RISPERIDONE
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use risperidone safely and effectively. See full prescribing information for risperidone oral solution, USP. RISPERIDONE Oral Solution, USPInitial U.S. Approval: 1993BOXED WARNING WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS See full prescribing information for complete boxed warning. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone is not approved for use in patients with dementia-related psychosis. (5.1) INDICATIONS AND USAGERisperidone is an atypical antipsychotic indicated for: Treatment of schizophrenia (1.1) As monotherapy or adjunctive therapy with lithium or valproate, for the treatment of acute manic or mixed episodes associated with Bipolar I Disorder (1.2) Treatment of irritability associated with autistic disorder (1.3) DOSAGE AND ADMINISTRATION Recommended daily dosage: Initial Dose Target Dose Effective Dose Range Schizophrenia: adults (2.1) 2 mg 4 to 8 mg 4 to 16 mg Schizophrenia: adolescents (2.1) 0.5 mg 3 mg 1 to 6 mg Bipolar mania: Adults (2.2) 2 to 3 mg 1 to 6 mg 1 to 6 mg Bipolar mania: in children and adolescents (2.2) 0.5 mg 1 to 2.5 mg 1 to 6 mg Irritability associated with autistic disorder (2.3) 0.25 mg (Weight < 20 kg) 0.5 mg (Weight ≥20 kg) 0.5 mg (5% and twice placebo) were parkinsonism, akathisia, dystonia, tremor, sedation, dizziness, anxiety, blurred vision, nausea, vomiting, upper abdominal pain, stomach discomfort, dyspepsia, diarrhea, salivary hypersecretion, constipation, dry mouth, increased appetite, increased weight, fatigue, rash, nasal congestion, upper respiratory tract infection, nasopharyngitis, and pharyngolaryngeal pain. (6) To report SUSPECTED ADVERSE REACTIONS, contact Aurobindo Pharma USA, Inc. at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONS Carbamazepine and other enzyme inducers decrease plasma concentrations of risperidone. Increase the risperidone dose up to double the patient's usual dose. Titrate slowly. (7.1) Fluoxetine, paroxetine, and other CYP 2D6 enzyme inhibitors increase plasma concentrations of risperidone. Reduce the initial dose. Do not exceed a final dose of 8 mg per day of risperidone. (7.1) USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, may cause fetal harm. (8.1) Nursing Mothers: Discontinue drug or nursing, taking into consideration the importance of drug to the mother. (8.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
- 1 RISPERIDONE INDICATIONS AND USAGE
- 2 RISPERIDONE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 RISPERIDONE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
- 5.2 Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with Dementia-Related Psychosis
- 5.3 Neuroleptic Malignant Syndrome
- 5.4 Tardive Dyskinesia
- 5.5 Metabolic Changes
- 5.6 Hyperprolactinemia
- 5.7 Orthostatic Hypotension
- 5.8 Leukopenia, Neutropenia, and Agranulocytosis
- 5.9 Potential for Cognitive and Motor Impairment
- 5.10 Seizures
- 5.11 Dysphagia
- 5.12 Priapism
- 5.13 Body Temperature Regulation
- 6 RISPERIDONE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 RISPERIDONE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
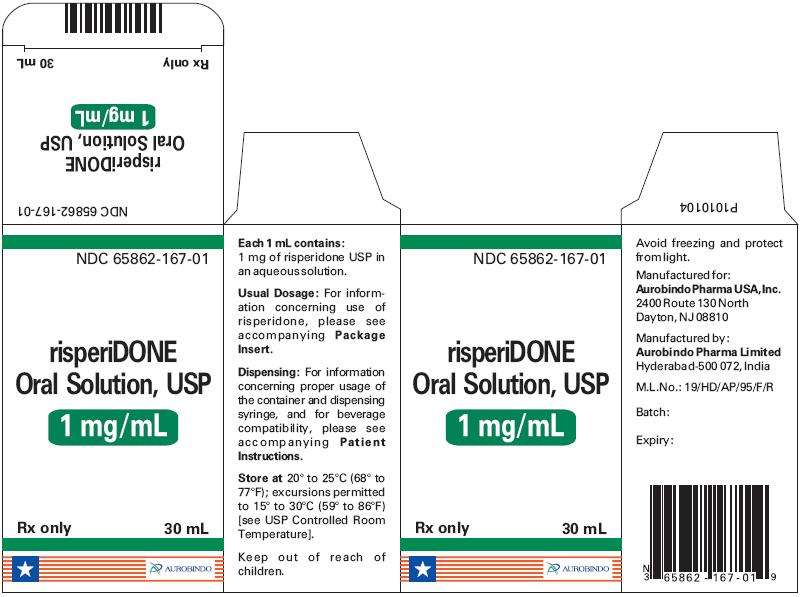
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 30 mL Container Label
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 30 mL Carton Label
FULL PRESCRIBING INFORMATION
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone is not approved for the treatment of patients with dementia-related psychosis. [See Warnings and Precautions (5.1).]
1 INDICATIONS AND USAGE
1.1 Schizophrenia
Risperidone oral solution, USP is indicated for the treatment of schizophrenia. Efficacy was established in 4 short-term trials in adults, 2 short-term trials in adolescents (ages 13 to 17 years), and one long-term maintenance trial in adults [see Clinical Studies (14.1)].
1.2 Bipolar Mania
Monotherapy
Risperidone oral solution, USP is indicated for the treatment of acute manic or mixed episodes associated with Bipolar I Disorder. Efficacy was established in 2 short-term trials in adults and one short-term trial in children and adolescents (ages 10 to 17 years) [see Clinical Studies (14.2)].
Adjunctive Therapy
Risperidone oral solution, USP adjunctive therapy with lithium or valproate is indicated for the treatment of acute manic or mixed episodes associated with Bipolar I Disorder. Efficacy was established in one short-term trial in adults [see Clinical Studies (14.3)].
1.3 Irritability Associated with Autistic Disorder
Risperidone oral solution, USP is indicated for the treatment of irritability associated with autistic disorder, including symptoms of aggression towards others, deliberate self-injuriousness, temper tantrums, and quickly changing moods. Efficacy was established in 3 short-term trials in children and adolescents (ages 5 to 17 years) [see Clinical Studies (14.4)].
2 DOSAGE AND ADMINISTRATION
| Initial Dose | Titration (Increments) |
Target Dose | Effective Dose Range |
|
|---|---|---|---|---|
|
Schizophrenia: adults (2.1)
|
2 mg |
1 to 2 mg |
4 to 8 mg |
4 to 16 mg |
|
Schizophrenia:
adolescents (2.2) |
0.5 mg |
0.5 to 1 mg |
3 mg |
1 to 6 mg |
|
Bipolar mania: adults (2.2)
|
2 to 3 mg |
1 mg |
1 to 6 mg |
1 to 6 mg |
|
Bipolar mania:
children and adolescents (2.2) |
0.5 mg |
0.5 to 1 mg |
1 to 2.5 mg |
1 to 6 mg |
|
Irritability in autistic disorder (2.3)
|
0.25 mg Can increase to 0.5 mg by Day 4: (body weight less than 20 kg) 0.5 mg Can increase to 1 mg by Day 4: (body weight greater than or equal to 20 kg) |
After Day 4, at intervals of > 2 weeks: 0.25 mg (body weight less than 20 kg) 0.5 mg (body weight greater than or equal to 20 kg) |
0.5 mg: (body weight less than 20 kg) 1 mg: (body weight greater than or equal to 20 kg) |
0.5 to 3 mg |
Severe Renal and Hepatic Impairment in Adults: use a lower starting dose of 0.5 mg twice daily. May increase to dosages above 1.5 mg twice daily at intervals of one week or longer
2.1 Schizophrenia
Adults
Usual Initial Dose
Risperidone oral solution can be administered once or twice daily. Initial dosing is 2 mg per day. May increase the dose at intervals of 24 hours or greater, in increments of 1 to 2 mg per day, as tolerated, to a recommended dose of 4 to 8 mg per day. In some patients, slower titration may be appropriate. Efficacy has been demonstrated in a range of 4 mg to 16 mg per day. However, doses above 6 mg per day for twice daily dosing were not demonstrated to be more efficacious than lower doses, were associated with more extrapyramidal symptoms and other adverse effects, and are generally not recommended. In a single study supporting once-daily dosing, the efficacy results were generally stronger for 8 mg than for 4 mg. The safety of doses above 16 mg per day has not been evaluated in clinical trials [see Clinical Studies (14.1)].
