Rivastigmine Tartrate
Sandoz Inc
Novartis Pharmaceuticals Corporation
HIGHLIGHTS OF PRESCRIBING INFORMATION RECENT MAJOR CHANGESDosage and Administration, Dosing in Specific Populations (2.2) 10/2013Contraindications (4) 10/2013Warnings and Precautions, Hypersensitivity Reactions of the Skin (5.2) 10/2013INDICATIONS AND USAGERivastigmine tartrate is an acetylcholinesterase inhibitor indicated for treatment of: Mild to moderate dementia of the Alzheimer’s type (1.1) Mild to moderate dementia associated with Parkinson’s disease (1.2) DOSAGE AND ADMINISTRATIONAlzheimer’s Disease: Initiate treatment with 1.5 mg twice a day After a minimum of 2 weeks, if tolerated, increase dose to 3 mg twice a day and further to 4.5 mg twice a day and 6 mg twice a day if tolerated with a minimum of 2 weeks at each dose (2.1) Parkinson’s Disease Dementia: Initiate treatment with 1.5 mg twice a day After a minimum of 4 weeks, if tolerated, increase dose to 3 mg twice a day and further to 4.5 mg twice a day and 6 mg twice a day if tolerated with a minimum of 4 weeks at each dose (2.2) Rivastigmine tartrate should be taken with meals in divided doses in the morning and evening. (2.1) Rivastigmine tartrate oral solution and rivastigmine tartrate capsules may be interchanged at equal doses. (2.3)DOSAGE FORMS AND STRENGTHS Capsules: 1.5 mg, 3 mg, 4.5 mg, or 6 mg (3.1) CONTRAINDICATIONS Known hypersensitivity to rivastigmine, other carbamate derivatives or other components of the formulation (4) History of application site reaction with rivastigmine transdermal patch suggestive of allergic contact dermatitis, in the absence of negative allergy testing (4, 5.2) WARNINGS AND PRECAUTIONS Gastrointestinal adverse reactions: may include significant nausea, vomiting, diarrhea, anorexia/decreased appetite, and weight loss, and may necessitate treatment interruption. Dehydration may result from prolonged vomiting or diarrhea and can be associated with serious outcomes. (5.1). Hypersensitivity reactions of the skin: Discontinue rivastigmine in case of disseminated hypersensitivity reaction of the skin, which may occur after oral or transdermal administration. (4, 5.2) In patients with suspected allergic contact dermatitis after transdermal rivastigmine use, switch to oral rivastigmine only after negative allergy testing. Side EffectsMost commonly observed adverse reactions (>5% and 2 times greater than placebo): nausea, vomiting, anorexia, dyspepsia, and asthenia. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSCholinomimetic and anticholinergic drugs: Avoid concomitant use unless clinically necessary. (7.1)
FULL PRESCRIBING INFORMATION
1.1 Alzheimer’s Disease
Rivastigmine Tartrate Capsules are indicated for the treatment of mild to moderate dementia of the Alzheimer's type.
1.2 Parkinson’s Disease Dementia
Rivastigmine Tartrate Capsules are indicated for the treatment of mild to moderate dementia associated with Parkinson’s disease.
2.1 Recommended Dosing
Rivastigmine tartrate should be taken with meals in divided doses in the morning and evening.
Alzheimer’s Disease
The dosage of rivastigmine tartrate shown to be effective in controlled clinical trials in Alzheimer’s disease is 6 mg to 12 mg per day, administered twice a day (daily doses of 3 mg to 6 mg twice a day). There is evidence from the clinical trials that doses at the higher end of this range may be more beneficial.
Initial Dose
Initiate treatment with the 1.5 mg twice a day with rivastigmine tartrate.
Dose Titration
After a minimum of 2 weeks and if well tolerated, increase the dose to 3 mg twice a day. Subsequent increases to 4.5 mg twice a day and 6 mg twice a day should be attempted after a minimum of 2 weeks at the previous dose and if well tolerated. The maximum dose is 6 mg twice a day (12 mg per day).
Parkinson’s Disease Dementia
The dosage of rivastigmine tartrate shown to be effective in the single controlled clinical trial conducted in dementia associated with Parkinson’s disease is 3 mg to 12 mg per day, administered twice a day (daily doses of 1.5 mg to 6 mg twice a day).
Initial Dose
Initiate treatment with the 1.5 mg twice a day with rivastigmine tartrate.
Dose Titration
After a minimum of 4 weeks and if well tolerated, increase the dose to 3 mg twice a day. Subsequent increases to 4.5 mg twice a day and 6 mg twice a day should be attempted after a minimum of 4 weeks at the previous dose and if well tolerated. The maximum dose is 6 mg twice a day (12 mg per day).
Interruption of Treatment
If adverse effects (e.g., nausea, vomiting, abdominal pain, loss of appetite) cause intolerance during treatment, the patient should be instructed to discontinue treatment for several doses and then restart at the same or next lower dose level.
If dosing is interrupted for 3 days or fewer, restart treatment with the same or lower dose of rivastigmine tartrate. If dosing is interrupted for more than 3 days, treatment should be restarted with 1.5 mg twice a day and titrated as described above [see Warnings and Precautions (5.1)].
2.2 Dosing in Specific Populations
Dosing Modifications in Patients with Renal or Hepatic Impairment
Pharmacokinetic studies of oral rivastigmine in patients with moderate to severe renal impairment (glomerular filtration rate [GFR] <50 mL/min) and mild to moderate hepatic impairment (Child-Pugh score 5 to 9) showed reduced clearance of the drug [see Use in Specific Populations (8.6, 8.7), Clinical Pharmacology (12.3)]. Accordingly, such patients may be able to only tolerate lower doses. No data are available on the use of rivastigmine in patients with severe hepatic impairment.
Dosing Modifications in Patients with Low Body Weight
Because rivastigmine blood levels vary with body weight [see Use in Specific Populations (8.8), Clinical Pharmacology (12.3)], careful titration and monitoring should be performed in patients with low body weight. In patients with low body weight (less than 50 kg), monitor closely for toxicities (e.g., excessive nausea, vomiting), and consider reducing the dose if such toxicities develop.
