PROCYSBI
HIGHLIGHTS OF PRESCRIBING INFORMATION INDICATIONS AND USAGEPROCYSBI is a cystine-depleting agent indicated for the management of nephropathic cystinosis in adults and children ages 6 years and older. (1) DOSAGE AND ADMINISTRATIONPROCYSBI should be prescribed by a physician experienced in management of nephropathic cystinosis. (2.1) Swallow capsules whole or after sprinkling on food or in recommended liquids. Administer via gastrostomy tube (12 F or larger) after mixing with food. (2.3) Total daily dose is 1.3 gram/m2/day in two divided doses, every 12 hours. (2.2) Take PROCYSBI at least 2 hours after and at least 30 minutes before eating. (2) Goal of therapy is to maintain a white blood cell (WBC) cystine level 0.1 mg/L. (2.6) Switching from Immediate-Release Cysteamine to PROCYSBI Total daily dose of PROCYSBI equal to their previous total daily dose of immediate-release cysteamine bitartrate. (2.7) Initial Dosage in Cysteamine-naïve patients Starting Dose: ⅙ to ¼ of the maintenance dose of PROCYSBI (2.1) Maintenance Dose: 1.3 gram/m2/day, in two divided doses every 12 hours (2.2) See Full Prescribing Information for details on administration. (2.3)DOSAGE FORMS AND STRENGTHSDelayed-release capsules: 25 mg and 75 mg (3)CONTRAINDICATIONSHypersensitivity to penicillamine (4)WARNINGS AND PRECAUTIONS Ehlers-Danlos like Syndrome: Reduce dosage if skin and bone lesions occur. (5.1) Skin Rash: Discontinue PROCYSBI if severe skin rash such as erythema multiforme bullosa or toxic epidermal necrolysis occurs. (5.2) Gastrointestinal: Monitor for symptoms of gastrointestinal ulceration and bleeding. (5.3) Central Nervous System: Monitor for seizures, lethargy, somnolence, depression, and encephalopathy. (5.4) Leukopenia and Elevated Alkaline Phosphatase Levels: Monitor white blood count and elevated alkaline phosphatase levels. (5.5) Benign Intracranial Hypertension: Monitor for signs and symptoms of benign intracranial hypertension. (5.6) Side EffectsMost commonly reported adverse reactions (≥5%) are vomiting, abdominal pain/discomfort, headaches, nausea, diarrhea, anorexia/decreased appetite, breath odor, fatigue, dizziness, skin odor, and rash. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Raptor Pharmaceuticals Inc. at 1-855-888-4004 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSPROCYSBI can be administered with electrolyte (except bicarbonate) and mineral replacements necessary for management of Fanconi Syndrome as well as vitamin D and thyroid hormone. (7) USE IN SPECIFIC POPULATIONSNursing Mothers: Breastfeeding is not recommended while taking PROCYSBI. (8.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 PROCYSBI INDICATIONS AND USAGE
- 2 PROCYSBI DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 PROCYSBI CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 PROCYSBI ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 PROCYSBI DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
PROCYSBI is indicated for the management of nephropathic cystinosis in adults and children ages 6 years and older.
2 DOSAGE AND ADMINISTRATION
PROCYSBI is available as a capsule in 25 mg and 75 mg strengths. Directions for use specific to the route and available methods of administration are presented below. PROCYSBI should be taken at least 2 hours after and at least 30 minutes before eating.
2.1 Starting Dose
PROCYSBI therapy should be initiated promptly once the diagnosis is confirmed (i.e., increased white blood cell (WBC) cystine concentration). Cysteamine-naïve patients should be started on ⅙ to ¼ of the maintenance dose of PROCYSBI. The dose should be raised gradually over 4 to 6 weeks to help reduce the risk of side-effects. WBC cystine level and/or cysteamine concentration measurements, taken 30 minutes after dose administration, are recommended for new patients after the maintenance dose is achieved.
2.2 Maintenance Dose
The recommended PROCYSBI maintenance dose is 1.3 gram/m2/day, in two divided doses given every 12 hours. [see Administration Options (2.3)] The dose can be increased up to 1.95 grams/m2/day if the white blood cell cystine level remains higher than the target WBC cystine level and/or the target cysteamine concentration has not been achieved. [see Dose Titration (2)]
|
Weight in Pounds |
mg of PROCYSBI Every 12 hours |
| 0-10 | 200 |
| 11-20 | 300 |
| 21-30 | 400 |
| 31-40 | 500 |
| 41-50 | 600 |
| 51-70 | 700 |
| 71-90 | 800 |
| 91-110 | 900 |
| >110 | 1000 |
2.3 Administration Options
PROCYSBI - Oral Administration
- PROCYSBI should be swallowed whole. Patients should not crush or chew capsules or capsule contents.
- Alternatively, for patients who have difficulty swallowing capsules, PROCYSBI can be opened and administered as follows:
- Open capsule.
- Sprinkle intact granules on approximately 4 ounces (½ cup) of applesauce or berry jelly.
- Eat mixture within 30 minutes of preparation.
- PROCYSBI may also be emptied into a small volume of either orange juice or apple juice:
- Mix or sprinkle intact granules into a small volume of either orange juice or apple juice (approximately 4 ounces (½cup)).
- Shake gently for 5 minutes then administer by spoon or cup within 30 minutes.
PROCYSBI - Feeding Tube Administration
- For patients who have a 12 French or larger gastrostomy (G)-tube in place, PROCYSBI can be administered as follows:
- Open capsule.
- Mix intact granules into approximately 4 ounces (½ cup) of applesauce.
- Administer mixture via feeding tube within 30 minutes.
- Flush with approximately 8 ounces (1 cup) of orange juice or apple juice to clear the tube.
USE IN OTHER FOODS AND LIQUIDS HAS NOT BEEN STUDIED CLINICALLY AND IS THEREFORE NOT RECOMMENDED.
2.4 Administration with Food
Patients should not eat for at least 2 hours before taking PROCYSBI and at least 30 minutes after taking PROCYSBI. Patients who are unable to take PROCYSBI without eating should eat only a small amount (approximately 4 ounces (½ cup)) of food between 1 hour before taking PROCYSBI and 1 hour after taking PROCYSBI. Patients should take PROCYSBI in a consistent manner in regard to food.
