Ropinirole Hydrochloride
HIGHLIGHTS OF PRESCRIBING INFORMATION INDICATIONS AND USAGERopinirole extended-release tablets are an orally administered, non-ergoline dopamine agonist indicated for the treatment of signs and symptoms of idiopathic Parkinson’s disease. (1.1)DOSAGE AND ADMINISTRATION Ropinirole extended-release tablets are taken once daily, with or without food. Tablets must be swallowed whole and must not be chewed, crushed, or divided. (2.1) The starting dose is 2 mg taken once daily for 1 to 2 weeks, followed by increases of 2 mg/day at 1 week or longer intervals as appropriate, depending on therapeutic response and tolerability, up to a maximally recommended dose of 24 mg/day. Patients should be assessed for therapeutic response and tolerability at a minimal interval of 1 week or longer after each dose increment. Caution should be exercised during dose titration because too rapid a rate of titration can lead to dose selection that does not provide additional benefit, but that increases the risk of adverse reactions. (2.2, 14.2) Patients may be switched directly from immediate-release ropinirole to ropinirole extended-release tablets. The initial switching dose of ropinirole extended-release tablets should most closely match the total daily dose of immediate-release ropinirole, see Table 1. (2.3) If ropinirole extended-release tablets must be discontinued, they should be tapered gradually over a 7-day period. (2.2) DOSAGE FORMS AND STRENGTHSTablets: 2 mg, 4 mg, 6 mg, 8 mg, and 12 mg (3)CONTRAINDICATIONSNoneWARNINGS AND PRECAUTIONS Falling asleep during activities of daily living may occur, including the operation of motor vehicles, which sometimes resulted in accidents. Sudden onset of sleep may occur without apparent warning or daytime drowsiness. Sedating medications (such as alcohol or CNS depressants), the presence of sleeping disorders, or other medications that increase plasma levels of ropinirole, may increase the risk of somnolence or falling asleep while engaged in activities of daily living. Before initiating treatment, patients should be advised of the potential of sudden onset of sleep or to develop drowsiness and asked about risk factors they may have. If a patient develops sudden onset of sleep during activities that require active participation (e.g., conversations, eating, etc.) and/or cannot avoid high-risk activities in the future, ropinirole extended-release tablets should ordinarily be discontinued. (5.1) Syncope, sometimes associated with bradycardia, may occur. (5.2) Symptomatic hypotension (including postural/orthostatic hypotension) may occur, especially during dose escalation. (5.3) Elevation of blood pressure and changes in heart rate may occur. (5.4) Hallucination may occur. (5.5) Dyskinesia may be caused or exacerbated. Decreasing the L-dopa dose may lessen or eliminate this side effect. (5.6) Presence of FD&C Yellow #6 (4 mg and 8 mg) (5.11) Side Effects Most common adverse reactions (incidence ≥5% and greater than placebo) in advanced Parkinson’s disease with concomitant L-dopa were dyskinesia, nausea, dizziness, hallucination, somnolence, abdominal pain/ discomfort, and orthostatic hypotension. (6.1) Most common adverse reactions (incidence ≥5%) in early Parkinson’s disease without L-dopa were nausea, somnolence, abdominal pain/ discomfort, dizziness, headache, and constipation. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Watson Laboratories, Inc. at 1-800-272-5525 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONSCYP1A2 is the major enzyme responsible for the metabolism of ropinirole. Thus inhibitors (e.g., ciprofloxacin, fluvoamine) or inducers (e.g., omeprazole or smoking) of CYP1A2 may alter the clearance of ropinirole. Adjustment of dosage of ropinirole extended-release tablets may be required. (7.1)Higher doses of estrogens, usually associated with hormone replacement therapy (HRT), reduced oral clearance of ropinirole. Starting or stopping HRT treatment may require adjustment of dosage of ropinirole extended-release tablets. (7.3)Dopamine antagonists, such as neuroleptics (e.g., phenothiazines, butyrophenones, thioxanthenes) or metoclopramide, may diminish effectiveness of ropinirole. (7.4)USE IN SPECIFIC POPULATIONSPregnancy: ropinirole extended-release tablets should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus. (8.1)
FULL PRESCRIBING INFORMATION
Ropinirole extended-release tablets are indicated for the treatment of the signs and symptoms of idiopathic Parkinson’s disease.
- Ropinirole extended-release tablets are taken once daily, with or without food. Taking ropinirole extended-release tablets with food may reduce the occurrence of nausea; this has not been established in controlled clinical trials [see
Clinical Pharmacology
(
12.3
)].
- Tablets must be swallowed whole and must not be chewed, crushed, or divided.
- If a significant interruption in therapy with ropinirole extended-release tablets has occurred, retitration of therapy may be warranted.
The starting dose is 2 mg taken once daily for 1 to 2 weeks, followed by increases of 2 mg/day at 1-week or longer intervals as appropriate, depending on therapeutic response and tolerability, up to a maximally recommended dose of 24 mg/day.
In clinical trials, dosage was initiated at 2 mg/day and gradually titrated based on individual therapeutic response and tolerability. Doses greater than 24 mg/day have not been studied in clinical trials. Patients should be assessed for therapeutic response and tolerability at a minimal interval of 1 week or longer after each dose increment. Caution should be exercised during dose titration because too rapid a rate of titration may lead to dose selection that may not provide additional benefit, but that may increase the risk of adverse reactions [see Clinical Studies ( 14.2 )]. Due to the flexible dosing design used in clinical studies, specific dose response information could not be determined.
When ropinirole extended-release tablets are administered as adjunct therapy to L-dopa, the concurrent dose of L-dopa may be decreased gradually as tolerated. In the placebo-controlled advanced Parkinson's disease study, the L-dopa dose was reduced once patients reached a dose of ropinirole extended-release tablets of 8 mg/day. Overall, L-dopa dose reduction was sustained in 93% of patients treated with ropinirole extended-release tablets and in 72% of patients on placebo. On average the L-dopa dose was reduced by 34% in patients treated with ropinirole extended-release tablets [see Clinical Studies ( 14 )]. Ropinirole extended-release tablets should be discontinued gradually over a 7–day period.
Patients may be switched directly from immediate-release ropinirole to ropinirole extended-release tablets. The initial dose of ropinirole extended-release tablets should most closely match the total daily dose of the immediate-release formulation of ropinirole tablets, as shown in Table 1.
| Immediate-Release
Ropinirole Tablets Total Daily Dose (mg) |
Ropinirole Extended-
Release Tablets Total Daily Dose (mg) |
| 0.75 to 2.25 | 2 |
| 3 to 4.5 | 4 |
| 6 | 6 |
| 7.5 to 9 | 8 |
| 12 | 12 |
| 15 to 18 | 16 |
| 21 | 20 |
| 24 | 24 |
Following conversion to ropinirole extended-release tablets, the dose may be adjusted depending on therapeutic response and tolerability [see Dosage and Administration ( 2.2 )].
