PURIXAN
Nova Laboratories, Ltd
Rare Disease Therapeutics, Inc.
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use PURIXAN safely and effectively. See full prescribing information for PURIXAN. PURIXAN (mercaptopurine) oral suspension Initial U.S. Approval: 1953INDICATIONS AND USAGE PURIXAN (mercaptopurine) is a nucleoside metabolic inhibitor indicated for the treatment of patients with acute lymphoblastic leukemia (ALL) as a component of a combination maintenance therapy regimen. (1.1) DOSAGE AND ADMINISTRATION The starting dose of PURIXAN in multi-agent combination chemotherapy maintenance regimens is 1.5 to 2.5 mg/kg (50 to 75 mg/m2) as a single daily dose. Use absolute neutrophil count to guide dosing. (2.1) DOSAGE FORMS AND STRENGTHS Oral suspension: 2000 mg/100 mL (20 mg/mL). (3) CONTRAINDICATIONS None. (4) WARNINGS AND PRECAUTIONS Myelosuppression: Monitor complete blood count (CBC) and adjust the dose of PURIXAN for severe neutropenia and thrombocytopenia. Evaluate patients with repeated severe myelosuppression for thiopurine S-methyltransferase (TPMT) deficiency. Patients with homozygous-TPMT deficiency require substantial dose reductions of PURIXAN. (5.1) Hepatotoxicity: Monitor transaminases and bilirubin. Hold or adjust the dose of PURIXAN. (5.2) Immunosuppression: Due to the immunosuppression associated with maintenance chemotherapy for ALL, response to all vaccines may be diminished and there is a risk of infection with live virus vaccines. Consult immunization guidelines for immunocompromised children. (5.3) Embryo-fetal toxicity: PURIXAN can cause fetal harm. Advise women of potential risk to a fetus. (5.4) Side Effects The most frequent adverse reaction (> 20% of patients) is myelosupression including anemia, neutropenia, and thrombocytopenia. Less common (5-20% of patients) adverse reactions include elevated transaminases, elevated bilirubin, intestinal ulceration, nausea, vomiting, anorexia, diarrhea and rashes. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Rare Disease Therapeutics, Inc., at 1 888-470-1904 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Allopurinol: Avoid use (7.1) Warfarin: PURIXAN may inhibit the anticoagulant effect. (7.2)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 PURIXAN INDICATIONS AND USAGE
- 2 PURIXAN DOSAGE AND ADMINISTRATION
- 2.1 Maintenance Therapy
- 2.2 Dosage in TPMT-deficient Patients
- 2.3 Administration Instructions
- 3 DOSAGE FORMS AND STRENGTHS
- 4 PURIXAN CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Myelosuppression
- 5.2 Hepatotoxicity
- 5.3 Immunosuppression
- 5.4 Embryo-Fetal Toxicity
- 5.5 Treatment Related Malignancies
- 5.6 Laboratory Tests
- 6 PURIXAN ADVERSE REACTIONS
- 6.1 Clinical Studies Experience
- 7 DRUG INTERACTIONS
- 7.1 Allopurinol
- 7.2 Warfarin
- 7.3 Myelosuppressants
- 7.4 Aminosalicylate Derivatives
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 PURIXAN DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PACKAGE LABEL
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Acute Lymphoblastic Leukemia
PURIXAN (mercaptopurine) is indicated for the treatment of patients with acute lymphoblastic leukemia as part of a combination regimen.
2 DOSAGE AND ADMINISTRATION
2.1 Maintenance Therapy
The starting dose of PURIXAN in multi-agent combination chemotherapy maintenance regimens is 1.5 to 2.5mg/kg (50 to 75 mg/m2) as a single daily dose.
After initiating PURIXAN, continuation of appropriate dosing requires periodic monitoring of absolute neutrophil count (ANC) and platelet count to assure sufficient drug exposure (that is to maintain ANC at a desirable level) and to adjust for excessive hematological toxicity.