Adolescents
The initial dose is 0.5 mg once daily, administered as a single-daily dose in the morning or evening. The dose may be adjusted at intervals of 24 hours or greater, in increments of 0.5 mg or 1 mg per day, as tolerated, to a recommended dose of 3 mg per day. Although efficacy has been demonstrated in studies of adolescent patients with schizophrenia at doses between 1 mg to 6 mg per day, no additional benefit was observed above 3 mg per day, and higher doses were associated with more adverse events. Doses higher than 6 mg per day have not been studied.
Patients experiencing persistent somnolence may benefit from administering half the daily dose twice daily.
Maintenance Therapy
While it is unknown how long a patient with schizophrenia should remain on risperidone oral solution, the effectiveness of risperidone oral solution 2 mg per day to 8 mg per day at delaying relapse was demonstrated in a controlled trial in adult patients who had been clinically stable for at least 4 weeks and were then followed for a period of 1 to 2 years [see Clinical Studies (14.1)]. Both adult and adolescent patients who respond acutely should generally be maintained on their effective dose beyond the acute episode. Patients should be periodically reassessed to determine the need for maintenance treatment.
Reinitiation of Treatment in Patients Previously Discontinued
Although there are no data to specifically address reinitiation of treatment, it is recommended that after an interval off risperidone oral solution, the initial titration schedule should be followed.
Switching From Other Antipsychotics
There are no systematically collected data to specifically address switching schizophrenic patients from other antipsychotics to risperidone oral solution, or treating patients with concomitant antipsychotics.
2.2 Bipolar Mania
Usual Dose
Adults
The initial dose range is 2 mg to 3 mg per day. The dose may be adjusted at intervals of 24 hours or greater, in increments of 1 mg per day. The effective dose range is 1 mg to 6 mg per day, as studied in the short-term, placebo-controlled trials. In these trials, short-term (3 week) anti-manic efficacy was demonstrated in a flexible dosage range of 1 mg to 6 mg per day [see Clinical Studies (14.2
,
14.3)]. Risperidone oral solution doses higher than 6 mg per day were not studied.
Pediatrics
The initial dose is 0.5 mg once daily, administered as a single-daily dose in the morning or evening. The dose may be adjusted at intervals of 24 hours or greater, in increments of 0.5 mg or 1 mg per day, as tolerated, to the recommended target dose of 1 mg to 2.5 mg per day. Although efficacy has been demonstrated in studies of pediatric patients with bipolar mania at doses between 0.5 mg and 6 mg per day, no additional benefit was observed above 2.5 mg per day, and higher doses were associated with more adverse events. Doses higher than 6 mg per day have not been studied.
Patients experiencing persistent somnolence may benefit from administering half the daily dose twice daily.
Maintenance Therapy
There is no body of evidence available from controlled trials to guide a clinician in the longer-term management of a patient who improves during treatment of an acute manic episode with risperidone oral solution. While it is generally agreed that pharmacological treatment beyond an acute response in mania is desirable, both for maintenance of the initial response and for prevention of new manic episodes, there are no systematically obtained data to support the use of risperidone oral solution in such longer-term treatment (i.e., beyond 3 weeks). The physician who elects to use risperidone oral solution for extended periods should periodically re-evaluate the long-term risks and benefits of the drug for the individual patient.
2.3 Irritability Associated with Autistic Disorder - Pediatrics (Children and Adolescents)
The dosage of risperidone oral solution should be individualized according to the response and tolerability of the patient. The total daily dose of risperidone oral solution can be administered once daily, or half the total daily dose can be administered twice daily.
For patients with body weight less than 20 kg, initiate dosing at 0.25 mg per day. For patients with body weight greater than or equal to 20 kg, initiate dosing at 0.5 mg per day. After a minimum of four days, the dose may be increased to the recommended dose of 0.5 mg per day for patients less than 20 kg and 1 mg per day for patients greater than or equal to 20 kg. Maintain this dose for a minimum of 14 days. In patients not achieving sufficient clinical response, the dose may be increased at intervals of 2 weeks or greater, in increments of 0.25 mg per day for patients less than 20 kg, or increments of 0.5 mg per day for patients greater than or equal to 20 kg. The effective dose range is 0.5 mg to 3 mg per day. No dosing data are available for children who weigh less than 15 kg.
Once sufficient clinical response has been achieved and maintained, consider gradually lowering the dose to achieve the optimal balance of efficacy and safety. The physician who elects to use risperidone oral solution for extended periods should periodically re-evaluate the long-term risks and benefits of the drug for the individual patient.
Patients experiencing persistent somnolence may benefit from a once-daily dose administered at bedtime or administering half the daily dose twice daily, or a reduction of the dose.
2.4 Dosing in Patients with Severe Renal or Hepatic Impairment
For patients with severe renal impairment (CLcr < 30 mL/min) or hepatic impairment (10 to 15 points on Child Pugh System), the initial starting dose is 0.5 mg twice daily. The dose may be increased in increments of 0.5 mg or less, administered twice daily. For doses above 1.5 mg twice daily, increase in intervals of one week or greater [see Use in Specific Populations (8.6 and 8.7)].
2.5 Dose Adjustments for Specific Drug Interactions
When risperidone oral solution is co-administered with enzyme inducers (e.g., carbamazepine), the dose of risperidone oral solution should be increased up to double the patient's usual dose. It may be necessary to decrease the risperidone oral solution dose when enzyme inducers such as carbamazepine are discontinued [see Drug Interactions (7.1)]. Similar effect may be expected with co-administration of risperidone oral solution with other enzyme inducers (e.g., phenytoin, rifampin, and phenobarbital).
When fluoxetine or paroxetine is co-administered with risperidone oral solution, the dose of risperidone oral solution should be reduced. The risperidone oral solution dose should not exceed 8 mg per day in adults when co-administered with these drugs. When initiating therapy, risperidone oral solution should be titrated slowly. It may be necessary to increase the risperidone oral solution dose when enzyme inhibitors such as fluoxetine or paroxetine are discontinued [see Drug Interactions (7.1)].
2.6 Administration of Risperidone Oral Solution
Risperidone
oral solution can be administered directly from the
dispensing syringe, or can be mixed with a beverage prior to administration. Risperidone
oral solution is compatible in the following beverages: water, coffee, orange juice, and low-fat milk; it is NOT compatible with either cola or tea.
3 DOSAGE FORMS AND STRENGTHS
Risperidone oral solution is available in a 1 mg/mL strength.
4 CONTRAINDICATIONS
Risperidone oral solution is contraindicated in patients with a known hypersensitivity to risperidone. Hypersensitivity reactions, including anaphylactic reactions and angioedema, have been observed in patients treated with risperidone.
5 WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear.
In two of four placebo-controlled trials in elderly patients with dementia-related psychosis, a higher incidence of mortality was observed in patients treated with furosemide plus risperidone when compared to patients treated with risperidone alone or with placebo plus furosemide. No pathological mechanism has been identified to explain this finding, and no consistent pattern for cause of death was observed.
Risperidone is not approved for the treatment of dementia-related psychosis [see Boxed Warning].
5.2 Cerebrovascular Side Effects, Including Stroke, in Elderly Patients with Dementia-Related Psychosis
Cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack), including fatalities, were reported in patients (mean age 85 years; range 73 to 97) in trials of risperidone in elderly patients with dementia-related psychosis. In placebo-controlled trials, there was a significantly higher incidence of cerebrovascular adverse events in patients treated with risperidone compared to patients treated with placebo. Risperidone is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions (5.1)].
5.3 Neuroleptic Malignant Syndrome
Antipsychotic drugs including risperidone can cause a potentially fatal symptom complex referred to as Neuroleptic Malignant Syndrome (NMS). Clinical manifestations of NMS include hyperpyrexia, muscle rigidity, altered mental status, and autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase (CPK), myoglobinuria, rhabdomyolysis, and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases in which the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system pathology.
The management of NMS should include: (1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; (2) intensive symptomatic treatment and medical monitoring; and (3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
5.4 Tardive Dyskinesia
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. The risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, prescribe risperidone in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that: (1) is known to respond to antipsychotic drugs, and (2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient treated with risperidone, consider drug discontinuation. However, some patients may require treatment with risperidone despite the presence of the syndrome.
5.5 Metabolic Changes
Atypical antipsychotic drugs have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include hyperglycemia, dyslipidemia, and body weight gain. While all of the drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia and Diabetes Mellitus
Hyperglycemia and diabetes mellitus, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, have been reported in patients treated with atypical antipsychotics including risperidone. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of treatment-emergent hyperglycemia-related adverse events in patients treated with the atypical antipsychotics. Precise risk estimates for hyperglycemia-related adverse events in patients treated with atypical antipsychotics are not available.
Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics, including risperidone, should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics, including risperidone, should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics, including risperidone, should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics, including risperidone, should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic, including risperidone, was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of risperidone.