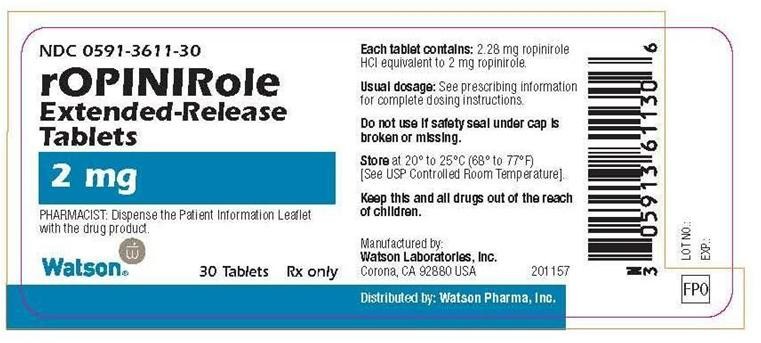
- 2 mg, pink, biconvex, oval, film-coated, tablets debossed with WATSON on one side and 3611 on the other side
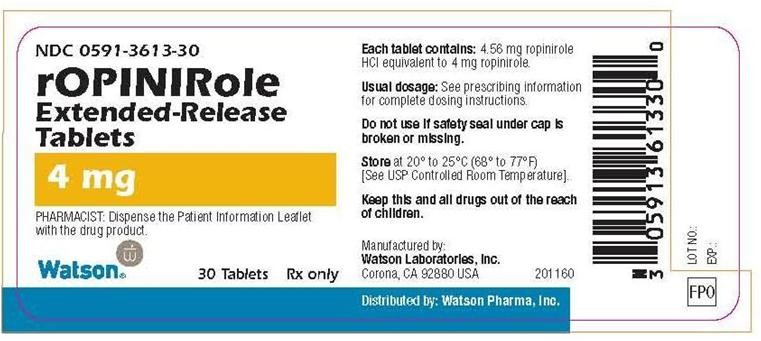
- 4 mg, beige, biconvex, oval, film-coated, tablets debossed with WATSON on one side and 3613 on the other side
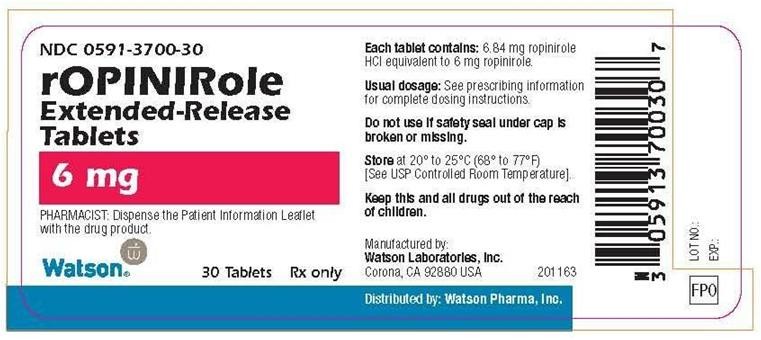
- 6 mg, white, biconvex, oval, film-coated, tablets debossed with WATSON on one side and 3700 on the other side
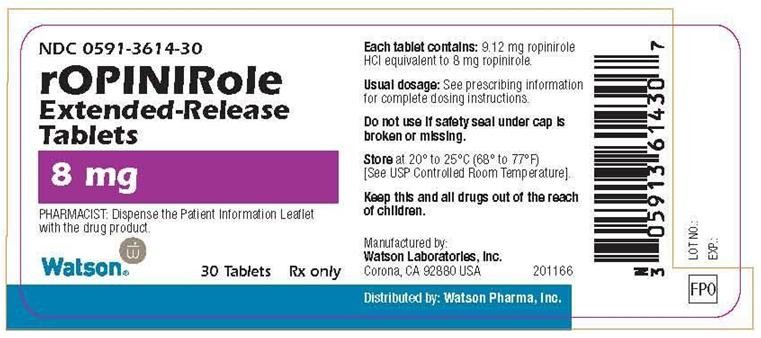
- 8 mg, red, biconvex, oval, film-coated, tablets debossed with WATSON on one side and 3614 on the other side
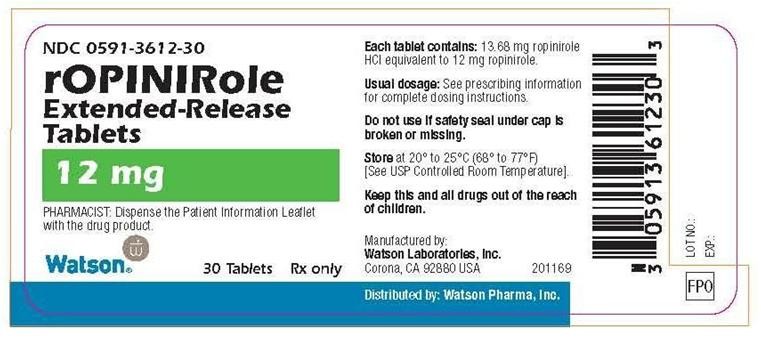
- 12 mg, green, biconvex, oval, film-coated, tablets debossed with WATSON on one side and 3612 on the other side
None.
Patients treated with ropinirole have reported falling asleep while engaged in activities of daily living, including the operation of motor vehicles, which sometimes resulted in accidents. Although many of these patients reported somnolence while on ropinirole, some perceived that they had no warning signs such as excessive drowsiness, and believed that they were alert immediately prior to the event. Some of these events have been reported more than 1 year after initiation of treatment.
Among the 613 patients who received ropinirole extended-release tablets in clinical trials, there were 5 cases of sudden onset of sleep and 2 cases of motor vehicle accident in which it is not known if falling asleep was a contributing factor.
During the 6-month trial in advanced Parkinson’s disease, somnolence was reported in 7% (14 of 202) of patients receiving ropinirole extended-release tablets compared with 4% (7 of 191) of patients receiving placebo. During the 36-week trial in early Parkinson’s disease, somnolence was reported in 11% (16 of 140) of patients receiving ropinirole extended-release tablets compared with 15% (22 of 149) of patients receiving the immediate-release formulation of ropinirole [see Adverse Reactions ( 6 )]. However, because dose-response was not systematically studied with ropinirole extended-release tablets, the occurrence of somnolence at the highest recommended doses may be higher than these reported frequencies [see Adverse Reactions ( 6 )].
Many clinical experts believe that falling asleep while engaged in activities of daily living always occurs in a setting of preexisting somnolence, although patients may not give such a history. For this reason, prescribers should continually reassess patients for drowsiness or sleepiness, especially since some of the events occur well after the start of treatment. Prescribers should also be aware that patients may not acknowledge drowsiness or sleepiness until directly questioned about drowsiness or sleepiness during specific activities.
Before initiating treatment with ropinirole extended-release tablets, patients should be advised of the potential to develop drowsiness and specifically asked about factors that may increase the risk with ropinirole extended-release tablets such as concomitant sedating medications, the presence of sleep disorders, and concomitant medications that increase ropinirole plasma levels (e.g., ciprofloxacin) [see Drug Interactions ( 7.1 )]. If a patient develops significant daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., driving a motor vehicle, conversations, eating, etc.), ropinirole extended-release tablets should ordinarily be discontinued [see Dosage and Administration for guidance in discontinuing ropinirole extended-release tablets ( 2.2 )]. If a decision is made to continue ropinirole extended-release tablets, patients should be advised to not drive and to avoid other potentially dangerous activities. There is insufficient information to establish that dose reduction will eliminate episodes of falling asleep while engaged in activities of daily living.
Syncope, sometimes associated with bradycardia, was observed during treatment with ropinirole in Parkinson’s disease patients.
In a placebo-controlled study involving patients with advanced Parkinson’s disease, syncope occurred in 2 of the 202 patients (1%) who received ropinirole extended-release tablets, and in none of the 191 patients who received placebo.
Because the study of ropinirole extended-release tablets excluded patients with significant cardiovascular disease, it is not known to what extent the estimated incidence figure applies to patients with Parkinson’s disease in clinical practice. Therefore, patients with significant cardiovascular disease should be treated with caution.
Dopamine agonists, in clinical studies and clinical experience, appear to impair the systemic regulation of blood pressure, with resulting postural hypotension, especially during dose escalation. In addition, patients with Parkinson’s disease appear to have an impaired capacity to respond to a postural challenge. For these reasons, patients being treated with dopaminergic agonists ordinarily (1) require careful monitoring for signs and symptoms of postural hypotension, especially during dose escalation, and (2) should be informed of this risk [see Patient Counseling Information ( 17.2 )].
In a placebo-controlled trial involving patients with advanced Parkinson’s disease, hypotension was reported as an adverse event in 5 of 202 patients (2%) receiving ropinirole extended-release tablets and in none of the 191 patients receiving placebo. Orthostatic hypotension was reported as an adverse event in 5% of patients receiving ropinirole extended-release tablets, and in 1% of placebo recipients.
An analysis of the randomized, double-blinded, placebo-controlled study in advanced Parkinson's disease was conducted using a variety of adverse event terms possibly suggestive of hypotension, including hypotension, orthostatic hypotension, dizziness, vertigo, and blood pressure decreased. This analysis showed a higher incidence of these events with ropinirole extended-release tablets (7%, 15 of 202) vs. placebo (3%, 6 of 191). This increased incidence was observed in a setting in which patients were very carefully titrated, and patients with clinically relevant cardiovascular disease or symptomatic orthostatic hypotension at baseline had been excluded from this study.
Orthostatic vital signs (semi-supine to standing) were monitored throughout the study in the advanced Parkinson’s disease study and changes related to ropinirole extended-release tablets (compared with placebo) from baseline were assessed.
The frequency of any orthostatic hypotension at any time during the study was 38% for ropinirole extended-release tablets vs. 31% for placebo for mild to moderate systolic blood pressure decrements (≥20 mm Hg), 63% for ropinirole extended-release tablets vs. 58% for placebo for mild to moderate diastolic blood pressure decrements (≥10 mm Hg), 10% for ropinirole extended-release tablets vs. 7% for placebo for severe diastolic blood pressure decrements (≥20 mm Hg), and 23% for ropinirole extended-release tablets vs. 19% for placebo for mild to moderate combined systolic and diastolic blood pressure decrements.
Significant decrements in blood pressure unrelated to standing were also reported in some patients taking ropinirole extended-release tablets. In the semi-supine position, the frequency was 10% for ropinirole extended-release tablets vs. 8% for placebo for severe systolic blood pressure decrease (≥40 mm Hg), and was 25% for ropinirole extended-release tablets vs. 21% for placebo for severe diastolic blood pressure decrease (≥20 mm Hg).
The increased incidence for hypotension and/or orthostatic hypotension was observed in both the titration and maintenance phases and in some cases persisted into the maintenance period after developing in the titration phase.
In the placebo-controlled study in advanced Parkinson’s disease, there were no clear effects of ropinirole extended-release tablets on average changes in blood pressure or heart rate compared with placebo. However, there was an increased incidence of patients treated with ropinirole extended-release tablets who met various outlier criteria, as described below.
In the semi-supine position, the frequency was 8% for ropinirole extended-release tablets vs. 5% for placebo for severe systolic blood pressure increase (≥40 mm Hg). In the standing position, the frequency was 9% for ropinirole extended-release tablets vs. 6% for placebo for severe systolic blood pressure increase (≥40 mm Hg).