2.2 Dosage in TPMT-deficient Patients
Patients with inherited little or no thiopurine S-methyltransferase (TPMT) activity are at increased risk for severe mercaptopurine toxicity from conventional doses of mercaptopurine and generally require dose reduction.
Testing for TPMT gene polymorphism should be considered in patients who experience severe bone marrow toxicities [
see Warnings and Precautions (5.1) and Clinical Pharmacology (12.5)
].
Homozygous deficient patients may require up to a 90% dosage reduction (10% of the standard PURIXAN dose). Most patients with heterozygous TPMT deficiency tolerated recommended mercaptopurine doses, but some require dose reduction based on toxicities.
2.3 Administration Instructions
The bottle should be shaken vigorously for at least 30 seconds to ensure the oral suspension is well mixed. PURIXAN is a pink to brown viscous oral suspension.
Once opened, PURIXAN should be used within 6 weeks. Dosing devices are not included with the product. The pharmacist should provide a commercially available oral syringe and suitable adaptor (if available), based on the dosing requirement for an individual patient.
If the syringe is intended for multiple use, instruct patients and caregivers to: wash the syringe with warm ‘soapy’ water and rinse well; hold the syringe under water and move the plunger up and down several times to make sure the inside of the syringe is clean;
ensure the syringe is completely dry before use of the syringe again for dosing; and store the syringe in a hygienic place with the medicine.
PURIXAN is a cytotoxic drug. Follow special handling and disposal procedures.1
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
The most consistent, dose-related toxicity of PURIXAN is bone marrow suppression, manifested by anemia, leukopenia, thrombocytopenia, or any combination of these.
Monitor CBC and adjust the dose of PURIXAN for severe neutropenia and thrombocytopenia.
Evaluate patients with repeated severe myelosuppression for thiopurine S-methyltransferase (TPMT) deficiency. Patients with homozygous-TPMT deficiency require substantial dose reductions of PURIXAN [
see Dosage and Administration (2.1), and Clinical Pharmacology (12.5)
].
Avoid the concurrent use of allopurinol and PURIXAN. Concomitant allopurinol and PURIXAN can result in a significant increase in bone marrow toxicity. Myelosuppression can be exacerbated by coadministration with drugs that inhibit TPMT (e.g., olsalazine, mesalamine, or sulfasalazine) or drugs whose primary or secondary toxicity is myelosuppression. [
see Drug Interactions (7.1, 7.3 and 7.4).
]
5.2 Hepatotoxicity
Mercaptopurine is hepatotoxic. There are reports of deaths attributed to hepatic necrosis associated with the administration of mercaptopurine. Hepatic injury can occur with any dosage, but seems to occur with greater frequency when the recommended dosage is exceeded.
In some patients jaundice has cleared following withdrawal of mercaptopurine and reappeared with rechallenge.
Usually, clinically detectable jaundice appears early in the course of treatment (1 to 2 months). However, jaundice has been reported as early as 1 week and as late as 8 years after the start of treatment with mercaptopurine.
The hepatotoxicity has been associated in some cases with anorexia, diarrhea, jaundice and ascites. Hepatic encephalopathy has occurred.
Monitor serum transaminase levels, alkaline phosphatase, and bilirubin levels at weekly intervals when first beginning therapy and at monthly intervals thereafter. Monitor liver function more frequently in patients who are receiving mercaptopurine with other hepatotoxic drugs or with known pre-existing liver disease.
Interrupt PURIXAN in patients with onset of clinical or laboratory evidence of hepatotoxicity.
5.3 Immunosuppression
Mercaptopurine is immunosuppressive and may impair the immune response to infectious agents or vaccines. Due to the immunosuppression associated with maintenance chemotherapy for ALL, response to all vaccines may be diminished and there is a risk of infection with live virus vaccines. Consult immunization guidelines for immunocompromised children.
