Tizanidine
Tizanidine Tablets USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- TIZANIDINE DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL STUDIES
- TIZANIDINE INDICATIONS AND USAGE
- TIZANIDINE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- TIZANIDINE ADVERSE REACTIONS
- OVERDOSAGE
- TIZANIDINE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
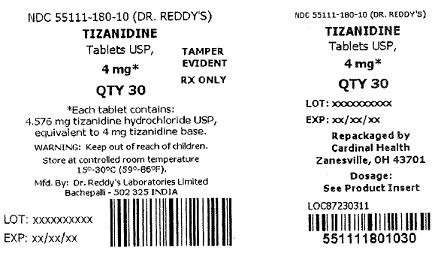
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
TIZANIDINE DESCRIPTION
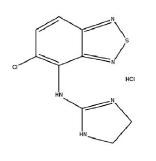
Tizanidine hydrochloride is a centrally acting α2-adrenergic agonist. Tizanidine HCl (tizanidine) is a white to off-white, fine crystalline powder, odorless or with a faint characteristic odor. Tizanidine is slightly soluble in water and methanol; solubility in water decreases as the pH increases. Its chemical name is 5-chloro-4-(2-imidazolin-2-ylamino)-2,1,3-benzothiodiazole hydrochloride. Tizanidine’s molecular formula is C9H8ClN5S.HCl, its molecular weight is 290.2 and its structural formula is:
Tizanidine hydrochloride is supplied as 2 mg and 4 mg tablets for oral administration. Tizanidine hydrochloride tablets are composed of the active ingredient, tizanidine hydrochloride (2.288 mg equivalent to 2 mg tizanidine base and 4.576 mg equivalent to 4 mg tizanidine base), and the inactive ingredients, anhydrous lactose, microcrystalline cellulose, colloidal silicon dioxide and stearic acid.
CLINICAL PHARMACOLOGY
Mechanism Of Action
Tizanidine is an agonist at α2-adrenergic receptor sites and presumably reduces spasticity by increasing presynaptic inhibition of motor neurons. In animal models, tizanidine has no direct effect on skeletal muscle fibers or the neuromuscular junction, and no major effect on monosynaptic spinal reflexes. The effects of tizanidine are greatest on polysynaptic pathways. The overall effect of these actions is thought to reduce facilitation of spinal motor neurons.
The imidazoline chemical structure of tizanidine is related to that of the antihypertensive drug clonidine and other α2-adrenergic agonists. Pharmacological studies in animals show similarities between the two compounds, but tizanidine was found to have one-tenth to one-fiftieth (1/50) of the potency of clonidine in lowering blood pressure.
PHARMACOKINETICS
Following oral administration, tizanidine is essentially completely absorbed and has a half-life of approximately 2.5 hours (coefficient of variation [CV] = 33%). Following administration of tizanidine, peak plasma concentrations occurred at 1.5 hours (CV = 40%) after dosing. Food increases Cmax by approximately one-third and shortens time to peak concentration by approximately 40 minutes, but the extent of tizanidine absorption is not affected. Tizanidine has linear pharmacokinetics over a dose of 1 to 20 mg. The absolute oral bioavailability of tizanidine is approximately 40% (CV = 24%), due to extensive first-pass metabolism in the liver; approximately 95% of an administered dose is metabolized. Tizanidine metabolites are not known to be active; their half-lives range from 20 to 40 hours. Tizanidine is widely distributed throughout the body; mean steady state volume of distribution is 2.4 L/kg (CV = 21 %) following intravenous administration in healthy adult volunteers.
Following single and multiple oral dosing of 14C-tizanidine, an average of 60% and 20% of total radioactivity was recovered in the urine and feces, respectively.
Tizanidine is approximately 30% bound to plasma proteins, independent of concentration over the therapeutic range.
SPECIAL POPULATIONS
Age Effects: No specific pharmacokinetic study was conducted to investigate age effects. Cross study comparison of pharmacokinetic data following single dose administration of 6 mg tizanidine showed that younger subjects cleared the drug four times faster than the elderly subjects. Tizanidine has not been evaluated in children (see PRECAUTIONS).
