Sentroxatine
HIGHLIGHTS OF PRESCRIBING INFORMATIONFluoxetine 10 mg These highlights do not include all the information needed to use fluoxetine capsules USP safely and effectively. See full prescribing information for fluoxetine capsules USP. Initial U.S. Approval: 1987BOXED WARNINGWARNING: SUICIDALITY AND ANTIDEPRESSANT DRUGS See full prescribing information for complete boxed warning Increased risk of suicidal thinking and behavior in children, adolescents, and young adults taking antidepressants for Major Depressive Disorder (MDD) and other psychiatric disorders (5.1).RECENT MAJOR CHANGESRECENT MAJOR CHANGES WARNINGS AND PRECAUTIONSSerotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions (5.2) 01/2009INDICATIONS AND USAGEINDICATIONS AND USAGE Fluoxetine is a selective serotonin reuptake inhibitor indicated for: - Acute and maintenance treatment of Major Depressive Disorder (MDD) in adult and pediatric patients aged 8 to 18 years (1.1) - Acute and maintenance treatment of Obsessive Compulsive Disorder (OCD) in adult and pediatric patients aged 7 to 17 years (1.2 ) - Acute and maintenance treatment of Bulimia Nervosa in adult patients (1.3) - Acute treatment of Panic Disorder, with or without agoraphobia, in adult patients (1.4) DOSAGE AND ADMINISTRATIONDOSAGE AND ADMINISTRATION Indication Adult Pediatric MDD (2.1) 20 mg/day in am (initialdose) 10 to 20 mg/day (initialdose) OCD (2.2) 20 mg/day in am (initialdose) 10 mg/day (initial dose) Bulimia Nervosa(2.3) 60 mg/day in am - Panic Disorder (2.4) 10 mg/day (initial dose) - - Consider tapering the dose of fluoxetine for pregnant women during the third trimester (2.7) - A lower or less frequent dosage should be used in patients with hepatic impairment, the elderly, and for patients with concurrent disease or on multiple concomitant medications (2.7 ) DOSAGE FORMS AND STRENGTHSDOSAGE FORMS AND STRENGTHS - Capsules: 10 mg (3) - Capsules: 20 mg (3) CONTRAINDICATIONSCONTRAINDICATIONS - Do not use with an MAOI or within 14 days of discontinuing an MAOI due to risk of drug interaction. At least 5 weeks should be allowed after stopping fluoxetine before treatment with an MAOI (4), 7.1) - Do not use with pimozide due to risk of drug interaction or QTc prolongation (4, 7.9) - Do not use with thioridazine due to QTc interval prolongation or potential for elevated thioridazine plasma levels. Do not use thioridazine within 5 weeks of discontinuing fluoxetine (4, 7.9)WARNINGS AND PRECAUTIONSWARNINGS AND PRECAUTIONS - Clinical Worsening and Suicide Risk: Monitor for clinical worsening and suicidal thinking and behavior (5.1) - Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions: Have been reported with fluoxetine. Discontinue fluoxetine and initiate supportive treatment (5.2) - Allergic Reactions and Rash: Discontinue upon appearance of rash or allergic phenomena (5.3) - Activation of Mania/Hypomania: Screen for Bipolar Disorder and monitor for mania/hypomania (5.4) - Seizures: Use cautiously in patients with a history of seizures or with conditions that potentially lower the seizure threshold (5.5) - Altered Appetite and Weight: Significant weight loss has occurred (5.6) - Abnormal Bleeding: May increase the risk of bleeding. Use with NSAIDs, aspirin, warfarin, or drugs that affect coagulation may potentiate the risk of gastrointestinal or other bleeding (5.7) - Hyponatremia: Has been reported with fluoxetine in association with syndrome of inappropriate antidiuretic hormone (SIADH) (5.8) - Anxiety and Insomnia: May occur (5.9) - Potential for Cognitive and Motor Impairment: Has potential to impair judgment, thinking, and motor skills. Use caution when operating machinery (5.11) - Long Half-Life: Changes in dose will not be fully reflected in plasma for several weeks (5.12)Side EffectsADVERSE REACTIONS Most common adverse reactions (≥ 5% and at least twice that for placebo) associated with: Major Depressive Disorder, Obsessive Compulsive Disorder, Bulimia, and Panic Disorder: abnormal dreams, abnormal ejaculation, anorexia, anxiety, asthenia, diarrhea, dry mouth, dyspepsia, flu syndrome, impotence, insomnia, libido decreased, nausea, nervousness, pharyngitis, rash, sinusitis, somnolence, sweating, tremor, vasodilatation, and yawn (6.1) To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-888-838-2872, x6351 or drug.safety@tevausa.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONSDRUG INTERACTIONS - Monoamine Oxidase Inhibitors (MAOI): Fluoxetine is contraindicated for use with MAOI’s, or within 14 days of discontinuing an MAOI due to risk of drug interaction. At least 5 weeks should be allowed after stopping fluoxetine before starting treatment with an MAOI (4, 7.1) - Pimozide: Fluoxetine is contraindicated for use with pimozide due to risk of drug interaction or QTc prolongation (4, 7.9) - Thioridazine: Fluoxetine is contraindicated for use with thioridazine due to QTc interval prolongation or potential for elevated thioridazine plasma levels. Do not use thioridazine within 5 weeks of discontinuing fluoxetine (4, 7.9) - Drugs Metabolized by CYP2D6: Fluoxetine is a potent inhibitor of CYP2D6 enzyme pathway (7.9) - Tricyclic Antidepressants (TCAs): Monitor TCA levels during coadministration with fluoxetine or when fluoxetine has been recently discontinued (7.9) - CNS Acting Drugs: Caution should be used when taken in combination with other centrally acting drugs (7.2) - Benzodiazepines: Diazepam – increased t1/2, alprazolam - further psychomotor performance decrement due to increased levels (7.9) - Antipsychotics: Potential for elevation of haloperidol and clozapine levels (7.9) - Anticonvulsants: Potential for elevated phenytoin and carbamazepine levels and clinical anticonvulsant toxicity (7.9) - Serotonergic Drugs: Potential for Serotonin Syndrome (5.2, 7.3) - Triptans: There have been rare postmarketing reports of Serotonin Syndrome with use of an SSRI and a triptan (5.2, 7.4) - Tryptophan: Concomitant use with tryptophan is not recommended (5.2, 7.5) - Drugs that Interfere with Hemostasis (e.g., NSAIDs, Aspirin, Warfarin): May potentiate the risk of bleeding (7.6) - Drugs Tightly Bound to Plasma Proteins: May cause a shift in plasma concentrations (7.8, 7.9)USE IN SPECIFIC POPULATIONSUSE IN SPECIFIC POPULATIONS - Pregnancy: Fluoxetine should be used during pregnancy only if the potential benefit justifies the potential risks to the fetus ( 8.1) - Nursing Mothers: Breast feeding is not recommended ( 8.3) - Hepatic Impairment: Lower or less frequent dosing may be appropriate in patients with cirrhosis ( 8.6) See 17 for PATIENT COUNSELING INFORMATION and the FDA-approved Medication GuideRevised: 12/2009
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1.1 Major Depressive Disorder 1.2 Obsessive Compulsive Disorder 1.3 Bulimia Nervosa 1.4 Panic Disorder
- 2.1 Major Depressive Disorder 2.2 Obsessive-Compulsive Disorder 2.3 Bulimia Nervosa 2.4 Panic Disorder 2.7 Dosing in Specific Populations 2.8 Discontinuation of Treatment
- 3 DOSAGE FORMS AND STRENGTHS
- 4 SENTROXATINE CONTRAINDICATIONS
- 5.1 Clinical Worsening and Suicide Risk 5.2 Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions 5.3 Allergic Reactions and Rash 5.4 Screening Patients for Bipolar Disorder and Monitoring for Mania/Hypomania 5.5 Seizures 5.6 Altered A
- * † ‡ Table 5 6.1 Clinical Trials Experience 6.2 Other Reactions 6.3 Postmarketing Experience
- 7.1 Monoamine Oxidase Inhibitors (MAOI) 7.2 CNS Acting Drugs 7.3 Serotonergic Drugs 7.4 Triptans 7.5 Tryptophan 7.6 Drugs That Interfere With Hemostasis (e.g., NSAIDS, Aspirin, Warfarin) 7.7 Electroconvulsive Therapy (ECT) 7.8 Potential for Other Drugs to
- 8.1 Pregnancy
- 8.2 Labor and Delivery
- 8.3 Nursing Mothers
- 8.4 Pediatric Use
- 8.5 Geriatric Use 8.6 Hepatic Impairment
- 9.3 Dependence
- 10.1 Human Experience 10.2 Animal Experience 10.3 Management of Overdose
- 12.1 Mechanism of Action
- 12.2 Pharmacodynamics
- 12.3 Pharmacokinetics 12.4 Specific Populations
- 14.1 Major Depressive Disorder 14.2 Obsessive Compulsive Disorder 14.3 Bulimia Nervosa 14.4 Panic Disorder
- 17.1 General Information 17.2 Clinical Worsening and Suicide Risk 17.3 Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions 17.4 Allergic Reactions and Rash 17.5 Abnormal Bleeding 17.6 Hyponatremia 17.7 Potential for Cognitive and Mot
FULL PRESCRIBING INFORMATION
Enter section text here
Enter section text here
Uses
Enter section text here
Enter section text here
Enter section text here
Enter section text here
Enter section text here
Enter section text here
Enter section text here
Enter section text here
EWARNING: SUICIDALITY AND ANTIDEPRESSANT DRUGS
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of Major Depressive Disorder (MDD) and other psychiatric disorders. Anyone considering the use of fluoxetine capsulesor any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Fluoxetineis approved for use in pediatric patients with MDD and Obsessive Compulsive Disorder (OCD) [see Warnings and Precautions (5.1) and Use in Specific Populations (8.4)].
1.1 Major Depressive Disorder 1.2 Obsessive Compulsive Disorder 1.3 Bulimia Nervosa 1.4 Panic Disorder
1 INDICATIONS AND USAGE
1.1 Major Depressive Disorder
Fluoxetine is indicated for the acute and maintenance treatment of Major Depressive Disorder in adult patients and in pediatric patients aged 8 to18 years [see Clinical Studies (14.1)].
The usefulness of the drug in adult and pediatric patients receiving fluoxetine for extended periods, should periodically be re-evaluated [see Dosage and Administration (2.1)].
1.2 Obsessive Compulsive Disorder
Fluoxetine is indicated for the acute and maintenance treatment of obsessions and compulsions in adult patients and in pediatric patients aged 7 to 17 years with Obsessive Compulsive Disorder (OCD) [see Clinical Studies (14.2)].
The effectiveness of fluoxetine in long-term use, i.e., for more than 13 weeks, has not been systematically evaluated in placebo-controlled trials. Therefore, the physician who elects to use fluoxetine for extended periods, should periodically re-evaluate the long-term usefulness of the drug for the individual patient [see Dosage and Administration (2.2)].
1.3 Bulimia Nervosa
Fluoxetine is indicated for the acute and maintenance treatment of binge-eating and vomiting behaviors in adult patients with moderate to severe Bulimia Nervosa [see Clinical Studies (14.3)].
The physician who elects to use fluoxetine for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient [see Dosage and Administration (2.3)].
1.4 Panic Disorder
Fluoxetine is indicated for the acute treatment of Panic Disorder, with or without agoraphobia, in adult patients [see Clinical Studies (14.4)].
The effectiveness of fluoxetine in long-term use, i.e., for more than 12 weeks, has not been established in placebo-controlled trials. Therefore, the physician who elects to use fluoxetine for extended periods, should periodically re-evaluate the long-term usefulness of the drug for the individual patient [see Dosage and Administration (2.4) ].
2.1 Major Depressive Disorder 2.2 Obsessive-Compulsive Disorder 2.3 Bulimia Nervosa 2.4 Panic Disorder 2.7 Dosing in Specific Populations 2.8 Discontinuation of Treatment
2 DOSAGE AND ADMINISTRATION
2.1 Major Depressive Disorder
Initial Treatment
Adult — In controlled trials used to support the efficacy of fluoxetine, patients were administered morning doses ranging from 20 to 80 mg/day. Studies comparing fluoxetine 20, 40, and 60 mg/day to placebo indicate that 20 mg/day is sufficient to obtain a satisfactory response in Major Depressive Disorder in most cases. Consequently, a dose of 20 mg/day, administered in the morning, is recommended as the initial dose.
