Terbinafine Hydrochloride
Dr.Reddys Laboratories Limited
HIGHLIGHTS OF PRESCRIBING INFORMATION INDICATIONS AND USAGETerbinafine tablets are an allylamine antifungal indicated for the treatment of onychomycosis of the toenail or fingernail due to dermatophytes (tinea unguium) DOSAGE AND ADMINISTRATION Fingernail onychomycosis: One 250 mg tablet, once daily for 6 weeks. Toenail onychomycosis: One 250 mg tablet, once daily for 12 weeks. DOSAGE FORMS AND STRENGTHSTablet, 250 mg CONTRAINDICATIONSTerbinafine tablets are contraindicated in individuals with a history of allergic reaction to oral terbinafine because of the risk of anaphylaxis. (4) WARNINGS AND PRECAUTIONS Liver failure, sometimes leading to liver transplant or death, has occurred with the use of oral terbinafine. Obtain pretreatment serum transaminases. Discontinue terbinafine tablets if liver injury develops. (5.1, 5.8) Taste disturbance, including taste loss, has been reported with the use of terbinafine tablets. Taste disturbance can be severe, may be prolonged, or may be permanent. Discontinue terbinafine tablets if taste disturbance occurs. (5.2) Smell disturbance, including loss of smell, has been reported with the use of terbinafine tablets. Smell disturbance may be prolonged, or may be permanent. Discontinue terbinafine tablets if smell disturbance occurs. (5.3) Depressive symptoms have been reported with terbinafine use. Prescribers should be alert to development of depressive symptoms. (5.4) Severe neutropenia has been reported. If the neutrophil count is ≤ 1,000 cells/mm3, terbinafine tablets should be discontinued. (5.5) Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported with oral terbinafine use. If progressive skin rash occurs, treatment with terbinafine tablets should be discontinued. (5.6) Side EffectsCommon (>2% in patients treated with terbinafine tablets) reported adverse events include headache, diarrhea, rash, dyspepsia, liver enzyme abnormalities, pruritus, taste disturbance, nausea, abdominal pain, and flatulence. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories, Inc. at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSTerbinafine is an inhibitor of CYP4502D6 isozyme and has an effect on metabolism of desipramine, cimetidine, fluconazole, cyclosporine, rifampin, and caffeine. (7.1)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 TERBINAFINE HYDROCHLORIDE INDICATIONS AND USAGE
- 2 TERBINAFINE HYDROCHLORIDE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 TERBINAFINE HYDROCHLORIDE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 TERBINAFINE HYDROCHLORIDE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 TERBINAFINE HYDROCHLORIDE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PATIENT PACKAGE INSERT SECTION
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Terbinafine tablets are indicated for the treatment of onychomycosis of the toenail or fingernail due to dermatophytes (tinea unguium).
Prior to initiating treatment, appropriate nail specimens for laboratory testing (KOH preparation, fungal culture, or nail biopsy) should be obtained to confirm the diagnosis of onychomycosis.
2 DOSAGE AND ADMINISTRATION
Fingernail onychomycosis: One 250 mg tablet once daily for 6 weeks.
Toenail onychomycosis: One 250 mg tablet once daily for 12 weeks.
The optimal clinical effect is seen some months after mycological cure and cessation of treatment. This is related to the period required for outgrowth of healthy nail.
3 DOSAGE FORMS AND STRENGTHS
Tablet, 250 mg are white, round, flat, beveled edged tablets embossed ‘250’ on one side and ‘RDY’ on other side
4 CONTRAINDICATIONS
Terbinafine tablets are contraindicated in individuals with a history of allergic reaction to oral terbinafine because of the risk of anaphylaxis.
5 WARNINGS AND PRECAUTIONS
Cases of liver failure, some leading to liver transplant or death, have occurred with the use of terbinafine tablets in individuals with and without pre-existing liver disease.
In the majority of liver cases reported in association with terbinafine hydrochloride use, the patients had serious underlying systemic conditions. The severity of hepatic events and/or their outcome may be worse in patients with active or chronic liver disease. Treatment with terbinafine tablets should be discontinued if biochemical or clinical evidence of liver injury develops.