Hepatic Impairment: Pharmacokinetic differences due to hepatic impairment have not been studied (see WARNINGS).
Renal Impairment: Tizanidine clearance is reduced by more than 50% in elderly patients with renal insufficiency (creatinine clearance < 25 mL/min) compared to healthy elderly subjects; this would be expected to lead to a longer duration of clinical effect. Tizanidine should be used with caution in renally impaired patients (see PRECAUTIONS).
Gender Effects: No specific pharmacokinetic study was conducted to investigate gender effects. Retrospective analysis of pharmacokinetic data, however, following single and multiple dose administration of 4 mg tizanidine showed that gender had no effect on the pharmacokinetics of tizanidine.
Race Effects: Pharmacokinetic differences due to race have not been studied.
Drug Interactions - Oral Contraceptives: No specific pharmacokinetic study was conducted to investigate interaction between oral contraceptives and tizanidine. Retrospective analysis of population pharmacokinetic data following single and multiple dose administration of 4 mg tizanidine, however, showed that women concurrently taking oral contraceptives had 50% lower clearance of tizanidine compared to women not on oral contraceptives (see PRECAUTIONS).
CLINICAL STUDIES
Tizanidine’s capacity to reduce increased muscle tone associated with spasticity was demonstrated in two adequate and well controlled studies in patients with multiple sclerosis or spinal cord injury.
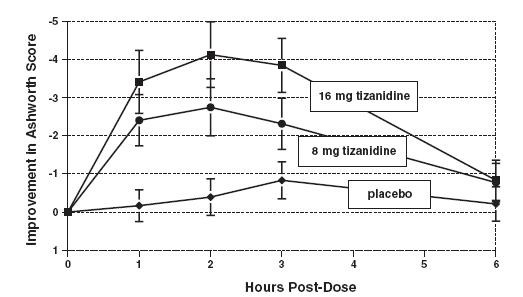
In one study, patients with multiple sclerosis were randomized to receive single oral doses of drug or placebo. Patients and assessors were blind to treatment assignment and efforts were made to reduce the likelihood that assessors would become aware indirectly of treatment assignment (e.g., they did not provide direct care to patients and were prohibited from asking questions about side effects). In all, 140 patients received either placebo, 8 mg or 16 mg of tizanidine.
Response was assessed by physical examination; muscle tone was rated on a 5 point scale (Ashworth score), with a score of 0 used to describe normal muscle tone. A score of 1 indicated a slight spastic catch while a score of 2 indicated more marked muscle resistance. A score of 3 was used to describe considerable increase in tone, making passive movement difficult. A muscle immobilized by spasticity was given a score of 4. Spasm counts were also collected.
Assessments were made at 1, 2, 3 and 6 hours after treatment. A statistically significant reduction of the Ashworth score for tizanidine compared to placebo was detected at 1, 2 and 3 hours after treatment. Figure 1 below shows a comparison of the mean change in muscle tone from baseline as measured by the Ashworth scale. The greatest reduction in muscle tone was 1 to 2 hours after treatment. By 6 hours after treatment, muscle tone in the 8 and 16 mg tizanidine groups was indistinguishable from muscle tone in placebo treated patients. Within a given patient, improvement in muscle tone was correlated with plasma concentration. Plasma concentrations were variable from patient to patient at a given dose. Although 16 mg produced a larger effect, adverse events including hypotension were more common and more severe than in the 8 mg group. There were no differences in the number of spasms occuring in each group.
FIGURE 1: Single Dose Study - Mean Change in Muscle Tone from Baseline as Measured by the Ashworth Scale ± 95% Confidence Interval (A Negative Ashworth Score Signifies an Improvement in Muscle Tone from Baseline)
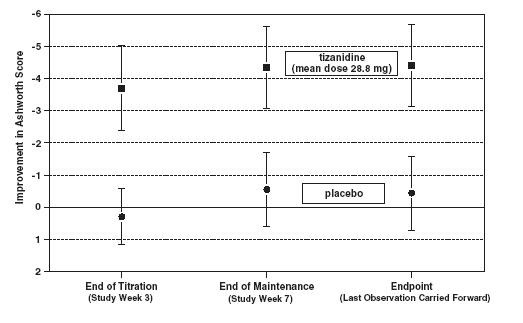
In a multiple dose study, 118 patients with spasticity secondary to spinal cord injury were randomized to either placebo or tizanidine. Steps similar to those taken in the first study were employed to ensure the integrity of blinding.