A dose increase may be considered after several weeks if insufficient clinical improvement is observed. Doses above 20 mg/day may be administered on a once-a-day (morning) or BID schedule (i.e., morning and noon) and should not exceed a maximum dose of 80 mg/day.
Pediatric (children and adolescents) — In the short-term (8 to 9 week) controlled clinical trials of fluoxetine supporting its effectiveness in the treatment of Major Depressive Disorder, patients were administered fluoxetine doses of 10 to 20 mg/day [see Clinical Studies (14.1)]. Treatment should be initiated with a dose of 10 or 20 mg/day. After 1 week at 10 mg/day, the dose should be increased to 20 mg/day.
However, due to higher plasma levels in lower weight children, the starting and target dose in this group may be 10 mg/day. A dose increase to 20 mg/day may be considered after several weeks if insufficient clinical improvement is observed.
All patients — As with other drugs effective in the treatment of Major Depressive Disorder, the full effect may be delayed until 4 weeks of treatment or longer.
Maintenance/Continuation/Extended Treatment — It is generally agreed that acute episodes of Major Depressive Disorder require several months or longer of sustained pharmacologic therapy. Whether the dose needed to induce remission is identical to the dose needed to maintain and/or sustain euthymia is unknown.
Daily Dosing — Systematic evaluation of fluoxetine in adult patients has shown that its efficacy in Major Depressive Disorder is maintained for periods of up to 38 weeks following 12 weeks of open-label acute treatment (50 weeks total) at a dose of 20 mg/day [see Clinical Studies (14.1)].
Switching Patients to a Tricyclic Antidepressant (TCA) — Dosage of a TCA may need to be reduced, and plasma TCA concentrations may need to be monitored temporarily when fluoxetine is coadministered or has been recently discontinued [see Drug Interactions (7.9)].
Switching Patients to or From a Monoamine Oxidase Inhibitor (MAOI) — At least 14 days should elapse between discontinuation of an MAOI and initiation of therapy with fluoxetine. In addition, at least 5 weeks, perhaps longer, should be allowed after stopping fluoxetine before starting an MAOI [see Contraindications (4) and Drug Interactions (7.1)].
2.2 Obsessive-Compulsive Disorder
Initial Treatment
Adult — In the controlled clinical trials of fluoxetine supporting its effectiveness in the treatment of OCD, patients were administered fixed daily doses of 20, 40, or 60 mg of fluoxetine or placebo [see Clinical Studies (14.2)]. In one of these studies, no dose-response relationship for effectiveness was demonstrated. Consequently, a dose of 20 mg/day, administered in the morning, is recommended as the initial dose. Since there was a suggestion of a possible dose-response relationship for effectiveness in the second study, a dose increase may be considered after several weeks if insufficient clinical improvement is observed. The full therapeutic effect may be delayed until 5 weeks of treatment or longer.
Doses above 20 mg/day may be administered on a once daily (i.e., morning) or BID schedule (i.e., morning and noon). A dose range of 20 to 60 mg/day is recommended; however, doses of up to 80 mg/day have been well tolerated in open studies of OCD. The maximum fluoxetine dose should not exceed 80 mg/day.
Pediatric (children and adolescents) — In the controlled clinical trial of fluoxetine supporting its effectiveness in the treatment of OCD, patients were administered fluoxetine doses in the range of 10 to 60 mg/day [see Clinical Studies (14.2)].
In adolescents and higher weight children, treatment should be initiated with a dose of 10 mg/day. After 2 weeks, the dose should be increased to 20 mg/day. Additional dose increases may be considered after several more weeks if insufficient clinical improvement is observed. A dose range of 20 to 60 mg/day is recommended.
In lower weight children, treatment should be initiated with a dose of 10 mg/day. Additional dose increases may be considered after several more weeks if insufficient clinical improvement is observed. A dose range of 20 to 30 mg/day is recommended. Experience with daily doses greater than 20 mg is very minimal, and there is no experience with doses greater than 60 mg.
Maintenance/Continuation Treatment — While there are no systematic studies that answer the question of how long to continue fluoxetine, OCD is a chronic condition and it is reasonable to consider continuation for a responding patient. Although the efficacy of fluoxetine after 13 weeks has not been documented in controlled trials, adult patients have been continued in therapy under double-blind conditions for up to an additional 6 months without loss of benefit. However, dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for treatment.
2.3 Bulimia Nervosa
Initial Treatment — In the controlled clinical trials of fluoxetine supporting its effectiveness in the treatment of Bulimia Nervosa, patients were administered fixed daily fluoxetine doses of 20 or 60 mg, or placebo [see Clinical Studies (14.3)]. Only the 60 mg dose was statistically significantly superior to placebo in reducing the frequency of binge-eating and vomiting. Consequently, the recommended dose is 60 mg/day, administered in the morning. For some patients it may be advisable to titrate up to this target dose over several days. Fluoxetine doses above 60 mg/day have not been systematically studied in patients with bulimia.
Maintenance/Continuation Treatment — Systematic evaluation of continuing fluoxetine 60 mg/day for periods of up to 52 weeks in patients with bulimia who have responded while taking fluoxetine 60 mg/day during an 8 week acute treatment phase has demonstrated a benefit of such maintenance treatment [see Clinical Studies (14.3)]. Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
2.4 Panic Disorder
Initial Treatment — In the controlled clinical trials of fluoxetine supporting its effectiveness in the treatment of Panic Disorder, patients were administered fluoxetine doses in the range of 10 to 60 mg/day [see Clinical Studies (14.4)]. Treatment should be initiated with a dose of 10 mg/day. After one week, the dose should be increased to 20 mg/day. The most frequently administered dose in the 2 flexible-dose clinical trials was 20 mg/day.
A dose increase may be considered after several weeks if no clinical improvement is observed. Fluoxetine doses above 60 mg/day have not been systematically evaluated in patients with Panic Disorder.
Maintenance/Continuation Treatment — While there are no systematic studies that answer the question of how long to continue fluoxetine, panic disorder is a chronic condition and it is reasonable to consider continuation for a responding patient. Nevertheless, patients should be periodically reassessed to determine the need for continued treatment.
2.7 Dosing in Specific Populations
Treatment of pregnant Women During the Third Trimester — When treating pregnant women with fluoxetine during the third trimester, the physician should carefully consider the potential risks and potential benefits of treatment. Neonates exposed to SNRIs or SSRIs late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. The physician may consider tapering fluoxetine in the third trimester [see Use in Specific Populations (8.1)].
Geriatrics — A lower or less frequent dosage should be considered for the elderly [see Use in Specific Populations (8.5)]
Hepatic Impairment — As with many other medications, a lower or less frequent dosage should be used in patients with hepatic impairment [see Clinical Pharmacology (12.4) and Use in Specific Populations ( 8.6)].
Concomitant Illness — Patients with concurrent disease or on multiple concomitant medications may require dosage adjustments [see Clinical Pharmacology (12.4) and Warnings and Precautions (5.10)].
2.8 Discontinuation of Treatment
Symptoms associated with discontinuation of fluoxetine, SNRIs, and SSRIs, have been reported [see Warnings and Precautions (5.13)].
3 DOSAGE FORMS AND STRENGTHS
3 DOSAGE FORMS AND STRENGTHS
Fluoxetine Capsules USP, 10 mg contain fluoxetine hydrochloride, equivalent to 10 mg fluoxetine, and are available as white, opaque capsules printed with PLIVA 647 in green band on cap and body.
Fluoxetine Capsules USP, 20 mg contain fluoxetine hydrochloride, equivalent to 20 mg fluoxetine, and are available as white, opaque capsules printed with PLIVA 648 in green band on cap only.
4 CONTRAINDICATIONS
4 CONTRAINDICATIONS
The use of fluoxetine is contraindicated with the following:
- Monoamine Oxidase Inhibitors [see Drug Interactions (7.1)]
- Pimozide [see Drug Interactions (7.9)]
- Thioridazine [see Drug Interactions (7.9)]
5.1 Clinical Worsening and Suicide Risk 5.2 Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions 5.3 Allergic Reactions and Rash 5.4 Screening Patients for Bipolar Disorder and Monitoring for Mania/Hypomania 5.5 Seizures 5.6 Altered A
5 WARNINGS AND PRECAUTIONS
5.1 Clinical Worsening and Suicide Risk
Patients with Major Depressive Disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with Major Depressive Disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older. The pooled analyses of placebo-controlled trials in children and adolescents with MDD, Obsessive Compulsive Disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients.
The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug versus placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 2.
| Age Range |
Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
|
|
Increases Compared to Placebo |
| less than 18 |
14 additional cases |
| 18 to 24 |
5 additional cases |
|
|
Decreases Compared to Placebo |
| 25 to 64 |
1 fewer case |
| greater than or equal to 65 |
6 fewer cases |
5.13
4 7.1
7.4
7.3
8.4
8.4
8.4
8.4
7.6
8.5
see Table 5:
12.3
* † ‡ Table 5 6.1 Clinical Trials Experience 6.2 Other Reactions 6.3 Postmarketing Experience
Table 3: Most Common Treatment-Emergent Adverse Reactions: Incidence in Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Placebo-Controlled Clinical Trials * †
|
|
|
|
Percentage of Patients Reporting Event |
|
|
|
|
|
|
|
Major Depressive Disorder |
|
OCD |
|
Bulimia |
|
Panic Disorder |
|
| Body System/Adverse Reaction |
Flouxetine (N=1728) |
Placebo (N=975) |
Flouxetine (N=266) | Placebo (N=89) | Flouxetine (N=450) | Placebo (N=267) | Flouxetine (N=425) | Placebo (N=342) |
| Body as a Whole |
|
|
|
|
|
|
|
|
| Asthenia |
9 |
5 |
15 |
11 |
21 |
9 |
7 |
7 |
| Flu Syndrome |
3 |
4 |
10 |
7 |
8 |
3 |
5 |
5 |
| Cardiovascular System |
|
|
|
|
|
|
|
|
| Vasodilation |
3 |
2 |
5 |
- |
2 |
1 |
1 |
- |
| Digestive System |
|
|
|
|
|
|
|
|
| Nausea |
21 |
9 |
26 |
13 |
29 |
11 |
12 |
7 |
| Diarrhea |
12 |
8 |
18 |
13 |
8 |
6 |
9 |
4 |
| Anorexia |
11 |
2 |
17 |
10 |
8 |
4 |
4 |
1 |
| Dry mouth |
10 |
7 |
12 |
3 |
9 |
6 |
4 |
4 |
| Dyspesia |
7 |
5 |
10 |
4 |
10 |
6 |
6 |
2 |
| Nervous System |
|
|
|
|
|
|
|
|
| Insomnia |
16 |
9 |
28 |
22 |
33 |
13 |
10 |
7 |
| Anxiety |
12 |
7 |
14 |
7 |
15 |
9 |
6 |
2 |
| Nervousness |
14 |
9 |
14 |
15 |
11 |
5 |
8 |
6 |
| Somnolence |
13 |
6 |
17 |
7 |
13 |
5 |
5 |
2 |
| Tremor |
10 |
3 |
9 |
1 |
13 |
1 |
3 |
1 |
| Libido decreased |
3 |
- |
11 |
2 |
5 |
1 |
1 |
2 |
| Abnormal dreams |
1 |
1 |
5 |
2 |
5 |
3 |
1 |
1 |
| Respiratory System |
|
|
|
|
|
|
|
|
| Pharyngitis |
3 |
3 |
22 |
9 |
10 |
5 |
3 |
3 |
| Sinusitis |
1 |
4 |
5 |
2 |
6 |
4 |
2 |
3 |
| Yawn |
- |
- |
7 |
- |
11 |
- |
1 |
- |
| Skin and Appendages |
|
|
|
|
|
|
|
|
| Sweating |
8 |
3 |
7 |
- |
8 |
3 |
2 |
2 |
| Rash |
4 |
3 |
6 |
3 |
4 |
4 |
2 |
2 |
| Urogenital System |
|
|
|
|
|
|
|
|
| Impotence |
2 |
- |
- |
- |
7 |
- |
1 |
- |
| Abnormal ejaculation |
- |
- |
7 |
- |
7 |
- |
2 |
1 |
|
* Incidence less than 1 % † Includes U.S. data for Major Depressive Disorder, OCD, Bulimia, and Panic Disorder clinical trials, plus non-U.S. data for Panic Disorder clinical trials. ‡ Denominator used was for males only (N = 690 fluoxetine Major Depressive Disorder; N = 410 placebo Major Depressive Disorder; N = 116 fluoxetine OCD; N = 43 placebo OCD; N = 14 fluoxetine bulimia; N = 1 placebo bulimia; N = 162 fluoxetine panic; N = 121 placebo panic). |
|
|
|
|
|
|
|
|
Table 4: Treatment-Emergent Adverse Reactions: Incidence in Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Placebo-Controlled Clinical Trials * †
|
|
Percentage of Patients Reporting Event |
|
|
|
Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Combined |
|
| Body System/Adverse Reaction |
Fluoxetine (N = 2869) |
Placebo (N = 1673) |
| Body as a Whole |
|
|
| Headache |
21 |
19 |
| Asthenia |
11 |
6 |
| Flu syndrome |
5 |
4 |
| Fever |
2 |
1 |
| Cardiovascular System |
|
|
| Vasodilatation |
2 |
1 |
| Digestive System |
|
|
| Nausea |
22 |
9 |
| Diarrhea |
11 |
7 |
| Anorexia |
10 |
3 |
| Dry mouth |
9 |
6 |
| Dyspepsia |
8 |
4 |
| Constipation |
5 |
4 |
| Flatulence |
3 |
2 |
| Vomiting |
3 |
2 |
| Metabolic and Nutritional Disorders |
|
|
| Weight loss |
2 |
1 |
| Nervous System |
|
|
| Insomnia |
19 |
10 |
| Nervousness |
13 |
8 |
| Anxiety |
12 |
6 |
| Somnolence |
12 |
5 |
| Dizziness |
9 |
6 |
| Tremor |
9 |
2 |
| Libido decreased |
4 |
1 |
| Thinking abnormal |
2 |
1 |
| Respiratory System |
|
|
| Yawn |
3 |
- - |
| Skin and Appendages |
|
|
| Sweating |
7 |
3 |
| Rash |
4 |
3 |
| Pruritus |
3 |
2 |
| Special Senses |
|
|
| Abnormal vision |
2 |
1 |
|
* Incidence less than 1%. † Includes U.S. data for Major Depressive Disorder, OCD, bulimia, and Panic Disorder clinical trials, plus non-U.S. data for Panic Disorder clinical trials. |
|
|
Table 5: Most Common Adverse Reactions Associated With Discontinuation in Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Placebo-Controlled Clinical Trials *
| Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Combined (N = 1533) |
Major Depressive Disorder (N = 392) |
OCD (N = 266) |
Bulimia (N = 450) |
Panic Disorder (N = 425 |
| Anxiety (1%) |
- - |
Anxiety (1%) |
- - |
Anxiety (2%) |
| - - |
- - |
- - |
Insomnia (2%) |
- - |
| - - |
Nervousness (1%) |
- - |
- - |
Nervousness (1%) |
| - - |
- - |
Rash (1%) |
- - |
- - |
|
* Includes U.S. data for Major Depressive Disorder, OCD, bulimia, and Panic Disorder clinical trials, plus non-U.S. Panic Disorder clinical trials. |
|
|
|
|
7.1 Monoamine Oxidase Inhibitors (MAOI) 7.2 CNS Acting Drugs 7.3 Serotonergic Drugs 7.4 Triptans 7.5 Tryptophan 7.6 Drugs That Interfere With Hemostasis (e.g., NSAIDS, Aspirin, Warfarin) 7.7 Electroconvulsive Therapy (ECT) 7.8 Potential for Other Drugs to
7 DRUG INTERACTIONS
As with all drugs, the potential for interaction by a variety of mechanisms (e.g., pharmacodynamic, pharmacokinetic drug inhibition or enhancement, etc.) is a possibility.
