Tretinoin
FULL PRESCRIBING INFORMATION
FOR TOPICAL USE ONLY
Rx Only
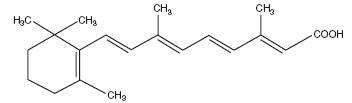
Tretinoin Cream, a topical retinoid, contains tretinoin 0.025% by weight in a hydrophilic cream vehicle of stearic acid, polyolprepolymer-2, isopropyl myristate, polyoxyl 40 stearate, propylene glycol, stearyl alcohol, xanthan gum, sorbic acid, butylated hydroxytoluene, and purified water. Chemically, tretinoin is all-transretinoic acid (C20H2802; molecular weight 300.44 vitamin A acid) and has the following structural formula:
Although the exact mode of action of tretinoin is unknown, current evidence suggests that topical tretinoin decreases cohesiveness of follicular epithelial cells with decreased microcomedo formation. Additionally, tretinoin stimulates mitotic activity and increased turnover of follicular epithelial cells causing extrusion of the comedones.
In vitro and in vivo pharmacokinetic studies with tretinoin cream indicate that less than 0.3% of the topically applied dose is bioavailable. Circulating plasma levels of both tretinoin and isotretinoin are only slightly elevated above those found in healthy normal controls.
In one vehicle-controlled clinical trial, tretinoin cream 0.025% applied once daily was more effective than vehicle in the treatment of facial acne vulgaris of mild to moderate severity. Percent reductions in lesion count after treatment for 12 weeks in this study are shown in the following table:
| TretinoinCream, | Vehicle | |
| 0.025% | Cream | |
| N = Number of Subjects | ||
| N = 75 | N = 58 | |
| Noninflammatory Lesions | 45% | 27% |
| Inflammatory Lesions | 46% | 32% |
| Total Lesions | 46% | 28% |
Tretinoin cream is indicated for topical application in the treatment of acne vulgaris. The safety and efficacy of this product in the treatment of other disorders have not been established.
The product should not be used if there is hypersensitivity to any of the ingredients.
If a reaction suggesting sensitivity or chemical irritation occurs, use of the medication should be discontinued. Exposure to sunlight, including sunlamps, should be minimized during the use of tretinoin cream, and patients with sunburn should be advised not to use the product until fully recovered because of heightened susceptibility to sunlight as a result of the use of tretinoin. Patients who may be required to have considerable sun exposure due to occupation and those with inherent sensitivity to the sun should exercise particular caution. Use of sunscreen products and protective clothing over treated areas is recommended when exposure cannot be avoided. Weather extremes, such as wind or cold, also may be irritating to patients under treatment with tretinoin.
Tretinoin cream, 0.025% should be kept away from the eyes, the mouth, the paranasal creases, and mucous membranes. Topical use may induce severe local erythema and peeling at the site of application. If the degree of local irritation warrants, patients should be directed to temporarily use the medication less frequently, discontinue use temporarily, or discontinue use altogether. Efficacy at reduced frequencies of application has not been established. Tretinoin has been reported to cause severe irritation on eczematous skin and should be used with utmost caution in patients with this condition.
See attached Patient Package Insert.
Concomitant topical medication, medicated or abrasive soaps and cleansers, soaps and cosmetics that have a strong drying effect, and products with high concentrations of alcohol, astringents, spices or lime should be used with caution because of possible interaction with tretinoin. Particular caution should be exercised in using preparations containing sulfur, resorcinol, or salicylic acid with tretinoin cream. It also is advisable to “rest” a patient’s skin until the effects of such preparations subside before use of tretinoin cream is begun.
In a life-time dermal study in CD-1 mice with another tretinoin cream, at 100 and 200 times the average recommended human topical clinical dose, a few skin tumors in the female mice and liver tumors in male mice were observed. The biological significance of these findings is not clear because they occurred at doses that exceeded the dermal maximally tolerated dose (MTD) of tretinoin and because they were within the background natural occurrence rate for these tumors in this strain of mice. There was no evidence of carcinogenic potential when tretinoin was administered topically at a dose five times the average recommended human topical clinical dose. For purposes of comparisons of the animal exposure to human exposure, the “recommended human topical clinical dose” is defined as 1.0 g of 0.025% tretinoin cream applied daily to a 50 kg person. In a chronic, two-year bioassay of vitamin A acid in mice performed by Tsubura and Yamamoto, generalized amyloid deposition was reported in all vitamin A treated groups in the basal layer of the skin. In CD-1 mice, a similar study reported hyalinization at the treated skin sites and the incidence of this finding was 0/50, 3/50, 3/50, and 2/50 in male mice and 1/50, 0/50, 4/50, and 2/50 in female mice from the vehicle control, 0.25 mg/kg, 0.5 mg/kg, and 1 mg/kg groups, respectively.