Terbinafine tablets are not recommended for patients with chronic or active liver disease. Before prescribing terbinafine tablets, pre-existing liver disease should be assessed. Hepatotoxicity may occur in patients with and without pre-existing liver disease. Patients prescribed terbinafine tablets should be warned to report immediately to their physician any symptoms of persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain or jaundice, dark urine or pale stools. Patients with these symptoms should discontinue taking oral terbinafine, and the patient’s liver function should be immediately evaluated.
Taste disturbance, including taste loss, has been reported with the use of terbinafine tablets. It can be severe enough to result in decreased food intake, weight loss, and depressive symptoms. Taste disturbance may resolve within several weeks after discontinuation of treatment, but may be prolonged (greater than one year), or may be permanent. If symptoms of a taste disturbance occur, terbinafine tablets should be discontinued.
Smell disturbance, including loss of smell, has been reported with the use of terbinafine tablets. Smell disturbance may resolve after discontinuation of treatment, but may be prolonged (greater than one year), or may be permanent. If symptoms of a smell disturbance occur, terbinafine tablets should be discontinued.
Depressive symptoms have occurred during postmarketing use of terbinafine. Prescribers should be alert to depressive symptoms, and patients should be instructed to report depressive symptoms to their physician.
Transient decreases in absolute lymphocyte counts (ALC) have been observed in controlled clinical trials. In placebo-controlled trials, 8/465 terbinafine hydrochloride-treated patients (1.7%) and 3/137 placebo-treated patients (2.2%) had decreases in ALC to below 1000/mm3 on two or more occasions. In patients with known or suspected immunodeficiency, physicians should consider monitoring complete blood counts if treatment continues for more than six weeks. Cases of severe neutropenia have been reported. These were reversible upon discontinuation of terbinafine hydrochloride, with or without supportive therapy. If clinical signs and symptoms suggestive of secondary infection occur, a complete blood count should be obtained. If the neutrophil count is <1,000 cells/mm3, terbinafine hydrochloride should be discontinued and supportive management started.
There have been postmarketing reports of serious skin reactions (e.g., Stevens-Johnson Syndrome and toxic epidermal necrolysis). If progressive skin rash occurs, treatment with terbinafine tablets should be discontinued.
During post-marketing experience, precipitation and exacerbation of cutaneous and systemic lupus erythematosus have been reported in patients taking terbinafine tablets. Terbinafine tablets should be discontinued in patients with clinical signs and symptoms suggestive of lupus erythematosus.
Measurement of serum transaminases (ALT and AST) is advised for all patients before taking terbinafine tablets.
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The most frequently reported adverse events observed in the three US/Canadian placebo-controlled trials are listed in the table below. The adverse events reported encompass gastrointestinal symptoms (including diarrhea, dyspepsia, and abdominal pain), liver test abnormalities, rashes, urticaria, pruritus, and taste disturbances. Changes in the ocular lens and retina have been reported following the use of terbinafine tablets in controlled trials. The clinical significance of these changes is unknown. In general, the adverse events were mild, transient, and did not lead to discontinuation from study participation.
| Adverse Event | Discontinuation | |||
| Terbinafine tablet | Placebo | Terbinafine tablet | Placebo | |
| (%) | (%) | (%) | (%) | |
| n=465 | n=137 | n=465 | n=137 | |
| Headache | 12.9 | 9.5 | 0.2 | 0.0 |
| Gastrointestinal | ||||
| Symptoms: | ||||
| Diarrhea | 5.6 | 2.9 | 0.6 | 0.0 |
| Dyspepsia | 4.3 | 2.9 | 0.4 | 0.0 |
| Abdominal Pain | 2.4 | 1.5 | 0.4 | 0.0 |
| Nausea | 2.6 | 2.9 | 0.2 | 0.0 |
| Flatulence | 2.2 | 2.2 | 0.0 | 0.0 |
| Dermatological | ||||
| Symptoms: | ||||
| Rash | 5.6 | 2.2 | 0.9 | 0.7 |
| Pruritus | 2.8 | 1.5 | 0.2 | 0.0 |
| Urticaria | 1.1 | 0.0 | 0.0 | 0.0 |
| Liver Enzyme | ||||
| Abnormalities* | 3.3 | 1.4 | 0.2 | 0.0 |
| Taste Disturbance | 2.8 | 0.7 | 0.2 | 0.0 |
| Visual Disturbance | 1.1 | 1.5 | 0.9 | 0.0 |
* Liver enzyme abnormalities ≥ 2x the upper limit of normal range.