7.1 Monoamine Oxidase Inhibitors (MAOI)
There have been reports of serious, sometimes fatal, reactions (including hyperthermia, rigidity, myoclonus, autonomic instability with possible rapid fluctuations of vital signs, and mental status changes that include extreme agitation progressing to delirium and coma) in patients receiving fluoxetine in combination with a monoamine oxidase inhibitor (MAOI), and in patients who have recently discontinued fluoxetine and are then started on an MAOI. Some cases presented with features resembling neuroleptic malignant syndrome. Therefore, fluoxetine should not be used in combination with an MAOI, or within a minimum of 14 days of discontinuing therapy with an MAOI [see Contraindications (4)]. Since fluoxetine and its major metabolite have very long elimination half-lives, at least 5 weeks perhaps longer, especially if fluoxetine has been prescribed chronically and/or at higher doses should be allowed after stopping fluoxetine before starting an MAOI [see Clinical Pharmacology (12.3)].
7.2 CNS Acting Drugs
Caution is advised if the concomitant administration of fluoxetine and such drugs is required. In evaluating individual cases, consideration should be given to using lower initial doses of the concomitantly administered drugs, using conservative titration schedules, and monitoring of clinical status [see Clinical Pharmacology (12.3)].
7.3 Serotonergic Drugs
Based on the mechanism of action of SNRIs and SSRIs, including fluoxetine, and the potential for serotonin syndrome, caution is advised when fluoxetine is coadministered with other drugs that may affect the serotonergic neurotransmitter systems, such as triptans, linezolid (an antibiotic which is a reversible non-selective MAOI), lithium, tramadol, or St. John’s Wort [see Warnings and Precautions (5.2)]. The concomitant use of fluoxetine with SNRIs, SSRIs, or tryptophan is not recommended [see Drug Interactions (7.4), (7.5)].
7.4 Triptans
There have been rare postmarketing reports of serotonin syndrome with use of an SSRI and a triptan. If concomitant treatment of fluoxetine with a triptan is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases [see Warnings and Precautions (5.2) and Drug Interactions (7.3)].
7.5 Tryptophan
Five patients receiving fluoxetine in combination with tryptophan experienced adverse reactions, including agitation, restlessness, and gastrointestinal distress. The concomitant use with tryptophan is not recommended [see Warnings and Precautions (5.2) and Drug Interactions (7.3)].
7.6 Drugs That Interfere With Hemostasis (e.g., NSAIDS, Aspirin, Warfarin)
Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies of the case-control and cohort design that have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding have also shown that concurrent use of an NSAID or aspirin may potentiate this risk of bleeding. Altered anticoagulant effects, including increased bleeding, have been reported when SNRIs or SSRIs are coadministered with warfarin. Patients receiving warfarin therapy should be carefully monitored when fluoxetine is initiated or discontinued [see Warnings and Precautions (5.7)].
7.7 Electroconvulsive Therapy (ECT)
There are no clinical studies establishing the benefit of the combined use of ECT and fluoxetine. There have been rare reports of prolonged seizures in patients on fluoxetine receiving ECT treatment.
7.8 Potential for Other Drugs to Affect Fluoxetine
Drugs Tightly Bound to Plasma Proteins – Because fluoxetine is tightly bound to plasma protein, adverse effects may result from displacement of protein-bound fluoxetine by other tightly-bound drugs [see Clinical Pharmacology (12.3)].
7.9 Potential for Fluoxetine to Affect Other Drugs
Pimozide – Concomitant use in patients taking pimozide is contraindicated. Clinical studies of pimozide with other antidepressants demonstrate an increase in drug interaction or QTc prolongation. While a specific study with pimozide and fluoxetine has not been conducted, the potential for drug interactions or QTc prolongation warrants restricting the concurrent use of pimozide and fluoxetine [see Contraindications (4)].
Thioridazine – Thioridazine should not be administered with fluoxetine or within a minimum of 5 weeks after fluoxetine has been discontinued [see Contraindications (4)].
In a study of 19 healthy male subjects, which included 6 slow and 13 rapid hydroxylators of debrisoquin, a single 25 mg oral dose of thioridazine produced a 2.4 fold higher Cmax and a 4.5 fold higher AUC for thioridazine in the slow hydroxylators compared with the rapid hydroxylators. The rate of debrisoquin hydroxylation is felt to depend on the level of CYP2D6 isozyme activity. Thus, this study suggests that drugs which inhibit CYP2D6, such as certain SSRIs, including fluoxetine, will produce elevated plasma levels of thioridazine.
Thioridazine administration produces a dose-related prolongation of the QTc interval, which is associated with serious ventricular arrhythmias, such as torsade de pointes-type arrhythmias, and sudden death. This risk is expected to increase with fluoxetine-induced inhibition of thioridazine metabolism.
Drugs Metabolized by CYP2D6 – Fluoxetine inhibits the activity of CYP2D6, and may make individuals with normal CYP2D6 metabolic activity resemble a poor metabolizer. Coadministration of fluoxetine with other drugs that are metabolized by CYP2D6, including certain antidepressants (e.g., TCAs), antipsychotics (e.g., phenothiazines and most atypicals), and antiarrhythmics (e.g., propafenone, flecainide, and others) should be approached with caution. Therapy with medications that are predominantly metabolized by the CYP2D6 system and that have a relatively narrow therapeutic index (see list below) should be initiated at the low end of the dose range if a patient is receiving fluoxetine concurrently or has taken it in the previous 5 weeks. Thus, his/her dosing requirements resemble those of poor metabolizers. If fluoxetine is added to the treatment regimen of a patient already receiving a drug metabolized by CYP2D6, the need for decreased dose of the original medication should be considered. Drugs with a narrow therapeutic index represent the greatest concern (e.g., flecainide, propafenone, vinblastine, and TCAs). Due to the risk of serious ventricular arrhythmias and sudden death potentially associated with elevated plasma levels of thioridazine, thioridazine should not be administered with fluoxetine or within a minimum of 5 weeks after fluoxetine has been discontinued [see Contraindications (4)].
Tricyclic Antidepressants (TCAs) — In 2 studies, previously stable plasma levels of imipramine and desipramine have increased greater than 2 to 10 fold when fluoxetine has been administered in combination. This influence may persist for 3 weeks or longer after fluoxetine is discontinued. Thus, the dose of TCAs may need to be reduced and plasma TCA concentrations may need to be monitored temporarily when fluoxetine is coadministered or has been recently discontinued [see Clinical Pharmacology (12.3)].
Benzodiazapines — The half-life of concurrently administered diazepam may be prolonged in some patients [see Clinical Pharmacology (12.2)]. Coadministration of alprazolam and fluoxetine has resulted in increased alprazolam plasma concentrations and in further psychomotor performance decrement due to increased alprazolam levels.
Antipsychotics — Some clinical data suggests a possible pharmacodynamic and/or pharmacokinetic interaction between SSRIs and antipsychotics. Elevation of blood levels of haloperidol and clozapine has been observed in patients receiving concomitant fluoxetine [see Contraindications (4)].
Anticonvulsants — Patients on stable doses of phenytoin and carbamazepine have developed elevated plasma anticonvulsant concentrations and clinical anticonvulsant toxicity following initiation of concomitant fluoxetine treatment.
Lithium — There have been reports of both increased and decreased lithium levels when lithium was used concomitantly with fluoxetine. Cases of lithium toxicity and increased serotonergic effects have been reported. Lithium levels should be monitored when these drugs are administered concomitantly.
Drugs Tightly Bound to Plasma Proteins — Because fluoxetine is tightly bound to plasma protein, the administration of fluoxetine to a patient taking another drug that is tightly bound to protein (e.g., Coumadin, digitoxin) may cause a shift in plasma concentrations potentially resulting in an adverse effect [see Clinical Pharmacology (12.3)].
Drugs Metabolized by CYP3A4 — In an in vivo interaction study involving coadministration of fluoxetine with single doses of terfenadine (a CYP3A4 substrate), no increase in plasma terfenadine concentrations occurred with concomitant fluoxetine.
Additionally, in vitro studies have shown ketoconazole, a potent inhibitor of CYP3A4 activity, to be at least 100 times more potent than fluoxetine or norfluoxetine as an inhibitor of the metabolism of several substrates for this enzyme, including astemizole, cisapride, and midazolam. These data indicate that fluoxetine’s extent of inhibition of CYP3A4 activity is not likely to be of clinical significance.
Olanzapine — Fluoxetine (60 mg single dose or 60 mg daily dose for 8 days) causes a small (mean 16%) increase in the maximum concentration of olanzapine and a small (mean 16%) decrease in olanzapine clearance. The magnitude of the impact of this factor is small in comparison to the overall variability between individuals, and therefore dose modification is not routinely recommended.
8.1 Pregnancy
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C — In embryo-fetal development studies in rats and rabbits, there was no evidence of teratogenicity following administration of up to 12.5 and 15 mg/kg/day, respectively (1.5 and 3.6 times, respectively, the MRHD of 80 mg on a mg/m2 basis) throughout organogenesis. However, in rat reproduction studies, an increase in stillborn pups, a decrease in pup weight, and an increase in pup deaths during the first 7 days postpartum occurred following maternal exposure to 12 mg/kg/day (1.5 times the maximum recommended human dose (MRHD) on a mg/m2 basis) during gestation or 7.5 mg/kg/day (0.9 times the MRHD on a mg/m2 basis) during gestation and lactation. There was no evidence of developmental neurotoxicity in the surviving offspring of rats treated with 12 mg/kg/day during gestation. The no-effect dose for rat pup mortality was 5 mg/kg/day (0.6 times the MRHD on a mg/m2 basis). Fluoxetine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Treatment of Pregnant Women During the Third Trimester — Neonates exposed to fluoxetine, SNRIs, or SSRIs, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SNRIs and SSRIs or, possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome.