Pooled data from three double-blind, placebo-controlled schizophrenia studies and four double-blind, placebo-controlled bipolar monotherapy studies are presented in Table 2.
| Risperidone
|
|||
| Placebo
|
1 to 8 mg/day
|
>8 to 16 mg/day
|
|
|
Mean change from baseline (mg/dL)
|
|||
|
n=555
|
n=748
|
n=164
|
|
| Serum Glucose
|
-1.4
|
0.8
|
0.6
|
|
Proportion of patients with shifts
|
|||
| Serum Glucose (<140 mg/dL to ≥200 mg/dL) |
0.6% (3/525) |
0.4% (3/702) |
0% (0/158) |
In longer-term, controlled and uncontrolled studies, risperidone was associated with a mean change in glucose of +2.8 mg/dL at Week 24 (n=151) and +4.1 mg/dL at Week 48 (n=50).
Data from the placebo-controlled 3- to 6-week study in children and adolescents with schizophrenia (13 to 17 years of age), bipolar mania (10 to 17 years of age), or autistic disorder (5 to 17 years of age) are presented in Table 3.
| Risperidone
|
||
| Placebo
|
0.5 to 6 mg/day
|
|
|
Mean change from baseline (mg/dL)
|
||
|
n=76
|
n=135
|
|
| Serum Glucose
|
-1.3
|
2.6
|
|
Proportion of patients with shifts
|
||
| Serum Glucose (<100 mg/dL to ≥126 mg/dL) |
0% (0/64) |
0.8% (1/120) |
In longer-term, uncontrolled, open-label extension pediatric studies, risperidone was associated with a mean change in fasting glucose of +5.2 mg/dL at Week 24 (n=119).
Dyslipidemia
Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.
Pooled data from 7 placebo-controlled, 3- to 8-week, fixed- or flexible-dose studies in adult subjects with schizophrenia or bipolar mania are presented in Table 4.
| Risperidone
|
|||
| Placebo
|
1 to 8 mg/day
|
>8 to 16 mg/day
|
|
|
Mean change from baseline (mg/dL)
|
|||
|
Cholesterol
|
n=559
|
n=742
|
n=156
|
| Change from baseline
|
0.6
|
6.9
|
1.8
|
|
Triglycerides
|
n=183
|
n=307
|
n=123
|
| Change from baseline
|
-17.4
|
-4.9
|
-8.3
|
|
Proportion of patients With Shifts
|
|||
|
Cholesterol
|
2.7%
|
4.3%
|
6.3%
|
| (<200 mg/dL to ≥240 mg/dL)
|
(10/368)
|
(22/516)
|
(6/96)
|
|
Triglycerides
|
1.1% |
2.7% |
2.5% |
| (<500 mg/dL to ≥500 mg/dL)
|
(2/180)
|
(8/301)
|
(3/121)
|
In longer-term, controlled and uncontrolled studies, risperidone was associated with a mean change in (a) non-fasting cholesterol of +4.4 mg/dL at Week 24 (n=231) and +5.5 mg/dL at Week 48 (n=86); and (b) non-fasting triglycerides of +19.9 mg/dL at Week 24 (n=52).
Pooled data from 3 placebo-controlled, 3- to 6-week, fixed-dose studies in children and adolescents with schizophrenia (13 to 17 years of age), bipolar mania (10 to 17 years of age), or autistic disorder (5 to 17 years of age) are presented in Table 5.
| Placebo
|
Risperidone 0.5 to 6 mg/day |
|
|
Mean change from baseline (mg/dL)
|
||
|
Cholesterol
|
n=74
|
n=133
|
| Change from baseline
|
0.3
|
-0.3
|
|
LDL
|
n=22
|
n=22
|
| Change from baseline
|
3.7
|
0.5
|
|
HDL
|
n=22
|
n=22
|
| Change from baseline
|
1.6
|
-1.9
|
|
Triglycerides
|
n=77
|
n=138
|
| Change from baseline |
-9
|
-2.6
|
| |
Proportion of patients with shifts
|
|
|
Cholesterol
|
2.4%
|
3.8%
|
| (<170 mg/dL to ≥200 mg/dL) |
(1/42)
|
(3/80)
|
|
LDL
|
0%
|
0%
|
| (<110 mg/dL to ≥130 mg/dL) |
(0/16)
|
(0/16)
|
|
HDL
|
0%
|
10%
|
| (≥40 mg/dL to <40 mg/dL)
|
(0/19)
|
(2/20)
|
|
Triglycerides
|
1.5%
|
7.1%
|
| (<150 mg/dL to ≥200 mg/dL)
|
(1/65)
|
(8/113)
|
In longer-term, uncontrolled, open-label extension pediatric studies, risperidone was associated with a mean change in (a) fasting cholesterol of +2.1 mg/dL at Week 24 (n=114); (b) fasting LDL of -0.2 mg/dL at Week 24 (n=103); (c) fasting HDL of +0.4 mg/dL at Week 24 (n=103); and (d) fasting triglycerides of +6.8 mg/dL at Week 24 (n=120).
Weight Gain
Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Data on mean changes in body weight and the proportion of subjects meeting a weight gain criterion of 7% or greater of body weight from 7 placebo-controlled, 3- to 8-week, fixed- or flexible-dose studies in adult subjects with schizophrenia or bipolar mania are presented in Table 6.
| Risperidone
|
|||
| Placebo (n=597) |
1 to 8 mg/day (n=769) |
>8 to 16 mg/day (n=158) |
|
|
Weight (kg)
|
|||
| Change from baseline
|
-0.3
|
0.7
|
2.2
|
|
Weight Gain
|
|||
| ≥7% increase from baseline
|
2.9%
|
8.7%
|
20.9%
|
In longer-term, controlled and uncontrolled studies, risperidone was associated with a mean change in weight of +4.3 kg at Week 24 (n=395) and +5.3 kg at Week 48 (n=203).
Data on mean changes in body weight and the proportion of subjects meeting the criterion of ≥7% gain in body weight from nine placebo-controlled, 3- to 8-week, fixed-dose studies in children and adolescents with schizophrenia (13 to 17 years of age), bipolar mania (10 to 17 years of age), autistic disorder (5 to 17 years of age), or other psychiatric disorders (5 to 17 years of age) are presented in Table 7.
| |
Placebo
(n=375) |
Risperidone
0.5 to 6 mg/day (n=448) |
|
Weight (kg)
|
|
|
| Change from baseline |
0.6 |
2 |
|
Weight Gain
|
|
|
| ≥7% increase from baseline |
6.9% |
32.6% |
In longer-term, uncontrolled, open-label extension pediatric studies, risperidone was associated with a mean change in weight of +5.5 kg at Week 24 (n=748) and +8 kg at Week 48 (n=242).
In a long-term, open-label extension study in adolescent patients with schizophrenia, weight increase was reported as a treatment-emergent adverse event in 14% of patients. In 103 adolescent patients with schizophrenia, a mean increase of 9 kg was observed after 8 months of risperidone treatment. The majority of that increase was observed within the first 6 months. The average percentiles at baseline and 8 months, respectively, were 56 and 72 for weight, 55 and 58 for height, and 51 and 71 for body mass index.
In long-term, open-label trials (studies in patients with autistic disorder or other psychiatric disorders), a mean increase of 7.5 kg after 12 months of risperidone treatment was observed, which was higher than the expected normal weight gain (approximately 3 to 3.5 kg per year adjusted for age, based on Centers for Disease Control and Prevention normative data). The majority of that increase occurred within the first 6 months of exposure to risperidone. The average percentiles at baseline and 12 months, respectively, were 49 and 60 for weight, 48 and 53 for height, and 50 and 62 for body mass index.
In one 3-week, placebo-controlled trial in children and adolescent patients with acute manic or mixed episodes of bipolar I disorder, increases in body weight were higher in the risperidone
groups than the placebo group, but not dose related (1.9 kg in the risperidone 0.5 to 2.5 mg group, 1.44 kg in the risperidone 3 to 6 mg group, and 0.65 kg in the placebo group). A similar trend was observed in the mean change from baseline in body mass index.
When treating pediatric patients with risperidone for any indication, weight gain should be assessed against that expected with normal growth.
5.6 Hyperprolactinemia
As with other drugs that antagonize dopamine D2 receptors, risperidone elevates prolactin levels and the elevation persists during chronic administration. Risperidone is associated with higher levels of prolactin elevation than other antipsychotic agents.
Hyperprolactinemia may suppress hypothalamic GnRH, resulting in reduced pituitary gonadotropin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds. Long-standing hyperprolactinemia when associated with hypogonadism may lead to decreased bone density in both female and male subjects.
Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin dependent in vitro, a factor of potential importance if the prescription of these drugs is contemplated in a patient with previously detected breast cancer. An increase in pituitary gland, mammary gland, and pancreatic islet cell neoplasia (mammary adenocarcinomas, pituitary and pancreatic adenomas) was observed in the risperidone carcinogenicity studies conducted in mice and rats [see Nonclinical Toxicology (13.1)]. Neither clinical studies nor epidemiologic studies conducted to date have shown an association between chronic administration of this class of drugs and tumorigenesis in humans; the available evidence is considered too limited to be conclusive at this time.
5.7 Orthostatic Hypotension
Risperidone may induce orthostatic hypotension associated with dizziness, tachycardia, and in some patients, syncope, especially during the initial dose-titration period, probably reflecting its alpha-adrenergic antagonistic properties. Syncope was reported in 0.2% (6/2607) of risperidone-treated patients in Phase 2 and 3 studies in adults with schizophrenia. The risk of orthostatic hypotension and syncope may be minimized by limiting the initial dose to 2 mg total (either once daily or 1 mg twice daily) in normal adults and 0.5 mg twice daily in the elderly and patients with renal or hepatic impairment [see Dosage and Administration (2.1, 2.4)]. Monitoring of orthostatic vital signs should be considered in patients for whom this is of concern. A dose reduction should be considered if hypotension occurs. Risperidone should be used with particular caution in patients with known cardiovascular disease (history of myocardial infarction or ischemia, heart failure, or conduction abnormalities), cerebrovascular disease, and conditions which would predispose patients to hypotension, e.g., dehydration and hypovolemia. Clinically significant hypotension has been observed with concomitant use of risperidone and antihypertensive medication.
5.8 Leukopenia, Neutropenia, and Agranulocytosis
Class Effect: In clinical trial and/or postmarketing experience, events of leukopenia/neutropenia have been reported temporally related to antipsychotic agents, including risperidone. Agranulocytosis has also been reported.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of risperidone should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1000/mm3) should discontinue risperidone and have their WBC followed until recovery.
5.9 Potential for Cognitive and Motor Impairment
Somnolence was a commonly reported adverse reaction associated with risperidone treatment, especially when ascertained by direct questioning of patients. This adverse reaction is dose-related, and in a study utilizing a checklist to detect adverse events, 41% of the high-dose patients (risperidone 16 mg/day) reported somnolence compared to 16% of placebo patients. Direct questioning is more sensitive for detecting adverse events than spontaneous reporting, by which 8% of risperidone 16 mg/day patients and 1% of placebo patients reported somnolence as an adverse reaction. Since risperidone has the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that risperidone therapy does not affect them adversely.
5.10 Seizures
During premarketing testing in adult patients with schizophrenia, seizures occurred in 0.3% (9/2607) of risperidone-treated patients, two in association with hyponatremia. Risperidone should be used cautiously in patients with a history of seizures.
5.11 Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use. Aspiration pneumonia is a common cause of morbidity and mortality in patients with advanced Alzheimer's dementia. Risperidone and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia [see Boxed Warning and Warnings and Precautions (5.1)].
5.12 Priapism
Priapism has been reported during postmarketing surveillance. Severe priapism may require surgical intervention.
5.13 Body Temperature Regulation
Disruption of body temperature regulation has been attributed to antipsychotic agents. Both hyperthermia and hypothermia have been reported in association with oral risperidone use. Caution is advised when prescribing for patients who will be exposed to temperature extremes.
6 ADVERSE REACTIONS
The following are discussed in more detail in other sections of the labeling:
- Increased mortality in elderly patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions (5.1)]
- Cerebrovascular adverse events, including stroke, in elderly patients with dementia-related psychosis [see Warnings and Precautions (5.2)]
- Neuroleptic malignant syndrome [see Warnings and Precautions (5.3)]
- Tardive dyskinesia [see Warnings and Precautions (5.4)]
- Metabolic Changes (Hyperglycemia and diabetes mellitus, Dyslipidemia, and Weight Gain) [see Warnings and Precautions (5.5)]
- Hyperprolactinemia [see Warnings and Precautions (5.6)]
- Orthostatic hypotension [see Warnings and Precautions (5.7)]
- Leukopenia, neutropenia, and agranulocytosis [see Warnings and Precautions (5.8)]
- Potential for cognitive and motor impairment [see Warnings and Precautions (5.9)]
- Seizures [see Warnings and Precautions (5.10)]
- Dysphagia [see Warnings and Precautions (5.11)]
- Priapism [see Warnings and Precautions (5.12)]
- Disruption of body temperature regulation [see Warnings and Precautions (5.13)]
The most common adverse reactions in clinical trials (>5% and twice placebo) were parkinsonism, akathisia, dystonia, tremor, sedation, dizziness, anxiety, blurred vision, nausea, vomiting, upper abdominal pain, stomach discomfort, dyspepsia, diarrhea, salivary hypersecretion, constipation, dry mouth, increased appetite, increased weight, fatigue, rash, nasal congestion, upper respiratory tract infection, nasopharyngitis, and pharyngolaryngeal pain.
The most common adverse reactions that were associated with discontinuation from clinical trials (causing discontinuation in >1% of adults and/or >2% of pediatrics) were nausea, somnolence, sedation, vomiting, dizziness, and akathisia [see Adverse Reactions, Discontinuations Due to Adverse Reactions (6.1)].
The data described in this section are derived from a clinical trial database consisting of 9803 adult and pediatric patients exposed to one or more doses of risperidone for the treatment of schizophrenia, bipolar mania, autistic disorder, and other psychiatric disorders in pediatrics and elderly patients with dementia. Of these 9803 patients, 2687 were patients who received risperidone while participating in double-blind, placebo-controlled trials. The conditions and duration of treatment with risperidone varied greatly and included (in overlapping categories) double-blind, fixed- and flexible-dose, placebo- or active-controlled studies and open-label phases of studies, inpatients and outpatients, and short-term (up to 12 weeks) and longer-term (up to 3 years) exposures. Safety was assessed by collecting adverse events and performing physical examinations, vital signs, body weights, laboratory analyses, and ECGs.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials - Schizophrenia
Adult Patients with Schizophrenia
Table 8 lists the adverse reactions reported in 2% or more of risperidone-treated adult patients with schizophrenia in three 4- to 8-week, double-blind, placebo-controlled trials.
| * Parkinsonism includes extrapyramidal disorder, musculoskeletal stiffness, parkinsonism, cogwheel rigidity, akinesia, bradykinesia, hypokinesia, masked facies, muscle rigidity, and Parkinson's disease. Akathisia includes akathisia and restlessness. Dystonia includes dystonia, muscle spasms, muscle contractions involuntary, muscle contracture, oculogyration, tongue paralysis. Tremor includes tremor and parkinsonian rest tremor. |
|||
|
System/Organ Class
Adverse Reaction |
Percentage of Patients Reporting Reaction
|
||
|
Risperidone
|
|
||
|
2 to 8 mg
per day (N=366) |
>8 to 16 mg
per day (N=198) |
Placebo
(N=225) |
|
|
Cardiac Disorders
|
|
|
|
| Tachycardia |
1 |
3 |
0 |
|
Eye Disorders
|
|
|
|
| Vision blurred |
3 |
1 |
1 |
|
Gastrointestinal Disorders
|
|
|
|
| Nausea |
9 |
4 |
4 |
| Constipation |
8 |
9 |
6 |
| Dyspepsia |
8 |
6 |
5 |
| Dry mouth |
4 |
0 |
1 |
| Abdominal discomfort |
3 |
1 |
1 |
| Salivary hypersecretion |
2 |
1 |
<1 |
| Diarrhea |
2 |
1 |
1 |
|
General Disorders
|
|
|
|
| Fatigue |
3 |
1 |
0 |
| Chest pain |
2 |
2 |
1 |
| Asthenia |
2 |
1 |
<1 |
|
Infections and Infestations
|
|
|
|
| Nasopharyngitis |
3 |
4 |
3 |
| Upper respiratory tract infection |
2 |
3 |
1 |
| Sinusitis |
1 |
2 |
1 |
| Urinary tract infection |
1 |
3 |
0 |
|
Investigations
|
|
|
|
| Blood creatine phosphokinase increased |
1 |
2 |
<1 |
| Heart rate increased |
<1 |
2 |
0 |
|
Musculoskeletal and Connective Tissue Disorders
|
|
|
|
| Back pain |
4 |
1 |
1 |
| Arthralgia |
2 |
3 |
<1 |
| Pain in extremity |
2 |
1 |
1 |
|
Nervous System Disorders
|
|
|
|
| Parkinsonism*
|
14 |
17 |
8 |
| Akathisia*
|
10 |
10 |
3 |
| Sedation
|
10 |
5 |
2 |
| Dizziness
|
7 |
4 |
2 |
| Dystonia*
|
3 |
4 |
2 |
| Tremor*
|
2 |
3 |
1 |
| Dizziness postural
|
2 |
0 |
0 |
|
Psychiatric Disorders
|
|
|
|
| Insomnia
|
32 |
25 |
27 |
| Anxiety
|
16 |
11 |
11 |
|
Respiratory, Thoracic and Mediastinal Disorders
|
|
|
|
| Nasal congestion
|
5 |
6 |
2 |
| Dyspnea
|
1 |
2 |
0 |
| Epistaxis
|
<1 |
2 |
0 |
|
Skin and Subcutaneous Tissue Disorders
|
|
|
|
| Rash
|
1 |
4 |
1 |
| Dry skin
|
1 |
3 |
0 |
|
Vascular Disorders
|
|
|
|
| Orthostatic hypotension
|
2 |
1 |
0 |
Pediatric Patients with Schizophrenia
Table 9 lists the adverse reactions reported in 5% or more of risperidone-treated pediatric patients with schizophrenia in a 6-week double-blind, placebo-controlled trial.