Patients were titrated over 3 weeks up to a maximum tolerated dose or 36 mg daily given in three unequal doses (e.g., 10 mg given in the morning and afternoon and 16 mg given at night). Patients were then maintained on their maximally tolerated dose for 4 additional weeks (i.e., maintenance phase). Throughout the maintenance phase, muscle tone was assessed on the Ashworth scale within a period of 2.5 hours following either the morning or afternoon dose. The number of daytime spasms was recorded daily by patients.
At endpoint (the protocol-specified time of outcome assessment), there was a statistically significant reduction in muscle tone and frequency of spasms in the tizanidine treated group compared to placebo. The reduction in muscle tone was not associated with a reduction in muscle strength (a desirable outcome) but also did not lead to any consistent advantage of tizanidine treated patients on measures of activities of daily living. Figure 2 below shows a comparison of the mean change in muscle tone from baseline as measured by the Ashworth scale.
FIGURE 2: Multiple Dose Study - Mean Change in Muscle Tone 0.5-2.5 Hours after Dosing as Measured by the Ashworth Scale +/- 95% Confidence Interval (A Negative Ashworth Score Signifies an Improvement in Muscle Tone from Baseline)
TIZANIDINE INDICATIONS AND USAGE
Tizanidine is a short-acting drug for the management of spasticity. Because of the short duration of effect, treatment with tizanidine should be reserved for those daily activities and times when relief of spasticity is most important (see DOSAGE AND ADMINISTRATION)
TIZANIDINE CONTRAINDICATIONS
Tizanidine is contraindicated in patients with known hypersensitivity to tizanidine or its ingredients.
WARNINGS
LIMITED DATA BASE FOR CHRONIC USE OF SINGLE DOSES ABOVE 8 MG AND MULTIPLE DOSES ABOVE 24 MG PER DAY
Clinical experience with long-term use of tizanidine at doses of 8 to 16 mg single doses or total daily doses of 24 to 36 mg (see DOSAGE AND ADMINISTRATION) is limited. Approximately 75 patients have been exposed to individual doses of 12 mg or more for at least one year or more and approximately 80 patients have been exposed to total daily doses of 30 to 36 mg/day for at least one year or more. There is essentially no long-term experience with single, daytime doses of 16 mg. Because long-term clinical study experience at high doses is limited, only those adverse events with a relatively high incidence are likely to have been identified (see WARNINGS, PRECAUTIONS AND ADVERSE REACTIONS).
HYPOTENSION
Tizanidine is an α2-adrenergic agonist (like clonidine) and can produce hypotension. In a single dose study where blood pressure was monitored closely after dosing, two-thirds of patients treated with 8 mg of tizanidine had a 20% reduction in either the diastolic or systolic BP. The reduction was seen within 1 hour after dosing, peaked 2 to 3 hours after dosing and was associated, at times, with bradycardia, orthostatic hypotension, lightheadedness/ dizziness and rarely syncope. The hypotensive effect is dose related and has been measured following single doses of ≥ 2 mg.
The chance of significant hypotension may possibly be minimized by titration of the dose and by focusing attention on signs and symptoms of hypotension prior to dose advancement. In addition, patients moving from a supine to a fixed upright position may be at increased risk for hypotension and orthostatic effects.
Caution is advised when tizanidine is to be used in patients receiving concurrent antihypertensive therapy and should not be used with other α2-adrenergic agonists.
