Seroquel
Lake Erie Medical DBA Quality Care Products LLC
Seroquel 300 mg
FULL PRESCRIBING INFORMATION
BOXED WARNING
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks) largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. SEROQUEL (quetiapine) is not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions (5.1)].
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of SEROQUEL or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. SEROQUEL is not approved for use in patients under ten years of age [see Warnings and Precautions (5.2)].
Uses
SEROQUEL is indicated for the treatment of schizophrenia. The efficacy of SEROQUEL in schizophrenia was established in three 6-week trials in adults and one 6–week trial in adolescents (13–17 years). The effectiveness of SEROQUEL for the maintenance treatment of schizophrenia has not been systematically evaluated in controlled clinical trials [see Clinical Studies (14.1)]
SEROQUEL is indicated for the acute treatment of manic episodes associated with bipolar I disorder, both as monotherapy and as an adjunct to lithium or divalproex. Efficacy was established in two 12-week monotherapy trials in adults, in one 3-week adjunctive trial in adults, and in one 3-week monotherapy trial in pediatric patients (10-17 years) [see Clinical Studies (14.2)]
SEROQUEL is indicated as monotherapy for the acute treatment of depressive episodes associated with bipolar disorder. Efficacy was established in two 8-week monotherapy trials in adult patients with bipolar I and bipolar II disorder [see Clinical Studies (14.2)].
SEROQUEL is indicated for the maintenance treatment of bipolar I disorder, as an adjunct to lithium or divalproex. Efficacy was established in two maintenance trials in adults. The effectiveness of SEROQUEL as monotherapy for the maintenance treatment of bipolar disorder has not been systematically evaluated in controlled clinical trials [see Clinical Studies (14.2)].
Pediatric schizophrenia and bipolar I disorder are serious mental disorders, however, diagnosis can be challenging. For pediatric schizophrenia, symptom profiles can be variable, and for bipolar I disorder, patients may have variable patterns of periodicity of manic or mixed symptoms. It is recommended that medication therapy for pediatric schizophrenia and bipolar I disorder be initiated only after a thorough diagnostic evaluation has been performed and careful consideration given to the risks associated with medication treatment. Medication treatment for both pediatric schizophrenia and bipolar I disorder is indicated as part of a total treatment program that often includes psychological, educational and social interventions.
Adults
Dose Selection
Maintenance Treatment
Adolescents (13-17 years)
Dose Selection—SEROQUEL should be administered twice daily. However, based on response and tolerability SEROQUEL may be administered three times daily where needed.
The total daily dose for the initial five days of therapy is 50 mg (Day 1), 100 mg (Day 2), 200 mg (Day 3), 300 mg (Day 4) and 400 mg (Day 5). After Day 5, the dose should be adjusted within the recommended dose range of 400 mg/day to 800 mg/day based on response and tolerability. Dosage adjustments should be in increments of no greater than 100 mg/day. Efficacy was demonstrated with SEROQUEL at both 400 mg and 800 mg; however, no additional benefit was seen in the 800 mg group.
Maintenance Treatment—The effectiveness of SEROQUEL for longer than 6 weeks has not been evaluated in controlled clinical trials. While there is no body of evidence available to answer the question of how long the patient treated with SEROQUEL should be maintained, it is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
Adults
Dose Selection
Dose Selection
| Day | Day 1 | Day 2 | Day 3 | Day 4 |
|---|---|---|---|---|
|
SEROQUEL |
50 mg |
100 mg |
200 mg |
300 mg |
Maintenance Treatment of Bipolar I Disorder
see Clinical Studies
Children and Adolescents (10 to 17 years)
Acute Treatment of Manic Episodes in Bipolar I Disorder
Dose Selection—SEROQUEL should be administered twice daily. However, based on response and tolerability SEROQUEL may be administered three times daily where needed.
The total daily dose for the initial five days of therapy is 50 mg (Day 1), 100 mg (Day 2), 200 mg (Day 3), 300 mg (Day 4) and 400 mg (Day 5). After Day 5, the dose should be adjusted within the recommended dose range of 400 to 600 mg/day based on response and tolerability. Dosage adjustments should be in increments of no greater than 100 mg/day. Efficacy was demonstrated with SEROQUEL at both 400 mg and 600 mg; however, no additional benefit was seen in the 600 mg group.
Maintenance Treatment of Bipolar I Disorder
The effectiveness of SEROQUEL for longer than 3 weeks has not been evaluated in controlled clinical trials of children and adolescents. While there is no body of evidence available to answer the question of how long the patient treated with SEROQUEL should be maintained, it is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
see Clinical Pharmacology
25 mg tablets
50 mg tablets
100 mg tablets
200 mg tablets
300 mg tablets
400 mg tablets
None known
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. SEROQUEL (quetiapine fumarate) is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning ].
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated
Adults
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
The information below is derived from a clinical trial database for SEROQUEL consisting of over 4300 patients. This database includes 698 patients exposed to SEROQUEL for the treatment of bipolar depression, 405 patients exposed to SEROQUEL for the treatment of acute bipolar mania (monotherapy and adjunct therapy), 646 patients exposed to SEROQUEL for the maintenance treatment of bipolar I disorder as adjunct therapy, and approximately 2600 patients and/or normal subjects exposed to 1 or more doses of SEROQUEL for the treatment of schizophrenia.
Of these approximately 4300 subjects, approximately 4000 (2300 in schizophrenia, 405 in acute bipolar mania, 698 in bipolar depression, and 646 for the maintenance treatment of bipolar I disorder) were patients who participated in multiple dose effectiveness trials, and their experience corresponded to approximately 2400 patient-years. The conditions and duration of treatment with SEROQUEL varied greatly and included (in overlapping categories) open-label and double-blind phases of studies, inpatients and outpatients, fixed-dose and dose-titration studies, and short-term or longer-term exposure. Adverse reactions were assessed by collecting adverse events, results of physical examinations, vital signs, weights, laboratory analyses, ECGs, and results of ophthalmologic examinations.
Adverse reactions during exposure were obtained by general inquiry and recorded by clinical investigators using terminology of their own choosing. Consequently, it is not possible to provide a meaningful estimate of the proportion of individuals experiencing adverse reactions without first grouping similar types of reactions into a smaller number of standardized reaction categories.
In the tables and tabulations that follow, standard COSTART terminology has been used to classify reported adverse reactions for schizophrenia and bipolar mania. MedDRA terminology has been used to classify reported adverse reactions for bipolar depression.
The stated frequencies of adverse reactions represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction was considered treatment emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation.