| * Parkinsonism includes extrapyramidal disorder, muscle rigidity, musculoskeletal stiffness, and hypokinesia. Akathisia includes akathisia and restlessness. Dystonia includes dystonia and oculogyration. |
|||
|
System/Organ Class
Adverse Reaction |
Percentage of Patients Reporting Reaction
|
||
|
Risperidone
|
|
||
|
1 to 3 mg per day
(N=55) |
4 to 6 mg per day
(N=51) |
Placebo
(N=54) |
|
|
Gastrointestinal Disorders
|
|
|
|
| Salivary hypersecretion |
0 |
10 |
2 |
|
Nervous System Disorders
|
|
|
|
| Sedation |
24 |
12 |
4 |
| Parkinsonism* |
16 |
28 |
11 |
| Tremor |
11 |
10 |
6 |
| Akathisia* |
9 |
10 |
4 |
| Dizziness |
7 |
14 |
2 |
| Dystonia* |
2 |
6 |
0 |
|
Psychiatric Disorders
|
|
|
|
| Anxiety
|
7 |
6 |
0 |
Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials - Bipolar Mania
Adult Patients with Bipolar Mania
Table 10 lists the adverse reactions reported in 2% or more of risperidone-treated adult patients with bipolar mania in four 3-week, double-blind, placebo-controlled monotherapy trials.
| * Parkinsonism includes extrapyramidal disorder, parkinsonism, musculoskeletal stiffness, hypokinesia, muscle rigidity, muscle tightness, bradykinesia, cogwheel rigidity. Akathisia includes akathisia and restlessness. Tremor includes tremor and parkinsonian rest tremor. Dystonia includes dystonia, muscle spasms, oculogyration, torticollis. |
||
|
System/Organ Class
Adverse Reaction |
Percentage of Patients Reporting Reaction
|
|
|
Risperidone
1 to 6 mg per day (N=448) |
Placebo
(N=424) |
|
|
Eye Disorders
|
|
|
| Vision blurred |
2 |
1 |
|
Gastrointestinal Disorders
|
|
|
| Nausea |
5 |
2 |
| Diarrhea |
3 |
2 |
| Salivary hypersecretion |
3 |
1 |
| Stomach discomfort |
2 |
<1 |
|
General Disorders
|
|
|
| Fatigue |
2 |
1 |
|
Nervous System Disorders
|
|
|
| Parkinsonism* |
25 |
9 |
| Sedation |
11 |
4 |
| Akathisia* |
9 |
3 |
| Tremor* |
6 |
3 |
| Dizziness |
6 |
5 |
| Dystonia* |
5 |
1 |
| Lethargy |
2 |
1 |
Table 11 lists the adverse reactions reported in 2% or more of risperidone-treated adult patients with bipolar mania in two 3-week, double-blind, placebo-controlled adjuvant therapy trials.
| * Parkinsonism includes extrapyramidal disorder, hypokinesia and bradykinesia. Akathisia includes hyperkinesia and akathisia. |
||
|
System/Organ Class
Adverse Reaction |
Percentage of Patients Reporting Reaction
|
|
|
Risperidone +
Mood Stabilizer (N=127) |
Placebo +
Mood Stabilizer (N=126) |
|
|
Cardiac Disorders
|
|
|
| Palpitations |
2 |
0 |
|
Gastrointestinal Disorders
|
|
|
| Dyspepsia |
9 |
8 |
| Nausea |
6 |
4 |
| Diarrhea |
6 |
4 |
| Salivary hypersecretion |
2 |
0 |
|
General Disorders
|
|
|
| Chest pain |
2 |
1 |
|
Infections and Infestations
|
|
|
| Urinary tract infection |
2 |
1 |
|
Nervous System Disorders
|
|
|
| Parkinsonism* |
14 |
4 |
| Sedation |
9 |
4 |
| Akathisia* |
8 |
0 |
| Dizziness |
7 |
2 |
| Tremor |
6 |
2 |
| Lethargy |
2 |
1 |
|
Psychiatric Disorders
|
|
|
| Anxiety |
3 |
2 |
|
Respiratory, Thoracic and Mediastinal Disorders
|
|
|
| Pharyngolaryngeal pain |
5 |
2 |
| Cough |
2 |
0 |
Pediatric Patients with Bipolar Mania
Table 12 lists the adverse reactions reported in 5% or more of risperidone-treated pediatric patients with bipolar mania in a 3-week double-blind, placebo-controlled trial.
| * Parkinsonism includes musculoskeletal stiffness, extrapyramidal disorder, bradykinesia, and nuchal rigidity. Dystonia includes dystonia, laryngospasm, and muscle spasms. Akathisia includes restlessness and akathisia. |
|||
|
System/Organ Class
Adverse Reaction |
Percentage of Patients Reporting Reaction
|
||
|
Risperidone
|
|||
|
0.5 to 2.5 mg
per day (N=50) |
3 to 6 mg
per day (N=61) |
Placebo
(N=58) |
|
|
Eye Disorders
|
|||
| Vision blurred
|
4 |
7 |
0 |
|
Gastrointestinal Disorders
|
|
|
|
| Abdominal pain upper
|
16 |
13 |
5 |
| Nausea
|
16 |
13 |
7 |
| Vomiting
|
10 |
10 |
5 |
| Diarrhea
|
8 |
7 |
2 |
| Dyspepsia
|
10 |
3 |
2 |
| Stomach discomfort
|
6 |
0 |
2 |
|
General Disorders
|
|
|
|
| Fatigue
|
18 |
30 |
3 |
|
Metabolism and Nutrition Disorders
|
|
|
|
| Increased appetite
|
4 |
7 |
2 |
|
Nervous System Disorders
|
|
|
|
| Sedation
|
42 |
56 |
19 |
| Dizziness
|
16 |
13 |
5 |
| Parkinsonism*
|
6 |
12 |
3 |
| Dystonia*
|
6 |
5 |
0 |
| Akathisia*
|
0 |
8 |
2 |
|
Psychiatric Disorders
|
|
|
|
| Anxiety
|
0 |
8 |
3 |
|
Respiratory, Thoracic and Mediastinal Disorders
|
|
|
|
| Pharyngolaryngeal pain
|
10 |
3 |
5 |
|
Skin and Subcutaneous Tissue Disorders
|
|
|
|
| Rash
|
0 |
7 |
2 |
Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials - Autistic Disorder
Table 13 lists the adverse reactions reported in 5% or more of risperidone-treated pediatric patients treated for irritability associated with autistic disorder in two 8-week, double-blind, placebo-controlled trials and one 6-week double-blind, placebo-controlled study.
| * Parkinsonism includes musculoskeletal stiffness, extrapyramidal disorder, muscle rigidity, cogwheel rigidity, and muscle tightness. |
||
|
System/Organ Class
Adverse Reaction |
Percentage of Patients Reporting Reaction
|
|
|
Risperidone
0.5 to 4 mg/day (N=107) |
Placebo
(N=115) |
|
|
Gastrointestinal Disorders
|
|
|
| Vomiting
|
20 |
17 |
| Constipation
|
17 |
6 |
| Dry mouth
|
10 |
4 |
| Nausea
|
8 |
5 |
| Salivary hypersecretion
|
7 |
1 |
|
General Disorders and Administration Site
Conditions
|
|
|
| Fatigue
|
31 |
9 |
| Pyrexia
|
16 |
13 |
| Thirst
|
7 |
4 |
|
Infections and Infestations
|
|
|
| Nasopharyngitis
|
19 |
9 |
| Rhinitis
|
9 |
7 |
| Upper respiratory tract infection
|
8 |
3 |
|
Investigations
|
|
|
| Weight increased
|
8 |
2 |
|
Metabolism and Nutrition Disorders
|
|
|
| Increased appetite
|
44 |
15 |
|
Nervous System Disorders
|
|
|
| Sedation
|
63 |
15 |
| Drooling
|
12 |
4 |
| Headache
|
12 |
10 |
| Tremor |
8 |
1 |
| Dizziness |
8 |
2 |
| Parkinsonism* |
8 |
1 |
|
Renal and Urinary Disorders
|
|
|
| Enuresis |
16 |
10 |
|
Respiratory, Thoracic and Mediastinal Disorders
|
|
|
| Cough |
17 |
12 |
| Rhinorrhea |
12 |
10 |
| Nasal congestion |
10 |
4 |
|
Skin and Subcutaneous Tissue Disorders
|
|
|
| Rash |
8 |
2 |
Other Adverse Reactions Observed During the Clinical Trial Evaluation of Risperidone
The following additional adverse reactions occurred across all placebo-controlled, active-controlled, and open-label studies of risperidone in adults and pediatric patients.