2.3 Important Administration Instructions
Rivastigmine tartrate oral solution and rivastigmine tartrate capsules may be interchanged at equal doses. Caregivers should direct questions about the administration of rivastigmine tartrate oral solution to either their physician or pharmacist [see Patient Counseling Information (17)].
3.1 Rivastigmine Tartrate Capsules
Capsules, containing rivastigmine tartrate equivalent to 1.5 mg, 3 mg, 4.5 mg, or 6 mg of rivastigmine base, are available as follows:
1.5 mg capsule – yellow, “SANDOZ 618” is printed in red on the body of the capsule.
3 mg capsule – orange, “SANDOZ 619” is printed in red on the body of the capsule.
4.5 mg capsule – red, “SANDOZ 620” is printed in white on the body of the capsule.
6 mg capsule – orange and red, “SANDOZ 625” is printed in red on the body of the capsule.
Rivastigmine tartrate is contraindicated in patients with:
- known hypersensitivity to rivastigmine, other carbamate derivatives or other components of the formulation [see Description (11)].
- a previous history of application site reaction with rivastigmine transdermal patch suggestive of allergic contact dermatitis, in the absence of negative allergy testing [see Warnings and Precautions (5.2)].
Isolated cases of generalized skin reactions have been described in postmarketing experience [see Adverse Reactions (6.2)].
5.1 Gastrointestinal Side Effects
Rivastigmine tartrate can cause gastrointestinal adverse reactions, including significant nausea, vomiting, diarrhea, anorexia/decreased appetite, and weight loss. Dehydration may result from prolonged vomiting or diarrhea and can be associated with serious outcomes. The incidence and severity of these reactions are dose-related [see Adverse Reactions (6.1)] . For this reason, patients should always be started at a dose of 1.5 mg twice a day and titrated to their maintenance dose.
If treatment is interrupted for longer than 3 days, treatment should be reinitiated with the lowest daily dose [see Dosage and Administration (2.1)] to reduce the possibility of severe vomiting and its potentially serious sequelae (e.g., there has been one postmarketing report of severe vomiting with esophageal rupture following inappropriate reinitiation of treatment with a 4.5-mg dose after 8 weeks of treatment interruption).
Inform caregivers to monitor for gastrointestinal adverse reactions and to inform the physician if they occur. It is critical to inform caregivers that if therapy has been interrupted for more than 3 days because of intolerance, the next dose should not be administered without contacting the physician regarding proper retitration.
5.2 Hypersensitivity Reactions of the Skin
There have been isolated postmarketing reports of patients experiencing disseminated hypersensitivity reactions of the skin when administered rivastigmine irrespective of the route of administration (oral or transdermal). Treatment should be discontinued if disseminated hypersensitivity reaction of the skin occurs [see Contraindications (4)]. Patients and caregivers should be instructed accordingly [see Patient Counseling Information (17)].
In patients who develop application site reactions suggestive of allergic contact dermatitis to rivastigmine transdermal patch and who still require rivastigmine, treatment should be switched to oral rivastigmine only after negative allergy testing and under close medical supervision. It is possible that some patients sensitized to rivastigmine by exposure to rivastigmine patch may not be able to take rivastigmine in any form.
5.3 Other Side Effects from Increased Cholinergic Activity
Neurologic Effects
Extrapyramidal Symptoms: Cholinomimetics, including rivastigmine may exacerbate or induce extrapyramidal symptoms. Worsening of parkinsonian symptoms, particularly tremor, has been observed in patients with dementia associated with Parkinson’s disease who were treated with rivastigmine tartrate capsules.
Seizures: Drugs that increase cholinergic activity are believed to have some potential for causing seizures. However, seizure activity also may be a manifestation of Alzheimer's disease.
Peptic Ulcers/Gastrointestinal Bleeding
Cholinesterase inhibitors, including rivastigmine, may be expected to increase gastric acid secretion due to increased cholinergic activity. Monitor patients using rivastigmine tartrate for symptoms of active or occult gastrointestinal bleeding, especially those at increased risk for developing ulcers, e.g., those with a history of ulcer disease or those receiving concurrent nonsteroidal anti-inflammatory drugs (NSAIDs). Clinical studies of rivastigmine have shown no significant increase, relative to placebo, in the incidence of either peptic ulcer disease or gastrointestinal bleeding.
Use with Anesthesia
Rivastigmine, as a cholinesterase inhibitor, is likely to exaggerate succinylcholine-type muscle relaxation during anesthesia.
Cardiac Conduction Effects
Because rivastigmine increases cholinergic activity, use of rivastigmine may have vagotonic effects on heart rate (e.g., bradycardia). The potential for this action may be particularly important in patients with sick sinus syndrome or other supraventricular cardiac conduction conditions. In clinical trials, rivastigmine was not associated with any increased incidence of cardiovascular adverse events, heart rate or blood pressure changes, or ECG abnormalities. Syncopal episodes have been reported in 3% of patients receiving 6 mg to 12 mg per day of rivastigmine tartrate, compared to 2% of placebo patients.
Genitourinary Effects
Although not observed in clinical trials of rivastigmine, drugs that increase cholinergic activity may cause urinary obstruction.
Pulmonary Effects
Drugs that increase cholinergic activity, including rivastigmine, should be used with care in patients with a history of asthma or obstructive pulmonary disease.
5.4 Impairment in Driving or Use of Machinery
Dementia may cause gradual impairment of driving performance or compromise the ability to use machinery. The administration of rivastigmine may also result in adverse reactions that are detrimental to these functions. During treatment with rivastigmine tartrate, routinely evaluate the patient’s ability to continue driving or operating machinery.
The following adverse reactions are described elsewhere in other sections of the prescribing information:
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.1)].
- Hypersensitivity Reactions of the Skin [see Warnings and Precautions (5.2)].