In the semi-supine position, the frequency was 23% for ropinirole extended-release tablets vs. 18% for placebo for moderate pulse increase (≥15 beats/minute), and 19% for ropinirole extended-release tablets vs. 17% for placebo for moderate pulse decrease (≥15 beats/minute). In the standing position, the frequency was 2% for ropinirole extended-release tablets vs. <1% for placebo for severe pulse increase (≥30 beats/minute), and 24% for ropinirole extended-release tablets vs. 19% for placebo for moderate pulse decrease (≥15 beats/minute).
The increased incidence for various elevations of systolic and/or diastolic blood pressure and/or changes in pulse was observed in both the titration and maintenance phases as well as persisting into the maintenance period after developing in the titration phase. Elevation of blood pressure and/or changes in heart rate in patients taking ropinirole extended-release tablets should be considered when treating patients with cardiovascular disease.
In the double-blind, placebo-controlled, advanced Parkinson’s disease trial 8% (17 of 202) of patients receiving ropinirole extended-release tablets reported hallucination compared with 2% (4 of 191) patients receiving placebo. Hallucination led to discontinuation of treatment in 2% (4 of 202) of patients on ropinirole extended-release tablets and 1% (2 of 191) of patients on placebo.
The incidence of hallucination is increased in patients over age 65. Coadministration of entacapone and L-dopa with ropinirole may also increase the risk of hallucination. In a placebo-controlled clinical trial, hallucination occurred in 0 of 43 patients taking entacapone plus L-dopa, in 9 of 155 patients taking ropinirole extended-release tablets plus L-dopa (6%), and in 7 of 47 patients taking entacapone with ropinirole extended-release tablets plus L-dopa (15%).
Ropinirole extended-release tablets may potentiate the dopaminergic side effects of L-dopa and may cause and/or exacerbate preexisting dyskinesia in patients treated with L-dopa for Parkinson's disease. Decreasing the dose of a dopaminergic drug may ameliorate this side effect.
Patients with a major psychotic disorder should ordinarily not be treated with ropinirole extended-release tablets because of the risk of exacerbating the psychosis. In addition, many treatments for psychosis may decrease the effectiveness of ropinirole extended-release tablets [see Drug Interactions ( 7.4 )].
Withdrawal-Emergent Hyperpyrexia and Confusion
Although not reported during the clinical development of ropinirole, a symptom complex resembling the neuroleptic malignant syndrome (characterized by elevated temperature, muscular rigidity, altered consciousness, and autonomic instability), with no other obvious etiology, has been reported in association with rapid dose reduction, withdrawal of, or changes in dopaminergic therapy. Therefore, it is recommended that the dose be tapered at the end of treatment with ropinirole extended-release tablets as a prophylactic measure [see
Dosage and Administration
(
2.2
)].
Fibrotic Complications
Cases of retroperitoneal fibrosis, pulmonary infiltrates, pleural effusion, pleural thickening, pericarditis, and cardiac valvulopathy have been reported in some patients treated with ergot-derived dopaminergic agents. While these complications may resolve when the drug is discontinued, complete resolution does not always occur.
Although these adverse reactions are believed to be related to the ergoline structure of these compounds, whether other, nonergot-derived dopamine agonists, such as ropinirole or ropinirole extended-release tablets, can cause them is unknown.
A small number of reports have been received of possible fibrotic complications, including pleural effusion, pleural fibrosis, interstitial lung disease, and cardiac valvulopathy, in the development program and postmarketing experience for ropinirole. In the clinical development program (N=613), 2 patients treated with ropinirole extended-release tablets had pleural effusion. While the evidence is not sufficient to establish a causal relationship between ropinirole and these fibrotic complications, a contribution of ropinirole cannot be completely ruled out in rare cases.
Melanoma
Some epidemiologic studies have shown that patients with Parkinson’s disease have a higher risk (perhaps 2- to 4-fold higher) of developing melanoma than the general population. Whether the observed increased risk was due to Parkinson’s disease or other factors, such as drugs used to treat Parkinson’s disease, was unclear. Ropinirole is one of the dopamine agonists used to treat Parkinson’s disease. Although ropinirole has not been associated with an increased risk of melanoma specifically, its potential role as a risk factor has not been systematically studied. In the clinical development program (N=613), one patient treated with ropinirole extended-release tablets and also levodopa/carbidopa developed melanoma. Patients using ropinirole extended-release tablets should be made aware of these results and undergo periodic dermatologic screening.
Human
Because of observations made in albino rats (see below), ocular electroretinogram (ERG) assessments were conducted during a 2-year, double-blind, multicenter, flexible-dose, L-dopa controlled clinical study of immediate-release ropinirole in patients with Parkinson's disease. A total of 156 patients (78 on immediate-release ropinirole, mean dose 11.9 mg/day and 78 on L-dopa, mean dose 555.2 mg/day) were evaluated for evidence of retinal dysfunction through electroretinograms. There was no clinically meaningful difference between the treatment groups in retinal function over the duration of the study.
Albino Rats
Retinal degeneration was observed in albino rats in the 2-year carcinogenicity study at all doses tested (equivalent to 0.6 to 20 times the maximum recommended human dose (MRHD) of 24 mg/day on a mg/m2 basis), but was statistically significant at the highest dose (50 mg/kg/day). Retinal degeneration was not observed in pigmented rats after 3 months in a 2-year carcinogenicity study in albino mice, or in 1-year studies in monkeys or albino rats. The potential significance of this effect for humans has not been established, but cannot be disregarded because disruption of a mechanism that is universally present in vertebrates (e.g., disk shedding) may be involved.
Ropinirole binds to melanin-containing tissues (i.e., eyes, skin) in pigmented rats. After a single dose, long-term retention of drug was demonstrated, with a half-life in the eye of 20 days.
This product contains color additives including FD&C Yellow #6 in the 4 mg and 8 mg tablets.
The following adverse reactions are described in more detail in the Warnings and Precautions section of the label:
- Falling asleep during activities of daily living (5.1)
- Syncope (5.2)
- Symptomatic hypotension, hypotension, postural/orthostatic hypotension (5.3)
- Elevation of blood pressure and changes in heart rate (5.4)
- Hallucination (5.5)
- Dyskinesia (5.6)
- Major psychotic disorders (5.7)
- Events with dopaminergic therapy (5.8)
- Retinal pathology (5.9)
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug (or of another development program of a different formulation of the same drug) and may not reflect the rates observed in practice.
During the premarketing development of ropinirole extended-release tablets, patients with advanced Parkinson’s disease received ropinirole extended-release tablets or placebo as adjunctive therapy in 1 clinical trial. In a second trial, patients with early Parkinson’s disease were treated with ropinirole extended-release tablets or the immediate-release formulation of ropinirole without L-dopa.
Advanced Parkinson’s Disease (With L-dopa)
The most commonly observed adverse reactions (≥5% and numerically greater than placebo) in the 24-week, double-blind, placebo-controlled trial for the treatment of advanced Parkinson’s disease during treatment with ropinirole extended-release tablets were, in order of decreasing incidence: dyskinesia, nausea, dizziness, hallucination, somnolence, abdominal pain/discomfort, and orthostatic hypotension.
Approximately 6% of 202 patients treated with ropinirole extended-release tablets discontinued treatment due to adverse event(s) compared with 5% of 191 patients who received placebo. The adverse event most commonly causing discontinuation of treatment with ropinirole extended-release tablets was hallucination (2%).
Table 2 lists adverse reactions that occurred with a frequency of at least 2% (and were numerically greater than placebo) in patients with advanced Parkinson’s disease treated with ropinirole extended-release tablets who participated in the 26-week, double-blind, placebo-controlled study. In this study, either ropinirole extended-release tablets or placebo was used as an adjunct to L-dopa. Adverse reactions were generally mild or moderate in intensity.
|
Ropinirole E xte nded-Release Tablets |
Placebo | |
| Body System/Adverse Reaction | (n = 202)
% |
(n = 191)
% |
| Ear and labyrinth disorders | ||
| Vertigo | 4 | 2 |
| Gastrointestinal disorders | ||
| Nausea | 11 | 4 |
| Constipation | 4 | 2 |
| Abdominal pain/discomfort | 6 | 3 |
| Diarrhea | 3 | 2 |
| Dry mouth | 2 | <1 |
| General disorders | ||
| Edema peripheral | 4 | 1 |
| Injury, poisoning, and procedural complication | ||
| Fall* | 2 | 1 |
| Musculoskeletal and connective tissue disorders | ||
| Back pain | 3 | 2 |
| Nervous system disorders | ||
| Dyskinesia* | 13 | 3 |
| Dizziness | 8 | 3 |
| Somnolence | 7 | 4 |
| Psychiatric disorders | ||
| Hallucination | 8 | 2 |
| Anxiety | 2 | 1 |
| Vascular disorders | ||
| Orthostatic hypotension | 5 | 1 |
| Hypotension | 2 | 0 |
| Hypertension* | 3 | 2 |
*Dose-related
Although this study was not designed for optimally characterizing dose-related adverse reactions, there was a suggestion (based upon comparison of incidence of adverse reactions across dose ranges for ropinirole extended-release tablets and placebo) that the incidence for dyskinesia, hypertension, and fall was dose-related to ropinirole extended-release tablets.