Blood and Lymphatic System Disorders: anemia, granulocytopenia, neutropenia
Cardiac Disorders: sinus bradycardia, sinus tachycardia, atrioventricular block first degree, bundle branch block left, bundle branch block right, atrioventricular block
Ear and Labyrinth Disorders: ear pain, tinnitus
Endocrine Disorders: hyperprolactinemia
Eye Disorders: ocular hyperemia, eye discharge, conjunctivitis, eye rolling, eyelid edema, eye swelling, eyelid margin crusting, dry eye, lacrimation increased, photophobia, glaucoma, visual acuity reduced
Gastrointestinal Disorders: dysphagia, fecaloma, fecal incontinence, gastritis, lip swelling, cheilitis, aptyalism
General Disorders: edema peripheral, thirst, gait disturbance, influenza-like illness, pitting edema, edema, chills, sluggishness, malaise, chest discomfort, face edema, discomfort, generalized edema, drug withdrawal syndrome, peripheral coldness, feeling abnormal
Immune System Disorders: drug hypersensitivity
Infections and Infestations: pneumonia, influenza, ear infection, viral infection, pharyngitis, tonsillitis, bronchitis, eye infection, localized infection, cystitis, cellulitis, otitis media, onychomycosis, acarodermatitis, bronchopneumonia, respiratory tract infection, tracheobronchitis, otitis media chronic
Investigations: body temperature increased, blood prolactin increased, alanine aminotransferase increased, electrocardiogram abnormal, eosinophil count increased, white blood cell count decreased, blood glucose increased, hemoglobin decreased, hematocrit decreased, body temperature decreased, blood pressure decreased, transaminases increased
Metabolism and Nutrition Disorders: decreased appetite, polydipsia, anorexia
Musculoskeletal and Connective Tissue Disorders: joint stiffness, joint swelling, musculoskeletal chest pain, posture abnormal, myalgia, neck pain, muscular weakness, rhabdomyolysis
Nervous System Disorders: balance disorder, disturbance in attention, dysarthria, unresponsive to stimuli, depressed level of consciousness, movement disorder, transient ischemic attack, coordination abnormal, cerebrovascular accident, speech disorder, syncope, loss of consciousness, hypoesthesia, tardive dyskinesia, dyskinesia, cerebral ischemia, cerebrovascular disorder, neuroleptic malignant syndrome, diabetic coma, head titubation
Psychiatric Disorders: agitation, blunted affect, confusional state, middle insomnia, nervousness, sleep disorder, listlessness, libido decreased, and anorgasmia
Renal and Urinary Disorders: enuresis, dysuria, pollakiuria, urinary incontinence
Reproductive System and Breast Disorders: menstruation irregular, amenorrhea, gynecomastia, galactorrhea, vaginal discharge, menstrual disorder, erectile dysfunction, retrograde ejaculation, ejaculation disorder, sexual dysfunction, breast enlargement
Respiratory, Thoracic, and Mediastinal Disorders: wheezing, pneumonia aspiration, sinus congestion, dysphonia, productive cough, pulmonary congestion, respiratory tract congestion, rales, respiratory disorder, hyperventilation, nasal edema
Skin and Subcutaneous Tissue Disorders: erythema, skin discoloration, skin lesion, pruritus, skin disorder, rash erythematous, rash papular, rash generalized, rash maculopapular, acne, hyperkeratosis, seborrheic dermatitis
Vascular Disorders: hypotension, flushing
Discontinuations Due to Adverse Reactions
Schizophrenia - Adults
Approximately 7% (39/564) of risperidone-treated patients in double-blind, placebo-controlled trials discontinued treatment due to an adverse reaction, compared with 4% (10/225) who were receiving placebo. The adverse reactions associated with discontinuation in 2 or more risperidone-treated patients were:
| Adverse Reaction | Risperidone | Placebo (N=225) |
|
|---|---|---|---|
| 2 to 8 mg/day (N=366) |
>8 to 16 mg/day (N=198) |
||
| Dizziness |
1.4% |
1% |
0% |
| Nausea |
1.4% |
0% |
0% |
| Vomiting |
0.8% |
0% |
0% |
| Parkinsonism |
0.8% |
0% |
0% |
| Somnolence |
0.8% |
0% |
0% |
| Dystonia |
0.5% |
0% |
0% |
| Agitation |
0.5% |
0% |
0% |
| Abdominal pain |
0.5% |
0% |
0% |
| Orthostatic hypotension |
0.3% |
0.5% |
0% |
| Akathisia |
0.3% |
2% |
0% |
Discontinuation for extrapyramidal symptoms (including Parkinsonism, akathisia, dystonia, and tardive dyskinesia) was 1% in placebo-treated patients, and 3.4% in active control-treated patients in a double-blind, placebo- and active-controlled trial.
Schizophrenia - Pediatrics
Approximately 7% (7/106), of risperidone-treated patients discontinued treatment due to an adverse reaction in a double-blind, placebo-controlled trial, compared with 4% (2/54) placebo-treated patients. The adverse reactions associated with discontinuation for at least one risperidone-treated patient were dizziness (2%), somnolence (1%), sedation (1%), lethargy (1%), anxiety (1%), balance disorder (1%), hypotension (1%), and palpitation (1%).
Bipolar Mania - Adults
In double-blind, placebo-controlled trials with risperidone as monotherapy, approximately 6% (25/448) of risperidone-treated patients discontinued treatment due to an adverse event, compared with approximately 5% (19/424) of placebo-treated patients. The adverse reactions associated with discontinuation in risperidone-treated patients were:
| Adverse Reaction | Risperidone 1 to 6 mg/day (N=448) |
Placebo (N=424) |
|---|---|---|
| Parkinsonism |
0.4% |
0% |
| Lethargy |
0.2% |
0% |
| Dizziness |
0.2% |
0% |
| Alanine aminotransferase increased |
0.2% |
0.2% |
| Aspartate aminotransferase increased |
0.2% |
0.2% |
Bipolar Mania - Pediatrics
In a double-blind, placebo-controlled trial 12% (13/111) of risperidone-treated patients discontinued due to an adverse reaction, compared with 7% (4/58) of placebo-treated patients. The adverse reactions associated with discontinuation in more than one risperidone-treated pediatric patient were nausea (3%), somnolence (2%), sedation (2%), and vomiting (2%).
Autistic Disorder - Pediatrics
In the two 8-week, placebo-controlled trials in pediatric patients treated for irritability associated with autistic disorder (n = 156), one risperidone-treated patient discontinued due to an adverse reaction (Parkinsonism), and one placebo-treated patient discontinued due to an adverse event.
Dose Dependency of Adverse Reactions in Clinical Trials
Extrapyramidal Symptoms
Data from two fixed-dose trials in adults with schizophrenia provided evidence of dose-relatedness for extrapyramidal symptoms associated with risperidone treatment.
Two methods were used to measure extrapyramidal symptoms (EPS) in an 8-week trial comparing 4 fixed doses of risperidone (2, 6, 10, and 16 mg/day), including (1) a Parkinsonism score (mean change from baseline) from the Extrapyramidal Symptom Rating Scale, and (2) incidence of spontaneous complaints of EPS:
| Dose Groups | Placebo | Risperidone 2 mg |
Risperidone 6 mg |
Risperidone 10 mg |
Risperidone 16 mg |
|---|---|---|---|---|---|
| Parkinsonism |
1.2 |
0.9 |
1.8 |
2.4 |
2.6 |
| EPS Incidence |
13% |
17% |
21% |
21% |
35% |
Similar methods were used to measure extrapyramidal symptoms (EPS) in an 8-week trial comparing 5 fixed doses of risperidone (1, 4, 8, 12, and 16 mg/day):
|
Dose Groups
|
Risperidone
1 mg |
Risperidone
4 mg |
Risperidone
8 mg |
Risperidone
12 mg |
Risperidone
16 mg |
| Parkinsonism |
0.6 |
1.7 |
2.4 |
2.9 |
4.1 |
| EPS Incidence |
7% |
12% |
17% |
18% |
20% |
Dystonia
Class Effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Other Adverse Reactions
Adverse event data elicited by a checklist for side effects from a large study comparing 5 fixed doses of risperidone (1, 4, 8, 12, and 16 mg/day) were explored for dose-relatedness of adverse events. A Cochran-Armitage Test for trend in these data revealed a positive trend (p<0.05) for the following adverse reactions: somnolence, vision abnormal, dizziness, palpitations, weight increase, erectile dysfunction, ejaculation disorder, sexual function abnormal, fatigue, and skin discoloration.