The following adverse events have been identified during post-approval use of terbinafine hydrochloride. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse events, based on worldwide experience with terbinafine tablets use, include: idiosyncratic and symptomatic hepatic injury and more rarely, cases of liver failure, some leading to death or liver transplant, serious skin reactions (e.g., Stevens-Johnson Syndrome and toxic epidermal necrolysis), severe neutropenia, thrombocytopenia, agranulocytosis, pancytopenia, anemia, angioedema, and allergic reactions (including anaphylaxis) [see Warnings and Precautions (5.1, 5.5 , and 5.6)].
Psoriasiform eruptions or exacerbation of psoriasis, acute generalized exanthematous pustulosis and precipitation and exacerbation of cutaneous and systemic lupus erythematosus have been reported in patients taking terbinafine hydrochloride [see Warnings and Precautions (5.7)].
Cases of taste disturbance, including taste loss, have been reported with the use of terbinafine tablets. It can be severe enough to result in decreased food intake, weight loss, and depressive symptoms [see Warnings and Precautions (5.2)]. Depressive symptoms independent of taste disturbance have been reported with use of terbinafine tablets. In some cases, depressive symptoms have been reported to subside with discontinuance of therapy and to recur with reinstitution of therapy [see Warnings and Precautions (5.4)]. Cases of smell disturbance, including smell loss, have been reported with the use of terbinafine tablets [see Warnings and Precautions (5.3)].
Other adverse reactions which have been reported include malaise, fatigue, vomiting, arthralgia, myalgia, rhabdomyolysis, reduced visual acuity, visual field defect, hair loss, serum sickness-like reaction, vasculitis, pancreatitis, influenza-like illness, pyrexia, increased blood creatine phosphokinase, photosensitivity reactions, tinnitus, hearing impairment and vertigo.
Altered prothrombin time (prolongation and reduction) in patients concomitantly treated with warfarin has been reported.
7 DRUG INTERACTIONS
In vivo studies have shown that terbinafine is an inhibitor of the CYP450 2D6 isozyme. Drugs predominantly metabolized by the CYP450 2D6 isozyme include the following drug classes: tricyclic antidepressants, selective serotonin reuptake inhibitors, beta-blockers, antiarrhythmics class 1C (e.g., flecainide and propafenone) and monoamine oxidase inhibitors Type B. Coadministration of terbinafine hydrochloride should be done with careful monitoring and may require a reduction in dose of the 2D6-metabolized drug. In a study to assess the effects of terbinafine on desipramine in healthy volunteers characterized as normal metabolizers, the administration of terbinafine resulted in a 2-fold increase in Cmax and a 5-fold increase in AUC. In this study, these effects were shown to persist at the last observation at 4 weeks after discontinuation of terbinafine tablets. In studies in healthy subjects characterized as extensive metabolizers of dextromethorphan (antitussive drug and CYP2D6 probe substrate), terbinafine increases the dextromethorphan/dextrorphan metabolite ratio in urine by 16- to 97-fold on average. Thus, terbinafine may convert extensive CYP2D6 metabolizers to poor metabolizer status.
In vitro studies with human liver microsomes showed that terbinafine does not inhibit the metabolism of tolbutamide, ethinylestradiol, ethoxycoumarin, cyclosporine, cisapride and fluvastatin. In vivo drug-drug interaction studies conducted in healthy volunteer subjects showed that terbinafine does not affect the clearance of antipyrine or digoxin. Terbinafine decreases the clearance of caffeine by 19%. Terbinafine increases the clearance of cyclosporine by 15%.
The influence of terbinafine on the pharmacokinetics of fluconazole, cotrimoxazole (trimethoprim and sulfamethoxazole), zidovudine or theophylline was not considered to be clinically significant.
Co-administration of a single dose of fluconazole (100mg) with a single dose of terbinafine resulted in a 52% and 69% increase in terbinafine Cmax and AUC, respectively. Fluconazole is an inhibitor of CYP2C9 and CYP3A enzymes. Based on this finding, it is likely that other inhibitors of both CYP2C9 and CYP3A4 (e.g., ketoconazole, amiodarone) may also lead to a substantial increase in the systemic exposure (Cmax and AUC) of terbinafine when concomitantly administered.
There have been spontaneous reports of increase or decrease in prothrombin times in patients concomitantly taking oral terbinafine and warfarin, however, a causal relationship between terbinafine tablets and these changes has not been established.