Incidence of Adverse Reactions in Short-Term, Placebo-Controlled Trials in Adults
Adverse Reactions Associated with Discontinuation of Treatment in Short-Term, Placebo-Controlled Trials:
Schizophrenia: Overall, there was little difference in the incidence of discontinuation due to adverse reactions (4% for SEROQUEL vs. 3% for placebo) in a pool of controlled trials. However, discontinuations due to somnolence (0.8% SEROQUEL vs. 0% placebo) and hypotension (0.4% SEROQUEL vs. 0% placebo) were considered to be drug related [see Warnings and Precautions (5.8 and 5.16)].
Bipolar Disorder:
Mania: Overall, discontinuations due to adverse reactions were 5.7% for SEROQUEL vs. 5.1% for placebo in monotherapy and 3.6% for SEROQUEL vs. 5.9% for placebo in adjunct therapy.
Depression: Overall, discontinuations due to adverse reactions were 12.3% for SEROQUEL 300 mg vs. 19.0% for SEROQUEL 600 mg and 5.2% for placebo.
Commonly Observed Adverse Reactions in Short-Term, Placebo-Controlled Trials:
In the acute therapy of schizophrenia (up to 6 weeks) and bipolar mania (up to 12 weeks) trials, the most commonly observed adverse reactions associated with the use of SEROQUEL monotherapy (incidence of 5% or greater) and observed at a rate on SEROQUEL at least twice that of placebo were somnolence (18%), dizziness (11%), dry mouth (9%), constipation (8%), ALT increased (5%), weight gain (5%), and dyspepsia (5%).
Adverse Reactions Occurring at an Incidence of 1% or More Among SEROQUEL Treated Patients in Short-Term, Placebo-Controlled Trials:
The prescriber should be aware that the figures in the tables and tabulations cannot be used to predict the incidence of side effects in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigations involving different treatments, uses, and investigators. The cited figures, however, do provide the prescribing physician with some basis for estimating the relative contribution of drug and nondrug factors to the side effect incidence in the population studied.
The risks of using SEROQUEL in combination with other drugs have not been extensively evaluated in systematic studies. Given the primary CNS effects of SEROQUEL, caution should be used when it is taken in combination with other centrally acting drugs. SEROQUEL potentiated the cognitive and motor effects of alcohol in a clinical trial in subjects with selected psychotic disorders, and alcoholic beverages should be avoided while taking SEROQUEL.
Because of its potential for inducing hypotension, SEROQUEL may enhance the effects of certain antihypertensive agents.
SEROQUEL may antagonize the effects of levodopa and dopamine agonists.
Caution should be exercised when quetiapine is used concomitantly with drugs known to cause electrolyte imbalance or to increase QT interval [see Warnings and Precautions (5.21)].
Phenytoin: Coadministration of quetiapine (250 mg three times daily) and phenytoin (100 mg three times daily) increased the mean oral clearance of quetiapine by 5-fold. Increased doses of SEROQUEL may be required to maintain control of symptoms of schizophrenia in patients receiving quetiapine and phenytoin, or other hepatic enzyme inducers (e.g., carbamazepine, barbiturates, rifampin, glucocorticoids). Caution should be taken if phenytoin is withdrawn and replaced with a non-inducer (e.g., valproate) [see Dosage and Administration (2)].
Divalproex: Coadministration of quetiapine (150 mg twice daily) and divalproex (500 mg twice daily) increased the mean maximum plasma concentration of quetiapine at steady state by 17% without affecting the extent of absorption or mean oral clearance.
Thioridazine: Thioridazine (200 mg twice daily) increased the oral clearance of quetiapine (300 mg twice daily) by 65%.
Cimetidine: Administration of multiple daily doses of cimetidine (400 mg three times daily for 4 days) resulted in a 20% decrease in the mean oral clearance of quetiapine (150 mg three times daily). Dosage adjustment for quetiapine is not required when it is given with cimetidine.
P450 3A Inhibitors: Coadministration of ketoconazole (200 mg once daily for 4 days), a potent inhibitor of cytochrome P450 3A, reduced oral clearance of quetiapine by 84%, resulting in a 335% increase in maximum plasma concentration of quetiapine. Caution (reduced dosage) is indicated when SEROQUEL is administered with ketoconazole and other inhibitors of cytochrome P450 3A (e.g., itraconazole, fluconazole, erythromycin, and protease inhibitors).
Fluoxetine, Imipramine, Haloperidol, and Risperidone: Coadministration of fluoxetine (60 mg once daily), imipramine (75 mg twice daily), haloperidol (7.5 mg twice daily), or risperidone (3 mg twice daily) with quetiapine (300 mg twice daily) did not alter the steady-state pharmacokinetics of quetiapine.
Lorazepam: The mean oral clearance of lorazepam (2 mg, single dose) was reduced by 20% in the presence of quetiapine administered as 250 mg three times daily dosing.
Divalproex: The mean maximum concentration and extent of absorption of total and free valproic acid at steady state were decreased by 10 to 12% when divalproex (500 mg twice daily) was administered with quetiapine (150 mg twice daily). The mean oral clearance of total valproic acid (administered as divalproex 500 mg twice daily) was increased by 11% in the presence of quetiapine (150 mg twice daily). The changes were not significant.
Lithium: Concomitant administration of quetiapine (250 mg three times daily) with lithium had no effect on any of the steady-state pharmacokinetic parameters of lithium.
Antipyrine: Administration of multiple daily doses up to 750 mg/day (on a three times daily schedule) of quetiapine to subjects with selected psychotic disorders had no clinically relevant effect on the clearance of antipyrine or urinary recovery of antipyrine metabolites. These results indicate that quetiapine does not significantly induce hepatic enzymes responsible for cytochrome P450 mediated metabolism of antipyrine.
8 USE IN SPECIFIC POPULATIONS
Pregnancy Category C:
22222222
SEROQUEL was excreted in milk of treated animals during lactation. It is not known if SEROQUEL is excreted in human milk. It is recommended that women receiving SEROQUEL should not breast feed.
In general, the adverse reactions observed in children and adolescents during the clinical trials were similar to those in the adult population with few exceptions. Increases in systolic and diastolic blood pressure occurred in children and adolescents and did not occur in adults. Orthostatic hypotension occurred more frequently in adults (4-7%) compared to children and adolescents
SchizophreniaThe efficacy and safety of SEROQUEL in the treatment of schizophrenia in adolescents aged 13 to 17 years were demonstrated in one 6–week, double-blind, placebo-controlled trial [see Indications and Usage (1.1), Dosage and Administration (2.1), Adverse Reactions (6.1), and Clinical Studies (14.1)].