The incidence for many adverse reactions with treatment with ropinirole extended-release tablets was increased relative to placebo (i.e., ropinirole extended-release tablets % - placebo % = treatment difference ≥2%) in either the titration or maintenance phases of the study. During the titration phase, an increased incidence (shown in descending order of % treatment difference) was observed for dyskinesia, nausea, abdominal pain/discomfort, orthostatic hypotension, dizziness, vertigo, hypertension, peripheral edema, and dry mouth. During the maintenance phase, an increased incidence was observed for dyskinesia, nausea, dizziness, hallucination, somnolence, fall, hypertension, abnormal dreams, constipation, chest pain, bronchitis, and nasopharyngitis. Some adverse reactions developing in the titration phase persisted (≥7 days) into the maintenance phase. These “persistent” adverse reactions included dyskinesia, hallucination, orthostatic hypotension, and dry mouth.
The incidence of adverse reactions was not clearly different between women and men.
Early Parkinson’s Disease (Without L-dopa)
The most commonly observed adverse reactions (≥5%) in the 36–week early Parkinson’s disease trial during treatment with ropinirole extended-release tablets were, in order of decreasing incidence: nausea (19%), somnolence (11%), abdominal pain/discomfort (7%), dizziness (6%), headache (6%), and constipation (5%). The type of adverse reactions and the frequency (i.e. incidence) with which they occurred were generally similar over the whole treatment period in this study of early Parkinson's disease patients who were initially treated with ropinirole extended-release tablets or the immediate-release formulation of ropinirole and subsequently crossed over to treatment with the other formulation.
During the titration phase, an increased incidence with ropinirole extended-release tablets compared with the immediate-release formulation of ropinirole (i.e., ropinirole extended-release formulation % - ropinirole immediate-release formulation % = treatment difference ≥2%), shown in descending order of % treatment difference, was observed for: constipation, hallucination, vertigo, abdominal pain/discomfort, nausea, vomiting, fall, headache, diarrhea, pyrexia, and flatulence. During the maintenance phase, an increased incidence was observed for fall, myalgia, and sleep disorder. Several adverse reactions developing in the titration phase persisted (≥7 days) into the maintenance phase. These “persistent” adverse reactions included: constipation, hallucination, muscle spasms, flatulence, insomnia, sleep disorder, abdominal pain/discomfort, cough, and nasopharyngitis.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug (or of another development program of a different formulation of the same drug) and may not reflect the rates observed in practice.
In patients with advanced Parkinson's disease who were treated with the immediate-release formulation of ropinirole, the most common adverse reactions (≥5% treatment difference from placebo; presented in order of decreasing treatment difference frequency) were dyskinesia (21%), somnolence (12%), nausea (12%), dizziness (10%), confusion (7%), hallucinations (6%), headache (5%), and increased sweating (5%). In patients with early Parkinson's disease who were treated with the immediate-release formulation of ropinirole, the most common adverse reactions (≥5% treatment difference from placebo; presented in order of decreasing treatment difference frequency) were nausea (38%), somnolence (34%), dizziness (18%), syncope (11%), viral infection (8%), fatigue (7%), leg edema (6%), asthenia (5%), and dyspepsia (5%).
In vitro metabolism studies showed that CYP1A2 is the major enzyme responsible for the metabolism of ropinirole. There is thus the potential for inducers or inhibitors of this enzyme to alter the clearance of ropinirole. Therefore, if therapy with a drug known to be a potent inducer or inhibitor of CYP1A2 is stopped or started during treatment with ropinirole, adjustment of the dose of ropinirole may be required.
Coadministration of ciprofloxacin, an inhibitor of CYP1A2, with immediate-release ropinirole increased the AUC of ropinirole by 84% on average and Cmax by 60% [see Clinical Pharmacology ( 12.3 )].
Cigarette smoking is expected to increase the clearance of ropinirole since CYP1A2 is known to be induced by smoking. In one study in patients with Restless Legs Syndrome, cigarette smokers had an approximate 30% lower Cmax and a 38% lower AUC than did nonsmokers, when those parameters were normalized for dose.
There is no evidence of interaction between ropinirole and other CYP1A2 substrates (e.g., theophylline).
Ropinirole and its circulating metabolites do not inhibit or induce P450 enzymes therefore ropinirole is unlikely to affect the pharmacokinetics of other drugs by a P450 mechanism [see Clinical Pharmacology ( 12.3 )].
Coadministration of carbidopa + L-dopa (SINEMET®*) with immediate-release ropinirole had no effect on the steady-state pharmacokinetics of ropinirole. Oral administration of immediate-release ropinirole increased mean steady-state Cmax of L-dopa by 20%, but its AUC was unaffected [see Clinical Pharmacology ( 12.3 )].
Population pharmacokinetic analysis revealed that higher doses of estrogens (usually associated with hormone replacement therapy [HRT]) reduced the oral clearance of ropinirole by approximately 35%. Dosage adjustment is not needed for initiating ropinirole extended-release tablets in patients on estrogen therapy because patients are individually titrated with ropinirole extended-release tablets to tolerance or adequate effect. If estrogen therapy is stopped or started during treatment with ropinirole extended-release tablets, then adjustment of the dose of ropinirole extended-release tablets may be required.
Since ropinirole is a dopamine agonist, it is possible that dopamine antagonists such as neuroleptics (e.g., phenothiazines, butyrophenones, thioxanthenes) or metoclopramide may diminish the effectiveness of ropinirole extended-release tablets. Patients with a history or presence of major psychotic disorders should be treated with dopamine agonists only if the potential benefits outweigh the risks.
Teratogenic Effects: Pregnancy Category C. There are no adequate and well-controlled studies using ropinirole in pregnant women. Ropinirole extended-release tablets should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus.
In animal reproduction studies, ropinirole has been shown to have adverse effects on embryo-fetal development, including teratogenic effects. Treatment of pregnant rats with ropinirole during organogenesis resulted in decreased fetal body weight, increased fetal death, and digital malformations at 24, 36, and 60 times the MRHD, respectively. The combined administration of ropinirole at 8 times the MRHD and a clinically relevant dose of L-dopa to pregnant rabbits during organogenesis produced a greater incidence and severity of fetal malformations (primarily digit defects) than were seen in the offspring of rabbits treated with L-dopa alone. In a perinatal-postnatal study in rats, impaired growth and development of nursing offspring and altered neurological development of female offspring were observed when dams were treated with 4 times the MRHD.
Ropinirole inhibits prolactin secretion in humans and could potentially inhibit lactation.
Ropinirole has been detected in the milk of lactating rats. Although many drugs are excreted in human milk, transfer of ropinirole into human milk has not been demonstrated. Due to the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of ropinirole to the mother.
Safety and effectiveness in the pediatric population have not been established.
Dosage adjustment is not necessary in the elderly (above 65 years), as the dose of ropinirole extended-release tablets is to be individually titrated to clinical response [see Clinical Pharmacology ( 12.3 )]. Pharmacokinetic studies conducted in patients demonstrated that oral clearance of ropinirole is reduced by 15% in patients above 65 years of age compared to younger patients.
Of the total number of patients who participated in clinical trials of ropinirole extended-release tablets for Parkinson’s disease, 387 patients were 65 and over and 107 patients were 75 and over. Among patients receiving ropinirole extended-release tablets, hallucination was more common in elderly subjects (10%) compared with non-elderly subjects (2%). The incidence of overall adverse events increased with increasing age for both patients receiving ropinirole extended-release tablets and placebo.
No dosage adjustment of ropinirole is needed in patients with moderate renal impairment (creatinine clearance of 30 to 50 mL/min). The use of ropinirole in patients with severe renal impairment has not been studied.
The pharmacokinetics of ropinirole have not been studied in patients with hepatic impairment. Since patients with hepatic impairment may have higher plasma levels and lower clearance, ropinirole should be titrated with caution in these patients.
Ropinirole is not a controlled substance.
Animal studies and human clinical trials with ropinirole did not reveal any potential for drug-seeking behavior or physical dependence.
In the Parkinson's disease program, there have been patients who accidentally or intentionally took more than their prescribed dose of ropinirole. The largest overdose reported with immediate-release ropinirole in clinical trials was 435 mg taken over a 7-day period (62.1 mg/day). Of patients who received a dose greater than 24 mg/day, reported symptoms included adverse events commonly reported during dopaminergic therapy (nausea, dizziness), as well as visual hallucination, hyperhidrosis, claustrophobia, chorea, palpitations, asthenia, and nightmares. Additional symptoms reported for doses of 24 mg or less or for overdoses of unknown amount included vomiting, increased coughing, fatigue, syncope, vasovagal syncope, dyskinesia, agitation, chest pain, orthostatic hypotension, somnolence, and confusional state.