Changes in Body Weight
Weight gain was observed in short-term, controlled trials and longer-term uncontrolled studies in adult and pediatric patients [see Warnings and Precautions (5.5), Adverse Reactions (6), and Use in Specific Populations (8.4)].
Changes in ECG Parameters
Between-group comparisons for pooled placebo-controlled trials in adults revealed no statistically significant differences between risperidone and placebo in mean changes from baseline in ECG parameters, including QT, QTc, and PR intervals, and heart rate. When all risperidone doses were pooled from randomized controlled trials in several indications, there was a mean increase in heart rate of 1 beat per minute compared to no change for placebo patients. In short-term schizophrenia trials, higher doses of risperidone (8 to 16 mg/day) were associated with a higher mean increase in heart rate compared to placebo (4 to 6 beats per minute). In pooled placebo-controlled acute mania trials in adults, there were small decreases in mean heart rate, similar among all treatment groups.
In the two placebo-controlled trials in children and adolescents with autistic disorder (aged 5 to 16 years) mean changes in heart rate were an increase of 8.4 beats per minute in the risperidone groups and 6.5 beats per minute in the placebo group. There were no other notable ECG changes.
In a placebo-controlled acute mania trial in children and adolescents (aged 10 to 17 years), there were no significant changes in ECG parameters, other than the effect of risperidone to transiently increase pulse rate (< 6 beats per minute). In two controlled schizophrenia trials in adolescents (aged 13 to 17 years), there were no clinically meaningful changes in ECG parameters including corrected QT intervals between treatment groups or within treatment groups over time.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of risperidone. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These adverse reactions include: alopecia, anaphylactic reaction, angioedema, atrial fibrillation, cardiopulmonary arrest, diabetic ketoacidosis in patients with impaired glucose metabolism, dysgeusia, hypoglycemia, hypothermia, ileus, inappropriate antidiuretic hormone secretion, intestinal obstruction, jaundice, mania, pancreatitis, pituitary adenoma, precocious puberty, pulmonary embolism, QT prolongation, sleep apnea syndrome, sudden death, thrombocytopenia, thrombotic thrombocytopenic purpura, urinary retention, and water intoxication.
7 DRUG INTERACTIONS
7.1 Pharmacokinetic-related Interactions
The dose of risperidone should be adjusted when used in combination with CYP2D6 enzyme inhibitors (e.g., fluoxetine, and paroxetine) and enzyme inducers (e.g., carbamazepine) [see Table 18 and Dosage and Administration (2.5)]. Dose adjustment is not recommended for risperidone when co-administered with ranitidine, cimetidine, amitriptyline, or erythromycin [see Table 18].
| * Change relative to reference |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Coadministered Drug |
Dosing Schedule |
Effect on Active Moiety (Risperidone + 9-Hydroxy- Risperidone Ratio*) |
Risperidone Dose Recommendation |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Coadministered Drug |
Risperidone |
AUC |
Cmax
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Enzyme (CYP2D6) Inhibitors |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Fluoxetine |
20 mg/day |
2 or 3 mg twice daily |
1.4 |
1.5 |
Re-evaluate dosing. Do not exceed 8 mg/day |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Paroxetine |
10 mg/day |
4 mg/day |
1.3 |
- |
Re-evaluate dosing. Do not exceed 8 mg/day |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20 mg/day |
4 mg/day |
1.6 |
- |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 40 mg/day |
4 mg/day |
1.8 |
- |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Enzyme (CYP3A/ PgP inducers) Inducers |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Carbamazepine |
573 ± 168 mg/day |
3 mg twice daily |
0.51 |
0.55 |
Titrate dose upwards. Do not exceed twice the patient7.2 Pharmacodynamic-related Interactions
Centrally-Acting Drugs and Alcohol
8 USE IN SPECIFIC POPULATIONS8.1 Pregnancy
Teratogenic Effects 8.2 Labor and DeliveryThe effect of risperidone on labor and delivery in humans is unknown. 8.3 Nursing MothersRisperidone and 9-hydroxyrisperidone are present in human breast milk. Because of the potential for serious adverse reactions in nursing infants from risperidone, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. 8.4 Pediatric Use
Approved Pediatric Indications
8.5 Geriatric UseClinical studies of risperidone in the treatment of schizophrenia did not include sufficient numbers of patients aged 65 and over to determine whether or not they respond differently than younger patients. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, a lower starting dose is recommended for an elderly patient, reflecting a decreased pharmacokinetic clearance in the elderly, as well as a greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy [see Clinical Pharmacology (12.3) and Dosage and Administration (2.4, 2.5)]. While elderly patients exhibit a greater tendency to orthostatic hypotension, its risk in the elderly may be minimized by limiting the initial dose to 0.5 mg twice daily followed by careful titration [see Warnings and Precautions (5.7)]. Monitoring of orthostatic vital signs should be considered in patients for whom this is of concern. 8.6 Renal ImpairmentIn patients with moderate to severe (Clcr 59 to 15 mL/min) renal disease, clearance of the sum of risperidone and its active metabolite decreased by 60%, compared to young healthy subjects. Risperidone doses should be reduced in patients with renal disease [see Dosage and Administration (2.4)]. 8.7 Hepatic ImpairmentWhile the pharmacokinetics of risperidone in subjects with liver disease were comparable to those in young healthy subjects, the mean free fraction of risperidone in plasma was increased by about 35% because of the diminished concentration of both albumin and α1-acid glycoprotein. Risperidone doses should be reduced in patients with liver disease [see Dosage and Administration (2.4)]. 8.8 Patients with Parkinson's Disease or Lewy Body DementiaPatients with Parkinson's Disease or Dementia with Lewy Bodies can experience increased sensitivity to risperidone. Manifestations can include confusion, obtundation, postural instability with frequent falls, extrapyramidal symptoms, and clinical features consistent with neuroleptic malignant syndrome. 9 DRUG ABUSE AND DEPENDENCE9.1 Controlled SubstanceRisperidone is not a controlled substance. 9.2 AbuseRisperidone has not been systematically studied in animals or humans for its potential for abuse. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of risperidone misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior). 9.3 DependenceRisperidone has not been systematically studied in animals or humans for its potential for tolerance or physical dependence. 10 OVERDOSAGE10.1 Human ExperiencePremarketing experience included eight reports of acute risperidone overdosage with estimated doses ranging from 20 to 300 mg and no fatalities. In general, reported signs and symptoms were those resulting from an exaggeration of the drug's known pharmacological effects, i.e., drowsiness and sedation, tachycardia and hypotension, and extrapyramidal symptoms. One case, involving an estimated overdose of 240 mg, was associated withhyponatremia, hypokalemia, prolonged QT, and widened QRS. Another case, involving an estimated overdose of 36 mg, was associated with a seizure. 10.2 Management of OverdosageFor the most up to date information on the management of risperidone overdosage, contact a certified poison control center (1-800-222-1222 or www.poison.org). Provide supportive care including close medical supervision and monitoring. Treatment should consist of general measures employed in the management of overdosage with any drug. Consider the possibility of multiple drug overdosage. Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. Use supportive and symptomatic measures. There is no specific antidote to risperidone. 11 DESCRIPTIONRisperidone oral solution, USP contains risperidone, an atypical antipsychotic belonging to the chemical class of benzisoxazole derivatives. The chemical designation is 3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)-1-piperidinyl]ethyl]-6,7,8,9-tetrahydro-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one. Its molecular formula is C23H27FN4O2 and its molecular weight is 410.49. The structural formula is: 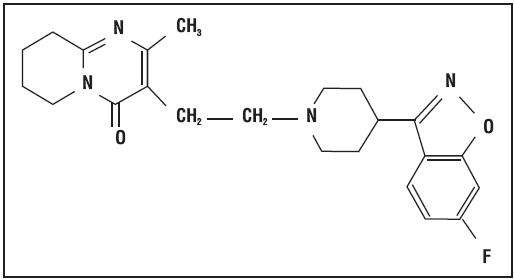 Risperidone USP is a white to slightly beige powder. It is practically insoluble in water, freely soluble in methylene chloride, and soluble in methanol and 0.1 N HCl. 12 CLINICAL PHARMACOLOGY12.1 Mechanism of ActionThe mechanism of action of risperidone, in schizophrenia, is unknown. However, it has been proposed that the drug's therapeutic activity in schizophrenia could be mediated through a combination of dopamine Type 2 (D2) and serotonin Type 2 (5HT2) receptor antagonism. The clinical effect from risperidone results from the combined concentrations of risperidone and its major metabolite, 9-hydroxyrisperidone [see Clinical Pharmacology (12.3)]. Antagonism at receptors other than D2 and 5HT2 [see Clinical Pharmacology (12.1)] may explain some of the other effects of risperidone. 12.2 PharmacodynamicsRisperidone is a selective monoaminergic antagonist with high affinity (Ki of 0.12 to 7.3 nM) for the serotonin Type 2 (5HT2), dopamine Type 2 (D2), α1 and α2 adrenergic, and H1 histaminergic receptors. Risperidone acts as an antagonist at other receptors, but with lower potency. Risperidone has low to moderate affinity (Ki of 47 to 253 nM) for the serotonin 5HT1C, 5HT1D, and 5HT1A receptors, weak affinity (Ki of 620 to 800 nM) for the dopamine D1 and haloperidol-sensitive sigma site, and no affinity (when tested at concentrations >10-5 M) for cholinergic muscarinic or β1 and β2 adrenergic receptors. 12.3 Pharmacokinetics