- Other Adverse Reactions from Increased Cholinergic Activity [see Warnings and Precautions (5.3)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Rivastigmine tartrate has been administered to over 5,297 individuals during clinical trials worldwide. Of these, 4,326 patients have been treated for at least 3 months, 3,407 patients have been treated for at least 6 months, 2,150 patients have been treated for 1 year, 1,250 patients have been treated for 2 years, and 168 patients have been treated for over 3 years. With regard to exposure to the highest dose, 2,809 patients were exposed to doses of 10 mg to 12 mg, 2,615 patients treated for 3 months, 2,328 patients treated for 6 months, 1,378 patients treated for 1 year, 917 patients treated for 2 years, and 129 patients treated for over 3 years.
Mild to Moderate Alzheimer’s Disease
Most Commonly Observed Adverse Reactions
The most common adverse reactions, defined as those occurring at a frequency of at least 5% and twice the placebo rate, are largely predicted by rivastigmine tartrate's cholinergic effects. These include nausea, vomiting, anorexia, dyspepsia, and asthenia.
Gastrointestinal Adverse Reactions
rivastigmine tartrate use is associated with significant nausea, vomiting, and weight loss [see Warnings and Precautions (5.1)].
Discontinuation Rates
The rate of discontinuation due to adverse events in controlled clinical trials of rivastigmine tartrate was 15% for patients receiving 6 mg to 12 mg per day compared to 5% for patients on placebo during forced weekly dose titration. While on a maintenance dose, the rates were 6% for patients on rivastigmine tartrate compared to 4% for those on placebo.
The most common adverse reactions leading to discontinuation, defined as those occurring in at least 2% of patients and at twice the incidence seen in placebo patients, are shown in Table 1.
| Study Phase | Titration | Maintenance | Overall | |||
|
Rivastigmine Tartrate
≥6-12 mg/day |
Placebo |
Rivastigmine Tartrate
≥6-12 mg/day |
Placebo |
Rivastigmine Tartrate
≥6-12 mg/day |
Placebo | |
| (n=1,189) | (n=868) | (n=987) | (n=788) | (n=1,189) | (n=868) | |
|
Event/%
Discontinuing |
||||||
| Nausea | 8 | <1 | 1 | <1 | 8 | 1 |
| Vomiting | 4 | <1 | 1 | <1 | 5 | <1 |
| Anorexia | 2 | 0 | 1 | <1 | 3 | <1 |
| Dizziness | 2 | <1 | 1 | <1 | 2 | <1 |
Adverse Reactions Observed at an Incidence of at Least 2%
Table 2 lists treatment-emergent signs and symptoms that were reported in at least 2% of patients in placebo-controlled trials and for which the rate of occurrence was greater for patients treated with rivastigmine tartrate doses of 6 mg to 12 mg per day than for those treated with placebo. The prescriber should be aware that these figures cannot be used to predict the frequency of adverse events in the course of usual medical practice when patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with figures obtained from other clinical investigations involving different treatments, uses, or investigators. An inspection of these frequencies, however, does provide the prescriber with one basis by which to estimate the relative contribution of drug and nondrug factors to the adverse event incidences in the population studied.
In general, adverse reactions were less frequent later in the course of treatment.
No systematic effect of race or age could be determined from the incidence of adverse events in the controlled studies. Nausea, vomiting and weight loss were more frequent in women than men.
|
Body System/Adverse Reaction |
Rivastigmine Tartrate
(6-12 mg/day) (n=1,189) |
Placebo
(n=868) |
| Percent of Patients with any Adverse Event | 92 | 79 |
| Autonomic Nervous System | ||
| Sweating Increased | 4 | 1 |
| Syncope | 3 | 2 |
| Body as a Whole | ||
| Fatigue | 9 | 5 |
| Asthenia | 6 | 2 |
| Malaise | 5 | 2 |
| Weight Decrease** | 3 | <1 |
| Cardiovascular Disorders, General | ||
| Hypertension | 3 | 2 |
| Central and Peripheral Nervous System | ||
| Dizziness | 21 | 11 |
| Headache | 17 | 12 |
| Somnolence | 5 | 3 |
| Tremor | 4 | 1 |
| Gastrointestinal System | ||
| Nausea* | 47 | 12 |
| Vomiting* | 31 | 6 |
| Diarrhea | 19 | 11 |
| Anorexia*** | 17 | 3 |
| Abdominal Pain | 13 | 6 |
| Dyspepsia | 9 | 4 |
| Psychiatric Disorders | ||
| Insomnia | 9 | 7 |
| Confusion | 8 | 7 |
| Depression | 6 | 4 |
| Anxiety | 5 | 3 |
| Hallucination | 4 | 3 |
| Aggressive Reaction | 3 | 2 |
| Resistance Mechanism Disorders | ||
| Urinary Tract Infection | 7 | 6 |
*Nausea and Vomiting: In the controlled clinical trials, 47% of the patients treated with a rivastigmine tartrate dose in the therapeutic range of 6 mg to 12 mg per day (n=1189) developed nausea (compared with 12% in placebo). A total of 31% of rivastigmine tartrate-treated patients developed at least 1 episode of vomiting (compared with 6% for placebo). The rate of vomiting was higher during the titration phase (24% versus 3% for placebo) than in the maintenance phase (14% versus 3% for placebo). The rates were higher in women than men. Five percent of patients discontinued for vomiting, compared to less than 1% for patients on placebo. Vomiting was severe in 2% of rivastigmine tartrate-treated patients and was rated as mild or moderate each in 14% of patients. The rate of nausea was higher during the titration phase (43% versus 9% for placebo) than in the maintenance phase (17% versus 4% for placebo).
**Weight Decreased: In the controlled trials, approximately 26% of women on high doses of rivastigmine tartrate (greater than 9 mg per day) had weight loss equal to or greater than 7% of their baseline weight compared to 6% in the placebo-treated patients. About 18% of the males in the high-dose group experienced a similar degree of weight loss compared to 4% in placebo-treated patients. It is not clear how much of the weight loss was associated with anorexia, nausea, vomiting, and the diarrhea associated with the drug.
***Anorexia: In the controlled clinical trials, of the patients treated with a rivastigmine tartrate dose of 6 mg to 12 mg per day, 17% developed anorexia compared to 3% of the placebo patients. Neither the time course nor the severity of the anorexia is known.
