Polocaine
FULL PRESCRIBING INFORMATION: CONTENTS*
- POLOCAINE DESCRIPTION:
- CLINICAL PHARMACOLOGY:
- POLOCAINE INDICATIONS AND USAGE:
- POLOCAINE CONTRAINDICATIONS:
- WARNINGS:
- PRECAUTIONS:
- POLOCAINE ADVERSE REACTIONS:
- OVERDOSAGE:
- POLOCAINE DOSAGE AND ADMINISTRATION:
- HOW SUPPLIED:
FULL PRESCRIBING INFORMATION
451105A/Revised: May 2008
Polocaine ® (Mepivacaine Hydrochloride Injection, USP)
Polocaine ® -MPF (Mepivacaine Hydrochloride Injection, USP)
THESE SOLUTIONS ARE NOT INTENDED FOR SPINAL ANESTHESIA OR DENTAL USE
Rx only
DESCRIPTION:
Mepivacaine hydrochloride is 2-Piperidinecarboxamide, N-(2, 6-dimethylphenyl)-1-methyl-, monohydrochloride and has the following structural formula:
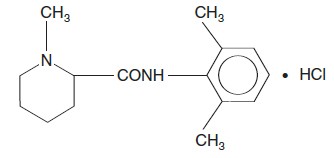
The molecular formula is C15H22N2O • HCl.
It is a white, crystalline odorless, powder, soluble in water, but very resistant to both acid and alkaline hydrolysis.
Mepivacaine hydrochloride is a local anesthetic available as sterile isotonic solutions (clear, colorless) in concentrations of 1%, 1.5% and 2% for injection via local infiltration, peripheral nerve block, and caudal and lumbar epidural blocks.
Mepivacaine hydrochloride is related chemically and pharmacologically to the amide-type local anesthetics. It contains an amide linkage between the aromatic nucleus and the amino group.
|
|
1% Single Dose 30 mL Vial mg/mL
|
1% Multiple Dose 50 mL Vial mg/mL
|
1.5% Single Dose 30 mL Vial mg/mL
|
2% Single Dose 20 mL Vial mg/mL
|
2% Multiple Dose 50 mL Vial mg/mL
|
|
Mepivacaine hydrochloride
|
10
|
10
|
15
|
20
|
20
|
|
Sodium chloride
|
6.6
|
7
|
5.6
|
4.6
|
5
|
|
Potassium chloride
|
0.3
|
|
0.3
|
0.3
|
|
|
Calcium chloride
|
0.33
|
|
0.33
|
0.33
|
|
|
Methylparaben
|
|
1
|
|
|
1
|
|
*In Water for Injection
|
|||||
The pH of the solution is adjusted between 4.5 and 6.8 with sodium hydroxide or hydrochloric acid.
CLINICAL PHARMACOLOGY:
Local anesthetics block the generation and the conduction of nerve impulses, presumably by increasing the threshold for electrical excitation in the nerve, by slowing the propagation of the nerve impulse, and by reducing the rate of rise of the action potential. In general, the progression of anesthesia is related to the diameter, myelination, and conduction velocity of affected nerve fibers. Clinically, the order of loss of nerve function is as follows: pain, temperature, touch, proprioception, and skeletal muscle tone.
Systemic absorption of local anesthetics produces effects on the cardiovascular and central nervous systems. At blood concentrations achieved with normal therapeutic doses, changes in cardiac conduction, excitability, refractoriness, contractility, and peripheral vascular resistance are minimal. However, toxic blood concentrations depress cardiac conduction and excitability, which may lead to atrioventricular block and ultimately to cardiac arrest. In addition, myocardial contractility is depressed and peripheral vasodilation occurs, leading to decreased cardiac output and arterial blood pressure.
Following systemic absorption, local anesthetics can produce central nervous system stimulation, depression, or both. Apparent central stimulation is manifested as restlessness, tremors, and shivering, progressing to convulsions, followed by depression and coma progressing ultimately to respiratory arrest. However, the local anesthetics have a primary depressant effect on the medulla and on higher centers. The depressed stage may occur without a prior excited stage.
A clinical study using 15 mL of 2% epidural mepivacaine at the T 9-10 interspace in 62 patients, 20-79 years of age, demonstrated a 40% decrease in the amount of mepivacaine required to block a given number of dermatomes in the elderly (60-79 years, N=13) as compared to young adults 20-39 years).
Another study using 10 mL of 2% lumbar epidural mepivacaine in 161 patients, 19-75 years of age, demonstrated a strong inverse relationship between patient age and the number of dermatomes blocked per cc of mepivacaine injected.
The rate of systemic absorption of local anesthetics is dependent upon the total dose and concentration of drug administered, the route of administration, the vascularity of the administration site, and the presence or absence of epinephrine in the anesthetic solution. A dilute concentration of epinephrine (1:200,000 or 5mcg/mL) usually reduces the rate of absorption and plasma concentration of mepivacaine, however, it has been reported that vasoconstrictors do not significantly prolong anesthesia with mepivacaine.