RISK OF LIVER INJURY
Tizanidine occasionally causes liver injury, most often hepatocellular in type. In controlled clinical studies, approximately 5% of patients treated with tizanidine had elevations of liver function tests (ALT/SGPT, AST/SGOT) to greater than 3 times the upper limit of normal (or 2 times if baseline levels were elevated) compared to 0.4% in the control patients. Most cases resolved rapidly upon drug withdrawal with no reported residual problems. In occasional symptomatic cases, nausea, vomiting, anorexia and jaundice have been reported. In postmarketing experience, three deaths associated with liver failure have been reported in patients treated with tizanidine. In one case, a 49 year old male developed jaundice and liver enlargement following 2 months of tizanidine treatment, primarily at 6 mg tid. A liver biopsy showed multilobular necrosis without eosinophilic infiltration. Treatment was discontinued and the patient died in hepatic coma 10 days later. There was no evidence of hepatitis B and C in this patient and other therapy included only oxazepam and ranitidine. There was thus no explanation, other than a reaction to tizanidine, to explain the liver injury. In the two other cases, patients were taking other drugs with known potential for liver toxicity. One patient, treated with tizanidine at a dose of 4 mg/day, was also on carbamazepine when he developed cholestatic jaundice after 2 months of treatment; this patient died with pneumonia about 20 days later. Another patient, treated with tizanidine for 11 days, was also treated with dantrolene for about 2 weeks prior to developing fatal fulminant hepatic failure.
Monitoring of aminotransferase levels is recommended during the first 6 months of treatment (e.g., baseline, 1, 3 and 6 months) and periodically thereafter, based on clinical status. Because of the potential toxic hepatic effect of tizanidine, the drug should be used only with extreme caution in patients with impaired hepatic function.
SEDATION
In the multiple dose, controlled clinical studies, 48% of patients receiving any dose of tizanidine reported sedation as an adverse event. In 10% of these cases, the sedation was rated as severe compared to <1% in the placebo treated patients. Sedation may interfere with everyday activity.
The effect appears to be dose related. In a single dose study, 92% of the patients receiving 16 mg, when asked, reported that they were drowsy during the 6 hour study. This compares to 76% of the patients on 8 mg and 35% of the patients on placebo. Patients began noting this effect 30 minutes following dosing. The effect peaked 1.5 hours following dosing. Of the patients who received a single dose of 16 mg, 51% continued to report drowsiness 6 hours following dosing compared to 13% in the patients receiving placebo or 8 mg of tizanidine.
In the multiple dose studies, the prevalence of patients with sedation peaked following the first week of titration and then remained stable for the duration of the maintenance phase of the study.
HALLUCINOSIS/PSYCHOTIC-LIKE SYMPTOMS
Tizanidine use has been associated with hallucinations. Formed, visual hallucinations or delusions have been reported in 5 of 170 patients (3%) in two North American controlled clinical studies. These 5 cases occurred within the first 6 weeks. Most of the patients were aware that the events were unreal. One patient developed psychoses in association with the hallucinations. One patient among these 5 continued to have problems for at least 2 weeks following discontinuation of tizanidine.
PRECAUTIONS
CARDIOVASCULAR
Prolongation of the QT interval and bradycardia were noted in chronic toxicity studies in dogs at doses equal to the maximum human dose on a mg/m2 basis. ECG evaluation was not performed in the controlled clinical studies. Reduction in pulse rate has been noted in association with decreases in blood pressure in the single dose controlled study (see WARNINGS).
OPHTHALMIC
Dose-related retinal degeneration and corneal opacities have been found in animal studies at doses equivalent to approximately the maximum recommended dose on a mg/m2 basis. There have been no reports of corneal opacities or retinal degeneration in the clinical studies.
USE IN RENALLY IMPAIRED PATIENTS
Tizanidine should be used with caution in patients with renal insufficiency (creatinine clearance < 25 mL/min), as clearance is reduced by more than 50%. In these patients, during titration, the individual doses should be reduced, If higher doses are required, individual doses rather than dosing frequency should be increased. These patients should be monitored closely for the onset or increase in severity of the common adverse events (dry mouth, somnolence, asthenia and dizziness) as indicators of potential overdose.
USE IN WOMEN TAKING ORAL CONTRACEPTIVES
Tizanidine should be used with caution in women taking oral contraceptives, as clearance of tizanidine is reduced by approximately 50% in such patients. In these patients, during titration, the individual doses should be reduced.
