Trimethobenzamide Hydrochloride
GAVIS Pharmaceuticals, LLC
GAVIS Pharmaceuticals, LLC
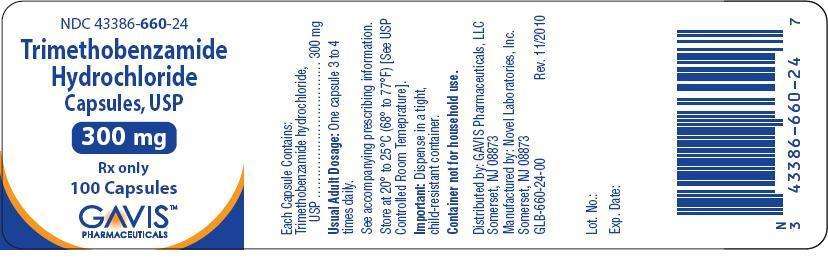
Trimethobenzamide Hydrochloride Capsules, USP Gavis Pharmaceuticals, LLC Rx only
FULL PRESCRIBING INFORMATION
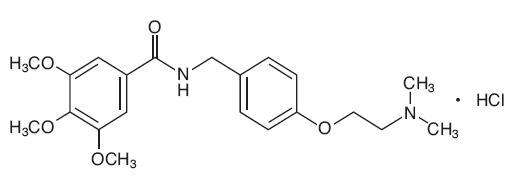
Chemically, trimethobenzamide hydrochloride is N-[ρ -[2-(dimethylamino)ethoxy]benzyl]-
3,4,5-trimethoxybenzamide monohydrochloride. It has a molecular weight of 424.92 and the following structural formula:
Each capsule for oral use contains trimethobenzamide hydrochloride equivalent to 300 mg.
Inactive Ingredients: Lactose monohydrate, magnesium stearate and pregelatinized starch. The capsule shell contains the following ingredients: D&C Red #28, FD&C Blue #1, FD&C Red #40, gelatin and titanium dioxide.
White ink contains the following ingredients: 2-ethoxyethanol, industrial methylated spirit, lecithin, purified water, shellac glaze, simethicone emulsion and titanium dioxide.
Mechanism of Action
The mechanism of action of trimethobenzamide hydrochloride as determined in animals is obscure, but may involve the chemoreceptor trigger zone (CTZ), an area in the medulla oblongata through which emetic impulses are conveyed to the vomiting center; direct impulses to the vomiting center apparently are not similarly inhibited. In dogs pretreated with trimethobenzamide hydrochloride, the emetic response to apomorphine is inhibited, while little or no protection is afforded against emesis induced by intragastric copper sulfate.
Pharmacokinetics
The pharmacokinetics of trimethobenzamide have been studied in healthy adult subjects. Following administration of 200 mg (100 mg/mL) trimethobenzamide I.M. injection, the time to reach maximum plasma concentration (Tmax) was about half an hour, about 15 minutes longer for trimethobenzamide 300 mg oral capsule than an I.M. injection. A single dose of trimethobenzamide 300 mg oral capsule provided a plasma concentration profile of trimethobenzamide similar to trimethobenzamide 200 mg I.M. The relative bioavailability of the capsule formulation compared to the solution is 100%. The mean elimination half-life of trimethobenzamide is 7 to 9 hours. Between 30 – 50 % of a single dose in humans is excreted unchanged in the urine within 48 – 72 hours. The major pathway of trimethobenzamide metabolism is through oxidation resulting in the formation of trimethobenzamide N-oxide metabolite. The pharmacologic activity of this major metabolite has not been evaluated.
Special Populations
Age
The clearance of trimethobenzamide is not known in patients with renal impairment. However, it may be advisable to consider reduction in the dosing of trimethobenzamide in elderly patients with renal impairment considering that a substantial amount of excretion and elimination of trimethobenzamide occurs via the kidney and that elderly patients may have various degrees of renal impairment. (See PRECAUTIONS: General and DOSAGE AND ADMINISTRATION).
Gender
Systemic exposure to trimethobenzamide was similar between men (N=40) and women (N=28).
Race
Pharmacokinetics appeared to be similar for Caucasians (N=53) and African Americans (N=12).
Renal Impairment
The clearance of trimethobenzamide is not known in patients with renal impairment. However, it may be advisable to consider reduction in the dosing of trimethobenzamide in patients with renal impairment considering that a substantial amount of excretion and elimination of trimethobenzamide occurs via the kidney. (See PRECAUTIONS: General and DOSAGE AND ADMNISTRATION).
Trimethobenzamide Hydrochloride Capsule, USP 300 mg is indicated for the treatment of postoperative nausea and vomiting and for nausea associated with gastroenteritis.
Use of any dosage forms in patients with known hypersensitivity to trimethobenzamide is contraindicated.