Terbinafine clearance is increased 100% by rifampin, a CYP450 enzyme inducer, and decreased 33% by cimetidine, a CYP450 enzyme inhibitor. Terbinafine clearance is unaffected by cyclosporine. There is no information available from adequate drug-drug interaction studies with the following classes of drugs: oral contraceptives, hormone replacement therapies, hypoglycemics, phenytoins, thiazide diuretics, and calcium channel blockers.
An evaluation of the effect of food on terbinafine tablets was conducted. An increase of less than 20% of the AUC (i.e. area under the curve) of terbinafine was observed when terbinafine tablets were administered with food. Terbinafine tablets can be taken with or without food.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B: There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, and because treatment of onychomycosis can be postponed until after pregnancy is completed, it is recommended that terbinafine hydrochloride not be initiated during pregnancy.
Oral reproduction studies have been performed in rabbits and rats at doses up to 300 mg/kg/day (12x to 23x the MRHD, in rabbits and rats, respectively, based on BSA) and have revealed no evidence of impaired fertility or harm to the fetus due to terbinafine.
8.3 Nursing Mothers
After oral administration, terbinafine is present in breast milk of nursing mothers. The ratio of terbinafine in milk to plasma is 7:1. Treatment with terbinafine hydrochloride is not recommended in nursing mothers.
8.4 Pediatric Use
The safety and efficacy of terbinafine tablets have not been established in pediatric patients with onychomycosis.
8.5 Geriatric Use
Clinical studies of terbinafine tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
10 OVERDOSAGE
Clinical experience regarding overdose with oral terbinafine is limited. Doses up to 5 grams (20 times the therapeutic daily dose) have been taken without inducing serious adverse reactions. The symptoms of overdose included nausea, vomiting, abdominal pain, dizziness, rash, frequent urination, and headache.
11 DESCRIPTION
Terbinafine tablets contain the synthetic allylamine antifungal compound terbinafine hydrochloride. Chemically, terbinafine hydrochloride is (E)-N-(6,6-dimethyl-2-hepten-4-ynyl)-N-methyl-1-naphthalenemethanamine hydrochloride. The molecular formula C21H26CIN with a molecular weight of 327.90, and the following structural formula:
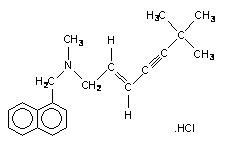
Terbinafine hydrochloride is a white to off-white fine crystalline powder. It is freely soluble in methanol and methylene chloride, soluble in ethanol, and slightly soluble in water.
Each tablet contains:
Active Ingredients: terbinafine hydrochloride (equivalent to 250 mg of terbinafine)
Inactive Ingredients: colloidal silicon dioxide, NF; croscarmellose sodium, NF; hypromellose, NF; magnesium stearate, NF; microcrystalline cellulose, NF.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Terbinafine is an allylamine antifungal [see Clinical Pharmacology (12.4)].
12.2 Pharmacodynamics
The pharmacodynamics of terbinafine hydrochloride is unknown.
12.3 Pharmacokinetics
Following oral administration, terbinafine is well absorbed (>70%) and the bioavailability of terbinafine tablets as a result of first-pass metabolism is approximately 40%. Peak plasma concentrations of 1 μg/mL appear within 2 hours after a single 250 mg dose; the AUC (area under the curve) is approximately 4.56 μg.h/mL. An increase in the AUC of terbinafine of less than 20% is observed when terbinafine tablets are administered with food.
In plasma, terbinafine is >99% bound to plasma proteins and there are no specific binding sites. At steady-state, in comparison to a single dose, the peak concentration of terbinafine is 25% higher and plasma AUC increases by a factor of 2.5; the increase in plasma AUC is consistent with an effective half-life of ~36 hours. Terbinafine is distributed to the sebum and skin. A terminal half-life of 200-400 hours may represent the slow elimination of terbinafine from tissues such as skin and adipose. Prior to excretion, terbinafine is extensively metabolized by at least seven CYP isoenzymes with major contributions from CYP2C9, CYP1A2, CYP3A4, CYP2C8 and CYP2C19. No metabolites have been identified that have antifungal activity similar to terbinafine. Approximately 70% of the administered dose is eliminated in the urine.
In patients with renal impairment (creatinine clearance <50 mL/min) or hepatic cirrhosis, the clearance of terbinafine is decreased by approximately 50% compared to normal volunteers. No effect of gender on the blood levels of terbinafine was detected in clinical trials. No clinically relevant age-dependent changes in steady-state plasma concentrations of terbinafine have been reported.
Terbinafine, an allylamine antifungal, inhibits biosynthesis of ergosterol, an essential component of fungal cell membrane, via inhibition of squalene epoxidase enzyme. This results in fungal cell death primarily due to the increased membrane permeability mediated by the accumulation of high concentrations of squalene but not due to ergosterol deficiency. Depending on the concentration of the drug and the fungal species test in vitro, terbinafine hydrochloride may be fungicidal. However, the clinical significance of in vitro data is unknown.
Terbinafine has been shown to be active against most strains of the following microorganisms both in vitro and in clinical infections:
Trichophyton mentagrophytes
Trichophyton rubrum
The following in vitro data are available, but their clinical significance is unknown. In vitro, terbinafine exhibits satisfactory MIC’s against most strains of the following microorganisms; however, the safety and efficacy of terbinafine in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials:
Candida albicans
Epidermophyton floccosum
Scopulariopsis brevicaulis
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
In a 28-month oral carcinogenicity study in rats, an increase in the incidence of liver tumors was observed in males at the highest dose tested, 69 mg/kg/day [2x the Maximum Recommended Human Dose (MRHD) based on AUC comparisons of the parent terbinafine]; however, even though dose-limiting toxicity was not achieved at the highest tested dose, higher doses were not tested.
The results of a variety of in vitro (mutations in E. coli and S. typhimurium, DNA repair in rat hepatocytes, mutagenicity in Chinese hamster fibroblasts, chromosome aberration and sister chromatid exchanges in Chinese hamster lung cells), and in vivo (chromosome aberration in Chinese hamsters, micronucleus test in mice) genotoxicity tests gave no evidence of a mutagenic or clastogenic potential.
Oral reproduction studies in rats at doses up to 300 mg/kg/day (approximately 12x the MRHD based on body surface area comparisons, BSA) did not reveal any specific effects on fertility or other reproductive parameters. Intravaginal application of terbinafine hydrochloride at 150 mg/day in pregnant rabbits did not increase the incidence of abortions or premature deliveries nor affect fetal parameters.
13.2 Animal Pharmacology and/or Toxicology
A wide range of in vivo studies in mice, rats, dogs, and monkeys, and in vitro studies using rat, monkey, and human hepatocytes suggest that peroxisome proliferation in the liver is a rat-specific finding. However, other effects, including increased liver weights and APTT, occurred in dogs and monkeys at doses giving Css trough levels of the parent terbinafine 2-3x those seen in humans at the MRHD. Higher doses were not tested.
14 CLINICAL STUDIES
The efficacy of terbinafine tablets in the treatment of onychomycosis is illustrated by the response of patients with toenail and/or fingernail infections who participated in three US/Canadian placebo-controlled clinical trials.
Results of the first toenail study, as assessed at week 48 (12 weeks of treatment with 36 weeks follow-up after completion of therapy), demonstrated mycological cure, defined as simultaneous occurrence of negative KOH plus negative culture, in 70% of patients. Fifty-nine percent (59%) of patients experienced effective treatment (mycological cure plus 0% nail involvement or >5mm of new unaffected nail growth); 38% of patients demonstrated mycological cure plus clinical cure (0% nail involvement).
In a second toenail study of dermatophytic onychomycosis, in which non-dermatophytes were also cultured, similar efficacy against the dermatophytes was demonstrated. The pathogenic role of the non-dermatophytes cultured in the presence of dermatophytic onychomycosis has not been established. The clinical significance of this association is unknown.
Results of the fingernail study, as assessed at week 24 (6 weeks of treatment with 18 weeks follow-up after completion of therapy), demonstrated mycological cure in 79% of patients, effective treatment in 75% of the patients, and mycological cure plus clinical cure in 59% of the patients.
The mean time to overall success was approximately 10 months for the first toenail study and 4 months for the fingernail study. In the first toenail study, for patients evaluated at least six months after achieving clinical cure and at least one year after completing terbinafine hydrochloride therapy, the clinical relapse rate was approximately 15%.
16 HOW SUPPLIED/STORAGE AND HANDLING
Terbinafine tablets USP, 250 mg are white, round, flat, beveled edged tablets embossed ‘250’ on one side and ‘RDY’ on other side and are supplied in bottles of 30, 90,100, 500 and unit dose packages of 100 (10 x 10).
Bottles of 30 NDC 55111-250-30
Bottles of 90 NDC 55111-250-90
Bottles of 100 NDC 55111-250-01
Bottles of 500 NDC 55111-250-05
Unit dose packages of 100 (10 x 10) NDC 55111-250-78
Store at 20°-25°C (68°-77°F) [see USP Controlled Room Temperature]; in a tight container. Protect from light.
17 PATIENT COUNSELING INFORMATION
[See FDA-Approved Patient Labeling (Patient Information)]
Patients taking terbinafine tablets should receive the following information and instructions:
- Patients should take one 250 mg tablet once daily for 6 weeks for treatment of fingernail onychomycosis or once daily for 12 weeks for treatment of toenail onychomycosis. The optimal clinical effect is seen some months after mycological cure and cessation of treatment due to the time period required for outgrowth of healthy nail.
- Patients should be advised to immediately report to their physician any symptoms of persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain, jaundice, dark urine or pale stools. Terbinafine tablets treatment should be discontinued.
- Patients should be advised to report to their physician any signs of taste disturbance, smell disturbance and/or depressive symptoms. Terbinafine tablets treatment should be discontinued.
- Patients should be advised to immediately report to their physician or get emergency help if they experience any of the following symptoms: hives, mouth sores, blistering and peeling of skin, swelling of face, lips, tongue, or throat, difficulty swallowing or breathing. Terbinafine tablets treatment should be discontinued.
- Patients should be advised to report to their physician any symptoms of new onset or worsening lupus erythematosus. Symptoms can include erythema, scaling, loss of pigment, and unusual photosensitivity that can result in a rash. Terbinafine hydrochloride treatment should be discontinued.
- Photosensitivity reactions have been reported with the use of Terbinafine hydrochloride. Patients should be advised to minimize exposure to natural and artificial sunlight (tanning beds or UVA/B treatment) while using Terbinafine hydrochloride.
- Measurement of serum transaminases (ALT and AST) is advised for all patients before taking terbinafine tablets.
- Patients should be advised that if they forget to take terbinafine tablets, to take their tablets as soon as they remember, unless it is less than four hours before the next dose is due. Patients should also be advised that if they take too many terbinafine tablets they should call their physician.
PATIENT PACKAGE INSERT SECTION
PATIENT INFORMATION
TERBINAFINE TABLETS USP
Read this Patient Information before you start taking terbinafine tablets and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment.
What are terbinafine tablets?
Terbinafine tablet is a prescription antifungal medicine used to treat fungal infections of the fingernails and toenails (onychomycosis).
Your doctor should do tests to check you for fungal infection of your nails before you start terbinafine tablets.
It is not known if terbinafine hydrochloride is safe and effective in children for the treatment of onychomycosis.
Who should not take terbinafine tablets?
Do not take terbinafine hydrochloride if you are allergic to terbinafine hydrochloride when taken by mouth.
What should I tell my doctor before taking terbinafine tablets?
Before you take terbinafine tablets, tell your doctor if you:
- have or had liver problems
- have a weakened immune system (immunocompromised)
- have lupus (an autoimmune disease)
- have kidney problems
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if terbinafine tablets will harm your unborn baby. You should not start using terbinafine tablets during pregnancy without talking with your doctor.
- are breast-feeding or plan to breast-feed. Some terbinafine tablets passes into your milk and may harm your baby. Talk to your doctor about the best way to feed your baby if you take terbinafine tablets.
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Terbinafine tablets may affect the way other medicines work and other medicines may affect how terbinafine tablet works. Especially tell your doctor if you take:
- a medicine for depression
- a medicine for high blood pressure
- a medicine for heart problems
- desipramine (Norpramin)
- caffeine
- cyclosporine (Gengraf, Neoral, Sandimmune)
- fluconazole (Diflucan)
- rifampin (Rifater, Rifamate, Rimactane, Rifadine)
- cimetidine (Tagamet)
If you are not sure if your medicine is one listed above, ask your doctor or pharmacist.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take terbinafine tablets?
- Take terbinafine tablets exactly as your doctor tells you to take it.