Onset of anesthesia with mepivacaine is rapid, the time of onset for sensory block ranging from about 3 to 20 minutes depending upon such factors as the anesthetic technique, the type of block, the concentration of the solution, and the individual patient. The degree of motor blockade produced is dependent on the concentration of the solution. A 0.5% solution will be effective in small superficial nerve blocks while the 1% concentration will block sensory and sympathetic conduction without loss of motor function. The 1.5% solution will provide extensive and often complete motor block and the 2% concentration of mepivacaine hydrochloride will produce complete sensory and motor block of any nerve group.
The duration of anesthesia also varies depending upon the technique and type of block, the concentration, and the individual. Mepivacaine will normally provide anesthesia which is adequate for 2 to 2½ hours of surgery.
Local anesthetics are bound to plasma proteins in varying degrees. Generally, the lower the plasma concentration of drug, the higher the percentage of drug bound to plasma.
Local anesthetics appear to cross the placenta by passive diffusion. The rate and degree of diffusion is governed by the degree of plasma protein binding, the degree of ionization, and the degree of lipid solubility. Fetal/maternal ratios of local anesthetics appear to be inversely related to the degree of plasma protein binding, because only the free, unbound drug is available for placental transfer. Mepivacaine is approximately 75% bound to plasma proteins. The extent of placental transfer is also determined by the degree of ionization and lipid solubility of the drug. Lipid soluble, nonionized drugs readily enter the fetal blood from the maternal circulation.
Depending upon the route of administration, local anesthetics are distributed to some extent to all body tissues, with high concentrations found in highly perfused organs such as the liver, lungs, heart, and brain.
Various pharmacokinetic parameters of the local anesthetics can be significantly altered by the presence of hepatic or renal disease, addition of epinephrine, factors affecting urinary pH, renal blood flow, the route of drug administration, and the age of the patient. The half-life of mepivacaine in adults is 1.9 to 3.2 hours and in neonates 8.7 to 9 hours.
Mepivacaine, because of its amide structure, is not detoxified by the circulating plasma esterases. It is rapidly metabolized, with only a small percentage of the anesthetic (5 percent to 10 percent) being excreted unchanged in the urine. The liver is the principal site of metabolism, with over 50% of the administered dose being excreted into the bile as metabolites. Most of the metabolized mepivacaine is probably resorbed in the intestine and then excreted into the urine since only a small percentage is found in the feces. The principal route of excretion is via the kidney. Most of the anesthetic and its metabolites are eliminated within 30 hours. It has been shown that hydroxylation and N-demethylation, which are detoxification reactions, play important roles in the metabolism of the anesthetic. Three metabolites of mepivacaine have been identified from human adults: two phenols, which are excreted almost exclusively as their glucuronide conjugates, and the N-demethylated compound (2’,6’-pipecoloxylidide).
Mepivacaine does not ordinarily produce irritation or tissue damage, and does not cause methemoglobinemia when administered in recommended doses and concentrations.
INDICATIONS AND USAGE:
POLOCAINE (Mepivacaine HCl Injection, USP), is indicated for production of local or regional analgesia and anesthesia by local infiltration, peripheral nerve block techniques, and central neural techniques including epidural and caudal blocks.
The routes of administration and indicated concentrations for mepivacaine are:
local infiltration 0.5% (via dilution) or 1%
|
peripheral nerve blocks
|
1% and 2%
|
|
epidural block
|
1%, 1.5%, 2%
|
|
caudal block
|
1%, 1.5%, 2%
|
See DOSAGE AND ADMINISTRATION for additional information. Standard textbooks should be consulted to determine the accepted procedures and techniques for the administration of mepivacaine.
CONTRAINDICATIONS:
Mepivacaine is contraindicated in patients with a known hypersensitivity to it or to any local anesthetic agent of the amide-type or to other components of mepivacaine solutions.
WARNINGS:
LOCAL ANESTHETICS SHOULD ONLY BE EMPLOYED BY CLINICIANS WHO ARE WELL VERSED IN DIAGNOSIS AND MANAGEMENT OF DOSE-RELATED TOXICITY AND OTHER ACUTE EMERGENCIES WHICH MIGHT ARISE FROM THE BLOCK TO BE EMPLOYED, AND THEN ONLY AFTER INSURING THE IMMEDIATE AVAILABILITY OF OXYGEN, OTHER RESUSCITATIVE DRUGS, CARDIOPULMONARY RESUSCITATIVE EQUIPMENT, AND THE PERSONNEL RESOURCES NEEDED FOR PROPER MANAGEMENT OF TOXIC REACTIONS AND RELATED EMERGENCIES. (See also ADVERSE REACTIONS and PRECAUTIONS .) DELAY IN PROPER MANAGEMENT OF DOSE-RELATED TOXICITY, UNDERVENTILATION FROM ANY CAUSE, AND/OR ALTERED SENSITIVITY MAY LEAD TO THE DEVELOPMENT OF ACIDOSIS, CARDIAC ARREST AND, POSSIBLY, DEATH.
Local anesthetic solutions containing antimicrobial preservatives (ie, those supplied in multiple-dose vials) should not be used for epidural or caudal anesthesia because safety has not been established with regard to intrathecal injection, either intentionally or inadvertently, of such preservatives.