2.5 Missed Doses
Patients should be instructed that if a dose is missed, it should be taken as soon as possible. However, if a patient has missed a dose and the next scheduled dose is due in less than 4 hours, the patient should be instructed to not take the missed dose, and to take the next dose on time. Patients should be instructed not to take 2 doses at one time to make up for a missed dose.
2.6 Dose Titration
Titration Based on WBC Cystine: Adjust the PROCYSBI dosage to produce the target WBC cystine level. Measured concentrations of cystine in WBCs vary according to analytical techniques for WBC protein levels. Therefore, target concentrations of cystine in WBC should be determined by individual analytical laboratories using local methodology and calibration of protein assay.
Titration Based on Plasma Cysteamine: If WBC cystine measurements are not available, plasma cysteamine measurement may be used to help guide PROCYSBI dose titration. Titrate the PROCYSBI dosage to maintain a cysteamine concentration >0.1 mg/L, 30 minutes after dosing.
WBC cystine levels (or plasma cysteamine concentration if adequate WBC cystine testing is not available) should be measured as follows:
- Monthly for 3 months, then quarterly for 1 year, then twice yearly at a minimum for patients never treated with immediate-release cysteamine before.
- Two weeks, then quarterly for 6 months, then twice yearly at a minimum for patients switching from immediate-release cysteamine to PROCYSBI.
Measurement Timing: WBC cystine and/or plasma cysteamine measurements must be obtained 12.5 hours after the evening dose the day before, and therefore 30 minutes after the following morning dose is given.
Measurement Interpretation:
- In well-controlled and adherent patients with nephropathic cystinosis, the plasma cysteamine is >0.1 mg/L, and the WBC cystine is <1.0 nmol ½ cystine/mg protein.
- If the plasma cysteamine is >0.1 mg/L, but the WBC cystine is >1.0 nmol ½ cystine/mg protein, the physician is advised to investigate the following parameters: adherence to dosing interval, adherence to medication, or the relationship between administration of PROCYSBI and fasted/fed state.
PROCYSBI dosing may need to be increased to achieve the target WBC cystine concentration (or plasma cysteamine concentration) or decreased if there is evidence of intolerance to PROCYSBI. [see Warnings and Precautions (5) and Adverse Reactions (6)]) If a dose adjustment is required, it is recommended to adjust the dose by 10%. The dose of PROCYSBI can be increased to a maximum of 1.95 grams/m2/day to achieve the target WBC cystine concentration (or plasma cysteamine concentration). The dose of 1.95 grams/m2/day of immediate-release cysteamine bitartrate has been associated with an increased rate of withdrawal from treatment due to intolerance and an increased incidence of adverse reactions.
Patients who initially tolerate PROCYSBI poorly should temporarily stop taking PROCYSBI, then re-start PROCYSBI at a lower dose and gradually increase the dose to the proper dose. [see Warnings and Precautions (5)] Some patients may be unable to achieve their therapeutic target due to poorer tolerability of PROCYSBI.
2.7 Transferring Patients from Immediate-release Cysteamine Bitartrate Capsules
Patients with cystinosis taking immediate-release cysteamine bitartrate may be transferred to a total daily dose of PROCYSBI equal to their previous total daily dose of immediate-release cysteamine bitartrate. Patients being transferred from immediate-release cysteamine bitartrate to PROCYSBI should have their WBC cystine levels and/or plasma cysteamine concentration measured in 2 weeks, and quarterly for 6 months, then twice yearly at a minimum.
3 DOSAGE FORMS AND STRENGTHS
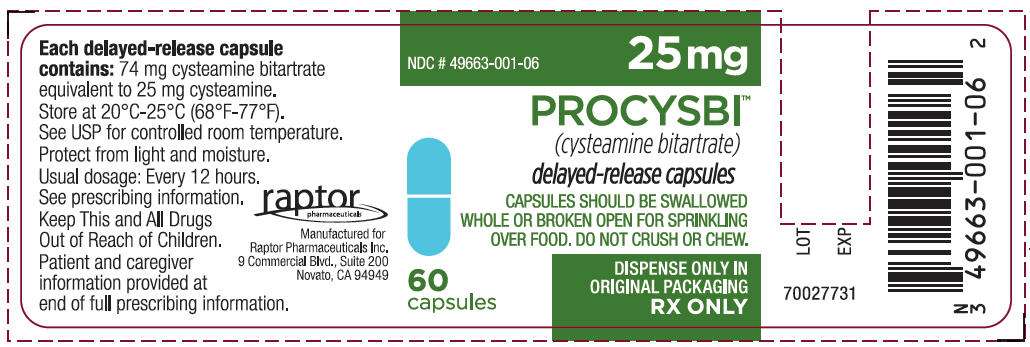
- Each 25 mg delayed-release capsule contains 74 mg cysteamine bitartrate, equivalent to 25 mg cysteamine. The capsules are light blue opaque cap imprinted with “Raptor” logo in white ink and light blue opaque body imprinted with “25 mg” in white ink.
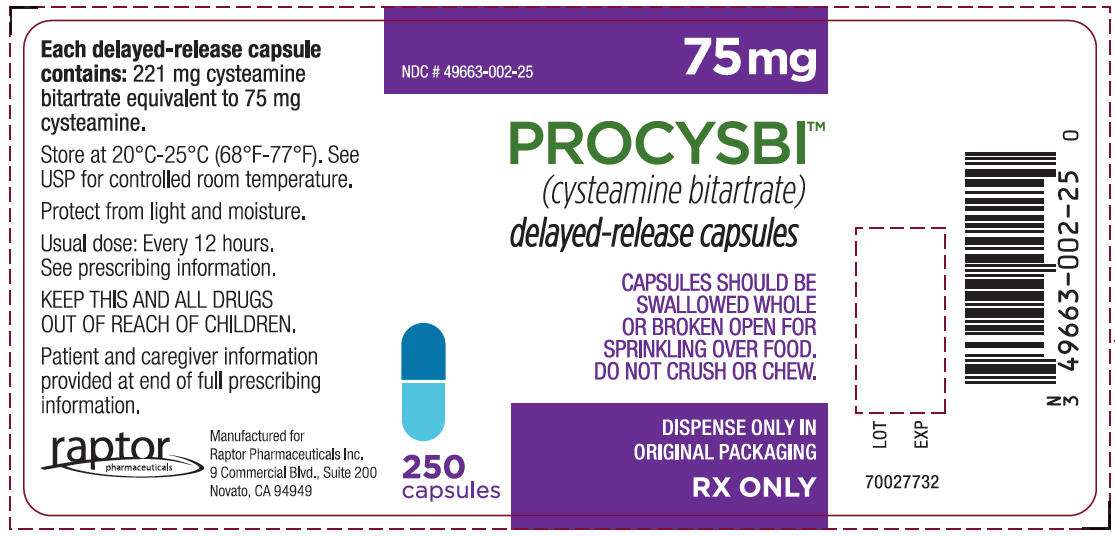
- Each 75 mg delayed-release capsule contains 221 mg cysteamine bitartrate, equivalent to 75 mg cysteamine. The capsules are dark blue opaque cap imprinted with “Raptor” logo in white ink and light blue opaque body imprinted with “75 mg” in white ink.