Safety and effectiveness of SEROQUEL in pediatric patients less than 13 years of age with schizophrenia have not been established.
Maintenance
The safety and effectiveness of SEROQUEL in the maintenance treatment of bipolar disorder has not been established in pediatric patients less than 18 years of age. The safety and effectiveness of SEROQUEL in the maintenance treatment of schizophrenia has not been established in any patient population, including pediatric patients.
Bipolar Mania
The efficacy and safety of SEROQUEL in the treatment of mania in children and adolescents ages 10 to 17 years with Bipolar I disorder was demonstrated in a 3-week, double-blind, placebo controlled, multicenter trial [see Indications and Usage (1.2), Dosage and Administration (2.2), Adverse Reactions (6.1), and Clinical Studies (14.2)].
Safety and effectiveness of SEROQUEL in pediatric patients less than 10 years of age with bipolar mania have not been established.
Bipolar Depression
Safety and effectiveness of SEROQUEL in pediatric patients less than 18 years of age with bipolar depression have not been established.
Some differences in the pharmacokinetics of quetiapine were noted between children/adolescents (10 to 17 years of age) and adults. When adjusted for weight, the AUC and Cmax of quetiapine were 41% and 39% lower, respectively, in children and adolescents compared to adults. The pharmacokinetics of the active metabolite, norquetiapine, were similar between children/adolescents and adults after adjusting for weight [see Clinical Pharmacology (12.3)].
Of the approximately 3700 patients in clinical studies with SEROQUEL, 7% (232) were 65 years of age or over. In general, there was no indication of any different tolerability of SEROQUEL in the elderly compared to younger adults. Nevertheless, the presence of factors that might decrease pharmacokinetic clearance, increase the pharmacodynamic response to SEROQUEL, or cause poorer tolerance or orthostasis, should lead to consideration of a lower starting dose, slower titration, and careful monitoring during the initial dosing period in the elderly. The mean plasma clearance of SEROQUEL was reduced by 30% to 50% in elderly patients when compared to younger patients [see Clinical Pharmacology (12) and Dosage and Administration (2)].
SEROQUEL is not a controlled substance.
SEROQUEL has not been systematically studied, in animals or humans, for its potential for abuse, tolerance or physical dependence. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of misuse or abuse of SEROQUEL, e.g., development of tolerance, increases in dose, drug-seeking behavior.
10 OVERDOSAGE
In clinical trials, survival has been reported in acute overdoses of up to 30 grams of quetiapine. Most patients who overdosed experienced no adverse reactions or recovered fully from the reported reactions. Death has been reported in a clinical trial following an overdose of 13.6 grams of quetiapine alone. In general, reported signs and symptoms were those resulting from an exaggeration of the drugs known pharmacological effects, ie, drowsiness and sedation, tachycardia and hypotension. Patients with pre-existing severe cardiovascular disease may be at an increased risk of the effects of overdose [see Warnings and Precautions (5)]. One case, involving an estimated overdose of 9600 mg, was associated with hypokalemia and first degree heart block. In post-marketing experience, there were cases reported of QT prolongation with overdose. There were also very rare reports of overdose of SEROQUEL alone resulting in death or coma.
In case of acute overdosage, establish and maintain an airway and ensure adequate oxygenation and ventilation. Gastric lavage (after intubation, if patient is unconscious) and administration of activated charcoal together with a laxative should be considered. The possibility of obtundation, seizure or dystonic reaction of the head and neck following overdose may create a risk of aspiration with induced emesis. Cardiovascular monitoring should commence immediately and should include continuous electrocardiographic monitoring to detect possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide and quinidine carry a theoretical hazard of additive QT-prolonging effects when administered in patients with acute overdosage of SEROQUEL. Similarly it is reasonable to expect that the alpha-adrenergic-blocking properties of bretylium might be additive to those of quetiapine, resulting in problematic hypotension.
There is no specific antidote to SEROQUEL. Therefore, appropriate supportive measures should be instituted. The possibility of multiple drug involvement should be considered. Hypotension and circulatory collapse should be treated with appropriate measures such as intravenous fluids and/or sympathomimetic agents (epinephrine and dopamine should not be used, since beta stimulation may worsen hypotension in the setting of quetiapine-induced alpha blockade). In cases of severe extrapyramidal symptoms, anticholinergic medication should be administered. Close medical supervision and monitoring should continue until the patient recovers.
®b,f4250642444
Quetiapine fumarate is a white to off-white crystalline powder which is moderately soluble in water.
SEROQUEL is supplied for oral administration as 25 mg (round, peach), 50 mg (round, white), 100 mg (round, yellow), 200 mg (round, white), 300 mg (capsule-shaped, white), and 400 mg (capsule-shaped, yellow) tablets.
Inactive ingredients are povidone, dibasic dicalcium phosphate dihydrate, microcrystalline cellulose, sodium starch glycolate, lactose monohydrate, magnesium stearate, hypromellose, polyethylene glycol and titanium dioxide.
The 25 mg tablets contain red ferric oxide and yellow ferric oxide and the 100 mg and 400 mg tablets contain only yellow ferric oxide.
The mechanism of action of SEROQUEL, as with other drugs having efficacy in the treatment of schizophrenia and bipolar disorder, is unknown. However, it has been proposed that the efficacy of SEROQUEL in schizophrenia and its mood stabilizing properties in bipolar depression and mania are mediated through a combination of dopamine type 2 (D2) and serotonin type 2 (5HT2) antagonism. Antagonism at receptors other than dopamine and 5HT2 with similar receptor affinities may explain some of the other effects of SEROQUEL.
SEROQUEL’s antagonism of histamine H1 receptors may explain the somnolence observed with this drug.
SEROQUEL’s antagonism of adrenergic α1 receptors may explain the orthostatic hypotension observed with this dr
Carcinogenesis
22222
Thyroid follicular cell adenomas may have resulted from chronic stimulation of the thyroid gland by thyroid stimulating hormone (TSH) resulting from enhanced metabolism and clearance of thyroxine by rodent liver. Changes in TSH, thyroxine, and thyroxine clearance consistent with this mechanism were observed in subchronic toxicity studies in rat and mouse and in a 1-year toxicity study in rat; however, the results of these studies were not definitive. The relevance of the increases in thyroid follicular cell adenomas to human risk, through whatever mechanism, is unknown.
Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum measurements in a 1-year toxicity study showed that quetiapine increased median serum prolactin levels a maximum of 32- and 13-fold in male and female rats, respectively. Increases in mammary neoplasms have been found in rodents after chronic administration of other antipsychotic drugs and are considered to be prolactin-mediated. The relevance of this increased incidence of prolactin-mediated mammary gland tumors in rats to human risk is unknown [see Warnings and Precautions (5.14)].