It is essential that aspiration for blood or cerebrospinal fluid (where applicable) be done prior to injecting any local anesthetic, both the original dose and all subsequent doses, to avoid intravascular or subarachnoid injection. However, a negative aspiration does not ensure against an intravascular or subarachnoid injection.
Reactions resulting in fatality have occurred on rare occasions with the use of local anesthetics.
Mepivacaine with epinephrine or other vasopressors should not be used concomitantly with ergot-type oxytocic drugs, because a severe persistent hypertension may occur. Likewise, solutions of mepivacaine containing a vasoconstrictor, such as epinephrine, should be used with extreme caution in patients receiving monoamine oxidase inhibitors (MAOI) or antidepressants of the triptyline or imipramine types, because severe prolonged hypertension may result.
Local anesthetic procedures should be used with caution when there is inflammation and/or sepsis in the region of the proposed injection.
Mixing or the prior or intercurrent use of any local anesthetic with mepivacaine cannot be recommended because of insufficient data on the clinical use of such mixtures.
PRECAUTIONS:
The safety and effectiveness of local anesthetics depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. Resuscitative equipment, oxygen, and other resuscitative drugs should be available for immediate use (see WARNINGS and ADVERSE REACTIONS ). During major regional nerve blocks, the patient should have IV fluids running via an indwelling catheter to assure a functioning intravenous pathway. The lowest dosage of local anesthetic that results in effective anesthesia should be used to avoid high plasma levels and serious adverse effects. Injections should be made slowly, with frequent aspirations before and during the injection to avoid intravascular injection. Current opinion favors fractional administration with constant attention to the patient, rather than rapid bolus injection. Syringe aspirations should also be performed before and during each supplemental injection in continuous (intermittent) catheter techniques. An intravascular injection is still possible even if aspirations for blood are negative.
During the administration of epidural anesthesia, it is recommended that a test dose be administered initially and the effects monitored before the full dose is given. When using a “continuous” catheter technique, test doses should be given prior to both the original and all reinforcing doses, because plastic tubing in the epidural space can migrate into a blood vessel or through the dura. When the clinical conditions permit, an effective test dose should contain epinephrine (10 mcg to 15 mcg have been suggested) to serve as a warning of unintended intravascular injection. If injected into a blood vessel, this amount of epinephrine is likely to produce an “epinephrine response” within 45 seconds, consisting of an increase of pulse and blood pressure, circumoral pallor, palpitations, and nervousness in the unsedated patient. The sedated patient may exhibit only a pulse rate increase of 20 or more beats per minute for 15 or more seconds. Therefore, following the test dose, the heart rate should be monitored for a heart rate increase. The test dose should also contain 45 mg to 50 mg of mepivacaine hydrochloride to detect an unintended intrathecal administration. This will be evidenced within a few minutes by signs of spinal block (eg, decreased sensation of the buttocks, paresis of the legs, or, in the sedated patient, absent knee jerk).
Injection of repeated doses of local anesthetics may cause significant increases in plasma levels with each repeated dose due to slow accumulation of the drug or its metabolites or to slow metabolic degradation. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients, and acutely ill patients should be given reduced doses commensurate with their age and physical status. Local anesthetics should also be used with caution in patients with severe disturbances of cardiac rhythm, shock, heart block, or hypotension.
Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs, and the patient’s state of consciousness should be performed after each local anesthetic injection. It should be kept in mind at such times that restlessness, anxiety, incoherent speech, lightheadedness, numbness and tingling of the mouth and lips, metallic taste, tinnitus, dizziness, blurred vision, tremors, twitching, depression, or drowsiness may be early warning signs of central nervous system toxicity.
Local anesthetic solutions containing a vasoconstrictor should be used cautiously and in carefully restricted quantities in areas of the body supplied by end arteries or having otherwise compromised blood supply such as digits, nose, external ear, penis. Patients with hypertensive vascular disease may exhibit exaggerated vasoconstrictor response. Ischemic injury or necrosis may result.
Mepivacaine should be used with caution in patients with known allergies and sensitivities.
Because amide-type local anesthetics such as mepivacaine are metabolized by the liver and excreted by the kidneys, these drugs, especially repeat doses, should be used cautiously in patients with hepatic and renal disease. Patients with severe hepatic disease, because of their inability to metabolize local anesthetics normally, are at greater risk of developing toxic plasma concentrations. Local anesthetics should also be used with caution in patients with impaired cardiovascular function because they may be less able to compensate for functional changes associated with the prolongation of AV conduction produced by these drugs.
Serious dose-related cardiac arrhythmias may occur if preparations containing a vasoconstrictor such as epinephrine are employed in patients during or following the administration of potent inhalation anesthetics. In deciding whether to use these products concurrently in the same patient, the combined action of both agents upon the myocardium, the concentration and volume of vasoconstrictor used, and the time since injection, when applicable, should be taken into account.