5.4 Embryo-Fetal Toxicity
PURIXAN can cause fetal harm when administered to a pregnant woman. Women receiving PURIXAN in the first trimester of pregnancy have an increased incidence of abortion.
Adverse embryo-fetal findings were reported in women receiving mercaptopurine after the first trimester of pregnancy and included abortion and stillbirth.
There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential hazard to a fetus.
Women of childbearing potential should be advised to avoid becoming pregnant while receiving PURIXAN [
see Use in Specific Populations (8.1)
].
5.5 Treatment Related Malignancies
Cases of hepatosplenic T-cell lymphoma have been reported in patients treated with mercaptopurine for inflammatory bowel disease, for which mercaptopurine is not approved. Mercaptopurine is mutagenic in animals and humans, carcinogenic in animals, and may increase the risk of secondary malignancies.
5.6 Laboratory Tests
Monitor the following laboratory tests in patients receiving PURIXAN: Complete blood counts (CBCs), transaminases, and bilirubin. Evaluate the bone marrow in patients with prolonged or repeated marrow suppression to assess leukemia status and marrow cellularity.
Evaluate TPMT status in patients with clinical or laboratory evidence of severe bone marrow toxicity, or repeated episodes of myelosuppression.
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Based on multicenter cooperative group ALL trials, the most common adverse reaction occurring in > 20% of patients is mylelosuppression including anemia, neutropenia, lymphopenia and thrombocytopenia.
Adverse reactions occurring 5 to 20 % include anorexia, nausea, vomiting, diarrhea, malaise, and rash. Rare adverse reactions occuring < 5 % include urticaria, hyperuricemia, oral lesions, elevated transaminases, hyperbilirubinemia, hyperpigmentation, pancreatitis.
Oral lesions resemble thrush rather than antifolic ulcerations. Delayed or late toxicities include hepatic fibrosis, hyperbilirubinemia, alopecia, pulmonary fibrosis, oligospermia and secondary malignancies. [
see Warnings and Precautions (5.1 and 5.2)
].
Drug fever has been very rarely reported with PURIXAN. Before attributing fever to PURIXAN, every attempt should be made to exclude more common causes of pyrexia, such as sepsis, in patients with acute leukemia.
7 DRUG INTERACTIONS
7.1 Allopurinol
Avoid concomitant use of PURIXAN and allopurinol. Concomitant use of allopurinol with PURIXAN inhibits the first-pass oxidative metabolism of mercaptopurine by xanthine oxidase, leading to mercaptopurine toxicity (bone marrow suppression, nausea, vomiting) [ see Warnings and Precautions (5.1) ].
7.2 Warfarin
Concurrent use of PURIXAN and warfarin may result in decreased anticoagulant effectiveness. Monitor prothrombin time or international normalized ratio (INR) in patients receiving oral anticoagulant therapy with warfarin. Adjustments of the warfarin dose may be necessary in order to maintain the desired level of anticoagulation.
7.3 Myelosuppressants
Bone marrow suppression may be increased when PURIXAN is combined with other drugs whose primary or secondary toxicity is myelosuppression. Enhanced marrow suppression has been noted in some patients also receiving trimethoprim-sulfamethoxazole. Monitor CBC and adjust the dose of PURIXAN for severe neutropenia and thrombocytopenia [ see Warnings and Precautions (5.1) ].
7.4 Aminosalicylate Derivatives
Concurrent use of PURIXAN and aminosalicylate derivatives (e.g., olsalazine, mesalamine, or sulfasalazine) may inhibit the TPMT enzyme, resulting in an increased risk of bone marrow suppression. Should aminosalicylate derivatives and PURIXAN be coadministered, use the lowest possible doses of each drug and closely monitor the patient for bone marrow suppression [ see Warnings and Precautions (5.1) ].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D [see Warnings and Precautions (5.4)
].
Risk Summary
PURIXAN can cause fetal harm when administered to a pregnant woman. Women receiving PURIXAN have an increased incidence of abortion and stillbirth.