Studies in hairless albino mice suggest that tretinoin may enhance the tumorigenic potential of carcinogenic doses of UVB and UVA light from a solar simulator. In other studies, when lightly pigmented hairless mice treated with tretinoin were exposed to carcinogenic doses of UVA/UVB light, the incidence and rate of development of skin tumors were either reduced or no effect was seen. Due to significantly different experimental conditions, no strict comparison of these disparate data is possible at this time. Although the significance of these studies to humans is not clear, patients should minimize exposure to sun.
The mutagenic potential of tretinoin was evaluated in the Ames assay and in the in vivo mouse micronucleus assay, both of which were negative.
Dermal Segment I and III studies with tretinoin cream have not been performed in any species. In oral Segment I and Segment III studies in rats with tretinoin, decreased survival of neonates and growth retardation were observed at doses in excess of 2 mg/kg/day (> 400 times the average recommended human topical clinical dose).
Pregnancy Category C.
Oral tretinoin has been shown to be teratogenic in rats, mice, rabbits, hamsters, and subhuman primates. It was teratogenic and fetotoxic in rats when given orally in doses 1000 times the average recommended human topical clinical dose. However, variations in teratogenic doses among various strains of rats have been reported. In the cynomolgus monkey, which metabolically is closer to humans for tretinoin than other species examined, fetal malformations were reported at oral doses of 10 mg/kg/day or greater, but none were observed at 5 mg/kg/day (1000 times the average recommended human topical clinical dose), although increased skeletal variations were observed at all doses. Dose-related increased embryolethality and abortion were reported. Similar results have also been reported in pigtail macaques.
Topical tretinoin in animal teratogenicity tests has generated equivocal results. There is evidence for teratogenicity (shortened or kinked tail) of topical tretinoin in Wistar rats at doses greater than 1 mg/kg/day (200 times the recommended human topical clinical dose). Anomalies (humerus: short 13%, bent 6%; os parietal incompletely ossified 14%) have also been reported in rats when 10 mg/kg/day was dermally applied.
Topical tretinoin (Tretinoin Cream, 0.1%) has been shown to be teratogenic in rabbits when given in doses 91 times the topical human dose for cream (assuming a 50 kg adult applies 1.0 g of 0.1% cream topically). In this study, increased incidence of cleft palate and hydrocephaly was reported in the tretinoin-treated animals.
There are other reports, in New Zealand White rabbits with doses of approximately 80 times the recommended human topical clinical dose, of an increased incidence of domed head and hydrocephaly, typical of retinoid-induced fetal malformations in this species.
When given subcutaneously to rabbits, tretinoin was teratogenic at 2 mg/kg/day but not at 1 mg/kg/day. These doses are approximately 400 and 200 times, respectively, the human topical dose of tretinoin cream, 0.025% (assuming a 50 kg adult applies 1.0 g of 0.025% cream topically).
In contrast, several well-controlled animal studies have shown that dermally applied tretinoin was not teratogenic at doses of 100 and 200 times the recommended human topical clinical dose, in rats and rabbits, respectively.
With widespread use of any drug, a small number of birth defect reports associated temporally with the administration of the drug would be expected by chance alone. Thirty cases of temporally associated congenital malformations have been reported during two decades of clinical use of another formulation of topical tretinoin (Retin-A). Although no definite pattern of teratogenicity and no causal association have been established from these cases, five of the reports describe the rare birth defect category, holoprosencephaly (defects associated with incomplete midline development of the forebrain). The significance of these spontaneous reports in terms of risk to the fetus is not known.
Dermal tretinoin has been shown to be fetotoxic in rabbits when administered in doses 100 times the recommended topical human clinical dose. Oral tretinoin has been shown to be fetotoxic in rats when administered in doses 500 times the recommended topical human clinical dose. There are, however, no adequate and well-controlled studies in pregnant women. Tretinoin Cream, 0.025% should not be used during pregnancy.
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when tretinoin cream is administered to a nursing woman.
The skin of certain sensitive individuals may become excessively red, edematous, blistered, or crusted. If these effects occur, the medication should either be discontinued until the integrity of the skin is restored, or the medication dosing frequency should be adjusted temporarily to a level the patient can tolerate. However, efficacy has not been established for lower dosing frequencies. True contact allergy to topical tretinoin is rarely encountered. Temporary hyper- or hypopigmentation has been reported with repeated application of tretinoin cream. Some individuals have been reported to have heightened susceptibility to sunlight while under treatment with tretinoin cream. Adverse effects of tretinoin cream have been reversible upon discontinuation of therapy (see DOSAGE AND ADMINISTRATION section).