Many drugs used during the conduct of anesthesia are considered potential triggering agents for familial malignant hyperthermia. Because it is not known whether amide-type local anesthetics may trigger this reaction and because the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for management should be available. Early unexplained signs of tachycardia, tachypnea, labile blood pressure, and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the suspect triggering agent(s), and institution of treatment, including oxygen therapy, indicated supportive measures, and dantrolene. (Consult dantrolene sodium intravenous package insert before using.)
Small doses of local anesthetics injected into the head and neck area may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. The injection procedures require the utmost care.
Confusion, convulsions, respiratory depression, and/or respiratory arrest, and cardiovascular stimulation or depression have been reported. These reactions may be due to intra-arterial injection of the local anesthetic with retrograde flow to the cerebral circulation. Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded.
When appropriate, patients should be informed in advance that they may experience temporary loss of sensation and motor activity, usually in the lower half of the body, following proper administration of caudal or epidural anesthesia. Also, when appropriate, the physician should discuss other information including adverse reactions listed in this package insert.
The administration of local anesthetic solutions containing epinephrine or norepinephrine to patients receiving monoamine oxidase inhibitors or tricyclic antidepressants may produce severe, prolonged hypertension. Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful patient monitoring is essential.
Concurrent administration of vasopressor drugs and of ergot-type oxytocic drugs may cause severe, persistent hypertension or cerebrovascular accidents.
Phenothiazines and butyrophenones may reduce or reverse the pressor effect of epinephrine.
Long-term studies in animals of most local anesthetics including mepivacaine to evaluate the carcinogenic potential have not been conducted. Mutagenic potential or the effect on fertility have not been determined. There is no evidence from human data that mepivacaine may be carcinogenic or mutagenic or that it impairs fertility.
Animal reproduction studies have not been conducted with mepivacaine. There are no adequate and well-controlled studies in pregnant women of the effect of mepivacaine on the developing fetus. Mepivacaine hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. This does not preclude the use of mepivacaine at term for obstetrical anesthesia or analgesia (see Labor and Delivery ).
Mepivacaine has been used for obstetrical analgesia by the epidural, caudal, and paracervical routes without evidence of adverse effects on the fetus when no more than the maximum safe dosages are used and strict adherence to technique is followed.
Local anesthetics rapidly cross the placenta, and when used for epidural, paracervical, caudal, or pudendal block anesthesia, can cause varying degrees of maternal, fetal, and neonatal toxicity (see CLINICAL PHARMACOLOGY , Pharmacokinetics ). The incidence and degree of toxicity depend upon the procedure performed, the type and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus, and neonate involve alterations of the central nervous system, peripheral vascular tone, and cardiac function.
Maternal hypotension has resulted from regional anesthesia. Local anesthetics produce vasodilation by blocking sympathetic nerves. Elevating the patient’s legs and positioning her on her left side will help prevent decreases in blood pressure. The fetal heart rate also should be monitored continuously and electronic fetal monitoring is highly advisable.
Epidural, paracervical, caudal, or pudendal anesthesia may alter the forces of parturition through changes in uterine contractility or maternal expulsive efforts. In one study, paracervical block anesthesia was associated with a decrease in the mean duration of first stage labor and facilitation of cervical dilation. Epidural anesthesia has been reported to prolong the second stage of labor by removing the parturient’s reflex urge to bear down or by interfering with motor function. The use of obstetrical anesthesia may increase the need for forceps assistance.
The use of some local anesthetic drug products during labor and delivery may be followed by diminished muscle strength and tone for the first day or two of life. The long-term significance of these observations is unknown.
Fetal bradycardia may occur in 20 to 30 percent of patients receiving para-cervical block anesthesia with the amide-type local anesthetics and may be associated with fetal acidosis. Fetal heart rate should always be monitored during paracervical anesthesia. Added risk appears to be present in prematurity, postmaturity, toxemia of pregnancy, and fetal distress. The physician should weigh the possible advantages against dangers when considering paracervical block in these conditions. Careful adherence to recommended dosage is of the utmost importance in obstetrical paracervical block. Failure to achieve adequate analgesia with recommended doses should arouse suspicion of intravascular or fetal intracranial injection.
Cases compatible with unintended fetal intracranial injection of local anesthetic solution have been reported following intended paracervical or pudendal block or both. Babies so affected present with unexplained neonatal depression at birth which correlates with high local anesthetic serum levels and usually manifest seizures within six hours. Prompt use of supportive measures combined with forced urinary excretion of the local anesthetic has been used successfully to manage this complication.
Case reports of maternal convulsions and cardiovascular collapse following use of some local anesthetics for paracervical block in early pregnancy (as anesthesia for elective abortion) suggest that systemic absorption under these circumstances may be rapid. The recommended maximum dose of the local anesthetic should not be exceeded. Injection should be made slowly and with frequent aspiration. Allow a five-minute interval between sides.
It is extremely important to avoid aortocaval compression by the gravid uterus during administration of regional block to parturients. To do this, the patient must be maintained in the left lateral decubitus position or a blanket roll or sandbag may be placed beneath the right hip and the gravid uterus displaced to the left.
It is not known whether local anesthetic drugs are excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when local anesthetics are administered to a nursing woman.