Mutagenesis
The mutagenic potential of quetiapine was tested in six in vitro bacterial gene mutation assays and in an in vitro mammalian gene mutation assay in Chinese Hamster Ovary cells. However, sufficiently high concentrations of quetiapine may not have been used for all tester strains. Quetiapine did produce a reproducible increase in mutations in one Salmonella typhimurium tester strain in the presence of metabolic activation. No evidence of clastogenic potential was obtained in an in vitro chromosomal aberration assay in cultured human lymphocytes or in the in vivo micronucleus assay in rats.
Impairment of Fertility
Quetiapine decreased mating and fertility in male Sprague-Dawley rats at oral doses of 50 and 150 mg/kg or 0.6 and 1.8 times the maximum human dose on a mg/m2 basis. Drug-related effects included increases in interval to mate and in the number of matings required for successful impregnation. These effects continued to be observed at 150 mg/kg even after a two-week period without treatment. The no-effect dose for impaired mating and fertility in male rats was 25 mg/kg, or 0.3 times the maximum human dose on a mg/m2 basis. Quetiapine adversely affected mating and fertility in female Sprague-Dawley rats at an oral dose of 50 mg/kg, or 0.6 times the maximum human dose on a mg/m2 basis. Drug-related effects included decreases in matings and in matings resulting in pregnancy, and an increase in the interval to mate. An increase in irregular estrus cycles was observed at doses of 10 and 50 mg/kg, or 0.1 and 0.6 times the maximum human dose on a mg/m2 basis. The no-effect dose in female rats was 1 mg/kg, or 0.01 times the maximum human dose on a mg/m2 basis.
Quetiapine caused a dose-related increase in pigment deposition in thyroid gland in rat toxicity studies which were 4 weeks in duration or longer and in a mouse 2–year carcinogenicity study. Doses were 10-250 mg/kg in rats, 75-750 mg/kg in mice; these doses are 0.1-3.0, and 0.1-4.5 times the maximum recommended human dose (on a mg/m2 basis), respectively. Pigment deposition was shown to be irreversible in rats. The identity of the pigment could not be determined, but was found to be co-localized with quetiapine in thyroid gland follicular epithelial cells. The functional effects and the relevance of this finding to human risk are unknown.
In dogs receiving quetiapine for 6 or 12 months, but not for 1 month, focal triangular cataracts occurred at the junction of posterior sutures in the outer cortex of the lens at a dose of 100 mg/kg, or 4 times the maximum recommended human dose on a mg/m2 basis. This finding may be due to inhibition of cholesterol biosynthesis by quetiapine. Quetiapine caused a dose-related reduction in plasma cholesterol levels in repeat-dose dog and monkey studies; however, there was no correlation between plasma cholesterol and the presence of cataracts in individual dogs. The appearance of delta–8–cholestanol in plasma is consistent with inhibition of a late stage in cholesterol biosynthesis in these species. There also was a 25% reduction in cholesterol content of the outer cortex of the lens observed in a special study in quetiapine treated female dogs. Drug-related cataracts have not been seen in any other species; however, in a 1-year study in monkeys, a striated appearance of the anterior lens surface was detected in 2/7 females at a dose of 225 mg/kg or 5.5 times the maximum recommended human dose on a mg/m2 basis.
Adults
The efficacy of SEROQUEL in the treatment of schizophrenia was established in 3 short-term (6-week) controlled trials of inpatients with schizophrenia who met DSM III-R criteria for schizophrenia. Although a single fixed dose haloperidol arm was included as a comparative treatment in one of the three trials, this single haloperidol dose group was inadequate to provide a reliable and valid comparison of SEROQUEL and haloperidol.
Several instruments were used for assessing psychiatric signs and symptoms in these studies, among them the Brief Psychiatric Rating Scale (BPRS), a multi-item inventory of general psychopathology traditionally used to evaluate the effects of drug treatment in schizophrenia. The BPRS psychosis cluster (conceptual disorganization, hallucinatory behavior, suspiciousness, and unusual thought content) is considered a particularly useful subset for assessing actively psychotic schizophrenic patients. A second traditional assessment, the Clinical Global Impression (CGI), reflects the impression of a skilled observer, fully familiar with the manifestations of schizophrenia, about the overall clinical state of the patient.
-
In a 6-week, placebo-controlled trial (n=361) involving 5 fixed doses of SEROQUEL (75 mg/day, 150 mg/day, 300 mg/day, 600 mg/day and 750 mg/day given in divided doses three times per day), the 4 highest doses of SEROQUEL were generally superior to placebo on the BPRS total score, the BPRS psychosis cluster and the CGI severity score, with the maximal effect seen at 300 mg/day, and the effects of doses of 150 mg/day to 750 mg/day were generally indistinguishable.
-
In a 6-week, placebo-controlled trial (n=286) involving titration of SEROQUEL in high (up to 750 mg/day given in divided doses three times per day) and low (up to 250 mg/day given in divided doses three times per day) doses, only the high dose SEROQUEL group (mean dose, 500 mg/day) was superior to placebo on the BPRS total score, the BPRS psychosis cluster, and the CGI severity score.
-
In a 6-week dose and dose regimen comparison trial (n=618) involving two fixed doses of SEROQUEL (450 mg/day given in divided doses both twice daily and three times daily and 50 mg/day given in divided doses twice daily), only the 450 mg/day (225 mg twice daily) dose group was superior to the 50 mg/day (25 mg given twice daily) SEROQUEL dose group on the BPRS total score, the BPRS psychosis cluster, and the CGI severity score.
Adolescents (ages 13-17)
The efficacy of SEROQUEL in the treatment of schizophrenia in adolescents (13–17 years of age) was demonstrated in a 6–week, double-blind, placebo-controlled trial. Patients who met DSM-IV diagnostic criteria for schizophrenia were randomized into one of three treatment groups: SEROQUEL 400 mg/day (n = 73), SEROQUEL 800 mg/day (n = 74), or placebo (n = 75). Study medication was initiated at 50 mg/day and on day 2 increased to 100 mg/per day (divided and given two or three times per day). Subsequently, the dose was titrated to the target dose of 400 mg/day or 800 mg/day using increments of 100 mg/day, divided and given two or three times daily. The primary efficacy variable was the mean change from baseline in total Positive and Negative Syndrome Scale (PANSS).
SEROQUEL at 400 mg/day and 800 mg/day was superior to placebo in the reduction of PANSS total score.