Advise women to avoid becoming pregnant while receiving PURIXAN. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
Human Data
Women receiving mercaptopurine in the first trimester of pregnancy have an increased incidence of abortion; the risk of malformation in offspring surviving first trimester exposure is not known.
In a series of 28 women receiving mercaptopurine after the first trimester of pregnancy, 3 mothers died prior to delivered, 1 delivered a stillborn child, and 1 aborted; there were no cases of macroscopically abnormal fetuses.
Animal Data
Mercaptopurine was embryo-lethal and teratogenic in several animal species (rat, mouse, rabbit, and hamster).
8.3 Nursing Mothers
It is not known whether mercaptopurine is excreted in human milk. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from mercaptopurine, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of mercaptopurine for the treatment of ALL in pediatric patients have not been established in adequate and well-controlled trials. The evidence for efficacy of mercaptopurine is derived from the published literature and clinical experience. The toxicities of mercaptopurine are similar in adults and children.
8.5 Geriatric Use
Clinical studies of mercaptopurine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
No formal clinical or pharmacokinetic studies have been conducted in patients with renal impairment.
Starting at the low end of the PURIXAN dosing range, or increasing the dosing interval to 36-48 hours can be considered in patients with baseline renal impairment.
Subsequent PURIXAN doses should be adjusted based on efficacy and toxicity [
see Dosage and Administration (2.1) and Warnings and Precautions (5.1)
].
8.7 Hepatic Impairment
No formal clinical or pharmacokinetic studies have been conducted in patients with hepatic impairment.
Mercaptopurine is hepatotoxic. In patients with baseline hepatic impairment, starting at the low end of the PURIXAN dose range should be considered and patients should be monitored for toxicity [
see Dosage and Administration (2.1) and
Warnings and Precautions (5.1,
5.2)
].
10 OVERDOSAGE
Signs and symptoms of mercaptopurine overdosage may be immediate (anorexia, nausea, vomiting, and diarrhea); or delayed (myelosuppression, liver dysfunction, and gastroenteritis).
Dialysis cannot be expected to clear mercaptopurine. Hemodialysis is thought to be of marginal use due to the rapid intracellular incorporation of mercaptopurine into active metabolites with long persistence.
The oral LD50 of mercaptopurine was determined to be 480mg/kg in the mouse and 425mg/kg in the rat.
There is no known pharmacologic antagonist of mercaptopurine. PURIXAN should be discontinued immediately if unintended toxicity occurs during treatment. If a patient is seen immediately following an accidental overdosage of PURIXAN, it may be useful to induce emesis.
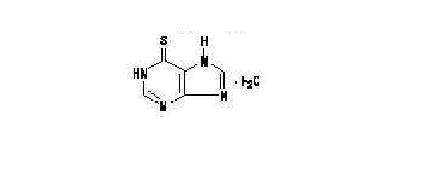
11 DESCRIPTION
Mercaptopurine, a nucleoside metabolic inhibitor, known chemically as 1,7-dihydro-6H-purine-6-thione monohydrate, is an analogue of the purine bases adenine and hypoxanthine. Mercaptopurine is a yellow, odorless or practically odorless, crystalline powder with a molecular formula of C5H4N4S•H2O and a molecular weight of 170.20 as a monohydrate. The structural formula is:
PURIXAN (mercaptopurine) oral suspension is supplied for oral administration and contains 2000 mg/100 mL (20 mg/mL) of mercaptopurine. The suspension also contains the following inactive ingredients: xanthan gum, aspartame, concentrated raspberry juice, sucrose, methyl parahydroxybenzoate, propyl parahydroxybenzoate and purified water. PURIXAN is a pink to brown viscous suspension.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Mercaptopurine activation occurs via hypoxanthine-guanine phosphoribosyl transferase (HGPRTase) and several enzymes to form 6-thioguanine nucleotides (6-TGNs). Incorporation of 6-TGN into nucleic acids (instead of purine bases) results in cell-cycle arrest and cell death. Mercaptopurine competes with hypoxanthine and guanine for HGPRTase and is itself converted to thioinosinic acid (TIMP). This intracellular nucleotide inhibits several reactions involving inosinic acid (IMP), including the conversion of IMP to xanthylic acid (XMP) and the conversion of IMP to adenylic acid (AMP) via adenylosuccinate (SAMP). In addition, 6-methylthioinosinate (MTIMP) is formed by the methylation of TIMP. Both TIMP and MTIMP have been reported to inhibit glutamine-5-phosphoribosylpyrophosphate amidotransferase, the first enzyme unique to the de novo pathway for purine ribonucleotide synthesis. Experiments indicate that radiolabeled mercaptopurine may be recovered from the DNA in the form of deoxythioguanosine. Some mercaptopurine is converted to nucleotide derivatives of 6-thioguanine (6-TG) by the sequential actions of inosinate (IMP) dehydrogenase and xanthylate (XMP) aminase, converting TIMP to thioguanylic acid (TGMP).
