Trifluridine
Trifluridine Ophthalmic Solution, 1% Sterile
FULL PRESCRIBING INFORMATION: CONTENTS*
- TRIFLURIDINE DESCRIPTION
- CLINICAL PHARMACOLOGY
- TRIFLURIDINE INDICATIONS AND USAGE
- TRIFLURIDINE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- TRIFLURIDINE ADVERSE REACTIONS
- OVERDOSAGE
- TRIFLURIDINE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- ANIMAL PHARMACOLOGY AND ANIMAL TOXICOLOGY
- PRINCIPAL DISPLAY PANEL - 7.5 mL Bottle Label
- PRINCIPAL DISPLAY PANEL - 7.5 mL Bottle Carton
FULL PRESCRIBING INFORMATION
TRIFLURIDINE DESCRIPTION
Trifluridine (also known as trifluorothymidine, F3TdR,F3T), is an antiviral drug for topical treatment of epithelial keratitis caused by herpes simplex virus. The chemical name of trifluridine is α,α,α -trifluorothymidine; it has the following structural formula:

Trifluridine sterile ophthalmic solution contains 1% trifluridine in an aqueous solution with acetic acid and sodium acetate (buffers), sodium chloride, and thimerosal 0.001% (added as a preservative). The pH range is 5.5 to 6.0 and osmolality is approximately 283 mOsm.
CLINICAL PHARMACOLOGY
Trifluridine is a fluorinated pyrimidine nucleoside with in vitro and in vivo activity against herpes simplex virus, types 1 and 2 and vacciniavirus. Some strains of adenovirus are also inhibited in vitro.
Trifluridine Ophthalmic Solution, 1% is also effective in the treatment of epithelial keratitis that has not responded clinically to the topical administration of idoxuridine or when ocular toxicity or hypersensitivity to idoxuridine has occurred. In a smaller number of patients found to be resistant to topical vidarabine, Trifluridine Ophthalmic Solution, 1% was also effective.
Trifluridine interferes with DNA synthesis in cultured mammalian cells. However, its antiviral mechanism of action is not completely known.
In vitro perfusion studies on excised rabbit corneas have shown that trifluridine penetrates the intact cornea as evidenced by recovery of parental drug and its major metabolite, 5-carboxy-2'-deoxyuridine, on the endothelial side of the cornea. Absence of the corneal epithelium enhances the penetration of trifluridine approximately two-fold.
Intraocular penetration of trifluridine occurs after topical instillation of Trifluridine Ophthalmic Solution, 1% into human eyes. Decreased corneal integrity or stromal or uveal inflammation may enhance the penetration of trifluridine into the aqueous humor. Unlike the results of ocular penetration of trifluridine in vitro, 5-carboxy-2'-deoxyuridine was not found in detectable concentrations within the aqueous humor of the human eye.
Systemic absorption of trifluridine following therapeutic dosing with Trifluridine Ophthalmic Solution, 1% appears to be negligible. No detectable concentrations of trifluridine or 5-carboxy-2'-deoxyuridine were found in the sera of adult healthy normal subjects who had Trifluridine Ophthalmic Solution, 1% instilled into their eyes seven times daily for 14 consecutive days.
Clinical Studies
During a controlled multicenter clinical trial, 92 of 97 (95%) patients (78 of 81 with dendritic and 14 of 16 with geographic ulcers) responded to therapy with Trifluridine Ophthalmic Solution, 1% as evidenced by complete corneal re-epithelialization within the 14-day therapy period. Fifty-six of 75 (75%) patients (49 of 58 with dendritic and 7 of 17 with geographic ulcers) responded to idoxuridine therapy. The mean time to corneal re-epithelialization for dendritic ulcers (6 days) and geographic ulcers (7 days) was similar for both therapies.
In other clinical studies, Trifluridine Ophthalmic Solution, 1% was evaluated in the treatment of herpes simplex virus keratitis in patients who were unresponsive or intolerant to the topical administration of idoxuridine or vidarabine. Trifluridine Ophthalmic Solution, 1% was effective in 138 of 150 (92%) patients (109 of 114 with dendritic and 29 of 36 with geographic ulcers) as evidenced by corneal re-epithelialization. The mean time to corneal re-epithelialization was 6 days for patients with dendritic ulcers and 12 days for patients with geographic ulcers.