Infants exposed to SSRIs in late pregnancy may have an increased risk for persistent pulmonary hypertension of the newborn (PPHN). PPHN occurs in 1 to 2 per 1000 live births in the general population and is associated with substantial neonatal morbidity and mortality. In a retrospective case-control study of 377 women whose infants were born with PPHN and 836 women whose infants were born healthy, the risk for developing PPHN was approximately six-fold higher for infants exposed to SSRIs after the 20th week of gestation compared to infants who had not been exposed to antidepressants during pregnancy. There is currently no corroborative evidence regarding the risk for PPHN following exposure to SSRIs in pregnancy; this is the first study that has investigated the potential risk. The study did not include enough cases with exposure to individual SSRIs to determine if all SSRIs posed similar levels of PPHN risk.
When treating pregnant women with fluoxetine during the third trimester, the physician should carefully consider both the potential risks and potential benefits of treatment. Physicians should note that in a prospective longitudinal study of 201 women with a history of major depression who were euthymic at the beginning of pregnancy, women who discontinued antidepressant medication during pregnancy were more likely to experience a relapse of major depression than women who continued antidepressant medication.
The physician may consider tapering fluoxetine in the third trimester.
8.2 Labor and Delivery
8.2 Labor and Delivery
The effect of fluoxetine on labor and delivery in humans is unknown. However, because fluoxetine crosses the placenta and because of the possibility that fluoxetine may have adverse effects on the newborn, fluoxetine should be used during labor and delivery only if the potential benefit justifies the potential risk to the fetus.
8.3 Nursing Mothers
8.3 Nursing Mothers
Because fluoxetine is excreted in human milk, nursing while on fluoxetine is not recommended. In one breast-milk sample, the concentration of fluoxetine plus norfluoxetine was 70.4 ng/mL. The concentration in the mother’s plasma was 295.0 ng/mL. No adverse effects on the infant were reported. In another case, an infant nursed by a mother on fluoxetine developed crying, sleep disturbance, vomiting, and watery stools. The infant’s plasma drug levels were 340 ng/mL of fluoxetine and 208 ng/mL of norfluoxetine on the second day of feeding.
8.4 Pediatric Use
8.4 Pediatric Use
The efficacy of fluoxetine for the treatment of Major Depressive Disorder was demonstrated in two 8 to 9 week placebo-controlled clinical trials with 315 pediatric outpatients ages 8 to less than or equal to 18 [see Clinical Studies (14.1)].
The efficacy of fluoxetine for the treatment of OCD was demonstrated in one 13 week placebo-controlled clinical trial with 103 pediatric outpatients ages 7 to less than 18 [see Clinical Studies (14.2)].
The safety and effectiveness in pediatric patients less than 8 years of age in Major Depressive Disorder and less than 7 years of age in OCD have not been established.
Fluoxetine pharmacokinetics were evaluated in 21 pediatric patients (ages 6 to less than or equal to 18) with Major Depressive Disorder or OCD [see Clinical Pharmacology (12.3)].
The acute adverse reaction profiles observed in the 3 studies (N = 418 randomized; 228 fluoxetine-treated, 190 placebo-treated) were generally similar to that observed in adult studies with fluoxetine. The longer-term adverse reaction profile observed in the 19 week Major Depressive Disorder study (N = 219 randomized; 109 fluoxetine-treated, 110 placebo-treated) was also similar to that observed in adult trials with fluoxetine [see Adverse Reactions (6.1)].
Manic reaction, including mania and hypomania, was reported in 6 (1 mania, 5 hypomania) out of 228 (2.6%) fluoxetine-treated patients and in 0 out of 190 (0%) placebo-treated patients. Mania/hypomania led to the discontinuation of 4 (1.8%) fluoxetine-treated patients from the acute phases of the 3 studies combined. Consequently, regular monitoring for the occurrence of mania/hypomania is recommended.
As with other SSRIs, decreased weight gain has been observed in association with the use of fluoxetine in children and adolescent patients. After 19 weeks of treatment in a clinical trial, pediatric subjects treated with fluoxetine gained an average of 1.1 cm less in height and 1.1 kg less in weight than subjects treated with placebo. In addition, fluoxetine treatment was associated with a decrease in alkaline phosphatase levels. The safety of fluoxetine treatment for pediatric patients has not been systematically assessed for chronic treatment longer than several months in duration. In particular, there are no studies that directly evaluate the longer-term effects of fluoxetine on the growth, development and maturation of children and adolescent patients. Therefore, height and weight should be monitored periodically in pediatric patients receiving fluoxetine [see Warnings and Precautions (5.6)].
Fluoxetine is approved for use in pediatric patients with MDD and OCD [see Box Warning and Warnings and Precautions (5.1)]. Anyone considering the use of fluoxetine in a child or adolescent must balance the potential risks with the clinical need.
Significant toxicity, including myotoxicity, long-term neurobehavioral and reproductive toxicity, and impaired bone development, has been observed following exposure of juvenile animals to fluoxetine. Some of these effects occurred at clinically relevant exposures.
In a study in which fluoxetine (3, 10, or 30 mg/kg) was orally administered to young rats from weaning (Postnatal Day 21) through adulthood (Day 90), male and female sexual development was delayed at all doses, and growth (body weight gain, femur length) was decreased during the dosing period in animals receiving the highest dose. At the end of the treatment period, serum levels of creatine kinase (marker of muscle damage) were increased at the intermediate and high doses, and abnormal muscle and reproductive organ histopathology (skeletal muscle degeneration and necrosis, testicular degeneration and necrosis, epididymal vacuolation and hypospermia) was observed at the high dose. When animals were evaluated after a recovery period (up to 11 weeks after cessation of dosing), neurobehavioral abnormalities (decreased reactivity at all doses and learning deficit at the high dose) and reproductive functional impairment (decreased mating at all doses and impaired fertility at the high dose) were seen; in addition, testicular and epididymal microscopic lesions and decreased sperm concentrations were found in the high dose group, indicating that the reproductive organ effects seen at the end of treatment were irreversible. The reversibility of fluoxetine-induced muscle damage was not assessed. Adverse effects similar to those observed in rats treated with fluoxetine during the juvenile period have not been reported after administration of fluoxetine to adult animals. Plasma exposures (AUC) to fluoxetine in juvenile rats receiving the low, intermediate, and high dose in this study were approximately 0.1 to 0.2, 1 to 2, and 5 to 10 times, respectively, the average exposure in pediatric patients receiving the maximum recommended dose (MRD) of 20 mg/day. Rat exposures to the major metabolite, norfluoxetine, were approximately 0.3 to 0.8, 1 to 8, and 3 to 20 times, respectively, pediatric exposure at the MRD.
A specific effect of fluoxetine on bone development has been reported in mice treated with fluoxetine during the juvenile period. When mice were treated with fluoxetine (5 or 20 mg/kg, intraperitoneal) for 4 weeks starting at 4 weeks of age, bone formation was reduced resulting in decreased bone mineral content and density. These doses did not affect overall growth (body weight gain or femoral length). The doses administered to juvenile mice in this study are approximately 0.5 and 2 times the MRD for pediatric patients on a body surface area (mg/m2) basis.
In another mouse study, administration of fluoxetine (10 mg/kg intraperitoneal) during early postnatal development (Postnatal Days 4 to 21) produced abnormal emotional behaviors (decreased exploratory behavior in elevated plus-maze, increase shock avoidance latency) in adulthood (12 weeks of age). The dose used in this study is approximately equal to the pediatric MRD on a mg/m2 basis. Because of the early dosing period in this study, the significance of these findings to the approved pediatric use in humans is uncertain.
8.5 Geriatric Use 8.6 Hepatic Impairment
8.5 Geriatric Use
U.S. fluoxetine clinical trials included 687 patients greater than or equal to 65 years of age and 93 patients greater than or equal to 75 years of age. The efficacy in geriatric patients has been established [see Clinical Studies (14.1)]. For pharmacokinetic information in geriatric patients, [see Clinical Pharmacology (12.4)]. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. SNRIs and SSRIs, including fluoxetine, have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse reaction [see Warnings and Precautions (5.8)].
8.6 Hepatic Impairment
In subjects with cirrhosis of the liver, the clearances of fluoxetine and its active metabolite, norfluoxetine, were decreased, thus increasing the elimination half-lives of these substances. A lower or less frequent dose of fluoxetine should be used in patients with cirrhosis. Caution is advised when using fluoxetine in patients with diseases or conditions that could affect its metabolism [see Dosage and Administration (2.7) and Clinical Pharmacology (12.4)].
9.3 Dependence
9 DRUG ABUSE AND DEPENDENCE
9.3 Dependence
Fluoxetine has not been systematically studied, in animals or humans, for its potential for abuse, tolerance, or physical dependence. While the premarketing clinical experience with fluoxetine did not reveal any tendency for a withdrawal syndrome or any drug seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS active drug will be misused, diverted, and/or abused once marketed. Consequently, physicians should carefully evaluate patients for history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of fluoxetine (e.g., development of tolerance, incrementation of dose, drug-seeking behavior).
10.1 Human Experience 10.2 Animal Experience 10.3 Management of Overdose
10 OVERDOSAGE
10.1 Human Experience
Worldwide exposure to fluoxetine hydrochloride is estimated to be over 38 million patients (circa 1999). Of the 1578 cases of overdose involving fluoxetine hydrochloride, alone or with other drugs, reported from this population, there were 195 deaths.
Among 633 adult patients who overdosed on fluoxetine hydrochloride alone, 34 resulted in a fatal outcome, 378 completely recovered, and 15 patients experienced sequelae after overdosage, including abnormal accommodation, abnormal gait, confusion, unresponsiveness, nervousness, pulmonary dysfunction, vertigo, tremor, elevated blood pressure, impotence, movement disorder, and hypomania. The remaining 206 patients had an unknown outcome. The most common signs and symptoms associated with non-fatal overdosage were seizures, somnolence, nausea, tachycardia, and vomiting. The largest known ingestion of fluoxetine hydrochloride in adult patients was 8 grams in a patient who took fluoxetine alone and who subsequently recovered. However, in an adult patient who took fluoxetine alone, an ingestion as low as 520 mg has been associated with lethal outcome, but causality has not been established.
Among pediatric patients (ages 3 months to 17 years), there were 156 cases of overdose involving fluoxetine alone or in combination with other drugs. Six patients died, 127 patients completely recovered, 1 patient experienced renal failure, and 22 patients had an unknown outcome. One of the six fatalities was a 9-year-old boy who had a history of OCD, Tourette’s syndrome with tics, attention deficit disorder, and fetal alcohol syndrome. He had been receiving 100 mg of fluoxetine daily for 6 months in addition to clonidine, methylphenidate, and promethazine. Mixed-drug ingestion or other methods of suicide complicated all 6 overdoses in children that resulted in fatalities. The largest ingestion in pediatric patients was 3 grams which was nonlethal.
Other important adverse reactions reported with fluoxetine overdose (single or multiple drugs) include coma, delirium, ECG abnormalities (such as QT interval prolongation and ventricular tachycardia, including torsade de pointes-type arrhythmias), hypotension, mania, neuroleptic malignant syndrome-like reactions, pyrexia, stupor, and syncope.
10.2 Animal Experience
Studies in animals do not provide precise or necessarily valid information about the treatment of human overdose. However, animal experiments can provide useful insights into possible treatment strategies.
The oral median lethal dose in rats and mice was found to be 452 and 248 mg/kg, respectively. Acute high oral doses produced hyperirritability and convulsions in several animal species.
Among 6 dogs purposely overdosed with oral fluoxetine, 5 experienced grand mal seizures. Seizures stopped immediately upon the bolus intravenous administration of a standard veterinary dose of diazepam. In this short-term study, the lowest plasma concentration at which a seizure occurred was only twice the maximum plasma concentration seen in humans taking 80 mg/day, chronically.
In a separate single-dose study, the ECG of dogs given high doses did not reveal prolongation of the PR, QRS, or QT intervals. Tachycardia and an increase in blood pressure were observed. Consequently, the value of the ECG in predicting cardiac toxicity is unknown. Nonetheless, the ECG should ordinarily be monitored in cases of human overdose [see Overdosage (10.3)].