Guidelines for the administration of mepivacaine to pediatric patients are presented in DOSAGE AND ADMINISTRATION .
Clinical studies and other reported clinical experience indicates that use of the drug in elderly patients requires a decreased dosage (see CLINICAL PHARMACOLOGY , PRECAUTIONS , General , and DOSAGE AND ADMINISTRATION ).
Mepivacaine and mepivacaine metabolites are known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
ADVERSE REACTIONS:
Reactions to mepivacaine are characteristic of those associated with other amide-type local anesthetics. A major cause of adverse reactions to this group of drugs is excessive plasma levels, which may be due to overdosage, inadvertent intravascular injection, or slow metabolic degradation.
The most commonly encountered acute adverse experiences which demand immediate countermeasures are related to the central nervous system and the cardiovascular system. These adverse experiences are generally dose related and due to high plasma levels which may result from overdosage, rapid absorption from the injection site, diminished tolerance, or from unintentional intravascular injection of the local anesthetic solution. In addition to systemic dose-related toxicity, unintentional subarachnoid injection of drug during the intended performance of caudal or lumbar epidural block or nerve blocks near the vertebral column (especially in the head and neck region) may result in underventilation or apnea (“Total or High Spinal”). Also, hypotension due to loss of sympathetic tone and respiratory paralysis or underventilation due to cephalad extension of the motor level of anesthesia may occur. This may lead to secondary cardiac arrest if untreated. Factors influencing plasma protein binding, such as acidosis, systemic diseases which alter protein production, or competition of other drugs for protein binding sites, may diminish individual tolerance.
These are characterized by excitation and/or depression. Restlessness, anxiety, dizziness, tinnitus, blurred vision, or tremors may occur, possibly proceeding to convulsions. However, excitement may be transient or absent, with depression being the first manifestation of an adverse reaction. This may quickly be followed by drowsiness merging into unconsciousness and respiratory arrest. Other central nervous system effects may be nausea, vomiting, chills, and constriction of the pupils.
The incidence of convulsions associated with the use of local anesthetics varies with the procedure used and the total dose administered. In a survey of studies of epidural anesthesia, overt toxicity progressing to convulsions occurred in approximately 0.1% of local anesthetic administrations.
High doses or, inadvertent intravascular injection, may lead to high plasma levels and related depression of the myocardium, decreased cardiac output, heart block, hypotension (or sometimes hypertension), bradycardia, ventricular arrhythmias, and possibly cardiac arrest (see WARNINGS , PRECAUTIONS , and OVERDOSAGE ).
Allergic-type reactions are rare and may occur as a result of sensitivity to the local anesthetic or to other formulation ingredients, such as the antimicrobial preservative methylparaben, contained in multiple-dose vials. These reactions are characterized by signs such as urticaria, pruritus, erythema, angioneurotic edema (including laryngeal edema), tachycardia, sneezing, nausea, vomiting, dizziness, syncope, excessive sweating, elevated temperature, and possibly, anaphylactoid-like symptomatology (including severe hypotension). Cross sensitivity among members of the amide-type local anesthetic group has been reported. The usefulness of screening for sensitivity has not been definitely established.
The incidences of adverse neurologic reactions associated with the use of local anesthetics may be related to the total dose of local anesthetic administered and are also dependent upon the particular drug used, the route of administration, and the physical status of the patient. Many of these effects may be related to local anesthetic techniques, with or without a contribution from the drug.
In the practice of caudal or lumbar epidural block, occasional unintentional penetration of the subarachnoid space by the catheter or needle may occur. Subsequent adverse effects may depend partially on the amount of drug administered intrathecally and the physiological and physical effects of a dural puncture. A high spinal is characterized by paralysis of the legs, loss of consciousness, respiratory paralysis, and bradycardia.
Neurologic effects following epidural or caudal anesthesia may include spinal block of varying magnitude (including high or total spinal block); hypotension secondary to spinal block; urinary retention; fecal and urinary incontinence; loss of perineal sensation and sexual function; persistent anesthesia, paresthesia, weakness, paralysis of the lower extremities, and loss of sphincter control all of which may have slow, incomplete, or no recovery; headache; backache; septic meningitis; meningismus; slowing of labor; increased incidence of forceps delivery; cranial nerve palsies due to traction on nerves from loss of cerebrospinal fluid.
Neurologic effects following other procedures or routes of administration may include persistent anesthesia, paresthesia, weakness, paralysis, all of which may have slow, incomplete or no recovery.
OVERDOSAGE:
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics or to unintended subarachnoid injection of local anesthetic solution (see ADVERSE REACTIONS , WARNINGS , and PRECAUTIONS ).
The first consideration is prevention, best accomplished by careful and constant monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic injection. At the first sign of change, oxygen should be administered.
The first step in the management of systemic toxic reactions, as well as underventilation or apnea due to unintentional subarachnoid injection of drug solution, consists of immediate attention to the establishment and maintenance of a patent airway and effective assisted or controlled ventilation with 100% oxygen with a delivery system capable of permitting immediate positive airway pressure by mask. This may prevent convulsions if they have not already occurred.