If medication is applied excessively, no more rapid or better results will be obtained and marked redness, peeling, or discomfort may occur. Oral ingestion of the drug may lead to the same side effects as those associated with excessive oral intake of vitamin A.
Tretinoin Cream should be applied once a day, in the evening, to the skin where acne lesions appear, using enough to cover the entire affected area lightly. Application may cause a transient feeling of warmth or slight stinging. In cases where it has been necessary to temporarily discontinue therapy or reduce the frequency of application, therapy may be resumed or frequency of application increased when the patients become able to tolerate the treatment. Alterations of dose frequency should be closely monitored by careful observation of the clinical therapeutic response and skin tolerance. Efficacy has not been established for less than once-daily dosing frequencies.
During the early weeks of therapy, an apparent increase in number and exacerbation of inflammatory acne lesions may occur. This is due, in part, to the action of the medication on deep, previously unseen lesions and should not be considered a reason to discontinue therapy. Therapeutic results should be noticed after two to three weeks but more than six weeks of therapy may be required before definite beneficial effects are seen.
Patients treated with tretinoin cream may use cosmetics, but the areas to be treated should be cleansed thoroughly before the medication is applied (see PRECAUTIONS section).
Tretinoin Cream 0.025% is supplied in 20 g (NDC 0472-0117-20) and 45 g (NDC 0472-0117-45) tubes.
Storage Conditions: Store below 30°C (86°F). Avoid freezing.
Keep this and all medications out of the reach of children.
Manufactured by:
Actavis Mid Atlantic LLC
1877 Kawai Road
Lincolnton, NC 28092 USA
FORM NO. 0117
Rev. 9/13
VC4135
TRETINOIN CREAM USP 0.025%
Acne Treatment
IMPORTANT
Read Directions Carefully Before Using
THIS LEAFLET TELLS YOU ABOUT TRETINOIN CREAM ACNE TREATMENT AS PRESCRIBED BY YOUR PHYSICIAN. THIS PRODUCT IS TO BE USED ONLY ACCORDING TO YOUR DOCTOR’S INSTRUCTIONS, AND IT SHOULD NOT BE APPLIED TO OTHER AREAS OF THE BODY OR TO OTHER GROWTHS OR LESIONS. THE SAFETY AND EFFECTIVENESS OF THIS PRODUCT IN OTHER DISORDERS HAVE NOT BEEN EVALUATED. IF YOU HAVE ANY QUESTIONS, BE SURE TO ASK YOUR DOCTOR.
PRECAUTIONS
The effects of the sun on your skin: As you know, overexposure to natural sunlight or the artificial sunlight of a sunlamp can cause sunburn. Overexposure to the sun over many years may cause premature aging of the skin and even skin cancer. The chances of these effects occurring will vary depending on skin type, the climate and the care taken to avoid overexposure to the sun. Therapy with tretinoin cream may make your skin more susceptible to sunburn and other adverse effects of the sun, so unprotected exposure to natural or artificial sunlight should be minimized.
Laboratory findings: When laboratory mice are exposed to artificial sunlight, they often develop skin tumors. These sunlight-induced tumors may appear more quickly and in greater number if the mouse is also topically treated with the active ingredient in tretinoin cream, tretinoin. In some studies, under different conditions, however, when mice treated with tretinoin were exposed to artificial sunlight, the incidence and rate of development of skin tumors were reduced. There is no evidence to date that tretinoin alone will cause the development of skin tumors in either laboratory animals or humans. However, investigations in this area are continuing.
Use caution in the sun: When outside, even on hazy days, areas treated with tretinoin cream should be protected. An effective sunscreen should be used any time you are outside (consult your physician for a recommendation of an SPF level which will provide you with the necessary high level of protection). For extended sun exposure, protective clothing, like a hat, should be worn. Do not use artificial sunlamps while you are using tretinoin cream, 0.025%. If you do become sunburned, stop your therapy with tretinoin cream until your skin has recovered.
Avoid excessive exposure to wind or cold: Extremes of climate tend to dry or burn normal skin. Skin treated with tretinoin cream may be more vulnerable to these extremes. Your physician can recommend ways to manage your acne treatment under such conditions.
Possible problems: The skin of certain sensitive individuals may become excessively red, swollen, blistered, or crusted. If you are experiencing severe or persistent irritation, discontinue the use of tretinoin cream and consult your physician.