4 CONTRAINDICATIONS
The use of PROCYSBI is contraindicated in patients who are hypersensitive to penicillamine.
5 WARNINGS AND PRECAUTIONS
5.1 Ehlers-Danlos like Syndrome
Skin and bone lesions that resemble clinical findings for Ehlers-Danlos syndrome have been reported in patients treated with high doses of immediate-release cysteamine bitartrate or other cysteamine salts. These include molluscoid pseudotumors (purplish hemorrhagic lesions), skin striae, bone lesions (including osteopenia, compression fractures, scoliosis and genu valgum), leg pain, and joint hyperextension. One patient on immediate-release cysteamine bitartrate with serious skin lesions subsequently died of acute cerebral ischemia with marked vasculopathy. Monitor patients for development of skin or bone lesions and interrupt PROCYSBI dosing if patients develop these lesions. PROCYSBI may be restarted at a lower dose under close supervision, then slowly increased to the appropriate therapeutic dose.
5.2 Skin Rash
Severe skin rashes such as erythema multiforme bullosa or toxic epidermal necrolysis have been reported in patients receiving immediate-release cysteamine bitartrate. If severe skin rashes develop, discontinue use of any cysteamine product permanently. [see Dosage and Administration (2)]
5.3 Gastrointestinal Ulcers and Bleeding
Gastrointestinal (GI) ulceration and bleeding have been reported in patients receiving immediate-release cysteamine bitartrate. GI tract symptoms including nausea, vomiting, anorexia and abdominal pain, sometimes severe, have been associated with cysteamine. If severe GI tract symptoms develop, consider decreasing the dose of PROCYSBI.
5.4 Central Nervous System Symptoms
Central Nervous System (CNS) symptoms such as seizures, lethargy, somnolence, depression, and encephalopathy have been associated with immediate-release cysteamine. Neurological complications have also been described in some patients with cystinosis who have not been treated with cysteamine. Carefully evaluate and monitor patients who develop CNS symptoms. Interrupt or adjust the dose as necessary for patients with severe symptoms or with symptoms that persist or progress. Patients should exercise caution when driving or engaging in other hazardous activities when taking cysteamine.
5.5 Leukopenia and Elevated Alkaline Phosphatase Levels
Cysteamine has been associated with reversible leukopenia and elevated alkaline phosphatase levels. Therefore, blood counts and alkaline phosphatase levels should be monitored.
5.6 Benign Intracranial Hypertension
Benign intracranial hypertension (pseudotumor cerebri; PTC) and/or papilledema has been reported in patients receiving immediate-release cysteamine bitartrate treatment. A causal relationship between PTC and cysteamine has not been established. Physicians should monitor patients for signs and symptoms of PTC, including headache, tinnitus, dizziness, nausea, diplopia, blurry vision, loss of vision, pain behind the eye or pain with eye movement.
6 ADVERSE REACTIONS
The following adverse reactions are also discussed in other sections of the labeling: gastrointestinal ulceration and bleeding, somnolence, encephalopathy, seizures, interstitial nephritis, elevated alkaline phosphatase, and leukopenia. [see Warnings and Precautions (5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. Causality of side-effects is sometimes difficult to determine because adverse effects may result from the underlying disease.
Clinical Trials Experience with Immediate-release Cysteamine
Cysteamine or phosphocysteamine have been administered to 246 children with cystinosis in three clinical trials (the National Collaborative Cysteamine Trial [NCCS], the Long-Term Trial, and a trial in the United Kingdom).
The most frequent adverse reactions involved the gastrointestinal and central nervous systems. These were especially prominent at the initiation of cysteamine therapy. Most patients were able to resume therapy at lower doses without incident of adverse reactions.
Adverse reactions were not collected systematically in the NCCS trial that treated 93 children but were often listed by investigators. The following rates may therefore be underestimated. The most common reactions (>5%) were vomiting (35%), anorexia (31%), fever (22%), diarrhea (16%), lethargy (11%), and rash (7%). Other adverse reactions included nausea, bad breath, abdominal pain, headache, dizziness, and urticaria.
Withdrawals due to intolerance, vomiting associated with medication, anorexia, lethargy, and fever occurred more frequently in those patients receiving 1.95 grams/m2/day as compared with 1.30 grams/m2/day of immediate-release cysteamine bitartrate.
Clinical Trials Experience with PROCYSBI
The data described below reflect exposure to PROCYSBI in 40 healthy volunteers in 3 clinical trials (Trials 2, 5, and 6) and 72 patients with nephropathic cystinosis in 3 clinical trials (Trials 1, 3 and 4). Healthy volunteers ranged in age from 19 to 64 years old and patients with nephropathic cystinosis ranged in age from 2 to 32 years old. Patients received PROCYSBI at doses ranging from 0.5 grams/m2/day to 2.23 grams/m2/day and included 45 males and 27 females. [see Clinical Studies (14)] The frequency of adverse reactions was similar across trials noting abdominal pain, nausea, and headache as the most commonly reported events in ≥5% of individuals in all trials.
The most commonly reported adverse reactions (≥5%) in healthy volunteers were diarrhea and nausea, abdominal pain /discomfort, headache, vomiting and abnormal urine odor. The most commonly reported adverse reactions (≥5%) in patients with nephropathic cystinosis were vomiting, abdominal pain/discomfort, headaches, nausea, diarrhea, anorexia/decreased appetite, breath odor, fatigue, dizziness, skin odor, and rash.