Manic Episodes
Adults
The efficacy of SEROQUEL in the acute treatment of manic episodes was established in 3 placebo-controlled trials in patients who met DSM-IV criteria for bipolar I disorder with manic episodes. These trials included patients with or without psychotic features and excluded patients with rapid cycling and mixed episodes. Of these trials, 2 were monotherapy (12 weeks) and 1 was adjunct therapy (3 weeks) to either lithium or divalproex. Key outcomes in these trials were change from baseline in the Young Mania Rating Scale (YMRS) score at 3 and 12 weeks for monotherapy and at 3 weeks for adjunct therapy. Adjunct therapy is defined as the simultaneous initiation or subsequent administration of SEROQUEL with lithium or divalproex.
The primary rating instrument used for assessing manic symptoms in these
trials was YMRS, an 11-item clinician-rated scale traditionally used to assess
the degree of manic symptomatology (irritability, disruptive/aggressive
behavior, sleep, elevated mood, speech, increased activity, sexual interest,
language/thought disorder, thought content, appearance, and insight) in a range
from 0 (no manic features) to 60 (maximum score).
Monotherapy
The efficacy of SEROQUEL in the acute treatment of bipolar mania was established in 2 placebo-controlled trials. In two 12-week trials (n=300, n=299) comparing SEROQUEL to placebo, SEROQUEL was superior to placebo in the reduction of the YMRS total score at weeks 3 and 12. The majority of patients in these trials taking SEROQUEL were dosed in a range between 400 mg/day and 800 mg per day.
Adjunct Therapy
In this 3-week placebo-controlled trial, 170 patients with bipolar mania (YMRS > 20) were randomized to receive SEROQUEL or placebo as adjunct treatment to lithium or divalproex. Patients may or may not have received an adequate treatment course of lithium or divalproex prior to randomization. SEROQUEL was superior to placebo when added to lithium or divalproex alone in the reduction of YMRS total score.
The majority of patients in this trial taking SEROQUEL were dosed in a range
between 400 mg/day and 800 mg per day. In a similarly designed trial (n=200),
SEROQUEL was associated with an improvement in YMRS scores but did not
demonstrate superiority to placebo, possibly due to a higher placebo effect.
Children and Adolescents (ages 10-17)
The efficacy of SEROQUEL in the acute treatment of manic episodes associated with bipolar I disorder in children and adolescents (10 to 17 years of age) was demonstrated in a 3-week, double-blind, placebo-controlled, multicenter trial. Patients who met DSM-IV diagnostic criteria for a manic episode were randomized into one of three treatment groups: SEROQUEL 400 mg/day (n = 95), SEROQUEL 600 mg/day (n = 98), or placebo (n = 91). Study medication was initiated at 50 mg/day and on day 2 increased to 100 mg/day (divided doses given two or three times daily). Subsequently, the dose was titrated to a target dose of 400 mg/day or 600 mg/day using increments of 100 mg/day, given in divided doses two or three times daily. The primary efficacy variable was the mean change from baseline in total YMRS score.
SEROQUEL 400 mg/day and 600 mg/day were superior to placebo in the reduction
of YMRS total score.
Depressive Episodes
Adults
The efficacy of SEROQUEL for the acute treatment of depressive episodes associated with bipolar disorder was established in 2 identically designed 8-week, randomized, double-blind, placebo-controlled studies (N=1045). These studies included patients with either bipolar I or II disorder and those with or without a rapid cycling course. Patients randomized to SEROQUEL were administered fixed doses of either 300 mg or 600 mg once daily.
The primary rating instrument used to assess depressive symptoms in these studies was the Montgomery-Asberg Depression Rating Scale (MADRS), a 10–item clinician-rated scale with scores ranging from 0 to 60. The primary endpoint in both studies was the change from baseline in MADRS score at week 8. In both studies, SEROQUEL was superior to placebo in reduction of MADRS score. Improvement in symptoms, as measured by change in MADRS score relative to placebo, was seen in both studies at Day 8 (week 1) and onwards. In these studies, no additional benefit was seen with the 600 mg dose. For the 300 mg dose group, statistically significant improvements over placebo were seen in overall quality of life and satisfaction related to various areas of functioning, as measured using the Q-LES-Q(SF).
Maintenance Treatment as an Adjunct to Lithium or Divalproex
The efficacy of SEROQUEL in the maintenance treatment of bipolar I disorder was established in 2 placebo-controlled trials in patients (n=1326) who met DSM-IV criteria for bipolar I disorder. The trials included patients whose most recent episode was manic, depressed, or mixed, with or without psychotic features. In the open-label phase, patients were required to be stable on SEROQUEL plus lithium or divalproex for at least 12 weeks in order to be randomized. On average, patients were stabilized for 15 weeks. In the randomization phase, patients continued treatment with lithium or divalproex and were randomized to receive either SEROQUEL (administered twice daily totaling 400 mg/day to 800 mg/day) or placebo. Approximately 50% of the patients had discontinued from the SEROQUEL group by day 280 and 50% of the placebo group had discontinued by day 117 of double-blind treatment. The primary endpoint in these studies was time to recurrence of a mood event (manic, mixed or depressed episode). A mood event was defined as medication initiation or hospitalization for a mood episode; YMRS score ≥ 20 or MADRS score ≥ 20 at 2 consecutive assessments; or study discontinuation due to a mood event.
In both studies, SEROQUEL was superior to placebo in increasing the time to
recurrence of any mood event. The treatment effect was present for increasing
time to recurrence of both manic and depressed episodes. The effect of SEROQUEL
was independent of any specific subgroup (assigned mood stabilizer, sex, age,
race, most recent bipolar episode, or rapid cycling course).
16 HOW SUPPLIED/STORAGE AND HANDLING
25 mg Tablets (NDC 0310-0275) peach, round, biconvex, film coated tablets, identified with 'SEROQUEL' and ‘25’ on one side and plain on the other side, are supplied in bottles of 100 tablets and 1000 tablets, and hospital unit dose packages of 100 tablets.
50 mg Tablets (NDC 0310-0278) white, round, biconvex, film coated tablets, identified with 'SEROQUEL' and ‘50’ on one side and plain on the other side, are supplied in bottles of 100 tablets and 1000 tablets, and hospital unit dose packages of 100 tablets.
100 mg Tablets (NDC 0310-0271) yellow, round, biconvex film coated tablets, identified with 'SEROQUEL' and ‘100’ on one side and plain on the other side, are supplied in bottles of 100 tablets, and hospital unit dose packages of 100 tablets.