10.3 Management of Overdose
Treatment should consist of those general measures employed in the management of overdosage with any drug effective in the treatment of Major Depressive Disorder.
Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. General supportive and symptomatic measures are also recommended. Induction of emesis is not recommended. Gastric lavage with a large-bore orogastric tube with appropriate airway protection, if needed, may be indicated if performed soon after ingestion, or in symptomatic patients.
Activated charcoal should be administered. Due to the large volume of distribution of this drug, forced diuresis, dialysis, hemoperfusion, and exchange transfusion are unlikely to be of benefit. No specific antidotes for fluoxetine are known.
A specific caution involves patients who are taking or have recently taken fluoxetine and might ingest excessive quantities of a TCA. In such a case, accumulation of the parent tricyclic and/or an active metabolite may increase the possibility of clinically significant sequelae and extend the time needed for close medical observation [see Drug Interactions (7.9)].
Based on experience in animals, which may not be relevant to humans, fluoxetine-induced seizures that fail to remit spontaneously may respond to diazepam.
In managing overdosage, consider the possibility of multiple drug involvement. The physician should consider contacting a poison control center for additional information on the treatment of any overdose. Telephone numbers for certified poison control centers are listed in the Physicians’ Desk Reference (PDR).
11 DESCRIPTION
Fluoxetine Hydrochloride is a psychotropic drug for oral administration. It is also marketed for the treatment of premenstrual dysphoric disorder (Sarafem®, fluoxetine hydrochloride). It is designated (±)-N-methyl-3-phenyl-3-[(α,α,α-trifluoro-p-tolyl)oxy]propylamine hydrochloride. Fluoxetine Hydrochloride has the following structural formula:
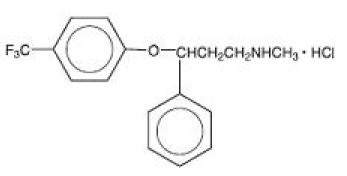
C17H18F3NO•HCl M.W. 345.79
Fluoxetine hydrochloride is a white to off-white crystalline solid with a solubility of 14 mg/mL in water.
Each capsule, for oral administration, contains fluoxetine hydrochloride equivalent to 10 mg (32.3 μmol) or 20 mg (64.7 μmol) of fluoxetine. In addition, the capsules also contain the following inactive ingredients: ammonium hydroxide, DandC yellow #10, FDandC blue #1, gelatin, magnesium stearate, pregelatinized corn starch, propylene glycol, shellac, and titanium dioxide.
12.1 Mechanism of Action
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Although the exact mechanism of fluoxetine is unknown, it is presumed to be linked to its inhibition of CNS neuronal uptake of serotonin.
12.2 Pharmacodynamics
12.2 Pharmacodynamics
Studies at clinically relevant doses in man have demonstrated that fluoxetine blocks the uptake of serotonin into human platelets. Studies in animals also suggest that fluoxetine is a much more potent uptake inhibitor of serotonin than of norepinephrine.
Antagonism of muscarinic, histaminergic, and α1-adrenergic receptors has been hypothesized to be associated with various anticholinergic, sedative, and cardiovascular effects of classical tricyclic antidepressant (TCA) drugs. Fluoxetine binds to these and other membrane receptors from brain tissue much less potently in vitro than do the tricyclic drugs.
12.3 Pharmacokinetics 12.4 Specific Populations
12.3 Pharmacokinetics
Systemic Bioavailability — In man, following a single oral 40 mg dose, peak plasma concentrations of fluoxetine from 15 to 55 ng/mL are observed after 6 to 8 hours.
The capsule, tablet, and oral solution dosage forms of fluoxetine are bioequivalent. Food does not appear to affect the systemic bioavailability of fluoxetine, although it may delay its absorption by 1 to 2 hours, which is probably not clinically significant. Thus, fluoxetine may be administered with or without food.
Protein Binding — Over the concentration range from 200 to 1000 ng/mL, approximately 94.5% of fluoxetine is bound in vitro to human serum proteins, including albumin and α1-glycoprotein. The interaction between fluoxetine and other highly protein-bound drugs has not been fully evaluated, but may be important.
Enantiomers — Fluoxetine is a racemic mixture (50/50) of R-fluoxetine and S-fluoxetine enantiomers. In animal models, both enantiomers are specific and potent serotonin uptake inhibitors with essentially equivalent pharmacologic activity. The S-fluoxetine enantiomer is eliminated more slowly and is the predominant enantiomer present in plasma at steady state.
Metabolism — Fluoxetine is extensively metabolized in the liver to norfluoxetine and a number of other unidentified metabolites. The only identified active metabolite, norfluoxetine, is formed by demethylation of fluoxetine. In animal models, S-norfluoxetine is a potent and selective inhibitor of serotonin uptake and has activity essentially equivalent to R- or S-fluoxetine. R-norfluoxetine is significantly less potent than the parent drug in the inhibition of serotonin uptake. The primary route of elimination appears to be hepatic metabolism to inactive metabolites excreted by the kidney.
Variability in Metabolism — A subset (about 7%) of the population has reduced activity of the drug metabolizing enzyme cytochrome P450 2D6 (CYP2D6). Such individuals are referred to as “poor metabolizers” of drugs such as debrisoquin, dextromethorphan, and the TCAs. In a study involving labeled and unlabeled enantiomers administered as a racemate, these individuals metabolized S-fluoxetine at a slower rate and thus achieved higher concentrations of S-fluoxetine. Consequently, concentrations of S-norfluoxetine at steady state were lower. The metabolism of R-fluoxetine in these poor metabolizers appears normal. When compared with normal metabolizers, the total sum at steady state of the plasma concentrations of the 4 active enantiomers was not significantly greater among poor metabolizers. Thus, the net pharmacodynamic activities were essentially the same. Alternative, nonsaturable pathways (non-2D6) also contribute to the metabolism of fluoxetine. This explains how fluoxetine achieves a steady-state concentration rather than increasing without limit.
Because fluoxetine’s metabolism, like that of a number of other compounds including TCAs and other selective serotonin reuptake inhibitors (SSRIs), involves the CYP2D6 system, concomitant therapy with drugs also metabolized by this enzyme system (such as the TCAs) may lead to drug interactions [see Drug Interactions (7.9)].
Accumulation and Slow Elimination — The relatively slow elimination of fluoxetine (elimination half-life of 1 to 3 days after acute administration and 4 to 6 days after chronic administration) and its active metabolite, norfluoxetine (elimination half-life of 4 to 16 days after acute and chronic administration), leads to significant accumulation of these active species in chronic use and delayed attainment of steady state, even when a fixed dose is used [see Warnings and Precautions (5.12)]. After 30 days of dosing at 40 mg/day, plasma concentrations of fluoxetine in the range of 91 to 302 ng/mL and norfluoxetine in the range of 72 to 258 ng/mL have been observed. Plasma concentrations of fluoxetine were higher than those predicted by single-dose studies, because fluoxetine’s metabolism is not proportional to dose. Norfluoxetine, however, appears to have linear pharmacokinetics. Its mean terminal half-life after a single dose was 8.6 days and after multiple dosing was 9.3 days. Steady-state levels after prolonged dosing are similar to levels seen at 4 to 5 weeks.
The long elimination half-lives of fluoxetine and norfluoxetine assure that, even when dosing is stopped, active drug substance will persist in the body for weeks (primarily depending on individual patient characteristics, previous dosing regimen, and length of previous therapy at discontinuation). This is of potential consequence when drug discontinuation is required or when drugs are prescribed that might interact with fluoxetine and norfluoxetine following the discontinuation of fluoxetine.
12.4 Specific Populations
Liver Disease — As might be predicted from its primary site of metabolism, liver impairment can affect the elimination of fluoxetine. The elimination half-life of fluoxetine was prolonged in a study of cirrhotic patients, with a mean of 7.6 days compared with the range of 2 to 3 days seen in subjects without liver disease; norfluoxetine elimination was also delayed, with a mean duration of 12 days for cirrhotic patients compared with the range of 7 to 9 days in normal subjects. This suggests that the use of fluoxetine in patients with liver disease must be approached with caution. If fluoxetine is administered to patients with liver disease, a lower or less frequent dose should be used [see Dosage and Administration (2.7), Use in Specific Populations (8.6)].
Renal Disease — In depressed patients on dialysis (N = 12), fluoxetine administered as 20 mg once daily for 2 months produced steady-state fluoxetine and norfluoxetine plasma concentrations comparable with those seen in patients with normal renal function. While the possibility exists that renally excreted metabolites of fluoxetine may accumulate to higher levels in patients with severe renal dysfunction, use of a lower or less frequent dose is not routinely necessary in renally impaired patients.
Geriatric Pharmacokinetics — The disposition of single doses of fluoxetine in healthy elderly subjects (greater than 65 years of age) did not differ significantly from that in younger normal subjects. However, given the long half-life and nonlinear disposition of the drug, a single-dose study is not adequate to rule out the possibility of altered pharmacokinetics in the elderly, particularly if they have systemic illness or are receiving multiple drugs for concomitant diseases. The effects of age upon the metabolism of fluoxetine have been investigated in 260 elderly but otherwise healthy depressed patients (greater than or equal to 60 years of age) who received 20 mg fluoxetine for 6 weeks. Combined fluoxetine plus norfluoxetine plasma concentrations were 209.3 ± 85.7 ng/mL at the end of 6 weeks. No unusual age-associated pattern of adverse reactions was observed in those elderly patients.
Pediatric Pharmacokinetics (children and adolescents) — Fluoxetine pharmacokinetics were evaluated in 21 pediatric patients (10 children ages 6 to less than 13, 11 adolescents ages 13 to less than 18) diagnosed with Major Depressive Disorder or Obsessive Compulsive Disorder (OCD). Fluoxetine 20 mg/day was administered for up to 62 days. The average steady-state concentrations of fluoxetine in these children were 2 fold higher than in adolescents (171 and 86 ng/mL, respectively). The average norfluoxetine steady-state concentrations in these children were 1.5 fold higher than in adolescents (195 and 113 ng/mL, respectively). These differences can be almost entirely explained by differences in weight. No gender-associated difference in fluoxetine pharmacokinetics was observed. Similar ranges of fluoxetine and norfluoxetine plasma concentrations were observed in another study in 94 pediatric patients (ages 8 to less than 18) diagnosed with Major Depressive Disorder.
Higher average steady-state fluoxetine and norfluoxetine concentrations were observed in children relative to adults; however, these concentrations were within the range of concentrations observed in the adult population. As in adults, fluoxetine and norfluoxetine accumulated extensively following multiple oral dosing; steady-state concentrations were achieved within 3 to 4 weeks of daily dosing.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity — The dietary administration of fluoxetine to rats and mice for 2 years at doses of up to 10 and 12 mg/kg/day, respectively [approximately 1.2 and 0.7 times, respectively, the maximum recommended human dose (MRHD) of 80 mg on a mg/m2 basis], produced no evidence of carcinogenicity.
Mutagenicity — Fluoxetine and norfluoxetine have been shown to have no genotoxic effects based on the following assays: bacterial mutation assay, DNA repair assay in cultured rat hepatocytes, mouse lymphoma assay, and in vivo sister chromatid exchange assay in Chinese hamster bone marrow cells.
Impairment of Fertility — Two fertility studies conducted in adult rats at doses of up to 7.5 and 12.5 mg/kg/day (approximately 0.9 and 1.5 times the MRHD on a mg/m2 basis) indicated that fluoxetine had no adverse effects on fertility. However, adverse effects on fertility were seen when juvenile rats were treated with fluoxetine [see Use in Specific Populations (8.4)].
13.2 Animal Toxicology and/or Pharmacology
Phospholipids are increased in some tissues of mice, rats, and dogs given fluoxetine chronically. This effect is reversible after cessation of fluoxetine treatment. Phospholipid accumulation in animals has been observed with many cationic amphiphilic drugs, including fenfluramine, imipramine, and ranitidine. The significance of this effect in humans is unknown.
14.1 Major Depressive Disorder 14.2 Obsessive Compulsive Disorder 14.3 Bulimia Nervosa 14.4 Panic Disorder
14 CLINICAL STUDIES
14.1 Major Depressive Disorder
Daily Dosing
Adult — The efficacy of fluoxetine was studied in 5 and 6 week placebo-controlled trials with depressed adult and geriatric outpatients (greater than or equal to 18 years of age) whose diagnoses corresponded most closely to the DSM-III (currently DSM-IV) category of Major Depressive Disorder. Fluoxetine was shown to be significantly more effective than placebo as measured by the Hamilton Depression Rating Scale (HAM-D). Fluoxetine was also significantly more effective than placebo on the HAM-D subscores for depressed mood, sleep disturbance, and the anxiety subfactor.