INFORMATION FOR PATIENTS
Patients should be advised of the limited clinical experience with tizanidine both in regard to duration of use and the higher doses required to reduce muscle tone (see WARNINGS).
Because of the possibility of tizanidine lowering blood pressure, patients should be warned about the risk of clinically significant orthostatic hypotension (see WARNINGS).
Because of the possibility of sedation, patients should be warned about performing activities requiring alertness, such as driving a vehicle or operating machinery (see WARNINGS). Patients should also be instructed that the sedation may be additive when tizanidine is taken in conjunction with drugs (baclofen, benzodiazepines) or substances (e.g., alcohol) that act as CNS depressants.
Tizanidine should be used with caution where spasticity is utilized to sustain posture and balance in locomotion or whenever spasticity is utilized to obtain increased function.
Drug Interactions
In vitro studies of cytochrome P450 isoenzymes using human liver microsomes indicate that neither tizanidine nor the major metabolites are likely to affect the metabolism of other drugs metabolized by cytochrome P450 isoenzymes.
Acetaminophen: Tizanidine delayed the Tmax of acetaminophen by 16 minutes. Acetaminophen did not affect the pharmacokinetics of tizanidine.
Alcohol: Alcohol increased the AUC of tizanidine by approximately 20% while also increasing its Cmax by approximately 15%. This was associated with an increase in side effects of tizanidine. The CNS depressant effects of tizanidine and alcohol are additive.
Oral Contraceptives: No specific pharmacokinetic study was conducted to investigate interaction between oral contraceptives and tizanidine, but retrospective analysis of population pharmacokinetic data following single and multiple dose administration of 4 mg tizanidine showed that women concurrently taking oral contraceptives had 50% lower clearance of tizanidine than women not on oral contraceptives.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence for carcinogenicity was seen in two dietary studies in rodents. Tizanidine was administered to mice for 78 weeks at doses up to 16 mg/kg, which is equivalent to 2 times the maximum recommended human dose on a mg/m2 basis. Tizanidine was also administered to rats for 104 weeks at doses up to 9 mg/kg, which is equivalent to 2.5 times the maximum recommended human dose on a mg/m2 basis. There was no statistically significant increase in tumors in either species.
Tizanidine was not mutagenic or clastogenic in the following in vitro assays: the bacterial Ames test and the mammalian gene mutation test and chromosomal aberration test in Chinese hamster cells. It was also negative in the following in vivo assays: the bone marrow micronucleus test in mice, the bone marrow micronucleus and cytogenicity test in Chinese hamsters, the dominant lethal mutagenicity test in mice, and the unscheduled DNA synthesis (UDS) test in mice.
Tizanidine did not affect fertility in male rats at doses of 10 mg/kg, approximately 2.7 times the maximum recommended human dose on a mg/m2 basis, and in females at doses of 3 mg/kg, approximately equal to the maximum recommended human dose on a mg/m2 basis; fertility was reduced in males receiving 30 mg/kg (8 times the maximum recommended human dose on a mg/m2 basis) and in females receiving 10 mg/kg (2.7 times the maximum recommended human dose on a mg/m2 basis). At these doses, maternal behavioral effects and clinical signs were observed including marked sedation, weight loss, and ataxia.
Pregnancy
Pregnancy Category C: Reproduction studies performed in rats at a dose of 3 mg/kg, equal to the maximum recommended human dose on a mg/m2 basis, and in rabbits at 30 mg/kg, 16 times the maximum recommended human dose on a mg/m2 basis, did not show evidence of teratogenicity. Tizanidine at doses that are equal to and up to 8 times the maximum recommended human dose on a mg/m2 basis increased gestation duration in rats. Prenatal and postnatal pup loss was increased and developmental retardation occurred. Postimplantation loss was increased in rabbits at doses of 1 mg/kg or greater, equal to or greater than 0.5 times the maximum recommended human dose on a mg/m2 basis. Tizanidine has not been studied in pregnant women. Tizanidine should be given to pregnant women only if clearly needed.