If necessary, use drugs to control the convulsions. A 50 mg to 100 mg bolus IV injection of succinylcholine will paralyze the patient without depressing the central nervous or cardiovascular systems and facilitate ventilation. A bolus IV dose of 5 mg to 10 mg of diazepam or 50 mg to 100 mg of thiopental will permit ventilation and counteract central nervous system stimulation, but these drugs also depress central nervous system, respiratory, and cardiac function, add to postictal depression and may result in apnea. Intravenous barbiturates, anticonvulsant agents, or muscle relaxants should only be administered by those familiar with their use. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated. Supportive treatment of circulatory depression may require administration of intravenous fluids, and when appropriate, a vasopressor dictated by the clinical situation (such as ephedrine or epinephrine to enhance myocardial contractile force).
Endotracheal intubation, employing drugs and techniques familiar to the clinician may be indicated after initial administration of oxygen by mask, if difficulty is encountered in the maintenance of patent airway or if prolonged ventilatory support (assisted or controlled) is indicated.
Recent clinical data from patients experiencing local anesthetic induced convulsions demonstrated rapid development of hypoxia, hypercarbia, and acidosis within a minute of the onset of convulsions. These observations suggest that oxygen consumption and carbon dioxide production are greatly increased during local anesthetic convulsions and emphasize the importance of immediate and effective ventilation with oxygen which may avoid cardiac arrest.
If not treated immediately, convulsions with simultaneous hypoxia, hypercarbia, and acidosis, plus myocardial depression from the direct effects of the local anesthetic may result in cardiac arrhythmias, bradycardia, asystole, ventricular fibrillation, or cardiac arrest. Respiratory abnormalities, including apnea, may occur. Underventilation or apnea due to unintentional subarachnoid injection of local anesthetic solution may produce these same signs and also lead to cardiac arrest if ventilatory support is not instituted. If cardiac arrest should occur, standard cardiopulmonary resuscitative measures should be instituted and maintained for a prolonged period if necessary. Recovery has been reported after prolonged resuscitative efforts.
The supine position is dangerous in pregnant women at term because of aortocaval compression by the gravid uterus. Therefore, during treatment of systemic toxicity, maternal hypotension, or fetal bradycardia following regional block, the parturient should be maintained in the left lateral decubitus position if possible, or manual displacement of the uterus off the great vessels should be accomplished.
The mean seizure dosage of mepivacaine in rhesus monkeys was found to be 18.8 mg/kg with mean arterial plasma concentration of 24.4 mcg/mL. The intravenous and subcutaneous LD50 in mice is 23 mg/kg to 35 mg/kg and 280 mg/kg respectively.
DOSAGE AND ADMINISTRATION:
The dose of any local anesthetic administered varies with the anesthetic procedure, the area to be anesthetized, the vascularity of the tissues, the number of neuronal segments to be blocked, the depth of anesthesia and degree of muscle relaxation required, the duration of anesthesia desired, individual tolerance and the physical condition of the patient. The smallest dose and concentration required to produce the desired result should be administered. Dosages of mepivacaine hydrochloride should be reduced for elderly and debilitated patients and patients with cardiac and/or liver disease. The rapid injection of a large volume of local anesthetic solution should be avoided and fractional doses should be used when feasible.
For specific techniques and procedures, refer to standard textbooks.
The recommended single adult dose (or the total of a series of doses given in one procedure) of mepivacaine hydrochloride for unsedated, healthy, normal-sized individuals should not usually exceed 400 mg. The recommended dosage is based on requirements for the average adult and should be reduced for elderly or debilitated patients.
While maximum doses of 7 mg/kg (550 mg) have been administered without adverse effect, these are not recommended, except in exceptional circumstances and under no circumstances should the administration be repeated at intervals of less than 1½ hours. The total dose for any 24-hour period should not exceed 1,000 mg because of a slow accumulation of the anesthetic or its derivatives or slower than normal metabolic degradation or detoxification with repeat administration (see CLINICAL PHARMACOLOGY and PRECAUTIONS ).
Pediatric patients tolerate the local anesthetic as well as adults. However, the pediatric dose should be carefully measured as a percentage of the total adult dose based on weight , and should not exceed 5 mg/kg to 6 mg/kg (2.5 mg/lb to 3 mg/lb) in pediatric patients, especially those weighing less than 30 lbs. In pediatric patients under 3 years of age or weighing less than 30 lbs concentrations less than 2% (eg, 0.5% to 1.5%) should be employed.
Unused portions of solutions not containing preservatives, ie, those supplied in single-dose vials, should be discarded following initial use.
This product should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Solutions which are discolored or which contain particulate matter should not be administered.