12.3 Pharmacokinetics
The relative bioavailability of PURIXAN was compared to mercaptopurine 50 mg tablets in 62 healthy subjects in a single-dose, two-period, crossover study under fasting conditions. Bioequivalence was demonstrated based on the primary PK parameters AUC(0-t) and AUC(0-∞). Cmax did not demonstrate bioequivalence. The mean Cmax following PURIXAN administration was 34% higher than the tablet.
Absorption and Bioavailability
Clinical studies have shown that the absorption of an oral dose of mercaptopurine in humans is incomplete and variable, averaging approximately 50% of the administered dose.
The factors influencing absorption are unknown.
Following a single 50 mg dose of PURIXAN under fasting conditions the median (range) AUC was 136 h*ng/mL (74.2-264.8 h*ng/mL) and Cmax was 95 ng/mL (39.5-204 ng/mL).
Distribution
The volume of distribution usually exceeded that of the total body water. There is negligible entry of mercaptopurine into cerebrospinal fluid.
Metabolism
Mercaptopurine is inactivated via two major pathways. One is thiol methylation, which is catalyzed by the polymorphic enzyme thiopurine S-methyltransferase (TPMT), to form the inactive metabolite methyl-mercaptopurine. The second inactivation pathway is oxidation, which is catalyzed by xanthine oxidase. The product of oxidation is the inactive metabolite 6-thiouric acid.
Elimination
Following administration of PURIXAN, the elimination half-life (t1/2) was approximately 2 hours.
After oral administration of 35S-6-mercaptopurine, urine contains intact mercaptopurine, thiouric acid (formed by direct oxidation by xanthine oxidase, probably via 6-mercapto-8-hydroxypurine), and a number of 6-methylated thiopurines. In one subject, a total of 46% of the dose could be accounted for in the urine (as parent drug and metabolites) in the first 24 hours.
12.5 Pharmacogenomics
TPMT enzyme activity is highly variable in patients because of a genetic polymorphism in the TPMT gene. For Caucasians and African Americans, approximately 0.3% (1:300) of patients have two non-functional alleles (homozygous-deficient) of the TPMT gene and have little or no detectable TMPT activity.
Approximately 10% of patients have one TPMT non-functional allele (heterozygous) leading to low or intermediate TPMT activity and 90% of patients have normal TPMT activity with two functional alleles.
Homozygous-deficient patients with little or no detectable TPMT activity, if given usual doses of mercaptopurine, accumulate excessive cellular concentrations of active 6-TGNs predisposing them to mercaptopurine toxicity.
Heterozygous patients with low or intermediate TPMT activity accumulate higher concentrations of active 6-TGNs than patients with normal TPMT activity and are more likely to experience mercaptopurine toxicity [
see Warnings and Precautions (5.1)
].