Two 6 week controlled studies (N = 671, randomized) comparing fluoxetine 20 mg and placebo have shown fluoxetine 20 mg daily to be effective in the treatment of elderly patients (greater than or equal to 60 years of age) with Major Depressive Disorder. In these studies, fluoxetine produced a significantly higher rate of response and remission as defined, respectively, by a 50% decrease in the HAM-D score and a total endpoint HAM-D score of less than or equal to 8. Fluoxetine was well tolerated and the rate of treatment discontinuations due to adverse reactions did not differ between fluoxetine (12%) and placebo (9%).
A study was conducted involving depressed outpatients who had responded (modified HAMD-17 score of ≤ 7 during each of the last 3 weeks of open-label treatment and absence of Major Depressive Disorder by DSM-III-R criteria) by the end of an initial 12 week open-treatment phase on fluoxetine 20 mg/day. These patients (N = 298) were randomized to continuation on double-blind fluoxetine 20 mg/day or placebo. At 38 weeks (50 weeks total), a statistically significantly lower relapse rate (defined as symptoms sufficient to meet a diagnosis of Major Depressive Disorder for 2 weeks or a modified HAMD-17 score of greater than or equal to 14 for 3 weeks) was observed for patients taking fluoxetine compared with those on placebo.
Pediatric (children and adolescents) — The efficacy of fluoxetine 20 mg/day in children and adolescents (N = 315 randomized; 170 children ages 8 to less than 13, 145 adolescents ages 13 to less than or equal to 18) was studied in two 8 to 9 week placebo-controlled clinical trials in depressed outpatients whose diagnoses corresponded most closely to the DSM-III-R or DSM-IV category of Major Depressive Disorder.
In both studies independently, fluoxetine produced a statistically significantly greater mean change on the Childhood Depression Rating Scale-Revised (CDRS-R) total score from baseline to endpoint than did placebo.
Subgroup analyses on the CDRS-R total score did not suggest any differential responsiveness on the basis of age or gender.
14.2 Obsessive Compulsive Disorder
Adult — The effectiveness of fluoxetine for the treatment of Obsessive Compulsive Disorder (OCD) was demonstrated in two 13 week, multicenter, parallel group studies (Studies 1 and 2) of adult outpatients who received fixed fluoxetine doses of 20, 40, or 60 mg/day (on a once-a-day schedule, in the morning) or placebo. Patients in both studies had moderate to severe OCD (DSM-III-R), with mean baseline ratings on the Yale-Brown Obsessive Compulsive Scale (YBOCS, total score) ranging from 22 to 26. In Study 1, patients receiving fluoxetine experienced mean reductions of approximately 4 to 6 units on the YBOCS total score, compared with a 1 unit reduction for placebo patients. In Study 2, patients receiving fluoxetine experienced mean reductions of approximately 4 to 9 units on the YBOCS total score, compared with a 1 unit reduction for placebo patients. While there was no indication of a dose-response relationship for effectiveness in Study 1, a dose-response relationship was observed in Study 2, with numerically better responses in the 2 higher dose groups. The following table provides the outcome classification by treatment group on the Clinical Global Impression (CGI) improvement scale for Studies 1 and 2 combined:
|
|
|
Fluoxetine |
|
|
| Outcome Classification |
Placebo |
20 mg |
40 mg |
60 mg |
| Worse |
8% |
0% |
0% |
0% |
| No change |
64% |
41% |
33% |
29% |
| Minimally improved |
17% |
23% |
28% |
24% |
| Much improved |
8% |
28% |
27% |
28% |
| Very much improved | 3% | 8% | 12% | 19% |
Exploratory analyses for age and gender effects on outcome did not suggest any differential responsiveness on the basis of age or sex.
Pediatric (children and adolescents) — In one 13 week clinical trial in pediatric patients (N = 103 randomized; 75 children ages 7 to less than 13, 28 adolescents ages 13 to less than 18) with OCD (DSM-IV), patients received fluoxetine 10 mg/day for 2 weeks, followed by 20 mg/day for 2 weeks. The dose was then adjusted in the range of 20 to 60 mg/day on the basis of clinical response and tolerability. Fluoxetine produced a statistically significantly greater mean change from baseline to endpoint than did placebo as measured by the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS).
Subgroup analyses on outcome did not suggest any differential responsiveness on the basis of age or gender.
14.3 Bulimia Nervosa
The effectiveness of fluoxetine for the treatment of bulimia was demonstrated in two 8 week and one 16 week, multicenter, parallel group studies of adult outpatients meeting DSM-III-R criteria for bulimia. Patients in the 8 week studies received either 20 or 60 mg/day of fluoxetine or placebo in the morning. Patients in the 16 week study received a fixed fluoxetine dose of 60 mg/day (once a day) or placebo. Patients in these 3 studies had moderate to severe bulimia with median binge-eating and vomiting frequencies ranging from 7 to 10 per week and 5 to 9 per week, respectively. In these 3 studies, fluoxetine 60 mg, but not 20 mg, was statistically significantly superior to placebo in reducing the number of binge-eating and vomiting episodes per week. The statistically significantly superior effect of 60 mg versus placebo was present as early as Week 1 and persisted throughout each study. The fluoxetine-related reduction in bulimic episodes appeared to be independent of baseline depression as assessed by the Hamilton Depression Rating Scale. In each of these 3 studies, the treatment effect, as measured by differences between fluoxetine 60 mg and placebo on median reduction from baseline in frequency of bulimic behaviors at endpoint, ranged from 1 to 2 episodes per week for binge-eating and 2 to 4 episodes per week for vomiting. The size of the effect was related to baseline frequency, with greater reductions seen in patients with higher baseline frequencies. Although some patients achieved freedom from binge-eating and purging as a result of treatment, for the majority, the benefit was a partial reduction in the frequency of binge-eating and purging.
In a longer-term trial, 150 patients meeting DSM-IV criteria for Bulimia Nervosa, purging subtype, who had responded during a single-blind, 8 week acute treatment phase with fluoxetine 60 mg/day, were randomized to continuation of fluoxetine 60 mg/day or placebo, for up to 52 weeks of observation for relapse. Response during the single-blind phase was defined by having achieved at least a 50% decrease in vomiting frequency compared with baseline. Relapse during the double-blind phase was defined as a persistent return to baseline vomiting frequency or physician judgment that the patient had relapsed. Patients receiving continued fluoxetine 60 mg/day experienced a significantly longer time to relapse over the subsequent 52 weeks compared with those receiving placebo.
14.4 Panic Disorder
The effectiveness of fluoxetine in the treatment of Panic Disorder was demonstrated in 2 double-blind, randomized, placebo-controlled, multicenter studies of adult outpatients who had a primary diagnosis of Panic Disorder (DSM-IV), with or without agoraphobia.
Study 1 (N = 180 randomized) was a 12 week flexible-dose study. Fluoxetine was initiated at 10 mg/day for the first week, after which patients were dosed in the range of 20 to 60 mg/day on the basis of clinical response and tolerability. A statistically significantly greater percentage of fluoxetine-treated patients were free from panic attacks at endpoint than placebo-treated patients, 42% versus 28%, respectively.
Study 2 (N = 214 randomized) was a 12 week flexible-dose study. Fluoxetine was initiated at 10 mg/day for the first week, after which patients were dosed in a range of 20 to 60 mg/day on the basis of clinical response and tolerability. A statistically significantly greater percentage of fluoxetine-treated patients were free from panic attacks at endpoint than placebo-treated patients, 62% versus 44%, respectively.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Fluoxetine Capsules USP 10 mg are available as white, opaque capsules in bottles of 100, 500 and 1000, printed PLIVA 647 in green band on cap and body.
Fluoxetine Capsules USP 20 mg are available as white, opaque capsules in bottles of 100, 500, 1000 and 2000, printed PLIVA 648 in green band on cap only.
PHARMACIST: Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
16.2 Storage and Handling
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
PROTECT FROM LIGHT
KEEP TIGHTLY CLOSED
Sarafem® is a registered trademark of Eli Lilly and Company.
17.1 General Information 17.2 Clinical Worsening and Suicide Risk 17.3 Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions 17.4 Allergic Reactions and Rash 17.5 Abnormal Bleeding 17.6 Hyponatremia 17.7 Potential for Cognitive and Mot
17 PATIENT COUNSELING INFORMATION
See the FDA-approved Medication Guide.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking fluoxetine.
17.1 General Information
Healthcare providers should instruct their patients to read the Medication Guide before starting therapy with fluoxetine capsules and to reread it each time the prescription is renewed.
Healthcare providers should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with fluoxetine capsules and should counsel them in its appropriate use. Healthcare providers should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have.
Patients should be advised of the following issues and asked to alert their healthcare provider if these occur while taking fluoxetine capsules.
17.2 Clinical Worsening and Suicide Risk
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient’s prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication [see Box Warning and Warnings and Precautions (5.1)].
17.3 Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-Like Reactions
Patients should be cautioned about the risk of serotonin syndrome or NMS-like reactions with the concomitant use of fluoxetine and triptans, tramadol, or other serotonergic agents [see Warnings and Precautions (5.2) and Drug Interactions (7.3)].
Patients should be advised of the signs and symptoms associated with serotonin syndrome or NMS-like reactions that may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination) and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Serotonin syndrome, in its most severe form can resemble neuroleptic malignant syndrome, in which the symptoms may include hyperthermia, muscle rigidity, autonomic instability with possible rapid fluctuation of vital signs, and mental status changes. Patients should be cautioned to seek medical care immediately if they experience these symptoms.
17.4 Allergic Reactions and Rash
Patients should be advised to notify their physician if they develop a rash or hives [see Warnings and Precautions (5.3)]. Patients should also be advised of the signs and symptoms associated with a severe allergic reaction, including swelling of the face, eyes, or mouth, or have trouble breathing. Patients should be cautioned to seek medical care immediately if they experience these symptoms.
17.5 Abnormal Bleeding
Patients should be cautioned about the concomitant use of fluoxetine and NSAIDs, aspirin, warfarin, or other drugs that affect coagulation since combined use of psychotropic drugs that interfere with serotonin reuptake and these agents have been associated with an increased risk of bleeding [see Warnings and Precautions (5.7) and Drug Interactions (7.6)]. Patients should be advised to call their doctor if they experience any increased or unusual bruising or bleeding while taking fluoxetine.
17.6 Hyponatremia
Patients should be advised that hyponatremia has been reported as a result of treatment with SNRIs and SSRIs, including fluoxetine. Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. More severe and/or acute cases have been associated with hallucination, syncope, seizure, coma, respiratory arrest, and death [see Warnings and Precautions (5.8)].
17.7 Potential for Cognitive and Motor Impairment
Fluoxetine may impair judgment, thinking, or motor skills. Patients should be advised to avoid driving a car or operating hazardous machinery until they are reasonably certain that their performance is not affected [see Warnings and Precautions (5.11)].
17.8 Use of Concomitant Medications
Patients should be advised to inform their physician if they are taking, or plan to take, any prescription medication, including Symbyax®, Sarafem®, or over-the-counter drugs, including herbal supplements or alcohol. Patients should also be advised to inform their physicians if they plan to discontinue any medications they are taking while on fluoxetine.
17.9 Discontinuation of Treatment
Patients should be advised to take fluoxetine exactly as prescribed, and to continue taking fluoxetine as prescribed even after their symptoms improve. Patients should be advised that they should not alter their dosing regimen, or stop taking fluoxetine without consulting their physician [see Warnings and Precautions (5.13)]. Patients should be advised to consult with their healthcare provider if their symptoms do not improve with fluoxetine.
17.10 Use in Specific Populations
Pregnancy — Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy. Fluoxetine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus [see Use in Specific Populations (8.1)].
Nursing Mothers — Patients should be advised to notify their physician if they intend to breast-feed an infant during therapy. Because fluoxetine is excreted in human milk, nursing while taking fluoxetine is not recommended [see Use in Specific Populations (8.3)].
Pediatric Use — Fluoxetine is approved for use in pediatric patients with MDD and OCD [see Box Warning and Warnings and Precautions (5.1)]. Limited evidence is available concerning the longer-term effects of fluoxetine on the development and maturation of children and adolescent patients. Height and weight should be monitored periodically in pediatric patients receiving fluoxetine [see Warnings and Precautions (5.6) and Use in Specific Populations (8.4)].