LABOR AND DELIVERY
The effect of tizanidine on labor and delivery in humans is unknown.
Nursing Mothers
It is not known whether tizanidine is excreted in human milk, although as a lipid soluble drug, it might be expected to pass into breast milk.
Geriatric Use
Tizanidine should be used with caution in elderly patients because clearance is decreased four-fold.
PEDIATRIC USE
There are no adequate and well-controlled studies to document the safety and efficacy of tizanidine in children.
TIZANIDINE ADVERSE REACTIONS
In multiple dose, placebo-controlled clinical studies, 264 patients were treated with tizanidine and 261 with placebo. Adverse events, including severe adverse events, were more frequently reported with tizanidine than with placebo.
COMMON ADVERSE EVENTS LEADING TO DISCONTINUATION
Forty-five of 264 (17%) patients receiving tizanidine and 13 of 261 (5%) patients receiving placebo in three multiple dose, placebo-controlled clinical studies discontinued treatment for adverse events. When patients withdrew from the study, they frequently had more than one reason for discontinuing. The adverse events most frequently leading to withdrawal of tizanidine treated patients in the controlled clinical studies were asthenia (weakness, fatigue and/or tiredness) (3%), somnolence (3%), dry mouth (3%), increased spasm or tone (2%) and dizziness (2%).
MOST FREQUENT ADVERSE CLINICAL EVENTS SEEN IN ASSOCIATION WITH THE USE OF TIZANIDINE
In multiple dose, placebo-controlled clinical studies involving 264 patients with spasticity, the most frequent adverse events were dry mouth, somnolence/sedation, asthenia (weakness, fatigue and/or tiredness) and dizziness. Three-quarters of the patients rated the events as mild to moderate and one-quarter of the patients rated the events as being severe. These events appeared to be dose related.
ADVERSE EVENTS REPORTED IN CONTROLLED STUDIES
The events cited reflect experience gained under closely monitored conditions of clinical studies in a highly selected patient population. In actual clinical practice or in other clinical studies, these frequency estimates may not apply, as the conditions of use, reporting behavior, and the kinds of patients treated may differ. Table 1 lists treatment emergent signs and symptoms that were reported in greater than 2% of patients in three multiple dose, placebo-controlled studies who received tizanidine where the frequency in the tizanidine group was at least as common as in the placebo group. These events are not necessarily related to tizanidine treatment. For comparison purposes, the corresponding frequency of the event (per 100 patients) among placebo treated patients is also provided.
| Event | Placebo N =261 % |
Tizanidine N =264 % |
| Dry mouth | 10 | 49 |
| Somnolence | 10 | 48 |
| Asthenia* | 16 | 41 |
| Dizziness | 4 | 16 |
| UTI | 7 | 10 |
| Infection | 5 | 6 |
| Constipation | 1 | 4 |
| Liver function tests abnormal | <1 | 3 |
| Vomiting | 0 | 3 |
| Speech disorder | 0 | 3 |
| Amblyopia (blurred vision) | <1 | 3 |
| Urinary frequency | 2 | 3 |
| Flu syndrom | 2 | 3 |
| SGPT/ALT increased | <1 | 3 |
| Dyskinesia | 0 | 3 |
| Nervousness | <1 | 3 |
| Pharyngitis | 1 | 3 |
| Rhinitis | 2 | 3 |
In the single dose, placebo-controlled study involving 142 patients with spasticity, the patients were specifically asked if they had experienced any of the four most common adverse events: dry mouth, somnolence (drowsiness), asthenia (weakness, fatigue and/or tiredness) and dizziness. In addition, hypotension and bradycardia were observed. The occurrence of these adverse events are summarized in Table 2. Other events were, in general, reported at a rate of 2% or less.