Recommended Concentrations and Doses of Mepivacaine Hydrochloride
|
Procedure
|
Concentration
|
mL |
Total Dose
|
mg |
Comments
|
|
Cervical,
|
1%
|
5-40
|
|
50-400
|
Pudendal block:
|
|
brachial, |
|
|
|
|
one half of total |
|
|
|
|
|
|
|
|
intercostal, |
|
|
|
|
dose injected |
|
|
|
|
|
|
|
|
pudendal |
2% |
5-20 |
|
100-400 |
each side. |
|
|
|
|
|
|
|
|
nerve block
|
|
|
|
|
|
|
Transvaginal
|
1%
|
up to 30
|
|
up to 300
|
One half of total
|
|
block |
|
(both sides) |
|
(both sides) |
dose injected |
|
|
|
|
|
|
|
|
(paracervical |
|
|
|
|
each side. See |
|
|
|
|
|
|
|
|
plus pudendal)
|
|
|
|
|
|
|
Paracervical
|
1%
|
up to 20
|
|
up to 200
|
One half of total
|
|
block |
|
(both sides) |
|
(both sides) |
dose injected each |
|
|
|
|
|
|
|
|
|
|
|
|
|
side. This is maxi- |
|
|
|
|
|
|
|
|
|
|
|
|
|
mum recommended |
|
|
|
|
|
|
|
|
|
|
|
|
|
dose per 90-minute |
|
|
|
|
|
|
|
|
|
|
|
|
|
period in obstetrical |
|
|
|
|
|
|
|
|
|
|
|
|
|
and non-obstetrical |
|
|
|
|
|
|
|
|
|
|
|
|
|
patients. Inject slowly, |
|
|
|
|
|
|
|
|
|
|
|
|
|
5 minutes between |
|
|
|
|
|
|
|
|
|
|
|
|
|
sides. See |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Caudal and
|
1%
|
15-30
|
|
150-300
|
*Use only single-dose
|
|
Epidural block |
1.5% |
10-25 |
|
150-375 |
vials which do not |
|
|
|
|
|
|
|
|
|
2%
|
10-20
|
|
200-400
|
contain a preservative.
|
|
Infiltration
|
1%
|
up to 40
|
|
up to 400
|
An equivalent amount
|
|
|
|
|
|
|
of a 0.5% solution |
|
|
|
|
|
|
|
|
|
|
|
|
|
(prepared by diluting |
|
|
|
|
|
|
|
|
|
|
|
|
|
the 1% solution with |
|
|
|
|
|
|
|
|
|
|
|
|
|
Sodium Chloride |
|
|
|
|
|
|
|
|
|
|
|
|
|
Injection, USP) may |
|
|
|
|
|
|
|
|
|
|
|
|
|
be used for large |
|
|
|
|
|
|
|
|
|
|
|
|
|
areas.
|
|
Therapeutic
|
1%
|
1-5
|
|
10-50
|
|
|
block (pain |
2% |
1-5 |
|
20-100 |
|
|
|
|
|
|
|
|
|
management) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Unused portions of solutions not containing preservatives should be discarded. |
|||||
* Dosage forms listed as POLOCAINE-MPF (Mepivacaine HCl Injection, USP) are single-dose solutions which do not contain a preservative.
HOW SUPPLIED:
Single-dose vials and multiple-dose vials of POLOCAINE may be sterilized by autoclaving at 15 pound pressure, 121°C (250°F) for 15 minutes. Solutions of POLOCAINE may be reautoclaved when necessary. Do not administer solutions which are discolored or which contain particulate matter.
THESE SOLUTIONS ARE NOT INTENDED FOR SPINAL ANESTHESIA OR DENTAL USE.
POLOCAINE-MPF (Mepivacaine HCl Injection, USP) without preservatives is available as follows:
|
Product No. |
NDC No. |
Strength |
Vial Size |
| 261030 | 63323-260-30 | 1% (10 mg/mL) | 30 mL single dose vial, packaged individually. |
| 293030 | 63323-293-30 | 1.5% (15 mg/mL) | 30 mL single dose vial, packaged individually. |
| 294020 | 63323-294-20 | 2% (20 mg/mL) | 20 mL single dose vial, packaged individually. |
POLOCAINE (mepivacaine HCl Injection, USP) with preservatives is available as follows:
|
Product No. |
NDC No. |
Strength |
Vial Size |
| 283050 | 63323-283-50 | 1% (10 mg/mL) | 50 mL multiple dose vial, packaged individually. |
| 296050 | 63323-296-50 | 2% (20 mg/mL) | 50 mL multiple dose vial, packaged individually. |
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]; brief exposure up to 40°C (104°F) does not adversely affect the product.
All trademarks are the property of APP Pharmaceuticals, LLC.
Manufactured for:
451105A/Revised: May 2008
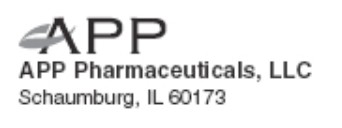
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine-MPF 30 mL Single Dose Vial Carton Panel
NDC 63323-260-30
261030
Polocaine ® -MPF
(mepivacaine HCl Injection, USP)
1%
10 mg/mL
For Nerve Block, Caudal, Epidural and Infiltration Anesthesia.
Not Intended for Spinal Anesthesia or Dental Use.