The symptoms of overdose with ropinirole are generally related to its dopaminergic activity; these symptoms may be alleviated by appropriate treatment with dopamine antagonists such as neuroleptics or metoclopramide. General supportive measures are recommended. Vital signs should be maintained, if necessary. Removal of any unabsorbed material (e.g., by gastric lavage) may be considered.
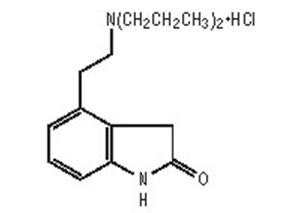
Ropinirole extended-release tablet (ropinirole) is an orally administered non-ergoline dopamine agonist. It is supplied as the hydrochloride salt of ropinirole 4-[2-(dipropylamino)ethyl]-1,3-dihydro-2H-indol-2-one and has a molecular formula of C16H24N2O•HCl. The molecular weight is 296.84 (260.38 as the free base).
The structural formula is:
Ropinirole hydrochloride is a white to yellow solid with a melting range of 243° to 250°C and a solubility of 133 mg/mL in water. Ropinirole extended-release tablets are formulated as a single-layer extended-release matrix tablet core that is completely surrounded by a barrier film-coating that further controls the drug release. Each biconvex, oval-shaped tablet contains 2.28 mg, 4.56 mg, 6.84 mg, 9.12 mg, or 13.68 mg ropinirole hydrochloride equivalent to ropinirole 2 mg, 4 mg, 6 mg, 8 mg, or 12 mg, respectively. Inactive ingredients consist of hypromellose, mannitol, glyceryl behenate, lactose monohydrate, hydrogenated castor oil, povidone, polyvinyl acetate dispersion 30% (stabilized with povidone and sodium lauryl sulfate), talc, magnesium stearate, colloidal silicon dioxide, triethyl citrate, titanium dioxide, polydextrose, triacetin, polyethylene glycol 8000, and one or more of the following: iron oxide red (2 mg), iron oxide yellow (2 mg and 12 mg), FD&C Yellow #6/Sunset Yellow aluminum lake (4 mg and 8 mg), FD&C Blue #2/Indigo Carmine aluminum lake (4 mg, 8 mg and 12 mg), and FD&C Red #40/Allura Red aluminum lake (8 mg).
Ropinirole is a non-ergoline dopamine agonist with high relative in vitro specificity and full intrinsic activity at the D2 and D3 dopamine receptor subtypes, binding with higher affinity to D3 than to D2 or D4 receptor subtypes.
Ropinirole has moderate in vitro affinity for opioid receptors. Ropinirole and its metabolites have negligible in vitro affinity for dopamine D1, 5-HT1, 5-HT2, benzodiazepine, GABA, muscarinic, alpha1-, alpha2-, and beta-adrenoreceptors.
The precise mechanism of action of ropinirole as a treatment for Parkinson’s disease is unknown, although it is believed to be due to stimulation of postsynaptic dopamine D2-type receptors within the caudate-putamen in the brain. This conclusion is supported by studies that show that ropinirole improves motor function in various animal models of Parkinson’s disease. In particular, ropinirole attenuates the motor deficits induced by lesioning the ascending nigrostriatal dopaminergic pathway with the neurotoxin 1-methyl-4phenyl-1,2,3,6-tetrahydropyridine (MPTP) in primates. The relevance of D3 receptor binding in Parkinson’s disease is unknown.
Clinical experience with dopamine agonists, including ropinirole, suggests an association with impaired ability to regulate blood pressure with resulting postural hypotension, especially during dose escalation. In some subjects in clinical trials, blood pressure changes were associated with the emergence of orthostatic symptoms, bradycardia, and, in one case in a healthy volunteer, transient sinus arrest with syncope.
The mechanism of postural hypotension induced by ropinirole is presumed to be due to a D2-mediated blunting of the noradrenergic response to standing and subsequent decrease in peripheral vascular resistance. Nausea is a common concomitant symptom of orthostatic signs and symptoms.
At oral doses as low as 0.2 mg, ropinirole suppressed serum prolactin concentrations in healthy male volunteers. Immediate-release ropinirole had no dose-related effect on ECG wave form and rhythm in young, healthy, male volunteers in the range of 0.01 to 2.5 mg. Immediate-release ropinirole had no dose- or exposure-related effect on mean QT intervals in healthy male and female volunteers titrated to doses up to 4 mg/day. The effect of ropinirole on QT intervals at higher exposures achieved either due to drug interactions, hepatic impairment, or at higher doses has not been systematically evaluated.
Absorption
In clinical studies with immediate-release ropinirole, over 88% of a radiolabeled dose was recovered in urine, and the absolute bioavailability was 45% to 55%, indicating approximately 50% first-pass effect.
Ropinirole displayed linear kinetics up to doses of 24 mg/day (8 mg immediate-release, 3 times a day). Increase in systemic exposure of ropinirole following oral administration of 2 to 12 mg of ropinirole extended-release tablets was approximately dose-proportional. For ropinirole extended-release tablets, steady-state concentrations of ropinirole are expected to be achieved within 4 days of dosing.
Relative bioavailability of ropinirole extended-release tablets compared with immediate-release tablets was approximately 100%. In a repeat-dose study in patients with Parkinson’s disease using 8 mg ropinirole extended-release tablets, the dose-normalized AUC(0-24) and Cmin for ropinirole extended-release tablets and immediate-release ropinirole were similar. Dose-normalized Cmax was, on average, 12% lower for ropinirole extended-release tablets than for the immediate-release formulation and the median time-to-peak concentration was 6 to 10 hours. In a single-dose study, administration of ropinirole extended-release tablets to healthy volunteers with food (i.e., high-fat meal) increased AUC by approximately 30% and Cmax by approximately 44%, compared with dosing under fasted conditions. In a repeat-dose study in patients with Parkinson’s disease, food (i.e., high-fat meal) increased AUC by approximately 20% and Cmax by approximately 44%; Tmax was prolonged by 3 hours (median prolongation) compared with dosing under fasted conditions [see Dosage and Administration ( 2.1 )].
Distribution
Ropinirole is widely distributed throughout the body, with an apparent volume of distribution of 7.5 L/kg (cv = 32%). It is up to 40% bound to plasma proteins and has a blood-to-plasma ratio of 1:1.
Metabolism
Ropinirole is extensively metabolized by the liver. The major metabolic pathways are N-despropylation and hydroxylation to form the inactive N-despropyl metabolite and hydroxy metabolites. The N-despropyl metabolite is converted to carbamyl glucuronide, carboxylic acid, and N-despropyl hydroxy metabolites. The hydroxy metabolite of ropinirole is rapidly glucuronidated. In vitro studies indicate that the major cytochrome P450 isozyme involved in the metabolism of ropinirole is CYP1A2, an enzyme known to be induced by smoking and omeprazole, and inhibited by, for example, fluvoxamine, mexiletine, and the older fluoroquinolones such as ciprofloxacin and norfloxacin.
Elimination
The clearance of ropinirole after oral administration to patients is 47 L/hr (cv = 45%) and its elimination half-life is approximately 6 hours. Less than 10% of the administered dose is excreted as unchanged drug in urine. N-despropyl ropinirole is the predominant metabolite found in urine (40%), followed by the carboxylic acid metabolite (10%), and the glucuronide of the hydroxy metabolite (10%).
Drug Interactions
Ciprofloxacin
Coadministration of ciprofloxacin (500 mg twice daily), an inhibitor of CYP1A2, with immediate-release ropinirole (2 mg 3 times daily) increased ropinirole AUC by 84% on average and Cmax by 60% (n = 12 patients).
Digoxin
Coadministration of immediate-release ropinirole (2 mg 3 times daily) with digoxin (0.125 to 0.25 mg once daily) did not alter the steady-state pharmacokinetics of digoxin in 10 patients.
Theophylline
Administration of theophylline (300 mg twice daily, a substrate of CYP1A2) did not alter the steady-state pharmacokinetics of immediate-release ropinirole (2 mg 3 times daily) in 12 patients with Parkinson’s disease. Immediate-release ropinirole (2 mg 3 times daily) did not alter the pharmacokinetics of theophylline (5 mg/kg IV) in 12 patients with Parkinson’s disease.
L-dopa
Coadministration of carbidopa + L-dopa (SINEMET®* 10/100 mg twice daily) with immediate-release ropinirole (2 mg 3 times daily) had no effect on the steady-state pharmacokinetics of ropinirole (n = 28 patients). Oral administration of immediate-release ropinirole 2 mg 3 times daily increased mean steady-state Cmax of L-dopa by 20%, but its AUC was unaffected (n = 23 patients).
Estrogens
Population pharmacokinetic analysis revealed that higher doses of estrogens (usually associated with hormone replacement therapy [HRT]) reduced the oral clearance of ropinirole by approximately 35%.
Commonly Administered Drugs
Population analysis showed that commonly administered drugs, e.g., selegiline, amantadine, tricyclic antidepressants, benzodiazepines, ibuprofen, thiazides, antihistamines, and anticholinergics, did not affect the oral clearance of ropinirole.
Population Subgroups
Because therapy with ropinirole extended-release tablets is initiated at a low dose and gradually titrated upward according to clinical tolerability to obtain the optimum therapeutic effect, adjustment of the initial dose based on gender, weight, or age is not necessary.