Absorption
13 NONCLINICAL TOXICOLOGY13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the risperidone carcinogenicity studies; however, measurements during subchronic toxicity studies showed that risperidone elevated serum prolactin levels 5 to 6 fold in mice and rats at the same doses used in the carcinogenicity studies. An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unknown [see Warnings and Precautions (5.6)]. 13.2 Animal ToxicologyJuvenile dogs were treated for 40 weeks with oral risperidone doses of 0.31, 1.25, or 5 mg/kg/day. Decreased bone length and density were observed with a no-effect dose of 0.31 mg/kg/day. This dose produced plasma AUC levels of risperidone plus its active metabolite paliperidone (9-hydroxy-risperidone) which were similar to those in children and adolescents receiving the maximum recommended human dose (MRHD) of 6 mg/day. In addition, a delay in sexual maturation was seen at all doses in both males and females. The above effects showed little or no reversibility in females after a 12 week drug-free recovery period. 14 CLINICAL STUDIES14.1 Schizophrenia
Adults
Long-Term Efficacy 14.2 Bipolar Mania - Monotherapy
Adults
Pediatrics
14.3 Bipolar Mania - Adjunctive Therapy with Lithium or ValproateThe efficacy of risperidone with concomitant lithium or valproate in the treatment of acute manic or mixed episodes was established in one controlled trial in adult patients who met the DSM-IV criteria for Bipolar I Disorder. This trial included patients with or without psychotic features and with or without a rapid-cycling course.
14.4 Irritability Associated with Autistic Disorder
Short-Term Efficacy
in the treatment of irritability associated with autistic disorder was established in two 8-week, placebo-controlled trials in children and adolescents (aged 5 to 16 years) who met the DSM-IV criteria for autistic disorder. Over 90% of these subjects were under 12 years of age and most weighed over 20 kg (16 to 104.3 kg).
A third trial was a 6-week, multicenter, randomized, double-blind, placebo-controlled, fixed-dose study to evaluate the efficacy and safety of a lower than recommended dose of risperidone in subjects (N=96) 5 to 17 years of age with autistic disorder (defined by DSM-IV criteria) and associated irritability and related behavioral symptoms. Approximately 77% of patients were younger than 12 years of age (mean age = 9), and 88% were male. Most patients (73%) weighed less than 45 kg (mean weight = 40 kg). Approximately 90% of patients were antipsychotic-naïve before entering the study. 16 HOW SUPPLIED/STORAGE AND HANDLING16.1 How Supplied
Risperidone Oral Solution USP, 1 mg/mL (NDC 65862-167-01) is supplied in 30 mL bottles with a calibrated (in milliliters and milligrams) syringe. The minimum calibrated volume is 0.25 mL, while the maximum calibrated volume is 3 mL. 16.2 Storage and HandlingStorage and Handling 17 PATIENT COUNSELING INFORMATIONPhysicians are advised to discuss the following issues with patients for whom they prescribe risperidone and their caregivers: 17.1 Orthostatic HypotensionAdvise patients and caregivers about the risk of orthostatic hypotension, especially during the period of initial dose titration [see Warnings and Precautions (5.7)]. 17.2 Interference with Cognitive and Motor PerformanceInform patients and caregivers that risperidone has the potential to impair judgment, thinking, or motor skills. Advise caution about operating hazardous machinery, including automobiles, until patients are reasonably certain that risperidone therapy does not affect them adversely [see Warnings and Precautions (5.9)]. 17.3 PregnancyAdvise patients and caregivers to notify their physician if the patient becomes pregnant or intends to become pregnant during therapy [see Use in Specific Populations (8.1)]. 17.4 NursingInform patients and caregivers that risperidone and its active metabolite are present in human breast milk; there is a potential for serious adverse reactions from risperidone in nursing infants. Advise patients that the decision whether to discontinue nursing or to discontinue the risperidone should take into account the importance of the drug to the patient [see Use in Specific Populations (8.3)]. 17.5 Concomitant MedicationAdvise patients and caregivers to inform their physicians if the patient is taking, or plans to take, any prescription or over-the-counter drugs, because there is a potential for interactions [see Drug Interactions (7)]. 17.6 AlcoholAdvise patients to avoid alcohol while taking risperidone [see Drug Interactions (7.2)]. 17.8 Metabolic ChangesInform patients and caregivers that treatment with risperidone can be associated with hyperglycemia and diabetes mellitus, dyslipidemia, and weight gain [see Warnings and Precautions (5.5)]. 17.9 Tardive DyskinesiaInform patients and caregivers about the risk of tardive dyskinesia [see Warnings and Precautions (5.4)]. PATIENT INSTRUCTIONS USING YOUR RISPERIDONE DISPENSING SYRINGE AND BOTTLE Use this product as indicated below, unless directed otherwise by your Physician. IMPORTANT: Please read these instructions before using risperidone oral solution. 1. Push the plastic screw-cap on the bottle down while turning it counter clockwise. Remove the unscrewed cap (see Figure 1). 2. Hold the pull tab of the seal and remove (see Figure 2). 3. Insert the adaptor into the mouth of the bottle and push down until it is completely seated in the neck of the bottle (Leave adaptor inserted in the bottle after use.) (see Figure 3). 4. Remove the secure tip from orifice of the dispensing syringe (see Figure 4). 5. Insert the dispensing syringe into the adaptor fixed to the bottle neck (see Figure 5). 6. After inserting the syringe into the adaptor, make the bottle upside down and pull the plunger up to the level (see markings on side) that equals the dosage prescribed by your physician (see Figure 6). 7. Upright the bottle to original position. Holding the outer barrel of the syringe, remove the dispensing syringe from the bottle, being careful not to depress the plunger prematurely (see Figure 7). Empty the entire contents of the dispensing syringe into 3 to 4 ounces (100 mL) of a beverage by pushing the plunger down inside the dispensing syringe barrel. Stir the mixture thoroughly before consuming. Risperidone is compatible with water, coffee, orange juice, or low-fat milk: IT IS NOT COMPATIBLE with cola or tea.
8. Replace the plastic cap on the bottle by screwing it clockwise; rinse the empty dispensing syringe with water. And close the orifice of the dispensing syringe by fixing the secure tip (see Figure 8). PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 30 mL Container Label
NDC 65862-167-01 PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 30 mL Carton Label
NDC 65862-167-01
PLEASE, BE CAREFUL! Be sure to consult your doctor before taking any medication!
Copyright © 2014. drugs-library.com. All rights reserved. Information on drugs-library.com is provided for educational purposes only and is not to be used for medical advice, diagnosis or treatment.
Support info@drugs-library.com. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 70) of poor metabolizers given risperidone do not suggest important differences between poor and extensive metabolizers. Second, co-administration of known enzyme inducers (e.g., carbamazepine, phenytoin, rifampin, and phenobarbital) with risperidone may cause a decrease in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone
70) of poor metabolizers given risperidone do not suggest important differences between poor and extensive metabolizers. Second, co-administration of known enzyme inducers (e.g., carbamazepine, phenytoin, rifampin, and phenobarbital) with risperidone may cause a decrease in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone