Sodium Iodide I-131
HIGHLIGHTS OF PRESCRIBING INFORMATION RECENT MAJOR CHANGES Contraindications (4) 01/2014INDICATIONS AND USAGESodium Iodide I 131 Solution Therapeutic is a radioactive therapeutic agent indicated for the treatment of hyperthyroidism and thyroid carcinomas that take up iodine. Palliative effects may be observed in patients with advanced thyroid malignancy if the metastatic lesions take up iodine. (1) DOSAGE AND ADMINISTRATIONUse safe handling measures to minimize inadvertent radiation exposure. (2.1) Hyperthyroidism 148 to 370 megabecquerels (MBq) (4 to 10 millicuries, mCi). Toxic nodular goiter and other situations may require larger doses. (2.2) Thyroid carcinoma For thyroid carcinoma, 3700 to 5550 MBq (100 to 150 mCi). (2.3) For post-operative ablation of normal thyroid tissue: 1850 MBq (50 mCi). (2.3) DOSAGE FORMS AND STRENGTHSSolution is supplied in 2 concentrations of 5 or 25 mCi per milliliter at the time of calibration. See full prescribing information for strengths in MBq. (3) CONTRAINDICATIONS Patients with vomiting and diarrhea (4) In treatment of thyroid malignancies shown to have no iodide uptake (4) Pregnancy (4) Breastfeeding (4) WARNINGS AND PRECAUTIONS Radiation-induced thyroiditis: may cause or worsen hyperthyroidism; Consider pre-treatment with anti-thyroid medications. (5.1) Thyroid enlargement, including that due to stimulating hormone concomitant therapy, may obstruct structures in the neck. Evaluate patients at high risk. (5.2) Multiple non-thyroid radiation toxicities have been reported following sodium iodide I-131 therapy, including increased risks for neoplasia, hematopoietic suppression, and fetal or reproductive toxicity. Individualize dosage, verify absence of pregnancy, monitor patients for toxicity, and advise patients on contraceptive use. (5.3, 5.5, 5.6) Side Effects Adverse reactions that have been reported with doses of sodium iodide I-131 used in the treatment of benign disease include sialadenitis, chest pain, tachycardia, iododerma, itching skin, rash, hives, hypothyroidism, hyperthyroidism, thyrotoxic crisis, hypoparathyroidism, and local swelling. (6) Adverse reactions that have been reported with doses of sodium iodide I-131 used in the treatment of malignant disease include radiation sickness, bone marrow depression, anemia, leucopenia, thrombocytopenia, blood dyscrasia, leukemia, solid cancers, lacrimal gland dysfunction, salivary gland dysfunction, congenital hypothyroidism, and chromosomal abnormalities. (6) To report SUSPECTED ADVERSE REACTIONS contact Mallinckrodt Inc. at 1-888-744-1414 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONSMany pharmacologic agents are known to interact with radioiodide. See full prescribing information complete list. (7) USE IN SPECIFIC POPULATIONS Nursing Mothers: to minimize the absorbed radiation dose to breast tissue, discontinue breastfeeding at least four weeks before sodium iodide I-131 therapy. If administered in the postpartum period, the lactating mother should not breast-feed. (8.3) Pediatric Use: safety and effectiveness in pediatric patients have not been established. (8.4) Geriatric Use: enhanced evaluation, dose-selection and follow-up procedures may be necessary for geriatric patients due to underlying co-morbidities, including renal dysfunction. (8.5) Renal Impairment: may increase radiation exposure. (8.6)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 SODIUM IODIDE I-131 INDICATIONS AND USAGE
- 2 SODIUM IODIDE I-131 DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 SODIUM IODIDE I-131 CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 SODIUM IODIDE I-131 ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 11 SODIUM IODIDE I-131 DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PRINCIPAL DISPLAY PANEL - 0019-9450
- PRINCIPAL DISPLAY PANEL - 0019-9451
FULL PRESCRIBING INFORMATION
Contraindications (4) 08/2013
1 INDICATIONS AND USAGE
Sodium Iodide I 131 Solution Therapeutic is indicated for the treatment of hyperthyroidism and thyroid carcinomas that take up iodide. Palliative effects may be observed in patients with advanced thyroid malignancy if the metastatic lesions take up iodide.
2 DOSAGE AND ADMINISTRATION
2.1 Radiation Safety
Sodium iodide I-131 solution emits radiation and must be handled with safety measures to minimize inadvertent radiation exposure to clinical personnel and patients [see Warnings and Precautions (5.7)].
- Radiopharmaceuticals should be used only by or under the direction of physicians who are qualified by training and experience in the safe use and handling of radionuclides and whose experience and training have been approved by the appropriate governmental agency authorized to license the use of radionuclides.
- Wear waterproof gloves during the entire sodium iodide I-131 solution handling and administration procedure.
- Maintain adequate shielding during the radiation-emitting life of the product.
- Measure the patient dose using a suitable radioactivity calibration system immediately prior to administration.
2.2 Hyperthyroidism
For hyperthyroidism, the usual sodium iodide I-131 dose range is 148 to 370 MBq (4 to 10 mCi). Higher doses may be necessary for the treatment of toxic nodular goiter and other special situations. Consider discontinuation of anti-thyroid therapy in a severely hyperthyroid patient three to four days before administration of sodium iodide I-131. Evaluate patients for risk of thyroid enlargement and obstruction of structures in the neck [see Warnings and Precautions (5.1, 5.2)].
2.3 Thyroid Carcinoma
For thyroid carcinoma, the usual sodium iodide I-131 therapeutic dose is 3700 to 5550 MBq (100 to 150 mCi). For ablation of post-operative residual thyroid tissue, the usual dose is 1850 MBq (50 mCi).
2.4 Individualization of Therapy
Individualize sodium iodide I-131 therapy, including dose selection, based upon patient-specific factors such as the nature of the underlying condition, co-morbidities, age, estimated thyroid tissue iodine uptake, thyroid size, as well as ability of the patient to comply with the therapeutic regimen and radiation safety procedures. Perform a clinical assessment, including history, physical examination and laboratory testing when preparing patients for sodium iodide I-131 therapy in order to detect conditions which may alter thyroid iodine uptake and increase the risks of the therapy or diminish its effectiveness. For example, intake of iodine in radiographic contrast may diminish thyroid iodine uptake while low serum chloride or nephrosis may increase thyroid iodine uptake. Obtain a drug history and ascertain whether any medications need to be withheld before the administration of the therapy [see Drug Interactions (7)].
2.5 Radiation Dosimetry
The estimated absorbed radiation doses International Commission on Radiological Protection. Radiation Dose to Patients from Radiopharmaceuticals. ICRP Publication 53, Pergamon Press, New York, NY, 1988.
Table 1. Absorbed Radiation Doses
|
Tissue |
Thyroid Uptake |
|||||
|
5% |
15% |
25% |
||||
|
mGy/ MBq |
rads/ mCi |
mGy/ MBq |
rads/ mCi |
mGy/ MBq |
rads/ mCi |
|
|
Thyroid |
72 |
266 |
210 |
777 |
360 |
1300 |
|
Stomach Wall |
0.45 |
1.7 |
0.46 |
1.7 |
0.46 |
1.7 |
|
Red Marrow |
0.038 |
0.14 |
0.054 |
0.20 |
0.07 |
0.26 |
|
Liver |
0.03 |
0.11 |
0.032 |
0.12 |
0.035 |
0.13 |
|
Testes |
0.029 |
0.11 |
0.028 |
0.10 |
0.027 |
0.10 |
|
Ovaries |
0.044 |
0.16 |
0.043 |
0.16 |
0.043 |
0.16 |
|
Urinary Bladder |
0.58 |
2.1 |
0.52 |
1.9 |
0.46 |
1.7 |
|
Salivary Glands
L. Johansson, S. Leide-Svegborn, S. Matteson, B. Nosslin. Biokinetics of Iodide in Man: Refinement of Current ICRP Dosimetry Models. Cancer Biotherapy & Radiopharmaceuticals, 18(3): 445-450, 2003. |
0.5 |
1.85 |
0.5 |
1.85 |
0.5 |
1.85 |
|
Other |
0.040 |
0.15 |
0.065 |
0.24 |
0.090 |
0.33 |
3 DOSAGE FORMS AND STRENGTHS
Sodium Iodide I 131 Solution Therapeutic is supplied in 15 mL glass vials of multiple strengths
(Table 2).
Table 2. Solution Strengths
|
Total Radioactivity* per Vial |
||
|
Concentration* |
Volume of Solution |
Total Radioactivity* |
|
185 MBq/mL (5 mCi/mL) |
1 mL 2 mL 3 mL 4 mL 5 mL 7 mL |
185 MBq (5 mCi) 370 MBq (10 mCi) 555 MBq (15 mCi) 740 MBq (20 mCi) 925 MBq (25 mCi) 1295 MBq (35 mCi) |
|
925 MBq/mL (25 mCi/mL) |
2 mL 3 mL 4 mL 6 mL |
1850 MBq (50 mCi) 2775 MBq (75 mCi) 3700 MBq (100 mCi) 5550 MBq (150 mCi) |
* At time of calibration
4 CONTRAINDICATIONS
Sodium Iodide I 131 Solution Therapeutic is contraindicated in:
- Patients with vomiting and diarrhea [see Warnings and Precautions (5.7)].
- The treatment of thyroid malignancies shown to have no iodide uptake, which include the majority of medullary and anaplastic carcinomas.
- Pregnancy [see Warnings and Precautions (5.5)].
- Breastfeeding [see Use in Specific Populations ( 8.3 )].
5 WARNINGS AND PRECAUTIONS
5.1 Radiation-induced Thyroiditis
Sodium iodide I-131 may cause thyroiditis with gland enlargement and release of thyroid hormone, particularly when used to treat hyperthyroidism. The thyroiditis may cause or worsen hyperthyroidism and may cause thyroid storm. When treating hyperthyroidism, consider pre-treatment with anti-thyroid medication to help deplete the thyroid hormone content within the gland. Discontinue the anti-thyroid medication at least three days before administration of sodium iodide I-131. Consider beta-blocker therapy before administration of sodium iodide I-131 to minimize the risk of hyperthyroidism and thyroid storm.
5.2 Thyroid-stimulating Hormone (TSH) and Thyroid Enlargement
Enhanced TSH secretion, e.g., following discontinuation of anti-thyroid medications, or the administration of TSH to enhance sodium iodide I-131 uptake, may cause thyroid enlargement and obstructive complications of the trachea, esophagus, or blood vessels in the neck. Evaluate patients at high risk of obstructive complications before preparative treatments known to cause thyroid enlargement.
5.3 Radiation-induced Toxicities
Radiation-induced toxicities, including dose-dependent fatalities, have been reported following sodium iodide I-131 therapy. Post-marketing reports have identified an increased risk for neoplasia, as well as risks for hematopoietic suppression. Salivary and lacrimal gland toxicity is relatively common and may manifest as conjunctivitis, xerophthalmia, epiphora, sialadenitis and xerostomia [see Adverse Reactions (6)].
5.4 Hypersensitivity Reactions
Hypersensitivity reactions, including rash and hives, have been reported following administration of sodium iodide I-131. Sodium iodide I-131 solution contains sodium bisulfite, a sulfite that may cause allergic-type reactions, including anaphylactic symptoms and life-threatening or less severe asthmatic episodes. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people. During the pre-therapy assessment, question patients about a history of hypersensitivity to sulfite [see Adverse Reactions (6)].
5.5 Fetal Risk
Transplacental passage of sodium iodide I-131 can cause severe and possibly irreversible hypothyroidism in neonates [see Contraindications (4)].
Females and Males of Childbearing Potential
When planning sodium iodide I-131 therapy for women of childbearing potential, obtain a pregnancy test and verify the absence of a pregnancy. Advise women and men of childbearing potential to use two effective methods of contraception to avoid pregnancy for at least six months after sodium iodide I-131 administration. Advise patients of the potential need to use two effective forms of contraception to avoid pregnancy for an even longer period of time (e.g., one year) if additional sodium iodide I-131 therapy or radionuclide imaging is anticipated.
5.6 Transient Infertility
Transient, dose-related impairment of testicular function has been reported after sodium iodide I-131 therapy. Consider sperm banking for men who are anticipated to receive a high cumulative sodium iodide I-131 dose (e.g., greater than 14 GBq).
In females, transient ovarian failure has been observed after sodium iodide I-131 therapy.
5.7 Radiation Exposure Risk to Other Individuals
Unwanted radiation exposure can occur from handling and administration of radiopharmaceuticals or from contaminated waste products, including urine and feces. Follow safe administration instructions to minimize unnecessary radiation exposure to patients and health care workers [see Dosage and Administration (2.1 )]. Instruct patients on how to reduce unnecessary radiation exposure to others, especially family members following treatment.
Review the most recent professional society guidelines and publications that describe the procedures for the safe use of sodium iodide I-131 therapy to minimize radiation toxicity risks to patients, radiation exposure risks to other individuals, and environmental radiation contamination risks.
6 ADVERSE REACTIONS
The following serious adverse reactions are described below and elsewhere in labeling:
- Radiation-induced Thyroiditis [see Warnings and Precautions (5.1)]
- Thyroid-stimulating Hormone and Thyroid Enlargement [see Warnings and Precautions (5.2)]
- Radiation-induced Toxicities [see Warnings and Precautions (5.3)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.4)]
- Fetal Risk [see Warnings and Precautions (5.5)]
- Transient Infertility [see Warnings and Precautions (5.6)]
- Radiation Exposure to Other Individuals [see Warnings and Precautions (5.7)]
Radiation-related adverse reactions are a function of the dose level received by the patient.
The following adverse reactions have been reported with doses of sodium iodide
I-131 used in the treatment of benign disease, such as hyperthyroidism:
- Gastrointestinal disorders: sialadenitis
- Cardiac disorders: chest pain and tachycardia
- Skin and subcutaneous tissue disorders: iododerma, itching skin, rash, and hives
- Endocrine disorders: hypothyroidism, hyperthyroidism, thyrotoxic crisis, hypoparathyroidism
- General disorders and administration site conditions: local swelling
The following adverse reactions have been reported with doses of sodium iodide
I-131 used in the treatment of malignant disease:
- Blood and lymphatic system disorders including fatalities: radiation sickness, bone marrow depression, anemia, leucopenia, thrombocytopenia, and blood dyscrasia
- Neoplasms benign, malignant and unspecified (including cysts and polyps): leukemia and solid cancers
- Eye disorders: lacrimal gland dysfunction
- Gastrointestinal disorders: salivary gland dysfunction, nausea, vomiting
- Congenital, familial and genetic disorders: congenital hypothyroidism and chromosomal abnormalities
Adverse reactions that occur after treatment of benign disease may also occur after treatment of malignant disease. Tenderness, pain on swallowing, sore throat, and cough have been reported, generally around the third day after sodium iodide I-131 administration.
7 DRUG INTERACTIONS
Many pharmacologic agents interact with sodium iodide I-131. These agents may affect the iodide protein binding and alter the iodide pharmacokinetics and pharmacodynamics.
Table 3. Drug Interactions
|
Substance |
Average Duration of Effect |
|
Anti-thyroid drugs
|
5 days |
|
Natural or synthetic thyroid hormone
|
4 weeks |
|
Iodine-containing medications |
4 weeks |
|
Topical iodide |
1-9 months |
|
X-ray contrast agents |
Up to 1 year |
|
Other drugs |
1 week |
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category X [see Warnings and Precautions (5.5)].
8.3 Nursing Mothers
Sodium iodide I-131 is excreted into human milk and may reach concentrations equal to or greater than concentrations in maternal plasma. To minimize the absorbed radiation dose to the breast tissue, breastfeeding and breast-pumping should be discontinued for at least four weeks before administration of sodium iodide I-131. Sodium iodide I-131 is contraindicated in pregnancy; if sodium iodide I-131 is administered in the postpartum period, the lactating mother should not breast-feed the infant. Breastfeeding may resume with the birth of another child, if the mother does not receive sodium iodide I-131 during that postpartum period.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. Published reports suggest that the thyroid gland of pediatric patients is more sensitive to the effects of sodium iodide I-131; however, it is unknown if the I-131 dose-response relationship is similar to that of adults. When considering the use of sodium iodide I-131 in pediatric patients, the risks, particularly carcinogenic risks, and benefits of sodium iodide I-131 must be carefully weighed against those of other possible treatments.
8.5 Geriatric Use
Because elderly patients are more likely to have decreased renal function and co-morbid conditions, enhanced evaluation, dose-selection consideration and follow-up may be necessary for elderly patients receiving sodium iodide I-131 therapy, compared to younger patients [see Use in Specific Populations (8.6)].
When treating hyperthyroidism in geriatric patients at risk of developing cardiac complications, pre-treatment and post-treatment with anti-thyroid drugs and/or beta-blockers may help minimize the risk of excessive post-treatment hyperthyroidism due to radiation-induced thyroiditis [see Warnings and Precautions (5.1)].