Age
Oral clearance of ropinirole is reduced by approximately 15% in patients above 65 years of age compared with younger patients. Dosage adjustment is not necessary in the elderly (above 65 years), as the dose of ropinirole is individually titrated to clinical response.
Gender
Female and male patients showed similar oral clearance.
Race
The influence of race on the pharmacokinetics of ropinirole has not been evaluated.
Renal Impairment
Based on population pharmacokinetic analysis, no difference was observed in the pharmacokinetics of ropinirole in patients with moderate renal impairment (creatinine clearance between 30 to 50 mL/min) compared with an age-matched population with creatinine clearance above 50 mL/min. Therefore, no dosage adjustment is necessary in patients with moderate renal impairment. The use of ropinirole in patients with severe renal impairment has not been studied.
The effect of hemodialysis on ropinirole clearance is not known, but because of the relatively high apparent volume of distribution of ropinirole (7.5 L/kg), significant removal of ropinirole by hemodialysis is unlikely.
Hepatic Impairment
The pharmacokinetics of ropinirole have not been studied in patients with hepatic impairment. These patients may have higher plasma levels and lower clearance of ropinirole than patients with normal hepatic function. Ropinirole extended-release tablets should be titrated with caution in this population.
Other Diseases
Population pharmacokinetic analysis revealed no change in the oral clearance of ropinirole in patients with concomitant diseases such as hypertension, depression, osteoporosis/arthritis, and insomnia compared with patients who had Parkinson’s disease only.
Two-year carcinogenicity studies were conducted in Charles River CD-1 mice at doses of 5, 15, and 50 mg/kg/day and in Sprague-Dawley rats at doses of 1.5, 15, and 50 mg/kg/day (top doses which, based on mg/m2, are equivalent to 10 and 20 times, respectively, the MRHD of 24 mg/day). In the male rat, there was a significant increase in testicular Leydig cell adenomas at all doses tested, i.e., ≥1.5 mg/kg (0.6 times the MRHD on a mg/m2 basis). This finding is of questionable significance because the endocrine mechanisms believed to be involved in the production of Leydig cell hyperplasia and adenomas in rats are not relevant to humans. In the female mouse, there was an increase in benign uterine endometrial polyps at a dose of 50 mg/kg/day (10 times the MRHD on a mg/m2 basis). Ropinirole was not mutagenic or clastogenic in the in vitro Ames test, the in vitro chromosome aberration test in human lymphocytes, the in vitro mouse lymphoma (L1578Y cells) assay, and the in vivo mouse micronucleus test.
When administered to female rats prior to and during mating and throughout pregnancy, ropinirole caused disruption of implantation at doses of 20 mg/kg/day (8 times the MRHD on a mg/m2 basis) or greater. This effect is thought to be due to the prolactin-lowering effect of ropinirole. In humans, chorionic gonadotropin, not prolactin, is essential for implantation. In rat studies using low doses (5 mg/kg) during the prolactin-dependent phase of early pregnancy (gestation days 0 to 8), ropinirole did not affect female fertility at dosages up to 100 mg/kg/day (40 times the MRHD on a mg/m2 basis). No effect on male fertility was observed in rats at dosages up to 125 mg/kg/day (50 times the MRHD on a mg/m2 basis).
The effectiveness of the immediate-release formulation of ropinirole (ropinirole tablets) in the treatment of early and advanced Parkinson’s disease was initially established in 3 randomized, double-blind, placebo-controlled trials.
The effectiveness of ropinirole extended-release tablets in the treatment of Parkinson’s disease was supported by 2 randomized, double-blind, multicenter clinical trials and clinical pharmacokinetic considerations. One trial conducted in advanced Parkinson’s disease patients compared ropinirole extended-release tablets with placebo as adjunctive therapy to L-dopa. A second trial compared ropinirole extended-release tablets with ropinirole tablets in early phase Parkinson’s disease patients not receiving L-dopa.
In these studies a variety of measures were used to assess the effects of treatment (e.g., patient diaries recording time “on” and “off,” tolerability of L-dopa dose reductions, and the Unified Parkinson’s Disease Rating Scale [UPDRS] scores). The UPDRS is a multi-item rating scale evaluating mentation (Part I), activities of daily living (Part II), motor performance (Part III), and complications of therapy (Part IV). Part III of the UPDRS contains 14 items designed to assess the severity of the cardinal motor findings in patients with Parkinson’s disease (e.g., tremor, rigidity, bradykinesia, postural instability, etc.) scored for different body regions and has a maximum (worst) score of 108.
The effectiveness of ropinirole extended-release tablets as adjunctive therapy to L-dopa in patients with Parkinson’s disease was established in a randomized, double-blind, placebo-controlled, parallel group, 24-week clinical trial in 393 patients (Hoehn & Yahr criteria Stages II-IV) who were not adequately controlled by L-dopa therapy. Patients were allowed to be on concomitant selegiline, amantadine, anticholinergics, and catechol-O-methyltransferase (COMT) inhibitors provided the doses were stable for at least 4 weeks prior to screening and throughout the trial. The primary efficacy endpoint evaluated was the mean change from baseline in total awake time spent “off”.
Patients in this study had a mean disease duration of 8.6 years, a mean duration of exposure to L-dopa of 6.5 years, had experienced a minimum of 3 hours awake time “off” with a baseline average of approximately 7 hours awake time “off”, and had a mean baseline UPDRS motor score of approximately 30 points with similar mean data in each treatment group. The mean baseline dose of L-dopa in the group receiving ropinirole extended-release tablets was 824 mg/day and 776 mg/day for the placebo group. Patients initiated treatment at 2 mg/day for 1 week followed by increases of 2 mg/day at weekly intervals to a minimum dose of 6 mg/day. The following week, the total daily dose of ropinirole extended-release tablets could be further increased (based upon therapeutic response and tolerability) to 8 mg/day. Once a daily dose of 8 mg/day was reached, the background L-dopa dosage was reduced. Thereafter, the daily dose could be increased by up to 4 mg/day approximately every 2 weeks until an optimal dose was achieved (based upon therapeutic response and tolerability). The mean dose of ropinirole extended-release tablets at the end of Week 24 was 18.8 mg/day. Dose titrations were based upon the degree of symptom control, planned L-dopa dosage reduction, and/or tolerability. The maximal allowed daily dosage for ropinirole extended-release tablets was 24 mg/day.
The primary efficacy endpoint was mean change from baseline in total awake time spent “off” at Week 24. At baseline the mean total awake time spent “off” was approximately 7 hours in each treatment group. At Week 24, the total awake time spent “off”, on average, had decreased by approximately 2 hours in the group receiving ropinirole extended-release tablets and by approximately half an hour in the placebo group. The adjusted mean difference in total awake time spent “off” between ropinirole extended-release tablets and placebo was -1.7 hours, which was statistically significant (ANCOVA, p< 0.0001). Results for this endpoint showing the statistical superiority of ropinirole extended-release tablets over placebo are presented in Table 3.
| Ropinirole Extended-Release Tablets | Placebo | |
| (n = 201) | (n = 190) | |
| Mean “Off” time at Baseline (hours) | 7.0 | 7.0 |
| Mean Change from Baseline in “Off “time (hours) | -2.1 | -0.4 |
The difference between groups in favor of ropinirole extended-release tablets, with regard to a decrease in total “off” hours, was primarily related to an increase in total “on” hours without troublesome dyskinesia. Patients treated with ropinirole extended-release tablets had a mean reduction in L-dopa dose of 278 mg/day (34%) while patients treated with placebo had a mean reduction of 164 mg/day (21%). In patients who reduced their L-dopa dose, reduction was sustained in 93% of patients treated with ropinirole extended-release tablets and in 72% of patients treated with placebo (p<0.001).
A 36-week multicenter, double-blind, titration/3-period maintenance, cross-over study compared the efficacy of ropinirole extended-release tablets with the immediate-release formulation of ropinirole (IR) in 161 patients with early phase Parkinson’s disease (Hoehn & Yahr Stages I-III) with limited prior exposure to L-dopa or dopamine agonists. Eligible subjects were randomized (1:1:1:1) to 4 treatment sequences (2 were titrated on the immediate-release formulation of ropinirole and 2 on ropinirole extended-release tablets). The ropinirole immediate-release titration was slower in rate than that of ropinirole extended-release tablets. Patients were titrated, during the 12-week titration period, to their optimal dosage, based upon tolerance and therapeutic response. This was followed by 3 consecutive 8-week maintenance periods, during which patients were either maintained on the prior formulation or switched to the alternative formulation. All switches were performed overnight by using the approximately equivalent doses of ropinirole. The primary efficacy endpoint was the change of UPDRS motor score within each maintenance period. Patients in all 4 groups started out with similar UPDRS motor scores (about 21) at baseline. All 4 groups exhibited similar improvement in UPDRS total motor scores from baseline until the completion of the titration phase, with a change in score of about -9 observed for the groups started on the immediate-release formulation of ropinirole and of about -10 for the groups started on ropinirole extended-release tablets. No difference was observed between groups when switches were made between identical formulations or between different formulations. This suggests therapeutic dosage equivalence between ropinirole immediate-release and ropinirole extended-release formulations.