There have been reports that, in some patients, areas treated with tretinoin cream developed a temporary increase or decrease in the amount of skin pigment (color) present.
Use other medication only on your physician’s advice: Only your physician knows which other medications may be helpful during treatment and will recommend them to you if necessary. Follow the physician’s instructions carefully. In addition, you should avoid preparations that may dry or irritate your skin. These preparations may include certain astringents, toiletries containing alcohol, spices or lime, or certain medicated soaps, shampoos, and hair permanent solutions. Do not allow anyone else to use this medication.
Do not use other medications with tretinoin cream which are not recommended by your doctor. The medications you have used in the past might cause unnecessary redness or peeling.
If you are pregnant, think you are pregnant, or are nursing an infant: No studies have been conducted in humans to establish the safety of tretinoin cream in pregnant women. If you are pregnant, think you are pregnant, or are nursing a baby, consult your physician before using this medication.
AND WHILE YOU’RE ON TRETINOIN THERAPY
Use a mild non-medicated soap. Avoid frequent washings and harsh scrubbing. Acne isn’t caused by dirt, so no matter how hard you scrub, you can’t wash it away. Washing too frequently or scrubbing too roughly may at times actually make your acne worse. Wash your skin gently with a mild, bland soap. Two or three times a day should be sufficient. Pat skin dry with a towel. Let the face dry 20 to 30 minutes before applying tretinoin cream, 0.025%. Remember, excessive irritation such as rubbing, too much washing, use of other medications not suggested by your physician, etc., may worsen your acne.
HOW TO USE TRETINOIN CREAM
To get the best results with tretinoin cream therapy, it is necessary to use it properly. Forget about the instructions given for other products and the advice of friends. Just stick to the special plan your doctor has laid out for you and be patient. Remember, when tretinoin cream is used properly, many users see improvement by 12 weeks.
AGAIN, FOLLOW INSTRUCTIONS - BE PATIENT - DON’T START AND STOP THERAPY ON YOUR OWN - IF YOU HAVE QUESTIONS, ASK YOUR DOCTOR.
To help you use the medication correctly, keep these simple instructions in mind.
- Tretinoin cream should be applied once a day, in the evening, or as directed by your physician, to the skin where acne lesions appear, using enough to cover the entire affected area lightly. First, wash with a mild soap and dry your skin gently. WAIT 20 to 30 MINUTES BEFORE APPLYING MEDICATION; it is important for skin to be completely dry in order to minimize possible irritation.
- It is better not to use more than the amount suggested by your physician or to apply more frequently than instructed. Too much may irritate the skin, waste medication, and won’t give faster or better results.
- Keep the medication away from the corners of the nose, mouth, eyes, and open wounds. Spread away from these areas when applying.
- Cream: Squeeze about a half inch or less of medication onto the fingertip. While that should be enough for your whole face, after you have had some experience with the medication you may find you need slightly more or less to do the job. The medication should become invisible almost immediately. If it is still visible, you are using too much. Cover the affected area lightly with tretinoin cream by first dabbing it on your forehead, chin, and both cheeks, then spreading it over the entire affected area. Smooth gently into the skin.
- If needed, you may apply a moisturizer or a moisturizer with sunscreen that will not aggravate your acne (noncomedogenic) in the morning after you wash.
WHAT TO EXPECT WITH YOUR NEW TREATMENT
Tretinoin cream, 0.025% works deep inside your skin and this takes time. You cannot make tretinoin cream work any faster by applying more than one dose each day, but an excess amount of tretinoin cream may irritate your skin. Be patient.
There may be some discomfort or peeling during the early days of treatment. Some patients also notice that their skin begins to take on a blush.
These reactions do not happen to everyone. If they do, it is just your skin adjusting to tretinoin cream and this usually subsides within two to four weeks. These reactions can usually be minimized by following instructions carefully. Should the effects become excessively troublesome, consult your doctor.
BY THREE TO SIX WEEKS, some patients notice an appearance of new blemishes (papules and pustules). At this stage, it is important to continue using tretinoin cream.
If tretinoin cream is going to have a beneficial effect for you, you should notice an improvement in your appearance by 6 to 12 weeks of therapy. Don’t be discouraged if you see no immediate improvement. Don’t stop treatment at the first signs of improvement.
Once your acne is under control, you should continue regular application of tretinoin cream until your physician instructs otherwise.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Manufactured by:
Actavis Mid Atlantic LLC
1877 Kawai Road
Lincolnton, NC 28092 USA
FORM NO. 0117
Rev. 9/13
VC4135
TretinoinTretinoin CREAM
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||