Manufactured by: PLIVA
for: PLIVA®, Inc., Pomona, NY 10970
Dist. by Barr Laboratories, Inc., Pomona, NY 10970
Iss. 1/2010
MEDICATION GUIDE
FLUOXETINE CAPSULES USP
Rx only
Read the Medication Guide that comes with fluoxetine capsules USP before you start taking them and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your doctor about your medical condition or treatment. Talk with your doctor or pharmacist if there is something you do not understand or you want to learn more about fluoxetine capsules USP.
What is the most important information I should know about fluoxetinecapsules USP?
Antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions:
Talk to your, or your family member’s, healthcare provider about:
- all risks and benefits of treatment with antidepressant medicines
- all treatment choices for depression or other serious mental illness
1. Antidepressant medicines may increase suicidal thoughts or actions in some
children, teenagers, and young adults within the first few months of treatment.
2. Depression and other serious mental illnesses are the most important causes
of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) bipolar illness (also called manic-depressive illness) or suicidal thoughts or actions.
3. How can I watch for and try to prevent suicidal thoughts and actions in
myself or a family member?
- Pay close attention to any changes, especially sudden changes, in mood,
behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed
- Call the healthcare provider right away to report new or sudden changes in
mood, behavior, thoughts, or feelings.
- Keep all follow-up visits with the healthcare provider as scheduled. Call
the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling very agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- or other unusual changes in behavior or mood
What else do I need to know about antidepressant medicines?
- Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms.
- Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.
- Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.
- Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member takes. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.
- Not all antidepressant medicines prescribed for children are FDA approved for use in children. Talk to your child’s healthcare provider for more information.
What are fluoxetine capsules USP?
Fluoxetine capsules USP are a prescription medicine used:
- for short and long-term treatment of depression in adults and children over the age of 8.
- for short and long-term treatment of Obsessive Compulsive Disorder (OCD) in adults and children over the age of 7.
- for short and long-term treatment of Bulimia Nervosa in adults.
- for short-term treatment of Panic Disorder, with or without agoraphobia, in adults.
The symptoms of depression (Major Depressive Disorder) include decreased mood, decreased interest, increased guilty feelings, decreased energy, decreased concentration, changes in appetite, and suicidal thoughts or behavior. With treatment, some of your symptoms of depression may improve.
OCD is an anxiety disorder and is characterized by recurrent, unwanted thoughts (obsessions) and/or repetitive behaviors (compulsions). With treatment, some of your symptoms of OCD may improve.
Panic Disorder is an anxiety disorder that includes panic attacks, which are sudden feelings of terror for no reason. You may also have physical symptoms, such as; fast heartbeat, chest pain, breathing difficulty, dizziness. With treatment, some of your symptoms of Panic Disorder may improve.
Bulimia Nervosa, involves periods of overeating followed by purging (e.g., vomiting, excessive laxative use). With treatment, some of your symptoms of Bulimia Nervosa may improve.
If you do not think you are getting better, call your doctor.
Who should not take fluoxetine capsules USP?
- Do not take fluoxetine capsules USP if you take a Monoamine Oxidase Inhibitor (MAOI) or if you stopped taking an MAOI in the last 2 weeks.
- Do not take an MAOI within 5 weeks of stopping fluoxetinecapsules USP. People who take fluoxetine capsules USP close in time to an MAOI can have serious and life-threatening side effects, with symptoms including:
- high fever
- continued muscle spasms that you can not control
- rigid muscles
- changes in heart rate and blood pressure that happen fast
- confusion
- unconsciousness
Ask your doctor or pharmacist if you are not sure if your medicine is an MAOI.
- Do not take fluoxetine capsules USP if you take Mellaril® (thioridazine). Do not take Mellaril®within 5 weeks of stopping fluoxetinecapsules USP. Mellaril® can cause serious heart rhythm problems and you could die suddenly.
- Do not take fluoxetine capsules USP if you take the antipsychotic medicine pimozide (Orap®).
What should I tell my doctor before taking fluoxetinecapsules USP?
Fluoxetine capsules USP may not be right for you. Before starting fluoxetine capsules USP, tell your doctor about all your medical conditions, including if you have or had any of the following:
- seizures (convulsions)
- bipolar disorder (mania)
- are pregnant or plan to become pregnant. It is not known if fluoxetine
capsules USP will harm your unborn baby.
- are breast-feeding or plan to breast-feed. Fluoxetine can pass into your
breast milk and may harm your baby. You should not breast-feed while taking fluoxetine capsules USP. Talk to your doctor about the best way to feed your baby if you take fluoxetine capsules USP.
Tell your doctor about all the medicines that you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Fluoxetine capsules USP and some medicines may interact with each other and may not work as well, or cause possible serious side effects. Your doctor can tell you if it is safe to take fluoxetine capsules USP with your other medicines. Do not start or stop any medicine while taking fluoxetine capsules USP without talking to your doctor first.
If you take fluoxetinecapsules USP, you should not take any other medicines that contain fluoxetine hydrochloride:
- Symbyax®
- Sarafem®
- Prozac® Weekly™
You could take too much medicine (overdose).
How should I take fluoxetinecapsules USP?
- Take fluoxetine capsules USP exactly as prescribed. Your doctor may need to change (adjust) the dose of fluoxetine capsules USP until it is right for you.
- If you miss a dose of fluoxetine capsules USP, take the missed dose as soon as you remember. If it is almost time for the next dose, skip the missed dose and take your next dose at the regular time. Do not take two doses of fluoxetine capsules USP at the same time.
- To prevent serious side effects, do not stop taking fluoxetinecapsules USP suddenly. If you need to stop taking fluoxetine capsules USP, your doctor can tell you how to safely stop taking them.
- If you take too many fluoxetine capsules USP, call your doctor or poison control center right away, or get emergency treatment.
- Fluoxetine capsules USP can be taken with or without food.
- Fluoxetine capsules USP are usually taken once a day.
- If you do not think you are getting better or have any concerns about your condition while taking fluoxetine capsules USP, call your doctor.
What should I avoid while taking fluoxetinecapsules USP?
- Fluoxetine capsules USP can cause sleepiness and may affect your ability to make decisions, think clearly, or react quickly. You should not drive, operate heavy machinery, or do other dangerous activities until you know how fluoxetine capsules USP affect you.
What are the possible side effects of fluoxetine capsules USP?
Fluoxetine capsules USP may be associated with the following serious risks:
- Serotonin Syndrome: This is a condition that can be life threatening. Call your doctor right away if you become severely ill and have some or all of these symptoms:
- agitation
- hallucinations
- problems with coordination
- racing heart beat
- over-active reflexes
- fever
- nausea, vomiting, and diarrhea
- Severe allergic reactions: Tell your doctor right away if you get red itchy welts (hives) or, a rash alone or with fever and joint pain, while taking fluoxetine capsules USP. Call your doctor right away if you become severely ill and have some or all of these symptoms:
- swelling of your face, eyes, or mouth
- trouble breathing
- Abnormal bleeding: Tell your doctor if you notice any increased or unusual bruising or bleeding while taking fluoxetine capsules USP, especially if you take one of these medicines:
- the blood thinner warfarin (Coumadin®, Jantoven®)
- a non-steroidal anti-inflammatory drug (NSAID)
- aspirin
- Mania: You may have a high mood, become extremely irritable, have too much energy, feel pressure to keep talking, or have a decreased need for sleep.
- Seizures
- Loss of appetite
- Low salt (sodium) levels in the blood (hyponatremia): Call your doctor right away if you become severely ill and have some or all of these symptoms:
- headache
- feel weak
- confusion
- problems concentrating
- memory problems
- feel unsteady
Common possible side effects of fluoxetine capsules USP include: abnormal dreams, orgasm problems, decreased appetite, anxiety, weakness, diarrhea, dry mouth, indigestion, flu, difficulty maintaining an erection for sexual activity, trouble sleeping, decreased sex drive, feeling sick to your stomach, nervousness, sore throat, rash, watery nasal discharge, sleepiness, sweating, tremor (shakes), hot flashes, and yawn.
Tell your doctor about any side effect that bothers you or that does not go away.
These are not all the possible side effects with fluoxetine capsules USP. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store fluoxetinecapsules USP?
- Store fluoxetine capsules USP at room temperature, between 68°F to 77°F (20°C to 25°C).
- Keep fluoxetine capsules USP away from light.
- Keep fluoxetine capsules USP bottle closed tightly.
Keep fluoxetinecapsules USP and all medicines out of the reach of children.
General information about fluoxetinecapsules USP
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use fluoxetine capsules USP for a condition for which they were not prescribed. Do not give fluoxetine capsules USP to other people, even if they have the same condition. They may harm them.
This Medication Guide summarizes the most important information about fluoxetine capsules USP. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about fluoxetine capsules USP that was written for healthcare professionals. For more information about fluoxetine capsules USP call 1-888-838-2872, MEDICAL AFFAIRS.
What are the ingredients in fluoxetine capsules USP?
Active ingredient: fluoxetine hydrochloride.
Inactive ingredients: ammonium hydroxide, DandC Yellow #10, FDandC Blue #1, gelatin, magnesium stearate, pregelatinized corn starch, propylene glycol, shellac, and titanium dioxide.
Symbyax® and Sarafem® are registered trademarks of Eli Lilly and Company.
Prozac® Weekly™ is a trademark of Eli Lilly and Company.
Mellaril® is a registered trademark of Novartis AG Corporation.
Orap® is a registered trademark of Teva Pharmaceuticals USA.
Coumadin® is a registered trademark of Bristol Myers Squibb.
Jantoven® is a registered trademark of Upsher-Smith Laboratories Inc.
Manufactured by: PLIVA Krakow Pharmaceutical Company S.A.
Krakow, Poland
for: PLIVA®, Inc., Pomona, NY 10970
Dist. by Barr Laboratories, Inc., Pomona, NY 10970
Iss. 1/2010
EACH CAPSULE CONTAINS:
*Fluoxetine Hydrochloride, USP
equivalent to Fluoxetine ................. 10 mg
Dispense in a tight, light-resistant container.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]..
PROTECT FROM LIGHT.
USUAL DOSAGE: See package brochure.
barr NDC 50111-647-01
Fluoxetine
Capsule, USP
10 mg*
PHARMACIST: PLEASE DISPENSE WITH ATTACHED MEDICATION GUIDE
R only
N3 50111 64701 5
Control No:
Exp. Date:
Sentra PM™PRODUCT INFORMATION
Sentra PM (U.S. patent pending) capsules by oral administration. A specially formulated Medical Food product, consisting of a proprietary blend of amino acids and polyphenol ingredients in specific proportions, for the dietary management of the metabolic processes of sleep disorders (SD). Must be administered under physician supervision.
Medical Foods Medical Food products are often used in hospitals (e.g., for burn victims or kidney dialysis patients) and outside of a hospital setting under a physician’s care for the dietary management of diseases in patients with particular medical or metabolic needs due to their disease or condition. Congress defined "Medical Food" in the Orphan Drug Act and Amendments of 1988 as "a system which is formulated to be consumed or administered enterally [or orally] under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation." Medical Foods are complex formulated products, requiring sophisticated and exacting technology. Sentra PM has been developed, manufactured, and labeled in accordance with both the statutory and the FDA regulatory definition of a Medical Food. Sentra PM must be used while the patient is under the ongoing care of a physician.
SLEEP DISORDERS (SD)
SD as a Metabolic Deficiency Disease A critical component of the definition of a Medical Food is the requirement for a distinctive nutritional deficiency. FDA scientists have proposed a physiologic definition of a distinctive nutritional deficiency as follows: “the dietary management of patients with specific diseases requires, in some instances, the ability to meet nutritional requirements that differ substantially from the needs of healthy persons. For example, in establishing the recommended dietary allowances for general, healthy population, the Food and Nutrition Board of the Institute of Medicine National Academy of Sciences, recognized that different or distinctive physiologic requirements may exist for certain persons with "special nutritional needs arising from metabolic disorders, chronic diseases, injuries, premature birth, other medical conditions and drug therapies. Thus, the distinctive nutritional needs associated with a disease reflect the total amount needed by a healthy person to support life or maintain homeostasis, adjusted for the distinctive changes in the nutritional needs of the patient as a result of the effects of the disease process on absorption, metabolism, and excretion.” It was also proposed that in patients with certain disease states who respond to nutritional therapies, a physiologic deficiency of the nutrient is assumed to exist. For example, if a patient with sleep disorders responds to a tryptophan formulation by improving the duration and quality of sleep, a deficiency of tryptophan is assumed to exist.