| Event | Placebo N =48 % |
Tizanidine 8 mg, N =45 % |
Tizanidine 16 mg, N =49 % |
| Somnolence | 31 | 78 | 92 |
| Dry mouth | 35 | 76 | 88 |
| Asthenia * | 40 | 67 | 78 |
| Dizziness | 4 | 22 | 45 |
| Hypotension | 0 | 16 | 33 |
| Bradycardia | 0 | 2 | 10 |
* (weakness, fatigue and/or tiredness)
OTHER ADVERSE EVENTS OBSERVED DURING THE EVALUATION OF TIZANIDINE
Tizanidine was administered to 1187 patients in additional clinical studies where adverse event information was available. The conditions and duration of exposure varied greatly, and included (in overlapping categories) double-blind and open-label studies, uncontrolled and controlled studies, inpatient and outpatient studies, and titration studies. Untoward events associated with this exposure were recorded by clinical investigators using terminology of their own choosing. Consequently, it is not possible to provide a meaningful estimate of the proportion of individuals experiencing adverse events without first grouping similar types of untoward events into a smaller number of standardized event categories.
In the tabulations that follow, reported adverse events were classified using a standard COSTART-based dictionary terminology. The frequencies presented, therefore, represent the proportion of the 1187 patients exposed to tizanidine who experienced an event of the type cited on at least one occasion while receiving tizanidine. All reported events are included except those already listed in Table 1. If the COSTART term for an event was so general as to be uninformative, it was replaced with a more informative term. It is important, to emphasize that, although the events reported occurred during treatment with tizanidine, they were not necessarily caused by it.
Events are further categorized by body system and listed in order of decreasing frequency according to the following definitions: frequent adverse events are those occurring on one or more occasions in at least 1/100 patients (only those not already listed in the tabulated results from placebo-controlled studies appear in this listing); infrequent adverse events are those occurring in 1/100 to 1/1000 patients.
BODY AS A WHOLE: Frequent: fever; Infrequent: allergic reaction, moniliasis, malaise, abscess, neck pain, sepsis, cellulitis, death, overdose; Rare: carcinoma, congenital anomaly, suicide attempt.
CARDIOVASCULAR SYSTEM: Infrequent: vasodilatation, postural hypotension, syncope, migraine, arrhythmia; Rare: angina pectoris, coronary artery disorder, heart failure, myocardial infarct, phlebitis, pulmonary embolus, ventricular extrasystoles, ventricular tachycardia.
DIGESTIVE SYSTEM: Frequent: abdomen pain, diarrhea, dyspepsia; Infrequent: dysphagia, cholelithiasis, fecal impaction, flatulence, gastrointestinal hemorrhage, hepatitis, melena; Rare: gastroenteritis, hematemesis, hepatoma, intestinal obstruction, liver damage.
HEMIC AND LYMPHATIC SYSTEM: Infrequent: ecchymosis, hypercholesteremia, anemia, hyperlipemia, leukopenia, leukocytosis, sepsis; Rare: petechia, purpura, thrombocythemia, thrombocytopenia.
METABOLIC AND NUTRITIONAL SYSTEM: Infrequent: edema, hypothyroidism, weight loss; Rare: adrenal cortex insufficiency, hyperglycemia, hypokalemia, hyponatremia, hypoproteinemia, respiratory acidosis.
MUSCULOSKELETAL SYSTEM: Frequent: myasthenia, back pain; Infrequent: pathological fracture, arthralgia, arthritis, bursitis.
NERVOUS SYSTEM: Frequent: depression, anxiety, paresthesia; Infrequent: tremor, emotional lability, convulsion, paralysis, thinking abnormal, vertigo, abnormal dreams, agitation, depersonalization, euphoria, migraine, stupor, dysautonomia, neuralgia; Rare: dementia, hemiplegia, neuropathy.
RESPIRATORY SYSTEM: Infrequent: sinusitis, pneumonia, bronchitis; Rare: asthma.
SKIN AND APPENDAGES: Frequent: rash, sweating, skin ulcer; Infrequent: pruritus, dry skin, acne, alopecia, urticaria; Rare: exfoliative dermatitis, herpes simplex, herpes zoster, skin carcinoma.
SPECIAL SENSES: Infrequent: ear pain, tinnitus, deafness, glaucoma, conjunctivitis, eye pain, optic neuritis, otitis media, retinal hemorrhage, visual field defect; Rare: iritis, keratitis, optic atrophy.