TPMT genotyping or phenotyping (red blood cell TPMT activity) can identify patients who are homozygous deficient or have low or intermediate TPMT activity.
TPMT Testing
Genotypic and phenotypic testing of TPMT status are available. Genotypic testing can determine the allelic pattern of a patient. Currently, 3 alleles—TPMT*2, TPMT*3A and TPMT*3C— account for about 95% of individuals with reduced levels of TPMT activity.
Individuals homozygous for these alleles are TPMT deficient and those heterozygous for these alleles have variable TPMT (low or intermediate) activity. Phenotypic testing determines the level of thiopurine nucleotides or TPMT activity in erythrocytes and can also be informative.
Caution must be used with phenotyping since some coadministered drugs can influence measurement of TPMT activity in blood, and recent blood transfusions will misrepresent a patient’s actual TPMT activity.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mercaptopurine is carcinogenic in animals and humans.
Mercaptopurine causes chromosomal aberrations in animals and humans and induces dominant-lethal mutations in male mice.
Mercaptopurine may impair fertility. In mice, surviving female offspring of mothers who received chronic low doses of mercaptopurine during pregnancy were found sterile, or if they became pregnant, had smaller litters and more dead fetuses as compared to control animals.
14 CLINICAL STUDIES
The safety and effectiveness of mercaptopurine for the treatment of ALL in pediatric and adult patients have not been established in adequate and well-controlled trials. [ see Clinical Pharmacology (12.3) ].
15 REFERENCES
1. OSHA Hazardous Drugs. OSHA. [Accessed on March 28, 2014, from http://www.osha.gov/SLTC/hazardousdrugs/index.html]
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
PURIXAN (mercaptopurine) oral suspension 2000 mg/100 mL (20 mg/mL) is a pink to brown viscous liquid supplied in amber glass multiple-dose bottles with a child resistant closure.
100 mL bottle NDC #62484-0020-1.
16.2 Storage and Handling
Store between 15 to 25ºC (59º to 77ºF) in a dry place.
PURIXAN is a cytotoxic drug. Follow special handling and disposal procedures1.
17 PATIENT COUNSELING INFORMATION
Major Toxicities
Inform patients and caregivers that the major toxicities of PURIXAN are related to myelosuppression, hepatotoxicity, and gastrointestinal toxicity.
Advise patients to contact their physician if they experience fever, sore throat, jaundice, nausea, vomiting, signs of local infection, bleeding from any site, or symptoms suggestive of anemia.
Pregnancy
Advise women of childbearing potential to avoid becoming pregnant.
Administration
Inform patients and caregivers to shake the bottle vigorously for at least 30 seconds to ensure the oral suspension is well mixed.
PURIXAN (mercaptopurine) oral suspension is pink in color but because it contains a natural fruit extract, the color of the suspension may vary from pink to brown.
Instruct patients and caregivers that once opened, PURIXAN should be used within 6 weeks.
Tell patients and caregivers to ensure that the pharmacist includes a commercially available oral syringe and suitable adaptor, based on the dosing requirement for an individual patient.
If the syringe is intended for multiple use, instruct patients and caregivers to: wash the syringe with warm ‘soapy’ water and rinse well; hold the syringe under water and move the plunger up and down several times to make sure the inside of the syringe is clean;
ensure the syringe is completely dry before use of the syringe again for dosing; and store the syringe in a hygienic place with the medicine.