There have not been any unexpected serious adverse events (SAEs) reported by patients in clinical trials attributable to PROCYSBI. In Trial 3, the pivotal clinical trial comparing PROCYSBI to the immediate-release cysteamine bitartrate, a higher incidence of adverse reactions was reported in patients during the PROCYSBI treatment period compared with the immediate-release cysteamine treatment period (see Table 2).
Other significant adverse reactions reported during clinical trials included anaphylaxis and allergic reaction.
| Adverse Reaction |
Immediate-release cysteamine |
PROCYSBI |
|
(n = 41) % |
(n = 43) % |
|
| Vomiting/emesis |
12 | 19 |
| Nausea |
7 | 16 |
| Abdominal pain/discomfort | 0 | 14 |
| Headache | 0 | 9 |
| Dizziness | 0 | 5 |
| Anorexia/loss of appetite | 5 | 2 |
Trial 4 includes patients continuing treatment from Trial 3. In Trial 4, 40 patients have been treated for longer than 1 year and 3 patients have been treated for at least 19 months. The most commonly reported adverse reactions (≥5%) were vomiting, abdominal pain, nausea, breath odor, diarrhea, skin odor, and decreased appetite.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of immediate-release cysteamine bitartrate: benign intracranial hypertension (or PTC) with papilledema; skin lesions, molluscoid pseudotumors, skin striae, skin fragility; joint hyperextension, leg pain, genu valgum, osteopenia, compression fracture and scoliosis. [see Warnings and Precautions (5.1, 5.6)]
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Following the pivotal Phase 3 trial, 40 subjects have been treated for at least 1 year with PROCYSBI in an Extension Trial. There were no unexpected or serious safety concerns experienced by subjects attributable to PROCYSBI. Based on the average number of gastrointestinal AEs per subject per month that went slightly downward from 0.11 gastrointestinal disorder AEs/subject/month to approximately 0.09 gastrointestinal disorder AEs/subject/month, there was a gradual decrease in gastrointestinal disorder AEs with long-term PROCYSBI therapy (p<0.05). This decrease was also seen in the average number of total AEs/subject/month; from approximately 0.15 total AEs/subject/month at the beginning of the trial to approximately 0.08 total AEs/subject/month (p<0.05, post-hoc analysis).
In two randomized clinical trials with healthy volunteers, there were no unexpected serious adverse events reported that were attributable to PROCYSBI. The most frequent adverse events (AEs) reported by the subjects related to PROCYSBI were GI symptoms (16%). The AE profile for healthy subjects was similar to the AE profile in patients relative to gastrointestinal disorders (diarrhea and abdominal pain).
7 DRUG INTERACTIONS
PROCYSBI can be administered with electrolyte (except bicarbonate) and mineral replacements necessary for management of Fanconi Syndrome as well as vitamin D and thyroid hormone.
An in-vitro study indicates cysteamine bitartrate is not an inhibitor of CYP enzymes (CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4). The potential for cysteamine to affect the pharmacokinetics of other drugs via these enzymes is low.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Risk Summary
There are no adequate and well-controlled studies in pregnant women. Cysteamine (administered as cysteamine bitartrate) was teratogenic and fetotoxic in rats at doses less than the recommended human maintenance dose.
PROCYSBI should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Animal Data
Embryo-fetal development studies were conducted in rats using oral administration of cysteamine bitartrate, with a dose range of 37.5 to 150 mg/kg/day of cysteamine equivalent (about 0.2 to 0.7 times the recommended human maintenance dose based on body surface area). Cysteamine bitartrate was fetotoxic and produced adverse developmental effects. Observed teratogenic findings were cleft palate, kyphosis, heart ventricular septal defects, microcephaly and exencephaly.
8.3 Nursing Mothers
It is not known whether cysteamine is present in human milk. A decrease in survival occurred in neonatal rats nursed by mothers receiving cysteamine. [see Nonclinical Toxicology (13)] Because many drugs are present in human milk and because of the potential for serious adverse reactions in nursing infants from cysteamine, nursing is not recommended.
8.4 Pediatric Use
PROCYSBI therapy should be initiated as soon as the diagnosis of nephropathic cystinosis has been confirmed in children greater than 6 years and adults. The risks and benefits of treatment with PROCYSBI in children under 6 years old are not yet established.
9 DRUG ABUSE AND DEPENDENCE
Cysteamine has not been associated with abuse potential, or psychological or physical dependence in humans.
10 OVERDOSAGE
A single oral dose of cysteamine at 660 mg/kg was lethal to rats. Symptoms of acute toxicity were reduction of motor activity and generalized hemorrhage in gastrointestinal tract and kidneys.
Two cases of human overdosing with immediate-release cysteamine bitartrate have been reported. In one case, the patient immediately vomited the drug and did not develop any symptoms. The second incident involved an accidental ingestion of a 200 to 250 mg/kg dose by a healthy 13-month-old child. Vomiting and dehydration were experienced. The child was hospitalized and fluids were administered. A full recovery was made.
Should overdosing occur, the respiratory and cardiovascular systems should be supported appropriately. No specific antidote is known. Hemodialysis may be considered since cysteamine is poorly bound to plasma proteins.
11 DESCRIPTION
PROCYSBI, for oral administration, is a cystine-depleting agent that lowers the cystine content of cells in patients with nephropathic cystinosis, an inherited defect of lysosomal transport.
PROCYSBI contains the bitartrate salt of cysteamine. The chemical name for cysteamine bitartrate is ethanethiol, 2-amino, (2R,3R)-2,3-dihydroxybutanedioate (1:1) (salt). Cysteamine bitartrate is a highly water soluble white powder with a molecular weight of 227.24 and the molecular formula C2H7NS • C4H6O6. It has the following chemical structure:
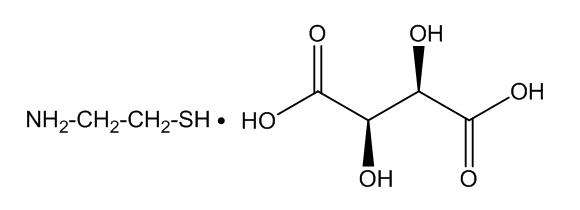
Each 25 mg delayed-release capsule contains 74 mg cysteamine bitartrate, equivalent to 25 mg cysteamine. Each 75 mg delayed-release capsule contains 221 mg cysteamine bitartrate, equivalent to 75 mg cysteamine. PROCYSBI contains the following inactive ingredients: microcrystalline cellulose, Eudragit® L 30 D-55, hypromellose, talc, triethyl citrate, sodium lauryl sulfate, and purified water. Capsule shell ingredients are gelatin, titanium dioxide, blue ink and white ink.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Cysteamine is an aminothiol that participates within lysosomes in a thiol-disulfide interchange reaction converting cystine into cysteine and cysteine-cysteamine mixed disulfide, both of which can exit the lysosome in patients with cystinosis.