Methylparaben Free
Rx only
30 mL Single Dose Vial
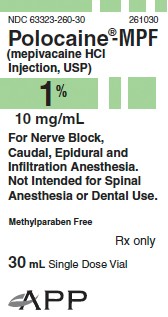
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine-MPF 30 mL Single Dose Vial Label
NDC 63323-260-30
261030
Polocaine ® -MPF
(mepivacaine HCl Injection, USP)
1% (10 mg/mL)
For Nerve Block, Caudal, Epidural and Infiltration Anesthesia.
Not Intended for Spinal Anesthesia or Dental Use.
Methylparaben Free
30 mL Single Dose Vial
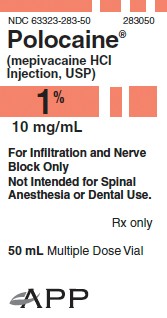
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine 50 mL Multiple Dose Vial Carton Panel
NDC 63323-283-50
283050
Polocaine ®
(mepivacaine HCl Injection, USP)
1%
10 mg/mL
For Infiltration and Nerve Block Only
Not Intended for Spinal Anesthesia or Dental Use.
Rx only
50 mL Multiple Dose Vial
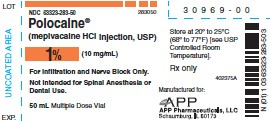
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine 50 mL Multiple Dose Vial Label
NDC 63323-283-50
283050
Polocaine ®
(mepivacaine HCl Injection, USP)
1% (10 mg/mL)
For Infiltration and Nerve Block Only.
Not Intended for Spinal Anesthesia or Dental Use.
50 mL Multiple Dose Vial
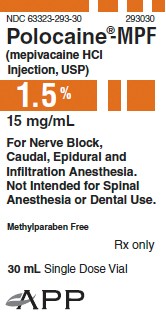
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine-MPF 30 mL Single Dose Vial Carton Panel
NDC 63323-293-30
293030
Polocaine®-MPF
(mepivacaine HCl Injection, USP)
1.5%
15 mg/mL
For Nerve Block, Caudal, Epidural and Infiltration Anesthesia.
Not Intended for Spinal Anesthesia or Dental Use.
Methylparaben Free
Rx only
30 mL Single Dose Vial
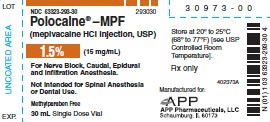
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine-MPF 30 mL Single Dose Vial Label
NDC 63323-293-30
293030
Polocaine®-MPF
(mepivacaine HCl Injection, USP)
1.5% (15 mg/mL)
For Nerve Block, Caudal, Epidural and Infiltration Anesthesia.
Not Intended for Spinal Anesthesia or Dental Use.
Methylparaben Free
30 mL Single Dose Vial
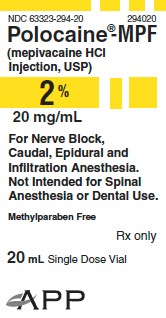
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine-MPF 20 mL Single Dose Vial Carton Panel
NDC 63323-294-20
294020
Polocaine®-MPF
(mepivacaine HCl Injection, USP)
2%
20 mg/mL
For Nerve Block, Caudal, Epidural and Infiltration Anesthesia.
Not Intended for Spinal Anesthesia or Dental Use.
Methylparaben Free
Rx only
20 mL Single Dose Vial
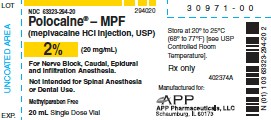
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine-MPF 20 mL Single Dose Vial Label
NDC 63323-294-20
294020
Polocaine®-MPF
(mepivacaine HCl Injection, USP)
2% (20 mg/mL)
For Nerve Block, Caudal, Epidural and Infiltration Anesthesia.
Not Intended for Spinal Anesthesia or Dental Use.
Methylparaben Free
20 mL Single Dose Vial
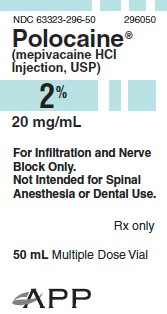
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine 50 mL Multiple Dose Vial Carton Panel
NDC 63323-296-50
296050
Polocaine ®
(mepivacaine HCl Injection, USP)
2%
20 mg/mL
For Infiltration and Nerve Block Only.
Not Intended for Spinal Anesthesia or Dental Use.
Rx only
50 mL Multiple Dose Vial
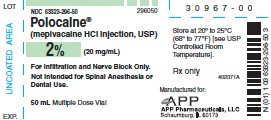
PACKAGE LABEL - PRINCIPAL DISPLAY - Polocaine 50 mL Multiple Dose Vial Label
NDC 63323-296-50
296050
Polocaine ®
(mepivacaine HCl Injection, USP)
2% (20 mg/mL)
For Infiltration and Nerve Block Only.
Not Intended for Spinal Anesthesia or Dental Use.
50 mL Multiple Dose Vial
PolocaineMEPIVACAINE HYDROCHLORIDE INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
PolocaineMEPIVACAINE HYDROCHLORIDE INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Polocaine-MPFMEPIVACAINE HYDROCHLORIDE INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Polocaine-MPFMEPIVACAINE HYDROCHLORIDE INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Polocaine-MPFMEPIVACAINE HYDROCHLORIDE INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||