Manufactured by:
Nova Laboratories Ltd
Leister
LEI 8 4YL
United Kingdom
Manufactured for:
Rare Disease Therapeutics
2550 Meridian Blvd., Suite 150
Franklin, TN 37067
www.raretx.com
Distributed by:
AnovoRx Distribution, LLC
1710 North Shelby Oaks Drive
Suite 6
Memphis, TN 38134
Part Number: D000532/1
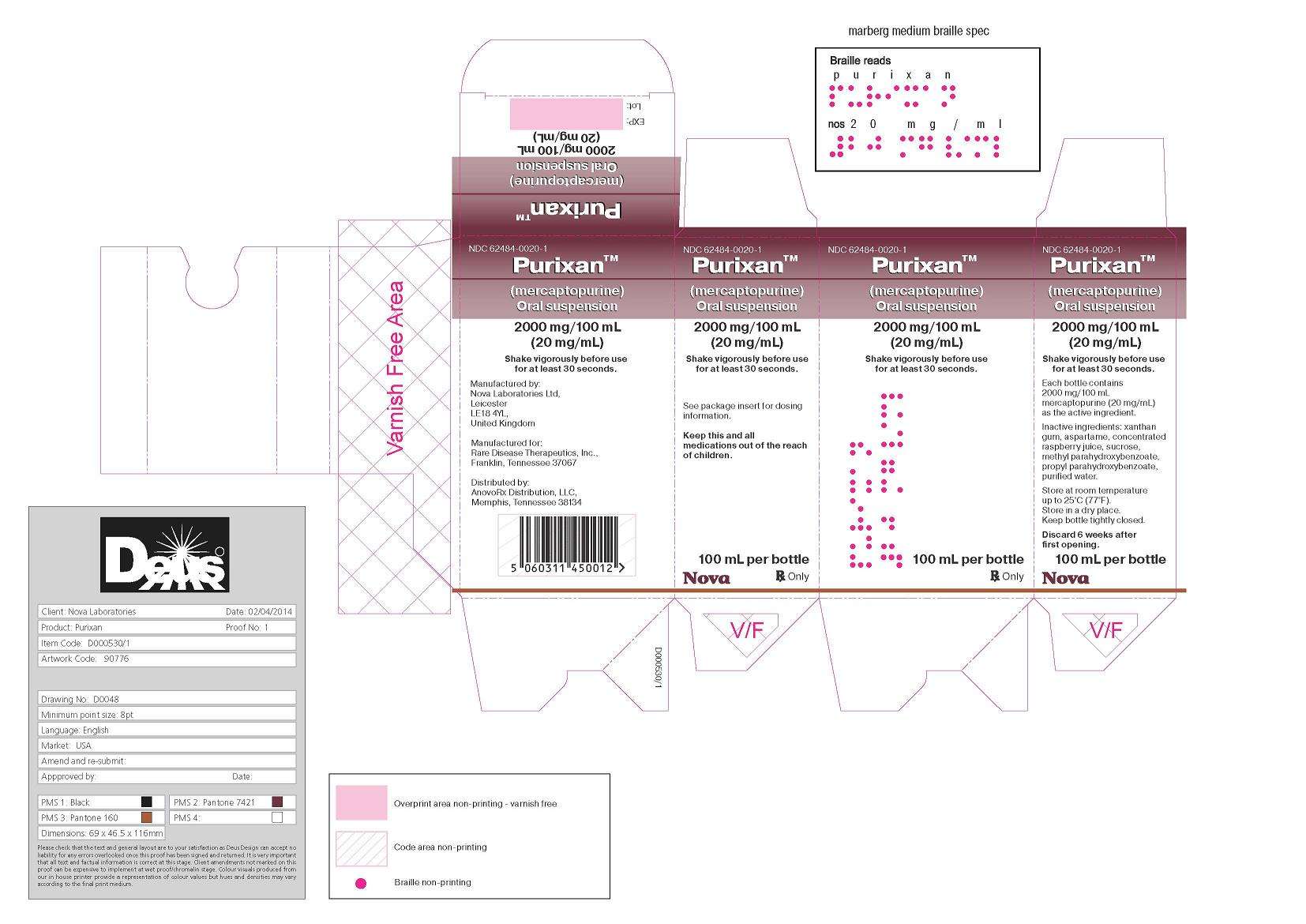
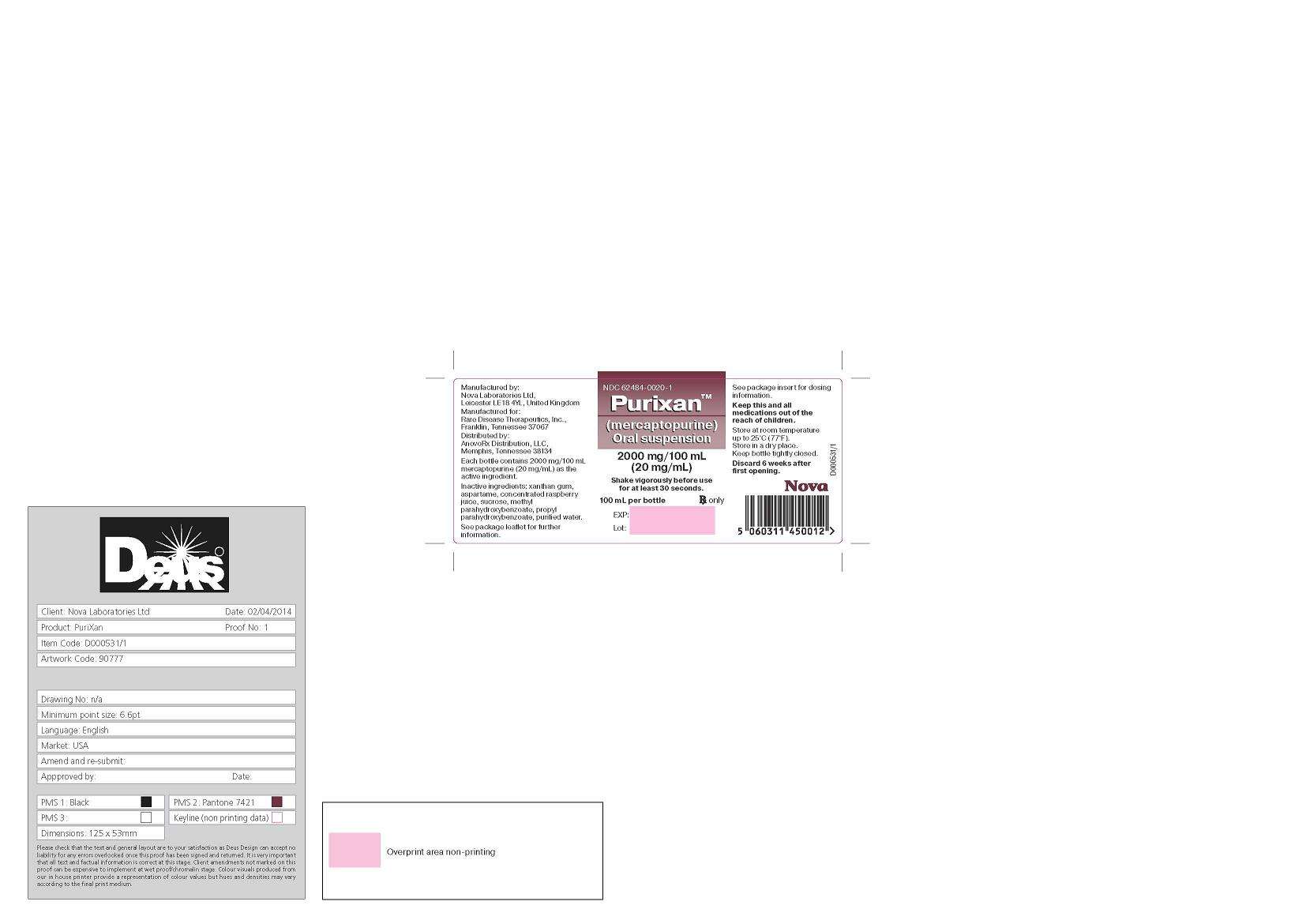
PACKAGE LABEL
Purixan Carton label
Purixan Bottle label
PURIXANPurixan SUSPENSION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||