The clinical efficacy of Trifluridine Ophthalmic Solution, 1% in the treatment of stromal keratitis and uveitis due to herpes simplex virus or ophthalmic infections caused by vacciniavirus and adenovirus has not been established by well-controlled clinical trials. Trifluridine Ophthalmic Solution, 1% has not been shown to be effective in the prophylaxis of herpes simplex virus keratoconjunctivitis and epithelial keratitis by well-controlled clinical trials. Trifluridine Ophthalmic Solution, 1% is not effective against bacterial, fungal, or chlamydial infections of the cornea or nonviral trophic lesions.
TRIFLURIDINE INDICATIONS AND USAGE
Trifluridine Ophthalmic Solution, 1% (trifluridine ophthalmic solution) is indicated for the treatment of primary keratoconjunctivitis and recurrent epithelial keratitis due to herpes simplex virus, types 1 and 2.
TRIFLURIDINE CONTRAINDICATIONS
Trifluridine Ophthalmic Solution, 1% is contraindicated for patients who develop hypersensitivity reactions or chemical intolerance to trifluridine.
WARNINGS
The recommended dosage and frequency of administration should not be exceeded (see DOSAGE AND ADMINISTRATION ).
PRECAUTIONS
General
Trifluridine Ophthalmic Solution, 1% should be prescribed only for patients who have a clinical diagnosis of herpetic keratitis.
Trifluridine Ophthalmic Solution, 1% may cause mild local irritation of the conjunctiva and cornea when instilled, but these effects are usually transient.
Although documented in vitro viral resistance to trifluridine has not been reported following multiple exposures to Trifluridine Ophthalmic Solution, 1% , the possibility of the development of viral resistance exists.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenic Potential
Trifluridine has been shown to exert mutagenic, DNA-damaging and cell-transforming activities in various standard in vitro test systems, and clastogenic activity in Vicia faba cells. It did not induce chromosome aberrations in bone marrow cells of male or female rats following a single subcutaneous dose of 100 mg/kg, but was weakly positive in female, but not in male, rats following daily subcutaneous administration at 700 mg/kg/day for 5 days.
Although the significance of these test results is not clear or fully understood, there exists the possibility that mutagenic agents may cause genetic damage in humans.
Oncogenic Potential
Lifetime carcinogenicity bioassays in rats and mice given daily subcutaneous doses of trifluridine have been performed. Rats tested at 1.5, 7.5, and 15 mg/kg/day had increased incidences of adenocarcinomas of the intestinal tract and mammary glands, hemangiosarcomas of the spleen and liver, carcinosarcomas of the prostate gland, and granulosa-thecal cell tumors of the ovary. Mice were tested at 1, 5, and 10 mg/kg/day; those given 10 mg/kg/day trifluridine had significantly increased incidences of adenocarcinomas of the intestinal tract and uterus. Those given 10 mg/kg/day also had a significantly increased incidence of testicular atrophy as compared to vehicle control mice.
Pregnancy
Teratogenic Effects
Pregnancy Category C
Trifluridine was not teratogenic at doses up to 5 mg/kg/day (23 times the estimated human exposure) when given subcutaneously to rats and rabbits. However, fetal toxicity consisting of delayed ossification of portions of the skeleton occurred at dose levels of 2.5 and 5 mg/kg/day in rats and at 2.5 mg/kg/day in rabbits. In addition, both 2.5 and 5 mg/kg/day produced fetal death and resorption in rabbits. In both rats and rabbits, 1 mg/kg/day (5 times the estimated human exposure) was a no-effect level. There were no teratogenic or fetotoxic effects after topical application of Trifluridine Ophthalmic Solution, 1% (approximately 5 times the estimated human exposure) to the eyes of rabbits on the 6th through the 18th days of pregnancy. In a non-standard test, trifluridine solution has been shown to be teratogenic when injected directly into the yolk sac of chicken eggs. There are no adequate and well-controlled studies in pregnant women. Trifluridine Ophthalmic Solution, 1% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is unlikely that trifluridine is excreted in human milk after ophthalmic instillation of Trifluridine Ophthalmic Solution, 1% because of the relatively small dosage (≤5 mg/day), its dilution in body fluids and its extremely short half-life (approximately 12 minutes). The drug should not be prescribed for nursing mothers unless the potential benefits outweigh the potential risks.
