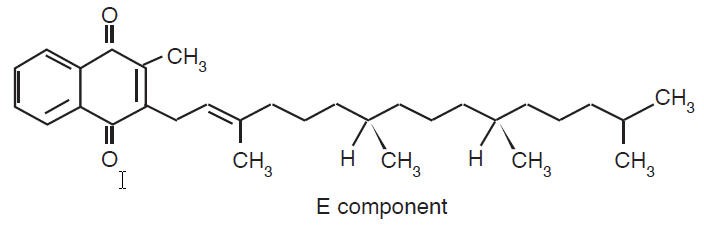
Phytonadione is 2-methyl-3-phytyl-1, 4-naphthoquinone. Its empirical formula is C31H4602; and its structural formula is:
Phytonadione Injectable Emulsion, USP, is a yellow, sterile, aqueous colloidal solution of vitamin K1, with a pH of 3.5 to 7.0. It is available for injection by the intravenous, intramuscular, and subcutaneous route.
Each 0.5 mL contains 1 mg phytonadione (Vitamin K1), 10 mg polysorbate 80, 10.4 mg propylene glycol, 0.17 mg sodium acetate anhydrous, and 0.00002 mL glacial acetic acid. Additional glacial acetic acid or sodium acetate anhydrous may have been added to adjust pH to meet USP limits of 3.5 to 7.0. The air above the liquid in the individual containers has been displaced by flushing with nitrogen during the filling operation.
CLINICAL PHARMACOLOGY
Phytonadione aqueous colloidal solution of vitamin K1 for parenteral injection, possesses the same type and degree of activity as does naturally-occurring vitamin K, which is necessary for the production via the liver of active prothrombin (factor II), proconvertin (factor VII), plasma thromboplastin component (factor IX), and Stuart factor (factor X). The prothrombin test is sensitive to the levels of three of these four factors—II, VII, and X. Vitamin K is an essential cofactor for a microsomal enzyme that catalyzes the posttranslational carboxylation of multiple, specific, peptidebound glutamic acid residues in inactive hepatic precursors of factors II, VII, IX, and X. The resulting gamma-carboxyglutamic acid residues convert the precursors into active coagulation factors that are subsequently secreted by liver cells into the blood.
Phytonadione is readily absorbed following intramuscular administration. After absorption, phytonadione is initially concentrated in the liver, but the concentration declines rapidly. Very little vitamin K accumulates in tissues. Little is known about the metabolic fate of vitamin K. Almost no free unmetabolized vitamin K appears in bile or urine.
In normal animals and humans, phytonadione is virtually devoid of pharmacodynamic activity. However, in animals and humans deficient in vitamin K, the pharmacological action of vitamin K is related to its normal physiological function, that is, to promote the hepatic biosynthesis of vitamin K dependent clotting factors.
The action of the aqueous colloidal solution, when administered intravenously, is generally detectable within an hour or two and hemorrhage is usually controlled within 3 to 6 hours. A normal prothrombin level may often be obtained in 12 to 14 hours.
In the prophylaxis and treatment of hemorrhagic disease of the newborn, phytonadione has demonstrated a greater margin of safety than that of the water-soluble vitamin K analogues.
PHYTONADIONE INDICATIONS AND USAGE
Phytonadione is indicated in the following coagulation disorders which are due to faulty formation of factors II, VII, IX and X when caused by vitamin K deficiency or interference with vitamin K activity.
Phytonadione injection is indicated in:
-
— anticoagulant-induced prothrombin deficiency caused by coumarin or indanedione derivatives; -
— prophylaxis and therapy of hemorrhagic disease of the newborn; -
— hypoprothrombinemia due to antibacterial therapy; -
— hypoprothrombinemia secondary to factors limiting absorption or synthesis of vitamin K, e.g., obstructive jaundice, biliary fistula, sprue, ulcerative colitis, celiac disease, intestinal resection, cystic fibrosis of the pancreas, and regional enteritis; -
— other drug-induced hypoprothrombinemia where it is definitely shown that the result is due to interference with vitamin K metabolism, e.g., salicylates.
CONTRAINDICATION
Hypersensitivity to any component of this medication.
WARNINGS
An immediate coagulant effect should not be expected after administration of phytonadione. It takes a minimum of 1 to 2 hours for measurable improvement in the prothrombin time. Whole blood or component therapy may also be necessary if bleeding is severe.
Phytonadione will not counteract the anticoagulant action of heparin.
When vitamin K1 is used to correct excessive anticoagulant-induced hypoprothrombinemia, anticoagulant therapy still being indicated, the patient is again faced with the clotting hazards existing prior to starting the anticoagulant therapy. Phytonadione is not a clotting agent, but overzealous therapy with vitamin K1 may restore conditions which originally permitted thromboembolic phenomena. Dosage should be kept as low as possible, and prothrombin time should be checked regularly as clinical conditions indicate.