Caution should be exercised when administering trimethobenzamide hydrochloride capsules to children for the treatment of vomiting. Antiemetics are not recommended for treatment of uncomplicated vomiting in children and their use should be limited to prolonged vomiting of known etiology. There are two principal reasons for caution:
1. The extrapyramidal symptoms which can occur secondary to trimethobenzamide hydrochloride capsules may be confused with the central nervous system signs of an undiagnosed primary disease responsible for the vomiting, e.g., Reye’s syndrome or other encephalopathy.
2. It has been suspected that drugs with hepatotoxic potential, such as trimethobenzamide hydrochloride capsules, may unfavorably alter the course of Reye’s syndrome. Such drugs should therefore be avoided in children whose signs and symptoms (vomiting) could represent Reye’s syndrome.
Trimethobenzamide hydrochloride capsules may produce drowsiness. Patients should not operate motor vehicles or other dangerous machinery until their individual responses have been determined.
Usage in Pregnancy: Trimethobenzamide hydrochloride was studied in reproduction experiments in rats and rabbits and no teratogenicity was suggested. The only effects observed were an increased percentage of embryonic resorptions or stillborn pups in rats administered 20 mg and 100 mg/kg and increased resorptions in rabbits receiving 100 mg/kg. In each study these adverse effects were attributed to one or two dams. The relevance to humans is not known. Since there is no adequate experience in pregnant or lactating women who have received this drug, safety in pregnancy or in nursing mothers has not been established.
Usage with Alcohol: Concomitant use of alcohol with trimethobenzamide hydrochloride capsules may result in an adverse drug interaction.
During the course of acute febrile illness, encephalitides, gastroenteritis, dehydration and electrolyte imbalance, especially in children and the elderly or debilitated, CNS reactions such as opisthotonos, convulsions, coma and extrapyramidal symptoms have been reported with and without use of trimethobenzamide hydrochloride capsules or other antiemetic agents. In such disorders caution should be exercised in administering trimethobenzamide hydrochloride capsules, particularly to patients who have recently received other CNS acting agents (phenothiazines, barbiturates, belladonna derivatives). Primary emphasis should be directed toward the restoration of body fluids and electrolyte balance, the relief of fever and relief of the causative disease process. Overhydration should be avoided since it may result in cerebral edema.
The antiemetic effects of trimethobenzamide hydrochloride capsules may render diagnosis more difficult in such conditions as appendicitis and obscure signs of toxicity due to overdosage of other drugs.
Adjustment of Dose in Renal Failure
A substantial route of elimination of unchanged trimethobenzamide is via the kidney. Dosage adjustment should be considered in patients with reduced renal function including some elderly patients. (See CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
Clinical studies of trimethobenzamide hydrochloride did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. Although there are studies reported in the literature that included elderly patients >65 years old with younger patients, it is not known if there are differences in efficacy or safety parameters for elderly and non-elderly patients treated with trimethobenzamide. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function. (See CLINCAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
There have been reports of hypersensitivity reactions and Parkinson-like symptoms. There have been instances of hypotension reported following parenteral administration to surgical patients. There have been reports of blood dyscrasias, blurring of vision, coma, convulsions, depression of mood, diarrhea, disorientation, dizziness, drowsiness, headache, jaundice, muscle cramps and opisthotonos. If these occur, the administration of the drug should be discontinued. Allergic-type skin reactions have been observed; therefore, the drug should be discontinued at the first sign of sensitization. While these symptoms will usually disappear spontaneously, symptomatic treatment may be indicated in some cases.
(See WARNINGS and PRECAUTIONS.)
Dosage should be adjusted according to the indication for therapy, severity of symptoms and the response of the patient.
Geriatric Patients
Dose adjustment such as reducing the total dose administered at each dosing or increasing the dosing interval should be considered in elderly patients with renal impairment (creatinine clearance ≤ 70 mL/min/1.73m2). Final dose adjustment should be based upon integration of clinical efficacy and safety considerations. (See CLINICAL PHARMACOLOGY and PRECAUTIONS).
Patients and Renal Impairment
In subjects with renal impairment (creatinine clearance ≤ 70 mL/min/1.73m2), dose adjustment such as reducing the total dose administered at each dosing or increasing the dosing interval should be considered. (See CLINICAL PHARMACOLOGY and PRECAUTIONS).
Usual Adult Dosage: One 300 mg capsule 3 or 4 times daily.
STORAGE
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Trimethobenzamide Hydrochloride Capsules, USP 300 mg are filled gelatin capsules size 1 lavender opaque cap/lavender opaque body with a white imprint "Novel 660" on cap and “300 mg” on body.
Available in bottles of 30’s, 100’s and 500’s.
Bottles of 30 capsules: 43386-660-03
Bottles of 100 capsules: 43386-660-24
Bottles of 500 capsules: 43386-660-26
Manufactured by:
Novel Laboratories, Inc.
Somerset, NJ 08873
Distributed by
GAVIS Pharmaceuticals, LLC
Somerset, NJ 08873

Trimethobenzamide HydrochlorideTrimethobenzamide Hydrochloride CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||