Mild to Moderate Parkinson’s Disease Dementia
Rivastigmine tartrate has been administered to 779 individuals during clinical trials worldwide. Of these, 663 patients have been treated for at least 3 months, 476 patients have been treated for at least 6 months, and 313 patients have been treated for 1 year.
Most Commonly Observed Adverse Reactions
The most common adverse events, defined as those occurring at a frequency of at least 5% and twice the placebo rate, are largely predicted by rivastigmine tartrate's cholinergic effects. These include nausea, vomiting, tremor, anorexia, and dizziness.
Discontinuation Rates
The rate of discontinuation due to adverse events in the single placebo-controlled trial of rivastigmine tartrate was 18.2% for patients receiving 3 mg to 12 mg per day compared to 11.2% for patients on placebo during the 24-week study.
The most frequent adverse events that led to discontinuation from this study, defined as those occurring in at least 1% of patients receiving rivastigmine tartrate and more frequent than those receiving placebo, were nausea (3.6% rivastigmine tartrate versus 0.6% placebo), vomiting (1.9% rivastigmine tartrate versus 0.6% placebo), and tremor (1.7% rivastigmine tartrate versus 0.0% placebo).
Adverse Reactions Observed at an Incidence of at Least 2%
Table 3 lists treatment-emergent signs and symptoms that were reported in at least 2% of patients in a single placebo-controlled trial and during the first 24 weeks of a 76-week open-label active-controlled trial for which the rate of occurrence was greater for patients treated with rivastigmine tartrate doses of 3 mg to 12 mg per day than for those treated with placebo in the placebo-controlled trial. The prescriber should be aware that these figures cannot be used to predict the frequency of adverse events in the course of usual medical practice when patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with figures obtained from other clinical investigations involving different treatments, uses, or investigators. An inspection of these frequencies, however, does provide the prescriber with 1 basis by which to estimate the relative contribution of drug and non-drug factors to the adverse event incidences in the population studied.
In general, adverse reactions were less frequent later in the course of treatment.
|
Active-Controlled Study |
Placebo-Controlled Study |
||
|
Body System/Adverse Reaction |
Rivastigmine Tartrate
(3-12 mg/day) (n=294) |
Rivastigmine Tartrate
(3-12 mg/day) (n=362) |
Placebo
(n=179) |
| Percent of Patients with any Adverse Event | 88 | 84 | 71 |
| Gastrointestinal Disorders | |||
| Nausea | 38 | 29 | 11 |
| Vomiting | 13 | 17 | 2 |
| Diarrhea | 8 | 7 | 4 |
| Upper Abdominal Pain | 4 | 4 | 1 |
| Salivary hypersecretion | 2 | 1 | 0 |
| General Disorders and Administrative Site Conditions | |||
| Fall | 10 | 6 | 6 |
| Fatigue | 5 | 4 | 3 |
| Asthenia | 4 | 2 | 1 |
| Metabolism and Nutritional Disorders | |||
| Anorexia | - | 6 | 3 |
| Decreased Appetite | 5 | 8 | 5 |
| Dehydration | 1 | 2 | 1 |
| Nervous System Disorders | |||
| Tremor | 23 | 10 | 4 |
| Dizziness | 8 | 6 | 1 |
| Headache | 4 | 4 | 3 |
| Somnolence | 6 | 4 | 3 |
| Parkinson’s Disease (worsening) | -* | 3 | 1 |
| Bradykinesia | 3 | 3 | 2 |
| Dyskinesia | 3 | 1 | 1 |
| Cogwheel rigidity | 3 | 1 | 0 |
| Hypokinesia | 2 | 1 | 0 |
| Parkinsonism | - | 2 | 1 |
| Psychiatric Disorders | |||
| Anxiety | 4 | 4 | 1 |
| Insomnia | 2 | 3 | 2 |
| Restlessness | 1 | 3 | 2 |
| Skin and Subcutaneous Tissue Disorders | |||
| Sweating increased | 2 | 2 | 1 |
*Parkinson’s disease (worsening) in the active-controlled study was assessed by reported pre-identified adverse events (tremor, cogwheel rigidity, fall), each of them listed with corresponding frequencies.
Other Adverse Events Observed During Clinical Trials
Mild to Moderate Alzheimer’s Disease
Treatment-emergent signs and symptoms that occurred during 8 controlled clinical trials and 9 open-label trials in North America, Western Europe, Australia, South Africa, and Japan were recorded as adverse events by the clinical investigators using terminology of their own choosing. To provide an overall estimate of the proportion of individuals having similar types of events, the events were grouped into a smaller number of standardized categories using a modified WHO dictionary, and event frequencies were calculated across all studies. These categories are used in the listing below. The frequencies represent the proportion of 5,297 patients from these trials who experienced that event while receiving rivastigmine tartrate. All adverse events occurring in at least 6 patients (approximately 0.1%) are included, except for those already listed elsewhere in labeling, WHO terms too general to be informative, relatively minor events, or events unlikely to be drug-caused.
Events are classified by body system and listed using the following definitions: frequent adverse events-those occurring in at least 1/100 patients; infrequent adverse events-those occurring in 1/100 to 1/1,000 patients. These adverse events are not necessarily related to rivastigmine tartrate treatment and in most cases were observed at a similar frequency in placebo-treated patients in the controlled studies.
Autonomic Nervous System: Infrequent: Increased saliva.
Body as a Whole: Frequent: Allergy, hot flushes.
Cardiovascular System: Frequent: Hypotension, postural hypotension.
Central and Peripheral Nervous System: Frequent: Abnormal gait, ataxia, paresthesia, convulsions. Infrequent: Dysphonia, hypoesthesia, migraine, nystagmus.
Gastrointestinal System: Frequent: Gastritis, constipation, flatulence. Infrequent: Gastric ulcer, gastroesophageal reflux, GI hemorrhage, hernia, melena, rectal hemorrhage, duodenal ulcer, hematemesis, pancreatitis.
Hearing and Vestibular Disorders: Frequent: Tinnitus.