12.2 Pharmacodynamics
Normal individuals and persons heterozygous for cystinosis have white blood cell cystine levels of <0.2 and usually below 1 nmol ½ cystine/mg protein, respectively. Untreated patients with nephropathic cystinosis have elevations of white blood cell cystine above 2 nmol ½ cystine/mg protein. White blood cell cystine is monitored in these patients to determine adequacy of dosing, levels being measured 30 minutes after dosing when treated with PROCYSBI. In a Long-Term Study [see Clinical Studies (14)], entry white blood cell cystine levels were 3.73 nmol ½ cystine/mg protein (range 0.13 to 19.80 nmol ½ cystine/mg protein) and were maintained close to 1 nmol ½ cystine/mg protein with an immediate-release cysteamine dose range of 1.3 to 1.95 g/m2/day. [see Dose Titration (2.6)]
12.3 Pharmacokinetics
Pharmacokinetic (PK) and pharmacodynamic (PD) relationships following a single dose of PROCYSBI was first studied in comparison to a single dose of immediate-release cysteamine bitartrate in a study with 9 patients. [see Clinical Studies (14)] Following normalization to a 450 mg dose, the maximum plasma levels Cmax, AUC0-6h and AUC0-12h (calculated directly from the plasma level data for PROCYSBI and from doubling the AUC0-6h value for immediate-release cysteamine to represent two doses) were lower for PROCYSBI (27.70 ± 14.99 µmol/L, 75.93 ± 39.22 µmol*h/L and 99.26 ± 44.21 µmol*h/L respectively) than for immediate-release cysteamine bitartrate (37.72 ± 12.10 µmol/L, 96.00 ± 37.81 µmol*h/L and 192.00 ± 75.62 µmol*h/L respectively.
The pharmacokinetics of PROCYSBI are consistent with a delayed-release formulation showing a Tmax of 2.78 ± 1.56 h for PROCYSBI cysteamine was moderately bound to human plasma proteins, predominantly to albumin, with mean protein binding of about 52%. Plasma protein binding was independent of concentration over the concentration range achieved clinically with the recommended doses.
After each dose of PROCYSBI the cysteamine concentration in the blood continues to decline for approximately 30 minutes and the level of WBC cystine increases accordingly. [see Clinical Studies (14)]
An exploratory study suggested that administering the contents of PROCYSBI mixed with a small amount (4 ounces) of applesauce had no effect on the rate and extent of cysteamine absorption as compared with administration of intact capsules.
An additional bioequivalence trial (n=20) was conducted in fasted healthy volunteers. In this bioequivalence trial, intact capsules were taken with orange juice instead of applesauce. Analysis showed bioequivalence between whole capsule and sprinkle administration in the fasted state.
An exploratory trial shows that food can reduce the systemic exposure of cysteamine; therefore, it is recommended that PROCYSBI be administered at least 30 minutes before or 2 hours after a meal.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Cysteamine has not been tested for its carcinogenic potential in long-term animal studies.
PROCYSBI was not mutagenic in the Ames test. It produced a negative response in an in-vitro sister chromatid exchange assay in human lymphocytes, but a positive response in a similar assay in hamster ovarian cells.
Repeat breeding reproduction studies were conducted in male and female rats. Cysteamine was found to have no effect on fertility and reproductive performance at an oral dose of 75 mg/kg/day (450 mg/m2/day, 0.4 times the recommended human dose based on body surface area). At an oral dose of 375 mg/kg/day (2,250 mg/m2/day, 1.7 times the recommended human maintenance dose based on body surface area), it reduced the fertility of the adult rats and the survival of their offspring.
14 CLINICAL STUDIES
14.1 Clinical Trials with Immediate-release Cysteamine
Three open-label clinical trials with either cysteamine hydrochloride or phosphocysteamine were used to support demonstration of efficacy of immediate-release cysteamine bitartrate.
In one of these trials, the National Collaborative Cysteamine Study (NCCS), 94 children (mainly from the United States) with nephropathic cystinosis were treated with increasing doses of cysteamine hydrochloride (mean dose 54 mg/kg/day) to attain white blood cell cystine levels of less than 2 nmol ½ cystine/mg protein 5 to 6 hours post-dose. The trial compared their outcome with an historical control group of 17 children who had been in the placebo group of a randomized placebo-controlled trial of ascorbic acid. Cysteamine-treated patients had been diagnosed at a mean age of 22 months and were a mean age of 46 months old at study entry; placebo patients had been diagnosed at about 29 months and were a mean age of about 52 months old at trial entry. The principal measures of effectiveness were serum creatinine and calculated creatinine clearance and growth (height).
The average median white blood cell cystine level attained during treatment in the NCCS was 1.7 ± 0.2 nmol ½ cystine/mg protein. There were 70 cysteamine patients with baseline serum creatinine less than 2 mg/dL who were followed for at least 1 year and 17 placebo patients. Twelve of the 94 cysteamine-treated patients required early dialysis or renal transplant. Median follow-up of cysteamine patients was over 32 months and 20% were followed more than 5 years. Median follow-up of the placebo group was 20 months; only 1 patient was followed more than 24 months. Glomerular function among cysteamine patients was maintained over time. Placebo treated patients experienced a gradual rise in serum creatinine. Renal tubular function was not affected by treatment.
Calculated creatinine clearances were evaluated for two groups of children, one with poor white blood cell cystine depletion (defined as median WBC cystine levels >3 nmol ½ cystine/mg protein or WBC cystine levels not measured at least 2 times per year) and one with good white blood cell cystine depletion. The final mean creatinine clearance of the good depletion group was 20.8 ml/min/1.73 m2 greater than the mean for the poor-depletion group.
Height-for-age measurements of treated patients were compared with height-for-age measurements of 143 patients initially screened for inclusion in the NCCS. Patients on treatment maintained growth (i.e., did not show increasing growth failure compared with normal scales) although growth velocity did not increase enough to allow patients to catch up to age norms for height.
The open-label Long-Term Trial, initiated in 1988, utilized both cysteamine hydrochloride and phosphocysteamine (patient's choice) in 46 patients who had completed the NCCS (averaging 6.5 years of treatment) and 93 new patients. Patients had cystinosis diagnosed by elevated white blood cell cystine (mean 3.63 nmol ½ cystine/mg). New patients and 46 continuing patients were required to have serum creatinine less than 3.0 mg/dL and 4.0 mg/dL, respectively. Patients were randomized to doses of 1.3 or 1.95 g/m2/day and stratified according to whether the serum creatinine was above 1.2 mg/dL or not. Doses could be raised if white cell cystine levels were approximately 2 nmol ½ cystine/mg protein and lowered due to intolerance. The mean patient age for new patients was about 49 months for the cysteamine group and about 34 months for the phosphocysteamine group, respectively. The mean patient age for patients in the long-term follow-up group was about 9 years.
Mean doses were 1.27 g/m2/day and 1.87 g/m2/day in the two groups and white blood cell cystine levels averaged 1.72 ± 1.65 nmol ½ cystine/mg protein and 1.86 ± 0.92 nmol ½ cystine/mg protein in the 1.3 and 1.95 g/m2/day in the two groups, respectively. In new patients, serum creatinine was essentially unchanged over the period of follow-up (about half of the patients were followed for 24 months) and phosphocysteamine and cysteamine hydrochloride had similar effects. The long-term follow-up group also had essentially no change in renal function (almost 80% were followed at least 2 years). In four studies of patients with untreated cystinosis, renal death (need for transplant or dialysis) occurred at median age of less than 10 years. [see Dosage and Administration (2)]
Both new patients and patients in the long-term follow-up group maintained height (although they did not catch up from baseline). There was no apparent difference in height maintenance between the two doses.
14.2 Clinical Trials with PROCYSBI
Trial 1 (RP103-01) was a single center, single-dose, open-label, non-randomized, 2-period, immediate-release cysteamine bitartrate vs. PROCYSBI pilot study in 9 (8 pediatric and 1 adult) patients with nephropathic cystinosis ages 6 years to 24 years; 78 % were male. The trial reported highly variable inter-patient bioavailability with both immediate-release cysteamine and PROCYSBI. The trial suggested that, when WBC cystine trough levels are used as a measurement of cellular cystine depletion, delayed-release cysteamine (PROCYSBI) administered every 12 hours (Q12H) is as effective as immediate-release cysteamine bitartrate administered every 6 hours (Q6H).
Trials 2, 5, and 6 (RP103-02, RP103-05, and RP103-06 respectively) were PK studies conducted in healthy volunteers. [see Nonclinical Toxicology (13)]
Trial 3 (RP103-03), the pivotal trial for PROCYSBI, was a phase 3 multicenter (US and EU), randomized, crossover, immediate-release cysteamine bitartrate vs. PROCYSBI trial in 43 (40 pediatric and 3 adult) patients with nephropathic cystinosis. Patient age ranged from 6 to 26 years (mean age 12 years) and 56% were male. Patients with white blood cell (WBC) cystine levels >2 nmol/½ cystine/mg protein and estimated glomerular filtration rate (eGFR corrected for body surface area) <30 mL/minute/1.73 m2 at the time of screening were excluded from the trial. Prior to randomization, patients were to be on a stable dose of immediate-release cysteamine bitartrate administered Q6H. PROCYSBI dose adjustments of up to approximately 100% of the total daily dose of immediate-release cysteamine bitartrate were allowed by trial criteria. The average total daily dose of PROCYSBI for patients completing the clinical trial was approximately 91 % of the average total daily dose of immediate-release cysteamine bitartrate for patients at trial entry. [see Dose Titration (2.6)]
Trial 3 demonstrated that at steady-state, PROCYSBI administered Q12H was non-inferior to immediate-release cysteamine bitartrate administered Q6H with respect to the depletion of WBC cystine levels (Table 3). Using a linear mixed effects statistical analysis model, the least-square-mean value of WBC cystine was 0.52 ± 0.06 nmol/½ cystine/mg protein after 12 hours under PROCYSBI and 0.44 ± 0.06 nmol/½ cystine/mg protein after 6 hours under immediate-release cysteamine; a difference of 0.08 ± 0.03 nmol/½ cystine/mg protein (95.8 % Confidence Interval = 0.01 to 0.15).
Forty out of 41 patients completing Trial 3 are continuing treatment with PROCYSBI in an ongoing, open-label extension trial, i.e. Trial 4 (RP103-04), for total treatment duration of 24 months. Twenty additional patients (14 pediatric patients, ages 1 to 6 years, and 6 (4 adult and 2 pediatric) renal transplant patients) have also been enrolled in Trial 4. An interim analysis was performed after all enrolled patients from Trial 3 had been treated with PROCYSBI for at least 12 months (n=33) and up to 19 months (n=3). The analysis indicated that patients switched from immediate-release cysteamine to a treatment regimen of PROCYSBI maintained a WBC level <1 nmol/½ cystine/mg protein for up to 19 months at a total daily dose equal to their total daily dose of immediate-release cysteamine at entry in Trial 3. During extended treatment there has been on average no worsening of the kidney function, as expressed by the estimated glomerular filtration rate (eGFR).
| Per–Protocol (PP) Population (N=39) |
Immediate-release cysteamine bitartrate |
PROCYSBI |
| WBC cystine level (LS Mean ± SE) in nmol/½ cystine/mg protein | 0.44 ± 0.06 | 0.52 ± 0.06 |
| Treatment effect (LS mean ± SE; 95.8% CI; p-value) |
0.08 ± 0.03 ; 0.01 to 0.15; <0.0001 | |
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
- 25 mg Delayed-release Capsule: A hard gelatin capsule with light blue opaque cap imprinted with “Raptor” Logo in white ink and light blue opaque body imprinted with “25 mg” in white ink, supplied as bottle of 60 capsules (NDC 49663-001-06).