Patients with sleep disorders are known to have nutritional deficiencies of tryptophan, choline, flavonoids, and certain antioxidants. Patients with sleep disorders frequently exhibit reduced plasma levels of tryptophan and have been shown to respond to oral administration of tryptophan or a 5-hydoxytryptophan formulation. Research has shown that tryptophan reduced diets result in a fall of circulating tryptophan. Patients with sleep disorders have activation of the tryptophan degradation pathway that increases the turnover of tryptophan leading to a reduced level of production of serotonin for a given tryptophan blood level. Research has also shown that a genetic predisposition can lead to increased tryptophan requirements in certain patients with sleep disorders.
Choline is required to fully potentiate acetylcholine synthesis by brain neurons. A deficiency of choline leads to reduced acetylcholine production by the neurons. Low fat diets, frequently used by patients with sleep disorders, are usually choline deficient. Flavonoids potentiate the production of acetylcholine by the neurons thereby inducing REM sleep. Low fat diets and diets deficient in flavonoid rich foods result in inadequate flavonoid concentrations, impeding acetylcholine production in certain patients with sleep disorders. Provision of tryptophan, choline, and flavonoids with antioxidants, in specific proportions can restore the production of beneficial serotonin and acetylcholine, thereby improving sleep quality.
PRODUCT DESCRIPTION
Primary Ingredients
Sentra PM consists of a proprietary blend of amino acids, cocoa, ginkgo biloba and flavonoids in specific proportions. These ingredients fall into the category of “Generally Regarded as Safe” (GRAS) as defined by the Food and Drug Administration (FDA) (Sections 201(s) and 409 of the Federal Food, Drug, and Cosmetic Act). A GRAS substance is distinguished from a food additive on the basis of the common knowledge about the safety of the substance for its intended use. The standard for an ingredient to achieve GRAS status requires not only technical demonstration of non-toxicity and safety, but also general recognition of safety through widespread usage and agreement of that safety by experts in the field. Many ingredients have been determined by the U.S. Food and Drug Administration (FDA) to be GRAS, and are listed as such by regulation, in Volume 21 Code of Federal Regulations (CFR) Sections 182, 184, and 186.
Amino Acids
Amino Acids are the building blocks of protein. All amino acids are GRAS listed as they have been ingested by humans for thousands of years. The doses of the amino acids in Sentra PM are equivalent to those found in the usual human diet; however the formulation uses specific ratios of the key ingredients to elicit a therapeutic response. Patients with sleep disorders may require an increased amount of certain amino acids that cannot be obtained from normal diet alone. Tryptophan, for example, is an obligatory amino acid. The body cannot make tryptophan and must obtain tryptophan from the diet. Tryptophan is needed to produce serotonin. Serotonin is required to induce sleep. Patients with sleep disorders have altered serotonin metabolism. Some patients with sleep disorders have a resistance to the use of tryptophan that is similar to the mechanism found in insulin resistance that is genetically determined. Patients with sleep disorders frequently cannot acquire sufficient tryptophan from the diet without ingesting a prohibitively large amount of calories, particularly protein rich calories.
Flavonoids
Flavonoids are a group of phytochemical compounds found in all vascular plants including fruits and vegetables. They are a part of a larger class of compounds known as polyphenols. Many of the therapeutic or health benefits of colored fruits and vegetables, cocoa, red wine, and green tea are directly related to their flavonoid content. The specially formulated flavonoids found in Sentra PM cannot be obtained from conventional foods in the necessary proportions to elicit a therapeutic response.
Other Ingredients
Sentra PM contains the following inactive or other ingredients, as fillers, excipients, and colorings: magnesium stearate, microcrystalline cellulose, Maltodextrin NF, gelatin (as the capsule material).
Physical Description
Sentra PM is a yellow to light brown powder. Sentra PM contains L-Glutamic Acid, 5-Hydroxytryptophan as Griffonia Seed Extract, Acetylcarnitine HCL, Choline Bitartrate, Cinnamon, Cocoa, Ginkgo Biloba, and Hawthorn Berry.
CLINICAL PHARMACOLOGY
Mechanism of Action
Sentra PM acts by restoring and maintaining the balance of the neurotransmitters, serotonin and acetylcholine, that are associated with sleep disorders.
Metabolism
The amino acids in Sentra PM are primarily absorbed by the stomach and small intestines. All cells metabolize the amino acids in Sentra PM. Circulating tryptophan and choline blood levels determine the production of serotonin and acetylcholine.
Excretion
Sentra PM is not an inhibitor of cytochrome P450 1A2, 2C9, 2C19, 2D6, or 3A4. These isoenzymes are principally responsible for 95% of all detoxification of drugs, with CYP3A4 being responsible for detoxification of roughly 50% of drugs. Amino acids do not appear to have an effect on drug metabolizing enzymes.
Uses
INDICATIONS FOR USE
Sentra PM is intended for the clinical dietary management of the metabolic processes associated with sleep disorders.
CLINICAL EXPERIENCE
The administration of Sentra PM has demonstrated significant functional improvement in the quality and quantity of sleep when used for the dietary management of the metabolic processes associated with sleep disorders. Administration of Sentra PM results in the induction and maintenance of sleep in patients with sleep disorders. Sentra PM has no effect on normal blood pressure.
PRECAUTIONS AND CONTRAINDICATIONS
Sentra PM is contraindicated in an extremely small number of patients with hypersensitivity to any of the nutritional components of Sentra PM.
ADVERSE REACTIONS
Oral supplementation with L-tryptophan or choline at high doses up to 15 grams daily is generally well tolerated. The most common adverse reactions of higher doses — from 15 to 30 grams daily — are nausea, abdominal cramps, and diarrhea. Some patients may experience these symptoms at lower doses. The total combined amount of amino acids in each Sentra PM capsule does not exceed 400 mg.
DRUG INTERACTIONS
Sentra PM does not directly influence the pharmacokinetics of prescription drugs. Clinical experience has shown that administration of Sentra PM may allow for lowering the dose of co-administered drugs under physician supervision.
OVERDOSE
There is a negligible risk of overdose with Sentra PM as the total dosage of amino acids in a one month supply (60 capsules) is less than 24 grams. Overdose symptoms may include diarrhea, weakness, and nausea.
POST-MARKETING SURVEILLANCE
Post-marketing surveillance has shown no serious adverse reactions. Reported cases of mild rash and itching may have been associated with allergies to Sentra PM flavonoid ingredients, including cinnamon, cocoa, and chocolate. The reactions were transient in nature and subsided within 24 hours.
DOSAGE AND ADMINISTRATION
Recommended Administration For the dietary management of the metabolic processes associated with sleep disorders. Take (2) capsules daily at bedtime. An additional dose of one or two capsules may be taken after awakenings during the night. As with most amino acid formulations Sentra PM should be taken without food to increase the absorption of key ingredients.
How Supplied
Sentra PM is supplied in red and white, size 0 capsules in bottles of 60 capsules.
Physician Supervision
Sentra PM is a Medical Food product available by prescription only and must be used while the patient is under ongoing physician supervision.
Sentra PM is supplied to physicians in a recyclable plastic bottle with a child-resistant cap.
U.S. patents pending.
Manufactured by Arizona Nutritional Supplements, Inc. Chandler AZ 85225
Distributed by Physician Therapeutics LLC, Los Angeles, CA 90077. www.ptlcentral.com
© Copyright 2003-2006, Physician Therapeutics LLC, all rights reserved
NDC # 68405-1003-02
Storage
Store at room temperature, 59-86OF (15-30OC). Protect from light and moisture.
PHYSICIAN THERAPEUTICS SENTRA PM Medical Food Rx only 60 Capsules Directions for use: Must be administered under medical supervision. For adults only. As a Medical Food, take two (2) capsules at bedtime or as directed by your medical practitioner. For the dietary management of sleep disorders. Contains no added sugar, starch, wheat, yeast, preservatives, artificial color or flavor. Storage: Keep tightly closed in a cool dry place 8-320 C (45-900F), relative humidity, below 50%. Warning: Keep this product out of the reach of children. NDC# 68405-1003-02 Ingredients: Each serving (2 capsules) contains: Proprietary Amino Acid blend Choline Bitartrate, Glutamic Acid (L-Glutamic Acid), Cocoa Extract (fruit), Proprietary Herbal Blend Ginkgo Biloba (leaves), Griffonia Seed Extract (5-HTP), Hawthorn Berry (fruit), Acetyl L-Carnitine HCl, Dextrose Other Ingredients: Gelatin, Cellulose, Dicalcium Phosphate, Silicon Dioxide and Vegetable Magnesium Stearate.
Distributed by: Physician Therapeutics LLC, Los Angeles, CA 90077 www.ptlcentral.com Patent Pending

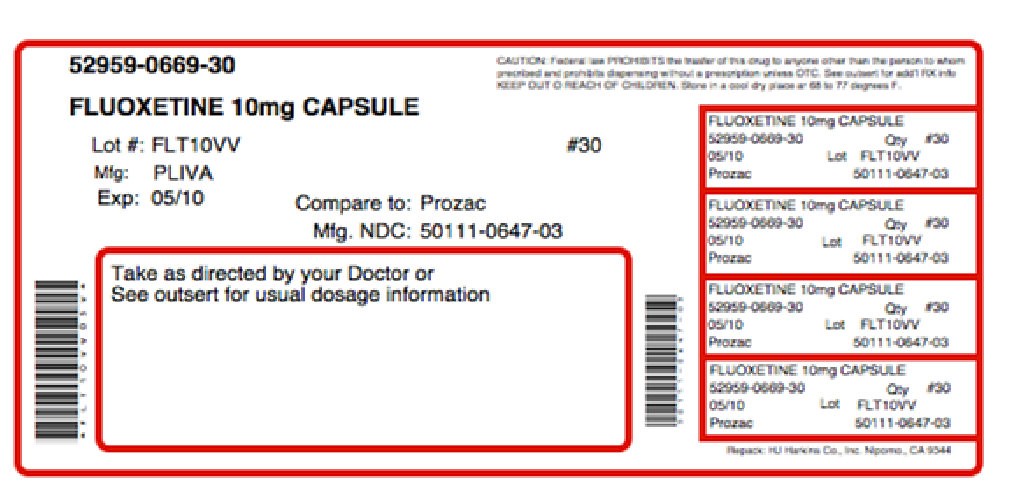
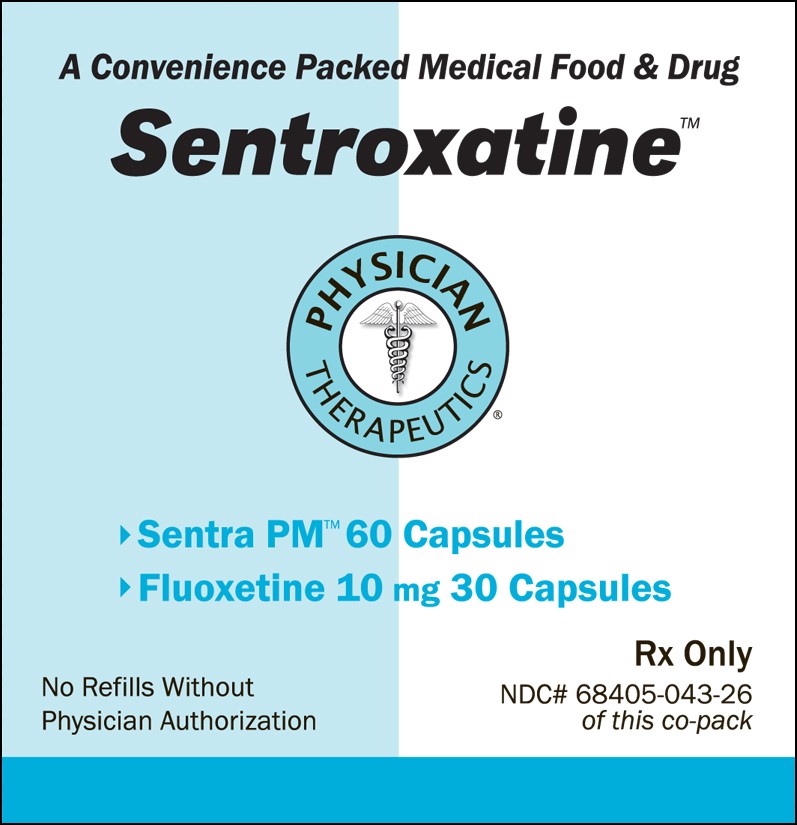
SentroxatineFLUOXETINE HYDROCHLORIDE, CHOLINE KIT
| ||||||||||||||||||||||||||||||||||||||||