Repeated large doses of vitamin K are not warranted in liver disease if the response to initial use of the vitamin is unsatisfactory. Failure to respond to vitamin K may indicate that the condition being treated is inherently unresponsive to vitamin K.
PRECAUTIONS
Drug Interactions
Temporary resistance to prothrombin-depressing anticoagulants may result, especially when larger doses of phytonadione are used. If relatively large doses have been employed, it may be necessary when reinstituting anticoagulant therapy to use somewhat larger doses of the prothrombin-depressing anticoagulant, or to use one which acts on a different principle, such as heparin sodium.
Laboratory Tests
Prothrombin time should be checked regularly as clinical conditions indicate.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies of carcinogenicity, mutagenesis or impairment of fertility have not been conducted with phytonadione.
Pregnancy
Pregnancy Category C
Animal reproduction studies have not been conducted with phytonadione. It is also not known whether phytonadione can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Phytonadione should be given to a pregnant woman only if clearly needed.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when phytonadione is administered to a nursing woman.
Pediatric Use
Hemolysis, jaundice, and hyperbilirubinemia in newborns, particularly in premature infants, may be related to the dose of phytonadione. Therefore, the recommended dose should not be exceeded (see ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION).
PHYTONADIONE ADVERSE REACTIONS
Severe hypersensitivity reactions, including anaphylactoid reactions and deaths have been reported following parenteral administration. The majority of these reported events occurred following intravenous administration (see Box Warning.)
The possibility of allergic sensitivity, including an anaphylactoid reaction, should be kept in mind following parenteral administration.
Transient "flushing sensations" and "peculiar" sensations of taste have been observed, as well as rare instances of dizziness, rapid and weak pulse, profuse sweating, brief hypotension dyspnea and cyanosis.
Pain, swelling, and tenderness at the injection site may occur.
Infrequently, usually after repeated injection, erythematous, indurated, pruritic plaques have occurred; rarely, these have progressed to scleroderma-like lesions that have persisted for long periods. In other cases, these lesions have resembled erythema perstans.
Hyperbilirubinemia has been observed in the newborn following administration of phytonadione. The has occurred rarely and primarily with doses above those recommended (See Precautions, Pediatric Use.)
OVERDOSAGE
The intravenous LD50 of Phytonadione Injection in the mouse is 41.5 and 52 mL/kg for the 0.2% and 1.0% concentrations, respectively.
PHYTONADIONE DOSAGE AND ADMINISTRATION
Whenever possible, phytonadione should be given by the subcutaneous or intramuscular route. When intravenous administration is considered unavoidable, the drug should be injected very slowly, not exceeding 1 mg per minute.
Protect from light at all times.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Directions for Dilution
Phytonadione may be diluted with 0.9% Sodium Chloride Injection, 5% Dextrose Injection, or 5% Dextrose and Sodium Chloride Injection. Benzyl alcohol as a preservative has been associated with toxicity in newborns. Therefore, all of the above diluents should be preservative-free. Other diluents should not be used. When dilutions are indicated, administration should be started immediately after mixture with the diluent, and unused portions of the dilution should be discarded, as well as unused contents of the vial.
Prophylaxis of Hemorrhagic Disease of the Newborn
The American Academy of Pediatrics recommends that vitamin K1 be given to the newborn. A single intramuscular dose of phytonadione 0.5 to 1 mg within one hour of birth is recommended.
Treatment of Hemorrhagic Disease of the Newborn
Empiric administration of vitamin K1 should not replace proper laboratory evaluation of the coagulation mechanism. A prompt response (shortening of the prothrombin time in 2 to 4 hours) following administration of vitamin K1 is usually diagnostic of hemorrhagic disease of the newborn, and failure to respond indicates another diagnosis or coagulation disorder.
Phytonadione 1 mg should be given either subcutaneously or intramuscularly. Higher doses may be necessary if the mother has been receiving oral anticoagulants.
Whole blood or component therapy may be indicated if bleeding is excessive. This therapy, however, does not correct the underlying disorder and phytonadione should be given concurrently.
Anticoagulant-Induced Prothrombin Deficiency in Adults
To correct excessively prolonged prothrombin time caused by oral anticoagulant therapy — 2.5 to 10 mg or up to 25 mg initially is recommended. In rare instances 50 mg may be required. Frequency and amount of subsequent doses should be determined by prothrombin time response or clinical condition (see WARNINGS). If in 6 to 8 hours after parenteral administration the prothrombin time has not been shortened satisfactorily, the dose should be repeated.