8.6 Renal Impairment
Sodium iodide I-131 is eliminated predominantly through renal clearance. Patients with renal impairment are subject to decreased excretion of sodium iodide I-131 and increased radiation exposure. Evaluate renal function for therapeutic planning [see Dosage and Administration (2.4)]. Sodium iodide I-131 is dialyzable. Hemodialysis can be used to reduce total body radiation exposure.
In case of exposure to a radioactive dose of sodium iodide I-131 exceeding the intended therapeutic dose provide general supportive care, monitor for bone marrow and thyroid suppression and consider administering a thyroid blocking agent such as potassium iodide (KI) or perchlorate promptly within 4 to 6 hours after the exposure. Thyroid blockade may reduce radiation exposure of thyroid tissue but would not prevent radiation injury to the rest of the body. Assess the benefit of administering a blocking agent against the risk of failure of sodium iodide I-131 therapy.
11 DESCRIPTION
Sodium Iodide I 131 (Na I-131) Solution Therapeutic is supplied for oral administration as a stabilized aqueous solution. The solution is available in vials that contain from 185 to 5550 MBq (5 to 150 mCi) iodine-131 at the time of calibration. Sodium Iodide I 131 Solution Therapeutic is packaged in shielded, screw-cap 15 mL vials.
The solution contains 0.1% sodium bisulfite and 0.2% edetate disodium as stabilizers, 0.5% sodium phosphate anhydrous as a buffer and sodium iodide I-131 at concentrations of 185 or 925 MBq (5 or 25 mCi) per milliliter. The pH has been adjusted to between 7.5 and 9. The iodine-131 utilized in the preparation of the solution contains not less than 99% iodine-131 at the time of calibration. The expiration date is not later than one month after the calibration date. The calibration date and the expiration date are stated on the label.
11.1 Physical Characteristics
Iodine-131 decays by beta emission and associated gamma emission with a physical half-life of 8.02 days
Table 4. Principal Radiation Emission Data
|
Radiation |
Mean Percent Per Disintegration |
Energy (keV) |
|
Beta-1 |
2.10 |
69.4 Avg. |
|
Beta-3 |
7.27 |
96.6 Avg. |
|
Beta-4 |
89.9 |
191.6 Avg. |
|
Gamma-7 |
6.14 |
284.3 |
|
Gamma-14 |
81.7 |
364.5 |
|
Gamma-17 |
7.17 |
637.0 |
11.2 External Radiation
The specific gamma ray constant for iodine-131 is 2.20 R/hr-mCi at 1 cm. The first half-value thickness of lead (Pb) for iodine-131 is 0.27 cm. A range of values for the relative attenuation of the radiation emitted by this radionuclide that results from interposition of various thicknesses of Pb is shown in Table 5. For example, the use of 4.5 cm of Pb will decrease the external radiation exposure by a factor of about 1,000.
Table 5. Radiation Attenuation by Lead Shielding4
|
Shield Thickness (Pb), cm |
Coefficient of Attenuation |
|
0.27 |
0.5 |
|
0.99 |
10-1 |
|
2.6 |
10-2 |
|
4.5 |
10-3 |
To correct for physical decay of this radionuclide, the fractions that remain at selected time intervals after the date of calibration are shown in Table 6.
Table 6. Physical Decay Chart
Iodine-131: Half-Life 8.02 Days
|
Days |
Fraction Remaining |
Days |
Fraction Remaining |
Days |
Fraction Remaining |
|
0* |
1.000 |
11 |
0.387 |
22 |
0.149 |
|
1 |
0.917 |
12 |
0.355 |
23 |
0.137 |
|
2 |
0.841 |
13 |
0.325 |
24 |
0.126 |
|
3 |
0.772 |
14 |
0.298 |
25 |
0.115 |
|
4 |
0.708 |
15 |
0.274 |
26 |
0.106 |
|
5 |
0.649 |
16 |
0.251 |
27 |
0.097 |
|
6 |
0.595 |
17 |
0.230 |
28 |
0.089 |
|
7 |
0.546 |
18 |
0.211 |
29 |
0.082 |
|
8 |
0.501 |
19 |
0.194 |
30 |
0.075 |
|
9 |
0.459 |
20 |
0.178 |
||
|
10 |
0.421 |
21 |
0.163 |
*Calibration Day
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Taken orally, sodium iodide I-131 is rapidly absorbed and distributed within the extracellular fluid of the body. The iodide is concentrated in the thyroid via the sodium/iodide symporter, and subsequently oxidized to iodine. The destruction of thyroidal tissue is achieved by the beta emission of sodium iodide I-131.