Heart Rate and Rhythm Disorders: Frequent: Atrial fibrillation, bradycardia, palpitation. Infrequent: AV block, sick sinus syndrome, supraventricular tachycardia, extrasystoles, tachycardia.
Liver and Biliary System Disorders: Infrequent: Abnormal hepatic function tests.
Metabolic and Nutritional Disorders: Frequent: Dehydration, hypokalemia. Infrequent: Hyponatremia.
Musculoskeletal Disorders: Infrequent: Muscle weakness.
Myo-, Endo-, Pericardial and Valve Disorders: Frequent: Angina pectoris, myocardial infarction.
Psychiatric Disorders: Frequent: Confusion. Infrequent: Apathy, suicide attempt, increased libido, suicidal ideation.
Reproductive Disorders (Female and Male): Infrequent: Breast pain.
Resistance Mechanism Disorders: Infrequent: Herpes simplex, otitis media.
Respiratory System: Infrequent: Bronchospasm.
Skin and Appendages: Frequent: Rashes of various kinds (maculopapular, eczema, bullous, exfoliative, psoriaform, erythematous). Infrequent: Urticaria, contact dermatitis.
Urinary System Disorders: Frequent: Hematuria. Infrequent: Acute renal failure, dysuria.
Vascular (extracardiac) Disorders: Infrequent: Peripheral ischemia, intracranial hemorrhage.
Vision Disorders: Frequent: Cataract. Infrequent: Diplopia, glaucoma.
White Cell and Resistance Disorders: Infrequent: Lymphadenopathy.
Mild to Moderate Parkinson’s Disease Dementia
Additional treatment-emergent adverse events in patients with Parkinson’s disease dementia occurring in at least 1 patient (approximately 0.3%) are listed below, excluding events that are already listed above for the dementia of the Alzheimer’s type or elsewhere in labeling, WHO terms too general to be informative, relatively minor events, or events unlikely to be drug-caused. Events are classified by body system and listed using the following definitions: frequent adverse events– those occurring in at least 1/100 patients; infrequent adverse events–those occurring in 1/100 to 1/1,000 patients. These adverse events are not necessarily related to rivastigmine tartrate treatment and in most cases were observed at a similar frequency in placebo-treated patients in the controlled studies.
Central and Peripheral Nervous System: Frequent: Transient ischemic attack.
Gastrointestinal System: Frequent: Dyspepsia. Infrequent: Fecaloma, dysphagia.
General Disorders and Administration Site Conditions: Frequent: Chest pain.
Liver and Biliary System Disorders: Infrequent: Elevated gamma-glutamyltransferase level.
Musculoskeletal Disorders: Frequent: Back pain. Infrequent: Muscle stiffness.
Psychiatric Disorders: Frequent: Agitation, depression.
Respiratory System: Frequent: Dyspnea. Infrequent: Cough.
Urinary System Disorders: Infrequent: Urinary incontinence.
Vision Disorders: Infrequent: Blurred vision.
Other Adverse Reactions Observed with Rivastigmine Transdermal Patch
The following additional adverse reactions have been observed with rivastigmine transdermal patch:
Cerebrovascular accident, delirium, psychomotor hyperactivity, erythema, blister, dermatitis allergic.
6.2 Postmarketing Experience
Voluntary reports of adverse events temporally associated with rivastigmine tartrate that have been received since market introduction that are not listed above, and that may or may not be causally related to the drug include the following:
Hepatobiliary Disorders: Hepatitis.
Psychiatric Disorders: Aggression.
Skin and Appendages: Stevens-Johnson syndrome, disseminated cutaneous hypersensitivity reactions.
7.1 Cholinomimetic and Anticholinergic Drugs
Increased cholinergic effects may be expected when rivastigmine is given with other cholinomimetic drugs. Rivastigmine may also interfere with the activity of anticholinergic medications. Avoid concomitant use of rivastigmine with drugs having these pharmacologic effects unless deemed clinically necessary.
8.1 Pregnancy
Pregnancy Category B
There are no adequate and well-controlled studies in pregnant women. Reproduction studies conducted in pregnant rats and rabbits at oral doses up to 2.3 mg-base/kg/day, or 2 (rat) and 4 (rabbit) times the maximum recommended human dose (MRHD) of 12 mg per day on a mg/m2 basis, revealed no evidence of teratogenicity. Studies in pregnant rats showed slightly decreased fetal/pup weight at doses that were below the MRHD but usually associated with some maternal toxicity. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Rivastigmine and its metabolites are excreted in rat milk following oral administration of rivastigmine; levels of rivastigmine plus metabolites in rat milk are approximately 2 times that in maternal plasma. It is not known whether rivastigmine is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from rivastigmine tartrate, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established and therefore the use of rivastigmine in children and adolescents (below 18 years of age) is not recommended.
8.5 Geriatric Use
Of the total number of subjects in clinical studies of rivastigmine tartrate, 86 percent were 65 years and older while 46 percent were 75 years and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
In patients with moderate to severe renal impairment (glomerular filtration rate [GFR] <50 mL/min), clearance of oral rivastigmine was reduced [see Clinical Pharmacology (12.3)]. Accordingly, such patients may be able to only tolerate lower doses.
8.7 Hepatic Impairment
In patients with mild or moderate hepatic impairment (Child-Pugh score 5 to 9), clearance of oral rivastigmine was reduced [see Clinical Pharmacology (12.3)]. Accordingly, such patients may be able to only tolerate lower doses. No data are available on the use of rivastigmine in patients with severe hepatic impairment.
8.8 Low or High Body Weight
Because rivastigmine blood levels vary with weight, careful titration and monitoring should be performed in patients with low or high body weights. Compared to a patient with a body weight of 65 kg, the rivastigmine steady-state concentrations in a patient with a body weight of 35 kg would be approximately doubled, while for a patient with a body weight of 100 kg the concentrations would be approximately halved. In patients with low body weight (<50 kg), monitor closely for toxicities (e.g., excessive nausea, vomiting), and consider reducing the dose of rivastigmine tartrate if such toxicities develop.
Because strategies for the management of overdose are continually evolving, it is advisable to contact a Poison Control Center to determine the latest recommendations for the management of an overdose of any drug.