- 75 mg Delayed-release Capsule: A hard gelatin capsule with dark blue opaque cap imprinted with “Raptor” Logo in white ink and light blue opaque body imprinted with “75 mg” in white ink, supplied as bottle of 250 capsules (NDC 49663-002-25).
Storage
Store at 20°C to 25°C (68° to 77°F); excursions permitted between 15° and 30°C (59° and 86°F) [See USP Controlled Room Temperature]. Protect from light and moisture.
Dispense only in original packaging. Do not subdivide or repackage. Do not remove desiccant or oxygen absorber from the container. Keep bottles tightly closed in a dry place.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information)
Instruct patients and caregivers that the constraints/risks associated with PROCYSBI include:
17.1 Laboratory Monitoring
Discuss with the patient and caregivers the requirement to do laboratory testing to determine the correct dose of PROCYSBI. WBC cystine levels (or plasma cysteamine concentration if adequate WBC cystine testing is not available) should be measured as follows:
- Monthly for 3 months, then quarterly for 1 year, then twice yearly at a minimum for patients never treated with immediate-release cysteamine before.
- Two weeks, then quarterly for 6 months, then twice yearly at a minimum for patients switching from immediate-release to PROCYSBI.
Measurement Timing: WBC cystine and/or plasma cysteamine measurements must be obtained 12.5 hours after the evening dose the day before, and therefore 30 minutes after the following morning dose is given.
Measurement Interpretation: In well-controlled and adherent patients with nephropathic cystinosis, the plasma cysteamine is >0.1 mg/L, and the WBC cystine is <1.0 nmol ½ cystine/mg protein. If the plasma cysteamine is >0.1 mg/L, but the WBC cystine is >1.0 nmol ½ cystine/mg protein, ask the patient about the following: adherence to dosing interval, adherence to medication, or the relationship between administration of PROCYSBI and fasted/fed state.
17.2 Dosing and Administration
Instruct patients and caregivers to take PROCYSBI consistently and to not miss doses. Advise patients to take a missed dose as soon as possible. If it is within 4 hours of the next dose, patients should skip the missed dose and take the next regularly scheduled dose. Patients should not double the dose.
Instruct patients and caregivers that taking PROCYSBI with meals may affect the absorption of PROCYSBI. Patients may take PROCYSBI at least 2 hours after and at least 30 minutes before eating. For patients who tolerate PROCYSBI better with food, it is permissible to eat approximately 4 ounces (½ cup) of food within 1 hour before and 1 hour after taking PROCYSBI. Instruct patients to take PROCYSBI consistently in relation to food (i.e., do not change between taking PROCYSBI while fasting and taking PROCYSBI with food) from one day to another. Avoid high fat food close to dosing of PROCYSBI.
17.3 Use by Pregnant Women
Patients should be instructed to immediately contact their physician if they suspect they may be pregnant. Discuss the individual risks and benefits of continuing PROCYSBI during pregnancy.
17.4 Breastfeeding
Breastfeeding is not recommended while taking PROCYSBI.
17.5 CNS Symptoms
Advise patients and caregivers that cysteamine may cause central nervous symptoms including seizures, lethargy, somnolence, depression, and encephalopathy that may require interrupting or decreasing the dose of PROCYSBI. Because somnolence may occur, patients should exercise caution in driving a car or engaging in other hazardous activities after taking PROCYSBI.
17.6 Gastrointestinal Ulcers and Bleeding
Advise patients and caregivers that PROCYSBI may cause ulcers and bleeding. Advise patients to contact their physician immediately if they experience stomach pain, nausea, vomiting, loss of appetite, or are vomiting blood.
17.7 Skin Rash
Advise patients and caregivers to contact their physician immediately if they experience a skin rash.
17.8 Neutropenia and Elevated Alkaline Phosphatase Levels
Advise patients that they should have laboratory testing to monitor for a low white blood count and elevated alkaline phosphatase while taking PROCYSBI.
17.9 Benign Intracranial Hypertension
Advise patients and caregivers that PROCYSBI may cause benign intracranial hypertension. Advise patients to contact their physician immediately if they experience headache, tinnitus, dizziness, nausea, double vision, blurry vision, loss of vision, or eye pain.
17.10 Ehlers-Danlos like Syndrome
Advise patients and caregivers that PROCYSBI may cause abnormalities of the skin, bones, and joints. Advise patients to report any skin changes to their physician.
Manufactured for:
Raptor Pharmaceuticals Inc.
9 Commercial Blvd, Suite 200
Novato, CA 94949
Update: April 2013
Part No. P1304402
Patient Information
PROCYSBI (Pro-CIS-bee)
(cysteamine bitartrate)
delayed-release capsules
What is PROCYSBI?
PROCYSBI is a prescription medicine used to manage a medical condition called nephropathic cystinosis in adults and children 6 years of age and older.
It is not known if PROCYSBI is safe and effective in children under 6 years of age.
Who should not take PROCYSBI?
Do not take PROCYSBI if you are allergic to penicillamine.
What should I tell my doctor before taking PROCYSBI?
Before you take PROCYSBI, tell your doctor if you:
- have a skin rash or bone problems
- have a history of seizures, exhaustion, sleepiness, depression, or other nervous system problems
- have or have had stomach or bowel (intestinal) problems including ulcers or bleeding
- have liver or blood problems
- are pregnant or plan to become pregnant. It is not known if PROCYSBI will harm your unborn baby. Tell your doctor right away if you think that you are pregnant. Talk with your doctor about the benefits and risks of taking PROCYSBI during pregnancy.
- are breastfeeding or plan to breastfeed. You should not breastfeed during treatment with PROCYSBI. Talk with your doctor about the best way to feed your baby if you take PROCYSBI.
Tell your doctor about all medicines that you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take PROCYSBI?
- Take PROCYSBI exactly as your doctor tells you to.
- Your doctor may start you on a low dose of PROCYSBI and slowly increase your dose to help avoid side-effects, especially if you have not taken a medicine that contains cysteamine bitartrate before.
- Do not change your dose of PROCYSBI unless your doctor tells you to.
- PROCYSBI is usually taken 2 times each day, every 12 hours.
- Take PROCYSBI the same way each time, either without eating or with a small amount of food, as follows:
- If you take PROCYSBI without eating, take PROCYSBI at least 30 minutes before you eat or at least 2 hours after you eat.