12.2 Pharmacodynamics
The therapeutic effects of sodium iodide I-131 are a result of the ionizing radiation absorbed by the thyroidal tissue. Tissue damage is the result of direct insult to molecules by ionization and excitation and the consequent dissociation of those molecules. About 90% of local irradiation from sodium iodide I-131 is the result of beta radiation and 10% is the result of gamma radiation.
12.3 Pharmacokinetics
After oral administration, sodium iodide I-131 is absorbed rapidly from the upper gastrointestinal tract (90% in 60 minutes). The pharmacokinetics follow that of unlabelled iodide. After entering the blood stream, the iodide is distributed into the extra thyroidal compartment. From here it is predominantly taken up by the thyroid or excreted renally. In the thyroid, the trapped iodide is oxidized to iodine and organified. The sodium/iodide symporter (NIS) is responsible for the concentration of iodide in the thyroid. This active transport process is capable of concentrating iodide 20 to 40 times the plasma concentration under normal circumstances, and this may increase tenfold in the hyperthyroid state. NIS also mediates active iodide transport in other tissues, including salivary glands, nasolacrimal duct, lacrimal sac, gastric mucosa, lactating mammary gland, and the choroid plexus. The non-thyroidal iodide transporting tissues do not have the ability to organify accumulated iodide.
Depending on renal and thyroid gland function, urinary excretion is 37 to 75% of the administered dose, fecal excretion is about 10%, and excretion in sweat is almost negligible.
15 REFERENCES
1 International Commission on Radiological Protection. Radiation Dose to Patients from Radiopharmaceuticals. ICRP Publication 53, Pergamon Press, New York, NY, 1988.
2 L. Johansson, S. Leide-Svegborn, S. Matteson, B. Nosslin. Biokinetics of Iodide in Man: Refinement of Current ICRP Dosimetry Models. Cancer Biotherapy & Radiopharmaceuticals, 18(3): 445-450, 2003.
3 Stabin MG, da Luz CQPL. Decay Data for Internal and External Dose Assessment, Health Phys. 83(4):471-475, 2002.
4 Smith David S., Stabin, Michael G. Exposure Rate Constants and Lead Shielding Values for Over 1,100 Radionuclides, Health Physics. 102(3):271-291, March 2012.
16 HOW SUPPLIED/STORAGE AND HANDLING
Sodium Iodide I 131 Solution Therapeutic is supplied in shielded, screw-cap 15 mL vials that contain from 185 to 5550 MBq (5 to 150 mCi) iodine-131 at the time of calibration. The expiration date is not later than one month after the calibration date. The calibration date and the expiration date are stated on the label. Do not use the product after the expiration date.
|
Sodium Iodide I 131 Solution Therapeutic |
|||
|
NDC |
Volume of Solution |
Total Radioactivity per Vial |
|
|
0019-9450-01 |
1 mL |
185 MBq |
(5 mCi) |
|
0019-9450-02 |
2 mL |
370 MBq |
(10 mCi) |
|
0019-9450-03 |
3 mL |
555 MBq |
(15 mCi) |
|
0019-9450-04 |
4 mL |
740 MBq |
(20 mCi) |
|
0019-9450-05 |
5 mL |
925 MBq |
(25 mCi) |
|
0019-9450-07 |
7 mL |
1295 MBq |
(35 mCi) |
|
0019-9451-02 |
2 mL |
1850 MBq |
(50 mCi) |
|
0019-9451-03 |
3 mL |
2775 MBq |
(75 mCi) |
|
0019-9451-04 |
4 mL |
3700 MBq |
(100 mCi) |
|
0019-9451-06 |
6 mL |
5550 MBq |
(150 mCi) |
Storage
Store at a controlled room temperature of 20° to 25°C (68° to 77°F). Storage and disposal of Sodium Iodide I 131 Solution Therapeutic should be controlled in a manner that is in compliance with the appropriate regulations of the government agency authorized to license the use of this radionuclide.
The U.S. Nuclear Regulatory Commission has approved distribution of this radiopharmaceutical to persons licensed to use byproduct material listed in 10 CFR 35.300, and to persons who hold an equivalent license issued by an Agreement State.
17 PATIENT COUNSELING INFORMATION
Review the most recent professional society guidelines and publications that describe important components of the patient counseling process.
- Discuss the measures to minimize inadvertent radiation exposure to the patient, members of the patient’s household, the public, and the environment.
- Advise females and males of reproductive potential of the need to use two effective methods of contraception to avoid pregnancy for at least 6 months after I-131 administration due to fetal risk. Advise patients of the potential need to use two effective methods of contraception to avoid pregnancy for an even longer period of time (e.g., one year) if additional sodium iodide I-131 therapy and further radionuclide imaging is anticipated.
- Advise patients of the possibility of transient infertility and possible use of sperm banking for males of reproductive potential.
- Among lactating females, discuss the need to discontinue breastfeeding and pumping at least four weeks before administration of sodium iodide I-131. If sodium iodide I-131 is administered in the postpartum period, advise the lactating mother to not breast-feed her infant.
Manufactured by:
Mallinckrodt Inc.
St. Louis, MO 63134 USA
A450I0
Rev 01/2014
tyco Healthcare
Mallinckrodt
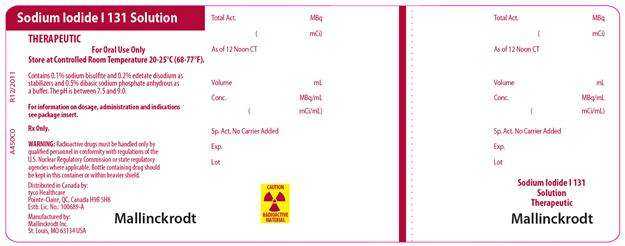
PRINCIPAL DISPLAY PANEL - 0019-9450
SODIUM IODIDE I 131 SOLUTION
THERAPEUTIC
For Oral Use Only
Store at Controlled Room Temperature 20 to 25°C (68 to 77°F).
Contains 0.1% sodium bisulfate and 0.2% edetate disodium as stabilizers and 0.5% dibasic sodium phosphate anhydrous as a buffer. The pH is between 7.5 and 9.0
For information on dosage, administration and indications see package insert.
Rx Only.
WARNING: Radioactive drugs must be handled only by qualified personnel in conformity with regulations of the U.S. Nuclear Regulatory Commission or state regulatory agencies where applicable. Bottle containing drug should be kept in this container or within heavier shield.
Distributed in Canada by:
tyco Healthcare
Pointe-Claire, QC Canada H9R 5H8
Estb. Lic. No.: 100689-A
Manufactured by:
Mallinckrodt Inc.
St. Louis, MO 63134 USA
MALLINCKRODT
CAUTION RADIOACTIVE MATERIAL
A450C0
R12/2011
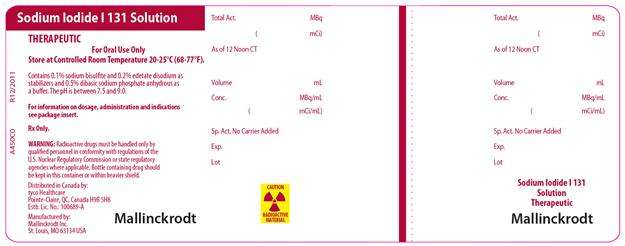
PRINCIPAL DISPLAY PANEL - 0019-9451
SODIUM IODIDE I 131 SOLUTION
THERAPEUTIC
For Oral Use Only
Store at Controlled Room Temperature 20 to 25°C (68 to 77°F).
Contains 0.1% sodium bisulfate and 0.2% edetate disodium as stabilizers and 0.5% dibasic sodium phosphate anhydrous as a buffer. The pH is between 7.5 and 9.0
For information on dosage, administration and indications see package insert.
Rx Only.
WARNING: Radioactive drugs must be handled only by qualified personnel in conformity with regulations of the U.S. Nuclear Regulatory Commission or state regulatory agencies where applicable. Bottle containing drug should be kept in this container or within heavier shield.
Distributed in Canada by:
tyco Healthcare
Pointe-Claire, QC Canada H9R 5H8
Estb. Lic. No.: 100689-A
Manufactured by:
Mallinckrodt Inc.
St. Louis, MO 63134 USA
MALLINCKRODT
CAUTION RADIOACTIVE MATERIAL
A450C0
R12/2011
Sodium Iodide I-131sodium iodide, i-131 SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sodium Iodide I-131sodium iodide, i-131 SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||