As rivastigmine has a short plasma half-life of about 1 hour and a moderate duration of acetylcholinesterase inhibition of 8 to 10 hours, it is recommended that in cases of asymptomatic overdoses, no further dose of rivastigmine tartrate should be administered for the next 24 hours.
As in any case of overdose, general supportive measures should be utilized. Overdosage with cholinesterase inhibitors can result in cholinergic crisis characterized by severe nausea, vomiting, salivation, sweating, bradycardia, hypotension, respiratory depression, collapse and convulsions. Increasing muscle weakness is a possibility and may result in death if respiratory muscles are involved. Atypical responses in blood pressure and heart rate have been reported with other drugs that increase cholinergic activity when coadministered with quaternary anticholinergics such as glycopyrrolate. Due to the short half-life of rivastigmine, dialysis (hemodialysis, peritoneal dialysis, or hemofiltration) would not be clinically indicated in the event of an overdose.
In overdoses accompanied by severe nausea and vomiting, the use of antiemetics should be considered. In a documented case of a 46 mg overdose with rivastigmine tartrate, the patient experienced vomiting, incontinence, hypertension, psychomotor retardation, and loss of consciousness. The patient fully recovered within 24 hours and conservative management was all that was required for treatment.
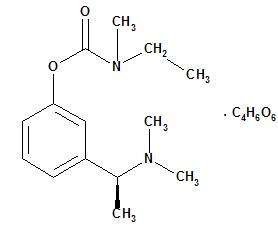
Rivastigmine tartrate is a reversible cholinesterase inhibitor and is known chemically as (S)-N-Ethyl-N-methyl-3-[1-(dimethylamino)ethyl]-phenyl carbamate hydrogen-(2R,3R)-tartrate. Rivastigmine tartrate is commonly referred to in the pharmacological literature as SDZ ENA 713 or ENA 713. It has an empirical formula of C14H22N2O2 • C4H6O6 (hydrogen tartrate salt-hta salt) and a molecular weight of 400.43 (hta salt). Rivastigmine tartrate is a white to off-white, fine crystalline powder that is very soluble in water, soluble in ethanol and acetonitrile, slightly soluble in n-octanol and very slightly soluble in ethyl acetate.
The distribution coefficient at 37°C in n-octanol/phosphate buffer solution pH 7 is 3.0.
Rivastigmine Tartrate Capsules contain rivastigmine tartrate, equivalent to 1.5 mg, 3 mg, 4.5 mg, and 6 mg of rivastigmine base for oral administration. Inactive ingredients are hydroxypropyl methylcellulose, magnesium stearate, microcrystalline cellulose, and silicon dioxide. Each hard-gelatin capsule contains gelatin, titanium dioxide and red and/or yellow iron oxides.
12.1 Mechanism of Action
Although the precise mechanism of action of rivastigmine is unknown, it is thought to exert its therapeutic effect by enhancing cholinergic function. This is accomplished by increasing the concentration of acetylcholine through reversible inhibition of its hydrolysis by cholinesterase. Therefore, the effect of rivastigmine may lessen as the disease process advances and fewer cholinergic neurons remain functionally intact. There is no evidence that rivastigmine alters the course of the underlying dementing process.
12.2 Pharmacodynamics
After a 6-mg dose of rivastigmine, anticholinesterase activity is present in cerebrospinal fluid (CSF) for about 10 hours, with a maximum inhibition of about 60% 5 hours after dosing.
In vitro and in vivo studies demonstrate that the inhibition of cholinesterase by rivastigmine is not affected by the concomitant administration of memantine, an N-methyl-D-aspartate receptor antagonist.
12.3 Pharmacokinetics
Rivastigmine shows linear pharmacokinetics up to 3 mg twice a day but is nonlinear at higher doses. Doubling the dose from 3 mg to 6 mg twice a day results in a 3-fold increase in AUC. The elimination half-life is about 1.5 hours, with most elimination as metabolites via the urine.
Absorption
Rivastigmine is rapidly and completely absorbed. Peak plasma concentrations are reached in approximately 1 hour. Absolute bioavailability after a 3-mg dose is about 36%. Administration of rivastigmine tartrate with food delays absorption (tmax) by 90 minutes lowers Cmax by approximately 30% and increases AUC by approximately 30%.
Distribution
Rivastigmine is weakly bound to plasma proteins (approximately 40%) over the therapeutic range. It readily crosses the blood-brain barrier, reaching CSF peak concentrations in 1.4 to 2.6 hours. It has an apparent volume of distribution in the range of 1.8 to 2.7 L/kg.
Metabolism
Rivastigmine is rapidly and extensively metabolized, primarily via cholinesterase-mediated hydrolysis to the decarbamylated metabolite. Based on evidence from in vitro and animal studies, the major cytochrome P450 isozymes are minimally involved in rivastigmine metabolism. Consistent with these observations is the finding that no drug interactions related to cytochrome P450 have been observed in humans [see Drug Interactions (7.1)].
Elimination
The major pathway of elimination is via the kidneys. Following administration of 14C-rivastigmine to 6 healthy volunteers, total recovery of radioactivity over 120 hours was 97% in urine and 0.4% in feces. No parent drug was detected in urine. The sulfate conjugate of the decarbamylated metabolite is the major component excreted in urine and represents 40% of the dose. Mean oral clearance of rivastigmine is 1.8 ± 0.6 L/min after 6 mg twice a day.
Renal Impairment
Following a single 3-mg dose, mean oral clearance of rivastigmine is 64% lower in moderately impaired renal patients (n=8, GFR=10 to 50 mL/min) than in healthy subjects (n=10, GFR≥60 mL/min); Cl/F=1.7 L/min and 4.8 L/min, respectively. In patients with severe renal impairment (n=8, GFR <10 mL/min), mean oral clearance of rivastigmine is 43% higher than in healthy subjects (n=10, GFR ≥60 mL/min); Cl/F=6.9 L/min and 4.8 L/min, respectively. For unexplained reasons, the severely impaired renal patients had a higher clearance of rivastigmine than moderately impaired patients. Despite this finding, such patients may be able to only tolerate lower doses.