Pediatric Use
Safety and effectiveness in pediatric patients below six years of age have not been established.
Geriatric Use
No overall clinical differences in safety or effectiveness have been observed between elderly and other adult patients.
TRIFLURIDINE ADVERSE REACTIONS
The most frequent adverse reactions reported during controlled clinical trials were mild, transient burning or stinging upon instillation (4.6%) and palpebral edema (2.8%). Other adverse reactions in decreasing order of reported frequency were superficial punctate keratopathy, epithelial keratopathy, hypersensitivity reaction, stromal edema, irritation, keratitis sicca, hyperemia, and increased intraocular pressure.
OVERDOSAGE
Overdosage by ocular instillation is unlikely because any excess solution should be quickly expelled from the conjunctival sac.
Acute overdosage by accidental oral ingestion of Trifluridine Ophthalmic Solution, 1% has not occurred. However, should such ingestion occur, the 75 mg dosage of trifluridine in a 7.5 mL bottle of Trifluridine Ophthalmic Solution, 1% is not likely to produce adverse effects. Single intravenous doses of 1.5 to 30 mg/kg/day in children and adults with neoplastic disease produce reversible bone marrow depression as the only potentially serious toxic effect and only after three to five courses of therapy. The acute oral LD50 in the mouse and rat was 4379 mg/kg or higher.
TRIFLURIDINE DOSAGE AND ADMINISTRATION
Instill one drop of Trifluridine Ophthalmic Solution, 1% onto the cornea of the affected eye every 2 hours while awake for a maximum daily dosage of nine drops until the corneal ulcer has completely re-epithelialized. Following re-epithelialization, treatment for an additional 7 days of one drop every 4 hours while awake for a minimum daily dosage of five drops is recommended.
If there are no signs of improvement after 7 days of therapy or complete re-epithelialization has not occurred after 14 days of therapy, other forms of therapy should be considered. Continuous administration of Trifluridine Ophthalmic Solution, 1% for periods exceeding 21 days should be avoided because of potential ocular toxicity.
HOW SUPPLIED
Trifluridine Ophthalmic Solution, 1% is supplied as a sterile ophthalmic solution in a plastic Drop Dose® dispenser bottle of 7.5 mL (NDC 59762-0040-1).
Store under refrigeration 2° to 8°C (36° to 46°F).
ANIMAL PHARMACOLOGY AND ANIMAL TOXICOLOGY
Corneal wound healing studies in rabbits showed that Trifluridine Ophthalmic Solution, 1% did not significantly retard closure of epithelial wounds. However, mild toxic changes such as intracellular edema of the basal cell layer, mild thinning of the overlying epithelium and reduced strength of stromal wounds were observed.
Whereas instillation of Trifluridine Ophthalmic Solution, 1% into rabbit eyes during a subchronic toxicity study produced some degree of corneal epithelial thinning, a 12-month chronic toxicity study in rabbits in which Trifluridine Ophthalmic Solution, 1% was instilled into eyes in intermittent, multiple, full-therapy courses showed no drug-related changes in the cornea.
Rx Only.

LAB-0596-1.0
February 2012
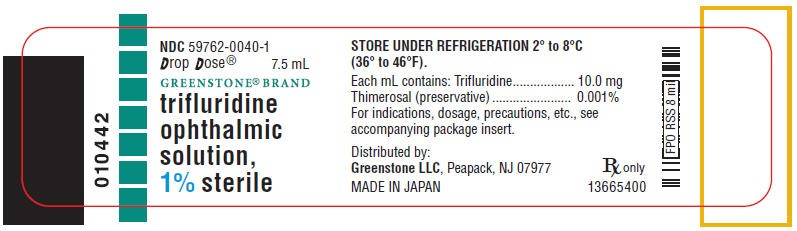
PRINCIPAL DISPLAY PANEL - 7.5 mL Bottle Label
NDC 59762-0040-1
Drop Dose®
7.5 mL
GREENSTONE ® BRAND
trifluridine
ophthalmic
solution,
1% sterile
PRINCIPAL DISPLAY PANEL - 7.5 mL Bottle Carton
NDC 59762-0040-1
Drop Dose®
7.5 mL
GREENSTONE ® BRAND
trifluridine ophthalmic solution,
1% sterile
Rx only

TrifluridineTRIFLURIDINE SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||