In the event of shock or excessive blood loss, the use of whole blood or component therapy is indicated.
Hypoprothrombinemia Due to Other Causes in Adults
A dosage of 2.5 to 25 mg or more (rarely up to 50 mg) is recommended, the amount and route of administration depending upon the severity of the condition and response obtained.
If possible, discontinuation or reduction of the dosage of drugs interfering with coagulation mechanisms (such as salicylates, antibiotics) is suggested as an alternative to administering concurrent phytonadione. The severity of the coagulation disorder should determine whether the immediate administration of phytonadione is required in addition to discontinuation or reduction of interfering drugs.
| Newborns | Dosage |
|---|---|
| Hemorrhagic Disease of the Newborn | |
| Prophylaxis | 0.5 - 1 mg IM within 1 hour of birth |
| Treatment | 1 mg SC or IM (Higher doses may be necessary if the mother has been receiving oral anti-coagulants) |
| Adults | Initial Dosage |
| Anticoagulant - induced Prothrombin Deficiency (caused by coumarin or indanedione derivatives) |
2.5 mg - 10 mg or up to 25 mg (rarely 50 mg) |
| Hypoprothrombinemia due to other causes (Antibiotics; Salicylates or other drugs; Factors limiting absorption or synthesis) |
2.5 mg - 25 mg or more (rarely up to 50 mg) |
HOW SUPPLIED
In unit use packages containing one single dose vial and a MIN-I-JET® vial injector, 25 G. × 5/8" needle.
Phytonadione Injectable Emulsion, USP, 1 mg in 0.5 mL
-
Packaged in units of 10 single use prefilled syringes.
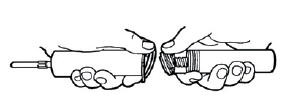
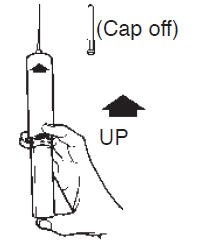
Syringe Assembly Directions:
USE ASEPTIC TECHNIQUE
Do not remove from carton or assemble until ready to use.
| Remove protective vial and injector end caps. | Thread vial into injector 3 half turns; this will allow the needle to penetrate the center of the stopper. |
|
|

|
|
| Align vial such that the injector needle is centered on the stopper. | DO NOT PUSH VIAL INTO INJECTOR; THIS MAY CAUSE MISALIGNMENT OF THE INJECTOR NEEDLE. | Removeneedlecover and expel air before injection. |
Store at controlled room temperature 15° to 30°C (59° to 86°F) [see USP]. Protect from light.
INTERNATIONAL MEDICATION SYSTEMS, LIMITED
SO. EL MONTE, CA 91733, U.S.A.
An Amphastar Pharmaceuticals Company
Rev. 4-05
6911400R
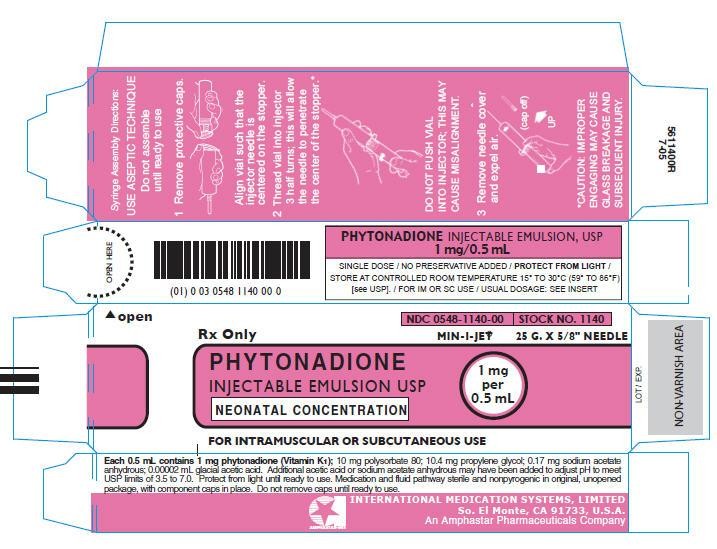
PRINCIPAL DISPLAY PANEL - MIN-I-JET vial injector Carton
NDC 0548-1140-00
STOCK NO. 1140
Rx Only
MIN-I-JET® 25 G. × 5/8" NEEDLE
PHYTONADIONE
INJECTABLE EMULSION USP
NEONATAL CONCENTRATION
1 mg
per
0.5 mL
FOR INTRAMUSCULAR OR SUBCUTANEOUS USE
PhytonadionePhytonadione INJECTION, EMULSION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||