The optimal daily dose at the end of the titration period for patients on the immediate-release formulation of ropinirole was substantially lower (mean 7 mg) compared to the dose at the end of the titration period for patients on ropinirole extended-release tablets (mean 18 mg). In this study, the marked difference in the final optimal dosages suggests that the higher doses afforded no additional benefit when compared to the lower doses [see Dosage and Administration ( 2 )].
Each biconvex, oval, barrier film-coated tablet contains ropinirole hydrochloride equivalent to the labeled amount of ropinirole as follows:
- 2 mg: pink tablets debossed with WATSON on one side and 3611 on the other side, in bottles of 30 (NDC 0591–3611–30), 90 (NDC 0591–3611-19) and 500 (NDC 0591–3611-05).
- 4 mg: beige tablets debossed with WATSON on one side and 3613 on the other side, in bottles of 30 (NDC 0591–3613–30), 90 (NDC 0591–3613-19) and 500 (NDC 0591–3613-05).
- 6 mg: white tablets debossed with WATSON on one side and 3700 on the other side, in bottles of 30 (NDC 0591–3700–30), 90 (NDC 0591–3700-19) and 500 (NDC 0591–3700-05).
- 8 mg: red tablets debossed with WATSON on one side and 3614 on the other side, in bottles of 30 (NDC 0591–3614–30), 90 (NDC 0591–3614-19) and 500 (NDC 0591–3614-05).
- 12 mg: green tablets debossed with WATSON on one side and 3612 on the other side, in bottles of 30 (NDC 0591–3612–30), 90 (NDC 0591–3612-19) and 500 (NDC 0591–3612-05).
Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Dispense in a tight, light-resistant container as defined in the USP.
See FDA-Approved Patient Labeling (17.9)
Physicians should instruct their patients to read the Patient Information leaflet before starting therapy with ropinirole extended-release tablets and to reread it upon prescription renewal for new information regarding the use of ropinirole extended-release tablets.
- Patients should be instructed to take ropinirole extended-release tablets only as prescribed. If a dose is missed, patients should be advised not to double their next dose.
- Ropinirole extended-release tablets can be taken with or without food. Taking ropinirole extended-release tablets with food may reduce the occurrence of nausea [see
Dosage and Administration
(
2.1
)]
- Ropinirole extended-release tablets should be swallowed whole. They should not be chewed, crushed, or divided [see
Dosage and Administration
(
2.1
)]
- Ropinirole is the active ingredient that is in both ropinirole extended-release tablets and ropinirole tablets (the immediate-release formulation). Ask your patient if they are taking another medication containing ropinirole.
Patients should be advised that they may develop postural (orthostatic) hypotension with or without symptoms such as dizziness, nausea, syncope, and sometimes sweating. Hypotension and/or orthostatic symptoms may occur more frequently during initial therapy or with an increase in dose at any time (cases have been seen after weeks of treatment). Accordingly, patients should be cautioned against standing up rapidly after sitting or lying down, especially if they have been doing so for prolonged periods, and especially at the initiation of treatment with ropinirole extended-release tablets [see Warnings and Precautions ( 5.2 , 5.3 )].
Patients should be alerted to the possibility of increases in blood pressure during treatment with ropinirole extended-release tablets. Exacerbation of hypertension may occur. Medication dose adjustment may be necessary if elevation of blood pressure is sustained over multiple evaluations. Patients with cardiovascular disease, who may not tolerate marked changes in heart rate, should also be alerted to the possibility that they may experience significant increases or decreases in heart rate during treatment with ropinirole extended-release tablets [see Warnings and Precautions ( 5.4 )].
Patients should be alerted to the potential sedating effects caused by ropinirole extended-release tablets, including somnolence and the possibility of falling asleep while engaged in activities of daily living. Since somnolence is a frequent adverse reaction with potentially serious consequences, patients should neither drive a car nor engage in other potentially dangerous activities until they have gained sufficient experience with ropinirole extended-release tablets to gauge whether or not it affects their mental and/or motor performance adversely. Patients should be advised that if increased somnolence or episodes of falling asleep during activities of daily living (e.g., conversations, eating, driving a motor vehicle, etc.) are experienced at any time during treatment, they should not drive or participate in potentially dangerous activities until they have contacted their physician.
Because of possible additive effects, caution should be advised when patients are taking other sedating medications, alcohol, or other CNS depressants (e.g., benzodiazepines, antipsychotics, antidepressants, etc.) in combination with ropinirole extended-release tablets or when taking concomitant medications that increase plasma levels of ropinirole (e.g., ciprofloxacin) [see Warnings and Precautions ( 5.1 )].
Patients should be informed they may experience hallucinations (unreal visions, sounds, or sensations) while taking ropinirole. The elderly are at greater risk than younger patients with Parkinson's disease; and the risk is greater in patients who are taking ropinirole with L-dopa or taking higher doses of ropinirole, and may also be further increased in patients taking any other drugs that increase dopaminergic tone [see Warnings and Precautions ( 5.5 )].
There have been reports of patients experiencing intense urges to gamble, increased sexual urges, and other intense urges and the inability to control these urges while taking one or more of the medications that increase central dopaminergic tone, that are generally used for the treatment of Parkinson’s disease or Restless Legs Syndrome, including ropinirole. In the clinical development program (N = 613), 6 patients treated with ropinirole extended-release tablets exhibited compulsive behaviors consisting of pathological gambling and/or hypersexuality. Although it is not proven that the medications caused these events, these urges were reported to have stopped in some cases when the dose was reduced or the medication was stopped. Prescribers should ask patients about the development of new or increased gambling urges, sexual urges or other urges while being treated with ropinirole extended-release tablets. Patients should inform their physician if they experience new or increased gambling urges, increased sexual urges or other intense urges while taking ropinirole extended-release tablets. Physicians should consider dose reduction or stopping the medication if a patient develops such urges while taking ropinirole extended-release tablets.
Because of the possibility that ropinirole may be excreted in breast milk, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother [see Use in Specific Populations ( 8.3 )]. Patients should be advised that ropinirole could inhibit lactation, as ropinirole inhibits prolactin secretion.
Because ropinirole has been shown to have adverse effects on embryo-fetal development, including teratogenic effects, in animals, and because experience in humans is limited, patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy [see Use in Specific Populations ( 8.1 )].
Patient labeling is provided as a tear-off leaflet at the end of this full prescribing information.
Physicians should instruct their patients to read the Patient Information leaflet before starting therapy with ropinirole extended-release tablets and to reread it upon prescription renewal for new information regarding the use of ropinirole extended-release tablets.
*SINEMET is a registered trademark of Merck & Co., Inc.
Manufactured by:
Watson Laboratories, Inc.
Corona, CA 92880 USA
Distributed by:
Watson
Pharma
, Inc.
Parsippany, NJ 07054
Revised: December 2011 201173-1
PHARMACIST--DETACH HERE AND GIVE INSTRUCTIONS TO PATIENT
PATIENT INFORMATION
rOPINIR ole Extended-Release Tablets
Rx only
| IMPORTANT NOTE: Ropinirole extended-release tablets have not been studied in Restless Legs Syndrome (RLS) and are not approved for the treatment of RLS. |
Read this information completely before you start taking ropinirole extended-release tablets. Read the information each time you get more medicine. There may be new information. This leaflet provides a summary about ropinirole extended-release tablets. It does not include everything there is to know about your medicine. This information should not take the place of discussions with your healthcare provider about your medical condition or treatment with ropinirole extended-release tablets.
What are ropinirole extended-release tablets?
Ropinirole extended-release tablets are a long-acting prescription medicine containing ropinirole (taken once a day) used to treat Parkinson’s disease.
You should not be taking more than one medicine containing ropinirole. Inform your physician if you are taking any other medicine containing ropinirole.
Ropinirole extended-release tablets have not been studied in children.
What is the most important information I should know about ropinirole extended-release tablets?
Ropinirole extended-release tablets can cause serious side effects including:
-
Falling asleep during normal activities. You may fall asleep while doing normal activities such as driving a car, doing physical tasks, or using hazardous machinery while taking ropinirole extended-release tablets. You may suddenly fall asleep without being drowsy or without warning. This may result in having accidents. Your chances of falling asleep while doing normal activities while taking ropinirole extended-release tablets are greater if you take other medicines that cause drowsiness. Tell your healthcare provider right away if this happens. Before starting ropinirole extended-release tablets, be sure to tell your healthcare provider if you take any medicines that make you drowsy.
-
Changes in blood pressure. Ropinirole extended-release tablets can decrease or increase your blood pressure. Lowering of your blood pressure is of special concern. If you faint, feel dizzy, nauseated, or sweaty when you stand up from sitting or lying down, this may mean that your blood pressure is decreased. If you notice this, you should contact your healthcare provider. Also, when changing position from lying down or sitting to standing up, you should do it carefully and slowly. Lowering of your blood pressure can happen especially when you start taking ropinirole extended-release tablets or when your dose is increased.