200 mg Tablets (NDC 0310-0272) white, round, biconvex, film coated tablets, identified with ‘SEROQUEL’ and ‘200’ on one side and plain on the other side, are supplied in bottles of 100 tablets, and hospital unit dose packages of 100 tablets.
300 mg Tablets (NDC 0310-0274) white, capsule-shaped, biconvex, film coated tablets, intagliated with ‘SEROQUEL’ on one side and ‘300’ on the other side, are supplied in bottles of 60 tablets, and hospital unit dose packages of 100 tablets.
400 mg Tablets (NDC 0310-0279) yellow, capsule-shaped, biconvex, film coated tablets, intagliated with ‘SEROQUEL’ on one side and ‘400’ on the other side, are supplied in bottles of 100 tablets, and hospital unit dose packages of 100 tablets.
Store at 25ºC (77ºF); excursions permitted to 15-30ºC (59-86ºF) [See USP].
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with SEROQUEL and should counsel them in its appropriate use. A patient Medication Guide about “Antidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions” is available for SEROQUEL. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking SEROQUEL.
Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Patients and caregivers should be advised that elderly patients with dementia-related psychosis treated with atypical antipsychotic drugs are at increased risk of death compared with placebo. Quetiapine is not approved for elderly patients with dementia-related psychosis [seeWarnings and Precautions (5.1)].
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication [see Warnings and Precautions (5.2)].
Neuroleptic Malignant Syndrome (NMS)
Patients should be advised to report to their physician any signs or symptoms that may be related to NMS. These may include muscle stiffness and high fever [see Warnings and Precautions (5.3)].
Hyperglycemia and Diabetes Mellitus
Patients should be aware of the symptoms of hyperglycemia (high blood sugar) and diabetes mellitus. Patients who are diagnosed with diabetes, those with risk factors for diabetes, or those that develop these symptoms during treatment should have their blood glucose monitored at the beginning of and periodically during treatment [see Warnings and Precautions (5.4)].
Hyperlipidemia
Patients should be advised that elevations in total cholesterol, LDL
cholesterol and triglycerides and decreases in HDL-cholesterol may occur.
Patients should have their lipid profile monitored at the beginning of and
periodically during treatment [see Warnings and Precautions
(5.5)].
Weight Gain
Patients should be advised that they may experience weight gain. Patients should have their weight monitored regularly [see Warnings and Precautions (5.6)].
Orthostatic Hypotension
Patients should be advised of the risk of orthostatic hypotension (symptoms include feeling dizzy or lightheaded upon standing, which may lead to falls), especially during the period of initial dose titration, and also at times of re-initiating treatment or increases in dose [see Warnings and Precautions (5.8)].
Increased Blood Pressure in Children and Adolescents
Blood pressure should be measured at the beginning of, and periodically during, treatment [see Warnings and Precautions (5.9)].
Leukopenia/Neutropenia
Patients with a pre-existing low WBC or a history of drug induced leukopenia/neutropenia should be advised that they should have their CBC monitored while taking SEROQUEL [see Warnings and Precautions (5.10)].
Interference with Cognitive and Motor Performance
Patients should be advised of the risk of somnolence or sedation (which may
lead to falls), especially during the period of initial dose titration. Patients
should be cautioned about performing any activity requiring mental alertness,
such as operating a motor vehicle (including automobiles) or operating
machinery, until they are reasonably certain quetiapine therapy does
Heat Exposure and Dehydration
Patients should be advised regarding appropriate care in avoiding overheating and dehydration [see Warnings and Precautions (5.18)].
Concomitant Medication
As with other medications, patients should be advised to notify their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs [see Warnings and Precautions (5.21)].
Pregnancy and Nursing
Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy. Patients should be advised not to breast feed if they are taking quetiapine [see Use in Specific Populations (8.1) and (8.3)].
Need for Comprehensive Treatment Program
SEROQUEL is indicated as an integral part of a total treatment program for adolescents with schizophrenia and pediatric bipolar disorder that may include other measures (psychological, educational, and social). Effectiveness and safety of SEROQUEL have not been established in pediatric patients less than 13 years of age for schizophrenia or less than 10 years of age for bipolar mania. Appropriate educational placement is essential and psychosocial intervention is often helpful. The decision to prescribe atypical antipsychotic medication will depend upon the physician’s assessment of the chronicity and severity of the patient’s symptoms.
Medication Guide
SEROQUEL XR (SER-oh-kwell)
quetiapine fumarate
Read this Medication Guide before you start taking SEROQUEL XR and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about SEROQUEL XR?
Serious side effects may happen when you take SEROQUEL XR, including:
-
Risk of death in the elderly with dementia: Medicines like SEROQUEL XR can raise the risk of death in elderly people who have lost touch with reality due to confusion and memory loss (dementia). SEROQUEL XR is not approved for treating psychosis in the elderly with dementia.
-
Risk of suicidal thoughts or actions: Antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions:
-
Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment.
-
Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) depression, bipolar illness (also called manic-depressive illness), or suicidal thoughts or actions.
-
How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
-
Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed.
-
Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
-
Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
-
thoughts about suicide or dying
-
attempts to commit suicide
-
new or worse depression
-
new or worse anxiety
-
feeling very agitated or restless
-
panic attacks
-
trouble sleeping (insomnia)
-
new or worse irritability
-
acting aggressive, being angry, or violent
-
acting on dangerous impulses
-
an extreme increase in activity and talking (mania)
-
other unusual changes in behavior or mood
What else do I need to know about antidepressant medicines?
-
Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms.
-
Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.
-
Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.
-
Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member take. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.
-
Not all antidepressant medicines prescribed for children are FDA approved for use in children. Talk to your child’s healthcare provider for more information.
What is SEROQUEL XR?
-
SEROQUEL XR is a prescription medicine used to treat schizophrenia in adults.
-
SEROQUEL XR is a prescription medicine used to treat bipolar disorder in adults, including:
-
manic episodes associated with bipolar disorder alone or with lithium or divalproex.
-
depressive episodes associated with bipolar disorder.
-
long-term treatment of bipolar I disorder with lithium or divalproex.
-
-
SEROQUEL XR is a prescription medicine used to treat major depressive disorder as add-on treatment with antidepressant medicines when your doctor determines that one antidepressant alone is not enough to treat your depression.
SEROQUEL XR is not approved for patients under 18 years of age.
What should I tell my healthcare provider before taking SEROQUEL XR?
Before taking SEROQUEL XR, tell your healthcare provider if you have or have had:
-
diabetes or high blood sugar in you or your family: your healthcare provider should check your blood sugar before you start SEROQUEL XR and also during therapy.