Hepatic Impairment
Following a single 3-mg dose, mean oral clearance of rivastigmine was 60% lower in hepatically impaired patients (n=10, biopsy proven) than in healthy subjects (n=10). After multiple 6-mg twice a day oral dosing, the mean clearance of rivastigmine was 65% lower in mild (n=7, Child-Pugh score 5 to 6) and moderate (n=3, Child-Pugh score 7 to 9) hepatically impaired patients (biopsy proven, liver cirrhosis) than in healthy subjects (n=10). Accordingly, such patients may be able to only tolerate lower doses.
Body Weight
A relationship between drug exposure at steady-state (rivastigmine and metabolite NAP226-90) and body weight was observed in Alzheimer’s dementia patients. Rivastigmine exposure is higher in subjects with low body weight. Compared to a patient with a body weight of 65 kg, the rivastigmine steady-state concentrations in a patient with a body weight of 35 kg would be approximately doubled, while for a patient with a body weight of 100 kg the concentrations would be approximately halved.
Age
Following a single 2.5-mg oral dose to elderly volunteers (60 years and older, n=24) and younger volunteers (n=24), mean oral clearance of rivastigmine was 30% lower in elderly (7 L/min) than in younger subjects (10 L/min).
Gender or Race
Population pharmacokinetic analysis of oral rivastigmine indicated that neither gender (n=277 males and 348 females) nor race (n=575 Caucasian, 34 Black, 4 Asian, and 12 Other) affected clearance of the drug.
Smoking
Population pharmacokinetic analysis showed that nicotine use increased the oral clearance of rivastigmine by 23% (n=75 smokers and 549 nonsmokers).
Drug Interaction Studies
Effect of Rivastigmine on the Metabolism of Other Drugs
Rivastigmine is primarily metabolized through hydrolysis by esterases. Minimal metabolism occurs via the major cytochrome P450 isoenzymes. Based on in vitro studies, no pharmacokinetic drug interactions with drugs metabolized by the following isoenzyme systems are expected: CYP1A2, CYP2D6, CYP3A4/5, CYP2E1, CYP2C9, CYP2C8, CYP2C19, or CYP2B6.
No pharmacokinetic interaction was observed between rivastigmine taken orally and digoxin, warfarin, diazepam or fluoxetine in studies in healthy volunteers. The increase in prothrombin time induced by warfarin is not affected by administration of rivastigmine.
Effect of Other Drugs on the Metabolism of Rivastigmine
Drugs that induce or inhibit CYP450 metabolism are not expected to alter the metabolism of rivastigmine.
Population pharmacokinetic analysis with a database of 625 patients showed that the pharmacokinetics of rivastigmine taken orally were not influenced by commonly prescribed medications such as antacids (n=77), antihypertensives (n=72), ß-blockers (n=42), calcium channel blockers (n=75), antidiabetics (n=21), NSAIDs (n=79), estrogens (n=70), salicylate analgesics (n=177), antianginals (n=35) and antihistamines (n=15).
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In oral carcinogenicity studies conducted at doses up to 1.1 mg-base/kg/day in rats and 1.6 mg-base/kg/day in mice, rivastigmine was not carcinogenic. These doses are less than the maximum recommended human dose (MRHD) of 12 mg per day on a mg/m2 basis.
Mutagenesis
Rivastigmine was clastogenic in in vitro chromosomal aberration assays in mammalian cells in the presence, but not the absence, of metabolic activation. Rivastigmine was negative in an in vitro bacterial reverse mutation (Ames) assay, an in vitro HGPRT assay, and in an in vivo mouse micronucleus test.
Impairment of Fertility
Rivastigmine had no effect on fertility or reproductive performance in rats at oral doses up to 1.1 mg-base/kg/day, a dose less than the MRHD on a mg/m2 basis.
Mild to Moderate Alzheimer’s Disease
The effectiveness of rivastigmine tartrate as a treatment for Alzheimer's disease is demonstrated by the results of 2 randomized, double-blind, placebo-controlled clinical investigations (Study 1 and Study 2) in patients with Alzheimer's disease [diagnosed by NINCDS-ADRDA and DSM-IV criteria, Mini-Mental State Examination (MMSE) ≥10 and ≤26, and the Global Deterioration Scale (GDS)]. The mean age of patients participating in rivastigmine tartrate trials was 73 years with a range of 41 to 95. Approximately 59% of patients were women and 41% were men. The racial distribution was Caucasian 87%, Black 4%, and other races 9%.
In each study, the effectiveness of rivastigmine tartrate was evaluated using a dual outcome assessment strategy.
The ability of rivastigmine tartrate to improve cognitive performance was assessed with the cognitive subscale of the Alzheimer's Disease Assessment Scale (ADAS-cog), a multi-item instrument that has been extensively validated in longitudinal cohorts of Alzheimer's disease patients. The ADAS-cog examines selected aspects of cognitive performance including elements of memory, orientation, attention, reasoning, language, and praxis. The ADAS-cog scoring range is from 0 to 70, with higher scores indicating greater cognitive impairment. Elderly normal adults may score as low as 0 or 1, but it is not unusual for non-demented adults to score slightly higher.
The patients recruited as participants in each study had mean scores on ADAS-cog of approximately 23 units, with a range from 1 to 61. Experience gained in longitudinal studies of ambulatory patients with mild to moderate Alzheimer's disease suggests that they gain 6 to 12 units a year on the ADAS-cog. Lesser degrees of change, however, are seen in patients with very mild or very advanced disease because the ADAS-cog is not uniformly sensitive to change over the course of the disease. The annualized rate of decline in the placebo patients participating in rivastigmine tartrate trials was approximately 3 to 8 units per year.