- Terbinafine tablets comes as a tablet that you take by mouth.
- Terbinafine tablets is usually taken:
- 1 time each day for 6 weeks to treat fungal infections of your fingernail, or
- 1 time each day for 12 weeks to treat fungal infections of your toenail
- You can take terbinafine tablets with or without food.
- If you forget to take terbinafine tablets, take your tablets as soon as you remember, unless it is less than 4 hours before your next dose is due. In this case, wait and take your next dose at the usual time.
- If you take too much terbinafine tablets call your doctor. You may have the following symptoms:
- nausea • vomiting
- stomach (abdominal) pain • dizziness
- rash • frequent urination
- headache
What are the possible side effects of terbinafine tablets?
Terbinafine tablets may cause serious side effects, including:
• liver problems that can lead to the need for liver transplant, or death. Tell your doctor right away if you get any of these symptoms of a liver problem:
- nausea • upper right stomach (abdominal) pain
- poor appetite • yellowing of your skin or eyes (jaundice)
- tiredness • dark (tea-colored) urine
- vomiting • pale or light colored stools
Your doctor should do a blood test to check you for liver problems before you take terbinafine tablets.
• change in taste or loss of taste may happen with terbinafine tablets. This usually improves within several weeks after stopping terbinafine tablets, but may last for a long time or may become permanent. Tell your doctor if you have:
- change in taste or loss of taste
- poor appetite
- unwanted weight loss, or
- change in mood or depressive symptoms
- change in smell or loss of smell may happen with terbinafine tablets. This may improve after stopping terbinafine tablets, but may last for a long time or may become permanent.
• depressive symptoms. Tell your doctor right away if you have any of these signs or symptoms:
- feel sad or worthless
- change in sleep pattern
- loss of energy or interest in daily activities
- restlessness
- mood changes
- serious skin or allergic reactions. Tell your doctor right away or get emergency help if you get any of these symptoms:
skin rash, hives, sores in your mouth, or your skin blisters and peels
swelling of your face, eyes, lips, tongue or throat, trouble swallowing or breathing
• new or worsening lupus (an autoimmune disease). Stop taking terbinafine tablets and tell your doctor if you experience any of the following:
- progressive skin rash that is scaly, red, shows scarring, or loss of pigment
- unusual sensitivity to the sun that can lead to a rash
The most common side effects of terbinafine tablets include: headache, diarrhea, rash, dyspepsia, liver enzyme abnormalities, pruritus, taste disturbance, nausea, abdominal pain, and flatulence.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of terbinafine tablets. For information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects.
You may report side effects to FDA at 1-800-FDA-1088.
How do I Store terbinafine tablets?
• Store terbinafine tablets at 20°-25°C (68°-77°F).
• Keep terbinafine tablets in a tightly closed container and away from light.
Keep terbinafine tablets and all medicines out of the reach of children.
General information about the safe and effective use of terbinafine tablets.
Medicines are sometimes prescribed for purposes other than those listed in Patient Information. Do not use terbinafine tablets for a condition for which it was not prescribed. Do not give terbinafine tablets to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information summarizes the most important information about terbinafine tablets. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about terbinafine tablets that is written for health professionals.
What are the ingredients in terbinafine tablets?
Active ingredient: terbinafine hydrochloride.
Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose, magnesium stearate, microcrystalline cellulose. This Patient Information has been approved by the U.S. Food and Drug Administration.
To reorder additional patient information sheets, please contact Dr. Reddy’s Customer Service at 1-866-733-3952.
Rx Only
Manufactured by:
Dr. Reddy’s Laboratories Limited
Bachupally - 500 090 INDIA
Revised: 0812
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
Container label
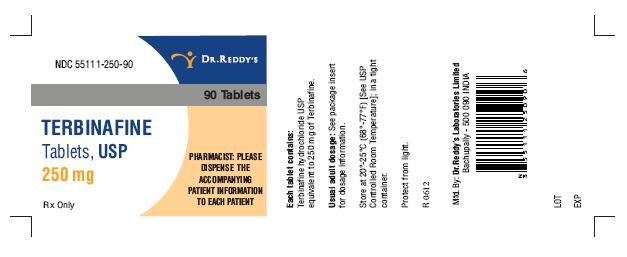
Terbinafine HydrochlorideTerbinafine Hydrochloride TABLET
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||