-
Fainting. Fainting can occur, and sometimes your heart rate may be decreased. This can happen especially when you start taking ropinirole extended-release tablets or your dose is increased. Tell your healthcare provider if you faint or feel dizzy.
-
Hallucinations (unreal visions, sounds, or sensations) can occur in patients taking ropinirole extended-release tablets. The chances of having hallucinations are higher in patients with Parkinson's disease who are elderly, taking ropinirole extended-release tablets with other Parkinson’s disease drugs, or taking higher doses of ropinirole extended-release tablets. If you have hallucinations, talk with your healthcare provider.
- Uncontrolled sudden movements. Ropinirole extended-release tablets may cause uncontrolled sudden movements or make such movements you already have worse or more frequent. Tell your healthcare provider if this happens. The doses of your anti-Parkinson’s medicines may need to be changed.
Unusual urges. Some patients taking ropinirole extended-release tablets get urges to behave in a way unusual for them. Examples of this are an unusual urge to gamble or increased sexual urges and behaviors. If you notice or your family notices that you are developing any unusual behaviors, talk to your healthcare provider.
See “What are the possible side effects of ropinirole extended-release tablets?”
What should I tell my healthcare provider before taking ropinirole extended-release tablets?
Be sure to tell your healthcare provider if you:
- have daytime sleepiness from a sleep disorder or have unexpected or unpredictable sleepiness or periods of sleep.
- are taking any other prescription or over-the-counter medicines. Some of these medicines may increase your chances of getting side effects while taking ropinirole extended-release tablets.
- start or stop taking other medicines while you are taking ropinirole extended-release tablets. This may increase your chances of getting side effects.
- start or stop smoking while you are taking ropinirole extended-release tablets. Smoking may decrease the treatment effect of ropinirole extended-release tablets.
- feel dizzy, nauseated, sweaty, or faint when you first stand up from sitting or lying down.
- drink alcoholic beverages. This may increase your chances of becoming drowsy or sleepy while taking ropinirole extended-release tablets.
- have high or low blood pressure.
- are pregnant or plan to become pregnant. Ropinirole extended-release tablets should only be used during pregnancy if needed.
- are breastfeeding. It is not known if ropinirole passes into your breast milk. Talk to your healthcare provider to decide whether you will breastfeed or take ropinirole extended-release tablets.
- are allergic to any of the ingredients in ropinirole extended-release tablets. See the end of this Patient Information leaflet for a complete list of the ingredients in ropinirole extended-release tablets.
How should I take ropinirole extended-release tablets for Parkinson's disease?
- Take ropinirole extended-release tablets exactly as directed by your healthcare provider.
- Do not suddenly stop taking ropinirole extended-release tablets without talking to your healthcare provider. If you stop this medicine suddenly, you may develop fever, confusion, or severe muscle stiffness.
- Before starting ropinirole extended-release tablets, you should talk to your healthcare provider about what to do if you miss a dose. If you have missed the previous dose and it is time for your next dose, do not double the dose
- Your healthcare provider will start you on a low dose of ropinirole extended-release tablets. Your healthcare provider will change the dose until you are taking the right amount of medicine to control your symptoms. It may take several weeks before you reach a dose that controls your symptoms.
If you are taking ropinirole extended-release tablets:
- Take ropinirole extended-release tablets 1 time each day for Parkinson’s disease, preferably at or around the same time of day
- Swallow ropinirole extended-release tablets whole. Do not chew, crush, or split ropinirole extended-release tablets.
- Contact your healthcare provider if you stop taking ropinirole extended-release tablets for any reason. Do not restart without talking with your healthcare provider.
- Your healthcare provider may prescribe ropinirole extended-release tablets alone, or add ropinirole extended-release tablets to medicine that you are already taking for Parkinson's disease.
- You should not substitute for ropinirole extended-release tablets without talking with your healthcare provider.
- You can take ropinirole extended-release tablets with or without food. If you experience nausea you may try taking ropinirole extended-release tablets with food.
What are the possible side effects of ropinirole extended-release tablets?
Serious side effects in people taking ropinirole extended-release tablets are described in the section “Ropinirole extended-release tablets can cause serious side effects including” and include:
- Falling asleep during normal activities
- Changes in blood pressure
- Fainting
- Hallucinations
- Uncontrolled sudden movements
Some patients taking ropinirole extended-release tablets get urges to behave in a way unusual for them. Examples of this are an unusual urge to gamble or increased sexual urges and behaviors. If you notice or your family notices that you are developing any unusual behaviors, talk to your healthcare provider.
You should be careful until you know if ropinirole extended-release tablets affects your ability to remain alert while doing normal daily activities, driving a car, operating machinery, or working at heights. You should also watch for the development of significant daytime sleepiness or episodes of falling asleep.
Common side effects in people taking ropinirole extended-release tablets include:
- Fainting
- Sleepiness
- Hallucinations
- Dizziness
- Nausea or vomiting
- Uncontrolled sudden movements
- Leg swelling
- Fatigue
- Headache
- Upset stomach
- Increased sweating
This is not a complete list of side effects and should not take the place of discussions with your healthcare providers. Your healthcare provider or pharmacist can give you a more complete list of possible side effects.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ropinirole extended-release tablets?
- Store ropinirole extended-release tablets at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
- Store ropinirole extended-release tablets at room temperature out of direct sunlight.
- Keep ropinirole extended-release tablets in a tightly closed container.
- Keep ropinirole extended-release tablets out of the reach of children.
Other Information about ropinirole extended-release tablets:
- Do not share ropinirole extended-release tablets with other people, even if they have the same symptoms you have.
- Studies of people with Parkinson’s disease show that they may be at an increased risk of developing melanoma, a form of skin cancer, when compared to people without Parkinson’s disease. It is not known if this problem is associated with Parkinson’s disease or the medicines used to treat Parkinson’s disease. Ropinirole extended-release tablets are used to treat Parkinson’s disease, therefore, patients being treated with ropinirole extended-release tablets should have periodic skin examinations.
This patient information leaflet summarizes the most important information about ropinirole extended-release tablets for Parkinson’s disease. Medicines are sometimes prescribed for purposes other than those listed in this leaflet. Do not take ropinirole extended-release tablets for a condition for which they were not prescribed. For more information, talk with your healthcare provider or pharmacist. They can give you information about ropinirole extended-release tablets that is written for healthcare professionals. For more information call 1-800-272-5525 (toll-free) or visit www.watson.com.
What are the ingredients in ropinirole extended-release tablets?
The following ingredients are in ropinirole extended-release tablets:
Active ingredient: ropinirole (as ropinirole hydrochloride)
Inactive ingredients: hypromellose, mannitol, glyceryl behenate, lactose monohydrate, hydrogenated castor oil, povidone, polyvinyl acetate dispersion 30% (stabilized with povidone and sodium lauryl sulfate), talc, magnesium stearate, colloidal silicon dioxide, triethyl citrate, titanium dioxide, polydextrose, triacetin, polyethylene glycol 8000, and one or more of the following: iron oxide red (2 mg), iron oxide yellow (2 mg and 12 mg), FD&C Yellow #6/Sunset Yellow aluminum lake (4 mg and 8 mg), FD&C Blue #2/Indigo Carmine aluminum lake (4 mg, 8 mg and 12 mg), and FD&C Red #40/Allura Red aluminum lake (8 mg).
This product contains color additives including FD&C Yellow #6 in the 4 mg and 8 mg tablets.
Manufactured by:
Watson Laboratories, Inc.
Corona, CA 92880 USA
Distributed by:
Watson
Pharma
, Inc.
Parsippany, NJ 07054
Issued: February 2011
NDC 0591-3611-30
rOPINIRole
Extended-Release
Tablets
2 mg
PHARMACIST: Dispense the Patient Information Leaflet with the drug product
Watson® 30 Tablets Rx only
NDC 0591-3613-30
rOPINIRole
Extended-Release
Tablets
4 mg
PHARMACIST: Dispense the Patient Information Leaflet with the drug product
Watson® 30 Tablets Rx only
NDC 0591-3700-30
rOPINIRole
Extended-Release
Tablets
6 mg
PHARMACIST: Dispense the Patient Information Leaflet with the drug product
Watson® 30 Tablets Rx only
NDC 0591-3614-30
rOPINIRole
Extended-Release
Tablets
8 mg
PHARMACIST: Dispense the Patient Information Leaflet with the drug product
Watson® 30 Tablets Rx only
NDC 0591-3612-30
rOPINIRole
Extended-Release
Tablets
12 mg
PHARMACIST: Dispense the Patient Information Leaflet with the drug product
Watson® 30 Tablets Rx only
Ropinirole HydrochlorideRopinirole Hydrochloride TABLET, FILM COATED, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Ropinirole HydrochlorideRopinirole Hydrochloride TABLET, FILM COATED, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Ropinirole HydrochlorideRopinirole Hydrochloride TABLET, FILM COATED, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Ropinirole HydrochlorideRopinirole Hydrochloride TABLET, FILM COATED, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Ropinirole HydrochlorideRopinirole Hydrochloride TABLET, FILM COATED, EXTENDED RELEASE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||