The ability of rivastigmine tartrate to produce an overall clinical effect was assessed using a Clinician's Interview-Based Impression of Change (CIBIC) that required the use of caregiver information, the CIBIC-Plus. The CIBIC-Plus is not a single instrument and is not a standardized instrument like the ADAS-cog. Clinical trials for investigational drugs have used a variety of CIBIC formats, each different in terms of depth and structure. As such, results from a CIBIC-Plus reflect clinical experience from the trial or trials in which it was used and cannot be compared directly with the results of CIBIC-Plus evaluations from other clinical trials. The CIBIC-Plus used in the rivastigmine tartrate trials was a structured instrument based on a comprehensive evaluation at baseline and subsequent time-points of 3 domains: patient cognition, behavior and functioning, including assessment of activities of daily living. It represents the assessment of a skilled clinician using validated scales based on his/her observation at interviews conducted separately with the patient and the caregiver familiar with the behavior of the patient over the interval rated. The CIBIC-Plus is scored as a 7-point categorical rating, ranging from a score of 1, indicating "markedly improved," to a score of 4, indicating "no change" to a score of 7, indicating "marked worsening." The CIBIC-Plus has not been systematically compared directly to assessments not using information from caregivers or other global methods.
U.S. 26-Week Study of Rivastigmine Tartrate in Mild to Moderate Alzheimer’s Disease (Study 1)
In a study of 26 weeks duration, 699 patients were randomized to either a dose range of 1 mg to 4 mg or 6 mg to 12 mg of rivastigmine tartrate per day or to placebo, each given in divided doses. The 26-week study was divided into a 12-week forced-dose titration phase and a 14-week maintenance phase. The patients in the active treatment arms of the study were maintained at their highest tolerated dose within the respective range.
Figure 1 illustrates the time course for the change from baseline in ADAS-cog scores for all 3 dose groups over the 26 weeks of the study. At 26 weeks of treatment, the mean differences in the ADAS-cog change scores for the rivastigmine tartrate-treated patients compared to the patients on placebo were 1.9 and 4.9 units for the 1 mg to 4 mg and 6 mg to 12 mg treatments, respectively. Both treatments were statistically significantly superior to placebo and the 6 mg to 12 mg per day range was significantly superior to the 1 mg to 4 mg per day range.
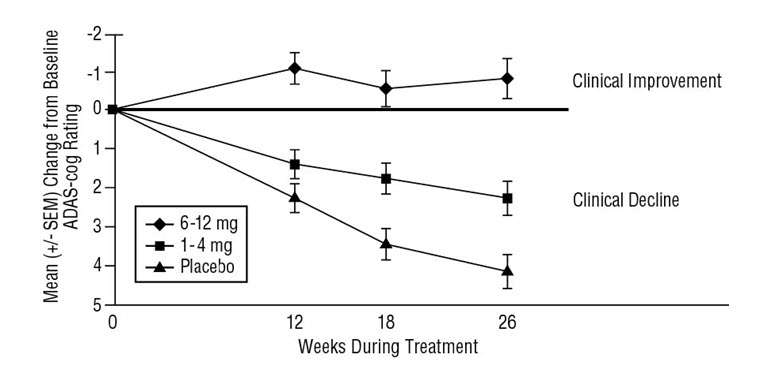
Patients’ age, gender, or race did not predict clinical outcome of rivastigmine tartrate treatment.
Rivastigmine Tartrate Capsules
Rivastigmine Tartrate Capsules equivalent to 1.5 mg, 3 mg, 4.5 mg, or 6 mg of rivastigmine base are available as follows:
1.5 mg capsule – yellow, “SANDOZ 618” is printed in red on the body of the capsule.
Bottles of 60 NDC 0781-2614-60
3 mg capsule – orange, “SANDOZ 619” is printed in red on the body of the capsule.
Bottles of 60 NDC 0781-2615-60
4.5 mg capsule – red, “SANDOZ 620” is printed in white on the body of the capsule.
Bottles of 60 NDC 0781-2616-60
6 mg capsule – orange and red, “SANDOZ 625” is printed in red on the body of the capsule.
Bottles of 60 NDC 0781-2617-60
Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F) [see USP Controlled Room Temperature]. Store in a tight container.
Gastrointestinal Adverse Reactions
Caregivers should be advised of the high incidence of nausea and vomiting associated with the use of the drug along with the possibility of anorexia and weight loss. Caregivers should be encouraged to monitor for these adverse events and inform the physician if they occur. It is critical to inform caregivers that if therapy has been interrupted for more than several days, the next dose should not be administered until they have discussed this with the physician [see Warnings and Precautions (5.1)].
Skin Reactions
Caregivers and patients should be advised that allergic skin reactions have been reported in association with rivastigmine tartrate regardless of formulation (capsules, oral solution or transdermal patch). In case of skin reaction while taking rivastigmine tartrate, patients should consult with their physician immediately [see Warnings and Precautions (5.2)].
Importance of Correct Usage
Caregivers should direct questions about the administration of rivastigmine tartrate to either their physician or pharmacist.
Concomitant Use of Drugs with Cholinergic Action
Caregivers and patients should be advised that cholinomimetics, including rivastigmine, may exacerbate or induce extrapyramidal symptoms. Worsening in patients with Parkinson’s disease, including an increased incidence or intensity of tremor, has been observed [see Warnings and Precautions (5.3)].
Manufactured by
Novartis Pharma Produktions GmbH
Wehr, Germany for
Sandoz Inc.
Princeton, NJ 08540
T2013-101
October 2013
Package Label – 1.5 mg
Rx Only NDC 0781-2614-60
Rivastigmine Tartrate Capsules
equivalent to 1.5 mg base
60 Capsules

Package Label – 3 mg
Rx Only NDC 0781-2615-60
Rivastigmine Tartrate Capsules
equivalent to 3 mg base
60 Capsules

Package Label – 4.5 mg
Rx Only NDC 0781-2616-60
Rivastigmine Tartrate Capsules
equivalent to 4.5 mg base
60 Capsules

Package Label – 6 mg
Rx Only NDC 0781-2617-60
Rivastigmine Tartrate Capsules
equivalent to 6 mg base
60 Capsules

Rivastigmine Tartraterivastigmine tartrate CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Rivastigmine Tartraterivastigmine tartrate CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Rivastigmine Tartraterivastigmine tartrate CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Rivastigmine Tartraterivastigmine tartrate CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||