UROGENITAL SYSTEM: Infrequent: urinary urgency, cystitis, menorrhagia, pyelonephritis, urinary retention, kidney calculus, uterine fibroids enlarged, vaginal moniliasis, vaginitis; Rare: albuminuria, glycosuria, hematuria, metrorrhagia.
DRUG ABUSE AND DEPENDENCE
Abuse potential was not evaluated in human studies. Rats were able to distinguish tizanidine from saline in a standard discrimination paradigm, after training, but failed to generalize the effects of morphine, cocaine, diazepam or phenobarbital to tizanidine. Monkeys were shown to self-administer tizanidine in a dose-dependent manner, and abrupt cessation of tizanidine produced transient signs of withdrawal at doses > 35 times the maximum recommended human dose on a mg/m2 basis. These transient withdrawal signs (increased locomotion, body twitching, and aversive behavior toward the observer) were not reversed by naloxone administration.
OVERDOSAGE
One significant overdosage of tizanidine has been reported. Attempted suicide by a 46 year-old male with multiple sclerosis resulted in coma very shortly after the ingestion of one-hundred 4 mg tizanidine tablets. Pupils were not dilated and nystagmus was not present. The patient had marked respiratory depression with Cheyne-Stokes respiration. Gastric lavage and forced diuresis with furosemide and mannitol were instituted. The patient recovered several hours later without sequelae. Laboratory findings were normal.
Should overdosage occur, basic steps to ensure the adequacy of an airway and the monitoring of cardiovascular and respiratory systems should be undertaken. For the most recent information concerning the management of overdose, contact a poison control center.
TIZANIDINE DOSAGE AND ADMINISTRATION
A single oral dose of 8 mg of tizanidine reduces muscle tone in patients with spasticity for a period of several hours. The effect peaks at approximately 1 to 2 hours and dissipates between 3 to 6 hours. Effects are dose-related.
Although single doses of less than 8 mg have not been demonstrated to be effective in controlled clinical studies, the dose-related nature of tizanidine's common adverse events make it prudent to begin treatment with single oral doses of 4 mg. Increase the dose gradually (2 to 4 mg steps) to optimum effect (satisfactory reduction of muscle tone at a tolerated dose).
The dose can be repeated at 6 to 8 hour intervals, as needed, to a maximum of three doses in 24 hours. The total daily dose should not exceed 36 mg.
Experience with single doses exceeding 8 mg and daily doses exceeding 24 mg is limited. There is essentially no experience with repeated, single, daytime doses greater than 12 mg or total daily doses greater than 36 mg (see WARNINGS).
HOW SUPPLIED
Tizanidine hydrochloride Tablets 2 mg are white to off white, oval, flat, beveled edged tablets embossed with "R179" on one side and "bisecting score" on other side. The tablets are available in bottles of 30,150, 300 and 1000.
Bottles of 30 NDC 55111-179-30
Bottles of 150 NDC 55111-179-15
Bottles of 300 NDC 55111-179-03
Bottles of 1000 NDC 55111-179-10
Tizanidine hydrochloride Tablets 4 mg are white to off white, oval, flat, beveled edged tablets embossed with "R180" on one side and "quadrisecting score" on other side. The tablets are available in bottles of 30,150, 300 and 1000.
Bottles of 30 NDC 55111-180-30
Bottles of 150 NDC 55111-180-15
Bottles of 300 NDC 55111-180-03
Bottles of 1000 NDC 55111-180-10
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP Controlled Room Temperature]. Dispense in containers with child resistant closure.
Rx Only
1514065
Manufactured by:
Dr. Reddy’s Laboratories Limited
Bachepalli – 502 325 INDIA
Revised: 0706
Dr. Reddy’s
Tizanidine hydrochloride Tablets 4 mg are available from Cardinal Health in unit dose cartons of 30.
Cardinal Health
Zanesville, OH 43701
OI87231010
PRINCIPAL DISPLAY PANEL
Tizanidine
Tablets USP,
4 mg
PRINCIPAL DISPLAY PANEL
Tizanidine
Tablets, USP
4 mg
QTY 30
TizanidineTizanidine TABLET
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||