-
high levels of total cholesterol, triglycerides or LDL-cholesterol or low levels of HDL- cholesterol
-
low or high blood pressure
-
low white blood cell count
-
cataracts
-
seizures
-
abnormal thyroid tests
-
high prolactin levels
-
heart problems
-
liver problems
-
any other medical condition
-
pregnancy or plans to become pregnant. It is not known if SEROQUEL XR will harm your unborn baby.
-
breast-feeding or plans to breast-feed. It is not known if SEROQUEL XR will pass into your breast milk. You and your healthcare provider should decide if you will take SEROQUEL XR or breast-feed. You should not do both.
Tell the healthcare provider about all the medicines that you take or recently have taken including prescription medicines, non-prescription medicines, herbal supplements and vitamins.
SEROQUEL XR and other medicines may affect each other causing serious side effects. SEROQUEL XR may affect the way other medicines work, and other medicines may affect how SEROQUEL XR works.
Especially tell your healthcare provider if you take or plan to take medicines for:
-
depression
-
high blood pressure
-
Parkinson's disease
-
trouble sleeping
Also tell your healthcare provider if you take or plan to take any of these medicines:
-
phenytoin, divalproex or carbamazepine (for epilepsy)
-
barbiturates (to help you sleep)
-
rifampin (for tuberculosis)
-
glucocorticoids (steroids for inflammation)
-
thioridazine (an antipsychotic)
-
ketoconazole, fluconazole or itraconazole (for fungal infections)
-
erythromycin (an antibiotic)
-
protease inhibitors (for HIV)
This is not a complete list of medicines that can affect or be affected by SEROQUEL XR. Your doctor can tell you if it is safe to take SEROQUEL XR with your other medicines. Do not start or stop any medicines while taking SEROQUEL XR without talking to your healthcare provider first. Know the medicines you take. Keep a list of your medicines to show your healthcare provider and pharmacist when you get a new medicine.
Tell your healthcare provider if you are having a urine drug screen because SEROQUEL XR may affect your test results. Tell those giving the test that you are taking SEROQUEL XR.
How should I take SEROQUEL XR?
-
Take SEROQUEL XR exactly as your healthcare provider tells you to take it. Do not change the dose yourself.
-
Take SEROQUEL XR by mouth, with a light meal or without food.
-
SEROQUEL XR should be swallowed whole and not split, chewed or crushed.
-
If you feel you need to stop SEROQUEL XR, talk with your healthcare provider first.
If you suddenly stop taking SEROQUEL XR, you may experience side effects such as trouble sleeping or trouble staying asleep (insomnia), nausea, and vomiting.
-
If you miss a dose, take it as soon as you remember. If it is close to the next dose, skip the missed dose. Just take the next dose at your regular time. Do not take 2 doses at the same time unless your healthcare provider tells you to. If you are not sure about your dosing, call your healthcare provider.
-
If you take too much SEROQUEL XR, call your healthcare provider or poison control center at 1-800-222-1222 right away or go to the nearest hospital emergency room.
What should I avoid while taking SEROQUEL XR?
Do not drive, operate machinery, or do other dangerous activities until you know how SEROQUEL XR affects you. SEROQUEL XR may make you drowsy.
-
Avoid getting over-heated or dehydrated.
-
Do not over-exercise.
-
In hot weather, stay inside in a cool place if possible.
-
Stay out of the sun. Do not wear too much or heavy clothing.
-
Drink plenty of water.
-
-
Do not drink alcohol while taking SEROQUEL XR. It may make some side effects of SEROQUEL XR worse.
What are possible side effects of SEROQUEL XR?
Serious side effects have been reported with SEROQUEL XR including:
Also see “What is the most important information I should know about SEROQUEL XR?” at the beginning of this Medication Guide
-
Neuroleptic malignant syndrome (NMS): Tell your healthcare provider right away if you have some or all of the following symptoms: high fever, stiff muscles, confusion, sweating, changes in pulse, heart rate, and blood pressure. These may be symptoms of a rare and serious condition that can lead to death. Stop SEROQUEL XR and call your healthcare provider right away.
-
High blood sugar (hyperglycemia): Increases in blood sugar can happen in some people who take SEROQUEL XR. Extremely high blood sugar can lead to coma or death. If you have diabetes or risk factors for diabetes (such as being overweight or a family history of diabetes) your healthcare provider should check your blood sugar before you start SEROQUEL XR and during therapy.
Call your healthcare provider if you have any of these symptoms of high blood sugar while taking SEROQUEL XR:
-
feel very thirsty
-
need to urinate more than usual
-
feel very hungry
-
feel weak or tired
-
feel sick to your stomach
-
feel confused, or your breath smells fruity.
-
-
High cholesterol and triglyceride levels in the blood (fat in the blood) Increases in total cholesterol, triglycerides and LDL (bad) cholesterol and decreases in HDL (good) cholesterol have been reported in clinical trials with SEROQUEL XR. You may not have any symptoms, so your healthcare provider should do blood tests to check your cholesterol and triglyceride levels before you start taking SEROQUEL XR and during therapy.
-
Increase in weight (weight gain): Weight gain has been seen in patients who take SEROQUEL XR so you and your healthcare provider should check your weight regularly.
-
Tardive dyskinesia: Tell your healthcare provider about any movements you cannot control in your face, tongue, or other body parts. These may be signs of a serious condition. Tardive dyskinesia may not go away, even if you stop taking SEROQUEL XR. Tardive dyskinesia may also start after you stop taking SEROQUEL XR.
-
Orthostatic hypotension (decreased blood pressure): lightheadedness or fainting caused by a sudden change in heart rate and blood pressure when rising too quickly from a sitting or lying position.
-
Increases in blood pressure: reported in children and teenagers. Your healthcare provider should check blood pressure in children and adolescents before starting SEROQUEL XR and during therapy. SEROQUEL XR is not approved for patients under 18 years of age.
-
Low white blood cell count
-
Cataracts
-
Seizures
-
Abnormal thyroid tests: Your healthcare provider may do blood tests to check your thyroid hormone level.
-
Increases in prolactin levels: Your healthcare provider may do blood tests to check your prolactin levels.
-
Increases in liver enzymes: Your healthcare provider may do blood tests to check your liver enzyme levels.
-
Long lasting and painful erection
-
Difficulty swallowing
Common possible side effects with SEROQUEL XR include:
-
drowsiness
-
dry mouth
-
constipation
-
dizziness
-
increased appetite
-
upset stomach
-
weight gain
-
fatigue
-
disturbance in speech and language
-
stuffy nose
These are not all the possible side effects of SEROQUEL XR. For more information, ask your healthcare provider or pharmacist.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store SEROQUEL XR?