- If you are not able to take PROCYSBI without eating, you can eat a small amount of food (½ cup) between 1 hour before you take PROCYSBI to 1 hour after you take it.
- Avoid eating foods that are high in fat close to the time that you will take a dose of PROCYSBI.
- Talk to your doctor or pharmacist if you have questions about how to take PROCYSBI.
- Swallow PROCYSBI capsules whole.
- Do not crush or chew PROCYSBI or the capsule contents.
- If you cannot swallow the whole capsule, you can open it and take the capsule contents with certain foods and juices. PROCYSBI can also be given through a gastrostomy tube, 12 French or larger.
Taking PROCYSBI with certain foods:
You can only use applesauce or berry jelly.
- Open the capsule.
- Sprinkle the granules on 4 ounces (½ cup) of applesauce or berry jelly. Swallow mixture within 30 minutes.
Taking PROCYSBI with certain juices:
You can only use apple juice or orange juice.
- Open the capsule.
- Sprinkle the granules into 4 ounces (about ½ cup) of apple juice or orange juice.
- Shake gently for 5 minutes.
- Drink within 30 minutes.
Taking PROCYSBI through a gastrostomy tube, 12 French or larger:
You can only use applesauce.
- Open the capsule.
- Sprinkle the granules on 4 ounces (½ cup) of applesauce. Mix the granules with the applesauce.
- Give the medicine through the gastrostomy tube into the stomach within 30 minutes.
- After giving the mixture, flush the gastrostomy tube with 8 ounces (about 1 cup) of apple juice or orange juice to clear the tube. Do not use other liquids to flush the tube.
- If you miss a dose, take it as soon as possible. If it is within 4 hours of the time the next dose is due, skip the missed dose. Take the next dose at your regularly scheduled time. Do not take 2 doses at one time to make up for a missed dose.
- If you take too much PROCYSBI, call your doctor or go to the nearest hospital emergency room right away.
- Your doctor should do blood tests to measure the amount of cystine inside your white blood cells or to measure the amount of PROCYSBI in your blood before you start taking it and regularly during treatment with PROCYSBI. This will help your doctor to prescribe the dose of PROCYSBI that is right for you.
- Take supplements if prescribed by your doctor, such as salt or mineral replacement supplements, vitamin D, or thyroid hormone.
What should I avoid while taking PROCYSBI?
Do not drive or operate heavy machinery until you know how PROCYSBI affects you. PROCYSBI can make you sleepy or less alert than normal.
What are the possible side-effects of PROCYSBI?
PROCYSBI can cause serious side-effects, including:
- Skin, bone, and joint problems. People treated with high doses of cysteamine bitartrate may develop abnormal changes of their skin and bones. These changes may include stretch marks, bone injuries (such as fractures), bone deformities, and joint problems. Check your skin while taking PROCYSBI. Tell your doctor if you notice any skin changes. Your doctor will check you for these problems.
- Skin rash. Skin rash is common with cysteamine bitartrate and may sometimes be severe. Tell your doctor right away if you get a skin rash. Your dose of PROCYSBI may need to be decreased until the rash goes away. If the rash is severe, your doctor may tell you to stop taking PROCYSBI.
- Central nervous system symptoms. Some people who take other medicines that contain cysteamine bitartrate develop seizures, depression, and become very sleepy. The medicine may affect how your brain is working (encephalopathy). Tell your doctor right away if you develop any of these symptoms.
-
Stomach and bowel (intestinal) problems. Some people who take other medicines that contain cysteamine bitartrate develop ulcers and bleeding in their stomach or bowel.
Tell your doctor right away if you get stomach-area pain, nausea, vomiting, loss of appetite, or vomit blood. - Low white blood cell count and certain abnormal liver function blood tests. Your doctor should check you for these problems.
-
Benign intracranial hypertension (pseudotumor cerebri) has happened in some people who take immediate-release cysteamine bitartrate. This is a condition where there is high pressure in the fluid around the brain. Your doctor should do eye examinations to find and treat this problem early.
Tell your doctor right away if you develop any of the following symptoms while taking PROCYSBI: headache, buzzing or "whooshing" sound in the ear, dizziness, nausea, double vision, blurry vision, loss of vision, pain behind the eye, or pain with eye movement.
The most common side-effects with PROCYSBI include:
- vomiting
- abdominal pain or discomfort
- headache
- nausea
- diarrhea
- loss of appetite or decreased appetite
- breath odor
- tiredness
- dizziness
- skin odor
- skin rash
Tell your doctor if you have any side-effect that bothers you or that does not go away.
These are not all of the possible side-effects of PROCYSBI. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side-effects. You may report side-effects to FDA at 1-800-FDA-1088.
How should I store PROCYSBI?
- Store PROCYSBI at room temperature between 68° to 77°F (20° to 25°C).
- Store PROCYSBI in a dry place away from light.
- Keep PROCYSBI tightly closed in the original bottle.
- The PROCYSBI bottle contains a desiccant packet to help keep your medicine dry. Do not eat or throw away the desiccant packet.
Keep PROCYSBI and all medicines out of the reach of children.
General information about PROCYSBI
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use PROCYSBI for a condition for which it was not prescribed. Do not give PROCYSBI to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about PROCYSBI, talk with your doctor. You can ask your doctor or pharmacist for information about PROCYSBI that is written for health professionals. For more information call 1-855-888-4004.
What are the ingredients in PROCYSBI?
Active ingredients: cysteamine bitartrate
Inactive ingredients: microcrystalline cellulose, Eudragit® L 30 D-55, hypromellose, talc, triethyl citrate, sodium lauryl sulfate, and purified water
Capsule shell ingredients: gelatin, titanium dioxide, blue ink and white ink
This Patient Information has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Raptor Pharmaceuticals Inc.
9 Commercial Blvd, Suite 200
Novato, CA 94949
Issued April 2013
Part no. P1304502
Package Label - Principal Display Panel – 25 mg, 60 ct Capsules
Package Label - Principal Display Panel – 75 mg, 250 ct Capsules
PROCYSBICysteamine Bitartrate CAPSULE, DELAYED RELEASE PELLETS
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
PROCYSBICysteamine Bitartrate CAPSULE, DELAYED RELEASE PELLETS
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||