-
Store SEROQUEL XR at room temperature, between 59°F to 86°F (15°C to 30°C).
-
Keep SEROQUEL XR and all medicines out of the reach of children.
General information about SEROQUEL XR
Do not take SEROQUEL XR unless your healthcare provider has prescribed it for you for your condition. Do not share SEROQUEL XR with other people, even if they have the same condition. It may harm them.
This Medication Guide provides a summary of important information about SEROQUEL XR. For more information about SEROQUEL XR, talk with your healthcare provider or pharmacist or call 1-800-236-9933. You can ask your healthcare provider for information about SEROQUEL XR that is written for health professionals.
What are the ingredients in SEROQUEL XR?
Active ingredient: quetiapine fumarate
Inactive ingredients: lactose monohydrate, microcrystalline cellulose, sodium citrate, hypromellose, and magnesium stearate. The film coating for all SEROQUEL XR tablets contain hypromellose, polyethylene glycol 400 and titanium dioxide. In addition, yellow iron oxide (50, 200 and 300 mg tablets) and red iron oxide (50 mg tablets) are included in the film coating of specific strengths.
The symptoms of Schizophrenia include:
-
Having lost touch with reality (psychosis),
-
Seeing things that are not there or hearing voices (hallucinations),
-
Believing things that are not true (delusions) and
-
Being suspicious (paranoia).
The symptoms of Bipolar Disorder include:
-
General symptoms of bipolar disorder include: extreme mood swings, along with other specific symptoms and behaviors. These mood swings, or "episodes," include manic (highs) and depressive (lows)
-
Common symptoms of a manic episode include feeling extremely happy, being very irritable, restless, talking too fast and too much, and having more energy and needing less sleep than usual
-
Common symptoms of a depressive episode include feelings of sadness or emptiness, increased tearfulness, a loss of interest in activities you once enjoyed, loss of energy, difficulty concentrating or making decisions, feelings of worthlessness or guilt, changes in sleep or appetite and
-
Thoughts of death or suicide.
The symptoms of Major Depressive Disorder (MDD) include:
-
Feeling of sadness, emptiness and increased tearfulness,
-
Loss of interest in activities that you once enjoyed and loss of energy,
-
Problems focusing and making decisions
-
Feeling of worthlessness or guilt
-
Changes in sleep or eating patterns
-
Thoughts of death or suicide
-
MDD symptoms last most of the day, nearly every day for at least two weeks, and interfere with daily life at home and at work.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
SEROQUEL XR is a trademark of the AstraZeneca group of companies
©AstraZeneca 2010
Distributed by:
AstraZeneca Pharmaceuticals LP
Wilmington, DE 19850
SIC 35537–03
Rev. 05/201
image of label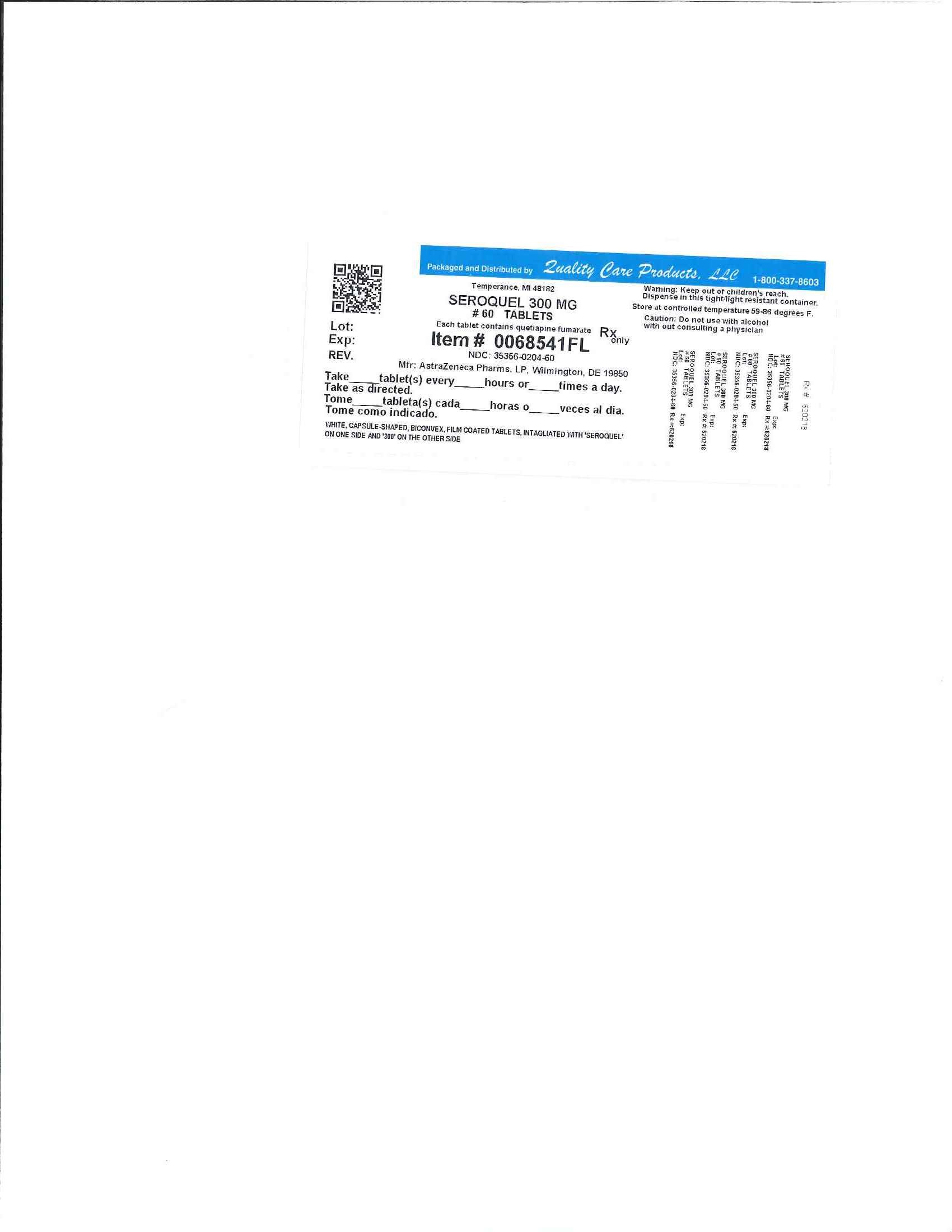
SeroquelQUETIAPINE FUMARATE TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||